Professional Documents
Culture Documents
Proximal Radial Compression Neuropathy: Brian Rinker, MD, Charles R. Effron, MD, and Robert W. Beasley, MD
Uploaded by
Rod VROriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Proximal Radial Compression Neuropathy: Brian Rinker, MD, Charles R. Effron, MD, and Robert W. Beasley, MD
Uploaded by
Rod VRCopyright:
Available Formats
ORIGINAL ARTICLE
Proximal Radial Compression Neuropathy
Brian Rinker, MD,* Charles R. Effron, MD, and Robert W. Beasley, MD*
Abstract: Proximal radial nerve compression occurs infrequently and is diagnosed successfully even less frequently. A large clinical series of patients with proximal radial nerve compression neuropathy was reviewed to determine better the common symptoms, physical ndings, and electrodiagnostic ndings, and to identify the predictors of better or worse outcome after surgical decompression. Seventy-nine proximal radial compression neuropathies were treated in 71 patients by the same surgeon between 1991 and 2000. The most consistent symptoms were deep aching pain in the forearm, pain radiation to the neck and shoulder, and a heavy sensation of the affected arm. The most common physical ndings were tenderness over the radial nerve at the supinator muscle level, pain on resisted supination, and the presence of a Tinel sign over the radial forearm. Electrophysiologic studies were of limited value in diagnosis, with 90% of patients having normal ndings. On operation, prominent pathology of the posterior interosseous nerve was observed in 36 of 79 limbs (46%). Follow-up ranged from 12 to 86 months (mean, 21 months) with no signicant complications or recurrence of symptoms. Of the 79 nerve decompressions, 77% had excellent recovery and 20% were judged to be good. Of 69 patients employed when treated, 60 resumed gainful employment, including 53 who returned to their regular jobs. Proximal radial compression neuropathies are uncommon but present with a basic constellation of symptoms and physical ndings, and decompression can provide excellent relief of symptoms. (Ann Plast Surg 2004;52: 174 180)
he idea that pain in the elbow and proximal forearm may be caused by compression of the posterior interosseous nerve was rst suggested by Winckworth1 in a letter to the
Received March 23, 2003, and accepted for publication, after revision, May 20, 2003. From the *Institute of Reconstructive Plastic Surgery, New York University Medical Center, and the Department of Neurology, The Mount Sinai Medical Center, New York, NY. Presented at the 81st annual meeting of the American Association of Plastic Surgeons, Seattle, WA, April 29, 2002. Reprints: Brian Rinker, MD, Division of Plastic Surgery, University of Kentucky, Kentucky Clinic K454, Lexington, KY 40536. Tel: 859-3235887, Fax: 859-323-3823, E-mail: brink2@uky.edu Copyright 2004 by Lippincott Williams & Wilkins ISSN: 0148-7043/04/5202-0174 DOI: 10.1097/01.SAP.0000099959.59748.85
editors of the British Medical Journal in 1883. This concept was revived in the modern era by Capener,2 and in 1972 Roles and Maudsley3 reported a series of 38 proximal forearm radial neuropathies treated successfully by surgical decompression. Recent reviews, however, have been more pessimistic, reporting unfavorable treatment results and even suggesting that the condition does not exist.4 6 The radial nerve emerges from the intermuscular septum on the lateral arm and descends distally along the border of the brachialis muscle. Approximately 2 cm distal to the elbow, the radial nerve divides into the posterior interosseous nerve and the supercial sensory divisions (Fig. 1). The posterior interosseous nerve passes beneath the brous proximal margin of the supinator muscle, known as the arcade of Frohse, and bifurcates to innervate the extensor carpi ulnaris muscle and the digital extensor muscles. Lister et al,7 in 1979, suggested 4 possible sites of radial nerve compression: (1) the brous bands anterior to the radial head, (2) the radial recurrent fan of vessels described by Henry, (3) the tendinous margin of the extensor carpi radialis brevis (ECRB), and (4) the arcade of Frohse. This list has been repeated in the literature sufciently to become dogma, but with the exception of the arcade of Frohse, there are few clinical or anatomic data to support any of these as notable causes of symptomatic radial neuropathy.8 10 Radial nerve compression neuropathies are rare clinical entities and are challenging to diagnose. The symptoms are vague and ill dened, and the physical examination ndings vary greatly. There are no well-established electrophysiologic criteria for diagnosing the condition. To complicate matters further, there is no agreement on the best mode of surgical treatment once the diagnosis has been made. The current study is a retrospective review of a clinical series and represents the largest in the English literature. The purpose of the study is to determine the most consistent symptoms, physical ndings, and electrodiagnostic ndings in patients with proximal radial compression neuropathies, and to determine the outcome of surgical treatment. It is hoped that with the establishment of more clearly dened diagnostic criteria, patient selection and ultimately the outcome of treatment might be improved.
Annals of Plastic Surgery Volume 52, Number 2, February 2004
174
Annals of Plastic Surgery Volume 52, Number 2, February 2004
Proximal Radial Compression Neuropathy
FIGURE 1. Anatomic diagram of the proximal forearm showing the course of the radial nerve and its divisions.
