Professional Documents
Culture Documents
Fluids and Electrolytes Lesson Outline For BB
Uploaded by
dlneisha61Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluids and Electrolytes Lesson Outline For BB
Uploaded by
dlneisha61Copyright:
Available Formats
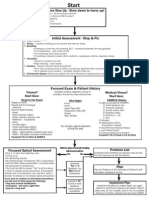
Student Preparation for Fluids and Electrolytes Lesson
1. Read all Nursing Alert boxes in chapter 14 of Brunner textbook
2. What is the relationship between fluid and body weight?
3. What is the best measure of fluid gains/losses?
4. Consider children, adults, and elderly adults:
• Who has more and who has less water?
• How does this impact fluid problems?
5. Consider adult males and adult females: who has more water?
6. Consider obesity versus normal weight: who has more water?
7. What is recommended amount of water for an adult?
(clue: answer is not just 8 glasses per day)
8. What is acceptable hourly urine output?
9. What does osmolarity/osmolality mean?
10. What is the difference between osmosis and diffusion?
11. What is hydrostatic pressure?
13. What is colloidal oncotic/osmotic pressure?
14. What is the difference in first, second, and third spacing of fluids?
15. What does ADH do? What stimulates its release? What happens after it is released?
16. What does renin do? What stimulates its release? What happens after it is released?
17. What does the lymphatic system have to do with fluid homeostasis?
18. What are the fluid compartments, and where is most of the body fluid?
19. See chart on IV Fluids:
• How are IV fluids described?
• What is used to determine that description?
• What are crystalloids?
• What are colloids?
• How do different IV fluids affect the body?
20. See chart on Electrolyte Imbalances
21. Be prepared to discuss this information on Monday, January 14, 2008.
FVD RT (can be intravascular, interstitial and/or intracellular)
• Decreased intake (elderly < thirst, fear incontinence, dementia)
• Increased fluid loss (<ADH, V/D, >diaphoresis, meds, blood loss, > glucose, hypertonic IV fluid/tube
feeding)
• Fluid shifts (decreased albumin)
FVD AMB or AEB : List what your physical assessment would show
List what labs would show:
• BUN
• Creatinine
• BUN: Creatinine ratio
• Serum osmolality
• Urine osmolality
• Hematocrit
FVD Plan—NOC : Fluid & electrolyte balance, AB balance, hydration, adequate nutrition (food/fluid), causes
corrected (must look for and treat problem)
FVD NIC: Fluid volume management
Goals for FVD Interventions and Eval
Client will: Rationales
1. Have moist mucous membranes
2. Have absence of orthostatic
hypotension <15 mm drop with
changes, < 15 increase in HR
3. Have balanced 24 hour I&O, at
least 30 mL/hour urine output
4. Have no further vomiting/diarrhea
(if this is RT)
5. Have BUN 10 – 20
6. Have BUN: Creatinine Ratio 10 –
20:1
7. Have serum osmolality 275 – 300
8. Have Na 135 – 145
9. Have Hct 40 - 50
10. Have no evidence of second or
third spaced fluids
11. Have no changes in mental status,
no seizure activity
12. Verbalize/demonstrate measures to
maintain balance
FVE RT
• Increased intake (oral or IV)
• Increased Na
• Increased fluid retention (CHF, renal failure)
• Fluid shifts (colloids, hypertonic IV)
AMB or AEB—List what your physical assessment would show
List what labs would show:
• BUN
• Srum osmolality
• Hematocrit
• Na
FVE Plan—NOC : Fluid & electrolyte balance, AB balance, hydration, adequate nutrition (food/fluid), causes
corrected (must look for and treat problem)
NIC: Fluid monitoring and management
Goals for FVE Interventions and Rationales Eval
