Professional Documents
Culture Documents
PRP in Gynecology Surgery - Fanning
Uploaded by
api-222634056Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PRP in Gynecology Surgery - Fanning
Uploaded by
api-222634056Copyright:
Available Formats
Journal of Minimally Invasive Gynecology (2007) 14, 633 637
Phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery
James Fanning, DO, Luis Murrain, DO, Robert Flora, MD, Timothy Hutchings, DO, Jil M. Johnson, DO, and Bradford W. Fenton, MD, PhD
From the Department of Obstetrics and Gynecology, Summa Health System, Northeastern Ohio Universities College of Medicine, Akron, Ohio (all authors). KEYWORDS:
Autologous platelet tissue graft; Gynecologic surgery; Pain Abstract STUDY OBJECTIVE: To perform the original phase I/II trial of autologous platelet tissue graft in gynecologic surgery to evaluate toxicity and efcacy on decreasing pain. DESIGN: Prospective nonrandomized trial (Canadian Task Force classication II-A). SETTING: Teaching hospital. PATIENTS: Fifty-ve consecutive patients undergoing major gynecologic surgery were entered into this prospective phase I/II trial and were matched with 55 patients from the previous 6 months. INTERVENTION: After anesthesia was induced, peripheral venous blood (55 mL) was obtained from the patient producing, autologous platelet tissue graft (20 mL). At completion of surgery, autologous platelet tissue graft was directly applied to the surgical site. MEASUREMENTS AND MAIN RESULTS: Median pain on the day of surgery was 2.7 (mild) in the autologous platelet tissue graft group vs 6.7 (severe) in the control group, p .001. Likewise, pain on postoperative day 1 was 2.1 (mild) in the autologous platelet tissue graft group vs 5.5 (moderate) in the control group, p .001. Median of morphine per hospital stay for the autologous platelet tissue graft group was 17 mg (range 198 mg) vs 26 mg (range 390 mg) in the control group, which was statistically signicant at p .02. There were no adverse effects associated with autologous platelet tissue graft. CONCLUSIONS: In the original phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery, there were no apparent adverse effects, and pain was signicantly reduced. 2007 AAGL. All rights reserved.
More than 350 000 women undergo major gynecologic surgery in the United States each year. Major morbidity associated with gynecologic surgery includes pain, bleed-
Supported in part by a research grant funded by BioMet Biologics. There was no direct funding of this trial to Summa by BioMet Biologics. BioMet Biologics has provided funding to Summa for a swine postoperative adhesion study. Corresponding author: James Fanning, DO, Department of Obstetrics and Gynecology, Summa Health System, Northeastern Ohio Universities College of Medicine, 525 E. Market Street, Medical II, Akron, OH 44309. E-mail: fanning@summa-health.org Submitted March 27, 2007. Accepted for publication May 18, 2007.
ing, infection, hernia, and wound dehiscence. Reduction in the incidence of these morbidities would improve patient care and decrease medical expense. Recently, several autologous platelet-rich plasma preparations, including autologous platelet tissue graft (BioMet Biologics, Warsaw, IN), have been used clinically to enhance hemostasis and wound healing.1,2 Application of autologous platelet tissue graft to the operative site has a 3-fold effect (Figure 1). First, the concentrated platelets form a brin clot that aids in hemostasis. Second, the platelets degranulate and release numerous chemotactic and mitogenic growth factors (including platelet-derived growth
1553-4650/$ -see front matter 2007 AAGL. All rights reserved. doi:10.1016/j.jmig.2007.05.014
634
Journal of Minimally Invasive Gynecology, Vol 14, No 5, September/October 2007 dures, and advanced urogynecologic procedures requiring multiple repairs), aged 18 years or older, nonpregnant, and able to give informed consent comprised the study group. Institutional review board approval was granted, and written informed consent was obtained from all patients.
Patient characteristics
From August 5, 2005, through February 6, 2006, 55 consecutive patients were entered into this phase I/II trial, and none were excluded. Two patients declined to enter the trial. Patients were recruited from 3 physician ofces1 private gynecology group, 1 academic urogynecologist, and 1 academic gynecologic oncologist. Patient characteristics are presented in Table 1. Median age was 55 years old (24 84 years old), median weight was 167 lbs (112260 lbs), and 78% had medical comorbidities. Twenty-ve percent of surgical procedures were laparoscopic-assisted vaginal hysterectomy, 20% were extended urogynecologic procedures, and 22% were laparoscopic gynecologic oncology procedures.
