Professional Documents
Culture Documents
N201 F07Ch45BBnotes
Uploaded by
dlneisha61Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
N201 F07Ch45BBnotes
Uploaded by
dlneisha61Copyright:
Available Formats
Chapter 45
Oxygenation
Factors Essential to Normal Functioning
of the Respiratory System
•Integrity of the airway system to transport air to and from lungs
•Properly functioning alveolar system
in lungs
–Oxygenate venous blood
–Remove carbon dioxide from blood
•Properly functioning cardiovascular and hematological system
–Carry nutrients and wastes to and from body cells
Upper Airway
•Function
•Components
Lower Airway
•Functions
•Components
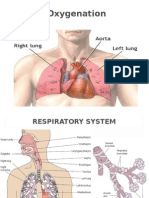
Anatomy of the Lungs
•Main organs of respiration
•Extend from the base of diaphragm to the apex above first rib
•The right lung has three lobes; left lung has two
•The lungs are composed of elastic tissue (alveoli, surfactant, pleura)
The Organs of the Respiratory Tract
Pulmonary Ventilation
•Inspiration—the active phase of ventilation
–Involves movement of
muscles and thorax to
bring air into the lungs
•Expiration—the passive phase
of ventilation
–Movement of air out
of the lungs
Process of Ventilation
Gas Exchange
Four Factors Influencing Diffusion
of Gases in the Lungs
Transport of Respiratory Gases
•Oxygen is carried in the body via plasma and red blood cells
•Most oxygen (97%) is carried by red blood cells in the form of
oxyhemoglobin
•Hemoglobin also carries carbon
dioxide in form of
carboxyhemoglobin
•Internal respiration between the
circulating blood and tissue cells
must occur
Respiratory Activity in the Infant
Respiratory Activity in the Child
Respiratory Functioning in the Older Adult
Factors Affecting Respiratory Functioning
•Levels of health
•Developmental considerations
•Medications
•Lifestyle
•Environment
•Psychological health
Guidelines for Obtaining a Nursing History
•Determine why the patient needs nursing care
•Determine what kind of care is needed to maintain a sufficient intake of air
•Identify current or potential health deviations
•Identify actions performed by the patient for meeting respiratory needs
•Make use of aids to improve intake of air and effects on patient’s lifestyle
and relationship with others
Sounds Heard Upon Percussion
of Chest Wall
Breath Sounds
Abnormal (Adventitious) Lung Sounds
Common Diagnostic Methods
•Pulmonary function studies
•Peak expiratory flow rate
•Pulse oximetry
•Thoracentesis
Lung Volumes
•Tidal volume (TV)—amount of air inspired and expired in normal
respiration (normal = 500 mL)
•Inspiratory reserve volume (IRV)—amount of air inspired beyond tidal
volume (normal = 3100 mL)
•Expiratory reserve volume (ERV)—amount of air that can be exhaled
beyond tidal volume (normal = 1200 mL)
•Residual volume (RV)—amount of air remaining in lungs after a maximal
expiration (normal = 1200 mL)
Lung Capacities
•Vital capacity (VC)—amount of air that can be exhaled after a maximal
inhalation (normal = 4800 mL)
•Inspiratory capacity (IC)—largest amount of air that can be inhaled after
normal quiet exhalation (normal = 3600 mL)
•Functional residual volume (FRV)—equal to the expiratory reserve
volume plus the residual volume (normal = 2400 mL)
•Total lung capacity (TLC)—the sum of the TV, IRV, ERV, and RV (normal
= 6000 mL)
Nursing Interventions Promoting Adequate
Respiratory Functioning
•Teaching about a pollution-free environment
•Promoting optimal function
•Promoting proper breathing and comfort
•Managing chest tubes
•Promoting and controlling coughing
•Promoting comfort
