Professional Documents
Culture Documents
Drug Study
Uploaded by
Diana Laura LeiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Study
Uploaded by
Diana Laura LeiCopyright:
Available Formats
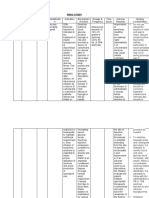
Drug Study Functional Classification: Chemical Class: Generic Name: Brand Name: Mechanism of Action: Contraindications: Usual Dose:
Antimicrobial Fluoroquinolones ciprofloxacin Ciprobay Inhibits DNA-gyrase in susceptible organism; inhibits relaxation o f supercoiled DNA and promotes breakage of double-stranded DNA. hyper sensitivity to ciprofloxacin or other quinolo nes. Children, adolescents, pregnancy and lactation. Tab 125-750 mg orally bid. Respiratory tract infections 500 mg bid. Acute gonorrhea 250mg orally as single dose. The normal dose must be reduced if creatinine clearance is <20 ml/min. 500 XR tab acute uncomplicated UTI (acute cystitis) 1 tab/day for 3 days IVinfusion 100-200 mg bid. Resp tract infections 200-400 mg bid. Acute, uncomplicatedU T I a n d e x t r a genital gonorrhea 100 mg bid. Pre -menopausal cystitis and a c u t e , uncomplicated gonorrhea single dose 100 mg. Complicated cystitis and diarrhea 200 mg bid. Severe infections 400 mg tid. Tablet (Film- coated) - 250mg, 500mg, 750mg; IV infusion- 100mg/ 50mL,200mg/ 100mL, 400mg/ 200mL nausea, vomiting, dizziness or drowsiness;blurred vision;feeling nervous, anxious, or agitated; or sleep problems (insomnia or nightmares). CNS: seizures, dizziness, dro wsiness, headache, inso mnia, acute psychosis, agitatio n, confusion, hallucination, increased intracranial pressure, light-headedness, tremorsCV: arrythmias, QT prolongation, vasodilationGI: hepatotoxicity, pseudomembranous colitis, abdominal pain, diarrhea, nausea, alteredtaste. GU: interstitial cystitis, vaginitis. Derm: photosensitivity, phototoxicityEndo: hyperglycemia, hypoglycemia. Local: phlebitis at IV siteMS: tendonitis, tendon ruptureMisc: hyp ersensitivity rea ctions including anap hylaxis, Stevens - Johnson syndro me, lymphadenopathy N/A Assess patient for infection prior to and during therapy. Obtain specimens for culture and sensitivity before initiating therapy Observe patient for signs and symp to ms of anap hylaxis (rash, pruritus, lar yngealedema, wheezing) Monitor prothrombin time closely in patients receiving f l u o r o q u i n o l o n e s a n d warfarin
Dosage Form: Side Effects: Adverse Effects:
Drug Interaction: Nursing Considerations:
Drug Study Functional Classification: Chemical Class: Generic Name: Brand Name: Mechanism of Action: Anti-tubercolosis isioniazid Pyrazinamide/rifampicin/ethambutol HCl/INH Myrin-P Forte The mechanism of action of ethambutol is not fully known. It diffuses into mycobacteria and appears to suppress multiplication by interfering with RNA synthesis. It is effective only against mycobacteria that are actively dividing. Rifampicin inhibits bacterial RNA synthesis by bonding strongly to the -subunit of DNA-dependent RNA polymerase, preventing the attachment of the enzyme to DNA and thus, blocking initiation of RNA transcription.Isoniazid is a bactericidal antitubercular agent, which is active against actively dividing mycobacteria, and its mode of action may relate to inhibition of mycolic acid synthesis and the disruption of the cell wall in susceptible organisms.The mechanism of action of pyrazinamide is unknown. Pyrazinamide may be bacteriostatic or bactericidal depending on its concentration and the susceptibility of the organism. Known hypersensitivity to ethambutol, isoniazid, rifampicin or pyrazinamide, or to any of the excipients of Myrin/Myrin-P Forte. In the presence of alcoholism, optic neuritis, impaired hepatic function and severe renal insufficiency, hyperuricemia and/or gouty arthritis, in the presence of jaundice, or in patients with known retrobulbar neuritis unless the doctor determines that it may be used. Patients who are unable to appreciate and report visual side effects or changes in vision (eg, young children and patients with mental illness or mental deficiency). Pyrazinamide: Patients with severe hepatic damage; on concomitant therapy with rifampicin who
