Professional Documents
Culture Documents
Normal Changes With Aging in The Cardiovascular System
Uploaded by
SheenarieOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Normal Changes With Aging in The Cardiovascular System
Uploaded by
SheenarieCopyright:
Available Formats
Cardiovascular System - Normal Aging The cardiovascular system is composed of the heart, the blood and the vasculature.
This system subserves many functions, most notably the delivery of oxygen throughout the body. The cardiovascular system also serves as a roadway for delivering: 1. 2. 3. 4. 5. 6. energy containing molecules like sugars and fats to needy tissues, amino acids and nucleic acids for the synthesis of new proteins and DNA, toxins and waste to the kidneys for elimination from the body, hormonal messages to distant target tissues, immune system cells to the site of foreign molecules, blood to and from the surface of the skin for regulating body temperature.
Each of these functions is minimally affected by age, but they can be severely altered by interactions that occur between aging and age-related diseases in the cardiovascular system. Before we attempt to dissect out the physiological changes that can be accounted for by aging, we need to eliminate from the sample individuals experiencing varying degrees of disease. Human studies of cardiovascular aging are limited by the prevalence of occult coronary stenosis, with 60% of men over the age of 60 having a 75-100% block in at least one coronary artery. Through rigorous screening of coronary disease and elimination of those with coronary artery disease, it has been demonstrated that cardiovascular reserve capacity decreases with aging. These changes in cardiovascular function can be explained by changes in cardiac muscle, connective tissue, cardiac adrenoreceptors, and the compliance or distensibility of the vasculature. In addition, there are changes in kidney function which can alter fluid homeostasis and contribute to age-dependent reactions to therapies for cardiovascular conditions. The Heart The contractile muscle of the heart is made up of a special type of cell referred to as a cardiac myocyte. These highly contractile cells have an enormous appetite for oxygen and glucose. These cells never rest, from the day of fetal formation to the last day of your life. The cardiac myocyte is also unique in that it is electrically coupled to neighboring cardiac myocytes. This property facilitates the simultaneous contraction of all myocytes during either atrial or ventricular systole (systole is the contracted state of heart muscle). There are numerous arteries that go directly from the aorta (the first major blood vessel leaving the left ventricle) to the heart to ensure the rapid delivery of oxygen and glucose to working cardiac muscle. These blood vessels are called the coronary arteries. There is an intrinsic, self-sustaining mechanism (a pace maker) that sets the strength of each contraction and the number of heart beats per minute, but both of these can be modulated by hormones and neurotransmitters found within the body. Aging in the Heart With aging, a few functions are preserved. For example, the cardiac output (the amount of blood pumped per minute) is not changed. But the efficiency of pumping the blood does change. More blood is left in the heart after a contraction, the thickness of the major pump, the left ventricle is increased and the response to stimulation of the heart rate is diminished. As a result, the maximum heart rate decreases with aging. Therefore, when we exercise, the maximum heart rate decreases by 1 for each year of aging (i.e., maximum heart rate at 20 is 200 and at 70 is 150). Functionally, these "normal" age-related changes are unlikely to compromise everyday living, but they will reduce the maximal performance. This can occur due to the demands placed upon the cardiovascular system during competitive exercise are greater in old age. The Vasculature The aorta and much of the arterial tree function as an elastic buffering chamber that act to dissipate the pressure wave resulting from ventricular contraction (systole). During diastole (resting state of the heart), the large arteries supply the volume of blood to the periphery as a continuous peripheral blood flow. The diameter of the individual arteries steadily decreases as you move away from the heart. With each successive branching of the artery the diameter decreases, but the sum of the cross sectional areas of these branches gradually increases and, thus, the rate of blood flow and blood pressure diminishes as the blood approaches the capillaries. The arteries and veins are multi-layered cylinders, with each layer serving specific functions. The thickness of each layer is far greater in the arteries, however.