•Meeting respiratory needs with medications
Promoting Proper Breathing
•Deep breathing
•Using incentive spirometry (IS)
•Pursed-lip breathing
•Abdominal or diaphragmatic breathing
Types of Cough Medications
•Cough suppressants
•Expectorants
•Lozenges
Performing Chest Physiotherapy
•Percussion
•Vibrating
•Providing postural
drainage
Administering Inhaled Medications
•Bronchodilators—open
narrowed airways
•Mucolytic agents—liquefy or
loosen thick secretions
•Corticosteroids—reduce
inflammation in airways
Types of Inhalers
•Nebulizers—disperse fine particles of medication into deeper passages of
respiratory tract where absorption occurs
•Metered dose inhalers (MDI)—deliver controlled dose of medication with
each compression of the canister
•Dry powder inhalers (DPI)— activated by the patient’s inspiration
Oxygen Delivery Systems
•Nasal cannula
•Nasal catheter
•Transtracheal catheter
•Simple mask
•Partial rebreather mask
•Nonrebreather mask
•Venturi mask
•Tent
Precautions for Oxygen Administration
•Avoid open flames in patient’s room
•Place no smoking signs in conspicuous places
•Check to see electrical equipment in room is in good working order
•Avoid wearing and using synthetic fabrics (builds up static electricity)
•Avoid using oils in the area (ignite spontaneously in oxygen)
Types of Artificial Airways
•Oropharangeal and nasopharyngeal airway
•Endotracheal tube (ET tube)
•Tracheostomy tube
Administering Cardiopulmonary Resuscitation (ABCs)
•Airway—tip the head and check for breathing
•Breathing—if victim is not breathing spontaneously, give two breaths lasting
1.5 to 2 seconds
•Circulation—check the pulse; if victim has no pulse, initiate chest
compressions
Planning: Expected Outcomes
•Demonstrate improved gas exchange in lungs by absence of cyanosis or
chest pain and a pulse oximetry reading >95%
•Relate the causative factors and demonstrate adaptive method of coping
•Preserve pulmonary function by maintaining an optimal level of activity
•Demonstrate self-care behaviors that provide relief from symptoms and
prevent further problems
You might also like
- The Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessFrom EverandThe Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessNo ratings yet
- Respiratory System DisordersDocument353 pagesRespiratory System Disordersይደግ አብነውNo ratings yet
- Nursing Fundamentals Focus VIII: OxygenationDocument72 pagesNursing Fundamentals Focus VIII: OxygenationTni JolieNo ratings yet
- Fundamentals of Nursing: OxygenationDocument56 pagesFundamentals of Nursing: OxygenationFEVIE ANNE BANATAONo ratings yet
- Kim LesterDocument6 pagesKim LesterKim Lester ValeraNo ratings yet
- Chapter 13 Student Version The Respiratory System 2020.ppt (1186)Document18 pagesChapter 13 Student Version The Respiratory System 2020.ppt (1186)S. MartinezNo ratings yet
- The Respiratory System Organs of The Respiratory System: © 2018 Pearson Education, Ltd. 1Document13 pagesThe Respiratory System Organs of The Respiratory System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Measurements of The Respiratory SystemDocument36 pagesMeasurements of The Respiratory SystemKrishnaswamy RajaNo ratings yet
- Science 9 1.1 LessonDocument25 pagesScience 9 1.1 LessonHdisbdbd NfjdnbdncNo ratings yet
- Assessment of Respi FXDocument133 pagesAssessment of Respi FXIrish Jane GalloNo ratings yet
- OxygenationDocument50 pagesOxygenationLulu MushiNo ratings yet
- Respiratory SystemDocument56 pagesRespiratory SystemBenjo100% (2)
- Respiratorysystem 101228012430 Phpapp01Document69 pagesRespiratorysystem 101228012430 Phpapp01Val Angelo BugayNo ratings yet
