Professional Documents
Culture Documents
PEBC Print Examination Blueprint
Uploaded by
shamram2005Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PEBC Print Examination Blueprint
Uploaded by
shamram2005Copyright:
Available Formats
http://www.pebc.ca/index.php/ci_id/3074/la_id/1/print/true/art_i...
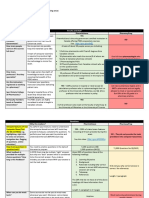
Examination Blueprint
The following competency statements1 summarize and outline the knowledge, skills and abilities that candidates are expected to have acquired before taking the Qualifying Examination and candidates are expected to demonstrate in answering the examination questions in Part I (MCQ) and completing the station tasks in Part II (OSCE). All of the Qualifying Examination questions and station tasks are linked to these competency statements. The proportion of each Part of the Qualifying Examination that focuses on the seven major competencies is shown, in the two columns on the left, as a percentage (%) of the total score for each Part. These percentages will indicate the relative importance of each competency in the overall score and pass-fail standard for each Part of the Qualifying Examination. The statements listed below each Competency2 provide additional detail regarding the competency. For more information on how the competencies relate to practice, refer to NAPRAs Model Standards of Practice for Canadian Pharmacists. (http://napra.ca/Content_Files/Files /Model_Standards_of_Prac_for_Cdn_Pharm_March09_Final_b.pdf)
1from Professional Competencies for Canadian Pharmacists at Entry to Practice (NAPRA, 2007) 2Significant job related knowledge, skills, abilities, attitudes, and/or judgments required for
competent performance by members of the profession. Parts I and II Overall % 38%
Part I (MCQ) 50.5%
Part II (OSCE) 26%
COMPETENCIES
Competency #1: Patient Care Pharmacists, in partnership with patients and other health care professionals, use their unique knowledge and skills to meet patients drug and health related needs and to achieve optimal patient outcomes and patient safety.
1.1 Develop a trusting professional relationship with the patient where both parties are interacting in a way where the obligations, expected benefits, and consequences are clearly defined. Establish and maintain rapport by using effective communication skills. Demonstrate a caring, empathetic, and professional attitude. Elicit the patients needs, values and desired level of care and desired outcomes regarding drug therapy.
1 of 7
13-04-08 10:12 AM
http://www.pebc.ca/index.php/ci_id/3074/la_id/1/print/true/art_i...
Assess the impact of factors that facilitate or impede the health of individual patients. Define mutual obligations, expected benefits, and consequences. . 1.2 Gather patient information. Identify and use appropriate sources of information (e.g., patient, laboratory data, chart, electronic health record, profile, other health care professionals, etc.) Actively listen and interpret the information provided (e.g., medical and social history, adverse drug reactions, allergies, medication use, etc.). Assess the relevance of the information. 1.3 Assess the health status and concerns of the patient. Use appropriate data, techniques and procedures to assess the patients health. Use knowledge base to comprehend the scope and breadth of the patients health problem. Identify factors (e.g., risk factors, financial, lifestyle, nutrition) that impact on the therapeutic outcome. 1.4 Identify the patients desired therapeutic outcomes. Integrate knowledge of the patients health status with knowledge of drug and non-drug treatment options. Outline the benefits and/or consequences of the treatment options. Enable the patient to make choices. 1.5 Identify and prioritize actual and potential drug therapy problems to determine if: The patient requires drug therapy but is not receiving it, The patient is taking or receiving the wrong drug, The patient is taking or receiving too little of the right drug, The patient is taking or receiving too much of the right drug, The patient is not taking or receiving the drug or is taking or receiving the drug inappropriately, The patient is experiencing an adverse reaction to the drug, The patient is experiencing a drug interaction (including drug-drug, drug-food, drug-laboratory test, drug-disease, or drug-blood product), The patient is taking or receiving a drug for no medically valid indication or substance abuse. 1.6 Develop a therapeutic plan. Identify and assess treatment strategies including drug and non-drug measures3 using an evidence-informed4 approach. Select therapeutic options. Recognize, solve and prevent actual and potential drug therapy problems. Consult with the patient and, if necessary, health care professionals. 1.7 Support the implementation of the therapeutic plan. Explain the rationale for the proposed treatment. Provide patient education (e.g., counseling information and education on adherence issues, either verbal or written). Assess patients understanding of the therapeutic plan. 1.8 Monitor the patients progress and assess therapeutic outcomes. Recognize the important clinical indicators (e.g., signs and symptoms, laboratory tests, adverse effects).
