Professional Documents
Culture Documents
Nephrology Chronic Renal Failure
Uploaded by
M PatelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nephrology Chronic Renal Failure
Uploaded by
M PatelCopyright:
Available Formats
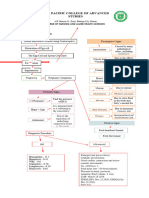
CKD/CRF
-DEFN: o *CKD is defined as EITHER: kidney damage decreased function (decreased GFR) for 3 or more months -kidney disease can be dx w/out knowledge of its cause -kidney damage is usually ascertained by MARKERS: o -rather than by kidney biopsy -MARKERS of kidney damage: o *PROTEINURIA -persistent proteinuria is the PRINCIPAL MARKER of kidney damage -an albumin/creatinine RATIO greater than 30 mg/g in SPOT urine samples is usually: *considered ABNORMAL o *other markers include: -urine sediment -abnormalities in BLOOD and URINE chemistry -abnormal findings on imaging studies o *persons w/: -normal GFR- BUT w/ MARKERS of kidney damage are: *at INCREASED RISK for adverse outcomes of CKD -CRF implies: *PERMANENT damage to the kidney -the normal architecture is gradually REPLACED by SCAR TISSUE -the HALLMARK of RENAL FAILURE is: *ELEVATION of the CREATININE and BUN concs in the extra-cellular fluid caused by: -a FALL in the GFR *other fns of the kidney are also impaired, such as: -SYNTHESIS of renal HORMONES *a wide range of sxs accompany the various degrees of renal failure -several TERMS are used to describe chronic renal injury:
*CRF: -is the general term used to describe IRREVERSIBLE loss of GFR over a prolonged period of time- usually YEARS *CHRONIC RENAL INSUFFICIENCY: -implies MILD CRF *AZOTEMIA: -refers to an ELEVATION in the BUN and CREATININE levels, and DOES NOT imply:*any sxs OR overt clinical manifestations of kidney disease -azotemia occurs w/ BOTH chronic and acute renal failure *UREMIA: -is the SYMPTOMATIC phase of renal failure during which: *sxs and signs of renal dysfn are DETECTED -for many individuals- uremic manifestations do NOT appear UNTIL: *the GFR is LESS than 10 ml/min (normal 120 ml/min) *END-STAGE RENAL DISEASE (ESRD): -refers to any form of CHRONIC (ieIRREVERSIBLE) renal failure at a stage that: *PERMANENT renal replacement therapy is indicated in the form of:-dialysis/transplant *NORMAL renal architecture is LOST and: -REPLACED w/ COLLAGEN -as this occurs: *the SIZE of the KIDNEYS generally DECREASES
* HYPER-FILTRATION HYPOTHESIS: ***a popular explanation for the PROGRESSIVE
NATURE of CRF is termed: -the HYPER-FILTRATION HYPOTHESIS: *this hypothesis states that- the INTACT nephrons are EVENTUALLY INJURED by: -the increased plasma flow AND hydrostatic pressure *healthy remnant nephrons sustain damage as a result of: -LONG-TERM exposure to: *INCREASED capillary PRESSURE and FLOW *hyper-filtration injury leads to a CHARACTERISTIC glomerular injury pattern known as:
-FOCAL GLOMERULAR SCLEROSIS *this hypothesis explains why renal failure CONTINUES to progress even when: -the initial renal insult is self-limited *acidosis *eg- some forms of glomerulonephritis *Na retention/water overload *HYPER-FILTRATION INJURY can be DIMINISHED by: *CHF/edema -REDUCING glomerular HYDROSTATIC PRESSURE *hyperkalemia -several methods of lowering glomerular pressure have been tried in an attempt to: *slow or halt the progression of CRF *hypertension, *anemia/hyperlipidemia *renal osteodystrophy -Co-morbs: *CV Disease /vasculardisease/malnutrx/neuroretinopathy/change drug handling/dehydraxn *ESRD COMPLICATIONS