Contraindications:
Usual Dose:
Dosage Form: Side Effects: Adverse Effects:
are concurrently taking other medications associated with liver injury, drink excessive amounts of alcohol (even if alcohol use is discontinued during treatment), have underlying liver disease, or have a history of isoniazid associated liver injury. WHO guidelines indicate that Myrin-P Forte should be given daily during the initial phase treatment of Category I and II patients with the dose adjusted according to body weight, as follows: Patients Weighing >71 kg: 5 tablets; 55-70 kg: 4 tablets; 40-54 kg: 3 tablets. Tablet Nausea, vomiting and loss of appetite. Blood and Lymphatic System Disorders: Leukopenia, thrombocytopenia, neutropenia. Immune System Disorders: Anaphylactic/anaphylactoid reaction (including shock and fatalities). Hypersensitivities syndrome consisting of cutaneous reaction (eg, rash or exfoliative dermatitis), eosinophilia, and 1 or more of the following: Hepatitis, pneumonitis, nephritis, myocarditis, and pericarditis. Fever and lymphadenopathy may be present. Metabolism and Nutrition Disorders: Anorexia, elevations of serum uric acid concentration. Nervous System Disorders: Dizziness, hypoesthesia, paresthesia. Eye Disorders: Ethambutol may produce decreases in visual acuity including irreversible blindness, which appear to be due to optic neuritis. This effect may be related to dose and duration of treatment, and patients receiving ethambutol for prolonged periods at doses >20 mg/kg have an increased risk of developing optic neuritis. Ethambutol: Concurrent administration of ethambutol with other neurotoxic medicines may increase the potential for neurotoxicity Antacids containing aluminum hydroxide have impaired the absorption of ethambutol. Ethambutol may react with phentolamine (Rogitine) to elicit a falsepositive test for pheochromocytoma. Rifampicin: Rifampicin has been observed to decrease the anticoagulant effect of coumarin-type drugs. Rifampicin may increase the metabolism of the following medicines by induction of hepatic microsomal enzymes, resulting in lower serum concentrations: Aminophylline, theophylline, sulphonylurea oral antidiabetic agents, phenobarbital, systemic -adrenergic blocking agents, chloramphenicol, clofibrate, corticosteroids, cyclosporin, dapsone, diazepam, digitalis glycosides, disopyramide, mexiletine, quinidine, tocainide, estramustine, fluconazole, methadone, phenytoin, trimethoprim, oral verapamil. Explain to patient to expect an orange urine and Monitor I & O
Drug Interaction:
Nursing Considerations:
Drug Study Functional Classification: Chemical Class: Generic Name: Brand Name: Mechanism of Action: Antimicrobial Sulfonamides cotrimoxazole Sulfamethoxazole inhibits bacterial synthesis of dihydrofolic acid by competing with PABA. Trimethoprim blocks production of tetrahydrofolic acid by inhibiting the enzyme dihydrofolate reductase. This combination blocks 2 consecutive steps in bacterial biosynthesis of essential nucleic acids and proteins and is usually bactericidal. 960mg twice daily tablet or powder suspension or suspension Tablet, Suspension and Powder for suspension Nausea, vomiting and loss of appetite. Blood - Decrease in blood cell counts. Allergic - Skin inflammation, eruptions, rash, itching, redness, hives, bruising and photosensitivity. Gastrointestinal - Liver inflammation/damage, jaundice, hepatic necrosis, elevation in liver enzymes, inflammation of intestine/pancreas/tongue, mouth ulcer, abdominal pain and diarrhea. Genitourinary - Kidney failure, Blood Urea Nitrogen and absence of urination. Central Nervous System - Brain inflammation, convulsions, incoordination, fainting, ringing in the ear, headache, hallucinations, depression and nervousness. Metabolic - Low blood sugar. Musculoskeletal - Joint/muscle pain. Respiratory - Cough, shortness of breath and lung infection. Miscellaneous - Weakness, fatigue and sleeplessness.
