Professional Documents
Culture Documents
Mnemonic Device
Uploaded by
Jonathan ObañaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mnemonic Device
Uploaded by
Jonathan ObañaCopyright:
Available Formats
Mnemonic device, is any learning technique that aids memory.
To improve long term memory, mnemonic systems are used to make memorization easier. They do so by increasing the efficiency of the process of consolidation. The HYPERKALEMIA "Machine" - Causes of Increased Serum K+ M - Medications - ACE inhibitors, NSAIDS A - Acidosis - Metabolic and respiratory C - Cellular destruction - Burns, traumatic injury H - Hypoaldosteronism, hemolysis I - Intake - Excesssive N - Nephrons, renal failure E - Excretion Impaired MURDER Signs and Symptoms of Increased Serum K+ M - Muscle weakness U - Urine, oliguria, anuria R- Respiratory distress D - Decreased cardiac contractility E - ECG changes R - Reflexes, hyperreflexia, or areflexia (flaccid) HYPONATREMIA "You Are Fried" F - Fever (low grade), flushed skin R - Restless (irritable) I - Increased fluid retention and increased BP E - Edema (peripheral and pitting) D - Decreased urinary output, dry mouth Can also use this one: SALT S = Skin flushed A = Agitation L = Low-grade fever T = Thirst "CATS" of "HYPOCALCEMIA" C - Convulsions A- Arrhythmias T - Tetany S - Spasms and stridor To remember which blood types are compatible, visualize the letter O as an orb representing the universe, because type O blood is the universal donor blood. Patients with any blood type can receive it. But O also means odd man out: Patients with type O blood can receive only type O blood. Think BEEP to remember the signs of minor bleeding: B: Bleeding gums
E: Ecchymoses (bruises) E: Epistaxis (nosebleed) P: Petechiae (tiny purplish spots) Hypo/Hyperplasia Having difficulty distinguishing hypoplasia from hyperplasia? When you see plasia in any word, think of "plastic." Plastic, in turn, means forming or developing. As for hypo and hyper, thats the easy part. Hypo means under, or below normal. Hyper means excessive, or above normal. Thus, hypoplasia means underdevelopment, and hyperplasia means overdevelopment. A stand-up comedian who gets no laughs might say his audience has humoral immunity. But humor is the Latin word for liquid, and humoral immunity comes from elements in the blood specifically, antibodies. Contrast this with cellular immunity, which comes about through the actions of T cells. "FARM" for serum sickness: each letter stands for a key sign or symptom of serum sickness. F: Fever A: Arthralgias R: Rash M: Malaise To remember the four causes of cell injury, think of how the injury tipped (or TIPD) the scale of homeostasis: T: Toxin or other lethal (cytotoxic) substance I: Infection P: Physical insult or injury D: Deficit, or lack of water, oxygen, or nutrients. When asking assessment questions, remember the American Cancer Societys mnemonic device CAUTION: C: Change in bowel or bladder habits A: A sore that doesnt heal U: Unusual bleeding or discharge T: Thickening or lump I: Indigestion or difficulty swallowing O: Obvious changes in a wart or mole N: Nagging cough or hoarseness. Use the ABCD rule to assess a moles malignant potential : A: Asymmetry--Is the mole irregular in shape? B: Border--Is the border irregular, notched, or poorly defined? C: Color--Does the color vary (for example, between shades of brown, red, white, blue, or black)? D: Diameter--Is the diameter more than 6 mm? Listening Heart Sound APE TO MAN Atrial, Pulmonic, Erb's point, Tricuspid, Mitral Side effects of steroids. The 5 S's. Sick- easier to get sick Sad-causes depression Sex-increases libido
Salt-retains more and causes weight gain Sugar-raises blood sugar 5F's... Cholecystectomy female fair fat forty fertile R Respiratory O Opposite ph > PCO2 < Alkalosis ph < PCO2 > Acidosis M Metabolic E Equal ph> HCO3 > Alkalosis ph< HC03 < Acidosis Immediate tx of MI, think MONA: M Morphine sulfate O Oxygen N Nitroglycerin A ASA Treatment of CHF, think UNLOAD FAST: U sit Upright N Nitro L Lasix O Oxygen A Aminophylline D Digoxin F Fluids- decrease A Afterload - decrease S Sodium - decrease T Tests: dig level, ABG, K+ Assistive devices -- Canes: C Cane O Opposite A Affected L Leg Signs of a Cholinergic Crisis, think SLUD: S Salivation L Lacrimation
U Urination D Defication Memory Trick:Need to remember which kind of beta blocker has which action? B1 Blocks the heart (you have only one heart) B2 Blocks the lungs (you have two lungs) CRAINIAL NERVES. im pretty sure most of you heard of these. Nerves Functions I Olfactory -Oh -Sensory -Some II Optic- Oh -Sensory -Say III Occulomotor -Oh -Motor -Mary IV Trochlear -To -Motor -Money V Trigeminal -Touch -Both -But VI Abducens -And -Motor -My VII Facial -Feel -Both -Brother VIII Acoustic (vestoblochlear) -A -Sensory -Says IX Glosopharyngeal -Green -Both -Bad X Vagus -Veggie -Both -Business XI Spinal Accessory- Soon At -Motor -Mary XII Hypoglosal -Harvest- Motor -Money Oh oh oh to touch and feel a green veggie soon at harvest
Mnemonic device, is any learning technique that aids memory. To improve long term memory, mnemonic systems are used to make memorization easier. They do so by increasing the efficiency of the process of consolidation.