Client will:
1. Have urine output at least
30 mL/hour
2. Achieve weight appropriate
for client
3. Have no edema, JVD
4. Have clear breath sounds
5. Have regular easy
respirations (no orthopnea,
dyspnea)
6. Have vital signs WNL for
client
7. Have BUN 10 – 20
8. Have BUN: Creatinine
Ratio 10 – 20:1
9. Have serum osmolality 275
– 300
10. Have Na 135 – 145
11. Have Hct 40 - 50
12. No mental status changes,
no seizure activity
13. Verbalize/demonstrate
knowledge regarding fluid
and Na restrictions
14. Have no skin breakdown
HOW IV OSMOLALITY AFFECTS THE BODY
Hypotonic Solution Isotonic Solution Hypertonic Solution
Osmolarity < 240 240 - 340 > 340
Physiologic Fluid shifts out of vascular Fluid stays in vascular Fluid shifts out of
Effect compartment into the cells compartment; no cells and interstitial
and interstitial movement into or out of compartments into
compartments; Cells cells; Cells aren’t vascular compartment;
swell affected Cells shrink
Indications Cellular dehydration Intravascular Intravascular
(Many times the vascular dehydration (FVD) dehydration (FVD)
bed gets into FVD first, with intracellular
then the cells get and interstitial
dehydrated as they send overload (FVE in
water out to try to restore those areas); Useful
homeostasis in serum in restoring volume in
osmolarity. Therefore, vascular bed and
usually if there is FVD in drawing water out of
vascular compartment, the the cells and
cells will soon be in FVD interstitial spaces
also. For this reason, you
may see orders to alternate
IV fluids between isotonic
and hypotonic--to restore
fluid volume in both
places)
Examples of .45%NS NS D5NS
these types of RL D5.45%NS
IV fluids D5W (initially, but then D5RL
becomes hypotonic after D10W (10% dextrose
dextrose is used for in water)
cellular energy) 3%NaCl
Imbalances of Major Electrolytes
ELECTROLYTE DEFICIT EXCESS
Sodium (135 - 145 mEq/L) Hyponatremia (<135) Hypernatremia (>145)
Fluid balance, osmolality, Weakness Irritability
transmission of nerve impulses
Cellular swelling, cerebral edema, Cellular shrinking may cause CNS
Foods high: canned, cheese, headache, seizure, stupor, coma, peripheral irritability, seizure, dry and flushed skin,
instant cereals, chips, etc. edema, polyuria, absence of thirst, hypertension, thirst, hyperthermia,
hypothermia, tachycardia, hypotension, N/V tachycardia, weight gain, oliguria, anuria
Foods low: fresh or frozen fruits
and vegetables
Potassium (3.5 - 5.5 mEq/L) Hypokalemia (<3.5) Hyperkalemia (>5.5)
Transmission of nerve impulses to
muscles, acid-base balance
Weakness Irritability
Cramps, decreased peristalsis, paralytic ileus, Muscle cramps, paresthesias, nausea,
Foods high: OJ, bananas, metabolic alkalosis explosive diarrhea, metabolic acidosis
cantaloupe, raisins
Heart muscle so weak it becomes irritable Depressed conductivity of heart because of
Foods low: corn, sweet potatoes, and has irregular rhythm; Beware of “dig excessive stimulation
apples toxicity” if on digoxin.
Phosphate (2.8 - 4.5 mg/dl) Hypophosphatemia (<2.8) Hyperphosphatemia (>4.5)
Bone integrity, acid-base balance
Weakness Irritability
Foods high: dairy products
Similar S&S/ efffects as elevated Similar S&S/effects as decreased calcium
calcium (Inverse relationship) (Inverse relationship)
Calcium ( Total 9 - 11 mg/dl) Hypocalcemia (< 9) Hypercalcemia (>11)
Transmission of nerve impulses to
muscles; clotting, bone strength
Excitability/Irritability Weakness
Has a sedative effect on Neuromuscular sedation, stupor to coma,
neuromuscular system.