METHODS
Between 1991 and 2000, 79 proximal radial compression neuropathies were treated surgically in 71 patients by the same surgeon. Data collection was performed by review of the medical records. Additional information (resolution of symptoms, work status) was obtained by telephone interviews in 30 patients. In the majority of patients this information was evident in the medical record. Follow-up, dened as the time from radial nerve decompression to the most recent physical examination, ranged from 12 to 86 months (average, 21 months). Patients were typically followed for 12 to 18 months after the surgical procedure, but occasionally returned for treatment of an unrelated complaint several years later, at which time a follow-up examination was performed.
Surgical Technique
Nonoperative management was used initially in 75 of 79 patients, which consisted of rest and a tapered course of oral corticosteroids. In our experience, favorable responses to nonoperative management are infrequent (probably less than 10%). Surgical decompression was generally performed after 3 months if symptoms warranted and if improvement had not been observed. In the patients in whom focal muscle weakness was present (n 4), prompt decompression was performed. The same surgical technique was used in all 79 patients. All surgical procedures were performed by the same surgeon.
2004 Lippincott Williams & Wilkins
General anesthesia was used in 77 patients; local inltration anesthesia was used for 2 patients in whom general anesthesia was contraindicated. A total of 100 mg hydrocortisone was administered intravenously before skin incision in all patients. Intravenous corticosteroids are administered before all proximal nerve decompressions in our practice. This has not been studied rigorously, but we believe it reduces postoperative swelling and inammation. A longitudinal incision directly over the course of the supercial branch of the radial nerve is used. This is along a line between the radial wrist extensors and the brachioradialis muscles, and begins approximately 1 cm distal to the skin exion crease of the elbow (Fig. 2, above). After opening the muscle fascia, passive extension and exion of the wrist permits identication of the demarcation between the radial wrist extensors (ECRB and extensor carpus radialis longus) and the brachioradialis muscle. Blunt dissection is used to open the physiologic plane between them, which leads to the radial nerve, with the supercial sensory branch being the rst encountered (Fig. 2, center). Dissection is carried distal to proximal along this nerves dorsal surface until the main trunk of the radial nerve is encountered. Immediately distal to the elbow, the radial nerve is consistently crossed transversely by several moderate-size vessels: the leash of Henry. These are divided to provide access to the nerve, but they do not seem to be a site of nerve compression. The nerve is lifted and rolled gently to expose the posterior interosseous branch arising from its deep surface. Dissection is then carried out in a proximal to distal fashion along this nerve, and a generous resection is performed of the brous proximal margin of the supinator muscle: the arcade of Frohse (Fig. 2, below). In all 79 patients, this structure was observed to be dense and ligamentous in nature. Closed blunt-tipped scissors are then passed distally down both the supercial and posterior interosseous nerve branches to conrm that no residual constrictions are present. They also are passed proximally along the main trunk of the radial nerve to 2 cm proximal to the elbow. Meticulous hemostasis is achieved and the wounds are closed by approximating subcutaneous tissues and wound margins. A simple soft dressing is applied, without elbow immobilization. Patients are instructed to rest for 24 hours and to maintain strict, continuous elevation of the limb for 48 hours. Finger, thumb, and shoulder exercises are begun on postoperative day 2. Formal therapy is not used. Sutures are removed on postoperative days 10 to 12, after which the scar is taped longitudinally with 1-inch paper tape for a minimum of 2 months. This has been shown to reduce scar hypertrophy markedly11 (Fig. 3).
175
Rinker et al
Annals of Plastic Surgery Volume 52, Number 2, February 2004
FIGURE 3. (Above) Longitudinal taping of the incision was used to minimize scar hypertrophy. (Below) A typically good scar 2 years after surgery.
Rating of Treatment Results
Treatment results were assessed according to the system of Roles and Maudsley,3 in which an excellent result is dened as no pain, full movement and full activity; a good result is dened as occasional discomfort, full movement, and full activity; and a fair result is dened as some continuous discomfort, but improved. All patients underwent a postoperative evaluation by the senior author. Using the list of presenting complaints as a guide, patients were questioned about their symptomatic relief and activity level. A thorough examination of the affected limb was performed to assess sensibility, strength, and motion. Results were recorded meticulously in a standardized fashion. The nal assignment of an excellent, good, or fair result was made by a review of this record. The timing of the evaluation ranged from 12 to 86 months postoperatively (mean, 21 months). The treatment goal of any nerve decompression procedure is symptomatic relief. With this in mind, the patients
2004 Lippincott Williams & Wilkins
FIGURE 2. (Above) A longitudinal incision is made over the interval between the radial wrist extensors and the brachioradialis muscles in the proximal forearm. (Center) Dissection is carried out in the physiologic plane between these muscles. The superficial branch is encountered first. (Below) The fibrous proximal margin of the supinator muscle, or arcade of Frohse, is divided. If gross pathology of the nerve is present, it is seen beneath this structure once it has been divided.
