Professional Documents
Culture Documents
Spontaneous Fracture of The Tibial Sesamoid
Uploaded by
shankardeshmukhaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Spontaneous Fracture of The Tibial Sesamoid
Uploaded by
shankardeshmukhaCopyright:
Available Formats
SPONTANEOUS FRACTURE OF THE TIBIAL SESAMOID: A CASE REPORT
Tibial sesamoid fracture is common in athletes and active individuals. Usually, the incident is preceded by stress injury or acute trauma from stressed dorsiflexion or hyperextension of the hallux. The first ray will transmit about 60% of a persons weight-bearing stress through the first metatarsophalangeal joint during the gait cycle. In acute instances, these stresses can be many times greater. Interestingly, there have been infrequent reports of tibial sesamoid fracture from non-acute injury such as walking. In nonacute injuries, many patients will present with a sharp initial pain followed by a dull ache or pain under the sesamoids. The differential diagnosis may include sesamoiditis, chondromalacia, first metatarsal joint capsulitis, flexor hallucis tendonitis and arthritis.
MRI and radiographic evaluation are the most common modalities used to differentiate injury and fracture from more subtle injuries such as sesamoiditis or capsulitis.
A clinical entity such as a bipartite sesamoid may confuse the clinician in the proper diagnosis. This condition was first described as early as 1904 by Stieda and confirmed by Dwight. [1] Bipartite sesamoids are a common finding on foot radiographs. They often look like tibial sesamoid fractures, however, close inspection of the radiograph usually reveals a well-defined, smoother partition between the two fragments. A fractured sesamoid will likely have a rough, irregular partition. Bipartite sesamoids are a normal variant when two ossification centers fail to fuse at maturity. This condition is present in about 10% of the population, and in that population, 25% are bilateral. [2] In cases of acute injury, diastasis of the bipartite sesamoid can lead to acute pain under the first metatarsal head. This has been reported in hyperextension or turf-toe injuries in football players. *3+
It is the authors opinion that bipartite sesamoids can also lead to sesamoid pain. Bone scintigraphy can also differentiate sesamoid fracture from congenital partition. [4]
In non-acute injuries of the tibial sesamoid, conservative treatments are designed to de-weight the sesamoid and allow for healing. Conservative methods of treatment can include wearing a surgical shoe to prevent extension of the toe or even casting and non-weightbearing. Once the correct diagnosis is made, appropriate treatment can be initiated. Conservative care for sesamoiditis can also include wearing an accommodative insert with first metatarsal padding. The pad can be placed just behind the sesamoid in order to decrease stress through the sesamoid apparatus. Other conservative treatments include 1) NSAIDS, 2) avoiding high heels, 3) off-loading shoes and 4) steroid injection. These injections may be used along with joint taping to prevent excessive extension of the first metatarsophalangeal
joint. Care must be taken in the injection of steroids to this region, especially if fracture is suspected. Injection of steroids can sometimes lead to avascular necrosis of a fractured tibial sesamoid.
In acute fracture, non-weightbearing in a cast is recommended for 6 to 8 weeks. [5,7] It appears, from experience and previous study, that the non-union rate of sesamoid fractures is high. This may be related to the vascular supply of the sesamoids and the forces placed on the bone fragments once fractured. It is theorized that the anatomical pull of soft tissue, once the sesamoid fractures, causes a distraction of the fracture line. Anatomically, the tibial sesamoid has anatomical attachments to the abductor hallucis muscle, plantar fascia, flexor hallucis brevis tendon, intersesamoidal ligament, medial metatarsal and phalangeal sesamoid ligaments. [4]
Once the tibial sesamoid fractures, these attachments tend to distract the fracture fragments. The vascularity of the tibial sesamoid is supplied by three sources: 1) the deep and superficial branches of the medial plantar artery, 2) branches from the lateral plantar artery and perforating branches of the dorsalis pedis artery, and 3) pole arteries through the length of the sesamoid. [4,6] One explanation for the high incidence of non-union is that the primary blood supply of all three sources originates from the proximal pole of the sesamoid through the tendon of the flexor hallucis brevis. [4] Since most fractures of the tibial sesamoid are transverse, once the fracture occurs, the distraction causes disruption of this vascular communication leading to non-union. Bone stimulators may also be effective in the conservative treatment of tibial sesamoid fractures. They are certainly indicated after immobilization and non-unions are suspected.