2 of 7
13-04-08 10:12 AM
http://www.pebc.ca/index.php/ci_id/3074/la_id/1/print/true/art_i...
Identify and apply monitoring/ intervention techniques and timelines. Specify outcomes with measurable therapeutic end points. Discuss with the patient the ongoing responsibilities of the pharmacist, patient and other health care professionals. Assess tolerance and safety of therapy. Assess adherence to therapy. Conduct follow-up consultation(s) to evaluate the therapeutic effectiveness. 1.9 Document and share within the circle of care5appropriate findings of patient information assessment, recommendations made and actions taken. Identify the purpose of the documentation. Maintain the patients health record. Document identified drug therapy problems. Prioritize and document the intervention, patients outcome, recommendations and follow-up. Document communication with patient and health care professionals.
3 4 5
Measures (in addition to drugs) that can be used to assist in the treatment of health conditions.
The conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients. Term of reference used to describe all members of the health care team who have direct responsibilities of providing care to an individual. Parts I and II Overall % 7%
Part I (MCQ) 4.5%
Part II (OSCE) 9.5%
COMPETENCIES
Competency #2: Professional Collaboration and Team Work Pharmacists work in collaboration with other health care professionals to optimize patient safety and improve health outcomes. 2.1 Develop collaborative6 relationships with health care professionals such that the obligations and expected benefits are clearly defined.
2.2 Cooperate with and show respect for all members of the interprofessional team. Make expertise available to others. Share relevant information. Contribute to defining objectives shared by all professions concerned. Support other professionals and accept their support to optimize health outcomes. 2.3 Refer patients to other health care providers when required. Determine if a referral is necessary. Identify the most appropriate health care provider or agency for the referral (e.g., medical or social). Work with other health care providers to determine the desired
3 of 7
13-04-08 10:12 AM
http://www.pebc.ca/index.php/ci_id/3074/la_id/1/print/true/art_i...
therapeutic outcome. 2.6 Understand, participate in and promote safety initiatives (e.g., medication safety, continuity of care).
A relationship between two or more health professionals that is developed to: facilitate communication; determine mutual goals of therapy that are acceptable to the patient; share relevant health information; establish the expectations of each participant. Parts I and II Overall % 10%
Part I (MCQ) 10%
Part II (OSCE) 9.5%
COMPETENCIES
Competency #3: Ethical, Legal and Professional Responsibilities Pharmacists practise within legal requirements, demonstrate professional integrity and act to uphold professional standards of practice and codes of ethics. 3.1 Apply legal and ethical requirements including federal and provincial/territorial legislation7, policies, by-laws and standards.
3.2 Uphold and act on the ethical principle that a pharmacists primary accountability is to the patient. Ensure patient confidentiality. Advocate on behalf of the patient. Involve the patient in decision-making. Respect the rights of the patient to make their own choices. Consider patient-specific circumstances. 3.3 Demonstrate personal and professional integrity. Accept responsibility for actions and decisions. Show respect for the dignity of the patient. Maintain appropriate professional boundaries. Practise within personal limits of knowledge, skills and abilities. 3.4 Demonstrate an understanding of the Canadian health care system and the role of the pharmacist and other health care professionals within it.
Provincial and territorial legislation are not tested in the PEBC Qualifying Examination. Federal legislation components that may be tested are those statutes, regulations and drug schedules pertaining to pharmacy practice, as listed in the Federal Leglislation section of Pharmaceutical References and Learning Resources. Parts I and II
Part I (MCQ)
Part II (OSCE)
COMPETENCIES
4 of 7
13-04-08 10:12 AM
http://www.pebc.ca/index.php/ci_id/3074/la_id/1/print/true/art_i...
Overall % 7% 5% Competency #4: Drug, Therapeutic and Practice Information Pharmacists assume responsibility for accessing, retrieving, evaluating and exchanging relevant information to ensure safe and effective patient care. 4.1 Clearly define the question(s) to be researched. Clarify requests for information. Identify key targets (audiences). 4.2 Identify appropriate sources of relevant information, using evidence-informed approaches where possible. Name major sources of information. Discuss the appropriateness of these sources. Assess the value of the sources. 4.3 Retrieve information from relevant sources. Use a variety of retrieval techniques to access relevant information. Assess the suitability and reliability of these techniques. 4.4 Evaluate scientific information. Assess the adequacy of research design (e.g., ethics, methodology, etc). Assess the relevance, applicability, accuracy, reliability, validity, and generalizability of information. 6%
Part I (MCQ) 2.5%
Part II (OSCE) 38%
COMPETENCIES
Parts I and II Overall % 20%
Competency #5: Communication and Education Pharmacists communicate with and provide education to groups and individuals in order to promote and support optimal patient care and well-being.