EYES Another way to remember the eyes is: You look OUt with Both eyes. Take the Right dose so you won't OD [overdose]. The only one that is Left is OS. Both eyes=OU, Right eye=OD, Left eye=OS. It is about fetal accelerations and decelerations!!! Just remember VEAL CHOP Variable Cord compression Early Head compression Accelerations OK Late Placental insufficiency
Heart sounds: S3= Heart fail-ure (3 syllables) S4=Hy-per-ten-sion (4 syllables) And the effects of anticholinergics: Can't see Can't pee Can't spit Can't --defecate Nine-point Postpartum Assessment... BUBBLEHER B- Breasts U- Uterus B- Bladder B- Bowel function L- Lochia E- Episiotomy H- Homan's sign E- Emotional Status R- Respiratory System LDL ("bad" cholesterol) L=Lowdown D=Dirty L=lipoprotein This one really helped me in the cardiac system when you need to know when you hear a murmur like on Mitral regurgitation you hear it on systole. (H)ARD ASS MRS. MSD ARD = Atrial regurgitation diastole ASS = Atrial stenosis systole MRS = Mitral regurgitation systole MSD = Mitral stenosis diastole The 5 P's of circulation loss in a limb. Pain, Pallor, Pulselessness, Parasthesia, Poikilothermia Heres one I learned about EKG Snow over Grass- white over green smoke over fire- black over red and ground in the middle- brown I finally know what METHODS mean on DISCHARGE PLANNING. M-edicine E-xercise T-reatment H-ealth Teaching O-ut patient follow-up or check-up
D-iet S-ex(sexual activity) Side effects & adverse reactions to immunizations: F- Fever I- Itching S- Stiffness H- Headache E- Edema R- Redness F- Fussy L- Localized Tenderness A- Appetite decrease G- General Aches Pains WHUTN- "Whutnthehell?" W- Wheezing H- Hypotension U- Uticaria T- Tachycardia N- Nasal Decongestion Assess for treatable causes of changes in cognition and behavior. The mnemonic DEMENTIA can be used to remember potential causes: D: Drugs and alcoholincluding over-the-counter drugs E: Eyes and earsdisorientation due to visual/auditory distortion M: Medical disorderse.g., diabetes, hypothyroidism E: Emotional and psychological disturbancese.g., mood or paranoid disorders N: Neurological disorderse.g., multiinfarct dementia T: Tumors and trauma I: Infectionse.g., urinary tract or upper respiratory tract A: Arteriosclerosisleading to heart failure, insufficient blood supply to heart and brain, and confusion ***GRANULOCYTES are Never Eat Bananas. Normal (Neutrophils) Monkeys (Monocytes) Like to (Lymphocytes) Eat (Eosinophils) Bananas (Basophils)
Parkinson's Medications: "Ali Loves Boxing Matches" A-Amantadine L- Levodopa B- Bromocriptine M-MAO inhibitors
The 4 H's that invalidate a neuro exam: Hypotension Hpoxia Hypoglycemia Hypothermia* 3 ICP waveforms: A is awful, B is bad and C is common Glasgow Coma Scale: #'s go low to high, with head to toe: eye, mouth, motor 1. Eye opening (1-4) 2. Verbal response (1-5) 3. Best Motor response (1-6) Glasgow Coma Scale: If they're <8, they intubate! To remember DECEREBRATE posturing, it is abnormal extension. Their hands look like the flippers of a seal - Think DESEALEBRATE! Pinpoint pupils: Drugs, drops & nearly dead Drugs: opiates Drops: meds for glaucoma Nearly dead: damage in the pons area of the brainstem Dilated pupils: Fear, Fits & Fast Living Fear: panic, extreme anxiety Fits: seizures Fast Living: cocaine, crack, phencyclidine (PCP) The pathophysiology of ARDS: Assault on the respiratory system Respiratory distress Decreased lung compliance Severe respiratory failure Diagnostic criteria of ARDS Acute onset Ratio (PaCO2/FiO2) <200 Diffuse infiltration Swan-Ganz wedge pressure (PAWP) <18mm Hg Acute respiratory failure (ARF) Type II (hypoventilation) criteria: 50/50 Rule PaCO2 >50 PaO2 <50 (on >50% oxygen) Alpha 1 Receptor stimulation: arteries & arterioles Causes vasoconstriction when stimulated which increases afterload dobutamine (Dobutrex) stimulates beta 1 receptors (increase contractility & CO/CI) Treatment of all acute coronary syndromes (unstable angina, NSTEMI or STEMI): OADH