(low protein diet (= hyperfiltraxn injury)= RBF and Pgc
*INCREASED SNGFR (ie- HYPER-filtration) occurs by: DILATATION of AFFERENT glomerular arterioles, resulting in:enhanced single-nephron PLASMA FLOW filtration may also be enhanced by: *INCREASED EFFERENT arteriolar TONE
DIET: protein ( Pgc)/ K (cuz hyperkalemia-arrythmias)/ Na (vol overloadedema and CHF)/ water if (hyponatremia)/P (hyperP- soft tissue deposits/osteodystrophy)
-Drugs: CRF CLINICAL SX -GFR<10 - SUMMARY: FINDINGS IN CRF: HTN (ACE inhibor-eff art dilaxn) EDEMA (diuretics=Na/h20 excrexn)
-in pts w/ NEPHROTIC SYNDROME (give diuretics) 1. Ca/Vit D-calcitrol (hypoCa, hyperPTH) /serum proteins/ EPO/Hb (anemia) P(soft tissue calcifixn)/K (hyperkalemia)/Renin (= Ang 2= BP/vol)/proteinuria *edema may also develop b/c of a: -LOW SERUM ALBUMIN conc *albumin is the SOURCE of ONCOTIC PRESSURE that determines: -the amt of FLUID HELD in the vascular compartment
2.
-PREVENT RENAL OSTEO (low P, give Ca/calcitrol)
Specific CRF Sx details -*SODIUM RETENTION (Na excrexn) results in: -EXPANSION of the extra-cellular space, which is manifest as: 1. EDEMA 2. HYPER-TENSION require: a sodium-RESTRICTED DIET *HYPERKALEMIA restrict K+ intake -(arrhythmias/Gut K+ secrexn) *CHANGE DRUG DOSAGE IN CRF PTS: -its necessary to: *REDUCE the DOSE -or- EXTEND the dosing INTERVAL of drugs that are: -EXCRETED by the KIDNEYS -drugs that are REMOVED by the KIDNEYS include: *aminoglycosides/vancomycin/PCN/allopurinol/digo -in CONTRAST- LIVER drugs dont req adjustment: *ACID-BASE: METABOLIC ACIDOSIS (RETAIN ammonia) bone buffers w/Ca rel-> bone Dx) (retain P -> anion gap acidosis) *erythromycin/phenytoin/anticoags/narcotics *CNS (uremic toxin accumulation leads to lower seizure threshold) -Asterixis: involuntary hand jerking -> seizures *BONE DISEASE: RENAL OSTEODYSTROPHY *RENAL OSTEODYSTROPHY summary: ___________________________________________ DECREASED vitamin D HYPO-calcemia AND DECREASED excretion of PO4HYPER-phosphatemia -subtle ECG changes -peripheral sensory neuropathy *CARDIOVASC -dyslipidemia/-stroke -the ability to ELIMINATE a SALT LOAD may become COMPROMISED is some pts w/ CRF, leading to: *EXPANSION of the extra-cellular VOLUME -EDEMA formation: CHF + pulm edema -w/ ADVANCED renal failure- pts may develop an: DECREASED vitamin D AND HYPER PTH *ACUTE PERICARDITIS (infl./hemmor): (uremic toxins in pericardial space) -Sx: chest pain/SOB/pericardial frixn rub/TAMPONADE (hypoTN)
___________________________________________
(osteitis fibrosa cystica/osteomalacia-antacid) HYPO-calcemia ___________________________________________ Secretion of PTH RENAL OSTEODYSTROPHY
*METABOLIC/ENDOCRINE: *glucose intolerance AND insulin resistance*hyperlipidemia/DECREASED levels of testosterone AND estrogen (fertility)
ACUTE RENAL FAILURE
