Professional Documents
Culture Documents
The Pharmacology of Fentanyl and Its Impact On Pain Management
Uploaded by
Diamond DustOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Pharmacology of Fentanyl and Its Impact On Pain Management
Uploaded by
Diamond DustCopyright:
Available Formats
6/9/13
The Pharmacology of Fentanyl and Its Impact on Pain Management (printer-friendly)
www.medscape.org
Donald R. Taylor, MD, Medical Director, Comprehensive Pain Care P.C., Marietta, Georgia Disclosure: Donald R. Taylor, MD, has disclosed that he has served as an advisor or consultant to Cephalon.
The Pharmacology of Fentanyl and Its Impact on the Management of Pain
Donald R. Taylor, MD
Posted: 12/13/2005
Fentanyl was first synthesized in 1960 and found to be significantly more potent than commonly used opioids, such as morphine or meperidine. At the time, researchers were looking for more potent opioids because potency seemed to be directly related to safety. More potent drugs were believed to be safer because it was thought that at equianalgesic doses there would be fewer unbound molecules to affect sites not related to analgesia but responsible for respiratory depression and other side effects. Consistent with this concept, in animal studies, fentanyl had a much larger safety margin when compared with older opioids. The large safety margin, relatively short duration of action, and minimal respiratory depression at analgesic doses observed for fentanyl soon made it the drug of choice for intravenous anesthesia.[1] Its ability to provide cardiovascular stability and to block the stress response to surgical stimuli at high doses made it the mainstay of cardiac anesthesia. However, when used at high doses to suppress the stress response during surgery, significant respiratory depression results and postoperative mechanical ventilation are usually needed.[2] Although fentanyl is still used extensively in the perioperative period, the clinical features that have made fentanyl so successful in this setting have also made this drug a uniquely useful tool in the management of chronic pain. For this reason, fentanyl has moved out of the operating room and into the clinic. This column focuses on why lipid solubility makes fentanyl uniquely useful in treating persistent chronic pain (basal pain) and sudden flares of breakthrough pain (BTP). BTP, which is also called "incident pain" or "episodic pain," is defined as a transitory exacerbation of pain that occurs on a background of otherwise controlled chronic pain.[3-5]
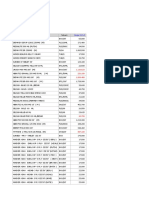
Lipid Solubility of Commonly Used Opioids
Of the clinically available pure mu agonists, fentanyl and sufentanil are the most lipid-soluble and morphine is the least lipid-soluble.[6] The octanol-water partition coefficient is a classic way of looking at the lipid solubility of drugs. The octanol-water partition coefficient for morphine is 6 and 9550 for fentanyl, thereby showing that fentanyl is highly lipid-soluble.[6] This difference in lipid solubility has profound effects on how we can use these 2 drugs in clinical practice.
www.medscape.org/viewarticle/518441_print 1/5
6/9/13
The Pharmacology of Fentanyl and Its Impact on Pain Management (printer-friendly)
Effects of Lipid Solubility on Drug Behavior
We normally think of fentanyl as short-acting and morphine as long-acting. However, the 2 drugs have similar elimination half-lives: 2-4 hours for morphine and 3-7 hours for fentanyl.[6] We often think of drug elimination as determining the duration of effect. However, morphine does not last longer than fentanyl because it is eliminated more slowly from the body; it lasts longer because once it enters the central nervous system it has a difficult time exiting the cellular lipid barrier (blood-brain barrier). It is this retention in the central nervous system that makes morphine longer-acting than fentanyl.[7] Because morphine is not very lipid-soluble, it takes a long time to cross the blood-brain barrier both going into and out of the brain. This produces what one might call a "slow-in, slow-out" drug. Indeed, when compared with lipid-soluble drugs, morphine is noted to be slower in onset. Fentanyl, on the other hand, is lipophilic and crosses the blood-brain barrier rapidly in both directions; it is a "fast-in, fast-out" drug. Therefore, fentanyl acts quickly and has a short duration of action because of its lipid solubility. Another factor that can play a role in how a drug behaves clinically is receptor affinity. If an opioid binds tightly to a mu receptor, it may have a surprisingly long duration of action. The mu receptor dissociation constant for fentanyl is 1.9 and 2.0 for morphine, indicating that they are very similar.[6] Because their elimination half-lives, as described above, and their mu receptor binding affinities are very similar, it is primarily differences in lipid solubility that govern the different behaviors of these 2 drugs. Lipid solubility not only confers the ability of fentanyl to pass readily through the blood-brain barrier ("fast-in, fastout"), but also to pass through other cellular barriers.[8,9] This ability to pass through cellular barriers and reach the capillary bed has led to the administration of fentanyl both by transdermal[10,11] and buccal[12] routes.
