Professional Documents
Culture Documents
Coping With Your Baby's NICU Stay
Uploaded by
Diego Jose ChoquectillaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Coping With Your Baby's NICU Stay
Uploaded by
Diego Jose ChoquectillaCopyright:
Available Formats
When Your Baby's in the NICU
New parents eagerly look forward to bringing their baby home, so it can be frightening if your newborn needs to be admitted to the neonatal intensive care unit (NICU). At first it may seem like a foreign place, but understanding the NICU and what goes on there can help reduce your fears and let you better help your baby.
About the NICU
If your baby is sent to the NICU, your first question probably will be: What is this place? With equipment designed for infants and a hospital staff who have special training in newborn care, the NICU is an intensive care unit created for sick newborns who need specialized treatment.
Sometimes the NICU is also called:
a special care nursery an intensive care nursery newborn intensive care
Babies who need to go to the unit are often admitted within the first 24 hours after birth. Babies may be sent to the NICU if:
they're born prematurely difficulties occur during their delivery they show signs of a problem in the first few days of life
Only very young babies (or babies with a condition linked to being born prematurely) are treated in the NICU they're usually infants who haven't gone home from the hospital yet after being born. How long they'll remain in the unit depends on the severity of their illness.
Who Will Be Taking Care of My Baby?
Although many people help care for babies in the NICU, those most responsible for day-to-day care are nurses. You might come to know them very well and rely on them for information and reassurances about your baby.
The nurses you might interact with include a:
charge nurse: the nurse in charge of the shift primary nurse: the one assigned to your baby neonatal nurse practitioner: someone with additional training in neonatology care
Other people who may help care for your baby include:
a neonatologist: a doctor specializing in newborn intensive care who heads up the medical team neonatology fellows, medical residents, and medical students: all pursuing their training at different levels
pediatric hospitalist: a pediatrician who works solely in the hospital setting various specialists: such as a neurologist, a cardiologist, or a surgeon to treat specific issues with the brain, heart, etc.
a respiratory therapist: who helps administer treatments that help with breathing a nutritionist: who can determine what babies receiving IV nutrition need a physical therapist and/or occupational therapist: who work with feeding and movement issues with the infants and their parents
a pharmacist: who helps manage a baby's medications lab technicians: who process the laboratory tests (e.g., urine, blood) taken a chaplain: who can counsel you and try to provide comfort; chaplains may be interfaith or of a particular religious affiliation but they're there to support anyone looking for a spiritual/religious connection
a social worker: who helps you get the services you need and also lends emotional support by connecting you to other families and therapists, if needed
Questions to Ask the Neonatologist or the Nurses
To better help you help your baby during a stay in intensive care, it's wise to get as much information as possible about what to expect. If you have questions, talk to the neonatologist or the nurses.
The nurses see your baby every day, so they can give you frequent updates on your little one. The plan of care for your infant is discussed on "rounds" every day. Nurses can help you to
understand the diagnosis and treatment plan, but it's also helpful to discuss these issues with other members of the medical team including:
the attending neonatologist neonatal fellow neonatal nurse practitioner the residents who are caring for your baby
All of these health professionals are involved in determining the best plan of care for your baby.
You might want to ask the neonatologist and other doctors and/or the nurses:
How long will my baby be in the unit?
What, specifically, is the problem? What will be involved in my baby's treatment and daily care? What medicines will my baby have to take? What types of tests will be done? What can my baby eat and when? Will I be able to nurse or bottle-feed my baby if so, when and how? Will someone help me learn how to nurse my baby? What can I do to help my baby? Will I be able to hold or touch my baby? How often and for how long can I stay in the unit? Can I sleep there? What sort of care will my baby need when we get home? Is there someone who can help us through the process?
You may also want to talk to the nurses in more detail about your baby's daily care and what to expect when you spend time with your little one. You should also learn the visiting schedule and any rules of the NICU so you'll know which family members can see the baby and when they can visit.
Questions to Ask the Social Worker
You might want to ask the social worker:
Where can we get food when we're here?
Can we eat in the NICU? Are cots or recliners available if we're allowed to stay overnight? What about blankets and pillows?
Is nearby temporary housing available (such as through a Ronald McDonald House)? If so, how do we get a room? Is the room free? If not, is the cost low and/or covered by our health insurance? Are computers with Internet access available for doing work or emailing friends and loved ones about our baby's progress?
Are phones available in or around the NICU? Can we use our cell phones in the NICU? If not, can we be reached in the NICU? Is there a support group or other parents of children in the NICU we can talk to?