GFR/ Cr+BUN (cuz urea reab=prerenal-low flow) (Cuz Cr secreted so Cr= UT obstruxn/hydronephrosis) SAME-ratio can be same if both Cr/BUN inc *THREE CAUSES OF ARF: 1. PRE-RENAL *ie- functional *generalized or local *DECREASE in RBF and/or Pgc *ARF DEFIXN --acute renal failure is a common clinical syndrome -its DEFINED as: *increase of 0.5 mg/dL from baseline occuring over days (< 1 month) of: -the BUN or CREATININE *OR- 50% DECLINE in calculated GFR *its easy to miss the early changes -the clinical manifestations of this d/o arise from the: *DECLINE in GFR *and the INABILITY of the KIDNEY to EXCRETE toxic wastes produced by the body -its recognized clinically by: *RISING levels of BUN and CREATININE *and usually a REDUCED URINE OUTPUT -most forms are REVERSIBLE processes -most physicians accept the definition of acute renal failure as a: *RISE in plasma CREATININE of 0.5 mg/day *and- a RISE in BUN of 10 mg/dl/day *over several days (crystals/BPH) *occurs DISTAL to the cd (Dx: oliguria -> anuria -> BUN/Cr is over 20:1 Suprapubic//flank pain Urinalysis: hematuria +uric acid crystals (urea/Cr ratio > 1) or normal (if BPH) 3. POST-RENAL *ie- obstructive *obstruction in the urinary tract -BUN/Cr = 20:1 *occurs BEFORE the GLOMERULUS (Esp if have: poor tissue perfusion= hypoTN/ dehydraxn/hemorrhage/edema due to CHF or nephrotic or cirrhosis) 2. INTRA-RENAL *ie- structural *intrinsic renal disease leading to: -DAMAGED NEPHRONS -KIDNEYS ENLARGED (-> GFR + Cr +BUN)
Urinalysis: hematuria +uric acid crystals (urea/Cr ratio > 1) or normal (if BPH)
*DIAGNOSIS OF PRERENAL AZOTEMIA:
*DIAGNOSIS: IMAGING: -in pts w/ VOLUME DEPLETION/DEHYDRATION: * DX of obstruction depends on radiography: * history of vomiting diarrhea, or diuretic use Ultrasonography *physical exam may reveal: -poor skin turgor -orthostatic hypo-tension -tachycardia -conversely- pts w/ RELATIVE DECLINES in EFFECTIVE ARTERIAL BV from : *CHF , nephrotic syndrome, or cirrhosis *may show: -peripheral edema OR ascites URINALYSIS UNREMARKABLE, except for -urinalysis becomes ABNORMAL -increased # of hyaline and granular casts + less Na -tubular fn DIMINISHES (Cuz kidney NOT intrinsically diseased) -signs of UREMIA develop -Response to poor perfusion in ARF: -Na reab (SNS/aldo) (=less Na in urine) - H20 reab (ADH) -BUN/Cr = 20:1 (cuz -Na reab -> coupled urea reab -> BUN) PRERENAL AZOTEMIA -Causes: ATN (85%)/ AIN (allergy/eosinos)/Acute GN (RPGN) -Intrarenal SX: -GFR (intrarenal vasoconstrixn -> RPF + O2 to outer medulla/PST/TAL -Segmental patches of NECROTIC lesions *DIAGNOSIS OF POSTRENAL AZOTEMIA: -OBSTRUCTIVE (DISTAL TO CD) revible (Causes: intrarenal crystals, renal pelvis or ureter caliculi, or BPH or neoplasia/ chemoTx leads to acute urea nephropathy ( lysed cells -> urea -> uric acid crystals -> ARF!) -Dx: oliguria -> anuria -> BUN/Cr is over 20:1 -> REDUCE renal EXCRETORY FN: Suprapubic//flank pain -URINALYSIS: Casts: -made up of CELLULAR DEBRIS from injured or necrotic renal tubule cells are freq found in the DISTAL NEPHRON, where they: *IMPEDE the FLOW of URINE *the necrotic cells SHED into the tubular LUMEN: *DIAGNOSIS OF INTRARENAL ARF (#1): --BUN/Creatinine BOTH RISE and: *ratio NORMALIZES -IVP (b/c of the decline in renal fn- the IVP vis ualization of the collecting system in obstruction may not occur until 6-24 hrs after dye administration -CT scanning -or- retrograde pyelography
