Professional Documents
Culture Documents
How To Read CT Scan
Uploaded by
parama_gandiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
How To Read CT Scan
Uploaded by
parama_gandiCopyright:
Available Formats
Chapter 69
How to Read a Head CT Scan
Andrew D. Perron
KEY POINTS
Cranial computed tomography (CT) is an extremely useful diagnostic tool used routinely in the care of ED patients. The EP needs to be able to accurately interpret and act upon certain CT ndings without specialist (e.g., radiologist) assistance, because many disease processes are timedependent and require immediate action. It has been shown that even a brief educational intervention can signicantly improve the EPs ability to interpret cranial CT scans. Using the mnemonic blood can be very bad (where blood = blood, can = cisterns, be = brain, very = ventricles, and bad = bone) the EP can quickly but thoroughly review a cranial CT scan for signicant pathology that demands immediate action.
Cranial CT has assumed a critical role in the practice of emergency medicine for the evaluation of intracranial emergencies, both traumatic and atraumatic. A number of published studies have revealed a deciency in the ability of EPs to interpret head CTs.1-6 Signicantly, a number of these same studies do show that with even a brief educational effort, EPs can gain considerable prociency in cranial CT scan interpretation.2,3 This is important because there are many situations where the EP must interpret and act upon head CT results in real time without assistance from other specialists such as neurologists, radiologists, or neuroradiologists.7,8 The advantages of CT scanning for CNS pathology in the ED are well known, and include widespread availability at most institutions, speed of imaging, patient accessibility, and sensitivity for a detection of many pathologic processes (particularly acute hemorrhage).
Basic Principles of CT
The fundamental principle behind radiography is the following statement: X-rays are absorbed to different degrees by different tissues. Dense tissues such as bone absorb the most x-rays, and hence allow the fewest passing through the body part being studied to reach the lm or detector opposite. Conversely, tissues with low density (e.g., air and fat) absorb almost none of the x-rays, allowing most to pass through to the lm or detector opposite. Conventional radiographs are two-dimensional images of threedimensional structures; they rely on a summation of tissue densities penetrated by x-rays as they pass through the body. It should be noted that in plain radiographs, denser objects, because they tend to absorb more x-rays, can obscure or attenuate less dense objects.
753
Ch069-X2872.indd 753
3/3/2008 1:44:04 PM
754
SECTION VIII
Injuries to Bones and Organs
As opposed to conventional radiographs, with CT scanning an x-ray source and detector, situated 180 degrees across from each other, move 360 degrees around the patient, continuously detecting and sending information about the attenuation of x-rays as they pass through the body. Very thin x-ray beams are utilized, which minimizes the degree of scatter or blurring that limits conventional radiographs. In CT, a computer manipulates and integrates the acquired data and assigns numerical values based on the subtle differences in x-ray attenuation. Based on these values, a gray-scale axial image is generated that can distinguish between objects with even small differences in density.
ATTENUATION COEFFICIENT
The tissue contained within each image unit (called a pixel) absorbs a certain proportion of the x-rays that pass through it (e.g., bone absorbs a lot, air almost none). This ability to block x-rays as they pass through a substance is known as attenuation. For a given body tissue, the amount of attenuation is relatively constant and is known as that tissues attenuation coefcient. In CT, these attenuation coefcients are mapped to an arbitrary scale between 1000 hounseld units [HU] (air) and +1000 HU (bone) (Box 69-1). This scale is the Hounseld scale (in honor of Sir Jeffrey Hounseld, who received a Nobel prize for his pioneering work with this technology).
to accurately interpret the images. Besides motion and metal artifact (self-explanatory), the two most common effects are called beam hardening and volume averaging. It is important to understand these effects and to be able to identify them, because they can mimic pathology as well as obscure actual signicant ndings. Beam hardening is a phenomenon that causes an abnormal signal when a relatively small amount of hypodense brain tissue is immediately adjacent to dense bone. The posterior fossa, where there is extremely dense bone surrounding the brain, is particularly subject to this phenomenon. It appears as either linear hyper- or hypodensities that can partially obscure the brainstem and cerebellum. Although beam hardening can be reduced with appropriate ltering, it cannot be eliminated. Volume averaging (also called partial volume artifact) arises when the imaged area contains different types of tissues (e.g., bone and brain). For that particular image unit, the CT pixel produced will represent an average density for all the contained structures. In the above instance of brain and bone, an intermediate density will be represented that may have the appearance of blood. As with beam hardening, certain techniques can minimize this type of artifact (e.g., thinner slice thickness, computer algorithms), but it cannot be eliminated, particularly in the posterior fossa.
WINDOWING
BOX 69-1
Windowing allows the CT scan reader to focus on certain tissues within a CT scan that fall within set parameters. Tissues of interest can be assigned the full range of blacks and whites, rather than a narrow portion of the gray scale. With this technique, subtle differences in tissue densities can be maximized. The image displayed will depend on both the centering of the viewing window and the width of the window. Most CT imaging includes windows that are optimized for brain, blood, and bone (Fig. 69-1).
Appearance and Density of Tissues on Cranial CT
Appearance Black White 1000 HU +1000 HU Air, fat, CSF, white matter, gray matter, acute hemorrhage, bone Important Densities Air = 1000 HU Water = 0 HU Bone = +1000 HU
CSF, cerebrospinal uid; HU, Hounseld units.