What to Expect in the NICU
Walking into the NICU can feel like stepping onto another planet the environment is probably unlike anything you've experienced. The unit is often busy, with lots of activity, people moving around, and beeping monitors.
Once settled in the unit, your baby will receive care tailored to your little one's specific needs. Most NICU babies are on special feeding schedules, depending on their level of development or any problems they have. For instance, some infants are too premature or too sick to eat on their own, so they have a feeding tube that runs through the mouth and into the stomach. Others need high-calorie diets to help them grow.
Medications are another crucial part of NICU care your child may take antibiotics, medicine to stimulate breathing, or something to help his or her blood pressure or heart rate, for example.
To ensure that your baby's care stays on track, the doctors also will order various tests, possibly including periodic blood and urine tests, X-rays, and ultrasounds. For infants whose care is
complicated and involved, the doctors or nurses will place a line into an artery or vein so they can draw blood without having to repeatedly stick the baby.
NICU staff try to make the infants' stay in the nursery as comforting as possible for the infant as well as the families. The nurses can explain what all of the monitors, tubes, tests, and machines do, which will go a long way toward demystifying the NICU.
NICU Equipment
Here's a brief look at what some of the unfamiliar equipment does and how it may help your baby, depending on your little one's condition and diagnosis:
Feeding tubes: Often, NICU babies cannot get as many calories as they need through regular feeding from a bottle, so the nurses will use a small feeding tube to deliver formula or breast milk (that the mother pumps). The tube is placed into the baby's stomach through the mouth or through the nose. If an infant is able to take some milk from the bottle, the nurse will just give the rest through the feeding tube. Sometimes, the babies get all their nutrition through the feeding tube so that they don't use excess energy trying to feed from the bottle. The feeding tubes shouldn't be painful they're taped in place so they won't move around and cause friction. However, if they're in place for a long time they can cause erosions in the stomach or nose where they rub, so are changed routinely to avoid this.
Infant warmers: These are beds with radiant heaters over them. Parents can touch their babies in the warmers, but it's always a good idea to talk to the NICU staff about it at first, just in case.
Isolettes: These are small beds enclosed by clear, hard plastic. The temperature of the isolette is controlled and closely monitored because premature infants frequently have difficulty maintaining their body temperature. Holes in the isolettes allow access to the infants so the nurses and doctors can examine the infants and parents can touch their babies.
IVs and lines: An intravenous catheter (or IV) is a thin flexible tube inserted into the vein with a small needle. Once in the vein, the needle is removed, leaving just the soft plastic tubing. Almost all babies in the NICU have an IV for fluids and medications usually in the
hands or arms, but sometimes in the feet, legs, or even scalp. At first, the IV may be inserted in the baby's umbilical cord. In the first hours after delivery, the umbilical cord provides a way for the doctors to insert arterial or venous lines without having to use a needle through the skin. Instead of giving your baby injections every few hours, IVs allow certain medications to be given continuously, several drops at a time. These are known as drips or infusions. Doctors may use these medications to help with heart function, blood pressure, or pain relief. Some situations require larger IVs to deliver greater volumes of fluids and medications. These special IVs are known as central lines because they're inserted into the larger, more central veins of the chest, neck, or groin, as opposed to the hands and feet. They're inserted by a specially trained pediatric surgeon. Arterial lines are very similar to IVs, but they're placed in arteries, not veins, and are used to monitor blood pressure and oxygen levels in the blood (although some babies may simply have blood pressure cuffs instead).
Monitors: Infants in the NICU are attached to monitors so the NICU staff are constantly aware of their vital signs. The nurses will often place the infants in positions that seem the most soothing, like on their tummies or on their sides. The single monitor (which picks up and displays all the necessary information in one place) is secured to your baby's body with chest leads, which are small painless stickers connected to wires. The chest leads can count your child's heart rate and breathing rate. A pulse oximetry (or pulse ox) machine also may display your baby's blood oxygen levels on the monitor. Also painless, the pulse ox is taped to your baby's fingers or toes like a small bandage and emits a soft red light. A temperature probe, a coated wire adhered to your baby's skin with a patch, can track your little one's temperature and display it on the monitor. And unless blood pressure is being directly monitored through an arterial line, your baby will usually have a blood pressure cuff in place.
Phototherapy: Often, premature infants or those with infections also have jaundice (a common newborn condition in which the skin and whites of the eyes turn yellow). Phototherapy is used to help get rid of the bilirubin that causes jaundice. The infants might lie on a special light therapy blanket and have lights attached to their beds or isolettes. Usually, they only need phototherapy for a few days.
