Professional Documents
Culture Documents
Appropriate Use of Blood Components: Clinical Practice Guidelines
Uploaded by
Estefani BlancoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Appropriate Use of Blood Components: Clinical Practice Guidelines
Uploaded by
Estefani BlancoCopyright:
Available Formats
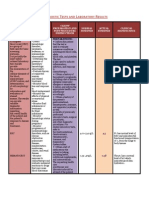
CLINICAL PRACTICE GUIDELINES Appropriate Use of Blood Components
Use of blood components for clinical or laboratory indications not listed here is likely to be inappropriate. Consult the NHMRC/ASBT guidelines (www.nhmrc.gov.au) for further details. Clinical and laboratory indications for use should be documented.
Red blood cells
Hb* <70g/L Considerations
Lower thresholds may be acceptable in patients without symptoms and/or where specific therapy is available. 70-100g/L Likely to be appropriate during surgery associated with major blood loss or if there are signs or symptoms of impaired oxygen transport. >80g/L May be appropriate to control anaemia-related symptoms in a patient on a chronic transfusion regimen or during marrow suppresive therapy. >100g/L Not likely to be appropriate unless there are specific indications.
* Hb should not be the sole deciding factor. Consider also patient factors, signs and symptoms of hypoxia, ongoing blood loss and the risk to the patient of anaemia.
Platelets Use of platelets is likely to be appropriate as prophylaxis:
Indication
Bone marrow failure
Considerations At a platelet count of <10x109/L in the absence of risk factors and <20x109/L in the presence of risk factors (eg fever, antibiotics, evidence of systemic haemostatic failure).
Surgery/ To maintain platelet count at >50x109/L. For surgical procedures invasive with high risk of bleeding (eg ocular or neurosurgery) it may be procedure appropriate to maintain at 100x109/L. Platelet function disorders
May be appropriate in inherited or acquired disorders, depending on clinical features and setting. In this situation, platelet count is not a reliable indicator.
Platelets Use of platelets is likely to be appropriate as therapy:
Indication
Bleeding Massive haemorrhage/ transfusion
Considerations May be appropriate in any patient in whom thrombocytopenia is considered a major contributory factor. Use should be confined to patients with thrombocytopenia and/or functional abnormalities who have significant bleeding from this cause. May be appropriate when the platelet count is <50x109/L (<100x109/L in the presence of diffuse microvascular bleeding).
Fresh frozen plasma Use of fresh frozen plasma is likely to be appropriate:
Indication
Single factor deficiencies Warfin effect Acute DIC TTP Coagulation inhibitor deficiencies
Considerations Use specific factors if available. In the presence of life-threatening bleeding. Use in addition to vitamin-K-dependent concentrates. Indicated where there is bleeding and abnormal coagulation. Not indicated for chronic DIC. Accepted treatment. May be appropriate in patients undergoing high-risk procedures. Use specific factors if available.
Following massive May be appropriate in the presence of bleeding and abnormal coagulation. transfusion or cardiac bypass Liver disease
May be appropriate in the presence of bleeding and abnormal coagulation.
Cryoprecipitate Use of cryoprecipitate is likely to be appropriate:
Indication
Fibrinogen deficiency
Considerations May be appropriate where there is clinical bleeding, an invasive procedure, trauma or DIC.
Abbreviations: Hb = haemoglobin; DIC = disseminated intravascular coagulation; TTP = thrombotic thrombocytopenic purpura.
