Professional Documents
Culture Documents
Dexibuprofen PDF
Uploaded by
Ashok KpOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dexibuprofen PDF
Uploaded by
Ashok KpCopyright:
Available Formats
J Clin Periodontol 2005; 32: 617621 doi: 10.1111/j.1600-051X.2005.00721.
Copyright r Blackwell Munksgaard 2005
The effect of a dexibuprofen mouth rinse on experimental gingivitis in humans
hler ST, Hessler M, Schwahn Ch, Kuhr A, Kocher T. The effect of a Rosin M, Ka dexibuprofen mouth rinse on experimental gingivitis in humans. J Clin Periodontol 2005; 32: 617621. doi: 10.1111/j.1600-051X.2005.00721.x. r Blackwell Munksgaard, 2005. Abstract Objectives: The pharmacodynamic properties of ibuprofen are related nearly exclusively to the S(1)enantiomer (dexibuprofen). This study investigated the effect of a 1.5% dexibuprofen mouth rinse in an experimentally induced gingivitis. Materials and Methods: The trial was a randomized, double-blinded, placebocontrolled, two-period and two-sequence parallel group cross-over study in 24 healthy volunteers aged 2130 years (16 males, eight females). Customized guards were worn during tooth brushing to prevent any plaque removal from the experimental area (rst and second pre-molars and molars in one upper quadrant). After 22 days of plaque accumulation, the mouth rinses (1.5% dexibuprofen and placebo) were administered under supervision three times daily (rinsing for 1 min. with 15 ml) for 8 days. The wash-out time between the two study periods was 14 days. Parameters evaluated at e & Silness gingival index (GI) and the Quigley & days 0, 7, 14, 22, and 30 were the Lo Hein plaque index (QHI). Data were tested for treatment, period, and carry-over effects (parametric cross-over analysis). Results: There was no statistically signicant difference (p 5 0.240) in GI between placebo and dexibuprofen. However, the decrease in QHI was signicantly greater (p 5 0.019) with dexibuprofen as compared with the placebo. Conclusion: In the present study, a 1.5% dexibuprofen mouth rinse had no effect on gingivitis whereas an anti-plaque effect was demonstrated.
hler3, M. Rosin1,2, S. T. Ka M. Hessler4, Ch. Schwahn5, A. Kuhr5 and T. Kocher5
Department of Periodontology, Eastman Dental Institute, University College London, London, UK; 2Department of Operative Dentistry, Periodontology and Pediatric Dentistry, University of Greifswald, Germany; 3 Gebro Pharma GmbH, Fieberbrunn, Austria; 4 Army Dentist Group of the Bundeswehr, Neubrandenburg, Germany; 5Unit of Periodontology, Department of Operative Dentistry, Periodontology and Pediatric Dentistry, University of Greifswald, Germany
1
Key words: dexibuprofen; gingivitis; mouth rinse; plaque Accepted for publication 19 October 2004
There is substantial evidence to suggest that biochemical mediators of host origin, including prostaglandin E2 (PGE2), thromboxane B2 (TxB2), and leukotriene B4 (LTB4), may play a key role in the development and establishment of gingivitis (Goodson et al. 1974, Offenbacher et al. 1986, Heasman et al. 1993b). PGE2 has also been implicated as an inammatory mediator in periodontitis contributing to alveolar bone resorption (Williams 1990, Page 1991). Therefore, pharmaceutical control of these host inammatory mediators may possibly prevent or interfere with the initiation and/or progression of periodontal diseases in spite of the presence of periodontopathic microorganisms. In view of the problems with and limitations of patient performed mechanical plaque control (De LaRosa
et al. 1979), this specic use of pharmaceuticals may therefore have an adjunctive preventive and/or treatment effect (Paquette & Williams 2000). PGE2 and TxB2 are products of the cyclo-oxygenase (COX) pathway of arachidonic acid metabolism, which is inhibited by non-steroidal anti-inammatory drugs (NSAIDs) (Samuelsson 1969, Flower 1974). A wealth of data from pre-clinical and clinical studies indicates that systemic as well as topical administration of NSAIDs diminishes periodontal inammation and reduces alveolar bone resorption (Howell & Williams 1993, Salvi et al. 1997). Among these drugs with potential therapeutic value, urbiprofen (Jeffcoat et al. 1986, 1988, Offenbacher et al. 1987, Williams et al. 1987, 1988a, c, 1989,
Heasman et al. 1989, 1993a) appears to be the most tested agent, however, other members of the propionic acid class, naproxen (Howell et al. 1991, Jeffcoat et al. 1991) and ibuprofen (Williams et al. 1988b, Kornman et al. 1990) have also been studied. Ibuprofen is a NSAID with an arylpropionic structure and exists in two enantiomeric forms (Evans 1992). The drug actions of ibuprofen appear to be enantioselective and are nearly exclusively restricted to the dextrorotatory S(1)enantiomer, the so-called dexibuprofen (Evans 1996). It is now possible to isolate optically pure dexibuprofen and to make it available for therapeutic applications (Leising et al. 1996, Kaehler et al. 2003). Administration of the pure S(1)enantiomer, either systemi-
617
618
Rosin et al.