*not only by- OBSTRUCTING urine flow BUT -BACK-LEAK OF GLOMERULAR FILTRAXN=leave gaps along the tubular epithelia thru which glomerular filtrate can RE-ENTER the circulation, a process called: BACK-LEAK OF GLOMERULAR FILTRATE
-CT Scans and angiograms deliver the most toxic dyes to pt 4. Endo-geneous Toxins myoglobin, hemoglobin, and myeloma light chains
TOXIC SX: kidneys ENLARGED (PCT) TYPES OF INTRARENAL ARF: -MICROSCOPIC: *focal (patchy lesions) *proximal tubule NECROSIS and APOPTOSIS *ATN -ISCHEMIC (#1) (HYPOTXN -> STRUCL DAMAGE) OR TOXIC -*CAUSES of ischemic insult include: -hemorrhage -hypo-tension (cardiac sepsis) -often occurs in the presence of: *NSAIDs, and ACE inhibitors -these are ALL the causes that give rise to: *PRE-RENAL AZOTEMIA (high ratio, but tubules look normal)*BUT- the nephron cannot tolerate this state long SO: -condition EVOLVES from pre-renal to: INTRARENAL *CAUSES OF TOXIC ATN: 1. Antibiotics Aminoglycoside/ amphotericin B/cyclosporine: (used to prevent graft -vs- host disease in transplants) 2. Heavy Metals -cis-platin- dose-dependent -salts of mercury, arsenic, bismuth, silver, chromium 3. Radio-contrast Agents -this form of nephrotoxic ATN can present w/ an FENa o fLESS than 1% ISCHEMIC SX -EOSINOPHILIC HYALINE CASTS as well as PIGMENTED GRANULAR CASTS are common, esp in the: *distal tubules and- collecting ducts -these CASTS consist of:*TAMM-HALL PROTEIN -a specific urinary glycoprotein normally secreted by the cells of ascending thick limb and distal tubules *in conjunction w/ Hb/Mg. -other findings in ischemic ATN are: *interstitial edema *and- accumulations of leukocytes w/in dilated vasa recta *DISTAL CASTS: -hyaline-and- PIGMENTED HALLMARK of ATN *sloughed tubular epithelial cells -they're RBCs (pigmented)
*LABORATORY TESTS: -the URINE SEDIMENT in the EARLY phase of ATN usually contains: *renal tubular epithelial cells/ granular and epithelial cell casts -b/c TUBULAR FN is IMPAIRED: *the kidney's ability to conserve Na and maximally concentratethe urine is diminished -in pts whose AZOTEMIA is SECONDARY to PRERENAL CAUSES: *the urinary indices usually show: -urinary osmolality GREATER than 500 mOsm/kg water -urinary Na conc LESS than 10 mEg/L -urine-plasma creatinine ration LESS than 20 -these ranges are diagnostic in ~80% of cases **FE NA *FENa is GREATER than 1% in pt's w/:-ATN *FENa is LESS than 1% in pts w/:-PRE-RENAL AZOTEMIA *pts w/ radiocontrast induced acute renal failure often have: -FENa values LESS than 1% though ATN is PRESENT
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Ketamine For Treatment-Resistant Depression (2016)Document167 pagesKetamine For Treatment-Resistant Depression (2016)JorgeMM67% (3)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Charts For Kidney and Lower Urinary Tract Pathology. NephrologyDocument34 pagesCharts For Kidney and Lower Urinary Tract Pathology. NephrologyM PatelNo ratings yet
