Professional Documents
Culture Documents
ACLS Practice Test2
Uploaded by
Ronald Rey MenorOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ACLS Practice Test2
Uploaded by
Ronald Rey MenorCopyright:
Available Formats
ACLS Provider Course Practice Test
January 2007
This is a single-answer multiple-choice examination. There is only one correct answer to each question.
1. CPR has been started on an elderly female. After attaching a monitor, it shows fine VF. Which action would you take next? a. Deliver up to 3 precordial thumps while observing the patients response on the monitor. b. Perform at least 5 minutes of vigorous CPR before attempting defibrillation. c. Deliver about 2 minutes or 5 cycles of CPR, and deliver a 360-J monophasic or equivalent-current biphasic shock. d. Insert an endotracheal tube, administer 2 to 2.5 mg epinephrine in 10 mL NS through the tube and then defibrillate. 2. Which of the following facts about identification of VF is true? a. b. c. d. Turning the signal amplitude (gain) to zero can enhance the VF signal A sudden drop in blood pressure indicates VF Artifact signals displayed on the monitor can look like VF A peripheral pulse that is both weak and irregular indicated VF
3. After a cardiac arrest, the patient is assessed as having PEA at 30 bpm. CPR continues, an airway is placed and confirmed and an IV has been established. Which of the following medications is most appropriate to give next? a. b. c. d. Sodium bicarbonate 1 mEq/kg IV Synchonized cardioversion at 200 J Epinephrine 1 mg IV Calcium chloride 5 mL/kg IV
4. Which of the following causes of PEA is most likely to respond to quick treatment? a. b. c. d. Massive pulmonary embolism Hypovolemia Massive acute myocardial infarction Myocardial rupture
5. Identify the true statement about IV administration of medications during attempted resuscitation. a. b. c. d. Run normal saline missed with sodium bicarbonate (100 mEq/l) while continuing CPR Follow IV medications through peripheral veins with a fluid bolus Give epinephrine via the intracardiac route if IV access is not obtained within 3 minutes Do not follow IV medications through central veins with a fluid bolus
6. An elderly woman with a history of narrow-complex PSVT has just arrived in the ED. She is alert and oriented but very pale. Her HR is 165 bpm, and the ECG documents SVT. BP is 105/70 mm Hg. Supplemental oxygen is being provided, and IV has been started. Which of the following drug-dose combinations is the most appropriate first treatment? a. b. c. d. Adenosine 6 mg rapic IV push Atropine 1 mg IV push Synchronized cardioversion with 25 to 50 J Epinephrine 1 mg IV push
innovative solutions in healthcare education, llc 5923 cherrycrest lane charlotte, nc 28217 704-527-5119
7. A patient in the ED is reporting 30 minutes of severe, crushing substernal chest pain. His BP is 110/70, his heart rate is 58 and the monitor shows regular sinus bradycardia. He has already been given 325 mg of aspirin PO, has oxygen via nasal cannula at 4 L/min and has already received 3 sublingual nitroglycerin 5 minutes apart, but he continues to have severe pain. Which should be given next? a. b. c. d. Atropine 0.5 sto 1 mg IV Furosemide 20 to 40 mg IV Lidocaine 1 to 1.5 mg/kg Morphine sulfate 2 to 4 mg IV
8. Early management of acute cardiac ischemia frequently can be handled by using. a. b. c. d. Calcium channel blockers plus IV furosemide Bolus of amiodarone followed by an oral ACE inhibitor Chewable aspirin, sublingual nitroglycerine and IV morphine Lidocaine bolus followed by a continuous infusion of lidocaine.
