Professional Documents
Culture Documents
Compendi A
Uploaded by
Ces MangaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Compendi A
Uploaded by
Ces MangaCopyright:
Available Formats
Ancylostoma Duodenale
Ancylostoma duodenale is an S-shaped worm because of its flexure at the frontal end. The worm is pinkish-white. Adult male hookworms range in size from 8-11 mm long, whereas adult females range in size from 10-13 mm long. This species is dimorphic, with the males having bursa characteristics and needle-like spicules with small tips, which are distally fused. Females have a vulva located approximately one-third of the body length from the posterior end. Both male and female hookworms have two powerful ventral teeth in the adult forms of the parasite, one along each side of the buccal capsule; smaller pairs of teeth are located deeper in the capsule.Hookworm eggs have a thin shell and the larvae possess amphids, large paired sensilla on each side of the mouth, which allow them to locate their host. The larvae are rod-shaped and are about 0.004 cm. It is a parasitic nematode worm and commonly known as Old World hookworm.It is small cylindrical worm, greyish-white in color.. The average lifespan of Ancylostoma duodenale is one year.When a filariform larva (infective stage) penetrates the intact skin, the larva enters the blood circulation. It is then carried to the lungs, coughed up, and swallowed back into the small intestine. The larva later matures into an adult in the small intestine and female worms can lay 25,000 eggs per day. The eggs are released into the feces and reside on soil. Embryonated eggs on
soil will hatch into juvenile 1 stage (rhabditiform or noninfective stage) and mature into filariform larvae. The filariform larvae can then penetrate another exposed skin and begin a new cycle of infection. Ancylostoma duodenale is prevalent in southern Europe, northern Africa, India, China, and southeast Asia, small areas of United States, the Caribbean islands, and South America. Transmission of Ancylostoma duodenale is by contact of skin with soil contaminated with larvae. Light infection causes abdominal pain, loss of appetite and geophagy. Heavy infection causes severe protein deficiency or iron deficiency anemia. Protein deficiency may lead to dry skin, edema and potbelly, while iron deficiency anemia might result in mental dullness and heart failure. The eggs of Ancylostoma duodenale and Necator americanus cannot be distinguished. Larvae cannot be found in stool specimen unless they are left at ambient temperature for a day or more.Education, improved sanitation and controlled disposal of human feces are important. Wearing shoes in endemic areas can reduce the prevalence of infection as well. Ancylostoma duodenale can be treated with albendazole, mebendazole and benzimidazoles. Pyrantel pamoate is an alternative. In severe cases of anemia, blood transfusion may be necessary.
Necator Americanus
Necator americanus has a cylindrical body, and a cuticle with three main outer layers made of collagen and other compounds, secreted by the epidermis. The cuticle layer protects the nematode so it can invade digestive tracts of animals. Eggs range in size from 65-75 micrometers x 36-40 micrometers and are virtually indistinguishable from those of Ancylostoma duodenale, another common hookworm. Necator americanus has four larval stages. The first stage is referred to as rhabditiform larvae because the esophagus has a large bulb separated from the rest of the esophagus by a region called the isthmus. The third stage is referred to as filariform larvae because the esophagus has no bulb. Adult females range in size from 9 mm to 11 mm while the smaller males range in size from 7 mm to 9 mm. The mouth of the adults has two pair of cutting plates, one dorsal and the other ventral. The males of the species are characterized by fused spicules found on the bursa. The common name "hookworm" comes from the dorsal curve at the anterior end. This worm starts out as an unembryonated egg in the soil. After 2448 hours under favorable conditions, the eggs become embryonated and hatch. This first juvenile stage 1 is known as 'rhabditiform'. The rhabditiform larvae grow and molt in the soil, transforming into a juvenile stage 2. The juvenile stage 2 molts once more until reaching the juvenile 3 stage, which
is also called 'filariform'; this is also the infective form. The transformation from rhabditiform to the filariform usually takes five to 10 days. This larval form is able to penetrate human skin, travel through the blood vessels and heart, and reach the lungs. Once there, they burrow through the pulmonary alveoli and travel up the trachea, where they are swallowed and are carried to the small intestine, where they mature into adults and reproduce by attaching themselves to the intestinal wall, causing an increase of blood loss by the host. The eggs end up on the soil after leaving the body through the feces. On average, most adult worms are eliminated in one to two years. When adult worms attach to the villi of the small intestine, they suck on the host's blood, which may cause abdominal pain, diarrhea, cramps, and weight loss that can lead to anorexia. Heavy infections can lead to the development of iron deficiency and hypochromic microcytic anemia. This form of anemia in children can give rise to physical and mental retardation. Infection caused by cutaneous larvae migrans, a skin disease in humans, is characterized by skin ruptures and severe itching.The most common technique used to diagnose a hookworm infection is to take a stool sample, fix it in 10% formalin, concentrate it using the formalin-ethyl acetate sedimentation technique, and then create a wet mount of the sediment for viewing under a microscope. However, the eggs of A. duodenale and N. americanus cannot be distinguished; thus, the larvae must be examined to identify these hookworms. An infection of N. americanus parasites can be treated by using benzimidazoles, albendazole, and mebendazole. A blood transfusion may be necessary in severe cases of anemia.