elsewhere in the mouth; no intra-oral appliances. In addition, subjects had not taken any medication, which could possibly affect the oral microora or oral health for at least 3 months prior to the study. The experimental area selected for this study comprised the rst and second pre-molars and molars in one quadrant of the maxilla. Localized plaque accumulation and hence localized experimental gingivitis were induced by means of plaque guards, which prevented plaque removal from the experimental teeth. Prior to the study, polyether impressions (Impregum Penta, ESPE, Seefeld, Germany) were taken of the experimental quadrant and stone casts poured. A wax relief (Thowax, Yeti Dental, Engen, Germany) was modelled on the stone casts, which covered approximately 2 mm of the gingival margins, approximately 3 mm of the adjacent tooth surfaces, and all proximal spaces of the experimental teeth. On duplicates of these models, moulded splints of 1 mm thick resin foil (Erkodur, Erkodent, Pfalzgrafenweiler, Germany) were fabricated. Extensions of these plaque guards over approximately 1 cm of the adjacent palate and vestibule as well as over half of the canine and the third molar (if present) provided support and permitted positive relocation. In the 2 weeks prior to the start of each study period, all participants were subjected to repeated professional maxillary tooth cleaning and instructed in good tooth-brushing techniques and the use of dental oss (Fig. 1). On day 0 of the induction period, all subjects were instructed to wear the plaque guards every time they cleaned their teeth, so that brushing and ossing were not performed on the rst and second premolars and molars of the test quadrant (Fig. 1). The induction phase lasted 22
X X 14 X X 22 X X 30 Repeated Professional prophylaxis X X 43
cally or topically, may reduce undesirable side effects not exposing the individual to the pharmacologically inactive enantiomeric ballast. Using pure S(1)enantiomer dexibuprofen, effectively doubles the dose when compared with the administration of racemic ibuprofen. With any pharmacological agent targeting solely periodontal diseases, there should be little doubt that a greater benet-to-risk ratio can be expected with topical rather than systemic application. The objective of the present study was to investigate the effect of locally applied dexibuprofen (a 1.5% dexibuprofen mouth rinse) on experimentally induced gingivitis.
Materials and Methods
Study design
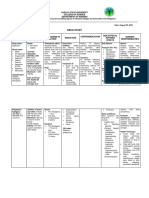
The study was performed as a doubleblind, randomized, placebo-controlled, cross-over design in a 4-week experimentally induced localized gingivitis model (Fig. 1). The wash-out period between the two plaque accumulation periods was 14 days. Approval for the study was obtained from the Ethics Committee of the Medical School of Greifswald University and volunteers gave written informed consent to participate. Twenty-four healthy subjects (16 males and eight females, between 21 and 30 years of age) were enrolled in the study. All subjects were students at Greifswald University, 22 of whom were dental students. Participants were selected based on the following criteria: at least one maxillary quadrant where the rst and second pre-molars and molars were free of restorations on palatal, buccal, and proximal surfaces; a high standard of oral hygiene and good gingival health, i.e. no probing depths 43 mm, no caries, and few restorations
Plaque index X Gingiva index X Day-14 Repeated Professional prophylaxis 0 X X 7
days. The rinse regimen began in the morning of day 23 and lasted 8 days by period. The subjects were allocated to use either the 1.5% dexibuprofen mouth rinse or the placebo according to a randomization list, which was produced using the validated software package Rancode professional, Version 3.6 (IDV Gauting, Munich, Germany). The mouth rinses were provided by Gebro Pharma GmbH (Fieberbrunn, Austria) and labelled to identify the subject and study period. Individual, sealed code breakers for the subjects and products were kept by the supervisor of the study (M. R.). The study preparations were administered in the morning, at midday, and in the evening (rinsing for 1 min. with 15 ml solution) under supervision of the investigator. Meals had to be taken before rinsing. Otherwise, intake of food and/or drinking was not allowed for 2 h after rinsing. Any sign or symptoms of adverse reactions of the oral mucosa and all other deteriorations of the health status of the study subjects were documented and analysed. At the end of each of the two trial periods, subjects received professional tooth cleaning to remove plaque, calculus, and staining from the test quadrant.
Clinical examinations
Localised experimental gingivitis Rinse Regimen 23 30
During each study period, clinical examinations were performed on days 0 (baseline), 7, 14, 22, and 30 (Fig. 1). Plaque was disclosed using a disclosing solution (MIRA-2-TON, Hager & Werken, Duisburg, Germany) and scored using the Turesky et al. (1970) modication of the Quigley & Hein (1962) plaque index system (QHI). The scores were taken at six surfaces of FDI teeth 4, 5, 6, and 7 of the test quadrant: distobuccal, buccal, mesiobuccal, distopalatal, palatal and mesiopalatal tooth surfaces. Gingival inammation was scored according to the Talbot et al. e & Sil(1977) modication of the Lo ness (1963) gingival index (GI). The GI was assessed at the same six sites of the selected teeth as the QHI using CP15UNC probes (HU-Friedy Europe, Leimen, Germany). The QHI and GI measurements were performed at each clinical examination.
Calibration of the clinical examiner
Fig. 1. Outline of the rst period of the clinical trial. Day 43 was the end of the wash-out period of the rst study period 1 and at the same time day 0 (baseline) of the second study period. The second study period was identical to days 030.
Screening and selection of volunteers was carried out by a single investigator (M. H.), who also scored all visits of the trial. Prior to the study, four calibration
Effect of dexibuprofen on gingivitis
sessions were performed to achieve high reproducibility of the QHI and GI scorings. An additional session was performed in the oral hygiene period preceding the second plaque accumulation period. The study investigator (M. H.) was calibrated against a very experienced investigator (T. K.). In the calibrating sessions, two patients were examined by a third clinician (M. R.) while the two investigators (M. H. and T. K.) scored independently. In the last calibration session before the start of the rst plaque accumulation period, an inter-examiner reproducibility of kX 0.81 and X0.76 was achieved for the QHI and GI, respectively. The respective values for the session prior to the second plaque accumulation period were kX0.79 for the QHI and kX0.77 for the GI.