Blood Pressure (on the average)
for
Average,
Aged,
and
Diseased
Arteries
At Maximum Animated Rest Flow Diagram Average 80 Aged 110 Average Artery Aged Artery Diseased Artery 110 140
Comparison Click here for Comparison
Diseased 110 180 Vascular Changes with Aging
With aging, there is a thickening of the artery walls. In hypertension, these normal age-related increases in the large arteries are enhanced. The generic term, arteriosclerosis, refers to a thickening and hardening of the arterial wall. Taken together, these agerelated changes all contribute to an increase in systolic blood pressure, which makes age a risk factor for hypertension. http://www.usc.edu/dept/gero/AgeWorks/core_courses/gero500_core/biology_a_lect/index_a.htm Normal Function The respiratory system is a conduit for the exchange of gases between the external environment and our blood. When we think about respiration we focus our attention upon the need to replenish our bodies with oxygen, but another important function is the maintenance of blood carbon dioxide levels and the effect carbon dioxide homeostasis has an blood pH. The organ for gas exchange is the lung, located deep within our bodies. Gases travel through our mouth and nose into the tracheobronchial tree which divides into millions of minute branches terminating in structures known as alveoli. The alveoli are made-up of an incredibly delicate membrane that serves as a fragile barrier between the outside world and our blood. Fragile is the operative word, since life-style choices like smoking or anything that allows the entry of small particles into the lungs can severely damage the membrane and compromise the ability to exchange gases across the pulmonary membrane. The trunk of the pulmonary tree is the trachea, which divides into two main branches referred to as bronchi. Each bronchi undergoes repeated branchings as bronchioles. The terminal bronchioles branch into alveolar ducts (2-11 ducts) which in turn terminate into alveolar sacs that have 2 or more alveoli. There are approximately 300 million alveoli in the adult lung. Each alveoli is intimately coated with capillaries specialized for the movement of gases into the bloodstream. The combined thickness of the alveolar epithelium and the capillary endothelium is less than 0.2 m (10-6 meters). An incredibly thin layering of membranes that has evolved to maximize the diffusion of gases between the environment and the blood. The alveoli are the only site for gas exchange in the lung and a key component to maintaining their structure is the secretion of a thin coating of fat (phospholipids) along their outer surface. This coating is known as surfactant and it functions to oppose the natural tendency of bubbles like alveoli to collapse from the surface tension that exists between water and air. The movement of air in and out of the lungs is voluntarily controlled by messages sent from the brain (medulla) to number of muscle groups, with the lungs acting passively like large rubber balloons. Enlargement of the chest (thorax) during inspiration is produced by a contraction of the diaphragm muscle, located below the lung, and a contraction of the intercostal and pectoral muscles which are attached to the rib cage. We exhale by simply allowing these muscles to relax and relying upon the numerous elastic fibers found within the lungs. This passive elasticity allows the lung to recoil to its smaller resting volume. The elastic recoil creates a net positive pressure within the lung to force a percentage of the lung air out. It is this elastic recoil that is most compromised in "successful aging" and as we will see later, it decreases the delivery of new oxygen and the removal of carbon dioxide. Evaluation of the functional movements of the lung are performed by respiratory therapists. You will be asked to inhale from and exhale into a tube connected to a spirometer (or pneometer) that functions to measure the volumes of air moving in and out of the lung. The following definitions of lung volumes come from such spirometric examinations: Tidal Air: the volume of air that enters and leaves the lungs during a resting breathing pattern. Inspiratory Reserve Volume: the volume of air taken in by a maximal inspiration that is over and above the tidal volume.
Forced Vital Capacity: the sum of the tidal volume and the inspiratory reserve volume. Expiratory Reserve Volume: the volume of air that can be expelled by the most powerful expiratory effort after the tidal volume has escaped naturally. Forced Expiratory Volume: the sum of the tidal volume and the expiratory reserve volume. Vital Capacity: the sum of the tidal air and the inspiratory and expiratory reserves (the volume of air expelled by the most vigorous expiratory effort after the deepest possible inspiration). Residual Volume: the volume of air remaining in the lungs after the strongest possible expiration. Total Lung Capacity: the sum of the vital capacity and the residual volume. Functional Residual Capacity: the volume of air left in the lungs at the end of a normal resting, unforced expiration. omparison of Normal and Aged Lung Function
The BLUE represents the amount of air inhaled at any time by a person. The RED represents the Lungs. The PINK (below the Lungs) represents the diaphram.