Ancylostoma Ceylanicum
Eggs are passed in the stool , and under favorable conditions (moisture, warmth, shade), larvae hatch in 1 to 2 days. The released rhabditiform larvae grow in the feces and/or the soil , and after 5 to 10 days (and two molts) they become filariform (third-stage) larvae that are infective . These infective larvae can survive 3 to 4 weeks in favorable environmental conditions. On contact with the human host, the larvae penetrate the skin and are carried through the blood vessels to the heart and then to the lungs. They penetrate into the pulmonary alveoli, ascend the bronchial tree to the pharynx, and are swallowed . The larvae reach the small intestine, where they reside and mature into adults. Adult worms live in the lumen of the small intestine, where they attach to the intestinal wall with resultant blood loss by the host . Most adult worms are eliminated in 1 to 2 years, but the longevity may reach several years. Necator americanus predominates in the Americas and Australia, while only.Iron deficiency anemia (caused by blood loss at the site of intestinal attachment of the adult worms) is the most common symptom of hookworm infection, and can be accompanied by cardiac complications. Gastrointestinal and nutritional/metabolic symptoms can also occur. In addition, local skin manifestations ('ground itch') can occur during penetration by the filariform (L3) larvae, and respiratory symptoms can be observed during pulmonary migration of the larvae.Treatment: albendazole, Mebendazole, or pyrantel pamoate.
Ancylostoma Braziliense
Males measure 7.5 to 8.5 mm. Females measure 9 to 10.5 mm. The buccal capsule has one pair of small medium teeth and one of larger outer teeth. Hosts: Definitive: dog (Canis Familiaris), Cat (Felis catus).Eggs are passed in feces. Larvae develop in soil to the L3 infective stage and then are ingested by the host or they enter the host through cutaneous contact and then the larvae migrate to the lungs, and then on to the intestinal tract of the host. In the intestinal tract, the larvae develop into adults. Eggs are then expelled in feces and the cycle continues.Eggs are found in fecal flotation,Eggs are 60 x 40 um. Puppies and kittens: Anemia, diarrhea, weight loss, weakness, poor growth, occasionally death. Adults: Usually asymptomatic but any of the above symptoms may be present. Treatment: Febantel, Febantel/Pyrantel embonate, Fenbendazole, Ivermectin,Mebendazole, Milbemycin oxime, Pyrantel Pamoate
Ancylostoma caninum
Ancylostoma caninum is usually gray, but appears reddish if there is blood in its alimentary canal. The body is covered by a non-living cuticle that sheds at molts allowing for growth of the nematode. A male is 10 to 12 mm long and 0.36 mm wide; a female is 14 to 20 mm long by 0.5 mm wide and has a pointed tail. The anterior end is bent dorsally so that the arrangement of the hookworm's ventral and dorsal sides are reversed. In the head of the hookworm is an area called the buccal capsule which contains one the mouth and teeth. Ventrally, there is one pair of teeth, each with three points. In the depth of the capsule there is a pair of triangular dorsal teeth and a pair of ventro-lateral teeth. At its posterior end, a male A. caninum has a prominent bursa. The rays inside the bursa are used in identifying species of hookworms, so A. caninum has a particular arrangement of rays in its bursa. The female reproductive organ, the vulva, is found near the junction of the second and last thirds of the body.