Increased neuromuscular excitability,
pathological fractures, skeletal muscle increased risk of bone fracture, vomiting,
constipation, kidney stones
Foods high: dairy, cheese, canned cramps, paresthesias, tetany,
fish w/bones laryngospasm, death! Similar S&S/effects as decreased phosphate
(Inverse relationship)
Foods low: bananas, pasta, beef Similar S&S/effects as elevated phophate
(Inverse relationship)
Magnesium (1.5 - 2.5 mEq/L) Hypomagnesemia (<1.5) Hypermagnesemia (>2.5)
Transmission of nerve impulses;
promotes vasodilation in peripheral
Irritability Weakness
arteries and arterioles. Hypertension, tachycardia, seizures, tetany, Hypotension, bradycardia, respiratory
convulsions depression
Foods high: green vegetables, nuts,
bananas, PB, chocolate
Foods low: chicken, eggs, white
bread
For the most part, electrolytes come from eating and drinking them and absorption from small
intestine.
Sodium: Major contributor to serum osmolality (normal 135 – 145)
Hyponatremia
RT:
• Na loss (diuretics, prolonged vomiting, NG suction)
• Diet restrictions
• Water gain (dilutional hyponatremia due to >, or too much ADH-pituitary problem SIADH)
AMB : symptoms due to muscle/nerve weakness and cellular swelling
List what you would see on physical assessment
Nursing Diagnoses for hyponatremia:
• FVE
• Nutrition < body requirements
• High risk for injury RT confusion, weakness, seizure potential secondary to low sodium
• Altered thought processes
Plan/Goals/Outcomes for Hyponatremia
NOC: Fluid and electrolyte balance, nutritional balance, no injury, normal mental status
Interventions for hyponatremia
List what you will do
Hypernatremia
RT:
• Na gain (increased intake, hypertonic IV, increased aldosterone, steroids)
• Water loss in excess of Na loss (very watery diarrhea, burns, osmotic diuresis, too little
ADA (diabetes insipidus—very clear, watery urine), impaired thirst (cause)
AMB : symptoms due to muscle/nerve irritability and cellular shrinking
List what you would see on physical assessment
Nursing Diagnoses for Hypernatremia:
• FVD
• Nutrition > body requirements
• Altered oral mucous membranes
• High risk for injury RT confusion, weakness, seizure potential secondary to low Na
• Altered thought processes
Plan/Goals/Outcomes for Hypernatremia
NOC: Fluid and electrolyte balance, nutritional balance, No injury, normal mental status
Nursing Interventions for Hypernatremia
What will you do?
Potassium Normal 3.5 – 5.5
96% is inside cells
Generally, as Na increases, K decreases, and vv
Plays role in AB balance
Hypokalemia RT:
• Decreased intake (starvation, alcoholism, NPO and no K in IV fluids)
• GI losses>>>alkalosis from vomiting, NG suction, intestinal malabsorption
• Medications (K wasting diuretics, steroids, insulin)
AMB (overall weakness and cardiac irritability)
• Hypoactive bowel sounds and constipation, lethargy, apathy, mental dullness
• Cardiac dysrhythmias, flattened or inverted T wave, Dig toxicity if on Dig and K is low
• Muscle irritability (cramping of legs)
Nursing Diagnoses for hypokalemia
• Nutrition < body requirements RT decreased intake, alcohol intake, acid-base imbalance
• Constipation RT hypoactive peristalsis secondary to decreased serum potassium
• Risk for injury RT muscle weakness, cardiac dysrhythmias
• Pain RT muscle cramping
• Knowledge deficit RT potassium replacement needed with potassium wasting diuretics, etc.
Plan/Goals/Outcomes for Hypokalemia: Fluid and electrolyte balance, nutritional
balance, No injury, normal mental status
Nursing Interventions for Hypokalemia
What will you do?