5.1 Demonstrate effective communication skills. Demonstrate comprehension and proficiency in written and verbal English or French. Demonstrate appropriate verbal, non-verbal and listening skills. Demonstrate effective interview techniques. Display clear, concise and effective writing skills. Select appropriate communication techniques for use with patients and other health care professionals
5 of 7
13-04-08 10:12 AM
http://www.pebc.ca/index.php/ci_id/3074/la_id/1/print/true/art_i...
5.2 Demonstrate sensitivity, respect and empathy when communicating with diverse groups or individuals. Demonstrate an understanding of the impact that individual differences have on communication. 5.3 Optimize individual and group health and wellness through education and health promotion. Use knowledge base to discuss health care issues and public health priorities. Identify factors that are barriers to, or facilitators of, health and wellness in individuals and groups. Collaborate with patients and other health care professionals in the development and implementation of health promotion strategies and public health initiatives.
Part I (MCQ) 22.5%
Part II (OSCE) 9.5%
COMPETENCIES
Parts I and II Overall % 16%
Competency #6: Drug Distribution Pharmacists manage the drug distribution system8 to ensure the safety, accuracy and quality of the supplied products.
6.1 Apply relevant knowledge in the performance of tasks related to: Interpretation of drug orders and/or prescriptions. Identification of bioequivalency and interchangeability of multi-source drugs. Performance of pharmaceutical calculations. Selection of quality products and ingredients. Demonstration of compounding and dispensing, including labelling. Preparation of sterile products. Identification of storage and handling conditions to ensure stability. Acquiring and disposing of drugs. Administration of drugs. Documentation. 6.2 Demonstrate ability to supervise drug distribution. Maintain safe and effective systems of drug supply and distribution. Adhere to distribution policies and procedures. Supervise support staff. 6.3 Participate in continuous quality assurance. Respond to actual or potential problems within the drug distribution system.
6 of 7
13-04-08 10:12 AM
http://www.pebc.ca/index.php/ci_id/3074/la_id/1/print/true/art_i...
Acknowledge the problem. Take steps to assess and resolve issues arising from the problem. Implement measures to prevent occurrences or recurrences. Document and report the problem and resolution. 6.4 Monitor drug distribution patterns. Recognize and respond to patterns of unusual drug distribution (e.g., diversion, drug misuse, fluctuations in utilization, etc.).
A system designed to facilitate the safe transfer of a medication from the manufacturer to the patient in a manner that preserves both the integrity of the medication and the safety of the patient. Steps in the drug distribution system include manufacturing, storage, procurement, dispensing, administration, and returns. Part I Part II (MCQ) (OSCE) 3% 2.5% COMPETENCIES Competency #7: Understanding Management Principles Pharmacists apply knowledge, principles and skills of management with the goal of optimizing patient care and interprofessional relationships. Parts I and II Overall % 3%
7.1 Supervise personnel such that delegated functions are carried out to meet accepted standards. Apply management principles and skills relevant to human and physical resources. Define accepted standards, policies and procedures. Demonstrate the principles of effective inter-professional and intraprofessional working relationships. 7.4 Interpret and apply the drug utilization, reimbursement and pharmaco-economic policies of health care facilities, agencies and third party payment plans9 (e.g., generic substitution, therapeutic interchange, use of formularies, co-payments, deductibles, prescription quantity limits, etc.).
Provincial issues are not tested in the PEBC Qualifying Examination.