176
Annals of Plastic Surgery Volume 52, Number 2, February 2004
Proximal Radial Compression Neuropathy
were divided into 2 groups: those with complete symptomatic relief (ie, an excellent outcome) and those with incomplete symptomatic relief (a good or worse outcome). Logistic regression analysis was used to assess which factors were predictive of better outcome. The factors subjected to analysis (independent variables) were duration of symptoms before consultation, gender, presenting complaint, abnormal ndings on electrodiagnostic testing, presence of a workers compensation claim, age, presence of visible nerve pathology on exploration, and prior hand surgery.
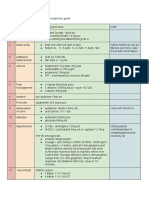
TABLE 2. Prior Hand Procedures Procedure Carpal tunnel release Ulnar nerve transposition Surgery for lateral epicondylitis Surgery for DeQuervain tendonitis Trigger nger release Proximal median nerve decompression n 25 8 7 7 6 6 % 35 11 10 10 8 8
RESULTS
The treatment group included 34 men and 37 women. The average age was 42 years (range, 2172 years). Fifty-one of the 71 patients (72%) had a workers compensation claim relating to the upper extremity complaint. Onset of symptoms averaged 24 months before our initial evaluation, and the majority of patients had sought help from at least 1 other hand surgeon (Table 1). Fifty-two patients (73%) had undergone at least 1 surgical procedure on their upper limb before our initial evaluation (Table 2). Seven patients had undergone surgical treatment of suspected lateral epicondylitis on the affected side without relief of primary symptoms. The most common presenting chief complaint, occurring in 62 patients (87%), was a deep aching pain in the proximal forearm. This was very often of acute onset and was usually associated with pain radiation into the shoulder and neck. The third most frequently reported complaint was a sense of heaviness of the arm, followed by an inability to sleep on the affected side (Table 3). Even a meticulous initial physical examination was often inconclusive. It was frequently necessary to examine a patient on 2 or more occasions before the diagnosis could be made condently, especially in patients in whom more than 1 neuropathy coexisted. The most consistent preoperative physical nding was localized and prominent tenderness over the radial nerve at the level of the proximal margin of the supinator muscle, with light digital pressure there accentuating the exact chief complaint (Fig. 4). This was found in 70 of 71 patients. Supinator muscle stress against resistance
TABLE 3. Presenting Complaints (N 71) Complaint Deep aching pain in forearm Pain radiation to neck and shoulder A heavy sensation in the arm Cannot sleep on affected side Weakness Fatigues easily n 62 43 19 19 14 12 % 87 61 27 27 20 17
FIGURE 4. The most consistent physical finding is localized tenderness over the radial nerve in the proximal forearm.
TABLE 1. Patient Data Variable No. of patients Age, y (average) Male/Female, n Right/left dominance, n Workers compensation, n (%) Average time between onset of symptoms and initial evaluation, n Data 71 2172 y (average) 34/37 68/3 51 (72) 24
reproduced the patients symptoms in 39 cases (55%). Sensory disturbances were rare. Only 14 patients (20%) had diminished skin sensibility in the radial nerve distribution. Only 4 patients (6%) had demonstrable weakness of nger extension. The oft-cited middle nger extension test was not found to be useful (Table 4). Electrophysiologic studies were performed before surgical decompression in 60 patients. In most instances, the patient had seen at least 1 other hand surgeon before the initial evaluation and had already undergone electrodiagnos-
2004 Lippincott Williams & Wilkins
177
Rinker et al
Annals of Plastic Surgery Volume 52, Number 2, February 2004
TABLE 4. Findings on Physical Examination (N 71) Finding Radial nerve tenderness at supinator Pain on resisted supination Tinel sign at radial nerve in forearm Diminished sensibility of hand EIP/EDC weakness n 70 39 30 14 4 % 99 55 42 20 6
tic testing. Nineteen patients did not undergo testing before surgical decompression. Abnormal ndings relating to the radial nerve were present in only 14 of 60 patients (23%). The most common nding was an increase in polyphasic electromyographic patterns in the EIP and EDC muscles (Table 5). The results of the electrophysiologic studies rarely impacted decision making. In a few cases in which the physical examination was equivocal, the studies were helpful in ruling out cervical radiculopathy. On operation, prominent pathology was observed in 36 of the 79 limbs (46%). When present, these changes consisted of increased vascularity and frequently a gross hourglass-type indentation of the posterior interosseous division of the radial nerve. In each case these changes were observed to be directly beneath the brous proximal margin of the supinator muscle, the arcade of Frohse, and were seen only after the release of this structure (Fig. 5) In this series, no abnormalities were observed at the margin of the ECRB or beneath the vascular leash of Henry. On 65 occasions (82%), the patient had other surgical procedures performed at the time of radial nerve decompression (Table 6). The most commonly performed were carpal tunnel release (42%) and proximal median nerve decompression (44%). Using the criteria dened earlier for evaluation of the 79 radial nerve decompressions performed, 61 (77%) had excellent results and 12 (20%) were judged to be good. Two
FIGURE 5. A gross indentation of the posterior interosseous nerve beneath the arcade of Frohse. This finding was present in 15% of patients, although inflammation of the nerve was observed in this location in 46%.
