Professional Documents
Culture Documents
Myocardial Infarction
Uploaded by
Ranela Kwinkee Pastor SalazarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Myocardial Infarction
Uploaded by
Ranela Kwinkee Pastor SalazarCopyright:
Available Formats
MYOCARDIAL INFARCTION First Heart Sound due to the coming of the AV valve, slaps at the beginning of ventricular systole
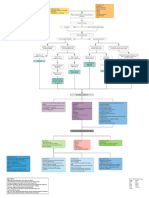
le Second Heart Sound due to the closure of the semi-lunar valve at the beginning of ventricular diastole Murmur can be heard as the blood flows thru a narrowed opening Conduction System - SA node > AV node > left and right bundle branches > Purkinje Fibers Automaticity the ability of the heart to initiate an impulse without external stimulus Excitability the ability of cardiac cells to reach a threshold and respond to a stimulus Conducting Cells make up the specialized conduction system in the heart and are responsible for initiating and spreading the electrical impulse. Contracting Cells make up the walls of atria and ventricles and are responsible for contraction of the chambers. Ischemia temporarily interrupts the blood supply to myocardial tissue but usually doesnt cause ECG changes T wave inversion Injury results from prolonged blood supply interruption causes further cell injury ECG changes elevated ST segment Infarction results when failure of perfusion causes myocardial cell death (necrosis) ECG changes pathologic Q wave SA Node Both Atria Delayed in AV node so that atria has time to contract Picks up speed to Purkinje fibers to the ventricular myocardium Pathophysiology Causes Coronary or Atherosclerotic heart disease Coronary or thrombosis or embolism Decreased blood flow with shock or hemorrhage Direct trauma 3 Is ischemia, injury, infarction MI Causes Myocardial Ischemia Decreased Myocardial Oxygen Supply Increased Cellular Hypoxia Altered Cell Membrane Integrity Decreased Myocardial Contractility Decreased Cardiac Output Decreased Arterial Pressure Stimulation of Baroreceptors Stimulation of Sympathetic Baroreceptors
Increased Peripheral Vasoconstriction Increased Afterload Increased Myocardial Oxygen Demand
Increased Myocardial Contractility
Increased Heartrate Decreased Diastolic Filling Decreased Myocardial Tissue Perfusion
Manifestations of MI Chest pain (crushing, severe, prolonged and not relieved by rest or nitroglycerin) Pain Upper cheek Neck and jaw Gastric
Intracapsular Beneath sternum, radiating to the neck and jaw. Beneath sternum radiating down left arm. Epigastric radiating to neck, jaw and arms Left shoulder, inner aspect of both arm Character: tight, heavy, constricting pain associated with restlessness, cold clammy skin Retrosternal area radiates to shoulder, jaw and left arm and sometimes the pain is in epigastric Factors that relieve the pain of infarction is not relieved by nitroglycerin (a coronary vasodilator) Narrowing of epicardial blood vessels due to atherosclerosis Plaque is the most common cause of MI Total occlusion of the blood vessel of more than 4 to 6 hours results to irreversible myocardial necrosis, but reperfusion can salvage the condition Diagnostic Procedures ECG elevated ST segment (initially ok but later turns convex) T wave inversion (refers ischemia) Pathologic Q wave (develops several hours) Plasma Enzymes Diagnostic Monitoring Requirement