Usual Dose: Dosage Form: Side Effects: Adverse Effects:
Drug Interaction: Nursing Considerations:
N/A Maintain adequate fluid intake to prevent crystalluria; infuse I.V. co-trimoxazole over 60-90 minutes; must be further diluted 1:25 (5 mL drug to 125 mL diluent, ie, D5W); in patients who require fluid restriction, a 1:15 dilution (5 mL drug to 75 mL diluent, ie, D 5W) or a 1:10 dilution (5 mL drug to 50 mL diluent, ie, D5W) can be administered Monitor CBC, renal function test, liver function test, urinalysis
Drug Study Functional Classification: Chemical Class: Generic Name: Brand Name: Mechanism of Action: Usual Dose: Dosage Form: Side Effects: Adverse Effects: Antiviral Purine analogues aciclovir Herpex Acyclovir interferes with viral DNA synthesis. Thus, it inhibits viral replication, decreased viral shedding and reduces time for healing of lesions. 960mg twice daily tablet or powder suspension or suspension Tablet, Suspension and Powder for suspension Nausea, vomiting and loss of appetite. Blood - Decrease in blood cell counts. Allergic - Skin inflammation, eruptions, rash, itching, redness, hives, bruising and photosensitivity. Gastrointestinal - Liver inflammation/damage, jaundice, hepatic necrosis, elevation in liver enzymes, inflammation of intestine/pancreas/tongue, mouth ulcer, abdominal pain and diarrhea. Genitourinary - Kidney failure, Blood Urea Nitrogen and absence of urination. Central Nervous System - Brain inflammation, convulsions, incoordination, fainting, ringing in the ear, headache, hallucinations, depression and nervousness. Metabolic - Low blood sugar. Musculoskeletal - Joint/muscle pain. Respiratory - Cough, shortness of breath and lung infection. Miscellaneous - Weakness, fatigue and sleeplessness. N/A Assess lesions before and daily during therapy. Shake the liquid well before each use to mix the medication evenly. (for suspension preparation) Acyclovir can be taken with or without food with a full glass of water.Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take acyclovir until you finish the prescription, even if you feel better. If you stop taking acyclovir too soon or skip doses, your infection may not be completely treated or may become more difficult to treat. Acyclovir treatment should be started as soon as possible after herpes simplex symptoms appear and within 24 hours of a herpes zoster break. For IV preparations, the infusion site should be observed for phlebitis. The infusion site should be rotated to prevent phlebitis.Watch out for signs of acyclovir overdose which are: Agitation, Seizures, Extreme tiredness, Loss of consciousness, Swelling of the hands, feet, ankles or lower legs Decreased urination
Drug Interaction: Nursing Considerations:
Drug Study
Functional Classification: Chemical Class: Generic Name: Brand Name: Mechanism of Action:
Antimalarial merafloquine Lariam Lariam acts on the asexual intra-erythrocytic forms of the human malaria parasites: Plasmodium falciparum, P. vivax, P. malariae and P. ovale. Lariam is effective against malaria parasites resistant to other antimalarials eg, chloroquine, proguanil, pyrimethamine and pyrimethaminesulfonamide combinations. Resistance of P. falciparum to mefloquine has been reported, predominantly in areas of multi-drug resistance in Southeast Asia. Cross-resistance between mefloquine and halofantrine and cross-resistance between mefloquine and quinine have been
Contraindications:
Usual Dose:
Dosage Form: Side Effects:
Adverse Effects:
Drug Interaction:
Nursing Considerations:
observed in some regions. Known hypersensitivity to mefloquine or related compounds (eg, quinine and quinidine) or to any of the excipients of Lariam. Not to be prescribed for prophylaxis in persons with active depression or with a history of psychosis or convulsions. Standard Dosage: The recommended prophylactic dose of Lariam is approximately 5 mg/kg body weight once weekly: >45 kg body weight: 1 tab; 30-45 kg: tab; 20-30 kg: tab; 10-20 kg: tab; 5-10 kg: 1/8 tab Tablet nausea, vomiting, loose stools or diarrhea and abdominal pain, dizziness or vertigo, loss of balance, and neuropsychological adverse events eg, headache, somnolence and sleep disorders (insomnia, abnormal dreams) Neuropsychiatric Disorders: Sensory and motor neuropathies (including paresthesia, tremor and ataxia), convulsions, agitation or restlessness, anxiety, depression, mood changes, panic attacks, forgetfulness, confusion, hallucinations, aggression, psychotic or paranoid reactions. There have been rare reports of suicidal ideations, but no relationship to drug administration has been established.Cardiovascular Disorders: Circulatory disturbances (hypotension, hypertension, flushing, syncope), chest pain, tachycardia or palpitation, bradycardia, irregular pulse, extrasystoles and other transient cardiac conduction alterations.Skin Disorders: Rash, exanthema, erythema, urticaria, pruritus, edema, hair loss.Musculoskeletal Disorders: Muscle weakness and muscle cramps, myalgia, arthralgia. Other Symptoms: Visual disturbances, vestibular disorders including tinnitus and hearing impairment, dyspnea, asthenia, malaise, fatigue, fever, sweating chills, dyspepsia and loss of appetite. Laboratory Abnormalities: Transient elevation of transaminases, leukopenia or leukocytosis, thrombocytopenia. Isolated cases of erythema multiforme, Stevens-Johnson syndrome, AV block, and encephalopathy have been reported. Concomitant administration of Lariam and other related compounds (eg, quinine, quinidine and chloroquine) may produce electrocardiographic abnormalities and increase the risk of convulsions There is evidence that the use of halofantrine after mefloquine causes a significant lengthening of the QTc interval. Clinically significant QTc prolongation has not been found with mefloquine alone. This appears to be the only clinically relevant interaction of this kind with Lariam, although theoretically co-administration of other drugs known to alter cardiac conduction (eg, antiarrhythmic or -adrenergic blocking agents, calcium-channel blockers, antihistamines or H1blocking agents, tricyclic antidepressants and phenothiazines) might also contribute to a prolongation of the QTc interval. There are no data that conclusively establish whether the concomitant administration of mefloquine and the previously mentioned agents has an effect on cardiac function. - Mefloquine doses in the BNF may differ from those in product literature.- Travellers should be informed about adverse reactions and, if they occur, that they should seek medical advice on alternative antimalarials before the next dose is due. - Travel to malarious areas should be avoided during pregnancy; if it is unavoidable, effective prophylaxis must be used but mefloquine should be avoided as a matter of principle. However, studies of mefloquine use in pregnancy (including in the first trimester) indicate that it can be considered for travel to chloroquine-resistant areas. Mefloquine is considered to be appropriate for use by people with renal impairment and does not require dosage reduction. - Warn travellers they should still avoid mosquito bites. - Ensure travellers understand the importance of taking prophylaxis regularly. - Advise travellers to seek urgent medical attention if ill within one year and especially within three months of return. Dizziness or a disturbed sense of balance may affect performance of skilled tasks such as driving. - The patient information leaflet that describes adverse reactions should always be provided with mefloquine. Nurses should refer to manufacturer's summary of product characteristics and to appropriate local guidelines
Drug Study Functional Classification: Chemical Class: Generic Name: Brand Name: Mechanism of Action: Antithelmintic mebendazole Antiox Vermicidal; may also be ovicidal for ova of most helminths; mebendazole causes degeneration of parasite's cytoplasmic microtubules and thereby selectively and irreversibly blocks glucose uptake in susceptible adult intestine-dwelling helminths and their tissue-dwelling larvae; inhibition of glucose uptake apparently results in depletion of the parasite's glycogen stores; this, in turn, results
Usual Dose: Dosage Form: Side Effects:
Adverse Effects:
in reduced formation of adenosine triphosphate (ATP) required for survival and reproduction of the helminth; corresponding energy levels are gradually reduced until death of the parasite ensues; mebendazole does not appear to affect serum glucose concentrations in humans, however. 100 mg taken once. TableT Mebendazole is relatively free of toxic side effects or adverse reactions, although patients may complain of transient abdominal pain, diarrhea, slight headache, fever, dizziness, exanthema, urticaria, and angioedema. Mebendazole is relatively free of toxic side effects or adverse reactions, although patients may complain of transient abdominal pain, diarrhea, slight headache, fever, dizziness, exanthema, urticaria, and angioedema. N/A Assess patients condition before therapy and regularly thereafter to monitor the drugs effectiveness. Be alert for adverse reactions and drug interactions. Assess patients and familys knowledge of drug therapy.Tablets may be chewed, swallowed whole or crushed and mixed with foods. No dietary restrictions, laxatives or enemas are needed.