Statistical analysis
619
Group placebo - verum GI Group verum - placebo 2.0
Group placebo - verum QHI Group verum - placebo 4.0
1.5
3.0
1.0
2.0
0.5
1.0
Inter-examiner reproducibility was determined by calculating k coefcients. The pairwise comparison of the clinical index values from all examination days with baseline was performed using ANOVA of repeated-measures data. The t-test was used for comparisons of the two treatments during the induction period. The GI and QHI data of the treatment phase were tested for difference using a parametric cross-over analysis (ANCOVA) with calculation of period, carry-over, and treatment effects (xed factor analysis) and adjustment by baseline values. Differences between test and reference were stated below the signicance level of 0.05.
Results
Compliance
0 0 7 14 22 0 7 14 22 Day in period 1 Day in period 2
e & Silness gingival index (GI) and Quigley & Hein plaque Fig. 2. Clinical parameters (Lo index (QHI)) during the induction phases of experimental gingivitis in the two study periods. Each box is characterized by the median as well as the 25th and 75th percentiles. The minimum and maximum values (without extreme cases) are indicated as whiskers.
Fig. 2. The increase of the GI and the QHI during the induction phase as compared with baseline was statistically signicant on all examination days (repeated-measures ANOVA, po0.01). The GI and QHI values for the respective dexibuprofen and placebo groups did not differ at any examination during the two induction periods (days 022).
Treatment regimen
for the QHI was observed for the pooled data of both study periods (p 5 0.019) and for the data of the rst study period only (p 5 0.034). No period or carry-over effects were observed for the QHI.
Adverse reactions
Twenty-one of the total of 24 subjects completed both periods of the clinical trial and were included in the analysis. One subject contracted tonsillitis shortly after the start of the study and had to withdraw. Two subjects had to be excluded from the study because of repeated failure to attend scheduled examination appointments. The observed pattern of plaque accumulation and gingivitis development in the remaining 21 subjects suggested a high degree of compliance with the study protocol (Fig. 2).
Induction of experimental gingivitis
The changes in the GI and QHI between days 0 and 22 (induction phase) of the experimental gingivitis are shown in
The examination on the last day of the induction phase (day 22) served as the baseline examination for the treatment regimen, which ended on day 30. The means and standard deviations for the GI and QHI before (day 22) and after the rinse regimen (day 30) are shown in Table 1. Parametric cross-over analysis revealed a signicant period effect for the GI (p 5 0.001). The same test was therefore used to analyse both the pooled data of both study periods and the data of just the rst study period. There was, however, no evidence of a signicant treatment effect for the GI with p 5 0.240 (both periods) and p 5 0.765 (rst period). Furthermore, no carry-over effect was observed for the GI. A statistically signicant treatment effect
No irritations of the oral mucosa were observed. Two adverse events, one tonsillitis (before the rst application of one of the test preparations) and one periimplantitis (affecting a central incisor), were documented and assessed as not related to either the test area or the test medications.
Discussion
The present study was undertaken to investigate the short-term effects of a 1.5% dexibuprofen mouth rinse on established gingival inammation in an experimental gingivitis model. Heasman et al. (1989), also utilizing an experimental gingivitis model, were barely able to demonstrate superiority of a topical 10 mM urbiprofen rinse (w/v concentration 0.24%) in a preventive application regimen (Heasman et al. 1989). Flurbiprofen was applied locally in 24 volunteers in a split-mouth model
620
Rosin et al.
Table 1. Mean ( SD) of GI and QHI during the treatment period (days 2230) in the dexibuprofen (Dex) and the placebo (Pla) group
GI Day 22 Dex Pla Dex Day 30 Pla Dex Day 22 Pla Dex QHI Day 30 Pla
First study period, 1.188 0.188 1.144 0.208 1.118 0.184 1.074 0.236 2.816 0.413 2.732 0.251 2.798 0.325 3.014 0.239 Dex n 5 12, Pla n 5 9 Second study period, 1.228 0.135 1.270 0.292 0.671 0.331 0.917 0.311 3.144 0.405 3.104 0.574 3.046 0.154 3.267 0.510 Dex n 5 9, Pla n 5 12 Both study periods, 1.205 0.164 1.216 0.262 0.927 0.337 0.984 0.286 2.956 0.433 2.945 0.492 2.905 0.289 3.159 0.427 n 5 21
Day 22, before commencing rinse regimen; day 30, after 8 days of rinse regimen.