ARTIFACT
CT of the brain is subject to a few predictable artifactual effects that can potentially inhibit the ability
FIGURE 69-1 CT scan windowing: A, brain. B, blood. C, bone.
Ch069-X2872.indd 754
3/3/2008 1:44:04 PM
CHAPTER 69
How to Read a Head CT Scan
755
Normal Neuroanatomy As Seen on Head CT Scans
As with radiologic interpretation of any body part, a working knowledge of normal anatomic structures and location is fundamental to the clinicians ability to detect pathologic variants. Cranial CT interpretation is no exception. Paramount in head CT interpretation is familiarity with the various structures, ranging from parenchymal areas such as basal ganglia to vasculature, cisterns, and ventricles. Finally, knowing neurologic functional regions of the brain helps when correlating CT results with physical examination ndings. Although a detailed knowledge of cranial neuroanatomy and its CT appearance is clearly in the realm of the neuroradiologist, familiarity with a relatively few structures, regions, and expected ndings allows sufcient interpretation of most head CT scans by the EP. Figures 69-2 through 69-5 demonstrate key structures of a normal head CT scan.
IDENTIFYING CNS PATHOLOGY ON CRANIAL CT SCANS
As long as one is systematic in the search for pathology, any number of techniques can be utilized in the review of head CT images. Some recommend a center-out technique, in which the examiner starts from the middle of the brain and works outward. Others advocate a problem-oriented approach, in which the clinical history directs the examiner to a particular portion of the scan. In the authors experience, both of these are of limited utility to the clinician who does not frequently review scans. A preferred method, one that has been demonstrated to work in the ED,2 is to use the mnemonic blood can be very bad (Box 69-2). In this mnemonic, the rst letter of each word prompts the clinician to search a certain portion of the cranial CT scan for pathology. The clinician is urged to use the entire mnemonic when examining a cranial CT scan because the presence of one pathologic state does not rule out the presence
AS Ethmoid sinus Sphenoid sinus Temporal lobe
FIGURE 69-2 Head CT Normal anatomy: A, posterior fossa; B, low cerebellum. L R L Medulla Cerebellum
Cerebellar tonsil
Medulla
Foramen magnum
Mastoid air cells
Frontal lobe Suprasellar cistern Dorsum sellae Temporal lobe FIGURE 69-3 Head CT Normal anatomy: A, high pons; B, cerebral peduncles. R Pons
Suprastellar cistern Sylvian cistern
L IVth ventricle
R Pons IVth ventricle Cerebellum
Cerebellum
Circummesencephalic (ambient) cistern
Circummesencephalic (ambient) cistern
Ch069-X2872.indd 755
3/3/2008 1:44:04 PM
756
SECTION VIII
Injuries to Bones and Organs Frontal horn (lateral ventricle) IIIrd ventricle Frontal horn Caudate nucleus Anterior limb (internal capsule)
FIGURE 69-4 Head CT Normal anatomy: A, high midbrain level; B, basal ganglia region. R L Sylvian cistern Cerebellum Quadrigeminal cistern Sylvian cistern Quadrigeminal cistern Lentiform nucleus Posterior limb (internal capsule)
Calcified falx Lateral ventricle Falx cerebri (calcified)
Central sulcus
FIGURE 69-5 Head CT Normal anatomy: A, lateral ventricles; B, upper cortex. R R L Calcified choroid Sulci Gyri L
Occipital horn
of another one. Following is a detailed description of the components of the mnemonic.
Blood
hematomas, subdural hematomas, intraparenchymal hemorrage, and subarachnoid hemorrhage each have a distinct appearance on the CT scan, as well as differing etiologies, complications, and associated conditions.
The appearance of blood on a head CT scan depends primarily on its location and size. Acute hemorrhage will appear hyperdense (bright white) on cranial CT images. This is attributed to the fact that the globin molecule is relatively dense, and hence effectively absorbs x-ray beams. Acute blood is typically in the range of 50 to 100 HU. As the blood becomes older and the globin molecule breaks down, it will lose this hyperdense appearance, beginning at the periphery and working in centrally. On the CT scan, blood will become isodense with the brain at 1 to 2 weeks, depending on clot size, and will become hypodense with the brain at approximately 2 to 3 weeks (Fig. 69-6). The precise localization of the blood is as important as identifying its presence (Fig. 69-7). Epidural
Epidural Hematoma
Epidural hematoma most frequently appears as a lens-shaped (biconvex) collection of blood, usually over the brain convexity. An epidural hematoma will not cross a suture line, as the dura is tacked down in these areas. Epidural hematomas arise primarily (85%) from arterial laceration due to a direct blow, with the middle meningeal artery the most common source. A small proportion, however, come from other injured arteries and can even be venous in origin.