Ventilators: Babies in the NICU sometimes need extra help to breathe. An infant is connected to the ventilator (or breathing machine) via an endotracheal tube (a plastic tube placed into the windpipe through the mouth or nose). Babies who've been in the NICU for a prolonged stay months at a time may have a tracheostomy (a plastic tube inserted directly into the trachea) that's connected to the ventilator on the other end. There are many different kinds of ventilators different situations call for different machines but they all accomplish the same basic purpose: to help a baby breathe.
Bonding With Your Baby in the NICU
All the machines may seem overwhelming, but don't let them keep you from interacting with your baby. Bonding with a baby in the NICU is as important as bonding with any newborn, sometimes even more so. You simply have to learn the best way to do it.
Parents can visit and spend time with their NICU babies. The number of people who can visit a baby in the NICU may be limited, but parents are usually allowed to stay most of the day (except when the medical team performs its daily examination and evaluation). Ask the NICU's social worker about what accommodations are available for parents cots, recliners, or nearby housing such as through the Ronald McDonald House Charities.
Other family members can visit only during specified hours and only a few at a time. And siblings may not be allowed in the NICU because children have a greater risk of introducing an infection. Check with the hospital staff about which family members can see your baby.
Depending on how sick your child is, you might be able to hold your little one even if he or she is on a ventilator or has an IV. If the doctors feel that would be too much for your baby, you can still hold his or her hand, stroke his or her head, and talk and sing to him or her. A gentle, consistent touch will be the most reassuring.
But for some very premature infants, touching is extremely stressful (if they were still in the womb, they would have little tactile stimulation). In these cases, doctors may suggest that you minimize physical contact but still spend as much time as possible with your baby. Check with the doctor or nurses to figure out how much and what type of contact is best.
A mother who can hold her baby might be able to breastfeed or pump milk and bottle-feed. Most NICUs have screens to allow mothers to breastfeed their babies at the bedside.
Kangaroo care (or skin-to-skin contact) is another option to help you forge a bond with your new baby. Here's how it works:
Place your baby (who's usually dressed in just a diaper and a hat) on your chest underneath your shirt, so your little one is resting directly on your skin.
Loosely close your shirt over your baby to help keep him or her warm.
Doctors and researchers have suggested that skin-to-skin contact can improve babies' recovery time and help them leave the NICU sooner.
But the best way for parents to help their babies in the NICU is to be there for them and learn to read their behaviors. This will help you to figure out:
when your baby is stressed and needs to rest when your baby is ready to bond with you what type of interaction your baby likes (stroking, singing, etc.) what time of day your baby is the most alert how long your baby can respond to you before getting tired
Although you want to interact with your infant, you also want to allow periods of undisturbed sleep. Let your baby set the pace for your time together and you'll both get more out of it.
Other NICU Basics
Here are some basics to help make the NICU a little less mysterious:
Everyone who comes into the NICU must wash their hands when they enter. (There will be a sink and antibacterial soap in the room and near the entrance of the NICU.) This is a crucial part of keeping the NICU environment as clean as possible so the babies won't be exposed to infections. Some units require visitors to wear hospital gowns, particularly if a child is in isolation. You may also need to wear gloves and a mask.
Ask the nurses what you're allowed to bring into the unit the risk of infection limits what you can leave with your baby. Some parents tape pictures to the isolette or decorate the incubator. If you want to give your child a stuffed toy, the staff may wrap it in plastic first.
When you're in the NICU, keep noise and bright lights to a minimum. Try not to bang things on the isolette or infant warmer, talk in a loud voice, or slam doors. If you're concerned about light, ask a nurse if you can drape a blanket partially over the isolette. Most important, let your baby sleep when he or she needs to.
Making the NICU Stay More Manageable
The time when your baby is in the NICU can be stressful you may be away from your friends and family, including any other children you may have. Your life may seem like it's been turned upside down as you wait for the day when your baby may be able to leave with you.
You may feel like you eat, sleep, and breathe the NICU 24 hours a day, 7 days a week. And you might feel especially confused and overwhelmed if your baby was unexpectedly born prematurely and/or if the NICU is located far away from your home and your usual support system.
As hard as it may be sometimes, it's important to pay attention to your own needs and those of the rest of the family, particularly other kids. Make plans for a weekly family activity, and sit down together and talk about how this experience makes you feel. Doing something for yourself can be as simple as taking a relaxing bath, going for a walk, or reading a favorite book for an hour.