Figure 1 Autologous platelet tissue graft: mechanism of action. EGF epidermal growth factor; PDGF platelet-derived growth factor; TGF transforming growth factor; VEGF vascular endothelial growth factor; WBC white blood cells.
factor, transforming growth factor, vascular endothelial growth factor, and epidermal growth factor), which aid in wound healing and decrease infection and pain. Third, increased white blood cell (WBC) concentration also aids in decreasing infection. Recent studies have shown that autologous platelet tissue graft produced by the Gravitational Platelet Separation system (BioMet Biologics) contains an 8-fold increase in platelet count, 5-fold increase in white blood cell count, a 4- to 6-fold increase in growth factors, and a 7-fold increase in serotonin3,4 compared with serum levels. Because autologous platelet tissue graft is obtained in the operating room and immediately directly applied to the patients own operative site, adverse effects should be minimal or nonexistent. Because of the small risk of adverse effects and encouraging initial empiric results, the use of autologous platelet tissue graft is increasing.1,2 However, the clinical effectiveness and safety in gynecologic surgery have not been proven. In general, there are 3 phases of clinical testing of new therapeutic agents.5 Phase I trials are designed to evaluate toxicity. Phase II trials determine efcacy. If phase I/II trials show safety and efcacy, a phase III trial is performed to determine whether the new treatment is more effective or safer than standard therapy. Therefore our purpose was to perform the original phase I/II trial of autologous platelet tissue graft in gynecologic surgery to evaluate toxicity and efcacy on pain.
Comparison group
Fifty-ve patients from the previous 6 months were matched by surgeon and surgical procedure. As can be seen from patient characteristics in Table 1, there was no difference between the groups in age, weight, race, medical comorbidities, or types of surgery. We believed this comparison group was justied because both groups had the same prospective pain evaluation by the same nursing staff who were blinded to the studys objectives. Also, the same preprinted postoperative pain management protocol was used for both groups.
Table 1
Patient characteristics APTG Control 49 (2776) 160 (67250) 80% 20% 63% (25) (22) (7) (25) (20) 14 10 4 12 15 (25) (18) (7) (22) (27) p .06 .13 .90 .10 .10
Materials and methods
Eligibility
Patients undergoing major gynecologic surgery (laparoscopic-assisted vaginal hysterectomy, laparoscopic-assisted vaginal hysterectomy with laparoscopic lymphadenectomy, abdominal hysterectomy, advanced laparoscopic proce-
Age (yrs) Weight (lbs) Race White Black Comorbidity Procedure (No., %) LAVH LAVH nodes Scope TAH Urogyn
55 (2484) 167 (112260) 87% 13% 78% 14 12 4 14 11
APTG autologous platelet tissue graft; LAVH laparoscopicassisted vaginal hysterectomy; LAVH nodes LAVH with lymphadenectomy; Scope advanced laparoscopic procedure; TAH abdominal hysterectomy; Urogyn advanced urogynecologic procedure.
Fanning et al
Phase I/II prospective trial of autologous platelet tissue graft
635
Technique of autologous platelet tissue graft (BioMet Biologics)
After induction of general anesthesia, peripheral venous blood (55 mL) was obtained from the patient and mixed with acid-citrate-dextrose-A 5 mL, an anticoagulant, in a 60-mL syringe. The syringe contents were transferred to the Gravitational Platelet Separation system disposable separation tube (GPSII; BioMet Biologics) (Figure 2) and spun in a BioMet centrifuge for 15 minutes at 3200 rpm. After centrifugation, 2 aliquots of 7 mL of platelet-poor plasma and 3 mL of platelet concentrate (platelets and WBCs) were obtained and transferred to two 10-mL syringes. An activation solution was prepared by mixing 1000 units of topical bovine thrombin (Jones Pharma, St. Louis, MO) per milliliter of 10% CaCl2 solution. The thrombin directly activates platelets, and the CaCL2 deactivates the acid-citrate-dextrose-A anticoagulant. The activation solution was drawn into two 1-mL syringes. The 10-mL platelet-poor plasma/ platelet concentrate syringe and the 1-mL activation syringe were connected, in tandem, to the BioMet Malleable Dual Cannula Tip, a dual-spray apparatus (Figure 3). This allows both syringe plungers to be advanced in unison, mixing the 2 sprays, which allows activation before reaching the wound bed. At completion of the surgical procedure and after ensuring adequate hemostasis, the autologous platelet tissue graft was directly applied to the surgical site (including the vaginal cuff, parametrium, and fascia). Depending on the surgical procedure, autologous platelet tissue graft was applied vaginally, laparoscopically, or transabdominally (Figure 4). Surgical application takes approximately 1 minute.