Top of page
7 of 7
13-04-08 10:12 AM
You might also like
- Community Pharmacy: Basic Principles and ConceptsFrom EverandCommunity Pharmacy: Basic Principles and ConceptsRating: 3 out of 5 stars3/5 (2)
- Moving Forward Integration of IPGsDocument104 pagesMoving Forward Integration of IPGsSanghyeon Shawn LeeNo ratings yet
- Cardiovascular and Metabolic Syndrome MOCK Test: Pharmacy PREPDocument26 pagesCardiovascular and Metabolic Syndrome MOCK Test: Pharmacy PREPNOORNo ratings yet
- PEBC Evaluation Exam 2015Document1 pagePEBC Evaluation Exam 2015Youssef Emil Hanna0% (2)
- PEBC - Credentials Evaluation ProcedureDocument5 pagesPEBC - Credentials Evaluation ProcedureGaurav Rooprai100% (1)
- 2005 Evaluation QuestionsDocument51 pages2005 Evaluation QuestionsAnn100% (1)
- PEBC Qualifying Exam References and Resources ListDocument5 pagesPEBC Qualifying Exam References and Resources ListAnkit ShahNo ratings yet
- Psychiatric and Neurological Drugs Mock TestDocument45 pagesPsychiatric and Neurological Drugs Mock TestNOORNo ratings yet
- Evaluating QuestionsDocument200 pagesEvaluating QuestionsMuhammad MosliNo ratings yet
- ETHICS-CODEDocument46 pagesETHICS-CODEZara Arun100% (7)
- Part I - Sample Questions: Representative in Format and Phrasing Style of The Types of Questions Found in The QualifyingDocument16 pagesPart I - Sample Questions: Representative in Format and Phrasing Style of The Types of Questions Found in The Qualifyingitsshuvro100% (1)
- PEBC EnglishDocument4 pagesPEBC EnglishSaiKai54No ratings yet
- InmjDocument8 pagesInmjParth100% (2)
- Jan 2009 by "N": PharmacistDocument22 pagesJan 2009 by "N": PharmacistAsahota100% (1)
- Pharmaceutical Sciences: Pharmacy PrepDocument238 pagesPharmaceutical Sciences: Pharmacy Prepabob619100% (1)
- Pebc Evaluating Exam Sample QuestionDocument50 pagesPebc Evaluating Exam Sample QuestionZain zanzoonNo ratings yet
- PEBC Cards 1Document4 pagesPEBC Cards 1VatsalPatelNo ratings yet
- Pharmachieve Fact Sheet Pa Vs PP Pebc Osce ResourcesDocument6 pagesPharmachieve Fact Sheet Pa Vs PP Pebc Osce ResourcesSylvia Amaka0% (1)
- Evaluating Examination Information 2011Document86 pagesEvaluating Examination Information 2011Bhavesh Nidhi100% (1)
- Calculating Osmolarity and Milliosmoles from Percentage SolutionsDocument29 pagesCalculating Osmolarity and Milliosmoles from Percentage SolutionsP D SpencerNo ratings yet
- Medspan's Pharmacy Guide For OSCEDocument8 pagesMedspan's Pharmacy Guide For OSCEDeviselvamNo ratings yet
- Pharmacology MCQ PebcDocument36 pagesPharmacology MCQ Pebcsnowden1100% (6)
- MCQs on Biostatistics TrialsDocument1 pageMCQs on Biostatistics TrialsGeorge Zachariah100% (2)
- Pebc Who Passed - UnknownDocument10 pagesPebc Who Passed - UnknownDeviselvam100% (3)
- Xpharmacy Practice (1) XDocument6 pagesXpharmacy Practice (1) Xaboaasy100% (1)
- PEBC Evaluation SampleDocument1 pagePEBC Evaluation Samplesnowden1No ratings yet
- Q and A-PEBC-evaluating-exam-mustpass-Misbah-2016 PDFDocument437 pagesQ and A-PEBC-evaluating-exam-mustpass-Misbah-2016 PDFGaurav ahir pharmacy100% (1)
- Pharmacy CounsellingDocument8 pagesPharmacy CounsellingChrissieNo ratings yet
- Canada ExamDocument6 pagesCanada ExamKrizza MacayaNo ratings yet
- Requirment For All CountriesDocument3 pagesRequirment For All Countriesbaniyo100% (1)
- Pharmacy Management: Misbah Biabani, PH.DDocument3 pagesPharmacy Management: Misbah Biabani, PH.DGame MerNo ratings yet
- Analyzing OSCE PDFDocument15 pagesAnalyzing OSCE PDFWaleed Mostafa100% (1)