Hyperkalemia
RT:
• Renal insufficiency or failure
• Traumatic injuries (ruptured cells releasing K)
• Acidosis (shock and decreased circulation leads to decreased perfusion to tissues, and glucose is used
without adequate oxygen and leads to lactic acidosis)
• Excessive intake (RL has K and other lytes)
• Serum drawn from IV line with K infusion
• Tourniquet too tight, Suction during blood draw, hemolyzed sample (be sure to match results to client)
AMB (cells become more irritable and them become weaker and paralyzed)
• Muscle cramps, hyperactive peristalsis and explosive diarrhea
• Heart muscle irritated at first, then becomes weak and contraction slows, cardiac output
decreases, cardiac arrest may occur)
• Tall T wave
Nursing Diagnoses for hyperkalemia
• High risk for injury RT muscle weakness, cardiac irritability secondary to elevated K levels
• Pain RT muscle cramping, bowel cramping
• FVD RT diarrhea secondary to muscle irritability due to elevated K levels
• Knowledge deficit of NURSE! (when we give out K meds and don’t even note labs)
Plan/Goals/Outcomes for Hyperkalemia: Fluid and electrolyte balance, nutritional balance,
No injury, normal mental status, no discomfort, no diarrhea
Nursing Interventions for Hyperkalemia
What will you do? Look at Kayexalate, renal dialysis, and insulin & glucose as therapies
Calcium (Normal Total serum Ca is 9 – 11, ionized is 4.5—5.5 )
99% of body calcium is found in bones and teeth
About 1/2 of Ca is bound to protein
Nerve impulses and muscle contractions like all the others & plays role in blood clotting
Has an inverse relationship with phosphorous
Hypocalcemia
RT:
• Decreased dietary intake
• Decreased absorption in small intestine
• Vitamin D deficiency
• Increased phosphorous levels (inverse relationship)
• Excessive losses secondary to loop diuretics
• Binding to necrotic areas in autodigestion of pancreas
• Hypofunction of parathyroid glands
• Decreased ionization of calcium secondary to alkalotic conditions
• Hypokalemic conditions that result in alkalosis
AMB (due to neuromuscular hyperexcitability)
What will you see on physical assessment? (paresthesias, Chvostek’s, Trousseau’s)
Nursing Diagnoses for hypocalcemia
• Nutrition < body requirements for calcium RT decreased intake, impaired absorption
• Nutrition > body requirements for phosphorous causing decreased calcium levels
• Risk for injury RT increased neuromuscular irritability
• Pain RT muscle spasms
• Risk for injury RT bone fractures due to increased losses from bones secondary to
decreased oral intake or due to hyperfunction of parathyroid glands,
• Knowledge deficit RT balanced nutrition, intake of Calcium supplements
Plan/Outcomes for hypocalcemia: Calcium levels WNL, Balanced nutrition, No
neuromuscular irritability, no discomfort, no respiratory distress, adequate clotting, no
fractures
Nursing Interventions for Hypocalcemia
What will you do?
How are oral calcium supplements best given?
How should IV calcium be given?
Hypercalcemia
RT:
• Increased intake of calcium and vitamin D
• Hyperfunction of parathyroid gland
• Prolonged immobility
• Altered cell growth (cancer): bone resorption and paraneoplastic syndrome
• Decreased phosphorous levels
• Acidotic conditions where ionization of calcium is increased
AMB (most symptoms due to sedation to nerves and muscles)
What will you see on physical assessment?
Nursing Diagnoses with Hypercalcemia
• Risk for injury RT pathological fractures,
RT cardiac dysrhymias,
RT treatment with thiazide diuretics,
RT mental confusion
• Knowledge deficit or altered health maintenance RT excessive ingestion of calcium products
• Nutrition < BR RT decreased intake secondary to nausea, vomiting, constipation due to elevated calcium
• FVD RT decreased intake secondary to nausea, vomiting, and increased urine output due to elevated
Calcium levels
Plan/Outcomes: Fluid and electrolyte balance, no fractures, no cardiac dysrhythmias, no changes in mental
status, no pain, no renal damage
Nursing Interventions for Hypercalcemia:
What will you do?