Figure 3
BioMet Malleable Duel Cannula Tip.
Data collection
All hospital data were collected prospectively before discharge. Patients were followed up for 28 days with outpatient checkups scheduled for the seventh and twenty-eighth postoperative day. Pain was evaluated with the visual analog scoring system6: 0 no pain, 2 mild, 5 moderate, 7 severe, 10 excruciating. At Summa, visual analog scoring is prospectively performed and recorded every 4 hours by the nursing staff. The highest visual analog score on postoperative day 0 and postoperative day 1 was used. Preprinted postoperative pain management protocol was the same for both groups: ketorolac 30 mg intravenously every 6 hours for 4 doses, morphine 2 to 5 mg intravenously every 2 hours as needed, and oxycodone/acetaminophen 5/325 mg 1 to 2 tablets orally every 6 hours as needed. For the few patients that required meperi-
Figure 2
Gravitational Platelet Separation (GPSII) tube.
Figure 4 graft.
Laparoscopic application of autologous platelet tissue
636
Journal of Minimally Invasive Gynecology, Vol 14, No 5, September/October 2007 No patient treated with autologous platelet tissue graft had a surgical site infection or postoperative dehiscence develop. Because the control group was not prospectively followed up, data on infection and dehiscence was not available. Autologous platelet tissue graft was not associated with any apparent adverse effects.
dine, a conversion of meperidine 75 mg to morphine 10 mg was used. The oxycodone/acetaminophen to morphine conversion was 2 tablets to 4 mg of morphine. For the comparison group, hospital data were collected, as well as outpatient follow-up for 28 days. Because the control group was not prospectively evaluated after hospital discharge, accurate visual analog scores for pain on postoperative day 7 and 28 are not available.
Statistics
Discreet variables were compared by use of 2 or Fishers exact test, and continuous variables were compared by t testing. A power analysis was performed with a p value .05, power of .80 and a 25% difference in pain as being medically signicant. Sample size calculation estimated a required sample size of 35 patients per group.
Discussion
Autologous platelet tissue graft is being used clinically to enhance hemostasis and wound healing after surgery.1,2 Concentrated platelets obtained from the patients own blood are applied directly to the operative site. The 8-fold increase in platelet count forms a brin clot, which aids in hemostasis3,4 (Figure 1). When the concentrated platelets degranulate they release numerous chemotactic and mitogenic growth factors (including platelet-derived growth factor, transforming growth factor, vascular endothelial growth factor, and epidermal growth factor), which aid in wound healing, decrease infection, and decrease pain3,4 (Figure 1). Growth factors have a chemotactic and mitogenic effect on broblasts and mesenchymal stem cells, which leads to reepithelialization, angiogenesis, and collagen formation, which accelerates wound healing. The 5-fold increase in white blood cell count along with the chemotactic and mitogenic effect of growth factors on neutrophils may help decrease infection. Also, the growth factor chemotactic effect increases the concentration of serotonin, which helps decrease pain. Although autologous platelet tissue graft is clinically being used,3,4 the clinical effectiveness and safety has not been proven, and thus we performed the original phase I/II trial of autologous platelet tissue graft (BioMet Biologics) in gynecologic surgery. None of the 55 patients treated developed a side effect from autologous platelet tissue graft. This was expected because autologous platelet tissue graft is obtained in the operating room from the patient and immediately directly applied to the patients own operative site. In the phase II portion, we found a signicant reduction in pain. Patients treated with autologous platelet tissue grafting had an approximate two-thirds reduction in pain resulting in mild postoperative pain versus moderate to severe postoperative pain in the control subjects (statistically signicant, p .001). Also, morphine use was reduced