Open coronary arteries Here, think MONA greets all MI's: Morphine Oxygen Nitroglycerin Aspirin (CHEWED) Anticoagulate & antiplatelet Destress the heart (with beta blockers; limited activity for 12h) Hemodynamic stability Complications of thrombolytic therapy: The 3 B's Bleeding Brady's (dysrhythmias) Bloodclots (d/t excessive thrombin) Complications of cardiopulmonary bypass (CPB): The 3 H's Hypothermia (to decrease O2 consumption)...Effects SVR (vasoconstriction) and causes myocardial depression (decreases contractility) Hemodilution (to improve macrocirculation)...fluid shifting (third-spacing), e-lyte imbalances (K+, Mg+ & Ca++ often need replacing!) Heparinzation (to prevent clots in circuit)...monitor aPTT. Signs and symptoms of cardiac tamponade (Beck's Triad): The Three D's Distant heart sounds Distended jugular veins Decreased pulse pressure (think of a narrow pulse pressure as opposed to a wide one) Atrial Arrhythmias: ABCDE Adenosine/amiodorone or anticoagulate (if Afib/Flutter has been present >48h) Beta blockers Calcium channel blockers Digoxin Electrocardiovert (if <48h) For ventricular arrhythmias: AL Amiodorone Lidocaine 8 A's for Hepatotoxic Drugs (Check SGPT/SGOT) Antituberculosi Anticonvulsant S - sodium Luminal G - gabapentin P - phenytoin T - tegretol Anticancer
Aspirin Alcohol Antifamily (contraceptice pills) Acetaminophen Aflatoxins Breast self examination (i made a song out of this) 1 little 2, little 3 little fingers Do BSE 7 days after menses Press nipple once check for discharge Call your doctor I'm sure you will do it more... STANDARD ROOM PRECAUTION A -irborne (PTB, SARS, Antrax) B -lood and body fluids - AIDS, Hepa B C -ontact - open wounds, lesions D - roplet - Diphtheria, Pneumonia, Pertussis E - nteric - GIT infections RIGHT SIDED HEART FAILURE A norexia and ascites B loating and indigestion C ardiomegaly D istended neck vein E dema-peripheral F acial puffiness G allop H epatomegaly I tchiness J aundice HYPERTHYROIDISM (GRAVE'S) G oiter R avenous appetite A gitation and nervousness V S increased E xophthalmos S kin is moist & heat intolerance:)
Essential Newborn Care " Unang Yakap" The Department of Health embarked on Essential Newborn Care , a new program to address neonatal deaths in the country. Under the umbrella of the Unang Yakap Campaign, Essential Newborn Care is an evidenced based strategic intervention aimed at improving newborn care and helping cub neonatal
mortality. The Essential Newborn Care package is a four-step newborn care time-bound intervention undertaken to lessen newborn death. 1. Immediate and thorough drying to stimulate breathing after delivery of the baby 2. Provision of appropriate thermal care through mother and newborn skin-to skin contact maintaining a delivery room temperature of 25-28 degrees centigrade and wrapping the newborn with clean, dry cloth. 3. Properly timed clamping and cutting of the umbilical cord, (1-3 minutes or until cord pulsation stops) 4. Non-separation of the newborn and mother for early breast-feeding. Immediate latching on and initiation of breastfeeding within first hour after birth. 5. Post-natal care required within 24 hours after birth also includes Cord care Breastfeeding Vitamin K injection Eye prophylaxis Delayed bathing until 6 hours of life BCG and first dose of Hepatitis B Immunization Newborn screening The Essential Newborn Care Package aims to reduce newborn mortality rate from 13 deaths (2006 FPS, NSO) to 10 per 1000 live births by 2015. Unang Yakap aims to save newborn lives.