Magnesium Normal is 1.5 – 2.5
Promotes vasodilation of peripheral arteries and arterioles
HYPOMAGNESEMIA
RT:
• Malnutrition (starvation, anorexia, alcoholism)
• Malabsorption
• Prolonged loss from GI or GU
• Prolonged NPO with IV/TPN without magnesium
AMB:
What will physical assessment reveal?
Nursing Diagnoses with Hypomagnesemia (Same as others)
Plan/Outcomes with Hypomagnesemia: No evidence of NM irritability, BP WNL, HR
regular rhythm and rate
Nursing Interventions for Hypomagnesemia:
What will you do?
Hypermagnesemia
RT:
• Impaired renal secretion (Renal insufficiency or failure)
• Excessive intake of Mg antacids or laxatives (Maalox, MOM)
• Excessive intake of IV magnesium (pregnancy)
AMB:
What will physical assessment reveal?
Nursing Interventions for Hypermagnesemia
What will you do?
You might also like
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- BMAT-Bedside Mobility Assessment Tool: by Amber Perez ADN, BSB, CSPHPDocument36 pagesBMAT-Bedside Mobility Assessment Tool: by Amber Perez ADN, BSB, CSPHPConvalescent Nursing HomeNo ratings yet
- Fecal Incontinence Treatment & ManagementDocument11 pagesFecal Incontinence Treatment & ManagementParijatak AurvedaNo ratings yet
- Ecg Crit - CareDocument55 pagesEcg Crit - CarekrismatactayNo ratings yet
- Senior Center StudyDocument117 pagesSenior Center StudyIulian TNo ratings yet
- Chronic Inflammatory Demyelinating PolyneuropathyDocument7 pagesChronic Inflammatory Demyelinating PolyneuropathyApriliaNo ratings yet
- Josie King: As Told by Josie's Mother, Sorrel KingDocument1 pageJosie King: As Told by Josie's Mother, Sorrel KingWidyaNo ratings yet
- Josie King Story - Nurs 442 1Document2 pagesJosie King Story - Nurs 442 1api-558100249No ratings yet
- ShockDocument9 pagesShockapocruNo ratings yet
- Assessing Neurologic FunctionsDocument10 pagesAssessing Neurologic FunctionsDenise DizonNo ratings yet
- Shock and Circulatory FailureDocument8 pagesShock and Circulatory FailureOktaviana Sari DewiNo ratings yet
- Immuno-Pharmacology: Dr. Harshika Patel Pharmacology and Therapeutics II Date:23/05/2018 Time: 11am - 1pmDocument90 pagesImmuno-Pharmacology: Dr. Harshika Patel Pharmacology and Therapeutics II Date:23/05/2018 Time: 11am - 1pmBob MuneneNo ratings yet
- Blood Sample Normal Panic Values For Abgs: Clinical SignificanceDocument7 pagesBlood Sample Normal Panic Values For Abgs: Clinical SignificancegeonarcisoNo ratings yet
- Ostomias PDFDocument17 pagesOstomias PDFRicardo Uzcategui Arregui100% (1)
- Ch35 CardiovascularDocument11 pagesCh35 CardiovascularJessie Jennings100% (3)
- Cardiac Dysfunction in Neurocritical Care.Document14 pagesCardiac Dysfunction in Neurocritical Care.Angela Moreira ArteagaNo ratings yet
- CKD EsrdDocument83 pagesCKD EsrdRita Lakhani100% (1)
- ThrombocytopeniaDocument1 pageThrombocytopeniaanum786110No ratings yet
- Job Description of A Nurse AnesthetistDocument3 pagesJob Description of A Nurse AnesthetistlhalamNo ratings yet
- Review 2Document12 pagesReview 2Christine Rubio100% (1)
- Downtime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimeDocument5 pagesDowntime Daily Nursing Assessment & Care Plan: 1 of 5 Date: TimerupaliNo ratings yet