approximately 50% in the autologous platelet tissue graft group compared with the control subjects, which was statistically signicant at p .02. Because this was a phase I/II trial, blinding was not performed, and therefore placebo effect can not be excluded. Although our study did not have enough power to evaluate efcacy on surgical site infection or postoperative dehiscence, no patients treated with autologous platelet tissue graft developed these complications. Multiple additional investigations of autologous platelet tissue graft are needed. We are presently evaluating postoperative adhesions in a swine model. In the future, we are planning to evaluate the effects of autologous platelet tissue grafting on
Results
Results are shown in Table 2. Median blood loss was 270 mL (10 500 mL), and median operative time was 163 minutes (75330 minutes). Median change of postoperative hemoglobin was 1.8 g, and median length of stay was 1.3 days. Comparing these results with the 55 matched control subjects (Table 2); there was no statistically signicant difference in blood loss, operative time, median change in hemoglobin, or length of stay. Comparing patients treated with autologous platelet tissue graft to matched controls, postoperative pain was signicantly reduced. Median pain on the day of surgery was 2.7 (mild) in the autologous platelet tissue graft group vs 6.7 (severe) in the control group, p .001. Likewise, pain on postoperative day 1 was 2.1 (mild) in the autologous platelet tissue graft group versus 5.5 (moderate) in the control group, p .001. Median pain in the autologous platelet tissue graft group was 0.3 on postoperative day 7 and 0 on postoperative day 28. The median dose of morphine per hospital stay for the autologous platelet tissue graft group was 17 mg (198 mg) vs 26 mg (390 mg) in the control group, which was statistically signicant at p .02.
Table 2
Surgical characteristics APTG Control 272 143 2.0 1.4 6.8 5.6 (501000) (40360) (15) (110) (110) p .48 .06 .16 .17 .001 .001 .02
Blood loss OR Time (min) Hgb (g/dL) LOS (days) Pain day 0 Pain day 1 Pain day 7 Pain day 28 Morphine (mg)
270 163 1.8 1.3 2.7 2.1 0.3 0 17
(1001500) (75330) (14) (07) (06) (03) (198)
26 (390)
APTG Autologous platelet tissue graft; Hgb change in hemoglobin level; LOS length of hospital stay.
Fanning et al
Phase I/II prospective trial of autologous platelet tissue graft
637
postoperative malignant growth. We are also planning to evaluate autologous platelet tissue grafting as a drug delivery system. Finally, because we performed a phase I/II trail, there was no control group. Therefore we are presently performing a phase III prospective randomized controlled trial on autologous platelet tissue graft in cesarean sections.
References
1. Berghoff W, Pietrzak W, Rhodes R. Platelet-rich plasma application during closure following total knee arthroplasty: a retrospective study. Orthopedics. 2006;29:590 598. 2. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34:1774 1778. 3. Woodell-May J, Ridderman D, Swift M, Higgins J. Producing accurate platelet counts for platelet rich plasma: validation of a hematology analyzer and preparation techniques for counting. J Craniofacial Surg. 2005;16:749 756. 4. Eppley B, Woodell J, Higgins J. Platelet quantication and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg. 2004;114:15021508. 5. Devita V, Hellman S, Rosenberg S. Design and conduct of clinical trials. Cancer Principles & Practice of Oncology. 4th ed. Philadelphia, PA: J.B. Lippincott; 1993:418 440. 6. Fishman B, Pasternak S, Wallerstein S, Houde RW, Holland JC, Foley KM. The Memorial Pain Assessment Card: a valid instrument for the assessment of cancer pain. Cancer. 1987;60:11511158.
Conclusion
In the original phase I/II prospective trial of autologous platelet tissue graft in gynecologic surgery, there were no adverse effects, and pain was signicantly reduced. We are presently developing a phase III prospective placebo-controlled randomized trial to verify the results of our phase I/II trial, evaluate placebo effect and to evaluate the efcacy of autologous platelet tissue graft on surgical site infection and postoperative dehiscence.