ISBN 1864960590 October 2001
You might also like
- INDICATION CODES FOR TRANSFUSION: AN AUDIT TOOLDocument3 pagesINDICATION CODES FOR TRANSFUSION: AN AUDIT TOOLtomreneyoNo ratings yet
- Blood Transfusion: Risks and BenefitsDocument31 pagesBlood Transfusion: Risks and Benefitsfenti nurul khafifahNo ratings yet
- Transfusion Guidelines HemDocument4 pagesTransfusion Guidelines HemnandhinisankaranNo ratings yet
- Clinical Indications For Platelets: Key MessagesDocument4 pagesClinical Indications For Platelets: Key MessagesKristian WilsonNo ratings yet
- Blood Transfusion.Document23 pagesBlood Transfusion.Madalina TalpauNo ratings yet
- 9 Transfusion Guidelines 2006Document6 pages9 Transfusion Guidelines 2006Melania OanaNo ratings yet
- PBM (Autosaved)Document36 pagesPBM (Autosaved)dr AmitNo ratings yet
- CRRT Therapy GuidelinesDocument5 pagesCRRT Therapy Guidelinesanon_361066654100% (1)
- 7: Effective Transfusion in Surgery and Critical CareDocument16 pages7: Effective Transfusion in Surgery and Critical CareNick-Hugh Sean WisdomNo ratings yet
- Upper GI BleedDocument8 pagesUpper GI BleedbbyesNo ratings yet
- 2013 BloodUsageCardDocument4 pages2013 BloodUsageCardtonnywongsoNo ratings yet
- Critical Care CoagulopathiesDocument20 pagesCritical Care CoagulopathiesKarina Mega WNo ratings yet
- HGF Covid-19Document4 pagesHGF Covid-19Chon ChiNo ratings yet
- Managing Coagulopathy ICUDocument38 pagesManaging Coagulopathy ICUMirabela Colac100% (1)
- Blood ProductsDocument2 pagesBlood ProductstechnoelfyNo ratings yet
- Blood ConservationDocument21 pagesBlood ConservationfraolNo ratings yet
- Blood Transfusion SeminarDocument58 pagesBlood Transfusion SeminarsharewdelelegnNo ratings yet
- Blood Transfusion Notes For StudentsDocument5 pagesBlood Transfusion Notes For StudentsMegan TurnerNo ratings yet
- Anaesthesia - 2018 - Mu OzDocument14 pagesAnaesthesia - 2018 - Mu OzCarp TheodorNo ratings yet
- Transfusion in Specfic SituationsDocument42 pagesTransfusion in Specfic SituationsAhmed EshraNo ratings yet
- Practice Guidelines For Perioperative Blood Management An Updated Report by The American Society of Anesthesiologists Task Force OnDocument13 pagesPractice Guidelines For Perioperative Blood Management An Updated Report by The American Society of Anesthesiologists Task Force OnMadalina TalpauNo ratings yet
- Hemorrhage DisordersDocument18 pagesHemorrhage DisordersTyreqe UsifNo ratings yet
- Use of Blood Products in The Critically IllDocument25 pagesUse of Blood Products in The Critically IllAna María Díaz MedinaNo ratings yet
- Blood Transfusion in Hemorrhagic ShockDocument28 pagesBlood Transfusion in Hemorrhagic Shocklas100% (2)
- Use of Blood Products in The Critically Ill - UpToDateDocument13 pagesUse of Blood Products in The Critically Ill - UpToDateOscar F RojasNo ratings yet
- Final DX ResultsDocument9 pagesFinal DX ResultszysheaiNo ratings yet
- Blood Product Transfusion in Adults: Indications, Adverse Reactions, and ModificationsDocument9 pagesBlood Product Transfusion in Adults: Indications, Adverse Reactions, and ModificationsYeseniaNo ratings yet
- Case Presentation DVTDocument26 pagesCase Presentation DVTimad mokalledNo ratings yet
- Autologous Transfusion Strategies to Reduce Allogeneic Blood UseDocument31 pagesAutologous Transfusion Strategies to Reduce Allogeneic Blood Usethalida24100% (1)
- Blood Transfusion TherapyDocument1 pageBlood Transfusion TherapyGabriela Cerón GarcíaNo ratings yet
- Heparin Sodium Injection, USP: RX Only DescriptionDocument29 pagesHeparin Sodium Injection, USP: RX Only DescriptionArchie TobiasNo ratings yet
- Blood Components Dosage and Their Administration (Compatibility Mode)Document7 pagesBlood Components Dosage and Their Administration (Compatibility Mode)Chandra SekarNo ratings yet