- ICBA NotesDocument60 pagesICBA NotesAndrew EldeiryNo ratings yet
- Chronic Inflammatory Demyelinating PolyradiculoneuropathyDocument12 pagesChronic Inflammatory Demyelinating Polyradiculoneuropathyrafael rocha novaesNo ratings yet
- CBQmedsurgDocument17 pagesCBQmedsurgshenric16No ratings yet
- PAS Quick GuideDocument1 pagePAS Quick GuideTracyNo ratings yet
- NURS 225V Principles III Data Collection ToolDocument2 pagesNURS 225V Principles III Data Collection ToolKrisNo ratings yet
- Pead 3 - Abdominal Pain and VommitingDocument22 pagesPead 3 - Abdominal Pain and Vommitingbbyes100% (1)
- MS Final 46 Blood or Lymphatic DisorderDocument4 pagesMS Final 46 Blood or Lymphatic DisorderZachary T Hall0% (1)
- Sinus Rhythm and Sinus and Atrial DysrhythmiasDocument41 pagesSinus Rhythm and Sinus and Atrial Dysrhythmiasclaudia brongNo ratings yet
- MS Final 49 UrinaryDocument3 pagesMS Final 49 UrinaryZachary T HallNo ratings yet
- Sinus Bradycardia: I. Sinus Dysrhythmias Description ManagementDocument4 pagesSinus Bradycardia: I. Sinus Dysrhythmias Description ManagementMargueretti Delos ReyesNo ratings yet
- Lab Workup: Practical Nursing Mohawk College 2014Document2 pagesLab Workup: Practical Nursing Mohawk College 2014Pawel PietruszczakNo ratings yet
- CH 27 Patient SafetyDocument11 pagesCH 27 Patient SafetyjoanneNo ratings yet
- LasixDocument1 pageLasixKatie McPeek100% (2)
- Chronic Kidney Disease: Prepared by Zakia RogerDocument27 pagesChronic Kidney Disease: Prepared by Zakia Rogerbene dugaNo ratings yet
- Disorders of Acid Base BalanceDocument1 pageDisorders of Acid Base BalanceLyn Domingo EllaquezNo ratings yet
- Constipation AlgorithmDocument1 pageConstipation AlgorithmIYERBKNo ratings yet
- This Study Resource Was: Assessment & Reasoning Cardiac SystemDocument6 pagesThis Study Resource Was: Assessment & Reasoning Cardiac SystemSharon TanveerNo ratings yet
- Chapter 06 NeuroDocument22 pagesChapter 06 NeuroKarla Fralala100% (1)
- Shockable RhythmsDocument37 pagesShockable RhythmsMike DavidNo ratings yet
- Peripheral Vascular Diseases NCLEXDocument6 pagesPeripheral Vascular Diseases NCLEXPotchiee PfizerNo ratings yet
- An Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFDocument6 pagesAn Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFkatherine dayagNo ratings yet
- Physical AssessmentDocument29 pagesPhysical AssessmentTheSweetpea501100% (1)
- Textbook ReadingDocument275 pagesTextbook ReadingNovitasari EkaNo ratings yet
- Code BlueDocument26 pagesCode BlueJenny CandraNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- AdultAcuteCareSetupAndCurriculumGuide 2017 02 21 LB 2 PDFDocument79 pagesAdultAcuteCareSetupAndCurriculumGuide 2017 02 21 LB 2 PDFShane LambertNo ratings yet
- Clinical ExaminationDocument11 pagesClinical ExaminationLaura GranadosNo ratings yet
- Drug StudyDocument9 pagesDrug StudyJannefer HernandezNo ratings yet
- How To Treat: Septic ShockDocument6 pagesHow To Treat: Septic ShockmeeandsoeNo ratings yet
- Patient's RightsDocument7 pagesPatient's RightsRichy100% (1)
- Ms Reviewer Renal UrinaryDocument5 pagesMs Reviewer Renal UrinaryAlyssa Nicole CajayonNo ratings yet