Transdermal Administration
Transdermal fentanyl has been established as a mainstay of chronic pain management in cancer and noncancer patients.[13-15] The first generation of transdermal fentanyl patches relied on simple diffusion of the drug down a concentration gradient. This simple diffusion results in a relatively slow delivery of fentanyl through the skin.[10] Thus, it takes about 16 hours after patch administration to achieve a clinically meaningful blood level,[16] and it takes about a week to achieve stable plasma levels.[17] This time course of action is acceptable for continuous chronic pain, but not for BTP or intermittent pain. New transdermal patch technology was recently developed that uses a small amount of iontophoretic electric current to drive fentanyl across the skin barrier. The application of the electric current drives the drug across the skin barrier much more rapidly than simple gradient-driven diffusion and allows for the treatment of BTP. Pushing a button on this transdermal system activates the current and drives a bolus of fentanyl across the skin. There is no continuous administration of fentanyl with these units; they only deliver drug if the button is pushed to activate the electrical current.[18] This "on-demand" administration of transdermal fentanyl has been shown to be as effective as intravenous patient-controlled analgesia (PCA) with morphine in the postoperative setting.[19] Although iontophoretic transdermal PCA systems offer a solution to acute postoperative pain, they are limited in their out-of-hospital use by the fact that each unit can only provide 80 doses or last for 24 hours, whichever comes first.[18]
Buccal Route
Another approach to treating BTP or incident pain is to provide fentanyl by the buccal route.[20,21] The buccal route is used with oral transmucosal fentanyl citrate (OTFC), the first commercially available rapid-onset opioid. Like transdermal PCA fentanyl, buccal fentanyl offers the advantage of being as effective as intravenous morphine, but unlike the iontophoretic transdermal PCA systems or intravenous morphine, buccal tablets or lozenges do not require any devices for administration.[22] The absorption of various opioids from the oral cavity was investigated in a study under conditions of controlled pH
www.medscape.org/viewarticle/518441_print 2/5
6/9/13
The Pharmacology of Fentanyl and Its Impact on Pain Management (printer-friendly)
and minimal swallowing with healthy volunteers over a 10-minute period.[23] Fentanyl was shown to be well absorbed from the buccal cavity, with 51% absorbed. Morphine, which is hydrophilic, is not well absorbed from the oral cavity; only 18% was absorbed. Methadone absorption is significantly pH-dependent; at higher (alkaline) pH, the absorption of methadone significantly improved. Alkaline pH also increases the absorption of other lipophilic opiates.[24] This fact is being exploited with fentanyl in an oral effervescent buccal tablet (FEBT) that is in clinical trials. FEBT is a dissolving buccal tablet that incorporates an alkalizing agent to raise the pH at the site where the tablet is applied (usually between the gum over the second or third molars and the buccal mucosa). This shift in pH increases the rate and magnitude of fentanyl absorption. Due to the pH manipulation, FEBT has an even more rapid onset of analgesia than OTFC (personal observation). The important point to note is that transmucosal absorption of fentanyl results in rapid uptake of the drug by the capillary bed of the buccal mucosa from where it rapidly reaches the brain, and that this results in the rapid onset of analgesia. The onset of BTP can be very rapid, sometimes peaking in minutes and usually only lasting 1-2 hours.[3] This means that to effectively treat BTP, a rapid-onset opioid is needed to match the temporal profile of the pain. OTFC and FEBT have properties that come closest to ideal for treating BTP. Being "fast-in" drugs, they provide the onset of meaningful pain relief in minutes, and being "fast-out," their duration of action is on the order of a few hours. The onset of analgesia with OTFC occurs in about 5 minutes, which is as rapid as with intravenous morphine.