on days 4, 6, 8, 11, 13, and 15 during a 17-day period of abstaining from tooth cleaning. In this study (Heasman et al. 1989), no differences were observed in GI scores between the urbiprofen and the placebo-treated side. However, in a follow-up study with six subjects from the original study population, when only the placebo was applied to one side, signicantly greater median GI values were found in their latter study as compared with their original investigation (Heasman et al. 1989). The authors concluded that systemic absorption of urbiprofen may have reduced the severity of the developing inammatory lesions in the original 17-day study period (Heasman et al. 1989). Using pure 1.5% S(1)enantiomer dexibuprofen we effectively doubled the dose as opposed to administration of racemic ibuprofen. We therefore hoped to demonstrate a clearer anti-inammatory effect than Heasman et al. (1989) using 0.24% urbiprofen. To avoid possible effects of systemically absorbed dexibuprofen, we used a cross-over design rather than a split-mouth design as in the study by Heasman et al. (1989). Therefore, the failure to demonstrate superiority of the dexibuprofen treatment over the placebo in the present study was somewhat unexpected. Our data, however, offer a possible explanation. The increase in inammation was more rapid and more pronounced in the second induction phase of our study (Fig. 2). Furthermore, the reduction of inammation in both the treatment and the placebo group were more pronounced in the second rinse phase (Table 1), leading to the observation of a signicant period effect. It is therefore possible, that the difference observed by Heasman et al. (1989) between the original and the follow-up study (both reported in Heasman et al. 1989) was caused by a similar period effect and not by a systemic effect of urbiprofen in
the original study. Nevertheless, the period effect strongly suggests that the 2-week wash-out period in our study was not sufcient and/or a cross-over design was not suitable. On the other hand, the observations and conclusions of Heasman et al. (1989) may be valid. The same group (Heasman et al. 1993c) established that urbiprofen, when applied systemically, was a potent inhibitor of gingival inammation with both preventive and therapeutic properties. Application of 50 mg b.i.d. urbiprofen between days 21 and 28 of an experimental gingivitis caused a signicant reduction in bleeding scores, while the control group demonstrated a highly signicant increase. Interestingly, this treatment effect appeared to be caused by a difference in the lipoxygenase product LTB4 as there was no difference between treatment and control in the COX products PGE2 and TxB2 (Heasman et al. 1993c). The possibility of this indirect NSAID effect having been less pronounced in our present study offers one explanation for the lack of an observed anti-inammatory effect. The effect of the splint in terms of accidental removal of plaque from the test teeth is not known. However, the QHI values for the respective dexibuprofen and placebo groups did not differ at any examination during the two induction periods (days 021). It may be assumed that any plaque-removing effects of the splints would have been similar in both study groups and that, therefore, the plaque reducing effect of ibuprofen was a valid observation. Furthermore, plaque values in the respective placebo groups increased during the investigational phase, resulting in a statistical difference between treatments. An in vivo plaque reducing effect of ibuprofen would be a novel nding and has not been reported before. However, our ndings are supported by a number of in vitro (Hersh et
al. 1991, Elvers & Wright 1995, PinaVaz et al. 2000) and in vivo (Hockertz et al. 1995, 1996) studies in which an antimicrobial effect of ibuprofen has been demonstrated. Hersh et al. (1991) observed an anti-bacterial effect for both urbiprofen and ibuprofen against Actinobacillus actinomycetemcomitans, Porphyromonas gingivalis, Prevotella intermedia, Fusobacterium nucleatum, Wollinella recta, and Eikenella corrodens at dosages of 125500 mg. In the study by Elvers & Wright (1995), growth of Staphylococcus aureus was suppressed by ibuprofen concentrations of 150 mg/ml at pH 7 with increased anti-bacterial potency of ibuprofen at lower pH values. Ibuprofen has also been shown to exhibit anti-fungal activity against Candida albicans and nonalbicans strains (Pina-Vaz et al. 2000). At 10 mg/ml, ibuprofen showed a rapid cidal activity while the effect at 5 mg/ml was mainly fungistatic. In view of these studies, an anti-plaque effect of our 1.5% dexibuprofen mouth rinse can be perceived as an anti-microbial effect of ibuprofen, which appears to be established at concentrations much lower than the ones applied in the present study (i.e. 15 mg/ml). Topical applications of NSAIDs, even if the effects are mostly caused by systemically absorbed drugs, will cause no gastrointestinal side effects. Plasma levels of urbiprofen in the study by Heasman et al. (1989) were 0.4 mg/ml and were comparable with those reported in adult monkeys (0.22 and 3.2 mg/ml), which signicantly inhibited gingival redness and bleeding on probing (Offenbacher et al. 1987). An additional plaque reducing effect would add further benet to a preventive and/or therapeutic regimen based on topical NSAID applications. This seems to justify further investigation into the effects of topical dexibuprofen using study designs different from the one employed here.
Effect of dexibuprofen on gingivitis
Acknowledgements
Howell, T. H., Jeffcoat, M.K, Goldhaber, P., Reddy, M. S., Kaplan, M. L., Johnson, H. G., Hall, C. M. & Williams, R. C. (1991) Inhibition of alveolar bone loss in beagles with the NSAID naproxen. Journal of Periodontal Research 26, 498501. Howell, T. H. & Williams, R. C. (1993) Nonsteroidal anti-inammatory drugs as inhibitors of periodontal disease progression. Critical Reviews in Oral Biology and Medicine 4, 177196. Jeffcoat, M. K., Page, R., Reddy, M., Wannawisute, A., Waite, P., Palcanis, K., Kogan, R., Williams, R. C. & Basch, C. (1991) Use of digital radiography to demonstrate the potential of naproxen as an adjunct in the treatment of progressive periodontitis. Journal of Periodontal Research 26, 415421. Jeffcoat, M. K., Williams, R., English, R. & Goldhaber, P. (1986) Flurbiprofen treatment of periodontal disease in beagles. Journal of Periodontal Research 21, 624633. Jeffcoat, M. K., Williams, R., English, R. & Goldhaber, P. (1988) Flurbiprofen treatment of human periodontitis: effect on alveolar bone height and metabolism. Journal of Periodontal Research 23, 381385. Kaehler, S. T., Phleps, W. & Hesse, E. (2003) Dexibuprofen: pharmacology, therapeutic uses and safety. Inammopharmacology 11, 371383. Kornman, K. S., Blodgett, R. F., Brunsvold, M. & Holt, S. C. (1990) Effects of topical applications of meclofenamic acid and ibuprofen on bone loss, subgingival microbiota and gingival PMN response in the primate Macaca fascicularis. Journal of Periodontal Research 25, 300307. Leising, G., Resel, R., Stelzer, F., Tasch, S., Lanziner, A. & Hantich, G. (1996) Physical aspects of dexibuprofen and racemic ibuprofen. Journal of Clinical Pharmacology 36, 36. e, H. & Silness, J. (1963) Periodontal disease Lo in pregnancy (I). Prevalence and severity. Acta Odontologica Scandinavica 21, 533551. Offenbacher, S., Braswell, L. D., Loos, A. S., Johnson, H. G., Hall, C. M., McClure, H., Orkin, J. L., Strobert, E. A., Green, M. D. & Odle, B. M. (1987) Effects of urbiprofen on the progression of periodontitis in Maccaca mulatta. Journal of Periodontal Research 22, 473481. Offenbacher, S., Odle, B. M. & Van Dyke, T. E. (1986) The use of crevicular uid prostaglandin E2 levels as predictor of periodontal attachment loss. Journal of Periodontal Research 21, 101112. Page, R. C. (1991) The role of inammatory mediators in the pathogenesis of periodontal disease. Journal of Periodontal Research 26, 230242. Paquette, D. W. & Williams, R. C. (2000) Modulation of host inammatory mediators as a treatment strategy for periodontal diseases. Periodontology 2000 24, 239252. Pina-Vaz, C., Sansonetty, F., Rodrigues, A. G., Martinez-De-Oliveira, J., Fonseca, A. F. &
621
The study was supported by Gebro Pharma GmbH (Fieberbrunn, Austria).