- N3102 Case Study: Musculoskeletal - Instructor Copy: Day 1 - Patient AssignmentDocument17 pagesN3102 Case Study: Musculoskeletal - Instructor Copy: Day 1 - Patient AssignmentBrittany LynnNo ratings yet
- Concept MapDocument6 pagesConcept Mapapi-499028250No ratings yet
- 8 Common Charting Mistakes To Avoi1aDocument4 pages8 Common Charting Mistakes To Avoi1aEggy PascualNo ratings yet
- Shock Types 141009102815 Conversion Gate01Document41 pagesShock Types 141009102815 Conversion Gate01Samjaisheel SamsonNo ratings yet
- ATI Flash Cards 05, Medications Affecting The Nervous SystemDocument110 pagesATI Flash Cards 05, Medications Affecting The Nervous SystemGiovanni MictilNo ratings yet
- Nursing 304 Nursing Care of The Client/Family With Select Sensory Health DeviationsDocument8 pagesNursing 304 Nursing Care of The Client/Family With Select Sensory Health Deviationsdlneisha61No ratings yet
- Nursing 304 Nursing Care of The Client/Family With Select Sensory Health DeviationsDocument8 pagesNursing 304 Nursing Care of The Client/Family With Select Sensory Health Deviationsdlneisha61No ratings yet
- Human Immunodeficiency Virus: Transmission of HIVDocument15 pagesHuman Immunodeficiency Virus: Transmission of HIVdlneisha61No ratings yet
- Integumentary Disorders Fall07ebDocument34 pagesIntegumentary Disorders Fall07ebdlneisha61No ratings yet
- Mental Health AssessmentDocument12 pagesMental Health Assessmentdlneisha61100% (4)
- Mental Health NursingDocument10 pagesMental Health Nursingdlneisha61100% (4)
- Mental Health Outline1Document25 pagesMental Health Outline1dlneisha61No ratings yet
- Hematology Outline For Blackboard Revised CDocument22 pagesHematology Outline For Blackboard Revised Cdlneisha61No ratings yet
- Impaired Skin Integrity and ConstipationDocument6 pagesImpaired Skin Integrity and Constipationdlneisha61100% (1)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Sexual Contact (Anal, Vaginal, Oral) With An HIV-infected PartnerDocument17 pagesSexual Contact (Anal, Vaginal, Oral) With An HIV-infected Partnerdlneisha61No ratings yet
- Hiv Study GuideDocument3 pagesHiv Study Guidedlneisha61No ratings yet
- Hematology Outline For Blackboard Revised CDocument22 pagesHematology Outline For Blackboard Revised Cdlneisha61No ratings yet
- GU Lisa RetypedDocument15 pagesGU Lisa Retypeddlneisha61No ratings yet
- Dosage Practice Problem GuideDocument20 pagesDosage Practice Problem Guidedlneisha6171% (7)
- Urinary System: TH RDDocument13 pagesUrinary System: TH RDdlneisha61No ratings yet
- Diabetes Mellitus Outline For BBDocument10 pagesDiabetes Mellitus Outline For BBdlneisha61No ratings yet
- GU Blackboard OutlineDocument15 pagesGU Blackboard Outlinedlneisha61No ratings yet
- Mental Health NursingDocument10 pagesMental Health Nursingdlneisha61100% (4)
- Concepts, Constructs, Variables and TheoryDocument6 pagesConcepts, Constructs, Variables and Theorydlneisha61100% (2)
- Girl: Dad, I Need A Few Supplies For School, and I Was Wondering If - . .Document3 pagesGirl: Dad, I Need A Few Supplies For School, and I Was Wondering If - . .AKSHATNo ratings yet
- Episode 5 The Global TeacherDocument8 pagesEpisode 5 The Global TeacherEllieza Bauto SantosNo ratings yet