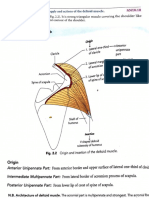
Anatomy and Sesamoid Position in its relation to Hallux Valgus
The sesamoid position may also play an important role in stresses that are directed through the metatarsophalangeal joint. Anatomically, both the tibial and fibular sesamoids act in unison during the propulsive phase of gait. The articular surfaces of both the tibial and fibular sesamoids glide along the sesamoidal groove and are separated by the central crista in its anatomical alignment. The crista is a central plantar ridge along the metatarsal head that separates the sesamoids. The glistening surfaces of the sesamoids are facet- shaped within the plantar groove of the metatarsal head. In hallux valgus, the sesamoid position is described in distinctive positions. These positions are described as positions 1-7 in the radiographic evaluation of hallux valgus. (Fig. 1.)
Figure 1 Tibial sesamoid position is radiographically described in seven positions. Position four is described as being directly under the crista of the first metatarsal head, likely increases stress forces
through the tibital sesamoid. The fibular sesamoid (FS) will rotate even further into the first interspace between the first and second metatarsal as the hallux valgus worsens.
It is commonly understood that these positions are dictated by the movement of the metatarsal head as the entire metatarsal subluxes medially in the classic hallux abductovalgus deformity.
It is theorized that position four is the most stressful position for the tibial sesamoid and could cause tibial sesamoid fracture under the right circumstances.
This may be even more plausible in a high-heeled shoe that causes increased stress along the plantar metatarsophalangeal joint.
Case Report
In February 2006, a 33 year old active female began to experience episodes of pain under the tibial sesamoid. She reported walking in the airport and experiencing a pain under the first metatarsophalangeal joint while in a high heel. She initially presented to another podiatrist, who diagnosed her with fractured tibial sesamoid. He instituted conservative treatment including padding and a local steroid injection. She did well for several months , but continued to have episodes of increasing pain.
She presented to our office in September 2006. Clinical evaluation revealed bunion pain and pain directly under the tibial sesamoid. She was ambulating and wearing shoes, but had episodes of pain and signs of non-healing of the tibial sesamoid fracture. Radiographs confirmed a tibial sesamoid fracture with a mild bunion deformity. (Fig. 3)
Figure 3 Radiographs confirm tibial sesamoid fracture. The fracture edges are irregular and sharp, consistent with fracture instead of bi-partite sesamoid. The tibial sesamoid is positioned directly under the crista in sesamoid position four.
We placed her on crutches with off-loading for 6 weeks and progression to a Darco walking shoe, then athletic sneakers with proper accommodative metatarsal padding. Despite these attempts, she continued to have pain and we decided to schedule her for simple bunionectomy and tibial sesamoid excision.
Surgical Technique
The patient was brought to the operating room and underwent simple bunionectomy and tibial sesamoid excision. A medial incision is made along the border of the first metatarsophalangeal joint. Care must be taken to identify the medial cutaneous nerve or bunion nerve.
The medial cutaneous nerve has variable branches and may run a course more medial and inferior to the dorsomedial branch. Once the nerve is identified, a medical capsular incision is made and the fracture is identified. (Figs. 4ab) Care must also be taken when excising the tibial sesamoid. The sesamoid is encased along the capsular tissue of the first metatarsophalangeal joint. It has attachments to the abductor hallucis muscle, plantar fascia, flexor hallucis brevis tendon, intersesamoidal ligament, medial metatarsal and phalangeal sesamoid ligaments. The flexor hallucis longus tendon also glides between the two sesamoids.
Figures 4ab (a) A medially placed incision along the sesamoid is fashioned. Care is taken to identify the medial cutaneous nerve. (identified at the tip of the blade). (b) Once the capsule is incised, the fractured tibial sesamoid is identified.
Care must be taken not to cut the tendon when excising the sesamoid. A number 15 blade is used to enucleate the sesamoid from these fibrous, soft tissue attachments. Once the sesamoid is removed, suture is used to approximate the ligamentous and capsular attachments. The sesamoid should be cleanly excised with little tissue attachment. (Fig. 5) The postoperative radiographs reveal a postexcisional tibial sesamoidectomy with simple bunionectomy. (Fig. 6).
Figure 5 After the tibial sesamoid fracture is excised, it appears as if the fracture recently occurred. There are no signs of attempted bone healing or calcification. This is testament to the distraction forces
that keep the sesamoid fracture apart.
Figure 6 Post-operative radiographs reveal removal of the tibial sesamoid and a simple bunionectomy performed.