TABLE 6. Other Procedures Done at the Time of Radial Nerve Decompression (N 79) Procedure Proximal median nerve decompression Carpal tunnel release Submuscular transposition of ulnar nerve Surgery for lateral epicondylitis Trigger nger release Decompression of DeQuervain tendonitis Ulnar nerve decompression at Guyons canal No other procedures Limbs, n 35 33 22 8 7 5 5 14 % 44 42 28 10 9 6 6 18
TABLE 5. Findings of Preoperative Electrophysiologic Studies (N 60) Finding Increased polyphasic EMG patterns in the EDC or EIP muscles Decreased sensory conduction velocity Decreased motor conduction velocity ECU irritability Normal study n 7 5 3 1 46 % 12 8 7 1 77
patients had fair results. Using a logistic regression analysis of multiple independent variables, no signicant difference in outcome existed between those patients involved in a workers compensation claim and those who were not. Nor was a significant difference in outcome found to be associated with age, duration of symptoms before surgery, prior hand surgery, presence of an abnormal electrophysiologic study, or evidence of gross nerve pathology at the time of operation. However, gender was found to be a signicant predictive factor, with female patients having a less favorable outcome (P 0.05). Of the 69 patients employed at the time of treatment, 60 returned to gainful employment, including 53 who returned to their regular job. The 9 others were either at retirement age or had multiple other problems.
DISCUSSION
Several series of radial nerve decompressions in the proximal forearm have been reported in the literature1214
2004 Lippincott Williams & Wilkins
EMG, electromyographic; EDC, extensor digitorum communis; EIP, extensor indicis proprius; ECU, extensor carpi ulnaris.
178
Annals of Plastic Surgery Volume 52, Number 2, February 2004
Proximal Radial Compression Neuropathy
since the report of Roles and Maudsley,3 but the current series is the largest in the English literature. The condition is uncommon. In the current series, 79 radial compression neuropathies were treated surgically during a 10-year period. In contrast, more than 400 patients underwent carpal tunnel release by the same surgeon during that time period. We are in agreement with the majority of previous authors that the most frequent presenting symptom is pain in the proximal forearm. We have noted that a large percentage of patients also complain of a peculiar heaviness of the affected arm, which we have not found to be present in other painful conditions of the elbow and forearm, and which may help to point the way toward the diagnosis. It may seem paradoxical that compression of a motor nerve should cause pain as the primary symptom. In addition to afferent bers, however, the posterior interosseous nerve carries sensory afferent bers from the wrist joint and afferent bers from the muscles it serves. Sensations of pain or heaviness may very well be mediated by these pathways. The key physical nding in radial nerve compression is tenderness of the nerve in the proximal forearm at the level of the supinator muscle. There is normally some tenderness over the nerve, but it should not be tender to light pressure, such as the light pressure used to palpate a peripheral pulse. When in doubt, the opposite limb should be tested for comparison. The resisted supination test was also found to be helpful. Unlike Roles and Maudsley,3 and Lister et al,7 we have not found the resisted middle nger test to be useful. The maneuver produces pain in some patients, but it is also painful in the setting of lateral epicondylitis, one of the conditions from which radial neuropathy needs to be differentiated. We do not perform or advocate lidocaine injection of the radial nerve as a diagnostic aid, because this may traumatize an already inamed nerve and may worsen symptoms. Twenty percent of patients in this series had evidence of skin sensibility changes in the distribution of the supercial sensory division of the radial nerve. This agrees with the experience of previous authors,13,15 but is somewhat difcult to explain in light of the fact that it is the posterior interosseous division alone that seems, in most if not all cases, to be the nerve that is compressed. As the sensory branch separates from the main trunk of the radial nerve just a few millimeters proximal to the arcade of Frohse, it may be that regional inammation can affect both nerves. In addition, compression at 1 point on a nerve may increase the susceptibility toward neuropathy along the entire course of the nerve, the so-called double-crush syndrome.16 We agree with previous authors that electrophysiologic testing offers very limited help in the diagnosis of radial neuropathy in the proximal forearm. Occasionally, testing can be useful in ruling out cervical radiculopathy if the physical examination is equivocal. (Patients with cervical radiculopathy may present with forearm pain, weakness, and a heavy
2004 Lippincott Williams & Wilkins
arm.) Reliable motor nerve conduction velocity data are rarely obtained because of technical factors relating to the tolerance of painful proximal stimulation and needle motion with stimulation. Surface electrodes are not sufciently sensitive. As mentioned earlier, abnormal electromyographic ndings are sometimes seen, but this is usually observed in severely affected patients with pronounced physical ndings whose diagnosis is not in question. (Three of the 7 patients with abnormal electromyographic ndings had weakness of nger extension.) As in all upper limb neuropathies, a careful history and physical examination should supersede electrodiagnostic testing in reaching a diagnosis if the 2 are not in full agreement. We do not believe electrodiagnostic testing should be considered mandatory before surgical decompression of the radial nerve, particularly if the history and physical examination are strongly suggestive. In this series, 73% of patients had at least 1 other prior inammatory condition of the hand, and in 65 limbs (82%) there was a coexisting condition for which a procedure was performed at the time of radial nerve decompression. The most common coexisting condition was median nerve compression in the