Hosts:Definitive: Dog (Canis familiaris) Paratenic: Rodents The larval stage penetrates the skin and makes it way through the circulatory system into the digestive tract, where adult forms lay eggs that are passed through the feces. Common symptoms include anemia and diarrhea. The parasite can also affect humans. It occasionally develops into an adult to cause eosinophilic enteritis in people, and their invasive larvae can cause an itchy rash called cutaneous larva migrans. Vaccination may soon be possible. Parasites are dioecious, with male and female organs in separate individuals.Following copulation, female lays her eggs in the hosts intestine. Eggs are passed out in the host feces.Usual daily output of eggs for a single female hookworm is between 10,000 and 30,000 eggs. In favorable conditions of moisture, temperature, and oxygen, eggs develop in the soil and hatch when they reach maturity. They release a rhabditiform larva which feeds for a short time and molts twice before becoming an infective filariform larva.Larva enters the host either by being swallowed or by burrowing into the skin through hair follicles. In the case of pregnant bitches, larvae may enter the fetus and infect prenatally.When it reaches the small intestine of the host, the larva molts a fourth and final time and develops to maturity in about five weeks.
Plasmodium Falciparum
The preferred method to diagnose malaria and determine which species of Plasmodium is causing the infection is by examination of a blood film under microscope in a laboratory. Each species has distinctive physical characteristics that are apparent under a microscope. In P. falciparum, only early (ring-form) trophozoites and gametocytes are seen in the peripheral blood. On occasion, faint, comma-shaped, red dots called "Maurer's dots" are seen on the red cell surface. The commashaped dots can also appear as pear-shaped blotches. Malaria is carried by Anopheles mosquitoes. Of the over 400 Anopheles species, only 3040 can transmit malaria. The infection starts, when a female mosquito injects (in her saliva) "sporozoites" (one form of P. falciparum) into human skin while taking a blood meal. A sporozoite travels (in the bloodstream) into the liver where it invades a liver cell. It matures into a "schizont" (mother cell) which produces 3000040000 "merozoites" (daughter cells) within six days. The merozoites burst out and invade red blood cells. Within two days one merozoite transforms into a trophozoite, then into a schizont and
finally 824 new merozoites burst out from the schizont and the red cell as it ruptures. Then the merozoites invade new red cells. P. falciparum can prevent an infected red cell from going to the spleen (the organ where old and damaged red cells are destroyed) by sending adhesive proteins to the cell membrane of the red cell. The proteins make the red cell to stick to small blood vessel walls. This poses a threat for the human host since the clustered red cells might create a blockage in the circulation system. A merozoite can also develop into a "gametocyte" which is the stage that can infect a mosquito. There are two kinds of gametocytes: males (microgametes) and females (macrogametes). They get ingested by a mosquito, when it drinks infected blood. Inside the mosquito's midgut, male and female gametocytes merge into "zygotes" which then develop into "ookinetes." The motile ookinetes penetrate the midgut wall and develop into "oocysts." The cysts eventually release sporozoites, which migrate into the salivary glands where they get injected into humans. The development inside a mosquito takes about two weeks and only after that time can the mosquito transmit the disease. P. falciparum cannot complete its life cycle at temperatures below 20 C. After being bitten by an infected mosquito, symptoms usually begin within 1030 days. Malaria is usually diagnosed by examining a blood sample under a microscope. Treatment: artemesinin,atovaquone-proguanil,chloroquine,doxycycline,mefloquine,quinine
Plasmodium vivax