for Diagnostic Test Sensitive Specific Early rise Prolonged rise Precise Simple and rapid Cheap Enzyme activities are greater in tissue than in plasma Enzyme clear slowly in blood Creatinine Kinase (CK) comprises 3 isoenzymes in myocardium. CPK (CKMB) increased within 3-12 hours of onset, peak at 24 hours, returns to normal level arter 48072 hours, sensitivity is 95% with very high specificity but not as high as troponin levels. Cardiac enzyme analysis CPK elevation within 4-8 hours of MI onset CPK-MB elevation within 4-8 hours of MI onset LDL elevation within 24-48 hours after MI onset LDH1 elevation within 8-24 hours after MI onset LDH1/LDH2 ration > 1 within 24048 hours after MI onset AST (SGOT) elevation within 8-12 hours after MI onset C-reactive Protein a marker of acute inflammation ESR rises within 3 days and remain elevated for several weeks CBC indicated if anemia is suspected as a precipitant Leukocytosis observed within several hours after MI Troponin not an enzyme but a protein. cTnT known as cardiac troponin T (cardiospecific polypeptide), rises within 3-4 hours after Mi and sustained after 10 days or more cTnT cardiac troponin I Nursing Diagnosis Alteration in comfort related to myocardial ischemia Rate the discomfort, assess the presence of discomfort, provide periods of rest Potential for anxiety Provide information regarding diagnosis, diagnostic procedures Alteration in cardiac output: decreased related Initiate cardiac monitoring Coping potential: ineffective related to diagnosis and fear of dying Encourage verbalization of feelings Monitor physiologic parameters closely Knowledge deficit regarding coronary artery disease Assess knowledge base and learning needs Utilize resources in teaching Nursing Interventions Provide oxygen inhalation at 2 L/min Semifowlers position Administer medications Morphine causes respiratory depression, check RR and HR, relaxes bronchioles and enhances respiration
Nitrates Throbolytic agents Anticoagulants Stool softeners Nitroglycerin causes relaxation Vasodilators Beta-adrenergic blocker Analgesic ACE inhibitors Streptokinase Minimize metabolic demands Provide soft diet Decreased cholesterol, decreased fat Provide rest periods Client teaching: METHOD of discharge planning Medication Environmental sanitation Transfer to lower floor Observe right diet Bed rest 1st 3 days ROM exercise Start dangling of feet at side of bed, if not chest pain sitting out of bed on chair for 30 minutes, if no chest pain ambulation in the room, if no chest pain go to comfort room or toilet, if no chest pain can go outside the room to hallway 3x/day, if no chest pain can go to other places, if no chest pain, can have sexual intercourse If patient can walk 3-4 miles/hour ready to resume SI
You might also like
- Anatomy & Physiology of the HeartDocument5 pagesAnatomy & Physiology of the HeartLyka Milo AvilaNo ratings yet
- Myocardial Infarction With CABG Concept MapDocument1 pageMyocardial Infarction With CABG Concept MapMaria Therese100% (1)
- CardiomyopathyDocument1 pageCardiomyopathyTrisha VergaraNo ratings yet
- Myocardial Infarction Guide: Causes, Symptoms & TreatmentDocument28 pagesMyocardial Infarction Guide: Causes, Symptoms & Treatmentshaitabligan100% (1)
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionYanna Habib-MangotaraNo ratings yet