- Transfusión IntraoperatoriaDocument24 pagesTransfusión IntraoperatoriaGiovany Salinas100% (1)
- WHO Blood Transfusion Safety GuidelinesDocument104 pagesWHO Blood Transfusion Safety GuidelinesrodelagapitoNo ratings yet
- Cytosorb Ebp IfuDocument16 pagesCytosorb Ebp IfuMuhammad Mahbøøb SadiqNo ratings yet
- Bleeding and TransfusionDocument32 pagesBleeding and TransfusionWalid KuncoroNo ratings yet
- Tumor Lysis Syndrome Guidelines 2014Document13 pagesTumor Lysis Syndrome Guidelines 2014Dinesh KamalNo ratings yet
- 11 Peri Operative CareDocument43 pages11 Peri Operative CareAdnan MaqboolNo ratings yet
- Blood TransfusionDocument57 pagesBlood Transfusionibzshan_No ratings yet
- 4.massive HemorrhageDocument44 pages4.massive HemorrhageyeabsraNo ratings yet
- A Concise Guide to ITP Treatment and ManagementDocument16 pagesA Concise Guide to ITP Treatment and ManagementFein MalricNo ratings yet
- St Mary's Adult Blood Transfusion Policy Medical StaffDocument15 pagesSt Mary's Adult Blood Transfusion Policy Medical StaffStanislaus JosephNo ratings yet
- Blood Components - DR. ETU-EFEOTOR T. P.Document40 pagesBlood Components - DR. ETU-EFEOTOR T. P.Princewill Seiyefa100% (1)
- Addison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresDocument12 pagesAddison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresAlvaro HaroNo ratings yet
- BldbnkguidelinesDocument14 pagesBldbnkguidelinesShoka SamyNo ratings yet
- Principles of Transfusion in Liver DiseasesDocument38 pagesPrinciples of Transfusion in Liver DiseasesNallagondla ThulasiramNo ratings yet
- Board Review HematologyDocument30 pagesBoard Review HematologyPPDS Geriatri IPD UANo ratings yet
- Blood Administration: NRS 108 Essec County CollegeDocument22 pagesBlood Administration: NRS 108 Essec County CollegeDiah Puspita RiniNo ratings yet
- Massive Transfusion Protocol 2017Document9 pagesMassive Transfusion Protocol 2017RosNo ratings yet
- Blood Transfusion Guidelines for NICU BabiesDocument8 pagesBlood Transfusion Guidelines for NICU BabiesanuNo ratings yet
- Aspects-Of-Platelet-Transfusion-Therapy?Sectionname Antiplatelet Agents&Anchor H262 0781574&source See - Link#H323107Document4 pagesAspects-Of-Platelet-Transfusion-Therapy?Sectionname Antiplatelet Agents&Anchor H262 0781574&source See - Link#H323107Huy LeNo ratings yet
- Blood Component TherapyDocument73 pagesBlood Component TherapySaikat Prasad DattaNo ratings yet
- Blood TransfusionDocument58 pagesBlood Transfusionmsat72100% (12)
- Blood ProductsDocument70 pagesBlood Productsjadhamade339No ratings yet
- Rami Dwairi, MD: Internal Medicine, HSDocument22 pagesRami Dwairi, MD: Internal Medicine, HSraed faisalNo ratings yet
- Guidelines for Blood TransfusionDocument40 pagesGuidelines for Blood TransfusionSakti WNo ratings yet
- Hypertension ESC Guideline 2018Document78 pagesHypertension ESC Guideline 2018Theresia KennyNo ratings yet
- Hemostatic Strategies For Minimizing Mortality in Major Blood LossDocument26 pagesHemostatic Strategies For Minimizing Mortality in Major Blood LossJonathan wiradinataNo ratings yet
- Fluid & Blood Therapy Key ConceptsDocument31 pagesFluid & Blood Therapy Key ConceptsMohammad Pino HakimNo ratings yet
- Clinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2From EverandClinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2No ratings yet
- A Final Project For The Course Title "Monetary Policy and Central Banking"Document11 pagesA Final Project For The Course Title "Monetary Policy and Central Banking"Elle SanchezNo ratings yet
- Compliance Risks and Controls: Speaker: Dott. Fabio AccardiDocument14 pagesCompliance Risks and Controls: Speaker: Dott. Fabio AccardiJefferson WidodoNo ratings yet