Subdural Hematoma
Subdural hematoma appears as a sickle- or crescentshaped collection of blood, usually over the cerebral
Ch069-X2872.indd 756
3/3/2008 1:44:04 PM
CHAPTER 69
How to Read a Head CT Scan
757
BOX 69-2
The Blood Can Be Very Bad Mnemonic*
BloodAcute hemorrhage appears hyperdense (bright white) on CT. This is due to the fact that the globin molecule is relatively dense and hence effectively absorbs x-ray beams. As the blood becomes older and the globin breaks down, it loses this hyperdense appearance, beginning at the periphery. The precise localization of the blood is as important as identifying its presence. CisternsCerebrospinal uid collections jacketing the brain; the following four key cisterns must be examined for blood, asymmetry, and effacement (representing increased intracranial pressure): CircummesencephalicCerebrospinal uid ring around the midbrain; rst to be effaced with increased intracranial pressure Suprasellar (star-shaped)Location of the circle of Willis; frequent site of aneurysmal subarachnoid hemorrhage QuadrigeminalW-shaped cistern at top of midbrain; effaced early by rostrocaudal herniation SylvianBetween temporal and frontal lobes; site of traumatic and distal mid-cerebral aneurysm and subarachnoid hemorrhage BrainExamine for: SymmetrySulcal pattern (gyri) well differentiated in adults and symmetric side-to-side. Gray-white differentiationEarliest sign of cerebrovascular aneurysm is loss of gray-white differentiation; metastatic lesions often found at gray-white border ShiftFalx should be midline, with ventricles evenly spaced to the sides; can also have rostrocaudal shift, evidenced by loss of cisternal space; unilateral effacement of sulci signals increased pressure in one compartment; bilateral effacement signals global increased pressure Hyper-/hypodensityIncreased density with blood, calcication, intravenous contrast media; decreased density with air/gas (pneumocephalus), fat, ischemia (cerebrovascular aneurysm), tumor VentriclesPathologic processes cause dilation (hydrocephalus) or compression/shift; hydrocephalus usually rst evident in dilation of the temporal horns (normally small and slit-like); examiner must take in the whole picture to determine if the ventricles are enlarged due to lack of brain tissue or to increased cerebrospinal uid pressure BoneHighest density on CT scan; diagnosis of skull fracture can be confusing due to the presence of sutures in the skull; compare other side of skull for symmetry (suture) versus asymmetry (fracture); basilar skull fractures commonly found in petrous ridge (look for blood in mastoid air cells)
*Blood = blood, Can = cisterns, Be = brain, Very = ventricles, Bad = bone.
FIGURE 69-6 CT scan appearance of central nervous system hemorrhage: A, acute; B, subacute; C, chronic.
Ch069-X2872.indd 757
3/3/2008 1:44:05 PM
758
SECTION VIII
Injuries to Bones and Organs 0 10
FIGURE 69-7 CT appearance of blood of differing etiologies: A, epidural hematoma; B, subdural hematoma; C, intraparenchymal and intraventricular hematomas.
convexity. Subdural hematomas can also be seen as isolated collections that appear in the interhemispheric ssures or along the tentorium. As opposed to epidural hematomas, subdural hematomas will cross suture lines, as there is no anatomic limitation to blood ow below the dura. A subdural hematoma can be either an acute lesion or a chronic one. While both occur primarily from disruption of surface and/ or bridging vessels, the magnitude of impact damage is usually much higher in acute lesions. As such, they are frequently accompanied by severe brain injury, contributing to a much poorer overall prognosis than epidural hematoma. Chronic subdural hematoma, in contrast with acute subdural hematoma, usually follows a more benign course than acute subdural hematoma. Attributed to slow venous oozing after even a minor closed head injury, the clot can gradually accumulate, allowing the patient to compensate. As the clot is frequently encased in a fragile vascular membrane, however, these patients are at signicant risk for rebleeding as the result of additional minor trauma. The CT appearance of a chronic subdural hematoma depends on the length of time since the initial bleeding. A subdural hematoma that is isodense with brain can be very difcult to detect on CT, and in these cases contrast may highlight the surrounding vascular membrane.
In distinction to traumatic lesions, nontraumatic hemorrhagic lesions due to hypertensive disease are typically seen in elderly patients and occur most frequently in the basal ganglia region. Hemorrhage from such lesions may rupture into the ventricular space, with the additional nding of intraventricular hemorrhage on CT. Posterior fossa bleeding (e.g., cerebellar) may dissect into the brainstem (pons, cerebellar peduncles) or rupture into the fourth ventricle. Besides hypertensive etiologies, intraparenchymal hemorrhages can be caused by arteriovenous malformations, bleeding from or into a tumor, amyloid angiopathy, or aneurysms that happen to rupture into the substance of the brain rather than into the subarachnoid space.
Intraventricular Hemorrhage
Intraparenchymal Hemorrhage
Cranial CT can reliably identify intraparenchymal (or intracerebral) hematomas as small as 5 mm. These appear as high-density areas on the CT scan, usually with much less mass effect than their apparent size would indictate. Traumatic intraparenchymal hemorrhages may be seen immediately following an injury, or they can appear in a delayed fashion, after there has been time for swelling. Additionally, contusions may enlarge and coalesce over rst 2 to 4 days. Traumatic contusions most commonly occur in areas where sudden deceleration of the head causes the brain to impact on bony prominences (e.g., temporal, frontal, occipital poles).
Intraventricular hemorrhage can be traumatic or secondary to intraparenchymal hemorrhage or subarachnoid hemorrhage with ventricular rupture. Identied as a white density in the normally black ventricular spaces, it is associated with a particularly poor outcome in cases of trauma (although this may be more of a marker than a causative issue). Hydrocephalus can be the end result regardless of the etiology. Cerebrospinal uid (CSF) is produced in the lateral ventricles at a rate of 0.5 to 1 mL per minute, and this will occur regardless of the intraventricular pressure. A block at any point in the CSF pathway (lateral ventricles foramen of Monro 3rd ventricle aqueduct of Sylvius 4th ventricle foramina of Luschka and Magendie cisterns arachnoid granulations) will result in hydrocephalus, with associated increased intracranial pressure and the ultimate potential for herniation.