proximal forearm. Despite its spatial proximity to the radial nerve, proximal median neuropathy is not difcult to distinguish clinically from radial neuropathy. Each has a unique set of symptoms and physical signs, and the results of treatment of the 2 conditions can be assessed independently. It should not be surprising that more than 1 nerve was affected in a large subset of the series population. It is a consistent observation that the individual who has developed 2 or more connective tissue inammatory disorders, such as carpal tunnel syndrome or lateral epicondylitis, has a high probability of developing subsequent inammatory disorders. There clearly is an -itis type, which was recognized and termed the mesenchymal syndrome, several decades ago.17 When gross compression or inammation of the radial nerve was observed on operation, it was invariably found beneath the brous arcade of Frohse. We have seen no convincing evidence, either clinically or in the several good anatomic papers on the subject, of another notable point of compression of the radial nerve or its branches in the proximal forearm. The vascular arcades formed by the radial recurrent vessels (leash of Henry) are always encountered and should be ligated carefully, but do not seem to be a cause of nerve compression. It is also noted that these vessels appear identical in fresh cadaveric dissections of presumably unaffected individuals. Spinner10 reported that the arcade of Frohse was brous in 30% of the adults he examined, and a more recent study found it to be brous in roughly 50%.9 This structure was observed to have a brous component in all the individuals in this series and may be an anatomic factor that predisposes certain individuals to radial neuropathy.
179
Rinker et al
Annals of Plastic Surgery Volume 52, Number 2, February 2004
Prominent pathology of the nerve was not observed in the majority of patients (54%). Despite this, most patients experienced improvement of symptoms. As in any uncontrolled study, there exists the possibility of a placebo effect, as was demonstrated in a recent paper on knee arthroscopy.18 However, prominent pathology is often not observed in other more common nerve compression syndromes, such as carpal tunnel, so it is reasonable to expect it would not always be observed in proximal radial nerve compression. Our large series of 79 nerve decompressions had 73 (79%) excellent or good results. This is comparable with the results reported in some early and smaller series. Roles and Maudsley3 reported good or excellent results in 35 of 38 limbs. Hagert et al12 and Lister et al7 described excellent or good results in 42 of 50 and 19 of 20 patients respectively. For reasons not entirely clear, some series after these have reported results that are signicantly less favorable.5,6 Treatment results were not impacted in our series by the presence of a workers compensation claim. We think this is largely the result of careful diagnosis. Often the patient was examined on 2 or more occasions to establish fully the diagnosis. Secondary gain and the unmotivated patient are unpleasant facts of life in hand surgery practice, but in our experience most patients want to get better and return to work. Results were also not affected by the duration of symptoms before initial consultation. In fact, many individuals made a full recovery even after experiencing symptoms for several years. This encouraging and somewhat surprising nding suggests that compression neuropathy of the radial nerve does not readily progress to irreversible nerve damage. This may relate to the fact that the affected nerve branch, the posterior interosseous, is almost entirely composed of heavily myelinated motor bers, which may not be as sensitive to ischemic injury as sensory bers. Radial compression neuropathy in the proximal forearm can be the cause of initially vague and ill-dened arm
complaints. We outlined the characteristic symptoms and ndings on physical examination that will lead to the diagnosis and have conrmed that with appropriate treatment most patients can be cured. REFERENCES
1. Winckworth CE. Lawn tennis elbow [letter]. BMJ. 1883;23:708. 2. Capener N. The vulnerability of the posterior interosseous nerve of the forearm. A case report and an anatomical study. J Bone Joint Surg Br. 1966;48:770 773. 3. Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972;54:499 508. 4. Rosenbaum R. Surgical treatment for radial tunnel syndrome [letter]. J Hand Surg [Am]. 1999;24A:13451346. 5. Sotereanos DG, Varitimidis SE, Giannakopoulos PN, et al. Results of surgical treatment for radial tunnel syndrome. J Hand Surg [Am]. 1999;24A:566 570. 6. Verhaar J, Spaans F. Radial tunnel syndrome: an investigation of compression neuropathy as a possible cause. J Bone Joint Surg Am. 1991;73A:539 544. 7. Lister GD, Belsole RB, Kleinert HE. The radial tunnel syndrome. J Hand Surg. 1979;4:5259. 8. Maffulli N, Maffulli F. Transient entrapment neuropathy of the posterior interosseous nerve in violin players. J Neurol Neurosurg Psychiatry. 1991;54:65 67. 9. Prasartritha T, Liupolvanish P, Rojanakit A. A study of the posterior interosseous nerve (PIN) and the radial tunnel in 30 Thai cadavers. J Hand Surg [Am]. 1993;18A:107112. 10. Spinner M. The arcade of Frohse and its relationship to posterior interosseous nerve paralysis. J Bone Joint Surg Br. 1968;50:809 812. 11. Reiffel R. Prevention of hypertrophic scars by long-term paper tape application. Plast Reconstr Surg. 1995;97:17151718. 12. Hagert CG, Lundborg G, Hansen T. Entrapment of the posterior interosseous nerve. Scand J Plast Reconstr Surg. 1977;11:205212. 13. Jebson PJL, Engber WD. Radial tunnel syndrome: long-term results of surgical decompression. J Hand Surg [Am]. 1997;22A:889 896. 14. Moss SH, Switzer HE. Radial tunnel syndrome: a spectrum of clinical presentations. J Hand Surg. 1983;8:414 420. 15. Crawford GP. Radial tunnel syndrome [letter]. J Hand Surg. 1984;9: 451 452. 16. Upton ARN, McComas AJ. The double crush in nerve entrapment syndromes. Lancet 1973;ii:359 362. 17. Nirschl RP. Mesenchymal syndrome. Va Med. 1969;96:659. 18. Moseley JB, OMalley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81 88.