9. Transcutaneous cardiac pacing is indicated for which of the following rhythms? a. b. c. d. Asystole that follows 6 or more defibrillation shocks Normal sinus rhythm with hypotension and shock Complete heart block with pulmonary edema Sinus bradycardia with no symptoms
10. Which of the following causes of out-of-hospital asystole is most likely to respond to treatment? a. b. c. d. Blunt multisystem trauma Drug overdose Prolonged submersion in warm water Prolonged cardiac arrest
11. You are working with an unstable 49 year-old woman with tachycardia. The monitor/defibrillator is in synchronization mode. The patient suddently becomes unresponsive and pulseless and then the rhythm changes to an irregular, chaotic, VF-like pattern. You charge to 200 J and then press the SHOCK button, but the defibrillator does not deliver a shock. Why? a. b. c. d. A monitor lead has lost contact, producing the pseudo-VF rhythm You cannot shock VF in sync mode The defibrillator/monitor battery failed The sync switch failed
12. For which of the following arrest patterns would you recommend Vasopressin? a. b. c. d. VF Asystole PEA All of the above
innovative solutions in healthcare education, llc 5923 cherrycrest lane charlotte, nc 28217 704-527-5119
13. The patient is in cardiac arrest. One of the team members is providing effective bag-mask ventilations. Compressions are adequate. The ECG documents asystole. Two minutes has passed since epinephrine 1 mg has been given. Which of the following actions should be done next? a. b. c. d. Administer atropine 1 mg IV Initiate transcutaneous pacing at a rate of 60 bpm Start a dopamine IV at 15 to 20 g/kg per minute Give epinephrine (1 mL of 1:10 000 solution) IV bolus
14. Each of the following patients were diagnosed with acute ischemic stroke. Which of these patients has NO stated contraindication for IV fibrinolytic therapy? a. b. c. d. A 65 year old who lives along and was found unresponsive by a neighbor A 65 year old man presenting approximately 4 hours after onset of symptoms A 65 year old woman presenting 1 hour after onset of symptoms A 65 year old man diagnosed with bleeding ulcers 1 week before the onset of symptoms
15. When a 25 year old woman presents to the ED, she says that she is having another episode of PSVT. Her medical history includes a electrophysiologic stimulation study (EPS) that confirmed that there was a reentry tachycardia, no Wolfe-Parkinson-White syndrome and no preexcitation. Heart rate is 180 bpm. The patient tells you that she hasj palpitations and mild shortness of breath. Vagal maneuvers with carotid sinus massage have no effect on HR or rhythm. Which of the following actions is your best intervention? a. b. c. d. IV adenosine IV propranolol IV diltiazem DC cardioversion
16. A patient with a heart rate of 30 to 40 bpm complains of feeling dizzy, cool and has clammy extremities and short of breath. He is in third-degree AV block. All treatment modalities are present. What would you do first? a. b. c. d. 17. Give epinephrine 1 mg IV push Start dopamine infusion 1 to 10 g/min Begin immediate transcutaneous pacing, sedate if possible Give atropine 0.5 to 1 mg IV
IDENTIFY THE FOLLOWING RHYTHMS:
Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Reentry Supraventricular Tachycardia
Monomorphic Ventricular Tachycardia Polymorphic Ventricular Tachycardia Ventricular Fibrillation Second-Degree Atrioventricular Block Third-Degree Atrioventricular Block
innovative solutions in healthcare education, llc 5923 cherrycrest lane charlotte, nc 28217 704-527-5119
18.
Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Reentry Supraventricular Tachycardia
Monomorphic Ventricular Tachycardia Polymorphic Ventricular Tachycardia Ventricular Fibrillation Second-Degree Atrioventricular Block Third-Degree Atrioventricular Block
19.
20.
Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Reentry Supraventricular Tachycardia
Monomorphic Ventricular Tachycardia Polymorphic Ventricular Tachycardia Ventricular Fibrillation Second-Degree Atrioventricular Block Third-Degree Atrioventricular Block
Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Reentry Supraventricular Tachycardia
Monomorphic Ventricular Tachycardia Polymorphic Ventricular Tachycardia Ventricular Fibrillation Second-Degree Atrioventricular Block Third-Degree Atrioventricular Block
innovative solutions in healthcare education, llc 5923 cherrycrest lane charlotte, nc 28217 704-527-5119
21.
22.
Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Reentry Supraventricular Tachycardia
Monomorphic Ventricular Tachycardia Polymorphic Ventricular Tachycardia Ventricular Fibrillation Second-Degree Atrioventricular Block Third-Degree Atrioventricular Block
Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Reentry Supraventricular Tachycardia
Monomorphic Ventricular Tachycardia Polymorphic Ventricular Tachycardia Ventricular Fibrillation Second-Degree Atrioventricular Block Third-Degree Atrioventricular Block
innovative solutions in healthcare education, llc 5923 cherrycrest lane charlotte, nc 28217 704-527-5119
23.
Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Reentry Supraventricular Tachycardia
Monomorphic Ventricular Tachycardia Polymorphic Ventricular Tachycardia Ventricular Fibrillation Second-Degree Atrioventricular Block Third-Degree Atrioventricular Block
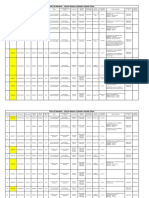
Answers: 1. C 2. C 3. C 4. B 5. B 6. A 7. D 8. C 9. C 10. B 14. C 15. A 16. C 17. Normal Sinus Rhythm 18. Sinus Bradycardia 19. Atrial Flutter 20. Third-Degree Atrioventricular Block 21. Atrial Fibrillation 22. Monomorphic Ventricular Tachycardia 23. Ventricular Fibrillation
11. B
12. D
13. A
innovative solutions in healthcare education, llc 5923 cherrycrest lane charlotte, nc 28217 704-527-5119
You might also like
- ACLS Exam Version ADocument11 pagesACLS Exam Version AAhmed - Sawalha96% (28)
- AHA ACLS Post Test Answer Key 2023Document33 pagesAHA ACLS Post Test Answer Key 2023c100% (9)
- ACLS Cheat SheetDocument8 pagesACLS Cheat SheetLenTheRN85% (27)
- 2021 ACLS Study GuideDocument20 pages2021 ACLS Study GuideShane Brown83% (12)
- AHA ACLS Precourse Self Assessment Answers 2023Document32 pagesAHA ACLS Precourse Self Assessment Answers 2023R100% (4)
- AHA ACLS Megacode ScenariosDocument6 pagesAHA ACLS Megacode ScenariosChad Sanford78% (18)
- ACLS Test PrintscreenedDocument13 pagesACLS Test Printscreenedhellfireomega67% (9)
- Acls Study GuideDocument24 pagesAcls Study GuideMohammad Gita100% (17)
- ACLS Exam ADocument8 pagesACLS Exam ASean Johnson83% (30)
- ACLS Exam ADocument8 pagesACLS Exam AAgil Rumboko Sumitro100% (3)
- Advance Cardiac Life Support: Short, Sweet and to the PointFrom EverandAdvance Cardiac Life Support: Short, Sweet and to the PointRating: 3 out of 5 stars3/5 (2)
- ACLS Test BankDocument13 pagesACLS Test BankSofiaSheikh94% (51)
- ACLS PrecourseAssessmentDocument19 pagesACLS PrecourseAssessmentBrigitte Elaine81% (21)
- ACLS Exam Version BDocument16 pagesACLS Exam Version BAhmed - Sawalha97% (62)
- ACLS PharmacologyDocument6 pagesACLS PharmacologyEunice Angela Fulgueras80% (5)
- ACLS Answer KeyDocument23 pagesACLS Answer KeyKirana Budhiarta94% (17)
- Acls - Megacode - UpdatedDocument4 pagesAcls - Megacode - UpdatedDivine Dela Pena100% (1)
- Acls QuestionsDocument28 pagesAcls QuestionsDsd100% (1)
- ACLS - Precourse Questions and AnswersDocument18 pagesACLS - Precourse Questions and Answerssuperdockk58% (12)
- Acls Test: 1. Start CPR, Beginning With Chest CompressionsDocument15 pagesAcls Test: 1. Start CPR, Beginning With Chest CompressionsBoby Jomol100% (11)
- ACLS Memory AidsDocument2 pagesACLS Memory Aidsmaur_jmp78% (9)
- ACLS Pretest Questions and Answers 2020 (Full Practice Test)Document23 pagesACLS Pretest Questions and Answers 2020 (Full Practice Test)김민길50% (4)
- ACLS Exams A and B 3-30-16Document67 pagesACLS Exams A and B 3-30-16bevjsn95% (64)
- ACLS Precourse Test AnswersDocument60 pagesACLS Precourse Test AnswersTip Piraya60% (5)
- ACLS Practice Exam 1Document10 pagesACLS Practice Exam 1Ken Evans87% (15)
- ECG Rhythms and Pharmacology GuideDocument20 pagesECG Rhythms and Pharmacology Guidequeennita69100% (4)
- AclsDocument13 pagesAclsMohamed Kelany100% (1)
- National CPR Association ACLS Study GuideDocument18 pagesNational CPR Association ACLS Study Guidekumar23No ratings yet