- Cardiac Fluid ManagementDocument9 pagesCardiac Fluid ManagementroseasNo ratings yet
- Peripheral Vascular Disease NursingDocument13 pagesPeripheral Vascular Disease NursingCatlyn Chatpman100% (1)
- Acute Lymphocytic LeukemiaDocument7 pagesAcute Lymphocytic Leukemiamildred alidon100% (1)
- Acute Respiratory Failure For StudentDocument41 pagesAcute Respiratory Failure For Studentapi-379952350% (4)
- Cardiogenic and Septic Shock LectureDocument27 pagesCardiogenic and Septic Shock LectureMohd EdieNo ratings yet
- PathophysiologyDocument2 pagesPathophysiologyKarla Karina Dela CruzNo ratings yet
- Cardiac Tamponade: Symptoms, Causes & Treatment of Heart CompressionDocument3 pagesCardiac Tamponade: Symptoms, Causes & Treatment of Heart Compressionscremo_xtreme100% (2)
- Cardiovascular Diseases ListDocument7 pagesCardiovascular Diseases ListAnant SinghNo ratings yet
- Pulmonary CirculationDocument4 pagesPulmonary CirculationDr Md Abedur RahmanNo ratings yet
- The University of Lahore: Stroke (Case Study Paper)Document13 pagesThe University of Lahore: Stroke (Case Study Paper)fazal rahmanNo ratings yet
- PathoPhysiology of Renal Failure OverviewDocument7 pagesPathoPhysiology of Renal Failure Overviewnursing concept maps100% (1)
- Critical Care Note PDFDocument10 pagesCritical Care Note PDFlml100% (1)
- ECG BasicsDocument15 pagesECG Basicsrohitmeena2889No ratings yet
- Diagnosis of Cardiovascular Disease - TranscriptionDocument11 pagesDiagnosis of Cardiovascular Disease - TranscriptionPauline Del MundoNo ratings yet
- Anatomy and Physiology SLEDocument27 pagesAnatomy and Physiology SLEMoti Pagador100% (4)
- DYSRHYTHMIASDocument9 pagesDYSRHYTHMIASgudobenNo ratings yet
- Transient Ischemic AttackDocument3 pagesTransient Ischemic AttackJevisco LauNo ratings yet
- Hypertensive Emergencies: When to Admit or DischargeDocument4 pagesHypertensive Emergencies: When to Admit or DischargeRara MuuztmuuztmuccuNo ratings yet
- Concept MapDocument6 pagesConcept Mapmenickel3100% (1)
- COPD NotesDocument4 pagesCOPD NotesjisooNo ratings yet
- SbarDocument2 pagesSbarbojums100% (2)
- Nursing Care PlanDocument8 pagesNursing Care PlanAngela SweetNo ratings yet
- SIADH (Syndrome of Inapproperiate Antidiuretic Hormone Secretion)Document11 pagesSIADH (Syndrome of Inapproperiate Antidiuretic Hormone Secretion)itsmesubu100% (2)
- Concept Map PEDocument3 pagesConcept Map PERobert MariasiNo ratings yet
- SBAR Report To Physician About A Critical SitutionDocument3 pagesSBAR Report To Physician About A Critical SitutionRandolph DjanieNo ratings yet
- Essential Stroke Nursing GuideDocument5 pagesEssential Stroke Nursing GuideAshleigh Johnstone100% (1)
- Myocardial InfarctionDocument2 pagesMyocardial InfarctionJuliusSerdeñaTrapalNo ratings yet
- Left Sided Heart FailureDocument25 pagesLeft Sided Heart FailurePaulNo ratings yet
- CopdDocument3 pagesCopdFawad HameediNo ratings yet
- NCPDocument3 pagesNCPJanie StubbertNo ratings yet
- Congestive Heart FailureDocument4 pagesCongestive Heart FailureAnnie Grace PoliranNo ratings yet
- Medical-Surgical Nursing Lecture NotesDocument90 pagesMedical-Surgical Nursing Lecture NotesJessica AnisNo ratings yet
- 1st, 2nd, 3rd Degree AV BLockDocument8 pages1st, 2nd, 3rd Degree AV BLockladydreamer_92No ratings yet
- Shock HypovolemicDocument19 pagesShock HypovolemicChance Jackson100% (1)