- Preview of Pharmacist OSCE Review BookDocument45 pagesPreview of Pharmacist OSCE Review BookChrissie100% (3)
- Canada ExamDocument6 pagesCanada Examshirazwarraich50% (2)
- Guidelines Minimum Standard Pharmacies HospitalsDocument11 pagesGuidelines Minimum Standard Pharmacies HospitalsEngyKamalNo ratings yet
- Pebc CompilationDocument14 pagesPebc CompilationAarti AroraNo ratings yet
- Drug Info+Document56 pagesDrug Info+zaidhusam100% (1)
- PEBC Test 1 CONCEPTS OF FITNESS W/ ANSWERSDocument13 pagesPEBC Test 1 CONCEPTS OF FITNESS W/ ANSWERSSarah C. Snooks100% (4)
- Mock TestDocument20 pagesMock Testironcahir61100% (1)
- Glucose: Carbohydrate Is Stored in The Body Principally AsDocument21 pagesGlucose: Carbohydrate Is Stored in The Body Principally Asironcahir61100% (2)
- MOCK TEST REVIEWDocument92 pagesMOCK TEST REVIEWMohit Koladia100% (2)
- Minor AilmentsDocument37 pagesMinor AilmentsNiamh Mone100% (3)
- Laws PebcDocument2 pagesLaws PebcAqsa Adnan100% (2)
- 001 Chapter Qualifying Pharmacy Review Content 2010 Ver1Document7 pages001 Chapter Qualifying Pharmacy Review Content 2010 Ver1Dr-Usman KhanNo ratings yet
- Ontario Jurisprudence Exam Notes - Ontario Drug Benefit Act (2/2)Document4 pagesOntario Jurisprudence Exam Notes - Ontario Drug Benefit Act (2/2)Herodotus100% (5)
- PHARMACY MCQ Quiz 1Document18 pagesPHARMACY MCQ Quiz 1Noah MrjNo ratings yet
- Pharmacist Licensing Process in CanadaDocument2 pagesPharmacist Licensing Process in CanadaUrugonda VenumadhavNo ratings yet
- OTC antifungals and medications for pregnancyDocument8 pagesOTC antifungals and medications for pregnancyNoah Mrj70% (10)
- North American Pharmacist Licensure Examination (NAPLEX) Study GuideDocument20 pagesNorth American Pharmacist Licensure Examination (NAPLEX) Study GuideMcRee Learning CenterNo ratings yet
- Pharmacy QuestionsDocument28 pagesPharmacy QuestionsKeziah Gill100% (1)
- Biomedical Sciences Content 2014Document3 pagesBiomedical Sciences Content 2014Bhavesh Nidhi0% (2)
- Compendium of Pharmaceuticals and Specialties PDFDocument2 pagesCompendium of Pharmaceuticals and Specialties PDFJainner Contreras100% (1)
- Here are the answers to the questions:1. a2. b 3. c4. d5. a6. b7. a8. c 9. a10. b11. c12. a13. c14. d15. a16. c17. b18. a19. c20. a21. b22. c23. a 24. d25. b26. cDocument29 pagesHere are the answers to the questions:1. a2. b 3. c4. d5. a6. b7. a8. c 9. a10. b11. c12. a13. c14. d15. a16. c17. b18. a19. c20. a21. b22. c23. a 24. d25. b26. cDr-Usman Khan100% (9)
- FOREIGN PHARMACY GRADUATES EQUIVALENCY EXAMINATION (FPGEE): Passbooks Study GuideFrom EverandFOREIGN PHARMACY GRADUATES EQUIVALENCY EXAMINATION (FPGEE): Passbooks Study GuideNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- NAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)From EverandNAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)Rating: 4.5 out of 5 stars4.5/5 (3)
- Fundamentals of Clinical Pharmacy PracticeFrom EverandFundamentals of Clinical Pharmacy PracticeRating: 4.5 out of 5 stars4.5/5 (2)
- Jurnal Skizofrenia PDFDocument10 pagesJurnal Skizofrenia PDFYayan Zan DoollNo ratings yet
- Project Proper TB CareDocument37 pagesProject Proper TB CareM LubisNo ratings yet
- Office of Director General of Civil Aviation: Government of India Technical Centre, Opp Safdarjang Airport, New DelhiDocument4 pagesOffice of Director General of Civil Aviation: Government of India Technical Centre, Opp Safdarjang Airport, New DelhiPraveen KumarNo ratings yet
- Assessment Centers - Lecture 6Document55 pagesAssessment Centers - Lecture 6krisdaryadi4014No ratings yet