How to Use Crutches, Canes, and Walkers General Guidelines
If you ever break a bone in your leg or foot, have a surgical procedure on your lower limb, or suffer a stroke, you may need to use crutches, a cane, or a walker. In the beginning, everything you do may seem difficult. But, with a few tips and some practice, you will gain confidence and learn to use your walking aid safely. General Guidelines 1. Remove scatter rugs, electrical cords, spills, and anything else that may cause you to fall. 2. In the bathroom, use nonslip bath mats, grab bars, a raised toilet seat, and a shower tub seat. 3. Simplify your household to keep the items you need handy and everything else out of the way. 4. Use a backpack, fanny pack, apron, or briefcase to help you carry things around. Crutches
If an injury or surgical procedure requires you to keep your weight off your leg or foot, you may have to use crutches. Proper Positioning The top of your crutches should reach between 1 and 1.5 inches below your armpits while you stand up straight. The handgrips of the crutches should be even with the top of your hip line. Your elbows should bend a bit when you use the handgrips. Hold the top of the crutches tightly to your sides, and use your hands to absorb the weight. Don't let the tops of the crutches press into your armpits. Walking Lean forward slightly and put your crutches about one foot ahead of you. Begin your step as if you were going to use the injured foot or leg, but shift your weight to the crutches instead of the injured foot. Your body swings forward between the crutches. Finish the step normally with your non-injured leg. When the non-injured leg is on the ground, move your crutches ahead in preparation for the next step. Keep focused on where you are walking, not on your feet.
Sitting Back up to a sturdy chair. Put your injured foot in front of you and both crutches in one hand. Use the other hand to feel for the seat of your chair. Slowly lower yourself into it. Lean your crutches upside down in a handy location. (Crutches tend to fall over when they are stood on their tips.) To stand up, inch yourself to the front of the chair. Hold both crutches in the hand on your good leg side. Push yourself up and stand on the good leg. Stairs
To walk up and down stairs with crutches, you need to be both strong and flexible. Facing the stairway, hold the handrail with one hand and tuck both crutches under your armpit on the other side. When you're going up, lead with your good foot, keeping the injured foot raised behind you. When you're going down, hold your injured foot up in front, and hop down each stair on your good foot. Take it one step at a time. You may want someone to help you, at least at first. If you're facing a stairway with no handrails, use the crutches under both arms and hop up or down each step on your good leg, using more strength. An easier way is to sit on the stairs and inch yourself up and down each step. Start by sitting on the lowest stair with your injured leg out in front. Hold both crutches flat against the stairs in your opposite hand.
Scoot your bottom up to the next step, using your free hand and good leg for support. Face the same direction when you go down the stairs this way.