180
2004 Lippincott Williams & Wilkins
You might also like
- Current Techniques in Canine and Feline NeurosurgeryFrom EverandCurrent Techniques in Canine and Feline NeurosurgeryAndy ShoresNo ratings yet
- Metastatic Spine Disease: A Guide to Diagnosis and ManagementFrom EverandMetastatic Spine Disease: A Guide to Diagnosis and ManagementRex A. W. MarcoNo ratings yet
- "Idiopathic" Shoulder Pain and Dysfunction From Carpal Tunnel Syndrome and Cubital Tunnel Syndrome - PMCDocument13 pages"Idiopathic" Shoulder Pain and Dysfunction From Carpal Tunnel Syndrome and Cubital Tunnel Syndrome - PMCArghya DebNo ratings yet
- 1 s2.0 S1878875018300159 MainDocument9 pages1 s2.0 S1878875018300159 MainAlexandreNo ratings yet
- Research ArticleDocument7 pagesResearch Articlefm_askaNo ratings yet
- Pi Is 0022522319367212Document8 pagesPi Is 0022522319367212Robert ChristevenNo ratings yet
- Original Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global OutcomeDocument6 pagesOriginal Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global Outcomeasep budiyantoNo ratings yet
- Denervation of Hand JointsDocument42 pagesDenervation of Hand JointsHand SurgeryNo ratings yet
- Clune Al Nerve 20Document20 pagesClune Al Nerve 20ironbody4lifeNo ratings yet
- Spinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SDocument3 pagesSpinal Epidural Cavernous Hemangiomas in The 2024 International Journal of SRonald QuezadaNo ratings yet
- Report Information From Proquest: 10 January 2015 11:43Document27 pagesReport Information From Proquest: 10 January 2015 11:43Ken SsdNo ratings yet
- Miyamoto 2010 JBJS Current Concepts Review Distal-Biceps-Tendon-Injuries PDFDocument12 pagesMiyamoto 2010 JBJS Current Concepts Review Distal-Biceps-Tendon-Injuries PDFKuozram No MasNo ratings yet
- Jns 2000 92 1 0052Document6 pagesJns 2000 92 1 0052Nicolas AdrianoNo ratings yet
- Weiner 2008Document6 pagesWeiner 2008Indira Ulfa DunandNo ratings yet
- Implications For The Treatment of Chronic HeadachesDocument5 pagesImplications For The Treatment of Chronic HeadachesCloé SzcNo ratings yet
- Upper Extremity Regional Anesthesia Techniques A Comprehensive Review For Clinical Anesthesiologists BestPracResAnest 2020Document17 pagesUpper Extremity Regional Anesthesia Techniques A Comprehensive Review For Clinical Anesthesiologists BestPracResAnest 2020RicardoNo ratings yet
- Songcharoen 1995Document5 pagesSongcharoen 1995Le Manh ThuongNo ratings yet
- Understanding Carpal Tunnel Syndrome.4Document8 pagesUnderstanding Carpal Tunnel Syndrome.4ayu permata dewiNo ratings yet
- Low Thoracic Erector Spinae Plane Block For PeriopDocument10 pagesLow Thoracic Erector Spinae Plane Block For Periopmelanicahyani4646No ratings yet
- Tens 1Document8 pagesTens 1marcelogascon.oNo ratings yet
- Case StudyDocument15 pagesCase StudyWincy Faith SalazarNo ratings yet
- Results of Surgical TreatmentDocument4 pagesResults of Surgical TreatmentChristine Yohana SianturiNo ratings yet
- Suprascapular Neuropathy in Volleyball Players: Original StudyDocument4 pagesSuprascapular Neuropathy in Volleyball Players: Original StudyborninbrooklynNo ratings yet
- Ajol File Journals - 414 - Articles - 212953 - Submission - Proof - 212953 4933 526597 1 10 20210819Document7 pagesAjol File Journals - 414 - Articles - 212953 - Submission - Proof - 212953 4933 526597 1 10 20210819Syifaihsani AzlaNo ratings yet
- Contreras 1998Document7 pagesContreras 1998Hương HuỳnhNo ratings yet
- Elbow Study 1Document8 pagesElbow Study 1Prashant SurtiNo ratings yet
- A Review of Lumbar Radiculopathy, Diagnosis, and TreatmentDocument7 pagesA Review of Lumbar Radiculopathy, Diagnosis, and TreatmentZuraidaNo ratings yet
- Arthroscopic Bursectomy For Recalcitrant Trochanteric BursitisDocument6 pagesArthroscopic Bursectomy For Recalcitrant Trochanteric BursitisGökhan PehlivanoğluNo ratings yet