- 160 LW Bending Tester v2.0Document4 pages160 LW Bending Tester v2.0Sá StrapassonNo ratings yet
- Literature Review LichenDocument7 pagesLiterature Review LichenNur Fazrina CGNo ratings yet
- PDF Certificacion 3dsmaxDocument2 pagesPDF Certificacion 3dsmaxAriel Carrasco AlmanzaNo ratings yet
- Lesson Plan in Science III ObservationDocument2 pagesLesson Plan in Science III ObservationTrishaAnnSantiagoFidelNo ratings yet
- Bad SenarioDocument19 pagesBad SenarioHussain ElboshyNo ratings yet
- BrookfieldDocument8 pagesBrookfieldFariha Naseer Haral - 28336/TCHR/JVAITNo ratings yet
- KFC 225 Installation ManualDocument2 pagesKFC 225 Installation Manualsunarya0% (1)
- Mis 2023Document62 pagesMis 2023Ana Mae MunsayacNo ratings yet
- The Impact of Video Gaming To The Academic Performance of The Psychology Students in San Beda UniversityDocument5 pagesThe Impact of Video Gaming To The Academic Performance of The Psychology Students in San Beda UniversityMarky Laury GameplaysNo ratings yet
- They Cried MonsterDocument13 pagesThey Cried MonstermassuroNo ratings yet
- Final BasantDocument22 pagesFinal BasantMuqaddas IsrarNo ratings yet
- Introduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF VersionDocument62 pagesIntroduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF Versionmary.krueger918100% (50)
- Landow - The Rhetoric of HypermediaDocument26 pagesLandow - The Rhetoric of HypermediaMario RossiNo ratings yet
- Sample Programs in CDocument37 pagesSample Programs in CNoel JosephNo ratings yet
- Securities and Exchange Commission: Non-Holding of Annual MeetingDocument2 pagesSecurities and Exchange Commission: Non-Holding of Annual MeetingBea AlonzoNo ratings yet
- A Portrayal of Gender and A Description of Gender Roles in SelectDocument429 pagesA Portrayal of Gender and A Description of Gender Roles in SelectPtah El100% (1)
- 10 Chapter 3Document29 pages10 Chapter 3felefel100% (1)
- Zone Raiders (Sci Fi 28mm)Document49 pagesZone Raiders (Sci Fi 28mm)Burrps Burrpington100% (3)
- Pengaruh Kompetensi Spiritual Guru Pendidikan Agama Kristen Terhadap Pertumbuhan Iman SiswaDocument13 pagesPengaruh Kompetensi Spiritual Guru Pendidikan Agama Kristen Terhadap Pertumbuhan Iman SiswaK'lala GrianNo ratings yet
- God As CreatorDocument2 pagesGod As CreatorNeil MayorNo ratings yet
- Faust Part Two - Johann Wolfgang Von GoetheDocument401 pagesFaust Part Two - Johann Wolfgang Von GoetherharsianiNo ratings yet
- Does Moore Succeed in Refuting IdealismDocument5 pagesDoes Moore Succeed in Refuting IdealismharryNo ratings yet
- Finding Roots of Equations Bracketing MethodsDocument11 pagesFinding Roots of Equations Bracketing MethodsmebrahtenNo ratings yet
- Lesson Plan 2 Revised - Morgan LegrandDocument19 pagesLesson Plan 2 Revised - Morgan Legrandapi-540805523No ratings yet
- FA2Document6 pagesFA2yuktiNo ratings yet
- Presente Progresive TenseDocument21 pagesPresente Progresive TenseAriana ChanganaquiNo ratings yet
- Book Review Leffel Cateura, Oil Painting SecretsDocument4 pagesBook Review Leffel Cateura, Oil Painting SecretsAnonymous H3kGwRFiENo ratings yet
- Software Quality Metrics MethodologyDocument17 pagesSoftware Quality Metrics MethodologySumit RajputNo ratings yet