References
De LaRosa, M., Guerra, J. Z., Johnston, D. A. & Radicke, A. W. (1979) Plaque growth and removal with daily toothbrushing. Journal of Periodontology 50, 661664. Elvers, K. T. & Wright, S. J. (1995) Antibacterial activity of the anti-inammatory compound ibuprofen. Letters in Applied Microbiology 20, 8284. Evans, A. M. (1992) Enantioselective pharmacodynamics and pharmacokinetics of chiral non-steroidal anti-inammatory drugs. European Journal of Clinical Pharmacology 42, 237256. Evans, A. M. (1996) Pharmacodynamics and pharmacokinetics of the profens: enantioselectivity, clinical implications, and special reference to S(1)-ibuprofen. Journal of Clinical Pharmacology 36, 715. Flower, R. J. (1974) Drugs which inhibit prostaglandin synthesis. Pharmacological Reviews 26, 3367. Goodson, J. M., Dewhirst, F. E. & Brunetti, A. (1974) Prostaglandin E2 levels in human periodontal disease. Prostaglandins 6, 8185. Heasman, P. A., Benn, D. K., Kelly, P. J., Seymour, R. A. & Aitken, D. (1993a) The use of topical urbiprofen as an adjunct to non-surgical management of periodontal disease. Journal of Periodontal Research 28, 457464. Heasman, P. A., Collins, J. G. & Offenbacher, S. (1993b) Changes in crevicular uid levels of interleukin 1b, leukotriene B4, prostaglandin E2, thromboxane B2 and tumor necrosis factor alpha in experimental gingivitis in humans. Journal of Periodontal Research 28, 241247. Heasman, P. A., Offenbacher, S., Collins, J. G., Edwards, G. & Seymour, R. A. (1993c) Flurbiprofen in the prevention and treatment of experimental gingivitis. Journal of Clinical Periodontology 20, 732738. Heasman, P. A., Seymour, R. A. & Boston, P. F. (1989) The effect of a topical non-steroidal anti-inammatory drug on the development of experimental gingivitis in man. Journal of Clinical Periodontology 16, 353358. Hersh, E. V., Hammond, B. F. & Fleury, A. A. P. (1991) Antimicrobial activity of urbiprofen and ibuprofen in vitro against six common periodontal pathogens. Journal of Clinical Dentistry 3, 15. Hockertz, S. & Heckenberger, R. (1996) Treatment of an acute bacterial infection with a combination of acetylsalicylic acid/ibuprofen and interferon gamma. Arzneimittelforschung 46, 10121015. Hockertz, S., Heckenberger, R., Emmendorffer, A. & Muller, M. (1995) Inuence of ibuprofen on the infection with listeria monocytogenes. Arzneimittelforschung 45, 104107.
Mardh, P. A. (2000) Antifungal activity of ibuprofen alone and in combination with uconazole against Candida species. Journal of Medical Microbiology 49, 831840. Quigley, G. A. & Hein, J. W. (1962) Comparative cleansing efciency of manual and power brushing. Journal of American Dental Association 65, 2629. Salvi, G. E., Williams, R. C. & Offenbacher, S. (1997) Nonsteroidal antiinammatory drugs as adjuncts in the management of periodontal diseases and peri-implantitis. Current Opinions in Periodontology 4, 5158. Samuelsson, B. (1969) Biosynthesis of prostaglandins. Progress in Biochemical Pharmacology 5, 109128. Talbot, K., Mandel, I. & Chilton, N. W. (1977) Reduction of baseline gingivitis scores with repeated prophylaxis. Journal of Preventive Dentistry 4, 2829. Turesky, S., Gilmore, N. D. & Glickman, I. (1970) Reduced plaque formation by the chlormethyl analogue of vitamin C. Journal of Periodontology 41, 4143. Williams, R. C. (1990) Medical progress. Periodontal disease. New England Journal of Medicine 322, 373382. Williams, R. C., Jeffcoat, M. K., Howell, T. H., Hall, C. M., Johnson, H. G., Wechter, W. J. & Goldhaber, P. (1987) Indomethacin or urbiprofen treatment of periodontitis in beagles: comparison of effect on bone loss. Journal of Periodontal Research 22, 403407. Williams, R. C., Jeffcoat, M. K., Howell, T. H., Reddy, M. S., Johnson, H. G., Hall, C. M. & Goldhaber, P. (1988a) Topical urbiprofen treatment of periodontitis in beagles. Journal of Periodontal Research 23, 166169. Williams, R. C., Jeffcoat, M. K., Howell, T. H., Reddy, M. S., Johnson, H. G., Hall, C. M. & Goldhaber, P. (1988b) Ibuprofen: an inhibitor of alveolar bone resorption in beagles. Journal of Periodontal Research 23, 225229. Williams, R. C., Jeffcoat, M. K., Howell, T. H., Rolla, A., Stubbs, D., Teoh, K. W., Reddy, M. S. & Goldhaber, P. (1989) Altering the progression of human alveolar bone loss with the nonsteroidal anti-inammatory drug urbiprofen. Journal of Periodontal Research 60, 485490. Williams, R. C., Offenbacher, S., Jeffcoat, M. K., Howell, T. H., Johnson, H. G., Hall, C. M., Wechter, W. J. & Goldhaber, P. (1988c) Indomethacin or urbiprofen treatment of periodontitis in beagles: effect on crevicular uid arachidonic acid metabolites compared with effect on alveolar bone. Journal of Periodontal Research 23, 134138. Address: Michael Rosin Department of Operative Dentistry, Periodontology and Paediatric Dentistry School of Dentistry University of Greifswald Rotgerberstr. 8, D 17489 Greifswald Germany E-mail: rosin@uni-greifswald.de