- Respiratory System Disorders R/T NursingDocument27 pagesRespiratory System Disorders R/T NursinggakuiNo ratings yet
- Chronic Bronchitis and EmphesemaDocument2 pagesChronic Bronchitis and Emphesemanursing concept maps100% (2)
- 2 NCP Chronic Heart FailureDocument5 pages2 NCP Chronic Heart FailureLovely CacapitNo ratings yet
- Care of Adults 25 Cardiovascular ManagementDocument39 pagesCare of Adults 25 Cardiovascular ManagementGaras AnnaBerniceNo ratings yet
- Unstable AnginaDocument10 pagesUnstable AnginaironNo ratings yet
- Fluids and Electrolytes Study GuideDocument13 pagesFluids and Electrolytes Study GuideElizabeth McKeeNo ratings yet
- Decreased Cardiac OutputDocument3 pagesDecreased Cardiac OutputRizalyn QuindipanNo ratings yet
- Rapid Assessment SheetDocument5 pagesRapid Assessment SheetElise HowardNo ratings yet
- MedSurg 2Document69 pagesMedSurg 2Claire Maurice JuaneroNo ratings yet
- Cerebral Aneurysms: Aneurysms Posterior Circulation Basilar Artery Vertebral Arteries Posterior Communicating ArteryDocument10 pagesCerebral Aneurysms: Aneurysms Posterior Circulation Basilar Artery Vertebral Arteries Posterior Communicating ArteryRani SujithNo ratings yet
- NUR100 Sherpath Skin Overview + Skin IntegrityDocument15 pagesNUR100 Sherpath Skin Overview + Skin Integritycaloy2345caloy100% (1)
- NCM 106 - Case Analysis - Nursing Care Plan of Heart FailureDocument2 pagesNCM 106 - Case Analysis - Nursing Care Plan of Heart FailureMarisol Jane JomayaNo ratings yet
- Atrial Fibrillation - Practice Essentials, Background, PathophysiologyDocument17 pagesAtrial Fibrillation - Practice Essentials, Background, PathophysiologyLorentina Den PanjaitanNo ratings yet
- Procedure ON Bladder Irrigation: SUBMITTED TO: Mr. EKE Lama TamangDocument17 pagesProcedure ON Bladder Irrigation: SUBMITTED TO: Mr. EKE Lama TamangRajaNo ratings yet
- Cardiogenic Shock HandoutsDocument2 pagesCardiogenic Shock HandoutsAileenNo ratings yet
- Infective EndocarditisDocument18 pagesInfective EndocarditisSam100% (1)
- Myocardial Infarction Causes, Symptoms, TreatmentDocument23 pagesMyocardial Infarction Causes, Symptoms, TreatmentAnelle Umali50% (2)
- Neurogenic ShockDocument11 pagesNeurogenic Shocklulu voxNo ratings yet
- The Pathophysiology and Pharmacotherapy of Myocardial InfarctionFrom EverandThe Pathophysiology and Pharmacotherapy of Myocardial InfarctionNabil El-SherifNo ratings yet
- Critical Care Nursing: Learning from PracticeFrom EverandCritical Care Nursing: Learning from PracticeSuzanne BenchNo ratings yet
- SLE PathophysiologyDocument3 pagesSLE PathophysiologyRanela Kwinkee Pastor Salazar100% (7)
- Disturbance of Immune SystemDocument14 pagesDisturbance of Immune SystemRanela Kwinkee Pastor SalazarNo ratings yet
- Case Study Acute Pyelonephritis FINALDocument20 pagesCase Study Acute Pyelonephritis FINALRanela Kwinkee Pastor SalazarNo ratings yet
- Managing Kimmelstiel-Wilson SyndromeDocument13 pagesManaging Kimmelstiel-Wilson SyndromeRanela Kwinkee Pastor SalazarNo ratings yet
- Nursing Memory JoggersDocument2 pagesNursing Memory JoggersMarcus, RN96% (24)
- Best Photo ContestDocument2 pagesBest Photo ContestRanela Kwinkee Pastor SalazarNo ratings yet
- Nicu CasesDocument1 pageNicu CasesRanela Kwinkee Pastor SalazarNo ratings yet
- Heart Dissection PDFDocument2 pagesHeart Dissection PDFharryNo ratings yet
- Part 02 EP TracingsDocument42 pagesPart 02 EP TracingsHany100% (1)