You also can turn to other parents in the NICU for comfort. They'll likely know better than anyone what you're feeling. Also be sure to talk to the NICU's social worker about parents' support groups, where you can share your feelings, worries, and triumphs together. The hospital's chaplain also might be able to provide you with support and even a shoulder to cry on.
When you take care of yourself, you'll be more rested and better prepared to take care of your baby. But that care doesn't have to center on your infant's illness. Enjoy your new baby, spend time together, and get to know your little one.
Your baby's NICU stay can be difficult, but also rewarding as you watch your little one grow and progress day after day.
Reviewed by: Jay S. Greenspan, MD Date reviewed: October 2011
You might also like
- Booklet v1Document5 pagesBooklet v1ddwrt1234No ratings yet
- A Guide To The Newborn Intensive Care Unit (NICU)Document36 pagesA Guide To The Newborn Intensive Care Unit (NICU)Jean Wallace100% (3)
- Original Work Newsletter 1Document9 pagesOriginal Work Newsletter 1api-492096909No ratings yet
- What Is The Neonatal Intensive Care Unit (NICU) ?Document4 pagesWhat Is The Neonatal Intensive Care Unit (NICU) ?Danesa GarciaNo ratings yet
- Paediatric Intensive Care Unit: Information For FamiliesDocument9 pagesPaediatric Intensive Care Unit: Information For FamiliesJaya PrabhaNo ratings yet
- Pat ResiaDocument8 pagesPat ResiarendyjiwonoNo ratings yet
- Organization of Neonatal Care Unit 1Document36 pagesOrganization of Neonatal Care Unit 1Varna Mohan100% (2)
- Youthetourist FinalDocument6 pagesYouthetourist Finalapi-356983145No ratings yet
- Anorectal MalformationDocument4 pagesAnorectal MalformationSabila RosyidaNo ratings yet
- The First Step in Treating Your Child Is Forming An Accurate and Complete DiagnosisDocument3 pagesThe First Step in Treating Your Child Is Forming An Accurate and Complete DiagnosisDimpuulina Erna Mariati SihombingNo ratings yet
- Nicu PaperDocument3 pagesNicu Paperapi-648586622No ratings yet
- Neonatal Intensive Care UnitDocument3 pagesNeonatal Intensive Care UnitwishywashyyyNo ratings yet
- 9503 Duodenal AtresiaDocument2 pages9503 Duodenal Atresiamudasir61No ratings yet
- Early Arrival: 9 Things Parents Need to Know About Life in the ICU Nursery A Doctor's Step-by-Step GuideFrom EverandEarly Arrival: 9 Things Parents Need to Know About Life in the ICU Nursery A Doctor's Step-by-Step GuideNo ratings yet
- Your Antenatal Care - NHS PDFDocument1 pageYour Antenatal Care - NHS PDFS SNo ratings yet
- Case Study 116Document4 pagesCase Study 116Jonah MaasinNo ratings yet
- Routine PNC (Post Natal Care) : What, When, Where and Who? What Is Routine PNC?Document4 pagesRoutine PNC (Post Natal Care) : What, When, Where and Who? What Is Routine PNC?Dex Aiiu SuryaNo ratings yet
- Discharge Planning: Intensive Care Nursery House Staff ManualDocument1 pageDischarge Planning: Intensive Care Nursery House Staff ManualSedaka DonaldsonNo ratings yet
- Provide Postpartum Care To Mother and InfantDocument35 pagesProvide Postpartum Care To Mother and InfantnshabimussakolleNo ratings yet
- Welcome To MUSC Children's HospitalDocument20 pagesWelcome To MUSC Children's Hospitalscott gulyasNo ratings yet
- CATALYST Key Elements of Postpartum Care at The Community Level Based On WHO GuidelinesDocument13 pagesCATALYST Key Elements of Postpartum Care at The Community Level Based On WHO GuidelinesSyifa RisanuhaNo ratings yet
- Antenatal Care What Is Meant by Antenatal Care?Document6 pagesAntenatal Care What Is Meant by Antenatal Care?Syed Haseeb AhmedNo ratings yet
- Delivery Room,.Document3 pagesDelivery Room,.Yukki CuartoNo ratings yet