- Rozgar Sutra EnglishDocument105 pagesRozgar Sutra EnglishRisingsun PradhanNo ratings yet
- Aluminium FOil SearchDocument8 pagesAluminium FOil SearchAtul KumarNo ratings yet
- TD EGGER Eurospan E1E05 TSCA Hydro P3 (Rec 224) enDocument2 pagesTD EGGER Eurospan E1E05 TSCA Hydro P3 (Rec 224) enClarencegiNo ratings yet
- Cross-Sectional Tomography: Oral and Maxillofacial RadiologyDocument7 pagesCross-Sectional Tomography: Oral and Maxillofacial RadiologyPhanQuangHuyNo ratings yet
- Ted Hughes's Crow - An Alternative Theological ParadigmDocument16 pagesTed Hughes's Crow - An Alternative Theological Paradigmsa46851No ratings yet
- Linear Circuit Analysis (ELEN-1100) : Lecture # 13: More On Mesh Current AnalysisDocument11 pagesLinear Circuit Analysis (ELEN-1100) : Lecture # 13: More On Mesh Current AnalysisPhD EENo ratings yet
- Organized Educator Seeks New OpportunityDocument1 pageOrganized Educator Seeks New OpportunityCaren Pogoy ManiquezNo ratings yet
- Hics 203-Organization Assignment ListDocument2 pagesHics 203-Organization Assignment ListslusafNo ratings yet
- Schedule For Semester III, Class of 2021Document7 pagesSchedule For Semester III, Class of 2021Jay PatelNo ratings yet
- Mod. 34 Classic Compact T06Document4 pagesMod. 34 Classic Compact T06Jaime Li AliNo ratings yet
- 1989 Volvo 740 Instruments and ControlsDocument107 pages1989 Volvo 740 Instruments and Controlsskyliner538No ratings yet
- Express VPN Activation CodeDocument5 pagesExpress VPN Activation CodeButler49JuulNo ratings yet
- Fees Structure For Government Sponsored (KUCCPS) Students: University of Eastern Africa, BaratonDocument3 pagesFees Structure For Government Sponsored (KUCCPS) Students: University of Eastern Africa, BaratonGiddy LerionkaNo ratings yet
- The English Center Articulation AgreementDocument9 pagesThe English Center Articulation AgreementJose CabreraNo ratings yet
- Chapter - 2 Fish MongeryDocument10 pagesChapter - 2 Fish MongeryKrishna ChaudharyNo ratings yet
- Dxgbvi Abdor Rahim OsmanmrDocument1 pageDxgbvi Abdor Rahim OsmanmrSakhipur TravelsNo ratings yet
- CSIR AnalysisDocument1 pageCSIR Analysisசெபா செல்வாNo ratings yet
- Iso 16399-2014-05Document52 pagesIso 16399-2014-05nadim100% (1)
- Subtracting-Fractions-Unlike DenominatorsDocument2 pagesSubtracting-Fractions-Unlike Denominatorsapi-3953531900% (1)
- 10 Compactness in Function Spaces: Ascoli-Arzel A TheoremDocument5 pages10 Compactness in Function Spaces: Ascoli-Arzel A TheoremronalduckNo ratings yet
- Name: Chakshu Purohit Course: BBA LLB Subject: Legal Research and Methodology Submitted To: Utkarsh MishraDocument5 pagesName: Chakshu Purohit Course: BBA LLB Subject: Legal Research and Methodology Submitted To: Utkarsh Mishrachakshu purohitNo ratings yet
- Nortek Quick Guide: - To Vectrino ProfilerDocument4 pagesNortek Quick Guide: - To Vectrino ProfilerAndresFelipePrietoAlarconNo ratings yet
- Froyen06-The Keynesian System I - The Role of Aggregate DemandDocument40 pagesFroyen06-The Keynesian System I - The Role of Aggregate DemandUditi BiswasNo ratings yet
- Communication Networks Chapter 1 SolutionsDocument10 pagesCommunication Networks Chapter 1 SolutionsJ PrakashNo ratings yet
- Blocked threads jstack analysisDocument69 pagesBlocked threads jstack analysisMike TNo ratings yet
- As 91435Document3 pagesAs 91435api-271057641No ratings yet
- Cambridge IGCSE: Computer Science 0478/12Document16 pagesCambridge IGCSE: Computer Science 0478/12Rodolph Smith100% (2)
- Vortex: Opencl Compatible Risc-V Gpgpu: Fares Elsabbagh Blaise Tine Priyadarshini Roshan Ethan Lyons Euna KimDocument7 pagesVortex: Opencl Compatible Risc-V Gpgpu: Fares Elsabbagh Blaise Tine Priyadarshini Roshan Ethan Lyons Euna KimhiraNo ratings yet