- John Titor TIME MACHINEDocument21 pagesJohn Titor TIME MACHINEKevin Carey100% (1)
- ACLS Provider Manual 2015 NotesDocument5 pagesACLS Provider Manual 2015 Notescrystalshe93% (14)
- Mushroom CultureDocument65 pagesMushroom Culturebhramhi86% (7)
- ACLS Post TestDocument6 pagesACLS Post TestSheila Tolentino-Belanio73% (77)
- ACLS Post Test (Copy) 낱말 카드 - QuizletDocument18 pagesACLS Post Test (Copy) 낱말 카드 - Quizlet김민길No ratings yet
- ACLS Pretest Exam AnnotatedDocument21 pagesACLS Pretest Exam AnnotatedMOLLYNo ratings yet
- American Heart Association: Precourse Written Examination May 2001Document10 pagesAmerican Heart Association: Precourse Written Examination May 2001Ericka SwordNo ratings yet
- ACLS2Document7 pagesACLS2Jennifer Kaye L. DucaoNo ratings yet
- ACLS ECGsDocument4 pagesACLS ECGsEman Elzeftawy100% (3)
- Critical Care Nursing Exam ReviewDocument16 pagesCritical Care Nursing Exam ReviewMarivy GalonNo ratings yet
- ACLS PrecourseAssessmentDocument19 pagesACLS PrecourseAssessmentRaiedKhaled100% (1)
- Acls Version B QuizDocument9 pagesAcls Version B QuizRokunuz Jahan Rudro0% (1)
- ACLS Review TestDocument5 pagesACLS Review Testtostc60% (5)
- This Is A Single-Answer Multiple-Choice Examination. There Is Only One Correct Answer To Each QuestionDocument8 pagesThis Is A Single-Answer Multiple-Choice Examination. There Is Only One Correct Answer To Each QuestionUgeshwaran Aristotle Reddy50% (2)
- Complete Guide To Sports Training PDFDocument105 pagesComplete Guide To Sports Training PDFShahana ShahNo ratings yet
- IGCSE Chemistry Section 5 Lesson 3Document43 pagesIGCSE Chemistry Section 5 Lesson 3Bhawana SinghNo ratings yet
- ACLS ECG Rhythms & Pharmacology ReviewDocument24 pagesACLS ECG Rhythms & Pharmacology Reviewkarenjlazarus86% (14)
- Hospital and Critical CareDocument16 pagesHospital and Critical CareMarivy GalonNo ratings yet
- ACLS Practice TestDocument5 pagesACLS Practice Testprettynpink0867% (3)
- 12 To 24 HoursDocument45 pages12 To 24 HoursstellaNo ratings yet
- In Is: Question 1 (1 Point)Document7 pagesIn Is: Question 1 (1 Point)schwad1No ratings yet
- ACLS Practice Test 1Document6 pagesACLS Practice Test 1tarrynwortmann5319100% (3)
- ACLS Pre Test AnswersDocument10 pagesACLS Pre Test AnswersAirene SibleNo ratings yet
- ACLS Exam - A&B VersionsDocument36 pagesACLS Exam - A&B VersionsMohamed El-sayed100% (1)
- ACLS PRE-TEST KEYDocument19 pagesACLS PRE-TEST KEYMohammed Abdou92% (13)
- Beef Broccoli: InstructionsDocument8 pagesBeef Broccoli: InstructionsRonald Rey MenorNo ratings yet
- Quality Management in Digital ImagingDocument71 pagesQuality Management in Digital ImagingKampus Atro Bali0% (1)
- TestDocument11 pagesTestzenagit123456100% (1)
- Quantification of Dell S Competitive AdvantageDocument3 pagesQuantification of Dell S Competitive AdvantageSandeep Yadav50% (2)
- Cals ReviewbjvjvjDocument14 pagesCals ReviewbjvjvjCarl Jay M Ocariza100% (1)
- CONCEPT - QuestionsDocument2 pagesCONCEPT - Questionsgreen_archerNo ratings yet
- Soalan MCQ Acls Fit Set BDocument3 pagesSoalan MCQ Acls Fit Set BAnonymous 89ilBIGhrmNo ratings yet
- ZYUPvN-UnknownDocument9 pagesZYUPvN-Unknownmohammed ahmedNo ratings yet