You might also like
- Experimental Gingivitis in ManDocument11 pagesExperimental Gingivitis in ManCassia Martins PereiraNo ratings yet
- Osteoarthritis Case StudyDocument29 pagesOsteoarthritis Case StudyColeen Mae CamaristaNo ratings yet
- Anti-Gingivitis Effect of A Dentifrice Containing Bioactive Glass (Novamin) ParticulateDocument6 pagesAnti-Gingivitis Effect of A Dentifrice Containing Bioactive Glass (Novamin) ParticulateDyah Wulan RamadhaniNo ratings yet
- Management of Dry Mouth: Assessment of Oral Symptoms After Use of A Polysaccharide-Based Oral RinseDocument8 pagesManagement of Dry Mouth: Assessment of Oral Symptoms After Use of A Polysaccharide-Based Oral Rinseotoralla1591No ratings yet
- Aloe Vera VS CHXDocument6 pagesAloe Vera VS CHXMai ThúyNo ratings yet
- Effects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialDocument13 pagesEffects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialMohammed Falih HassanNo ratings yet
- NIH Public Access: Author ManuscriptDocument19 pagesNIH Public Access: Author ManuscriptJean PradoNo ratings yet
- Bahan JurnalDocument6 pagesBahan JurnalDwi ApriyantiNo ratings yet
- GJHS 8 211Document6 pagesGJHS 8 211Susi SimangunsongNo ratings yet
- The Effect of A 0,3% Triclosan Containing Dentrifice On The Microbial Composition of Supragingival PlaqueDocument9 pagesThe Effect of A 0,3% Triclosan Containing Dentrifice On The Microbial Composition of Supragingival PlaqueIndahIsmatulRahmataNo ratings yet
- Effect of Tongue Brushing On Oral Malodor in AdolescentsDocument5 pagesEffect of Tongue Brushing On Oral Malodor in AdolescentsMarian Si Teofana HasnaNo ratings yet
- Oral Care in Ventilation MechanicDocument8 pagesOral Care in Ventilation MechanicRusida LiyaniNo ratings yet
- Three MouthwashDocument12 pagesThree MouthwashrashmitanayakNo ratings yet
- Antihistamin in OMEDocument4 pagesAntihistamin in OMERahma NovitasariNo ratings yet
- Tic Treatment of Teeth With Apical Period On Tit Is Single vs. Multi Visit TreatmentDocument6 pagesTic Treatment of Teeth With Apical Period On Tit Is Single vs. Multi Visit Treatmentgpv38No ratings yet
- Population CellDocument9 pagesPopulation CellIana RusuNo ratings yet
- The Effect of Delmopinol Mouthwash On Aphthous StomatitisDocument19 pagesThe Effect of Delmopinol Mouthwash On Aphthous StomatitisAthenaeum Scientific PublishersNo ratings yet
- The Efficacy of Palatal Augmentation Prostheses For Speech and Swallowing in Patients Undergoing Glossectomy: A Review of The LiteratureDocument8 pagesThe Efficacy of Palatal Augmentation Prostheses For Speech and Swallowing in Patients Undergoing Glossectomy: A Review of The LiteraturemujtabaNo ratings yet
- Journal of Clinical PeriodontolDocument11 pagesJournal of Clinical PeriodontolIonut HusdupNo ratings yet
- BogrenDocument8 pagesBogrenballolsrNo ratings yet
- Quirinen EnglDocument7 pagesQuirinen EnglOctavian BoaruNo ratings yet
- Effectiveness of A New Toothbrush Design Versus A Conventional Tongue Scraper in Improving Breath Odor and Reducing Tongue MicrobiotaDocument4 pagesEffectiveness of A New Toothbrush Design Versus A Conventional Tongue Scraper in Improving Breath Odor and Reducing Tongue MicrobiotaEra GaluhNo ratings yet
- Free DocumentDocument8 pagesFree DocumentSuma_DewiNo ratings yet
- Al-Sharani (2019), THE EFFECT OF NANOSILVER AND CHLORHEXIDINE MOUTHWASH ON ANAEROBIC PERIODONTAL PATHOGENS COUNTSDocument6 pagesAl-Sharani (2019), THE EFFECT OF NANOSILVER AND CHLORHEXIDINE MOUTHWASH ON ANAEROBIC PERIODONTAL PATHOGENS COUNTSPhuong ThaoNo ratings yet
- Comparative Study of A Stabilized 0.1 %chlorine Dioxide With 0.2% Chlorhexidine Mouthrinse in Inhibiting The Formation of Volatile Sulphur Compounds (VSC)Document6 pagesComparative Study of A Stabilized 0.1 %chlorine Dioxide With 0.2% Chlorhexidine Mouthrinse in Inhibiting The Formation of Volatile Sulphur Compounds (VSC)KurniawanGamatyaNo ratings yet
- Journal of Functional FoodsDocument6 pagesJournal of Functional FoodsAnggita RizkaNo ratings yet
- Apjcp 2205 8094Document8 pagesApjcp 2205 8094SAGAR ADHIKARINo ratings yet
- 1 PBDocument6 pages1 PBfaizkanwarNo ratings yet
- Podj 4Document6 pagesPodj 4cutchaimahNo ratings yet