Aging and Respiration Changes in pulmonary function with age are critical, since severe impairment is a direct risk for death. Aging not only affects ventilation and gas exchange within the lungs, but through compromise in another physiological system -the immune system, it also decreased the ability of the lungs to defend against infectious diseases and toxic insults. In the worst case scenario, the combined effect of age and chronic or acute insults can lead to airway obstruction which increases the risk for death due to: Chronic obstructive pulmonary disease Cardiovascular disease Heart disease Stroke Diabetes mellitus Lung cancer Mechanical Changes
Age-related changes in pulmonary function, independent of disease or a history of environmental insults, can be accounted for by 1) decreases in lung elasticity, 2) decreases in chest compliance (stiffening of chest wall) and 3) a decrease in the strength of the inspiratory muscles (diaphragm, intercostals, pectorals). The decrease in lung elasticity is due to the generalized decrease in the turnover and function of the protein elastin throughout the body and the loss of elastic fiber attachments within the lungs. This change in the elastic recoil underlies the age-related increase in residual volume and the decrease in vital capacity. Which means: more stale air remains in the lungs and less fresh air is brought in with each breath.
The decrease in chest compliance is due to an ossification (calcification) of cartilage and rib articulations. The decrease in strength of respiratory muscles is due to a general age-related loss of skeletal muscles fibers with age (see musculoskeletal system in week 8). These later changes contribute significantly to the age-related change in forced expiratory volume. All of the air flow measures reach a stable maximum between the ages of 20-25 in both sexes. Thereafter linear declines tend to occur, although changes due to attrition of respiratory system tissue are not accountable until age 40. Diffusional Changes Age-related decreases in alveolar surface area contribute to a decrease in blood oxygenation. This change is due to a partial collapse of the most distal (peripheral) airways entering the alveoli. These changes can result in a mismatch between the ventilation of the lung and the perfusion of the lung capillaries with blood. This mismatch decreases the diffusion of oxygen into the blood and the movement of carbon dioxide out of the blood. This change is further exacerbated by decreases in cardiac output, which together result in a lowered arterial oxygen content. The control center for breathing lies deep in the brain in a structure called the medulla. The medullas receives information on blood oxygen and carbon dioxide content from specialized nerve cells known as chemoreceptors located peripherally in nodules known as the carotid and aortic bodies (located on the aorta and carotid artery). There is also evidence that neurons within the medulla react to changes in cerebral spinal fluid pH secondary to hypercapnia (elevated carbon dioxide content). Together, these chemodetectors generate a response which increases both heart and ventilatory rates. With age there is a decrease in these detectors or receptors and thus the response to hypoxia or hypercapnia is diminished as much as 50% in healthy older subjects (65-75 years). Defense Mechanisms We use mucus secretion to collect inhaled particulate matter and then we expel the mucus through the motion of ciliated cells found within the bronchioles. When the cilia are overloaded, we rely upon the cough mechanism to expel the mucus. With age, this clearance system is decreased leaving our lung vulnerable to damage associated with mucus obstructions. The cough reflex is further subdued by sedative use and neurologic disease, which are common in the elderly. Once our initial defense mechanism of mucus has been penetrated, we rely upon our immune system to eliminate foreign bodies. As discussed in the immune system section of the course, we have an impaired immune response as we get older that leaves the elderly easier targets to infectious disease in the lungs (i.e. pneumonia and tuberculosis).
Source: Tabloski, P. (2006). Essentials of Gerontological nursing. Singapore: Pearson Education South Asia Pte Ltd.