- He Runs Three Marathons Each YearDocument4 pagesHe Runs Three Marathons Each YearJILL ANGELESNo ratings yet
- Advance Cardiac SuppDocument32 pagesAdvance Cardiac SuppVijith.V.kumarNo ratings yet
- CCS - Handbook of Anesthesiology (2005)Document180 pagesCCS - Handbook of Anesthesiology (2005)Rojelle LezamaNo ratings yet
- DEFIBrilatorDocument43 pagesDEFIBrilatoranon_632568468No ratings yet
- Current Clinical Strategies: Handbook of AnesthesiologyDocument180 pagesCurrent Clinical Strategies: Handbook of AnesthesiologydramaganaNo ratings yet
- Effect of Cochlear Implantation On Quality of Life in Adults With Unilateral Hearing LossDocument13 pagesEffect of Cochlear Implantation On Quality of Life in Adults With Unilateral Hearing LossRonald Rey MenorNo ratings yet
- Al Farabi College of Nursing Nursing Informatics (Nur 329) Midterm Examination Attendance Sheet: APRIL 10, 2013 NO Name Academic Number SignatureDocument1 pageAl Farabi College of Nursing Nursing Informatics (Nur 329) Midterm Examination Attendance Sheet: APRIL 10, 2013 NO Name Academic Number SignatureRonald Rey MenorNo ratings yet
- Patient Benefit From Cochlear Implantation in Single-Sided Deafness: A 1-Year Follow-UpDocument5 pagesPatient Benefit From Cochlear Implantation in Single-Sided Deafness: A 1-Year Follow-UpRonald Rey MenorNo ratings yet
- Neurotology Audiology: ProceedingsDocument8 pagesNeurotology Audiology: ProceedingsRonald Rey MenorNo ratings yet
- LMR Alternative GroupingDocument1 pageLMR Alternative GroupingRonald Rey MenorNo ratings yet
- Emergency DrugsDocument2 pagesEmergency DrugsRonald Rey MenorNo ratings yet
- Canex - Product InformationDocument2 pagesCanex - Product InformationRonald Rey MenorNo ratings yet
- Arndt2017 PDFDocument11 pagesArndt2017 PDFRonald Rey MenorNo ratings yet
- 10.1007@s00106 019 0705 8Document10 pages10.1007@s00106 019 0705 8Ronald Rey MenorNo ratings yet
- FpathoDocument8 pagesFpathoRonald Rey MenorNo ratings yet
- Articulation Therapy LogDocument2 pagesArticulation Therapy LogRonald Rey MenorNo ratings yet
- NUR 226 Instructional Design Course GuideDocument3 pagesNUR 226 Instructional Design Course GuideRonald Rey MenorNo ratings yet
- Mean Length of UtteranceDocument4 pagesMean Length of UtteranceRonald Rey MenorNo ratings yet
- GroupingDocument3 pagesGroupingRonald Rey MenorNo ratings yet
- Liver PathoDocument2 pagesLiver PathoRonald Rey MenorNo ratings yet
- Liver PathoDocument2 pagesLiver PathoRonald Rey MenorNo ratings yet
- Pricelist Santos 1Document1 pagePricelist Santos 1Ronald Rey MenorNo ratings yet
- Vital SignsDocument21 pagesVital SignsRonald Rey MenorNo ratings yet
- Vital SignsDocument30 pagesVital SignsRonald Rey MenorNo ratings yet
- Al Farabi College of Nursing Nursing Informatics (Nur 329) Midterm Examination Attendance Sheet: APRIL 10, 2013 NO Name Academic Number SignatureDocument1 pageAl Farabi College of Nursing Nursing Informatics (Nur 329) Midterm Examination Attendance Sheet: APRIL 10, 2013 NO Name Academic Number SignatureRonald Rey MenorNo ratings yet
- MS Gastro Intestinal (Hepa)Document12 pagesMS Gastro Intestinal (Hepa)Ronald Rey MenorNo ratings yet