Discussion
Surgical excision of the entire tibial sesamoid appears to be a viable alternative of treatment to nonhealing fractures of the tibial sesamoid. One of the earliest reports of tibial sesamoidectomy with relief of symptoms was described by Mller in 1911. [1] Recently, Jones et al., reported the results of tibial sesamoid excision following tibial sesamoid fracture in a softball player. After 1 year, the patient was free of pain in all shoe types. *5+ There is only one report to date of attempting internal fixation to repair the tibial sesamoid fracture.
In 2001, Riley and Selner reported using monofilament wire to internally fixate a tibial sesamoid fracture with excellent results in a 17 year old female. [7] This approach may be more desirable in the acute fracture of young, active patients. In our case, surgical excision was more desirable since the tibial sesamoid was directly placed under the crista. Reported complications of removing the tibial sesamoid include hallux valgus, transfer pain, tendonitis, arthritis and hallux extensus. [5,7]
In this particular case, the association of hallux valgus and the placement of the tibial sesasmoid in position four appear to increase the likelihood of fracture when wearing a high-heeled shoe. The association of hallux valgus as a risk for tibial sesamoid fracture was first described in 1929, although most cases of fractures are related to direct trauma and a sudden increase in weight-bearing force, Hobart reported an association with hallux valgus is often found. *8+ Anatomically, the central rise of the crista may explain the increased force through a sesamoid. Stressed dorsiflexion in a high heeled shoe after extensive walking could directly lead to spontaneous fracture. In this case, our surgical goals were straight forward: simple bumpectomy with sesamoid removal.
To date, the patient has returned to activity with accommodative sesamoid padding and without pain or discomfort.
Conclusion
The tibial sesamoid fracture is now demonstrated to be a common fracture of the foot. The diagnosis is usually made by clinical presentation, using radiographs and MRI for confirmation. Bone scans can also be used. The stresses placed through the metatarsal head during gait can be complicated. This report suggests that an abnormally placed sesamoid due to associated hallux valgus or bunion may lead to increased stress of the sesamoid and can lead to fracture. This is especially true in patients who attempt to walk for extended periods in a high-heel shoe. It is suggested that patients with hallux valgus wear a simple accommodative device, such as a dress orthotic, in an attempt to off-load the stress through the sesamoids. This case also demonstrates that if the sesamoid does fracture, total tibial sesamoidectomy is a viable procedure in cases of non-union or delayed healing.
References
1. Mller, G.P. Fracture of the Sesamoid Bones. Ann Surg, Read before the Philadelphia Academy of Surgery, October 2, 1911. [Online-PDF] 2. Neerajana, DODA, Wilfred, C.G. PEH Woman with possible right toe fracture: Radiology Series Asia Pacific Journal of Family Medicine, Volume 5, Issue 3, 2006. 3. Rodeo, SA, et al Diastasis of bipartite sesamoids of the first metatsophalangeal joint. Foot Ankle, 14(8): 425-34. Oct. 1993. 4. Swierzewski, J. Acute and Chronic Injuries to the Sesamoids: Etiology and Treatment CPMA, Vol 10, No. 4, Fall 2001. 5. Jones, J.L., Losito, J.M. Tibial Sesamoid Fracture in a Softball Player JAPMA Vol. 97, No. 1 Jan/Feb 2007. 6. Banks, A.S., Downey, M.S., et al McGlamrys Comprehensive Textbook of Foot and Ankle Surgery, 3rd ed. Lipcott and Williams, 2001. 7. Riley, J., Selner, M. Internal Fixation of a Displaced Tibial Sesamoid Fracture JAPMA, Vol. 91, No. 10, 2001. 8. Hobart, M. Fracture of Sesamoid Bones of the Foot: With Report of a Case JBJS (Am) 11:298-302, 1929.