- Oxygen Therapy - Facemask, Nasal ProngDocument47 pagesOxygen Therapy - Facemask, Nasal ProngLimYiNo ratings yet
- Module 2Document40 pagesModule 2Sharanya BasakNo ratings yet
- Air 213 2Document56 pagesAir 213 2gr0442No ratings yet
- 2018 Respiratory System HandoutDocument10 pages2018 Respiratory System HandoutMr. DummyNo ratings yet
- Respiratory SystemDocument56 pagesRespiratory SystemLorenz PasensyosoNo ratings yet
- The Respiratory SystemDocument53 pagesThe Respiratory SystemShaila AliNo ratings yet
- Stressors That Affect Oxygen NeedsDocument40 pagesStressors That Affect Oxygen NeedsChucky VergaraNo ratings yet
- Pulmonary Function Tests: Measuring The Capacity For Life Esmeralda E. Morales, MD September 21, 2004Document54 pagesPulmonary Function Tests: Measuring The Capacity For Life Esmeralda E. Morales, MD September 21, 2004Ronnie JaderNo ratings yet
- Sains Tingkatan 3: Science Form 3Document27 pagesSains Tingkatan 3: Science Form 3Nadzirah RedzuanNo ratings yet
- CBS RespsystemDocument34 pagesCBS RespsystemtyhbbhhNo ratings yet
- Respiratory System: Assessment & Disorders Dr. Mohamed IdrissDocument41 pagesRespiratory System: Assessment & Disorders Dr. Mohamed IdrissBsoom .iNo ratings yet
- Basic Concept of OxygenationDocument50 pagesBasic Concept of OxygenationWiradianto PutroNo ratings yet
- The Mechanics of Breathing: Mashmum Shababa ShahidDocument31 pagesThe Mechanics of Breathing: Mashmum Shababa ShahidSHANJIDA ALI RIANo ratings yet
- Neonatal ResuscitationDocument46 pagesNeonatal ResuscitationAsaliwe BorahNo ratings yet
- Respiration and Gas ExchangeDocument48 pagesRespiration and Gas ExchangeIbrahim NOORZADNo ratings yet
- Gas Exchange StructuresDocument13 pagesGas Exchange Structuresmohamed komiNo ratings yet
- Mechanics of Ventilation and Control of Breathing: Moderated by - Dr. Anjali Mehta Presented By-Dr. Sonal SharmaDocument65 pagesMechanics of Ventilation and Control of Breathing: Moderated by - Dr. Anjali Mehta Presented By-Dr. Sonal Sharmamanzoor bhatNo ratings yet
- Respiratory AssessmentDocument27 pagesRespiratory AssessmentAinaB ManaloNo ratings yet
- Respiratory Physiology FBSDocument58 pagesRespiratory Physiology FBStriana abidahNo ratings yet
- Diving PhysiologyDocument334 pagesDiving PhysiologyemilidiverNo ratings yet
- Gas Exchange in Humans PDFDocument32 pagesGas Exchange in Humans PDFNaomi LimNo ratings yet
- Lecure-10 Measurements of The Respiratory SystemDocument48 pagesLecure-10 Measurements of The Respiratory SystemNoor Ahmed100% (1)
- Lecure-10 Measurements of The Respiratory SystemDocument48 pagesLecure-10 Measurements of The Respiratory SystemNoor AhmedNo ratings yet
- Oxygenation Lesson 3Document78 pagesOxygenation Lesson 3Yjah Cheimira ASEBONo ratings yet
- Mtless 8 F 99 RespiratoryDocument28 pagesMtless 8 F 99 RespiratorytiejeitorresNo ratings yet
- Stressors That Affect Oxygen Needs: NUR101 FALL 2008 K. Burger, Msed, MSN, RN, Cne Lecture #19Document39 pagesStressors That Affect Oxygen Needs: NUR101 FALL 2008 K. Burger, Msed, MSN, RN, Cne Lecture #19TobiDaNo ratings yet
- Respiratory Unit 1 Structure and FunctionDocument21 pagesRespiratory Unit 1 Structure and FunctionNethul PereraNo ratings yet
- Respiratory Physio UsmleDocument61 pagesRespiratory Physio UsmleDr.G.Bhanu Prakash100% (2)
- Respiratory PhysiologyDocument53 pagesRespiratory Physiologychichura9No ratings yet
- Anatomy & Physiology of Cardiovascular & Respiratory SystemDocument34 pagesAnatomy & Physiology of Cardiovascular & Respiratory SystemSalman KhanNo ratings yet