http://www.slideshare.net/SandraLaranjo/comprehensive-nursing-board-exam-reviewer
You might also like
- AnalgesicDocument62 pagesAnalgesicAnjum IslamNo ratings yet
- Mnemonic SDocument4 pagesMnemonic S1a2b3c4aNo ratings yet
- Mnemonic SDocument41 pagesMnemonic SJane CobicoNo ratings yet
- Megaloblastic AnemiaDocument34 pagesMegaloblastic AnemiaAmir MuhrizNo ratings yet
- Physician Licensure Exam Feb 2010 Top Performing SchoolsDocument2 pagesPhysician Licensure Exam Feb 2010 Top Performing SchoolsSandy Chiong MaganitoNo ratings yet
- PSM Prep LadderDocument43 pagesPSM Prep LadderMayanka SaxenaNo ratings yet
- Jarvis 12 Skin Hair NailsDocument11 pagesJarvis 12 Skin Hair NailsSarah C. SnooksNo ratings yet
- Hematology Oncology Notes Syrian StudentDocument2 pagesHematology Oncology Notes Syrian StudentLoyla RoseNo ratings yet
- Recall QuestionsDocument2 pagesRecall QuestionsAymen BekirNo ratings yet
- High-Impact Outline: Source: Classroom To Clinic Study System by Sedrak and MasseyDocument14 pagesHigh-Impact Outline: Source: Classroom To Clinic Study System by Sedrak and MasseyHannah JosephNo ratings yet
- Benign Paroxysmal Positional VertigoDocument8 pagesBenign Paroxysmal Positional VertigoSubynk RidwanNo ratings yet
- Bhupendra Panchal Lecturer in MSNDocument26 pagesBhupendra Panchal Lecturer in MSNRachel JohnNo ratings yet
- CNS Seizures in ChildhoodDocument42 pagesCNS Seizures in ChildhoodDr.P.NatarajanNo ratings yet
- 1семестр Екзамен на місу іноз нове PDFDocument9 pages1семестр Екзамен на місу іноз нове PDFHart ElettNo ratings yet
- Comprehensive ExaminationDocument36 pagesComprehensive ExaminationZuhair Al Alim AhmedNo ratings yet
- Nclex ReviewDocument5 pagesNclex ReviewOncologynNo ratings yet
- Impactednurse Nurses Reference PackDocument2 pagesImpactednurse Nurses Reference PackRaenell CurryNo ratings yet
- ARISE MEDICAL ACADEMY STUDENTS RECALL RECENT FMGE EXAM QUESTIONSDocument75 pagesARISE MEDICAL ACADEMY STUDENTS RECALL RECENT FMGE EXAM QUESTIONSshimailNo ratings yet
- CTT InsertionDocument18 pagesCTT InsertionRen-Ren NazarenoNo ratings yet
- Principles of BiopsyDocument4 pagesPrinciples of BiopsyTohin TurjoNo ratings yet
- Step 12sem 4Document438 pagesStep 12sem 4opeyemi daramolaNo ratings yet
- Coagulation Disorders-First Aid Book: SS DX TXDocument6 pagesCoagulation Disorders-First Aid Book: SS DX TXMAINo ratings yet
- Skin Pathology Lab Diagnoses and HistologyDocument54 pagesSkin Pathology Lab Diagnoses and HistologyMJO79No ratings yet
- NCLEX MnemonicDocument2 pagesNCLEX MnemonicJem BondocNo ratings yet
- PharmacologyDocument120 pagesPharmacologyFluffy_iceNo ratings yet
- Dermatology - LoveDocument433 pagesDermatology - LoveAntonio EscobarNo ratings yet
- Heart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesDocument3 pagesHeart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesPrarthana Thiagarajan100% (3)
- Applications of Leukocyte - and Platelet-Rich Plasma (L-PRP) in TraumaDocument12 pagesApplications of Leukocyte - and Platelet-Rich Plasma (L-PRP) in TraumaEdgar PantojaNo ratings yet
- SplitPDFFile 801 To 1000Document200 pagesSplitPDFFile 801 To 1000Shafan ShajahanNo ratings yet
- Question 1 of 13 on pityriasis rosea diagnosisDocument23 pagesQuestion 1 of 13 on pityriasis rosea diagnosisjonyNo ratings yet
- Fmge De'C. 2017Document21 pagesFmge De'C. 2017Subhodeep MondalNo ratings yet
- By DR - Mohammad Z. Abu Sheikha@: +pigmented Stones (Black Stone - Non Infected) (Brown Stone - Infected)Document11 pagesBy DR - Mohammad Z. Abu Sheikha@: +pigmented Stones (Black Stone - Non Infected) (Brown Stone - Infected)Nisreen Al-shareNo ratings yet
- Clinical Pearls DermatologíamatologyDocument4 pagesClinical Pearls DermatologíamatologyMaritza24No ratings yet