- Gingival Transcriptome Patterns During Induction and Resolution of Experimental Gingivitis in HumansDocument20 pagesGingival Transcriptome Patterns During Induction and Resolution of Experimental Gingivitis in HumansShuo NainiNo ratings yet
- Effectiveness OzoneDocument7 pagesEffectiveness OzoneSeptina Anggun PNo ratings yet
- High-Fluoride Toothpaste: A Multicenter Randomized Controlled Trial in AdultsDocument8 pagesHigh-Fluoride Toothpaste: A Multicenter Randomized Controlled Trial in Adultskalbani raisaNo ratings yet
- HalitoseDocument7 pagesHalitoseLavínia SoaresNo ratings yet
- Carranza's Clinical Periodontology 2002Document6 pagesCarranza's Clinical Periodontology 2002Lia Optimeze Alwayz100% (1)
- Oral Hygiene and Dietary Habits in Adolescents With Fixed OrthodonticDocument6 pagesOral Hygiene and Dietary Habits in Adolescents With Fixed OrthodonticNaliana LupascuNo ratings yet
- A Cytopathological Study of The Effect of Smoking On The Oral Epithelial Cells in Relation To Oral Health Status by The Micronucleus AssayDocument4 pagesA Cytopathological Study of The Effect of Smoking On The Oral Epithelial Cells in Relation To Oral Health Status by The Micronucleus AssayShirmayne TangNo ratings yet
- Clinical Evaluation of Halitosis Patients in KoreaDocument6 pagesClinical Evaluation of Halitosis Patients in KoreaBilly TrầnNo ratings yet
- The Effect of Fixed Orthodontic Appliances and Fluoride Mouthwash On The Oral Microbiome of Adolescents - A Randomized Controlled Clinical TrialDocument17 pagesThe Effect of Fixed Orthodontic Appliances and Fluoride Mouthwash On The Oral Microbiome of Adolescents - A Randomized Controlled Clinical Trialsurya saputraNo ratings yet
- PerioDocument6 pagesPeriohusenahNo ratings yet
- Asha Annie 2014Document4 pagesAsha Annie 2014Ratna Puspa RahayuNo ratings yet
- The Long-Term Effect of A Zinc Acetate and Chlorhexidine Diacetate Containing Mouth Rinse On Intra-Oral Halitosis-A Randomized Clinical TrialDocument35 pagesThe Long-Term Effect of A Zinc Acetate and Chlorhexidine Diacetate Containing Mouth Rinse On Intra-Oral Halitosis-A Randomized Clinical TrialPhuong ThaoNo ratings yet
- Appropriate Oral Hygiene Motivation Method For Patients With Fixed AppliancesDocument5 pagesAppropriate Oral Hygiene Motivation Method For Patients With Fixed AppliancesMelati WiraNo ratings yet
- Success Rate of Zinc Oxide Eugenol in Pulpectomy of Necrotic Primary Molars: A Retrospective StudyDocument7 pagesSuccess Rate of Zinc Oxide Eugenol in Pulpectomy of Necrotic Primary Molars: A Retrospective StudyAsriNo ratings yet
- Vol09 2 84-88strDocument5 pagesVol09 2 84-88strJoe Sam AbrahamNo ratings yet
- Charalambous2018 OkDocument9 pagesCharalambous2018 Okdayana nopridaNo ratings yet
- JIntClinDentResOrgan62103-2760784 074007Document4 pagesJIntClinDentResOrgan62103-2760784 074007daniel_siitompulNo ratings yet
- Recent Advancements in Management of Alveolar Osteitis (Dry Socket)Document5 pagesRecent Advancements in Management of Alveolar Osteitis (Dry Socket)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical Efficacy of Local Delivered Minocycline in The Treatment of Chronic Periodontitis Smoker PatientsDocument5 pagesClinical Efficacy of Local Delivered Minocycline in The Treatment of Chronic Periodontitis Smoker PatientsvivigaitanNo ratings yet
- Gingival Inflammation in Mouth Breathing PatientsDocument5 pagesGingival Inflammation in Mouth Breathing PatientsCamiLunaNo ratings yet
- Nascimento2014Document10 pagesNascimento2014Tiara IkaNo ratings yet
- Ijn 11 2641Document13 pagesIjn 11 2641gilangNo ratings yet
- Expert Guidance: Head and Neck Cancer DysphagiaDocument3 pagesExpert Guidance: Head and Neck Cancer DysphagiaSpeech & Language Therapy in PracticeNo ratings yet
- Incidence and Factors Associated With Flare-Ups in A Post Graduate Programme in The Indian PopulationDocument6 pagesIncidence and Factors Associated With Flare-Ups in A Post Graduate Programme in The Indian PopulationLeticia RiveraNo ratings yet
- JIAP October 2011 - The Influence of Restorations and Prosthetic Crowns Finishing Lines On Inflammatory Levels After Non-Surgical Periodontal TherapyDocument8 pagesJIAP October 2011 - The Influence of Restorations and Prosthetic Crowns Finishing Lines On Inflammatory Levels After Non-Surgical Periodontal TherapyMedstudNo ratings yet
- TurmericDocument4 pagesTurmericEllizabeth LilantiNo ratings yet
- Chen 2012Document8 pagesChen 2012Hamza GaaloulNo ratings yet
- Dehghan IDocument7 pagesDehghan IincisivusNo ratings yet