You might also like
- Acog Practice Bulletin: Thromboembolism in PregnancyDocument17 pagesAcog Practice Bulletin: Thromboembolism in PregnancytriNo ratings yet
- Abortion KuliahDocument38 pagesAbortion KuliahElsa Hasibuan100% (1)
- Gyn & ObsDocument68 pagesGyn & ObsEsraa AlmassriNo ratings yet
- Pop, RevDocument139 pagesPop, RevYusof AndreiNo ratings yet
- Minimally Invasive Versus Abdominal Radical HysterectomyDocument10 pagesMinimally Invasive Versus Abdominal Radical HysterectomyClinton Franda Markus SitanggangNo ratings yet
- Dopplerinpregnancy 130823082426 Phpapp02Document64 pagesDopplerinpregnancy 130823082426 Phpapp02Herry SasukeNo ratings yet
- (Advanced Trauma Life Support) Moderator: Dr. Deepak S: Ganesh Kumar VIII TermDocument20 pages(Advanced Trauma Life Support) Moderator: Dr. Deepak S: Ganesh Kumar VIII Termabhaymalur100% (1)
- Management of Benign Breast Conditions: Part 2 - Breast Lumps and LesionsDocument3 pagesManagement of Benign Breast Conditions: Part 2 - Breast Lumps and Lesionspeter_mrNo ratings yet
- Vaginal Vault ProlapseDocument9 pagesVaginal Vault ProlapseOanaNo ratings yet
- Obs Sakshi Arora, E 9 ReducedDocument536 pagesObs Sakshi Arora, E 9 ReducedAman PareekNo ratings yet
- Difficulties in Vaginal HysterctomyDocument66 pagesDifficulties in Vaginal HysterctomyManamita NiphadkarNo ratings yet
- BronchosDocument17 pagesBronchosravigadaniNo ratings yet
- Evaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusDocument7 pagesEvaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusGabyliz Gonzalez CastilloNo ratings yet
- Toprank Review Pediatric Nursing NotesDocument12 pagesToprank Review Pediatric Nursing NotesCose online shopNo ratings yet
- PA Genitalia WanitaDocument100 pagesPA Genitalia WanitaBNo ratings yet
- Singer and Monaghan's Cervical and Lower Genital Tract Precancer: Diagnosis and TreatmentFrom EverandSinger and Monaghan's Cervical and Lower Genital Tract Precancer: Diagnosis and TreatmentRating: 5 out of 5 stars5/5 (1)
- Ambulatory HysterosDocument8 pagesAmbulatory Hysteroskomlanihou_890233161100% (1)
- Mullarian AnomoliesDocument85 pagesMullarian AnomoliesPrathibha GuruguriNo ratings yet
- C SectionDocument50 pagesC SectionAlano S. LimgasNo ratings yet
- The Ten-Step Vaginal Hysterectomy - A Newer and Better ApproachDocument8 pagesThe Ten-Step Vaginal Hysterectomy - A Newer and Better ApproachqisthiaufaNo ratings yet
- Libro Medicina Reproductiva 2022Document645 pagesLibro Medicina Reproductiva 2022Luisa Moreno100% (1)
- 2019 - Bowel and Bladder Injury Repair and Follow-Up After Gynecologic Surgery - 00006250-201902000-00012Document10 pages2019 - Bowel and Bladder Injury Repair and Follow-Up After Gynecologic Surgery - 00006250-201902000-00012Polyana FloresNo ratings yet
- Clarks Essential Guide To Clinical UltrasoundDocument77 pagesClarks Essential Guide To Clinical Ultrasoundrobertlinon0% (1)
- The Diagnosis and Management of The Acute Abdomen in Pregnancy-Greenspan, Peter, Springer Verlag (2017)Document284 pagesThe Diagnosis and Management of The Acute Abdomen in Pregnancy-Greenspan, Peter, Springer Verlag (2017)AndreaAlexandraNo ratings yet
- Basic Investigation of An Infertile CoupleDocument53 pagesBasic Investigation of An Infertile CoupleRemelou Garchitorena AlfelorNo ratings yet
- CPG - Management of Breast Cancer (2nd Edition)Document100 pagesCPG - Management of Breast Cancer (2nd Edition)umiraihana1No ratings yet
- The Management of Asherman Syndrome: A Review of LiteratureDocument11 pagesThe Management of Asherman Syndrome: A Review of LiteratureEuphra Adellheid100% (1)