The infection of Plasmodium vivax takes place in human when an infected female anopheles mosquito sucks blood from a healthy person. During feeding, the mosquito injects saliva to prevent blood clotting (along with sporozoites), thousands of sporozoites are inoculated into human blood; within a half-hour the sporozoites reach the liver. There they enter hepatic cells, transform into the tropozoite form and feed on hepatic cells, and reproduce asexually. This process gives rise to thousands of merozoites (plasmodium daughter cells) in the circulatory system and the liver. The P. vivax sporozoite enters a hepatocyte and begins its exoerythrocytic schizogony stage. This is characterized by multiple rounds of nuclear division without cellular segmentation. After a certain number of nuclear divisions, the parasite cell will segment and merozoites are formed. The parasite uses the Duffy blood group antigens (Fy6) to penetrate red blood cells. This antigen does not occur in the majority of humans in West Africa .As a result P. vivax occurs less frequently in West Africa. The parasitised red blood cell is up to twice as large as a normal red cell and Schffner's dots (also known as Schffner's stippling or Schffner's granules) is seen on the infected cell's surface, the spotted appearance of which varies in color
from light pink, to red, to red-yellow, as coloured with Romanovsky stains. The parasite within it is often wildly irregular in shape (described as "amoeboid"). Schizonts of P. vivax have up to twenty merozoites within them. It is rare to see cells with more than one parasite within them. Plasmodium Malariae
The primary mode of transmission from host to host by these four species uses a female Anopheles mosquito as a vector. The life cycle is initiated when the mosquito vector injects sporozites into the human hosts during a blood-meal. The sporozites then migrate to the liver, where they reproduce asexually and produce merozites. These merozites then enter the bloodstream and infect erythrocytes, becoming trophozoites. The period of time that the trophozoites are enlarging is called the trophic period, and this ends when several divisions occur, but none of these cycles go through the cytokinesis stage, forming what is called a schizont. The erythrocyte then lyses, introducing new merozites into the blood cycle and starting the cycle over again, until an uninfected Anopheles mosquito takes a blood-meal from the infected host, and transmits the infection to another host. The main physical manifestations of malaria in a human host are febrile attacks that are known as malarial paroxysms. These symptoms appear during the blood stage of the life cycle; no symptoms will appear during other stages. The severity of the infection depends on the infecting species of Plasmodium and the health of the host prior to
infection.The preferable method for diagnosis of P. malariae is through the examination of peripheral blood films stained with Giemsa stain.P. malariae is the only human malaria parasite that causes fevers that recur at approximately three-day intervals (therefore occurring evey fourth Plasmodium Ovale
While it is frequently said that P. ovale is very limited in its range being limited to West Africa, the Philippines, eastern Indonesia, and Papua New Guinea., it has been reported from Bangladesh, Cambodia, India,Thailand and Vietnam..The P. ovale sporozoite enters a hepatocyte and begins its exoerythrocytic schizogony stage. This is characterized by multiple rounds of nuclear division without cellular segmentation. After a certain number of nuclear divisions, the parasite cell will segment and merozoites are formed. There are situations where some of the sporozoites do not immediately start to grow and divide after entering the hepatocyte, but remain in a dormant, hypnozoite stage for weeks or months. The duration of latency is variable from one hypnozoite to another and the factors that will eventually trigger growth are not known; this explains how a single infection can be responsible for a series of waves of parasitaemia or "relapses".While similar to P. vivax, P. ovale is able to infect individuals who are negative for the Duffy blood group, which is the case for many residents of sub Saharan Africa. This explains the greater prevalence of P. ovale (rather than P. vivax) in most of AfricaThe prepatent period in the human
ranges from 12 to 20 days. Some forms in the liver have delayed development and relapse may occur after periods of up to 4 years after infection. Standard treatment is concurrent treatment with chloroquine and primaquine.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Prescott Harley Klein's Microbiology 7th EditionDocument37 pagesPrescott Harley Klein's Microbiology 7th EditionJendri Mamangkey-kossoh25% (4)