Subarachnoid Hemorrhage
Subarachnoid hemorrhage is dened as hemorrhage into any subarachnoid space that is normally lled with CSF (e.g., cistern, brain convexity). The hyperdensity of blood in the subarachnoid space is frequently visible on CT imaging within minutes of the onset of hemorrhage (Fig. 69-8). Subarachnoid
Ch069-X2872.indd 758
3/3/2008 1:44:05 PM
CHAPTER 69
How to Read a Head CT Scan
759
FIGURE 69-8 CT appearance of subarachnoid hemorrhage: A, blood lling the suprasellar cistern; B, blood lling the sylvian cistern.
A
hemorrhage is most commonly aneurysmal (75%80%), but it can also occur with trauma, tumor, arteriovenous malformations and dural malformations. As a result of arachnoid granulations becoming plugged with red blood cells or their degradation products, hydrocephalus complicates approximately 20% of cases of subarachnoid hemorrhage. The ability of a CT scanner to demonstrate subarachnoid hemorrhage depends on a number of factors, including the generation of scanner, the time since the initial bleeding, and the skill of the examiner. According to some studies, the CT scan is 95% to 98% sensitive for subarachnoid hemorrhage in the rst 12 hours after the ictus.9-11 This sensitivity is reported to decrease as follows: 90%-95% at 24 hours 80% at 3 days 50% at 1 week 30% at 2 weeks
B
CircummesencephalicHypodense CSF ring around the midbrain; most sensitive marker for increased intracranial pressure; will become effaced rst with increased pressure and herniation syndromes. SuprasellarStar-shaped hypodense space above the sella and pituitary; location of the circle of Willis, hence an excellent location for identifying aneurysmal subarachnoid hemorrhage. QuadrigeminalW-shaped cistern at the top of the midbrain; can be a location for identifying traumatic subarachnoid hemorrhage, as well as an early marker of increased intracranial pressure and rostrocaudal herniation (Fig. 69-10). SylvianBilateral CSF space located between the temporal and frontal lobes of the brain; another good location to identify subarachnoid hemorrhage, whether caused by trauma or aneurysm leak (particularly distal middle cerebral artery aneurysms).
Extracranial Hemorrhage Brain
Normal brain parenchyma has an inhomogeneous appearance where the gray and white matter interface. Cortical gray matter is denser than subcortical white matter; therefore the cortex will appear lighter on CT imaging. Given that many disease processes we are looking for in the ED are unilateral (e.g., cerebrovascular aneurysm, tumor, abscess), the clinician should be aware that there will normally be side-toside symmetry on the scan. Similarly, the cortical gyral and sulcal pattern should be symmetric (Fig. 69-11). Besides symmetry, it is important to examine the brain parenchyma for: Gray-white differentiationThe earliest sign of an ischemic cerebrovascular aneurysm will be loss of gray-white differentiation. Tumors can also obscure this interface, particularly when there is associated edema (hypodensity). ShiftThe falx should be midline, with ventricles evenly spaced to the sides. With rostrocaudal herniation the midline will be preserved, but this
The presence and signicance of extracranial blood and soft-tissue swelling on CT imaging is often overlooked. The examiner should use this nding to lead to subtle fractures that can be identied in areas of maximal impact (and hence maximal soft-tissue swelling). This will also direct the examiner to search the underlying brain parenchyma in these areas for parenchymal contusions, as well as to areas opposite maximal impact to search for contrecoup injuries.
Cisterns
Cisterns are potential spaces formed where there is a collection of CSF that is pooled as it works its way up to the superior sagittal sinus from the 4th ventricle. Of the numerous named cisterns (and some with multiple names), there are four key cisterns that the EP needs to be familiar with in order to identify increased intracranial pressure as well as the presence of blood in the subarachnoid space (Fig. 69-9). These cisterns are:
Ch069-X2872.indd 759
3/3/2008 1:44:05 PM
760
SECTION VIII
Injuries to Bones and Organs
Pons Top of fourth ventricle
Suprasellar cistern Circumesencephalic cistern
Cerebral peduncles Quadrigeminal cistern
Quadrigeminal Circumesencephalic cistern cistern Tempocal horn of lateral ventricle Occipital horn of lateral ventricle
Suprasellar cistern
Sylvian cistern
Interhemispheric cistern
FIGURE 69-9 Three important cerebrospinal uid cisterns: A, cisterns viewed at high pontine level; B, cisterns viewed at level of cerebral peduncles; C, cisterns viewed at high midbrain level.
FIGURE 69-10 CT appearance of increased intracranial pressure: A, normal intracranial pressure; B, elevated intracranial pressure.
Ch069-X2872.indd 760
3/3/2008 1:44:05 PM
CHAPTER 69
How to Read a Head CT Scan
761
FIGURE 69-11 CT appearance of normal brain.