- Comparative Effect of Neemstick and Toothbrush On Plaque Removal and Gingival Health - A Clinical TrialDocument6 pagesComparative Effect of Neemstick and Toothbrush On Plaque Removal and Gingival Health - A Clinical TrialnavinlewisNo ratings yet
- Postlaryngectomy voice rehabilitation with voice prosthesesFrom EverandPostlaryngectomy voice rehabilitation with voice prosthesesNo ratings yet
- Inflammation and Oral Cancer: From Bench to BedsideFrom EverandInflammation and Oral Cancer: From Bench to BedsideHiroyuki TomitaNo ratings yet
- Osteomyelitis Classification Read PDFDocument33 pagesOsteomyelitis Classification Read PDFNavatha MorthaNo ratings yet
- Black TriangleDocument4 pagesBlack TriangleAshok KpNo ratings yet
- Role of Treponema in Periodontal DiseasesDocument16 pagesRole of Treponema in Periodontal DiseasesAshok KpNo ratings yet
- Ameloblastoma PathophysiologyDocument2 pagesAmeloblastoma PathophysiologyAshok KpNo ratings yet
- Factors Influencing The Outcome of Root-Resection Therapy in Molars: A 10-Year Retrospective StudyDocument9 pagesFactors Influencing The Outcome of Root-Resection Therapy in Molars: A 10-Year Retrospective StudyAshok KpNo ratings yet
- Infectious Aspects of Periodontal RegenerationDocument9 pagesInfectious Aspects of Periodontal RegenerationAshok KpNo ratings yet
- 23wasan FDocument4 pages23wasan FAshok KpNo ratings yet
- Anti Inflamatory Drugs AINSDocument39 pagesAnti Inflamatory Drugs AINSEl FaroukNo ratings yet
- Analgesic Drug MonitroringDocument14 pagesAnalgesic Drug MonitroringINDRANo ratings yet
- Balance Wheel Vs JuvenileDocument17 pagesBalance Wheel Vs JuvenileWiljohn de la CruzNo ratings yet
- Bp503t Pcol Unit-IIIDocument38 pagesBp503t Pcol Unit-IIIAakkkNo ratings yet
- Drug Lists 1 3Document6 pagesDrug Lists 1 3Paulene Marie SicatNo ratings yet
- Meniscal Injury 01 (1) .02.10Document64 pagesMeniscal Injury 01 (1) .02.10naren99No ratings yet
- Trade Name Generic Name Group: TetracyclinesDocument11 pagesTrade Name Generic Name Group: Tetracyclinesmisfer72No ratings yet
- Glucosamine SulfateDocument9 pagesGlucosamine Sulfateriga_ayuNo ratings yet
- OTC wv1Document42 pagesOTC wv1Sheena GagarinNo ratings yet
- Top 100 ListDocument124 pagesTop 100 Listtawhide_islamicNo ratings yet
- Naproxen Drug StudyDocument4 pagesNaproxen Drug StudyTimz GatdulaNo ratings yet
- Nsaids Nonsteroidal Anti-Inflammatory Drugs: Maher Khdour Msc. Phd. Clinical PharmacyDocument65 pagesNsaids Nonsteroidal Anti-Inflammatory Drugs: Maher Khdour Msc. Phd. Clinical PharmacyYousef JafarNo ratings yet
- Drugs Study and NCP For ACL Repair: By: Cristine PeradillaDocument6 pagesDrugs Study and NCP For ACL Repair: By: Cristine PeradillaJedeth Mara Gaba BalbastroNo ratings yet
- SerratiopeptidaseDocument4 pagesSerratiopeptidaseMo KhanNo ratings yet
- 6-Aspirin, NSAIDs, and COX-2 InhibitorsDocument2 pages6-Aspirin, NSAIDs, and COX-2 InhibitorsNgọc TrânNo ratings yet
- Nonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinDocument13 pagesNonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinMaBe MejíaNo ratings yet
- Product Monograph: ASPIRIN® Regular StrengthDocument44 pagesProduct Monograph: ASPIRIN® Regular StrengthMohammed shamiul ShahidNo ratings yet
- Drug Used in Orthopedic ConditionsDocument105 pagesDrug Used in Orthopedic ConditionsnavenNo ratings yet
- Cox 2 InhibitorsDocument9 pagesCox 2 InhibitorsirlandagarandaNo ratings yet
- Rheumatology Best of Five DONEDocument28 pagesRheumatology Best of Five DONEAlo'a NajjarNo ratings yet
- Health T Eaching PlanDocument17 pagesHealth T Eaching PlanChrezavelle MoonNo ratings yet
- GastritisDocument6 pagesGastritisNader Smadi100% (5)
- Naproxen-Eudragit Microspheres: Screening of Process and Formulation Variables For The Preparation of Extended Release TabletsDocument4 pagesNaproxen-Eudragit Microspheres: Screening of Process and Formulation Variables For The Preparation of Extended Release TabletsDebby NovriozaNo ratings yet
- Mims Doctor May 2017 My2Document60 pagesMims Doctor May 2017 My2Budak ComotNo ratings yet
- Drug Study: Tabije, Arvie Jayselle P. Marbella, IvyDocument15 pagesDrug Study: Tabije, Arvie Jayselle P. Marbella, IvyJaysellePuguonTabijeNo ratings yet
- Curcumae: Dosen Pengampu: Rohima Robby, S.PD., M.PDDocument14 pagesCurcumae: Dosen Pengampu: Rohima Robby, S.PD., M.PDRezkya HenantoNo ratings yet
- Side Effects of NSAIDsDocument8 pagesSide Effects of NSAIDsAlmas PrawotoNo ratings yet
- NCM 116 Notes FinalsDocument44 pagesNCM 116 Notes Finalsyra capiliNo ratings yet
- Pharm Review. Anticoagulant.Document56 pagesPharm Review. Anticoagulant.Ranger100% (1)