- Indikasi Masuk CvcuDocument4 pagesIndikasi Masuk CvcuMukarramah Ummi UmayyahNo ratings yet
- Defibrillator Sync TestingDocument4 pagesDefibrillator Sync TestingYahya SalemNo ratings yet
- Multiple Choice Questions (MCQ) Topic Quiz Cardiovascular SystemDocument18 pagesMultiple Choice Questions (MCQ) Topic Quiz Cardiovascular Systemahsan gujjar100% (1)
- Blood Pressure ChartDocument3 pagesBlood Pressure ChartmickeyNo ratings yet
- CardiomyopathyDocument17 pagesCardiomyopathysarguss1450% (2)
- Anatomy and Physiology of The HeartDocument3 pagesAnatomy and Physiology of The HeartjeffcaselNo ratings yet
- Algorithm Extracts LVEF from Echocardiogram ReportsDocument2 pagesAlgorithm Extracts LVEF from Echocardiogram ReportsPunjabi FootballNo ratings yet
- NCP 1Document1 pageNCP 1hsiriaNo ratings yet
- Institute of Nursing and Allied Health SciencesDocument4 pagesInstitute of Nursing and Allied Health Sciencesshadow gonzalezNo ratings yet
- Bedah - Buerger's DiseaseDocument20 pagesBedah - Buerger's DiseaseDessy KusumadewiNo ratings yet
- Bioset 9000Document34 pagesBioset 9000Pavel RashkovNo ratings yet
- Gore Meetformulier Excluder AbdominaalDocument2 pagesGore Meetformulier Excluder AbdominaalAndreas PanagiotopoulosNo ratings yet
- Autoregulation of The Cardiovascular SystemDocument15 pagesAutoregulation of The Cardiovascular SystemErinne DefrianiNo ratings yet
- Circulatory System Lesson PlanDocument14 pagesCirculatory System Lesson PlanHarold Jay LamangNo ratings yet
- Improving Neonatal Tissue Perfusion for SepsisDocument2 pagesImproving Neonatal Tissue Perfusion for SepsisNiña Montejo Ealdama100% (1)
- Daftar InventarisDocument47 pagesDaftar InventarisTri NastitiNo ratings yet
- Drug Study - Amiodaron HydrochlorideDocument4 pagesDrug Study - Amiodaron HydrochlorideTwinkle SalongaNo ratings yet
- 4 Med LongDocument135 pages4 Med LongElla H. LeeNo ratings yet
- Laporan Kasus Kardiovaskuler (Fransiska - C11107156)Document32 pagesLaporan Kasus Kardiovaskuler (Fransiska - C11107156)Fransiska Carmelia SubenoNo ratings yet
- Azmi, Et Al. (2015) Quality of Life Among Patients With Acute Coronary Syndrome in MalaysiaDocument4 pagesAzmi, Et Al. (2015) Quality of Life Among Patients With Acute Coronary Syndrome in Malaysiacipto susiloNo ratings yet
- Vertebrobasilar Insufficiency/Syndrome: Hitesh Rohit (3 Year BPT)Document14 pagesVertebrobasilar Insufficiency/Syndrome: Hitesh Rohit (3 Year BPT)Hitesh N RohitNo ratings yet
- Management of Acute MI, Role of Streptokinase, NicvdDocument22 pagesManagement of Acute MI, Role of Streptokinase, NicvdNavojit ChowdhuryNo ratings yet
- BIOCHEMISTRY AND PHYSIOLOGY Nuggets PDFDocument137 pagesBIOCHEMISTRY AND PHYSIOLOGY Nuggets PDFHKNo ratings yet
- Assisting Central Venous Catheter (CVC) Insertion (Procedure1)Document7 pagesAssisting Central Venous Catheter (CVC) Insertion (Procedure1)BsBs A7medNo ratings yet
- Imperial College Medical Finals Notes SummaryDocument138 pagesImperial College Medical Finals Notes SummaryThistell ThistleNo ratings yet
- Anatomy and Physiology of the Cardiovascular SystemDocument103 pagesAnatomy and Physiology of the Cardiovascular SystemChristina GonezNo ratings yet
- Microlife bprm100 Usersmanual PDFDocument66 pagesMicrolife bprm100 Usersmanual PDFanon_188270051No ratings yet
- PTCADocument51 pagesPTCAJasmin Jacob100% (1)