- CKD Pocket GuideDocument2 pagesCKD Pocket GuideLutfi MalefoNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Borax Conspiracy How The Arthritis Cure Has Been Stopped Walter LastDocument12 pagesThe Borax Conspiracy How The Arthritis Cure Has Been Stopped Walter Lastevimagg100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Name Types Disease Mechanism AE Other C. Cycle Resistance (CP Pg. 326) Alkylating AgentsDocument12 pagesName Types Disease Mechanism AE Other C. Cycle Resistance (CP Pg. 326) Alkylating AgentsM PatelNo ratings yet
- Psychiatry MnemonicsDocument7 pagesPsychiatry MnemonicsFahad Almalki93% (15)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Anemias ChartDocument14 pagesAnemias ChartM Patel100% (2)
- Biostatistics Epidemiology Definitions ChartDocument10 pagesBiostatistics Epidemiology Definitions ChartM PatelNo ratings yet
- Biochemistry Word AssociationDocument12 pagesBiochemistry Word AssociationM PatelNo ratings yet
- Surgery Oral ExamDocument46 pagesSurgery Oral ExamM Patel100% (9)
- Embroyology Word AssociationDocument5 pagesEmbroyology Word AssociationM PatelNo ratings yet
- Hyperemesis Gravidarum PresentationDocument22 pagesHyperemesis Gravidarum PresentationMaricar Sanson FelicianoNo ratings yet
- Nephrology FormulasDocument3 pagesNephrology FormulasM Patel0% (1)
- Nina Bacteria Chart Medical School Step 1Document11 pagesNina Bacteria Chart Medical School Step 1M PatelNo ratings yet
- DRUG STUDY LactuloseDocument2 pagesDRUG STUDY LactuloseKayki LouiseNo ratings yet
- Giovanni Maciocia Menorrhagia NotesDocument22 pagesGiovanni Maciocia Menorrhagia Noteshihi12100% (5)
- Pharm AntibioticsDocument8 pagesPharm AntibioticsM PatelNo ratings yet
- E Coli Types-PrintedDocument2 pagesE Coli Types-PrintedM PatelNo ratings yet
- Tumor Genes Growth FactorsDocument4 pagesTumor Genes Growth FactorsM PatelNo ratings yet
- Microbiology Step 1 Antimicrobials ChartDocument6 pagesMicrobiology Step 1 Antimicrobials ChartM Patel100% (1)
- Iv. Concentric Hypertrophy: A. Increase Vent Mass Relative To VolumeDocument8 pagesIv. Concentric Hypertrophy: A. Increase Vent Mass Relative To VolumeM PatelNo ratings yet
- Kidney Acidosis-Alkalosis PRoblemsDocument3 pagesKidney Acidosis-Alkalosis PRoblemsM PatelNo ratings yet
- Microbiolology Medical School Cultivation Media For BacteriaDocument11 pagesMicrobiolology Medical School Cultivation Media For BacteriaM PatelNo ratings yet
- Micriobiology Medical School Flowchart PrintedDocument1 pageMicriobiology Medical School Flowchart PrintedM PatelNo ratings yet
- Cardiology Arteritis ChartDocument3 pagesCardiology Arteritis ChartM PatelNo ratings yet
- Psych Drugs List - To Be Filled inDocument3 pagesPsych Drugs List - To Be Filled inM Patel100% (1)
- Digestive Domain Diarrhea, IBSDocument3 pagesDigestive Domain Diarrhea, IBSM PatelNo ratings yet
- Heme-Onc-Anemia Blank TableDocument2 pagesHeme-Onc-Anemia Blank TableM PatelNo ratings yet
- Newborn ChartDocument1 pageNewborn ChartM PatelNo ratings yet
- COPD ChartDocument6 pagesCOPD ChartM PatelNo ratings yet
- Mnemonics CondensedDocument4 pagesMnemonics CondensedM PatelNo ratings yet
- Newborn ChartDocument1 pageNewborn ChartM PatelNo ratings yet
- Mnemonics CondensedDocument4 pagesMnemonics CondensedM PatelNo ratings yet
- GI Tract Epithelium - GastroenterologyDocument3 pagesGI Tract Epithelium - GastroenterologyM PatelNo ratings yet