- Spinal Diseases DetensorDocument4 pagesSpinal Diseases DetensorАлексNo ratings yet
- Giacalone 2015Document7 pagesGiacalone 2015Joseval FilhoNo ratings yet
- Compartement SyndromeDocument6 pagesCompartement SyndromeAnna ApsariNo ratings yet
- Bifid Median Nerve in Patients With Carpal Tunnel SyndromeDocument8 pagesBifid Median Nerve in Patients With Carpal Tunnel SyndromeAnnandra RahmanNo ratings yet
- Loukas Et Al-2013-Clinical AnatomyDocument3 pagesLoukas Et Al-2013-Clinical AnatomyChrissNo ratings yet
- Gay 2010Document6 pagesGay 2010Tania salais obregonNo ratings yet
- Radial Nerve Entrapment in A Humeral Fracture Callus: Case ReportDocument4 pagesRadial Nerve Entrapment in A Humeral Fracture Callus: Case ReportMuhammad RezaNo ratings yet
- Paper Laringeo SuperiorDocument8 pagesPaper Laringeo SuperiorKaren PalaciosNo ratings yet
- Headache Terapi RadiofrequencyDocument14 pagesHeadache Terapi RadiofrequencyHardiyanti HermanNo ratings yet
- Rodilla Inervación Tran2018 PDFDocument8 pagesRodilla Inervación Tran2018 PDFLore BarreraNo ratings yet
- Original Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve BlockDocument7 pagesOriginal Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve Blockandrew herringNo ratings yet
- (2017) RCT - Efficacy of Radial Extracorporeal Shock Wave Therapy on Lateral Epicondylosis, and Changes in the Common Extensor Tendon Stiffness with Pretherapy and Posttherapy in Real-Time SonoelastographyDocument8 pages(2017) RCT - Efficacy of Radial Extracorporeal Shock Wave Therapy on Lateral Epicondylosis, and Changes in the Common Extensor Tendon Stiffness with Pretherapy and Posttherapy in Real-Time Sonoelastographycalixto1995No ratings yet
- Patient Safety in The Operating RoomDocument5 pagesPatient Safety in The Operating RoompabelloncatNo ratings yet
- Mejrh 134171Document9 pagesMejrh 134171Amazonia clinicaNo ratings yet
- Spec MRI Distinguish Acue TM of NMOSD N Infarction. Kister Et Al 2015Document21 pagesSpec MRI Distinguish Acue TM of NMOSD N Infarction. Kister Et Al 2015Ido BramantyaNo ratings yet
- Compression of The Posterior Interosseous Nerve Sec 2024 International JournDocument4 pagesCompression of The Posterior Interosseous Nerve Sec 2024 International JournRonald QuezadaNo ratings yet
- Concurrent Effects of Dry Needling and Electrical Stimulation in The Management of Upper Extremity HemiparesisDocument5 pagesConcurrent Effects of Dry Needling and Electrical Stimulation in The Management of Upper Extremity HemiparesisFarel LaisyaNo ratings yet
- Efficacy of Contra-Lateral Neurodynamics On Median Nerve Extensibility in Cervical Radiculopathy PatientsDocument6 pagesEfficacy of Contra-Lateral Neurodynamics On Median Nerve Extensibility in Cervical Radiculopathy PatientsSylvia Grace100% (1)
- EpicondilteDocument7 pagesEpicondilteRicardo fariaNo ratings yet
- Uncorrected Author ProofDocument11 pagesUncorrected Author Proofprakashborade6No ratings yet
- 7 12011 9 Focus11187 PDFDocument8 pages7 12011 9 Focus11187 PDFSatria Bayu PratamaNo ratings yet
- Brachial Plexus Anesthesia: A Review of The Relevant Anatomy, Complications, and Anatomical VariationsDocument12 pagesBrachial Plexus Anesthesia: A Review of The Relevant Anatomy, Complications, and Anatomical VariationsLucille IlaganNo ratings yet
- Ultrasound-Guided Nerve Blocks in The Head and Neck For Chronic Pain Management - The Anatomy, Sonoanatomy, and ProcedureDocument16 pagesUltrasound-Guided Nerve Blocks in The Head and Neck For Chronic Pain Management - The Anatomy, Sonoanatomy, and Proceduremarcus moraisNo ratings yet
- Chronic Daily Headache: Suggestion For The Neuromuscular Oral TherapyDocument4 pagesChronic Daily Headache: Suggestion For The Neuromuscular Oral TherapyFuioaga Codrin-PaulNo ratings yet
- Dis EctomyDocument10 pagesDis EctomyNicholas ChenNo ratings yet