You might also like
- Circulatory System: A Tutorial Study GuideFrom EverandCirculatory System: A Tutorial Study GuideRating: 5 out of 5 stars5/5 (3)
- Circulatory System of MammalsDocument10 pagesCirculatory System of Mammalsben-jNo ratings yet
- Circulation and Cardiovascular SystemDocument12 pagesCirculation and Cardiovascular SystemSatria MandalaNo ratings yet
- Cardiac Control CentreDocument8 pagesCardiac Control CentregeorgeloxdaleNo ratings yet
- Note On Pressure Flow and ResistanceDocument43 pagesNote On Pressure Flow and ResistanceSilver FestusNo ratings yet
- Transport in Man NotesDocument9 pagesTransport in Man NotesYeo JhNo ratings yet
- Circulatory System and Heart Biology Summarisation.Document5 pagesCirculatory System and Heart Biology Summarisation.Jumana ElkhateebNo ratings yet
- Physical Therapy in Cardiovasculer and Pulmonary Conditions: Dila Rahmawati Meri Pita Lokasari Rika RachmahaniDocument31 pagesPhysical Therapy in Cardiovasculer and Pulmonary Conditions: Dila Rahmawati Meri Pita Lokasari Rika RachmahaniDilah RahmaNo ratings yet
- Ana and Pys Note 3Document11 pagesAna and Pys Note 3bashir auwalNo ratings yet
- The Circulatory SystemDocument51 pagesThe Circulatory SystemMohammed ahmedNo ratings yet
- Cardiovascular System - Lecture IIDocument5 pagesCardiovascular System - Lecture IIpragantraNo ratings yet
- CV PathoDocument32 pagesCV PathoSaif AliNo ratings yet
- KS3 Science Year 9 The Circulatory System-2Document15 pagesKS3 Science Year 9 The Circulatory System-2f72ktyd78nNo ratings yet
- Biology Unit 1Document11 pagesBiology Unit 1Islam ElsayedNo ratings yet
- ReviewerDocument10 pagesReviewerMaybelyn Rivera PagkatotohanNo ratings yet
- POINTERS-SCIENCE Grade 9 Quarter 1Document7 pagesPOINTERS-SCIENCE Grade 9 Quarter 1Lunyl DelloNo ratings yet
- SystemDocument3 pagesSystemJanina MaligayaNo ratings yet
- The Pathway: The Human Respiratory SystemDocument25 pagesThe Pathway: The Human Respiratory SystemKenneth Decker PrietoNo ratings yet
- Physiology of Cardiovascular System 1 2 Term: ST NDDocument14 pagesPhysiology of Cardiovascular System 1 2 Term: ST NDalialnema67No ratings yet
- Circulation or Peripheral CirculationDocument3 pagesCirculation or Peripheral CirculationOldy MutiaraNo ratings yet
- Anatomy & PhysiologyDocument57 pagesAnatomy & PhysiologyBrittanie MouzonNo ratings yet
- Chapter III - Cardiovascular System: Blood PressureDocument5 pagesChapter III - Cardiovascular System: Blood PressureIndranil SinhaNo ratings yet
- 8Qghuzdwhu3K/Vlrorj/: 3-1 PurposeDocument54 pages8Qghuzdwhu3K/Vlrorj/: 3-1 PurposejaimeNo ratings yet
- Human Circulatory System: The HeartDocument8 pagesHuman Circulatory System: The HeartRocheal WhittinghamNo ratings yet
- Chapter 42 Reading GuideDocument5 pagesChapter 42 Reading GuideCaleb SchantzNo ratings yet
- Circulatory SystemDocument7 pagesCirculatory SystemWisdom DzombeNo ratings yet
- The Circulatory SystemDocument10 pagesThe Circulatory SystemRezki RasyakNo ratings yet
- CHP 05 (Blood and Circulation) DrRiyadAhmed PC 3Document69 pagesCHP 05 (Blood and Circulation) DrRiyadAhmed PC 3Kamrun NaherNo ratings yet
- Transport in Animals-Topic 9Document14 pagesTransport in Animals-Topic 9sukiiNo ratings yet
- Cardio 1Document4 pagesCardio 1Liam Jacque LapuzNo ratings yet
- The Human Heart: Location, Size and ShapeDocument9 pagesThe Human Heart: Location, Size and ShapeL I G-Arijit HisabiaNo ratings yet