- Haematologic EmergenciesDocument33 pagesHaematologic Emergenciessalmamaged7619No ratings yet
- Marrow Medicine Notes 1 3 6nbsped CompressDocument2 pagesMarrow Medicine Notes 1 3 6nbsped CompressRaam NaikNo ratings yet
- CH 01Document3 pagesCH 01JamieNo ratings yet
- Bipolar Disorder Background: Hypomania Has The Same Symptoms of Mania Without Psychotic SymptomsDocument2 pagesBipolar Disorder Background: Hypomania Has The Same Symptoms of Mania Without Psychotic SymptomshumdingerNo ratings yet
- KNH 413 - Case Study - Type 1 DMDocument14 pagesKNH 413 - Case Study - Type 1 DMapi-301118772No ratings yet
- FMGE June 2019 questions and answersDocument20 pagesFMGE June 2019 questions and answersSugithaTamilarasanNo ratings yet
- AIIMS StrategyDocument12 pagesAIIMS StrategyMahi Reddy100% (1)
- SARP (Skin Anesthesia Radiology Psychiatry) Review 2010Document4 pagesSARP (Skin Anesthesia Radiology Psychiatry) Review 2010QworldNo ratings yet
- Not Mine Survival GuideDocument21 pagesNot Mine Survival GuideJestin AquinoNo ratings yet
- 1 4927329208029413644 PDFDocument578 pages1 4927329208029413644 PDFWaseem UllahNo ratings yet
- Last Hour Review 2020 by Mci Gurukul DR Bhuoendra Armaan Chourasiya PDFDocument49 pagesLast Hour Review 2020 by Mci Gurukul DR Bhuoendra Armaan Chourasiya PDFadiNo ratings yet
- Review of Dermatology Ebook Ebook Alikhan, Ali, Hocker, Thomas L. H Kindle StoreDocument1 pageReview of Dermatology Ebook Ebook Alikhan, Ali, Hocker, Thomas L. H Kindle StoreSally dossNo ratings yet
- GlabellaDocument18 pagesGlabellaghinaNo ratings yet
- EmergencyDocument86 pagesEmergencyyazzNo ratings yet
- Dermatology Review NotesDocument8 pagesDermatology Review Notesnmb1986No ratings yet
- Pulmonary First Aid GuideDocument6 pagesPulmonary First Aid GuideMAINo ratings yet
- PDFDocument570 pagesPDFEshaal FatimaNo ratings yet
- Acute Purulent Diseases of Fingers and HandDocument9 pagesAcute Purulent Diseases of Fingers and Handvem_nikhil4uNo ratings yet
- Anat Recall Que - Dr. AzamDocument24 pagesAnat Recall Que - Dr. AzamSurya VummadisettyNo ratings yet
- Skin Module McqsDocument5 pagesSkin Module McqsSyed Usama Rashid100% (1)
- Treatment of Hemostasis DisordersDocument17 pagesTreatment of Hemostasis DisordersDiana HyltonNo ratings yet
- Aiims PG May 2019Document108 pagesAiims PG May 2019MarcelNo ratings yet
- Mnemonics in DermatologyDocument2 pagesMnemonics in DermatologyShree ShresthaNo ratings yet
- Pharmacology QuestionsDocument20 pagesPharmacology Questionsdelluismanuel100% (2)
- Applied Anatomy - Trigeminal NerveDocument8 pagesApplied Anatomy - Trigeminal NervefrabziNo ratings yet
- MCQsDocument95 pagesMCQsMarcus GrisomNo ratings yet
- Nursing MnemonicsDocument11 pagesNursing MnemonicsMarco CalvaraNo ratings yet
- PRC Form Cmo 14 IrishDocument6 pagesPRC Form Cmo 14 IrishJonathan ObañaNo ratings yet
- Hirschprung DiseaseDocument9 pagesHirschprung DiseaseJonathan ObañaNo ratings yet
- Assessing pedal pulses in patients with hip fracturesDocument5 pagesAssessing pedal pulses in patients with hip fracturesJonathan ObañaNo ratings yet
- Plan of ActivityDocument2 pagesPlan of ActivityJonathan ObañaNo ratings yet
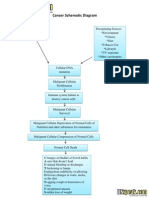
- Cancer Schematic DiagramDocument1 pageCancer Schematic DiagramJonathan ObañaNo ratings yet
- Alkylating AgentsDocument3 pagesAlkylating AgentsJonathan ObañaNo ratings yet
- Statistics and its role in data analysis, interpretation and decision makingDocument1 pageStatistics and its role in data analysis, interpretation and decision makingJonathan ObañaNo ratings yet
- Herniated Nucleus PulposusDocument4 pagesHerniated Nucleus PulposusJonathan ObañaNo ratings yet
- In IvfusionDocument5 pagesIn IvfusionJonathan ObañaNo ratings yet