- BSC Nursing FinalDocument131 pagesBSC Nursing FinalRonald Rey MenorNo ratings yet
- Pasta Aglio e OlioDocument3 pagesPasta Aglio e OlioRonald Rey MenorNo ratings yet
- PansitDocument4 pagesPansitRonald Rey MenorNo ratings yet
- Pansit LomiDocument3 pagesPansit LomiRonald Rey MenorNo ratings yet
- Pansit LomiDocument3 pagesPansit LomiRonald Rey MenorNo ratings yet
- Pasta Aglio e OlioDocument3 pagesPasta Aglio e OlioRonald Rey MenorNo ratings yet
- JurnalDocument9 pagesJurnalClarisa Noveria Erika PutriNo ratings yet
- Striedter - 2015 - Evolution of The Hippocampus in Reptiles and BirdsDocument22 pagesStriedter - 2015 - Evolution of The Hippocampus in Reptiles and BirdsOsny SillasNo ratings yet
- NAT Order of Operations 82Document39 pagesNAT Order of Operations 82Kike PadillaNo ratings yet
- Obstetrical Hemorrhage: Reynold John D. ValenciaDocument82 pagesObstetrical Hemorrhage: Reynold John D. ValenciaReynold John ValenciaNo ratings yet
- WSP Global EnvironmentDocument20 pagesWSP Global EnvironmentOrcunNo ratings yet
- DNA Gel Electrophoresis Lab Solves MysteryDocument8 pagesDNA Gel Electrophoresis Lab Solves MysteryAmit KumarNo ratings yet
- Prof Ram Charan Awards Brochure2020 PDFDocument5 pagesProf Ram Charan Awards Brochure2020 PDFSubindu HalderNo ratings yet
- Malware Reverse Engineering Part 1 Static AnalysisDocument27 pagesMalware Reverse Engineering Part 1 Static AnalysisBik AshNo ratings yet
- Bluetooth TutorialDocument349 pagesBluetooth Tutorialjohn bougsNo ratings yet
- Orc & Goblins VII - 2000pts - New ABDocument1 pageOrc & Goblins VII - 2000pts - New ABDave KnattNo ratings yet
- Why Genentech Is 1Document7 pagesWhy Genentech Is 1panmongolsNo ratings yet
- Estimation of Working CapitalDocument12 pagesEstimation of Working CapitalsnehalgaikwadNo ratings yet
- SEG Newsletter 65 2006 AprilDocument48 pagesSEG Newsletter 65 2006 AprilMilton Agustin GonzagaNo ratings yet
- Olympics Notes by Yousuf Jalal - PDF Version 1Document13 pagesOlympics Notes by Yousuf Jalal - PDF Version 1saad jahangirNo ratings yet
- System: Boehringer Mannheim/Hitachi AnalysisDocument20 pagesSystem: Boehringer Mannheim/Hitachi Analysismaran.suguNo ratings yet
- Break Even AnalysisDocument4 pagesBreak Even Analysiscyper zoonNo ratings yet
- QueriesDocument50 pagesQueriesBajji RajinishNo ratings yet
- 8dd8 P2 Program Food MFG Final PublicDocument19 pages8dd8 P2 Program Food MFG Final PublicNemanja RadonjicNo ratings yet
- Ujian Madrasah Kelas VIDocument6 pagesUjian Madrasah Kelas VIrahniez faurizkaNo ratings yet
- Iso 9001 CRMDocument6 pagesIso 9001 CRMleovenceNo ratings yet
- Circular Flow of Process 4 Stages Powerpoint Slides TemplatesDocument9 pagesCircular Flow of Process 4 Stages Powerpoint Slides TemplatesAryan JainNo ratings yet
- Unit-1: Introduction: Question BankDocument12 pagesUnit-1: Introduction: Question BankAmit BharadwajNo ratings yet
- Three-D Failure Criteria Based on Hoek-BrownDocument5 pagesThree-D Failure Criteria Based on Hoek-BrownLuis Alonso SANo ratings yet
- CMC Ready ReckonerxlsxDocument3 pagesCMC Ready ReckonerxlsxShalaniNo ratings yet
- Audit Acq Pay Cycle & InventoryDocument39 pagesAudit Acq Pay Cycle & InventoryVianney Claire RabeNo ratings yet