- Circulatory System SystemDocument4 pagesCirculatory System Systemleah rualesNo ratings yet
- Pathophysiology of Cardiovascular System Arterial Hypertension Heart ArrhythmiasDocument38 pagesPathophysiology of Cardiovascular System Arterial Hypertension Heart ArrhythmiasLunguVictoriaNo ratings yet
- Science 9 ReviewerDocument7 pagesScience 9 ReviewerArgie MabagNo ratings yet
- 8 Transport in AnimalsDocument24 pages8 Transport in AnimalsMariam ShehabNo ratings yet
- Cardiac CycleDocument3 pagesCardiac CycleKhadijah HabeebahNo ratings yet
- Functional Organization of Cardiovascular SystemDocument19 pagesFunctional Organization of Cardiovascular SystemIbtesam Mohammed100% (2)
- Anaphy Heart and LungsDocument7 pagesAnaphy Heart and Lungsbryan leguiabNo ratings yet
- 565656Document61 pages565656Bashar AntriNo ratings yet
- Cardiovascular SystemDocument5 pagesCardiovascular SystemDaniel PancuNo ratings yet
- Transport in AnimalsDocument12 pagesTransport in AnimalsJedidiah DickNo ratings yet
- Cardiovascular System Lecture 1 2020 2021Document5 pagesCardiovascular System Lecture 1 2020 2021olawandeilo123No ratings yet
- 5.2 Transport in HumansDocument11 pages5.2 Transport in Humans박찬우No ratings yet
- BIO2 - 4.04 - ANIMAL GAS EXCHANGE AND CIRCULATION (v.2023 WITH VITAL SIGN MONITORING)Document80 pagesBIO2 - 4.04 - ANIMAL GAS EXCHANGE AND CIRCULATION (v.2023 WITH VITAL SIGN MONITORING)MARKIEL JUSTINE DOMOSMOGNo ratings yet
- Candon City, Ilocos Sur Grade 9 Reviewer School Year 2021 - 2022Document7 pagesCandon City, Ilocos Sur Grade 9 Reviewer School Year 2021 - 2022Aleah TungbabanNo ratings yet
- CirculationDocument9 pagesCirculationakkaranniNo ratings yet
- Physiology of Cardiovascular SystemDocument19 pagesPhysiology of Cardiovascular SystemDavid JishkarianiNo ratings yet
- BMAT Biology Revision NotesDocument9 pagesBMAT Biology Revision Notesmissymar123100% (5)
- Anatomy of The Heart: Epicardium Myocardium EndocardiumDocument8 pagesAnatomy of The Heart: Epicardium Myocardium EndocardiumTrishna ShahNo ratings yet
- Clinical PaperDocument18 pagesClinical Paperapi-356406300No ratings yet
- Biology - Circulatory System Notes 1Document13 pagesBiology - Circulatory System Notes 1archit.kulkarni7756No ratings yet
- Circulatory System Research PaperDocument6 pagesCirculatory System Research Papergbjtjrwgf100% (1)
- Cnat AllDocument7 pagesCnat AllZaid Bin salmanNo ratings yet
- Anatomy and PhysiologyDocument6 pagesAnatomy and PhysiologybrowneyesgirltooNo ratings yet
- Topic 1 NotesDocument18 pagesTopic 1 NotesKesithan AnandarashNo ratings yet
- Circulatory SystemDocument21 pagesCirculatory SystemYusuf AzeezNo ratings yet
- Respiratory System: Nose and NostrilsDocument8 pagesRespiratory System: Nose and NostrilsKabang MoaNo ratings yet
- Operation of The Heart ValvesDocument10 pagesOperation of The Heart Valvesgadis_wawa267friendlyNo ratings yet
- Pulmonary CirculationDocument4 pagesPulmonary CirculationDr Md Abedur RahmanNo ratings yet
- Subcostal TAPSE - A Retrospective Analysis of A Novel Right Ventricle Function Assessment Method From The Subcostal Position in Patients With SepsisDocument8 pagesSubcostal TAPSE - A Retrospective Analysis of A Novel Right Ventricle Function Assessment Method From The Subcostal Position in Patients With SepsisblanquishemNo ratings yet