Drug Interaction: Nursing Considerations:
PENICILLIN CEPHALOSPORIN MACROLIDES TETRACYCLINE FLUOROQUINOLONES SULFONAMIDE ANTI-TB ANTI-MALARIAL ANTITHELMINTIC ANTIHISTAMINE DECONGESTANT ANTITUSSIVE
EXPECTORANT STEROID INHALER MUCOLYTIC ANTI-EMETICS ANTI-DIARRHEALS LAXATIVES ANTACIDS H2 RECEPTOR ANTAGONIST PROTON PUMP INHIBITOR ANTIHYPERTENSIVES ANTICOAGULANT & ANTIPLATELET ANTILIPIDEMICS ANTI-ARRYTHMIA ANTI-ANGINAL HEART FAILURE VITAMINS & MINERALS ANTI-DIABETICS DRUGS DURING LABOR
You might also like
- Stonehell Dungeon 1 Down Night Haunted Halls (LL)Document138 pagesStonehell Dungeon 1 Down Night Haunted Halls (LL)some dude100% (9)
- Drug Study: Davao Doctors College General Malvar ST., Davao City Nursing ProgramDocument3 pagesDrug Study: Davao Doctors College General Malvar ST., Davao City Nursing ProgramJear RomeroNo ratings yet
- Drug Study - HRZEDocument4 pagesDrug Study - HRZEEunice Ordonez67% (3)
- ST3 ManualDocument48 pagesST3 ManualRon FosterNo ratings yet
- Drug StudyDocument3 pagesDrug StudyKwin SaludaresNo ratings yet
- Emergency Drug StudyDocument3 pagesEmergency Drug StudyGrace Santos MirandaNo ratings yet
- ER Drug StudyDocument13 pagesER Drug StudyJaessa FelicianoNo ratings yet
- CiprofloxacinDocument3 pagesCiprofloxacinapi-3797941No ratings yet
- 8 Drug StudyDocument9 pages8 Drug StudyJohn Michael M. RosalesNo ratings yet
- Drug StudyDocument12 pagesDrug StudyIsha Catimbang GenerilloNo ratings yet
- Furosemide ChlorthalidoneDocument5 pagesFurosemide ChlorthalidoneLIEZEL GRACE VELAYONo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Activity-11 - Nursing Care Plan - ICPDocument6 pagesActivity-11 - Nursing Care Plan - ICPCloe CorpuzNo ratings yet
- Succinylcholine ChlorideDocument19 pagesSuccinylcholine ChlorideAgungBudiPamungkas100% (1)
- Triamcinolone (Topical) - Drug InformationDocument5 pagesTriamcinolone (Topical) - Drug InformationMauricio Sv0% (1)
- MinoxidilDocument2 pagesMinoxidilHenna AhmedNo ratings yet
- Anatomy and Physiology of NeonatesDocument17 pagesAnatomy and Physiology of NeonatesYu ShiNo ratings yet
- Drug Study On EPINEPHRINEDocument6 pagesDrug Study On EPINEPHRINEshadow gonzalezNo ratings yet
- Drug Study CellulitsDocument2 pagesDrug Study CellulitsCzarina CullenNo ratings yet
- Med Template - NifedipineDocument2 pagesMed Template - NifedipineAshlee KeeferNo ratings yet
- PrimaquineDocument3 pagesPrimaquineVijayakumar NsNo ratings yet
- Drug Study HeparinDocument2 pagesDrug Study HeparinArianne NicoleNo ratings yet
- Drug Study: Francisco Tampos JRDocument37 pagesDrug Study: Francisco Tampos JRCarlmeister Ambray JudillaNo ratings yet
- CefiximeDocument2 pagesCefiximeapi-4070990100% (2)
- Drug Study 1Document15 pagesDrug Study 1Czarina Isabela TuazonNo ratings yet
- Drug Study NursingDocument27 pagesDrug Study Nursingbilliam123No ratings yet
- Drug Study RivastigmineDocument6 pagesDrug Study RivastigmineRaijenne VersolaNo ratings yet
- NAHCO3Document2 pagesNAHCO3Krizha Angela NicolasNo ratings yet