- The Respiratory SystemDocument18 pagesThe Respiratory SystemTamilore WilliamsNo ratings yet
- OXYGENATIONDocument69 pagesOXYGENATIONTina Talmadge100% (4)
- Hole'S Human Anatomy and Physiology: Powerpoint Lecture Outlines To AccompanyDocument52 pagesHole'S Human Anatomy and Physiology: Powerpoint Lecture Outlines To AccompanyEllen LiberaceNo ratings yet
- Respiration Grade 10 Biology - StudentDocument65 pagesRespiration Grade 10 Biology - StudentAsawni McDowellNo ratings yet
- Respiratory SystemDocument50 pagesRespiratory SystemsowjanyaNo ratings yet
- Respiratory Disorders 2.1Document70 pagesRespiratory Disorders 2.1Deenjane Nishi IgnacioNo ratings yet
- CH 13 - Respiratory SystemDocument56 pagesCH 13 - Respiratory SystemAna Ats Yvi100% (4)
- Respiration SystemDocument49 pagesRespiration Systemfebe_aldellaNo ratings yet
- Respiratory SystemDocument16 pagesRespiratory Systemapi-277775953No ratings yet
- Biology 2 Lecture 8 - Respiratory SystemDocument24 pagesBiology 2 Lecture 8 - Respiratory Systemryle34No ratings yet
- Respiratory SystemDocument24 pagesRespiratory SystemRhod Jayson RicaldeNo ratings yet
- Respiratory NeedsDocument24 pagesRespiratory NeedsJoyceNo ratings yet
- Respiratorysystem 16Document35 pagesRespiratorysystem 16api-340406981No ratings yet
- Chest PhysiotherapyDocument79 pagesChest PhysiotherapyRabab Ahmed100% (2)
- Anatomy of Respiratory SystemDocument61 pagesAnatomy of Respiratory SystemLalu Fatria ZulhadiNo ratings yet
- ScienceDocument14 pagesSciencesheanellerenzsantosNo ratings yet
- Nursing 304 Nursing Care of The Client/Family With Select Sensory Health DeviationsDocument8 pagesNursing 304 Nursing Care of The Client/Family With Select Sensory Health Deviationsdlneisha61No ratings yet
- Mental Health AssessmentDocument12 pagesMental Health Assessmentdlneisha61100% (4)
- Nursing 304 Nursing Care of The Client/Family With Select Sensory Health DeviationsDocument8 pagesNursing 304 Nursing Care of The Client/Family With Select Sensory Health Deviationsdlneisha61No ratings yet
- Human Immunodeficiency Virus: Transmission of HIVDocument15 pagesHuman Immunodeficiency Virus: Transmission of HIVdlneisha61No ratings yet
- Mental Health NursingDocument10 pagesMental Health Nursingdlneisha61100% (4)
- Mental Health Outline1Document25 pagesMental Health Outline1dlneisha61No ratings yet
- Impaired Skin Integrity and ConstipationDocument6 pagesImpaired Skin Integrity and Constipationdlneisha61100% (1)
- Hiv Study GuideDocument3 pagesHiv Study Guidedlneisha61No ratings yet
- Integumentary Disorders Fall07ebDocument34 pagesIntegumentary Disorders Fall07ebdlneisha61No ratings yet
- Sexual Contact (Anal, Vaginal, Oral) With An HIV-infected PartnerDocument17 pagesSexual Contact (Anal, Vaginal, Oral) With An HIV-infected Partnerdlneisha61No ratings yet
- Hematology Outline For Blackboard Revised CDocument22 pagesHematology Outline For Blackboard Revised Cdlneisha61No ratings yet
- Fluids and Electrolytes Lesson Outline For BBDocument14 pagesFluids and Electrolytes Lesson Outline For BBdlneisha61100% (1)
- Hematology Outline For Blackboard Revised CDocument22 pagesHematology Outline For Blackboard Revised Cdlneisha61No ratings yet
- GU Lisa RetypedDocument15 pagesGU Lisa Retypeddlneisha61No ratings yet
- GU Blackboard OutlineDocument15 pagesGU Blackboard Outlinedlneisha61No ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Urinary System: TH RDDocument13 pagesUrinary System: TH RDdlneisha61No ratings yet
- Diabetes Mellitus Outline For BBDocument10 pagesDiabetes Mellitus Outline For BBdlneisha61No ratings yet