- Healthcare StatisticsDocument20 pagesHealthcare StatisticsAnonymous ibmeej9No ratings yet
- Laparoscopic Gynecologist Surgeon in HSR Layout BangaloreDocument8 pagesLaparoscopic Gynecologist Surgeon in HSR Layout BangaloreDr.Beena JeysinghNo ratings yet
- WeBSurg Winners 42 1Document129 pagesWeBSurg Winners 42 1Ana Adam100% (1)
- TOG Vaginal HysterectomyDocument6 pagesTOG Vaginal HysterectomyYasmin AlkhatibNo ratings yet
- MRCOG Module SummaryDocument4 pagesMRCOG Module SummaryAmadeus KQNo ratings yet
- Training in Obstetrics and Gynaecology - Ippokratis SarrisDocument4 pagesTraining in Obstetrics and Gynaecology - Ippokratis Sarriszuxifoho0% (1)
- 62 Colposcopy StandardsDocument73 pages62 Colposcopy Standardsrijal mahdiy pNo ratings yet
- 8surgical Management of Dysfunctional Uterine Bleeding - KabilanDocument14 pages8surgical Management of Dysfunctional Uterine Bleeding - KabilanNavani TharanNo ratings yet
- 2015 Oncology CREOG Review PDFDocument76 pages2015 Oncology CREOG Review PDFRima HajjarNo ratings yet
- Ruptur OASISDocument41 pagesRuptur OASISHen DriNo ratings yet
- Acog Practice Bulletin Summary: Pregestational Diabetes MellitusDocument3 pagesAcog Practice Bulletin Summary: Pregestational Diabetes MellitusMaría Fernanda Palma AcostaNo ratings yet
- Handbook of Obstetric MedicineDocument15 pagesHandbook of Obstetric MedicineSara Zoi Lu50% (2)
- Craniofacial AbnormalitiesDocument12 pagesCraniofacial Abnormalitiesnpr00No ratings yet
- Dystocia and Augmentation of LAbor PDFDocument10 pagesDystocia and Augmentation of LAbor PDFKathleenNo ratings yet
- E-Poster Rcog 2018Document1 pageE-Poster Rcog 2018Ana MarianaNo ratings yet
- ACOG On CA EndometriumDocument14 pagesACOG On CA EndometriumzoviNo ratings yet
- E. Prior Phenotypically Normal Infant Delivered at 34 Weeks Due To Spontaneous Preterm LaborDocument10 pagesE. Prior Phenotypically Normal Infant Delivered at 34 Weeks Due To Spontaneous Preterm LaborSK ASIF ALINo ratings yet
- Tuberculosis in Obstetrics and GynecologyDocument42 pagesTuberculosis in Obstetrics and GynecologyameenNo ratings yet
- O&G - Abnormal PresentationDocument32 pagesO&G - Abnormal PresentationAnironOrionNo ratings yet
- Idea of OSCE in Obstetric.4012829.Powerpoint 1Document19 pagesIdea of OSCE in Obstetric.4012829.Powerpoint 1Aitzaz AhmedNo ratings yet
- 2023 OB/GYN Coding Manual: Components of Correct CodingFrom Everand2023 OB/GYN Coding Manual: Components of Correct CodingNo ratings yet
- Obstetrics and Gynecology Sixth Edition Obstetrics and Gynecology Beckman Chapter 36Document8 pagesObstetrics and Gynecology Sixth Edition Obstetrics and Gynecology Beckman Chapter 363hondoNo ratings yet
- Ultrasound - A GuideDocument9 pagesUltrasound - A GuideDebasish KunduNo ratings yet
- Pop QDocument45 pagesPop QObgyn Maret2016No ratings yet
- Ad en Om Yo SisDocument6 pagesAd en Om Yo SisMariaa EndahhNo ratings yet
- FIGO Clasificación HUA 2011Document11 pagesFIGO Clasificación HUA 2011dickenskevinNo ratings yet
- Presented by DR - Shahbaz Ahmad Professor of Community MedicineDocument76 pagesPresented by DR - Shahbaz Ahmad Professor of Community MedicinePriya bhattiNo ratings yet
- ACOG Practice Bulletin No 99 Management of 39 PDFDocument26 pagesACOG Practice Bulletin No 99 Management of 39 PDFhkdawnwongNo ratings yet
- Stats For CreogDocument1 pageStats For CreogzareeneyNo ratings yet
- 2022 Mendoza Eligibility CriteriaDocument21 pages2022 Mendoza Eligibility CriteriaТатьяна ТутченкоNo ratings yet
- IUGA Scoring SystemDocument40 pagesIUGA Scoring SystemBudi Iman SantosoNo ratings yet