- A Review of Lumbar Radiculopathy, Diagnosis, and TreatmentDocument7 pagesA Review of Lumbar Radiculopathy, Diagnosis, and TreatmentMatthew PhillipsNo ratings yet
- Toorthj 11 327Document8 pagesToorthj 11 327Apri PerdanaNo ratings yet
- Case Report ESPB AnakDocument11 pagesCase Report ESPB Anakmartindeng92_mdNo ratings yet
- RsssDocument3 pagesRsssMuhammad AhmadNo ratings yet
- Journal Homepage: - : IntroductionDocument7 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Asor 03 0156Document5 pagesAsor 03 0156kike kikeNo ratings yet
- Abat F. 2019. Comparison US Guided vs. Blind Interventions Supraspinatus TendinopathyDocument10 pagesAbat F. 2019. Comparison US Guided vs. Blind Interventions Supraspinatus TendinopathyJavier MartinNo ratings yet
- Viral Diarrheal Diseases CorrectDocument39 pagesViral Diarrheal Diseases Correctmehrshad Farahpour Gp5No ratings yet
- Great Critical Care ReliefDocument9 pagesGreat Critical Care ReliefBenedict FongNo ratings yet
- Oral RevalidaDocument3 pagesOral RevalidaJaye DangoNo ratings yet
- Actinomycetes Staining MethodsDocument14 pagesActinomycetes Staining MethodsvikasNo ratings yet
- Renal Trauma: Schwartz Principle of Surgery 10Th EditionDocument31 pagesRenal Trauma: Schwartz Principle of Surgery 10Th EditionMustika RanyNo ratings yet
- Keith R Poskitt - Chronic Ulceration of The LegDocument5 pagesKeith R Poskitt - Chronic Ulceration of The LegKovoor LedchumananNo ratings yet
- A Clinical Success in The Management of Kotha (Digital Gangrene) by Leech Therapyandpanchtiktaghritaguggulu - A Single Case StudyDocument5 pagesA Clinical Success in The Management of Kotha (Digital Gangrene) by Leech Therapyandpanchtiktaghritaguggulu - A Single Case StudyIJAR JOURNALNo ratings yet
- LaporanDocument214 pagesLaporankadek sariNo ratings yet
- 53 JMSCRDocument7 pages53 JMSCRAddinul FitryNo ratings yet
- JNC 6 Vs 7Document2 pagesJNC 6 Vs 7Diwan AyuNo ratings yet
- Irda Non Payable ListDocument21 pagesIrda Non Payable ListMUKESH SINGHNo ratings yet
- Meyer Et Al 2001Document38 pagesMeyer Et Al 2001MIANo ratings yet
- 5th ReflectionDocument2 pages5th Reflectionapi-478150357No ratings yet
- AmenorrheaDocument2 pagesAmenorrheaVirag PatilNo ratings yet
- 10th Monthly Compliance Report On Parkland Memorial HospitalDocument92 pages10th Monthly Compliance Report On Parkland Memorial HospitalmilesmoffeitNo ratings yet
- Concepts of DiseaseDocument55 pagesConcepts of DiseaseKailash NagarNo ratings yet
- PAF Rev. 2.0 (FILLABLE)Document1 pagePAF Rev. 2.0 (FILLABLE)Melody Joy CantosNo ratings yet
- Preterm Labour: Muhammad Hanif Final Year MBBSDocument32 pagesPreterm Labour: Muhammad Hanif Final Year MBBSArslan HassanNo ratings yet
- Fped 2019 00227Document7 pagesFped 2019 00227Syaifudin LutfiNo ratings yet
- Rules and Guidelines For Mortality and Morbidity CodingDocument5 pagesRules and Guidelines For Mortality and Morbidity Codingzulfikar100% (2)
- A Case Study On MalariaDocument10 pagesA Case Study On MalariaAnant KumarNo ratings yet
- CataractDocument52 pagesCataracttammycristobalmd100% (4)
- Brosur - Ageloc Youth enDocument20 pagesBrosur - Ageloc Youth enLidya ZhuangNo ratings yet
- Ferraris M La HermeneuticaDocument310 pagesFerraris M La HermeneuticaantoniomarkusNo ratings yet
- XELOX Chemotherapy Guide: For Patients With Colorectal CancerDocument32 pagesXELOX Chemotherapy Guide: For Patients With Colorectal CancerBeatrice FiranNo ratings yet
- Master Drug ChartDocument22 pagesMaster Drug ChartMahadhir AkmalNo ratings yet
- Midwifery KitDocument3 pagesMidwifery KitRitzel CreusNo ratings yet
- Summer Eyetalk BrochureDocument4 pagesSummer Eyetalk BrochureRey EspinuevaNo ratings yet
- Internal Medicine Consult/New PetsDocument2 pagesInternal Medicine Consult/New PetssequoiavetNo ratings yet
- Praktikum PA UrogenitalDocument20 pagesPraktikum PA UrogenitalNisrina Nur AzisahNo ratings yet