- Dosage Practice Problem GuideDocument20 pagesDosage Practice Problem Guidedlneisha6171% (7)
- Mental Health NursingDocument10 pagesMental Health Nursingdlneisha61100% (4)
- Concepts, Constructs, Variables and TheoryDocument6 pagesConcepts, Constructs, Variables and Theorydlneisha61100% (2)
- Fire Drill Senarios ToolDocument5 pagesFire Drill Senarios ToolAzmatRaoNo ratings yet
- Hipo - Hiper SubDocument123 pagesHipo - Hiper SubdankouzielNo ratings yet
- Range of Motion Exercises 2Document5 pagesRange of Motion Exercises 2Attila TamasNo ratings yet
- Approach To in Born Errors of MetabolismDocument112 pagesApproach To in Born Errors of MetabolismGurpreet Singh100% (3)
- 58f6anesthesia For Laparoscopic SurgeriesDocument56 pages58f6anesthesia For Laparoscopic SurgeriesSayed NourNo ratings yet
- SBARDocument4 pagesSBARIka AnggreIta SafitriNo ratings yet
- UHMS HBO2 Indications 13th Ed. Front Matter ReferencesDocument172 pagesUHMS HBO2 Indications 13th Ed. Front Matter ReferencesJeffry Hertanto50% (2)
- A Review of The Family CrucibleDocument5 pagesA Review of The Family CrucibleywaitereNo ratings yet
- Hospitalityin HospitalsDocument18 pagesHospitalityin HospitalsRANDY ADMINo ratings yet
- Anaesthesia NotesDocument61 pagesAnaesthesia NotessuggaplumNo ratings yet
- Hypertrophic Pyloric StenosisDocument28 pagesHypertrophic Pyloric StenosisAhmad Abu Kush100% (2)
- Case Report OsteochondromaDocument43 pagesCase Report OsteochondromaFidesha Nurganiah SiregarNo ratings yet
- FryetteDocument2 pagesFryetteSaba KhanNo ratings yet
- Subluxation and Dislocation of Ac JointDocument26 pagesSubluxation and Dislocation of Ac JointGan Quan FuNo ratings yet
- Healing ArchitectureDocument5 pagesHealing ArchitectureSUDHAKARMANI100% (2)
- Indirect Patient Duty oDocument5 pagesIndirect Patient Duty oJiansong ChangNo ratings yet
- Communicable Disease Nursing Clinical FocusDocument2 pagesCommunicable Disease Nursing Clinical Focusrceponelas1127No ratings yet
- Answer: 1Document4 pagesAnswer: 1Jeffrey ViernesNo ratings yet
- Admission ProcedureDocument20 pagesAdmission ProcedureSumit Yadav67% (6)
- Up Date Psychosomatic Medicine 2015Document15 pagesUp Date Psychosomatic Medicine 2015AlexisMolinaCampuzanoNo ratings yet
- Peplau's Theory of Interpersonal Relations: An Alternate Factor Structure For Patient Experience Data?Document9 pagesPeplau's Theory of Interpersonal Relations: An Alternate Factor Structure For Patient Experience Data?Rila LuaduNo ratings yet
- Cleft Lip and Cleft PalateDocument22 pagesCleft Lip and Cleft PalateOm VaishNav0% (1)
- Performance Improvement Plan Template 1 - 908445459Document3 pagesPerformance Improvement Plan Template 1 - 908445459api-534828007No ratings yet
- MS RatioDocument82 pagesMS RatioMei JoyNo ratings yet
- Hematology - Oncology GlossaryDocument18 pagesHematology - Oncology GlossaryFran CescaNo ratings yet
- Notre Dame of Educational Association.Document10 pagesNotre Dame of Educational Association.Maui TingNo ratings yet
- Charting by ExceptionDocument7 pagesCharting by Exceptionafini aninditaNo ratings yet
- Research Paper - DsDocument4 pagesResearch Paper - Dsapi-247111687No ratings yet
- Fiber-Reinforced Onlay Composite (Unlocked by WWW - Freemypdf.com)Document7 pagesFiber-Reinforced Onlay Composite (Unlocked by WWW - Freemypdf.com)Adrian DjohanNo ratings yet
- Certificate of Professional Competence - Tudorache Andrei MarianDocument2 pagesCertificate of Professional Competence - Tudorache Andrei MarianAndrei TudoracheNo ratings yet