- Treatment of Acute Endometritis. Medication and DosesDocument3 pagesTreatment of Acute Endometritis. Medication and DosesTitoun LettounNo ratings yet
- Creog Urogyn ReviewDocument97 pagesCreog Urogyn ReviewAlexandriah AlasNo ratings yet
- Abdul Malik Hassim Lecturer DMA Management & Science UniversityDocument21 pagesAbdul Malik Hassim Lecturer DMA Management & Science UniversitykimmgizelleNo ratings yet
- Fetal Medicine - Bidyut KumarDocument4 pagesFetal Medicine - Bidyut KumarpatoxyzuNo ratings yet
- Handbook of Current and Novel Protocols for the Treatment of InfertilityFrom EverandHandbook of Current and Novel Protocols for the Treatment of InfertilityMichael H. DahanNo ratings yet
- Clinical Impact and Biomaterial Evaluation of Platelet Gel in Cardiac Surgery Gunaydin 2008Document8 pagesClinical Impact and Biomaterial Evaluation of Platelet Gel in Cardiac Surgery Gunaydin 2008api-222634056No ratings yet
- Dhillon PRP Knee OsteoarthritisDocument9 pagesDhillon PRP Knee Osteoarthritisapi-222634056No ratings yet
- Orthopedic PRPDocument27 pagesOrthopedic PRPapi-222634056No ratings yet
- Tang - Antimicrobial Peptides From Human Platelets - 2002Document11 pagesTang - Antimicrobial Peptides From Human Platelets - 2002api-222634056No ratings yet
- J Orthopaedic Research Involvement of Platelets in StimulatDocument9 pagesJ Orthopaedic Research Involvement of Platelets in Stimulatapi-222634056No ratings yet
- Platelet Gel As An Intraoperative Procured Platelet Based AlDocument2 pagesPlatelet Gel As An Intraoperative Procured Platelet Based Alapi-222634056No ratings yet
- PRP For Dental Implants and Soft Tissue Grafting - GargDocument8 pagesPRP For Dental Implants and Soft Tissue Grafting - Gargapi-222634056No ratings yet
- Case Series - Use of PRP in Bariatric Surgery - BradyDocument4 pagesCase Series - Use of PRP in Bariatric Surgery - Bradyapi-222634056No ratings yet
- PRP in Coronary Artery Bypass Grafting-Effects On Surgical Wound Healing - VangDocument8 pagesPRP in Coronary Artery Bypass Grafting-Effects On Surgical Wound Healing - Vangapi-222634056No ratings yet
- Use of PRP in Cosmetic Surgery - ManDocument11 pagesUse of PRP in Cosmetic Surgery - Manapi-222634056No ratings yet
- PRP To Promote Healing in Abdominoplasty - JacksonDocument10 pagesPRP To Promote Healing in Abdominoplasty - Jacksonapi-222634056No ratings yet
- Ehancing Wound Healing With Growth Factors - AdlerDocument18 pagesEhancing Wound Healing With Growth Factors - Adlerapi-222634056No ratings yet
- PRP To Promote Healing in Abdominoplasty - JacksonDocument10 pagesPRP To Promote Healing in Abdominoplasty - Jacksonapi-222634056No ratings yet
- Pilot Study - Use of Platelet Gel To Treat Nonhelaing WoundDocument6 pagesPilot Study - Use of Platelet Gel To Treat Nonhelaing Woundapi-222634056No ratings yet
- Platelet Gel For Endoscopic Sinus Surgery - PomerantzDocument7 pagesPlatelet Gel For Endoscopic Sinus Surgery - Pomerantzapi-222634056No ratings yet
- Cost Effectiveness of PRP For Diabetic Foot Ulcers Dougherty 2008Document8 pagesCost Effectiveness of PRP For Diabetic Foot Ulcers Dougherty 2008api-222634056No ratings yet
- Use of PRP and Its Effects On Infection in Cardiac Surgery - StammersDocument6 pagesUse of PRP and Its Effects On Infection in Cardiac Surgery - Stammersapi-222634056No ratings yet
- Platelet Gel Final Protocol BWHDocument7 pagesPlatelet Gel Final Protocol BWHapi-222634056No ratings yet
- Osu Paper 120005Document2 pagesOsu Paper 120005api-222634056No ratings yet