- Australia Jandj Babycenter Pregnancy DiaryDocument57 pagesAustralia Jandj Babycenter Pregnancy Diarymohamed Ali ahbichNo ratings yet
- Hospitalization: Meaning of Hospitalization:-" DefinitionDocument12 pagesHospitalization: Meaning of Hospitalization:-" DefinitionPriyaNo ratings yet
- Urinary Tract Infection PIAG 84Document3 pagesUrinary Tract Infection PIAG 84madimadi11No ratings yet
- 110613pyloricstenosis PDFDocument8 pages110613pyloricstenosis PDFSandeep KaurNo ratings yet
- Mother's Guide To Breastfeeding: The New York CityDocument28 pagesMother's Guide To Breastfeeding: The New York CityAntonio Miguel García SempereNo ratings yet
- A Guide For Parents Using The Neonatal Service V2 10.2019 Web PDFDocument24 pagesA Guide For Parents Using The Neonatal Service V2 10.2019 Web PDFMihaela CosteaNo ratings yet
- First-Time Mom Handbook: All the Steps from Being Pregnant, Getting Ready and Embracing Motherhood: Motherhood & ChildbirthFrom EverandFirst-Time Mom Handbook: All the Steps from Being Pregnant, Getting Ready and Embracing Motherhood: Motherhood & ChildbirthNo ratings yet
- Maternity and Women Chapter 21Document7 pagesMaternity and Women Chapter 21Sam JonesNo ratings yet
- Korea DeliveriesDocument4 pagesKorea Deliveriesseri ChannelNo ratings yet
- Immediate Care in PostnatalDocument12 pagesImmediate Care in Postnatalvarshasharma05No ratings yet
- Maternal HealthDocument11 pagesMaternal Healthvishoth_kumar100% (2)
- High Risk InfantDocument30 pagesHigh Risk Infantjtongco100% (3)
- Germany CV Format-Sample OnlyDocument6 pagesGermany CV Format-Sample Onlydeamhi nursing serviceNo ratings yet
- NICU Journal: A Parent's JourneyFrom EverandNICU Journal: A Parent's JourneyNo ratings yet
- Routine Antenatal Care For Healthy Pregnant WomenDocument44 pagesRoutine Antenatal Care For Healthy Pregnant Womenewo jatmikoNo ratings yet
- Continued From Page 1 (31st Week Follows)Document6 pagesContinued From Page 1 (31st Week Follows)Naveenbabu SoundararajanNo ratings yet
- Caring After enDocument73 pagesCaring After enbonigirlNo ratings yet
- Hillingdon Health Visiting ServiceDocument12 pagesHillingdon Health Visiting ServiceAnnikaNo ratings yet
- Birth GuideDocument8 pagesBirth GuideMikayla LizuckNo ratings yet
- Hospital JudioDocument14 pagesHospital JudiococoavenNo ratings yet
- Gastrostomy: The Children's HospitalDocument16 pagesGastrostomy: The Children's Hospitalikke alma alukaNo ratings yet
- C-Section Guide: What to Expect with Cesarean DeliveryDocument3 pagesC-Section Guide: What to Expect with Cesarean DeliveryFEALABREPORTSNo ratings yet
- Breastfeeding Lecture 14dec2011 DR EsposDocument164 pagesBreastfeeding Lecture 14dec2011 DR EsposAkimBiNo ratings yet
- What Is Antenatal CareDocument4 pagesWhat Is Antenatal CareSienny Agustin100% (1)
- The Pi$$ed Off Midwife's Guide to having a Baby: What every parent should knowFrom EverandThe Pi$$ed Off Midwife's Guide to having a Baby: What every parent should knowNo ratings yet
- Comfort Techniques and Positions InformaticsDocument16 pagesComfort Techniques and Positions Informaticsapi-341737434No ratings yet
- Discharge Deck - FINAL 2020Document44 pagesDischarge Deck - FINAL 2020Zion OlmosNo ratings yet
- Postpartum After DeliveryDocument6 pagesPostpartum After DeliveryJelly Joy VillanuevaNo ratings yet
- Home Visit Bag Technique and Steam Inhalation-ScriptDocument63 pagesHome Visit Bag Technique and Steam Inhalation-ScriptDaryl Grace SuarezNo ratings yet
- NICU ObservationDocument3 pagesNICU ObservationJessica WitthuhnNo ratings yet
- Coming to the Hospital to Have Your Baby: Frequently Asked QuestionsDocument8 pagesComing to the Hospital to Have Your Baby: Frequently Asked QuestionsCatherine MifsudNo ratings yet