- Yaman Walid KassabDocument282 pagesYaman Walid KassabHeryanti PusparisaNo ratings yet
- Plenary 5 - Louie MalixiDocument46 pagesPlenary 5 - Louie MalixiAsian Development Bank ConferencesNo ratings yet
- 366-Article Text-1258-1-10-20220824Document7 pages366-Article Text-1258-1-10-20220824YunitafazaksNo ratings yet
- Adherence To Supportive Periodontal TreatmentDocument10 pagesAdherence To Supportive Periodontal TreatmentFabian SanabriaNo ratings yet
- Family Psychoeducation PsychosisDocument3 pagesFamily Psychoeducation PsychosisCharlesNo ratings yet
- 10 Chaney Et Al 2004 A New Asthma Spacer Device To Improve ComplianceDocument8 pages10 Chaney Et Al 2004 A New Asthma Spacer Device To Improve ComplianceFrancis Gladstone-QuintupletNo ratings yet
- What Does Good Regulatory: Decision Making Look Like?Document10 pagesWhat Does Good Regulatory: Decision Making Look Like?Sonal KaliaNo ratings yet
- SMHS HIPAA Compliance Quiz ResultsDocument3 pagesSMHS HIPAA Compliance Quiz Resultslexi_2706No ratings yet
- PT Safty JDocument6 pagesPT Safty JMyo Min HtunNo ratings yet
- The Role of Minimally Invasive Glaucoma Surgery.12Document8 pagesThe Role of Minimally Invasive Glaucoma Surgery.12georginaNo ratings yet
- 8098 28638 1 SM PDFDocument88 pages8098 28638 1 SM PDFDilukshi WickramasingheNo ratings yet
- Effect of Whatsapp Reminder On Antenatal Care RevisitDocument11 pagesEffect of Whatsapp Reminder On Antenatal Care RevisitElita NapiaNo ratings yet
- Aaa - THAMARA - Comparing Hot Pack, Short-Wave Diathermy, Ultrasound, and Tens On Isokinetic Strength, Pain and Functional StatusDocument9 pagesAaa - THAMARA - Comparing Hot Pack, Short-Wave Diathermy, Ultrasound, and Tens On Isokinetic Strength, Pain and Functional StatusBruno FellipeNo ratings yet
- The Effects of Self-Management Education Tailored To Health Literacy OnDocument7 pagesThe Effects of Self-Management Education Tailored To Health Literacy OnDINDA PUTRI SAVIRANo ratings yet
- Nejmc 070603Document3 pagesNejmc 070603Redentor MagdayaoNo ratings yet
- Board Certified Nurse Practitioner in Savannah GA Resume Michele StephensDocument4 pagesBoard Certified Nurse Practitioner in Savannah GA Resume Michele StephensMicheleStephens100% (1)
- Amanda Cravinho Resume FinalDocument2 pagesAmanda Cravinho Resume Finalapi-301376054No ratings yet
- Telehealth Delivery of Memory Rehabilitation Following StrokDocument14 pagesTelehealth Delivery of Memory Rehabilitation Following StrokMica Ballito de TroyaNo ratings yet
- Payer Brochure 03222021Document2 pagesPayer Brochure 03222021Dan JecanNo ratings yet
- Nursing Assistant Resume SampleDocument9 pagesNursing Assistant Resume Samplef5b2q8e3100% (2)
- Tingkat Kepatuhan Minum Obat HipertensiDocument6 pagesTingkat Kepatuhan Minum Obat HipertensiNinin KepoNo ratings yet
- Xpharmacy Practice (1) XDocument6 pagesXpharmacy Practice (1) Xaboaasy100% (1)
- Eportfolio Mental Health Case StudyDocument12 pagesEportfolio Mental Health Case Studyapi-663116972No ratings yet
- MALAYSIAN RESEARCH ON DIABETES MELLITUSDocument39 pagesMALAYSIAN RESEARCH ON DIABETES MELLITUSChe HaniffNo ratings yet
- Impact of Multimodal Intervention Strategies On Compliance To Hand Hygiene Practices Among Staff Nurses in Obstetric and Gynaecological WardsDocument1 pageImpact of Multimodal Intervention Strategies On Compliance To Hand Hygiene Practices Among Staff Nurses in Obstetric and Gynaecological WardsALYSSA MARIE MATANo ratings yet
- Ais YesDocument15 pagesAis YesLauriz Dillumas MachonNo ratings yet