FIGURE 69-12 CT scan appearance of tumor with edema and midline shift.
will usually be evidenced by loss of cisternal spaces. A unilateral effacement of sulci signals increased pressure in one compartment. Bilateral effacement signals global increased pressure. Hyper/hypodensityBrain will take on increased density with blood, calcication, and intravenous contrast media. It will take on decreased density with air (pneumocephalus), water, fat, and ischemia (cerebrovascular accident). Tumor may result in either increased or decreased density on CT imaging, depending on tumor type and amount of associated water density (edema).
following information: location and sizeintraaxial (within the brain parenchyma) or extraaxial; degree of edema and mass effectfor example, herniation may be impending due to swelling. Abscess. Brain abscess will appear as an ill-dened hypodensity on non-contrast CT scan. A variable amount of edema is usually associated with such lesions and, like tumors, they will frequently demonstrate ring-enhancement with the addition of an intravenous contrast agent. Ischemic Infarction. Strokes are classied as either hemorrhagic or nonhemorrhagic. Nonhemorrhagic infarctions can be seen as early as 2 to 3 hours following ictus, but most will not begin to be clearly evident on the CT scan for 12 to 24 hours. The earliest change seen in areas of ischemia is loss of graywhite differentiation, due to inux of water into the metabolically active gray matter. With the loss of blood ow, the energy-dependent cellular ion pumps fail, and the movement of ions such as sodium and potassium is no longer regulated. By osmotic forces, water follows the ions into the cells, where they cease metabolic activity. Because gray matter is metabolically more active than white matter, the gray cells are affected rst, become water-lled, and take on the CT appearance of white matter. This loss of graywhite differentiation can initially be a subtle nding but ultimately will become evident and will usually be maximal between days 3 and 5 (Fig. 69-13). Any vascular distribution can be affected by ischemic lesions (e.g., middle cerebral artery aneurysm, posterior inferior cerebellar artery). One specialized type of stroke frequently identied on CT imaging is
Specic Brain Parenchymal Lesions
Tumor. Brain tumors usually appear as hypodense, poorly dened lesions on noncontrast CT scans. It is estimated that 70% to 80% of brain tumors will be apparent on plain scans without the use of an intravenous contrast agent. Calcication and hemorrhage associated with a tumor can cause it to have a hyperdense appearance. Tumors should be suspected on a noncontrast CT scan when signicant edema is associated with an ill-dened mass. This vasogenic edema occurs because of a loss of integrity of the bloodbrain barrier, allowing uid to pass into the extracellular space. Edema, because of the increased water content, appears hypodense on the CT scan (Fig. 69-12). Intravenous contrast material can help dene brain tumors. Contrast media will leak through the incompetent blood-brain barrier into the extracellular space surrounding the mass lesion, resulting in a contrast-enhancing ring. Once a tumor is identied, the clinician should make some determination of the
Ch069-X2872.indd 761
3/3/2008 1:44:05 PM
762
SECTION VIII
Injuries to Bones and Organs
through egress from the 4th ventricle. Hydrocephalus frequently is rst evident in dilation of the temporal horns, which are normally small with a slit-like morphology. When examining the ventricular system for hydrocephalus, the clinician needs to take in the entire picture of the brain, as ventricles can be large for reasons other than increased pressure (e.g., atrophy). If the ventricles are large, the clinician should investigate whether other CSF spaces in the brain are large (e.g., sulci, cisterns). In this case, it is likely that this enlargement is the result of brain volume loss rather than the increased ventricle size. Conversely, if the ventricles are large, but the brain appears tight with sulcal effacement and loss of sulcal space, then the likelihood of hydrocephalus is high. The clinician also should look for evidence of increased intracranial pressure (e.g., cisternal effacement).
Bone
FIGURE 69-13 CT scan appearance of a large left middle cerebral artery stroke. The hypodense brain is the infarcted region. Note midline shift from left to right.
a lacunar infarction, which are small, discrete nonhemorrhagic lesions usually secondary to hypertension and found in the basal ganglia region. They frequently are clinically silent.
Ventricles
Pathologic processes can cause either dilation (hydrocephalus) or compression/shift of the ventricular system (Fig. 69-14). Additionally, hemorrhage can occur into any of the ventricles, resulting in the potential for obstruction of ow and resulting hydrocephalus. The term communicating hydrocephalus is used when there is free CSF egress from the ventricular system, with a blockage at the level of the arachnoid granulations. The term noncommunicating hydrocephalus is used if there is obstruction anywhere along the course of ow from the lateral ventricles
As demonstrated earlier, bone has the highest density on the CT scan (+1000 HU). Because of this, depressed or comminuted skull fractures can usually be easily identied on the CT scan; however, small linear (nondepressed) skull fractures and fractures of the skull base may be more difcult to nd (Fig. 69-15). Also, making the diagnosis of a skull fracture can be confusing due to the presence of sutures in the skull. Fractures may occur at any portion of the bony skull. The presence of a skull fracture should increase the index of suspicion for intracranial injury. If intracranial air is seen on a CT scan, this indicates that the skull and dura have been violated at some point (Fig. 69-16). Basilar skull fractures are most commonly found in the petrous ridge (the dense pyramidal-shaped portion of the temporal bone). Due to the density of this bone, the fracture line may not be easily identied in this area. The clinician should not only search for such a fracture line but should also pay close attention to the normally aerated mastoid air cells that are contained within this bone. Any blood in the mastoid air cells means that a skull base fracture is likely. Analogous to the mastoid air cells, the maxillary, ethmoid, and sphenoid sinuses should
FIGURE 69-14 CT appearance of abnormal ventricles.