- Chapter 20Document52 pagesChapter 20api-3743202No ratings yet
- Pediatric Anal Dilation InstructionsDocument4 pagesPediatric Anal Dilation InstructionsPeter Fer NandoNo ratings yet
- Infants Exposed To Substance AbuseDocument8 pagesInfants Exposed To Substance AbuseAdoptionParentEduNo ratings yet
- Pi Your Babys Movements in PregnancyDocument4 pagesPi Your Babys Movements in PregnancyJohanna NathasiaNo ratings yet
- Section 09 - Traction Electrification SystemDocument47 pagesSection 09 - Traction Electrification SystemAbu Monsur Ali100% (1)
- Is This Normal or ADHDDocument52 pagesIs This Normal or ADHDDianaNo ratings yet
- Din en 50155 (Vde 0115-200) - 2008-03Document42 pagesDin en 50155 (Vde 0115-200) - 2008-03Collins Akhimien100% (1)
- Raise The Limits: Eppendorf Research PlusDocument12 pagesRaise The Limits: Eppendorf Research PlusZahia Slama Ep AchourNo ratings yet
- Yara Crop Nutrition For HorticultureDocument8 pagesYara Crop Nutrition For HorticultureadjieNo ratings yet
- Team Handball SG Pratt v2Document2 pagesTeam Handball SG Pratt v2Peter StonesNo ratings yet
- Reviewer On Nervous System Grade VIDocument4 pagesReviewer On Nervous System Grade VIKent Francis LayaguinNo ratings yet
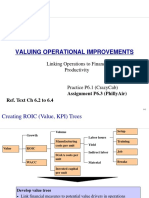
- 2 Linking Operations To Finance and ProductivityDocument14 pages2 Linking Operations To Finance and ProductivityAidan HonnoldNo ratings yet
- Strategic Capacity ManagementDocument36 pagesStrategic Capacity ManagementRahul KhannaNo ratings yet
- Oral Hygiene: Presented By: Anis Anis Andreas KyriakidisDocument60 pagesOral Hygiene: Presented By: Anis Anis Andreas Kyriakidislenami_91No ratings yet
- MSE Admission and Degree RequirementsDocument6 pagesMSE Admission and Degree Requirementsdeathbuddy_87No ratings yet
- B. WoolworthsDocument5 pagesB. WoolworthsNjabulo Shakes NtuliNo ratings yet
- Sir ClanDocument109 pagesSir ClanJames AbendanNo ratings yet
- Comparing characteristics and properties of various crude oilsDocument2 pagesComparing characteristics and properties of various crude oilsnishant bhushanNo ratings yet
- Coyle Chapter 2 PowerPoint SlidesDocument33 pagesCoyle Chapter 2 PowerPoint SlidesKhaled Sheykh0% (1)
- Explore the Precambrian EraDocument3 pagesExplore the Precambrian EraArjay CarolinoNo ratings yet
- Ashrae 62.1-2019Document92 pagesAshrae 62.1-2019Alejandro Castillo100% (16)
- Wattgate 381 Audio Grade Duplex Socket - y CableDocument20 pagesWattgate 381 Audio Grade Duplex Socket - y Cableapi-11530725100% (1)
- Data Sheet 2.07 Issue A: Water Flow Detector Model: WFDENDocument2 pagesData Sheet 2.07 Issue A: Water Flow Detector Model: WFDENOvidiu GavrilasNo ratings yet
- Heidegger On Destruction - Chung ChinDocument16 pagesHeidegger On Destruction - Chung ChinAprilo DielovaNo ratings yet
- End UserDocument205 pagesEnd Userghica05No ratings yet
- AR M205 BrochureDocument4 pagesAR M205 BrochurenickypanzeNo ratings yet
- Tabel Benkelman Beam Baru - AsisDocument21 pagesTabel Benkelman Beam Baru - AsisAsisNo ratings yet
- Understanding the Process of OogenesisDocument52 pagesUnderstanding the Process of OogenesisBharat ThapaNo ratings yet
- TOPFLYtech Product - April 2023 - 4GDocument56 pagesTOPFLYtech Product - April 2023 - 4GmosorioNo ratings yet
- Alimak AustraliancontractminingDocument5 pagesAlimak AustraliancontractminingmanudemNo ratings yet
- Water Demand Fire Flow Calculation Hydraulic ModelingDocument110 pagesWater Demand Fire Flow Calculation Hydraulic ModelingArthur DeiparineNo ratings yet
- Simple LED Flasher CircuitsDocument5 pagesSimple LED Flasher CircuitsVivek BNo ratings yet
- Ring OnlyDocument2 pagesRing Onlyapi-3834777No ratings yet