- Obstetrics Gynecology TableDocument22 pagesObstetrics Gynecology TableM PatelNo ratings yet
- Anaphy ReviewerDocument19 pagesAnaphy ReviewerGian Paolo P. CHAVEZNo ratings yet
- Fluid Balance Case StudyDocument9 pagesFluid Balance Case StudyAna BienneNo ratings yet
- dm2020 0202 PDFDocument6 pagesdm2020 0202 PDFcode4saleNo ratings yet
- Diagnostic Approach To The Adult With Jaundice or Asymptomatic Hyperbilirubinemia - UpToDateDocument17 pagesDiagnostic Approach To The Adult With Jaundice or Asymptomatic Hyperbilirubinemia - UpToDateVictor MarquesNo ratings yet
- Acupressure Points For Constipation and Diarrhrea ReliefDocument5 pagesAcupressure Points For Constipation and Diarrhrea ReliefConstantin-Mihail PopescuNo ratings yet
- Thrombolytic Therapy in Acute Myocardial InfarctionDocument7 pagesThrombolytic Therapy in Acute Myocardial InfarctionRumela Ganguly ChakrabortyNo ratings yet
- Structure and Function of The Human EyeDocument10 pagesStructure and Function of The Human EyeSyed MujtabaNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofahmadto80No ratings yet
- Final Result Special Mop Up Round IIDocument12 pagesFinal Result Special Mop Up Round IIDr.vidyaNo ratings yet
- 2 AleDocument10 pages2 AleAna María ReyesNo ratings yet
- Case PresDocument22 pagesCase Presandrei jinNo ratings yet
- Effects of The Treatment Method of Reproductive Performance in Cows With Retention of Fetal MembranesDocument10 pagesEffects of The Treatment Method of Reproductive Performance in Cows With Retention of Fetal MembranesAlberto BrahmNo ratings yet
- Jurnal SinusitisDocument4 pagesJurnal SinusitisAndriyani YaniNo ratings yet
- Perspektif Keperawatan PaliatifDocument11 pagesPerspektif Keperawatan PaliatifAyudina FebrianiNo ratings yet
- Oxygen Therapy For NurseDocument46 pagesOxygen Therapy For NurseselviiNo ratings yet
- Instrument Cleaning ProgramDocument6 pagesInstrument Cleaning ProgramGood M ArifinNo ratings yet
- Implementasi Program Antenatal Terpadu Di Puskesmas Tanjung Agung Kabupaten Ogan Komering Ulu Dengan Pendekatan Balance ScorecardDocument9 pagesImplementasi Program Antenatal Terpadu Di Puskesmas Tanjung Agung Kabupaten Ogan Komering Ulu Dengan Pendekatan Balance ScorecardRosinta Dwi OktaviaNo ratings yet
- Comparison - of - ABAcard - p30 - and RSID - Semen - Test - Kits - For - Forensic - Semen - Identification PDFDocument5 pagesComparison - of - ABAcard - p30 - and RSID - Semen - Test - Kits - For - Forensic - Semen - Identification PDFEdward Arthur IskandarNo ratings yet
- Chapter 43 - Thrombocytopenia and ThrombocytosisDocument6 pagesChapter 43 - Thrombocytopenia and ThrombocytosisNathaniel SimNo ratings yet
- 1st Prelim Exam Wellness MassageDocument2 pages1st Prelim Exam Wellness MassageAnnaVictory Tamse CrisolNo ratings yet
- Covid-19 HelpDocument35 pagesCovid-19 HelptayrochaaraujoNo ratings yet
- 3 PBDocument9 pages3 PBSusana Tito LuceroNo ratings yet
- The Influence of Probiotics and Antibiotic Growth PromoterDocument7 pagesThe Influence of Probiotics and Antibiotic Growth PromoterOliver TalipNo ratings yet
- Self Care Management and Puberty Health IssuesDocument10 pagesSelf Care Management and Puberty Health IssuesIan Atienza0% (1)