- Method of Preparation and Systematic Examination of A Direct Fecal SmearDocument3 pagesMethod of Preparation and Systematic Examination of A Direct Fecal SmearCelne CentinoNo ratings yet
- Comparative Study On Hospitality Management Instructors' Teaching Competence and Students' Performance in The Hospitality IndusrtyDocument7 pagesComparative Study On Hospitality Management Instructors' Teaching Competence and Students' Performance in The Hospitality IndusrtyIOER International Multidisciplinary Research Journal ( IIMRJ)No ratings yet
- LKPD ApplicationLetterDocument5 pagesLKPD ApplicationLetterDheaNo ratings yet
- Party Event Planner Services ProposalDocument7 pagesParty Event Planner Services ProposalAnton KenshuseiNo ratings yet
- Prospects and Challenges of Tourism in NepalDocument12 pagesProspects and Challenges of Tourism in NepalShrestha MilanNo ratings yet
- Sp1u C0Document4 pagesSp1u C0Драган РодићNo ratings yet
- Digital Art Syllabus 2015Document3 pagesDigital Art Syllabus 2015api-245305578No ratings yet
- Sample Paper - 2012 Class - XII Subject - Computer Science: InstructionsDocument9 pagesSample Paper - 2012 Class - XII Subject - Computer Science: InstructionsAtif ImamNo ratings yet
- Separation Techniques Virtual LabDocument3 pagesSeparation Techniques Virtual LabRj ReyesNo ratings yet
- Department of Labor: Form WH-516 EnglishDocument1 pageDepartment of Labor: Form WH-516 EnglishUSA_DepartmentOfLabor100% (1)
- KPSC Assistant Professor in CS Question PaperDocument22 pagesKPSC Assistant Professor in CS Question PaperBabaNo ratings yet
- REIT Industry OutlookDocument49 pagesREIT Industry OutlookNicholas FrenchNo ratings yet
- Linear Panel FeaturesDocument12 pagesLinear Panel FeaturesJj ForoNo ratings yet
- OTTO - SMART ROBOT ARCHITECTUREDocument1 pageOTTO - SMART ROBOT ARCHITECTURESuscripcion BelaundeNo ratings yet
- Internship Guidelines MEDocument8 pagesInternship Guidelines MESrinivas SreekantanNo ratings yet
- Batangas CATV Vs CADocument10 pagesBatangas CATV Vs CAMary Joyce Lacambra AquinoNo ratings yet
- Miracle Morning For Writers PDFDocument203 pagesMiracle Morning For Writers PDFIgnacio Bermúdez RothschildNo ratings yet
- Leybold SV40-65BI-FC 1Document29 pagesLeybold SV40-65BI-FC 1Luis LagunaNo ratings yet
- Adhi Wardana 405120042: Blok PenginderaanDocument51 pagesAdhi Wardana 405120042: Blok PenginderaanErwin DiprajaNo ratings yet
- Global FSBDocument68 pagesGlobal FSBJoannaNo ratings yet
- Control Choke Valve 9000Document8 pagesControl Choke Valve 9000sabi_shi100% (2)
- English Learning Kit: Senior High SchoolDocument19 pagesEnglish Learning Kit: Senior High SchoolKare CaspeNo ratings yet
- Vitamins, Minerals Plus Iron, Iodine, Taurine, and Zinc: Nutrition InformationDocument1 pageVitamins, Minerals Plus Iron, Iodine, Taurine, and Zinc: Nutrition InformationWonder PsychNo ratings yet
- MAX3-ONE THERMO-SVC Manual RT43ENSW5 XPEDocument65 pagesMAX3-ONE THERMO-SVC Manual RT43ENSW5 XPECesar Calderon Gr100% (2)
- Dist Relay Test ProcedureDocument7 pagesDist Relay Test ProcedureTamilventhan S100% (1)
- Oliveboard Seaports Airports of India Banking Government Exam Ebook 2017Document8 pagesOliveboard Seaports Airports of India Banking Government Exam Ebook 2017samarjeetNo ratings yet
- Case Study On Barriers To CommunicationDocument3 pagesCase Study On Barriers To CommunicationDivya Gill100% (1)
- 09GMK 6250 - Hydraulikanlage - EnglDocument8 pages09GMK 6250 - Hydraulikanlage - EnglВиталий РогожинскийNo ratings yet
- User Manual Xiaomi Redmi Note 11S (English - 59 Pages)Document3 pagesUser Manual Xiaomi Redmi Note 11S (English - 59 Pages)Abdallah AbdallahNo ratings yet
- WJ9 JDTMFController V5Document41 pagesWJ9 JDTMFController V5commit_to_truthNo ratings yet