- CLARITIN Is Indicated For The Relief ofDocument12 pagesCLARITIN Is Indicated For The Relief oflalaineperlascuteNo ratings yet
- Anti Tetanus Serum IDocument2 pagesAnti Tetanus Serum IRobby EffendyNo ratings yet
- Metformin, Glucophage, Glucophage XR, Glumetza, Fortamet, RiometDocument5 pagesMetformin, Glucophage, Glucophage XR, Glumetza, Fortamet, RiometAgronaSlaughterNo ratings yet
- Viii. Pharmacologic Intervention (Drug Study)Document10 pagesViii. Pharmacologic Intervention (Drug Study)Cyril Jane Caanyagan AcutNo ratings yet
- Drug Study....Document5 pagesDrug Study....Maria Jelyn SarmientoNo ratings yet
- Drug Study, NCPDocument8 pagesDrug Study, NCPtintinNo ratings yet
- The Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016Document10 pagesThe Format of This Leaflet Was Determined by The Ministry of Health and Its Content Was Checked and Approved by It On February 2016ddandan_2No ratings yet
- Drug StudyDocument16 pagesDrug StudyMonica Luz FajardoNo ratings yet
- Drug Study..DokcyDocument7 pagesDrug Study..DokcyPeArl Peralta0% (1)
- Generic Name TizanidineDocument3 pagesGeneric Name TizanidinemadamcloudnineNo ratings yet
- PEDIADRUGDocument6 pagesPEDIADRUGPatrice LimNo ratings yet
- 3B Drug Study 2Document23 pages3B Drug Study 2Kristine Dela CruzNo ratings yet
- Atropine: Drug Study: NCM 106 PharmacologyDocument6 pagesAtropine: Drug Study: NCM 106 PharmacologyKevin RosalesNo ratings yet
- Drug StudyDocument2 pagesDrug Studypopoyoio100% (2)
- Haloperidol PDFDocument1 pageHaloperidol PDFAda AlvarezNo ratings yet
- Drug StudyDocument1 pageDrug StudyDanian AntonioNo ratings yet
- Drug Study Pyrantel & CefuroximeDocument2 pagesDrug Study Pyrantel & CefuroximeMikhael Briones ApasNo ratings yet
- Meningitis Pathophysiology PDFDocument59 pagesMeningitis Pathophysiology PDFpaswordnyalupa100% (1)
- MiconazoleDocument3 pagesMiconazoleapi-3797941No ratings yet
- Pregnancy Induced HypertensionDocument25 pagesPregnancy Induced HypertensionPauPauNo ratings yet
- DrugStudy MetoclopramideDocument2 pagesDrugStudy MetoclopramideAshknee Khainna AlejoNo ratings yet
- NizoralDocument4 pagesNizoralianecunar100% (2)
- BumetanideDocument3 pagesBumetanideapi-3797941No ratings yet
- Drug Presentation On: Aminoven: Submitted To Submitted byDocument6 pagesDrug Presentation On: Aminoven: Submitted To Submitted byShilpi SinghNo ratings yet
- Cretenism Case StudyDocument8 pagesCretenism Case StudyMonica Marie MoralesNo ratings yet
- HaemaccelinfDocument9 pagesHaemaccelinfSisca YulistianaNo ratings yet
- Drug StudyDocument7 pagesDrug StudyCharm LorenzoNo ratings yet
- Brand Name: Generic Name: Drug ClassificationDocument2 pagesBrand Name: Generic Name: Drug ClassificationChristine Pialan SalimbagatNo ratings yet
- Burn - Daily Physical AssessmentDocument8 pagesBurn - Daily Physical AssessmentkrishcelNo ratings yet
- Drug Study inDocument3 pagesDrug Study inaycee0316No ratings yet
- ORS Package InsertDocument1 pageORS Package InsertwhothehellisarcticmonkeysNo ratings yet