- October 2017 (IAL) MS - Unit 1 Edexcel Biology A-LevelDocument21 pagesOctober 2017 (IAL) MS - Unit 1 Edexcel Biology A-LevelCheung PhilaNo ratings yet
- AnaPhy Lab Exercise 24-41Document6 pagesAnaPhy Lab Exercise 24-41Angelyka Cabalo50% (2)
- PembahasanDocument32 pagesPembahasanwening gbNo ratings yet
- Animal Circulation and RespirationDocument56 pagesAnimal Circulation and Respirationacooper6No ratings yet
- Unit 1 New Syllabus NotesDocument69 pagesUnit 1 New Syllabus Notesmalak sherif100% (1)
- Arterial Line Analysis PresentationDocument35 pagesArterial Line Analysis PresentationLisa GilbertNo ratings yet
- Ati Teas 7 Biology ReviewDocument51 pagesAti Teas 7 Biology ReviewSAMUEL WAMNo ratings yet
- CNCQ Basic Reading Chapter 7Document10 pagesCNCQ Basic Reading Chapter 7Thiện NguyễnNo ratings yet
- Cardiovascular System AnatomyDocument54 pagesCardiovascular System AnatomyAyen LatosaNo ratings yet
- Hypertensive Heart Disease: A Proposed Clinical ClassificationDocument2 pagesHypertensive Heart Disease: A Proposed Clinical ClassificationireneaureliaNo ratings yet
- Etextbook PDF For Huszars Ecg and 12 Lead Interpretation 5th EditionDocument61 pagesEtextbook PDF For Huszars Ecg and 12 Lead Interpretation 5th Editioneve.sampson314100% (42)
- Acute Pericarditis: Clinical PracticeDocument8 pagesAcute Pericarditis: Clinical PracticeGaby Alejandra Ordonez AndradeNo ratings yet
- Senka Mesihovic-Dinarevic Lutvo Sporisevic Anes Joguncic, Chapter VIDocument23 pagesSenka Mesihovic-Dinarevic Lutvo Sporisevic Anes Joguncic, Chapter VIvaria5No ratings yet
- Biology 3rd ESO Full DossierDocument54 pagesBiology 3rd ESO Full DossierNinaNo ratings yet
- Circulatory System NotesDocument10 pagesCirculatory System Notesdanlayton75% (4)
- Cardiac MR (CMR) Imaging Planes and Pulse SequencesDocument60 pagesCardiac MR (CMR) Imaging Planes and Pulse SequencesmailandaredonaNo ratings yet
- Assessment of Left Ventricular Fraction by Real-Time,: Ejection and Volumes Two-DimensionalDocument8 pagesAssessment of Left Ventricular Fraction by Real-Time,: Ejection and Volumes Two-DimensionalAinil MardiahNo ratings yet
- Guideline Title: Intra-Aortic Balloon Pump ManagementDocument16 pagesGuideline Title: Intra-Aortic Balloon Pump ManagementJansen ChNo ratings yet
- Anatomy and Cardiovascular AssessmentDocument52 pagesAnatomy and Cardiovascular AssessmentNaomi Anne AsuntoNo ratings yet
- CVS System: Bader Al-Mukhtar - RCSI - SCDocument8 pagesCVS System: Bader Al-Mukhtar - RCSI - SCmuhammadridhwanNo ratings yet
- Module NCM112Document69 pagesModule NCM112Potato Banana100% (1)
- June 2014 (IAL) MS - Unit 1 Edexcel Biology A-LevelDocument22 pagesJune 2014 (IAL) MS - Unit 1 Edexcel Biology A-LevelCheung PhilaNo ratings yet
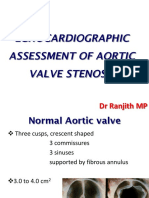
- Echocardiographic Assessment of Aortic Valve Stenosis DR RanjitDocument93 pagesEchocardiographic Assessment of Aortic Valve Stenosis DR RanjitNavojit ChowdhuryNo ratings yet
- JJDocument34 pagesJJJalil MujawarNo ratings yet
- Cardiac Physiology Dissertation IdeasDocument6 pagesCardiac Physiology Dissertation IdeasBuyAPhilosophyPaperUK100% (2)
- GENBIO REVIEWER - FinalsDocument6 pagesGENBIO REVIEWER - FinalsFiona CagolNo ratings yet
- Cardiac AssessmentDocument54 pagesCardiac AssessmentAthira PSNo ratings yet
- Snab AS Biology (Summary)Document23 pagesSnab AS Biology (Summary)BenNo ratings yet
- Pathophysiology On ArrhythmiaDocument34 pagesPathophysiology On ArrhythmiaYhr Yh100% (1)