- Test Bank For Biology The Essentials 3rd EditionDocument8 pagesTest Bank For Biology The Essentials 3rd EditionKristi Markus100% (35)
- NOTESmtlaws LectureDocument11 pagesNOTESmtlaws LectureCes Manga100% (1)
- NotesCM (CEFI)Document30 pagesNotesCM (CEFI)Ces MangaNo ratings yet
- Books OverviewDocument10 pagesBooks OverviewCes MangaNo ratings yet
- The Measurement of Blood PressureDocument2 pagesThe Measurement of Blood PressureCes MangaNo ratings yet
- Animal Behavior Biological RhythmsDocument3 pagesAnimal Behavior Biological RhythmsAlok PatraNo ratings yet
- Yeast Make-Accumulate-Consume'' Life Strategy Evolved As A Multi-Step Process That Predates The Whole Genome DuplicationDocument12 pagesYeast Make-Accumulate-Consume'' Life Strategy Evolved As A Multi-Step Process That Predates The Whole Genome DuplicationdaveNo ratings yet
- Descriptive Text and A Diagram or Plan, Which You Have To Label According To TheDocument6 pagesDescriptive Text and A Diagram or Plan, Which You Have To Label According To TheJoanna BinanNo ratings yet
- The Role of Insulin in Maintaining Blood Glucose HomeostasisDocument2 pagesThe Role of Insulin in Maintaining Blood Glucose HomeostasisyaniqueNo ratings yet
- La Signifiance GnayoroDocument15 pagesLa Signifiance GnayorojeuneppNo ratings yet
- Animal Behaviour - Syamala Devi Natarajan - 1Document21 pagesAnimal Behaviour - Syamala Devi Natarajan - 1Syamala NatarajanNo ratings yet
- Ncku Courses Taught in English, AY2018-19: White Background: Undergraduate Level Gray Background: Graduate LevelDocument17 pagesNcku Courses Taught in English, AY2018-19: White Background: Undergraduate Level Gray Background: Graduate Levelasistensi varaNo ratings yet
- 19 Soft Tissue Tumors by DR NazishDocument55 pages19 Soft Tissue Tumors by DR NazishAhmed YTNo ratings yet
- Kalyanaraman B, 2013 - Teaching The Basic of Redox BiologyDocument14 pagesKalyanaraman B, 2013 - Teaching The Basic of Redox BiologyAnia Scholastika PutriNo ratings yet
- Surgical Pathology of Liver TumorsDocument480 pagesSurgical Pathology of Liver TumorsGeorgiana BuhociNo ratings yet
- Lesson 4 The Nucleus and DNA Organization and PBL Write Shops 5 6Document15 pagesLesson 4 The Nucleus and DNA Organization and PBL Write Shops 5 6Macky IbayNo ratings yet
- Oliveira Et Al. 2003Document8 pagesOliveira Et Al. 2003la_lu_izaNo ratings yet
- Nutrient Cycles: Answer The Questions BelowDocument7 pagesNutrient Cycles: Answer The Questions BelowNunuNo ratings yet
- 18 JL 7Document15 pages18 JL 7Irma SihotangNo ratings yet
- 17 BioDocument3 pages17 Biomuskan FatimaNo ratings yet
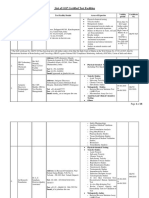
- List of GLP Certified Test FacilitiesDocument18 pagesList of GLP Certified Test FacilitiesBhushanNo ratings yet
- Biomedical Applications of CollagenDocument22 pagesBiomedical Applications of Collagenkiks123No ratings yet
- Tumour VirusesDocument57 pagesTumour VirusesCharles TownsendNo ratings yet
- 3rd Grading Exam ScienceDocument4 pages3rd Grading Exam ScienceRussel OchoNo ratings yet
- To Life Science: Maryrose Mallorca Peter Joedale Daling John Carlo Santiago "Pogi"Document33 pagesTo Life Science: Maryrose Mallorca Peter Joedale Daling John Carlo Santiago "Pogi"Jhen BonNo ratings yet
- Chemistry Education Research and Practice: Accepted ManuscriptDocument55 pagesChemistry Education Research and Practice: Accepted ManuscriptMusic HitzNo ratings yet
- Ethics in Behavioral GeneticsDocument8 pagesEthics in Behavioral GeneticsLavinia MariaNo ratings yet
- Bio 111 Biomolecules and CellsDocument2 pagesBio 111 Biomolecules and CellsDerrickNo ratings yet
- Brock Biology of MicrooDocument6 pagesBrock Biology of MicrooÇağla Koca100% (1)
- DR Vidya SagarDocument7 pagesDR Vidya SagarAnil KumarNo ratings yet
- Carbohydrates: Why Are Carbohydrates Important?Document4 pagesCarbohydrates: Why Are Carbohydrates Important?ir123No ratings yet
- Stem Cell Based Therapy Option in COVID-19 - Is It Really Promising?Document17 pagesStem Cell Based Therapy Option in COVID-19 - Is It Really Promising?diana.alyNo ratings yet
- Kelompok 2 - Keuntungan SSFDocument7 pagesKelompok 2 - Keuntungan SSFVirga ArgaNo ratings yet