Ch069-X2872.indd 762
3/3/2008 1:44:06 PM
CHAPTER 69
How to Read a Head CT Scan
763
FIGURE 69-15 CT appearance in bone pathology: A, linear skull fracture; B, depressed, comminuted skull fracture; C, basilar skull fracture.
care of ED patients. An important tenet in the use of cranial CT is that accurate interpretation is required to make good clinical decisions. Cranial CT interpretation is a skill, like ECG interpretation, that can be learned through education, practice, and repetition.
REFERENCES
1. Schreiger DL, Kalafut M, Starkman S, et al: Cranial computed tomography interpretation in acute stroke. JAMA 1998;279:1293-1297. 2. Perron AD, Huff JS, Ullrich CG, et al: A multicenter study to improve emergency medicine residents recognition of intracranial emergencies on computed tomography. Ann Emerg Med 1998;32:554-562. 3. Leavitt MA, Dawkins R, Williams V, et al: Abbreviated educational session improves cranial computed tomography scan interpretations by EPs. Ann Emerg Med 1997; 30:616-621. 4. Alfaro DA, Levitt MA, English DK, et al: Accuracy of interpretation of cranial computed tomography in an emergency medicine residency program. Ann Emerg Med 1995; 25:169-174. 5. Roszler MH, McCarroll KA, Donovan RT, et al: Resident interpretation of emergency computed tomographic scans. Invest Radiol 1991;26:374-376. 6. Arendts G, Manovel A, Chai A: Cranial CT interpretation by senior emergency departments staff. Australas Radiol 2003;47:368-374. 7. Saketkhoo DD, Bhargavan M, Sunshine JH, et al: Emergency department image interpretation services at private community hospitals. Radiology 2004;231:190-197. 8. Lowe RA, Abbuhl SB, Baumritter A, et al: Radiology services in emergency medicine residency programs: A national survey. Acad Emerg Med 2002;9:587-594. 9. Boesiger BM. Shiber JR: Subarachnoid hemorrhage diagnosis by computed tomography and lumbar puncture: Are fth generation CT scanners better at identifying subarachnoid hemorrhage? J Emerg Med 2005;29:23-27. 10. Van der Wee N, Rinkel GJE, van Gijn J: Detection of subarachnoid hemorrhage on early CT: Is lumbar puncture still needed after a negative scan? J Neurol Neurosug Psychiatry 1995;58:357-359. 11. Morgenstern LB: Worst headache and subarachnoid hemorrhage prospective, modern computed tomography and spinal uid analysis. Ann Emerg Med 1998;32:297-304.
FIGURE 69-16 CT scan appearance of intracranial air.
be visible and aerated; the presence of uid in any of these sinuses in the setting of trauma should raise suspicion of a skull fracture. In nontraumatic cases, uid in the mastoids may indicate mastoiditis, and uid in the sinuses may indicate sinusitis.
Summary
Cranial CT is integral to the practice of emergency medicine and is used on a daily basis to make important, time-critical decisions that directly impact the
Ch069-X2872.indd 763
3/3/2008 1:44:06 PM
Ch069-X2872.indd 764
3/3/2008 1:44:07 PM
You might also like
- Basics of How To Read ScansDocument12 pagesBasics of How To Read Scanslexi_2706No ratings yet
- Unit 5 Medical UltrasoundDocument6 pagesUnit 5 Medical Ultrasoundtwy113No ratings yet
- CSF Flowmetry MriDocument5 pagesCSF Flowmetry MribricklaneNo ratings yet
- X-Ray Reveals Skull Lesions in Multiple Myeloma PatientDocument63 pagesX-Ray Reveals Skull Lesions in Multiple Myeloma Patient李建明No ratings yet
- Retrohepatic Gallbladder Masquerading As Hydatid Cyst in ADocument18 pagesRetrohepatic Gallbladder Masquerading As Hydatid Cyst in AMadalina BlagaNo ratings yet
- Liquor CerebrospinalisDocument25 pagesLiquor CerebrospinalisIhda ParidahNo ratings yet
- Clinical Imaging of Liver, Gallbladder, BiliaryDocument93 pagesClinical Imaging of Liver, Gallbladder, Biliaryapi-3856051100% (1)
- Classical Radiological SignsDocument2 pagesClassical Radiological SignsMuntaha JavedNo ratings yet
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDocument42 pagesHepatobiliary Disorders: Katrina Saludar Jimenez, R. NreykatNo ratings yet
- Brain Ventricles AnatomyDocument25 pagesBrain Ventricles AnatomyMiazan SheikhNo ratings yet
- Infertile Couple - Role of Ultrasound FinalDocument31 pagesInfertile Couple - Role of Ultrasound FinalKalpavriksha1974No ratings yet
- The Normal CSFDocument2 pagesThe Normal CSFUm MahmoudNo ratings yet
- DR Kaushal CSF Physiology PresentationDocument39 pagesDR Kaushal CSF Physiology Presentationoddie333No ratings yet
- Fluid CerebrospinalDocument3 pagesFluid CerebrospinalAurelia AlexandraNo ratings yet