- Nasogastric FeedingDocument2 pagesNasogastric FeedingShella LaguatanNo ratings yet
- Drug StudyDocument9 pagesDrug Studyjanelee2824No ratings yet
- I Choose JesusDocument1 pageI Choose JesusDiana Laura LeiNo ratings yet
- Product Load CentralDocument17 pagesProduct Load CentralObed AndalisNo ratings yet
- Eng1 5Document2 pagesEng1 5Diana Laura LeiNo ratings yet
- Basic Ethical Principles 1. StewardshipDocument2 pagesBasic Ethical Principles 1. StewardshipDiana Laura LeiNo ratings yet
- The Palawan Chamber Choir, IncDocument1 pageThe Palawan Chamber Choir, IncDiana Laura LeiNo ratings yet
- My Plans For Puerto Princesa CityDocument18 pagesMy Plans For Puerto Princesa CityDiana Laura LeiNo ratings yet
- Chapter 1 - 5 Updated To Past TenseDocument81 pagesChapter 1 - 5 Updated To Past TenseDiana Laura Lei100% (2)
- BioethicsDocument6 pagesBioethicsDiana Laura LeiNo ratings yet
- I Choose JesusDocument1 pageI Choose JesusDiana Laura LeiNo ratings yet
- Four Great River Valley Civilizations-1Document48 pagesFour Great River Valley Civilizations-1Diana Laura LeiNo ratings yet
- PSUS PosterDocument1 pagePSUS PosterDiana Laura LeiNo ratings yet
- UMPDocument2 pagesUMPDiana Laura LeiNo ratings yet
- Basic Ethical Principles 1. StewardshipDocument2 pagesBasic Ethical Principles 1. StewardshipDiana Laura LeiNo ratings yet
- E. The Qualities and Responsibilities of A Good Health Care Provider To The Client, Society and Its Profession Basic Qualities of A Health Care PractitionerDocument3 pagesE. The Qualities and Responsibilities of A Good Health Care Provider To The Client, Society and Its Profession Basic Qualities of A Health Care PractitionerDiana Laura LeiNo ratings yet
- Img 0006Document1 pageImg 0006Diana Laura LeiNo ratings yet
- Invitro FertilizationDocument3 pagesInvitro FertilizationDiana Laura LeiNo ratings yet
- TheologyDocument11 pagesTheologyDiana Laura LeiNo ratings yet
- Fie RVH ") GFR: and Ery: Ti EiDocument1 pageFie RVH ") GFR: and Ery: Ti EiDiana Laura LeiNo ratings yet
- Icp RecruitmentDocument3 pagesIcp RecruitmentDiana Laura LeiNo ratings yet
- ForevermoreDocument2 pagesForevermoreDiana Laura LeiNo ratings yet
- LFDDocument4 pagesLFDDiana Laura LeiNo ratings yet
- Invitation R.A 9173Document5 pagesInvitation R.A 9173Diana Laura LeiNo ratings yet
- 8 Intro MortalityDocument43 pages8 Intro MortalityDiana Laura LeiNo ratings yet
- EthicsDocument2 pagesEthicsDiana Laura LeiNo ratings yet
- The ,.. 3-f 1, ( (Fs G.: Lle TDocument1 pageThe ,.. 3-f 1, ( (Fs G.: Lle TDiana Laura LeiNo ratings yet
- PICDOCDocument15 pagesPICDOCDiana Laura LeiNo ratings yet
- New Emergency Seizure Treatment For Children: Jennifer Warner Brunilda Nazario, MDDocument1 pageNew Emergency Seizure Treatment For Children: Jennifer Warner Brunilda Nazario, MDDiana Laura LeiNo ratings yet
- DiseasesDocument2 pagesDiseasesDiana Laura LeiNo ratings yet
- Process DocumentationDocument3 pagesProcess DocumentationDiana Laura LeiNo ratings yet
- NCP Case StudyDocument6 pagesNCP Case StudyDiana Laura LeiNo ratings yet