You might also like
- Alopecia Areata Part 1Document12 pagesAlopecia Areata Part 1shankardeshmukhaNo ratings yet
- Tej Pal YadavDocument2 pagesTej Pal YadavshankardeshmukhaNo ratings yet
- Structured Knowledge Questionnaire To Assess The Knowledge of Women Regarding Prevention of Breast Cancer Instruction To The ParticipantDocument3 pagesStructured Knowledge Questionnaire To Assess The Knowledge of Women Regarding Prevention of Breast Cancer Instruction To The ParticipantshankardeshmukhaNo ratings yet
- Complants BookDocument1 pageComplants BookshankardeshmukhaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Calcaneal FractureDocument34 pagesCalcaneal Fracturemmm.orthoNo ratings yet
- Muscular - System McgrawhillDocument60 pagesMuscular - System Mcgrawhillkhara teanoNo ratings yet
- Fragment-Specific Fixation in Distal Radius Fractures: AnatomyDocument8 pagesFragment-Specific Fixation in Distal Radius Fractures: Anatomyosman gorkemNo ratings yet
- The Bones of The Upper LimbDocument1 pageThe Bones of The Upper Limbmarisonomia100% (1)
- Sulaiman2015 Article TheSensoryDistributionInTheDorDocument7 pagesSulaiman2015 Article TheSensoryDistributionInTheDorAslı Beril KarakaşNo ratings yet
- Splints For The NBCOT: Stephanie Shane OTR/L NBCOT TutorDocument29 pagesSplints For The NBCOT: Stephanie Shane OTR/L NBCOT TutorMarina EskandrousNo ratings yet
- Beginner Phase 1 - CompressedDocument21 pagesBeginner Phase 1 - CompressedwonderkidgunzNo ratings yet
- Mindful Motion CaspariDocument103 pagesMindful Motion CaspariKian Fallahi100% (1)
- Brachial PlexopathyDocument17 pagesBrachial Plexopathyemilio9fernandez9gatNo ratings yet
- Latarjet Rehabilitation Protocol: General NotesDocument5 pagesLatarjet Rehabilitation Protocol: General NotesNico BrantesNo ratings yet
- Anatomy - Board Ii: Abdomen - Oral PartDocument25 pagesAnatomy - Board Ii: Abdomen - Oral Partbadiuzzaman2010No ratings yet
- Anatomy 2Document15 pagesAnatomy 2christinejoanNo ratings yet
- Acute Carpal Tunnel Syndrome: A Review of Current LiteratureDocument9 pagesAcute Carpal Tunnel Syndrome: A Review of Current LiteratureUlos BenardNo ratings yet
- Fitness - Weight Training (Grades 11-12) - Free Printable Tests and WorksheetsDocument2 pagesFitness - Weight Training (Grades 11-12) - Free Printable Tests and WorksheetsSuave RevillasNo ratings yet
- Systematizing Closed Guard - FlowChart 1.2Document1 pageSystematizing Closed Guard - FlowChart 1.2Christian LuongNo ratings yet
- The Upper Limb Muscles: ShoulderDocument13 pagesThe Upper Limb Muscles: ShoulderAjay Pal NattNo ratings yet
- Single-Stage Reconstruction of Elbow Flexion Associated With Massive Soft-Tissue Defect Using The Latissimus Dorsi Muscle Bipolar Rotational TransferDocument9 pagesSingle-Stage Reconstruction of Elbow Flexion Associated With Massive Soft-Tissue Defect Using The Latissimus Dorsi Muscle Bipolar Rotational TransferSherif HantashNo ratings yet
- Isncsci Asia Iscos LowDocument2 pagesIsncsci Asia Iscos LowmanuelmayoralNo ratings yet
- Deltoid MuscleDocument2 pagesDeltoid Muscledivyanshu ranjanNo ratings yet
- Shoulder DislocationDocument10 pagesShoulder DislocationMargaret BaleNo ratings yet
- Annotated Bibliography 1Document1 pageAnnotated Bibliography 1api-653977695No ratings yet
- 1471 2474 14 189Document11 pages1471 2474 14 189Evans JohnNo ratings yet
- David Butler Neural Tissue Mobilisation-1Document11 pagesDavid Butler Neural Tissue Mobilisation-1Himani BhondgeNo ratings yet
- Anatomical TerminologiesDocument5 pagesAnatomical TerminologiesAngela RaeNo ratings yet
- The Lower LimbDocument89 pagesThe Lower LimbSantiFaridKalukuNo ratings yet
- G7 - Bones and SkeletonDocument27 pagesG7 - Bones and SkeletonListya RahmawatiNo ratings yet
- 5 Point Touch TherapyDocument8 pages5 Point Touch Therapyantou74No ratings yet
- Guia Vocabulario Ingles HEALTH and ILLNESS Salud y EnfermedadDocument5 pagesGuia Vocabulario Ingles HEALTH and ILLNESS Salud y Enfermedadfarturo22No ratings yet
- Galeazzi Fracture-Dislocation: DR Jaffar Alsayigh DR Abdullah Alshehri Orthopedic Department - KFHUDocument25 pagesGaleazzi Fracture-Dislocation: DR Jaffar Alsayigh DR Abdullah Alshehri Orthopedic Department - KFHUammarNo ratings yet
- Variations of The Flexor Digitorum SuperficialisDocument7 pagesVariations of The Flexor Digitorum SuperficialisGracen33No ratings yet