- BILIARY TRACT DISEASE: GALLSTONES, CHOLECYSTITIS, CHOLEDOCHOLITHIASIS, AND CHOLANGITISDocument6 pagesBILIARY TRACT DISEASE: GALLSTONES, CHOLECYSTITIS, CHOLEDOCHOLITHIASIS, AND CHOLANGITISRafael KameradNo ratings yet
- CSF and Cerebral Blood FlowDocument58 pagesCSF and Cerebral Blood FlowCindy PrayogoNo ratings yet
- CSFDocument21 pagesCSFjannatin aliya indrinaNo ratings yet
- Cerebrospinal, Pleural and Ascitic Uids: Case 1Document6 pagesCerebrospinal, Pleural and Ascitic Uids: Case 1Amelia PebriantiNo ratings yet
- m2 Bony Anatomy of LegDocument3 pagesm2 Bony Anatomy of LegabidalibpNo ratings yet
- Lower Limb Radiology GuideDocument65 pagesLower Limb Radiology GuideVivien EnriquezNo ratings yet
- Chest X-ray Interpretation Methodical ApproachDocument13 pagesChest X-ray Interpretation Methodical ApproachduncanNo ratings yet
- Molar Pregnancy PDFDocument8 pagesMolar Pregnancy PDFEgaSuharnoNo ratings yet
- 7 PRINCIPLES BREAKTHROUGH THINKINGDocument5 pages7 PRINCIPLES BREAKTHROUGH THINKINGNaysia Kartika100% (1)
- AngiographyDocument17 pagesAngiographyPimsiree MameawNo ratings yet
- Lower Limb: Fig. (1) : A Photoradiograph of A Plain X Ray of The Pelvis (Antero-Posterior View) ShowingDocument8 pagesLower Limb: Fig. (1) : A Photoradiograph of A Plain X Ray of The Pelvis (Antero-Posterior View) ShowingAmany AliNo ratings yet
- Cerebrospinal Fluid: Dr. Anupriya JDocument33 pagesCerebrospinal Fluid: Dr. Anupriya JVivek PatelNo ratings yet
- Ultrasound Și DopplerDocument3 pagesUltrasound Și DopplerAurelia AlexandraNo ratings yet
- Jaundice MasterDocument76 pagesJaundice MasterVinoth KumarNo ratings yet
- Some Techniques of Problem Solving: Work Out The Major Factors InvolvedDocument19 pagesSome Techniques of Problem Solving: Work Out The Major Factors InvolvedRahul M PatilNo ratings yet
- AnatomyDocument94 pagesAnatomypshahNo ratings yet
- Septum Formation in The VentriclesDocument43 pagesSeptum Formation in The VentriclesAhsan IslamNo ratings yet
- Figures Liver and GallbladderDocument32 pagesFigures Liver and GallbladdermarkNo ratings yet
- Liver: Presented by Dr. Tahmina Islam MD Third PartDocument121 pagesLiver: Presented by Dr. Tahmina Islam MD Third PartNajib JamilNo ratings yet
- Bls (Basic Life Support) & Acls (Advanced Care Life Support) : PresenterDocument135 pagesBls (Basic Life Support) & Acls (Advanced Care Life Support) : PresenterbernarduswidodoNo ratings yet
- Ultrasonography of The Hepatobiliary TractDocument9 pagesUltrasonography of The Hepatobiliary TractPaola Méndez NeciosupNo ratings yet
- Cardiovascular Diseases and LiverDocument20 pagesCardiovascular Diseases and LiverKrishna KumarNo ratings yet
- Abdominal US in Hepatobiliary DiseasesDocument76 pagesAbdominal US in Hepatobiliary DiseasesSyafari D. MangopoNo ratings yet
- EVOLUTIONARY BLUNDERSDocument3 pagesEVOLUTIONARY BLUNDERSeustoque2668No ratings yet
- Interventional Radiology & AngiographyDocument45 pagesInterventional Radiology & AngiographyRyBone95No ratings yet
- Cerebrospinal CSFDocument31 pagesCerebrospinal CSFRashid MohamedNo ratings yet
- CXR Interpretation Guide: ABCDE ApproachDocument1 pageCXR Interpretation Guide: ABCDE ApproachValentina SepúlvedaNo ratings yet
- Wave Propogation EffectDocument4 pagesWave Propogation EffectPrashanth ChikkannanavarNo ratings yet
- LiverultrasoundDocument62 pagesLiverultrasoundiuliia94No ratings yet
- Pediatric Echocardiography: Understanding Congenital Heart DefectsDocument159 pagesPediatric Echocardiography: Understanding Congenital Heart DefectsSergiu NiculitaNo ratings yet
- Carotid Stenosis CriteriaDocument50 pagesCarotid Stenosis CriteriafiuliaNo ratings yet
- Classic Radiology SignsDocument9 pagesClassic Radiology SignsJui DirDapNo ratings yet
- Embryology Respiratory System: Formation of Lung BudsDocument1 pageEmbryology Respiratory System: Formation of Lung Budsrezairfan221No ratings yet
- Scrotum Protocol 14Document2 pagesScrotum Protocol 14api-349402240No ratings yet
- Neurovascular SonographyDocument539 pagesNeurovascular SonographyAlexandra MoraesNo ratings yet
- Foldings of Embryo Foetal Period 1Document22 pagesFoldings of Embryo Foetal Period 1Riya SinghNo ratings yet
- High-Resolution Ultrasound in The Assessment of Soft Tissue Tumors and Tumor-Like LesionsDocument41 pagesHigh-Resolution Ultrasound in The Assessment of Soft Tissue Tumors and Tumor-Like LesionsAlvin JulianNo ratings yet