- Efficacy of PRP in Pain Control and Blood Loss in Tka - GardnerDocument5 pagesEfficacy of PRP in Pain Control and Blood Loss in Tka - Gardnerapi-222634056No ratings yet
- Platelet Gel Final Protocol BWHDocument7 pagesPlatelet Gel Final Protocol BWHapi-222634056No ratings yet
- Laparoscopic SurgeryDocument4 pagesLaparoscopic SurgerycaioaccorsiNo ratings yet
- Phinma Cagayan de Oro CollegeDocument14 pagesPhinma Cagayan de Oro CollegeYasmin MagsaysayNo ratings yet
- Diagnosis and Managment of Gaynecologic CancersDocument1,067 pagesDiagnosis and Managment of Gaynecologic CancersarisNo ratings yet
- Lasers and Lights e Book Procedures in Cosmetic Dermatology Series 4th Edition Ebook PDFDocument58 pagesLasers and Lights e Book Procedures in Cosmetic Dermatology Series 4th Edition Ebook PDFlouis.starks790100% (46)
- Normal Tissue Tolerance Master 11-2016Document15 pagesNormal Tissue Tolerance Master 11-2016Virgilio Rafael Tovar VasquezNo ratings yet
- Evd Evd Evd Evd Accudrain Accudrain Accudrain Accudrain: External Ventricular DeviceDocument1 pageEvd Evd Evd Evd Accudrain Accudrain Accudrain Accudrain: External Ventricular DeviceQueenNo ratings yet
- A Global TextBook of Radiology IIDocument705 pagesA Global TextBook of Radiology IIannatabashidzeNo ratings yet
- BronchosDocument3 pagesBronchosNAENAENo ratings yet
- Renal FailureDocument60 pagesRenal Failuredr_shamimrNo ratings yet
- Label The Circulatory SystemDocument2 pagesLabel The Circulatory SystemIzzu PenielNo ratings yet
- Erich Arch Bar Versus Hanger Plate Technique For Intermaxillary Fixation in Fracture MandibleDocument6 pagesErich Arch Bar Versus Hanger Plate Technique For Intermaxillary Fixation in Fracture MandibleAndrés Faúndez TeránNo ratings yet
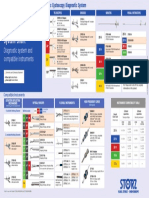
- Karl Storz Cystoscope System Chart: Diagnostic System and Compatible InstrumentsDocument1 pageKarl Storz Cystoscope System Chart: Diagnostic System and Compatible InstrumentsRaydoon SadeqNo ratings yet
- RicaDocument9 pagesRicarica mae narbaizNo ratings yet
- Ophthalmic Viscosurgical Devices: DR A Debata DrsrpatiDocument48 pagesOphthalmic Viscosurgical Devices: DR A Debata Drsrpatidrsrp84No ratings yet
- SCAI SHOCK Bedside Checklist 2022Document1 pageSCAI SHOCK Bedside Checklist 2022Katherine AzocarNo ratings yet
- Medical BookletDocument35 pagesMedical BookletNesanNo ratings yet
- An Ovarian Granulosa Cell Tumor in A Patient With Polycystic Ovarian Syndrome: A Case ReportDocument5 pagesAn Ovarian Granulosa Cell Tumor in A Patient With Polycystic Ovarian Syndrome: A Case ReportIJAR JOURNALNo ratings yet
- Knee Next Generation in Repair and Reconstruction 2022Document118 pagesKnee Next Generation in Repair and Reconstruction 2022Jose SantiagoNo ratings yet
- Epi Zone Articles 1Document8 pagesEpi Zone Articles 1kai xinNo ratings yet
- Preparation For Children and Their Families: Voiding Cystourethrogram (VCUG)Document2 pagesPreparation For Children and Their Families: Voiding Cystourethrogram (VCUG)NataliaMaedyNo ratings yet
- Wound Healing: Healing by First Intention (Primary Union)Document31 pagesWound Healing: Healing by First Intention (Primary Union)Muhammad Masoom AkhtarNo ratings yet
- PDD Instrument Set Brochure 001 V1-En 20000101Document16 pagesPDD Instrument Set Brochure 001 V1-En 20000101javixojdnNo ratings yet
- ANPH M3 CU11. Urinary SystemDocument13 pagesANPH M3 CU11. Urinary Systemmia LoremiaNo ratings yet
- CAOS Final ExamDocument34 pagesCAOS Final ExamNaimenur KorkmazNo ratings yet
- What Is A Retained Placenta?Document4 pagesWhat Is A Retained Placenta?Baharudin Yusuf Ramadhani0% (1)