- Pedagogy MCQS 03Document54 pagesPedagogy MCQS 03Nawab Ali MalikNo ratings yet
- Honda IzyDocument16 pagesHonda IzyTerry FordNo ratings yet
- SAFE RC Design ForDocument425 pagesSAFE RC Design ForMarlon Braggian Burgos FloresNo ratings yet
- Crisis of The World Split Apart: Solzhenitsyn On The WestDocument52 pagesCrisis of The World Split Apart: Solzhenitsyn On The WestdodnkaNo ratings yet
- Chapter 2.3.3 History of Visual Arts Modernism Post ModernismDocument17 pagesChapter 2.3.3 History of Visual Arts Modernism Post ModernismKim Ashley SarmientoNo ratings yet
- Arts 6 Week 6Document9 pagesArts 6 Week 6JENNEFER ESCALANo ratings yet
- Beyond Models and Metaphors Complexity Theory, Systems Thinking and - Bousquet & CurtisDocument21 pagesBeyond Models and Metaphors Complexity Theory, Systems Thinking and - Bousquet & CurtisEra B. LargisNo ratings yet
- Microwave EngineeringDocument2 pagesMicrowave Engineeringசுந்தர் சின்னையா0% (9)
- Data Network Unit 6 - UCDocument15 pagesData Network Unit 6 - UCANISHA DONDENo ratings yet
- 105 2Document17 pages105 2Diego TobrNo ratings yet
- Manual de Operacion y MantenimientoDocument236 pagesManual de Operacion y MantenimientoalexNo ratings yet
- (Isaac Asimov) How Did We Find Out About AntarcticDocument24 pages(Isaac Asimov) How Did We Find Out About AntarcticDrBabu PSNo ratings yet
- Twin PregnancyDocument73 pagesTwin Pregnancykrishna mandalNo ratings yet
- Tài Liệu Hướng Dẫn Cài Đặt Rơ Le MPS 3000Document55 pagesTài Liệu Hướng Dẫn Cài Đặt Rơ Le MPS 3000nguyenquangtonNo ratings yet
- Daewoo 710B PDFDocument59 pagesDaewoo 710B PDFbgmentNo ratings yet
- MCQ Floyd ElexDocument87 pagesMCQ Floyd ElexnicoleNo ratings yet
- Designing and Drawing PropellerDocument4 pagesDesigning and Drawing Propellercumpio425428100% (1)
- Latest ResumeDocument2 pagesLatest Resumesamy1234567No ratings yet
- Gastroesophagea L of Reflux Disease (GERD)Document34 pagesGastroesophagea L of Reflux Disease (GERD)Alyda Choirunnissa SudiratnaNo ratings yet
- On Animal Language in The Medieval Classification of Signs PDFDocument24 pagesOn Animal Language in The Medieval Classification of Signs PDFDearNoodlesNo ratings yet
- Sales Forecast Template DownloadDocument9 pagesSales Forecast Template DownloadAshokNo ratings yet
- EX200Document7 pagesEX200shubbyNo ratings yet
- Aribah Ahmed CertificateDocument2 pagesAribah Ahmed CertificateBahadur AliNo ratings yet
- Coal Bottom Ash As Sand Replacement in ConcreteDocument9 pagesCoal Bottom Ash As Sand Replacement in ConcretexxqNo ratings yet
- Resistance & Resistivity: Question Paper 1Document15 pagesResistance & Resistivity: Question Paper 1leon19730% (1)
- Term Paper Inorganic PolymersDocument24 pagesTerm Paper Inorganic PolymersCasey Karua0% (1)
- IOT Architecture IIDocument29 pagesIOT Architecture IIfaisul faryNo ratings yet
- Working Capital Management 2012 of HINDALCO INDUSTRIES LTD.Document98 pagesWorking Capital Management 2012 of HINDALCO INDUSTRIES LTD.Pratyush Dubey100% (1)