- Normal Variant in Abdominal UltrasounDocument20 pagesNormal Variant in Abdominal Ultrasounshanks spearsonNo ratings yet
- Liver Imaging: MRI with CT CorrelationFrom EverandLiver Imaging: MRI with CT CorrelationErsan AltunNo ratings yet
- Women's Imaging: MRI with Multimodality CorrelationFrom EverandWomen's Imaging: MRI with Multimodality CorrelationMichele A. BrownRating: 5 out of 5 stars5/5 (1)
- P1Document12 pagesP1Roykedona Lisa TrixieNo ratings yet
- Reading A Head CT, What Every EP Should Know PDFDocument62 pagesReading A Head CT, What Every EP Should Know PDFAdistya Sari100% (1)
- CT ScanDocument12 pagesCT ScanNita ThrenitatiaNo ratings yet
- Interpretasi CT ScanDocument19 pagesInterpretasi CT ScanAB KristiadiNo ratings yet
- San 12193Document6 pagesSan 12193Karla BFNo ratings yet
- Wereldleiders Op TwitterDocument24 pagesWereldleiders Op TwitterHerman CouwenberghNo ratings yet
- TRAI Data Till 31st March, 2014Document19 pagesTRAI Data Till 31st March, 2014Tamanna Bavishi ShahNo ratings yet
- Nightingales - Philips Healthcare Tie UpDocument3 pagesNightingales - Philips Healthcare Tie UpSumit RoyNo ratings yet
- The State of Airline Marketing Airlinetrends Simpliflying April2013Document21 pagesThe State of Airline Marketing Airlinetrends Simpliflying April2013Sumit RoyNo ratings yet
- Mobile Advertising Research Trends and InsightsDocument15 pagesMobile Advertising Research Trends and InsightsSumit RoyNo ratings yet
- World Health Days 2014: JanuaryDocument2 pagesWorld Health Days 2014: JanuaryIvy Jorene Roman RodriguezNo ratings yet
- Risk Factors From Hepatitis BCDDocument1 pageRisk Factors From Hepatitis BCDSumit RoyNo ratings yet
- Calendário de Jogos Do Mundial de Futebol-Brasil 2014Document0 pagesCalendário de Jogos Do Mundial de Futebol-Brasil 2014Miguel RodriguesNo ratings yet
- Hepatitis A eDocument1 pageHepatitis A eSumit RoyNo ratings yet
- Hepatitis A eDocument1 pageHepatitis A eSumit RoyNo ratings yet
- NokiaDocument1 pageNokiaSumit RoyNo ratings yet
- The State of Mobile Advertising in Emerging Countries TLS EmergingMarketsDocument8 pagesThe State of Mobile Advertising in Emerging Countries TLS EmergingMarketsSumit RoyNo ratings yet
- MGI China E-Tailing Executive Summary March 2013Document18 pagesMGI China E-Tailing Executive Summary March 2013Sumit RoyNo ratings yet
- Mediamind Comscore Research Dwelling On EntertainmentDocument20 pagesMediamind Comscore Research Dwelling On EntertainmentSumit RoyNo ratings yet
- Global Top 100 Most Valueable Brands Brandz2014 - Infographic PDFDocument1 pageGlobal Top 100 Most Valueable Brands Brandz2014 - Infographic PDFSumit RoyNo ratings yet
- Gender and Social Networking Activity :facebook Vs OthersDocument18 pagesGender and Social Networking Activity :facebook Vs OthersSumit RoyNo ratings yet
- FINAL - Mobile Advertising DeckDocument73 pagesFINAL - Mobile Advertising DecksumitkroyNo ratings yet
- World Health Statisitics FullDocument180 pagesWorld Health Statisitics FullClarice SalidoNo ratings yet
- CEO Survey On Hiring, Profitability and PeopleDocument36 pagesCEO Survey On Hiring, Profitability and PeopleSumit RoyNo ratings yet
- Calendar 14Document57 pagesCalendar 14Hanan AhmedNo ratings yet
- The 5 Free Alternatives To Microsoft WordDocument60 pagesThe 5 Free Alternatives To Microsoft WordSumit RoyNo ratings yet
- The State of Maternal Health, D Nutrition in Asia " World Vision DataDocument4 pagesThe State of Maternal Health, D Nutrition in Asia " World Vision DataSumit RoyNo ratings yet
- 2014 Bill and Melinda Gates Foundation Report On Global PovertyDocument28 pages2014 Bill and Melinda Gates Foundation Report On Global PovertySumit RoyNo ratings yet
- The 5 Free Alternatives To Microsoft WordDocument60 pagesThe 5 Free Alternatives To Microsoft WordSumit RoyNo ratings yet
- CVD Atlas 16 Death From Stroke PDFDocument1 pageCVD Atlas 16 Death From Stroke PDFRisti KhafidahNo ratings yet
- 10 Historical Speeches Nobody Ever HeardDocument20 pages10 Historical Speeches Nobody Ever HeardSumit Roy100% (1)
- India InfographicsDocument3 pagesIndia InfographicsSumit RoyNo ratings yet
- The Evolution of Digital Advertising 3.0: Adobe Research InsightsDocument1 pageThe Evolution of Digital Advertising 3.0: Adobe Research InsightsSumit RoyNo ratings yet
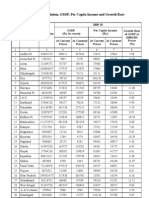
- Statewise GSDP PCI and G.RDocument3 pagesStatewise GSDP PCI and G.RArchit SingalNo ratings yet