[22,25] The duration of analgesia with OTFC is approximately 2 hours compared with 4-6 hours for morphine.[6] OTFC has a longer duration of action than one might predict from its "fast-in, fast-out" lipophilic nature. This is because some of the swallowed drug is absorbed from the gastrointestinal tract and contributes to the longer than expected duration of action. In a study conducted to determine the bioavailability and absorption of fentanyl from OTFC, volunteers were given the same dose (15 mcg/kg) of fentanyl administered by 3 different routes: intravenous (IV fentanyl), oral transmucosal (OT fentanyl), and dissolved in water and swallowed (oral fentanyl).[26] The peak plasma concentration of OTFC rose rapidly after administration and the concentration decreased within 75-135 minutes after administration. This pattern is observed because part of the drug is absorbed via the buccal membrane and part is swallowed. The slow absorption from the gastrointestinal tract accounts for the duration of action of transmucosal fentanyl and accounts for its rapid onset and intermediate offset. Fortuitously, this time course of action is nearly ideal for treating BTP. The lipophilic nature of fentanyl allows it to cross cellular barriers that are impervious to hydrophilic drugs, such as morphine. This property has made fentanyl uniquely useful in treating chronic persistent (basal) pain when used as a transdermal patch. When transfer of fentanyl across the skin is accelerated by iontophoresis, the transdermal route can also be used to treat acute postoperative pain. The most important development in the treatment of BTP in the last decade has been the introduction of OTFC. This formulation is uniquely useful in treating rapid-onset BTP and incident pain. It is beyond the scope of this column to discuss all the advantages of transdermal and transmucosal fentanyl; however, it is clear that lipid solubility plays a critical role in the action of this drug, and it can be anticipated that future formulations of fentanyl will further exploit this physiochemical property.
1. Jansen PA. The development of new synthetic narcotics. In: Estafanous FG, ed. Opioids in Anesthesia. Boston, Mass: Butterworth Publishers; 1984:37-44. 2. Sebel PS. Cardiovascular, metabolic, and neurophysiologic effects of opioids. In: Estafanous FG, ed. Opioids in Anesthesia. Boston, Mass: Butterworth Publishers; 1984:45-49. 3. Portenoy RK, Hagen NA. Breakthrough pain: definition, prevalence and characteristics. Pain. 1990;41:273www.medscape.org/viewarticle/518441_print 3/5
6/9/13
The Pharmacology of Fentanyl and Its Impact on Pain Management (printer-friendly)
281. Abstract 4. McQuay HJ, Jadad AR. Incident pain. Cancer Surv. 1994;2:17-24. 5. Mercadante S, Radbruch L, Caraceni A, et al. Episodic (breakthrough) pain. Consensus conference of an expert working group of the European Association for Palliative Care. Cancer. 2002;94:832-839. Abstract 6. Data on file, Cephalon Inc. 7. Hug CC Jr, Murphy MR, Rigel EP, Olson WA. Pharmacokinetics of morphine injected intravenously into the anesthetized dog. Anesthesiology. 1981;54:38-47. Abstract 8. Roy SD, Flynn GL. Transdermal delivery of narcotic analgesics: pH, anatomical, and subject influences on cutaneous permeability of fentanyl and sufentanil. Pharm Res. 1990;7:842-847. Abstract 9. Varvel JR, Shafer SL, Hwang SS, Coen PA, Stanski DR. Absorption characteristics of transdermally administered fentanyl. Anesthesiology. 1989;70:928-934. Abstract 10. Plezia PM, Kramer TH, Linford J, Hameroff SR. Transdermal fentanyl: pharmacokinetics and preliminary clinical evaluation. Pharmacotherapy. 1989;9:2-9. Abstract 11. Sebel PS, Barrett CW, Kirk CJ, Heykants J. Transdermal absorption of fentanyl and sufentanil in man. Eur J Clin Pharmacol. 1987;32:529-531. Abstract 12. Fine PG, Streisand JB. A review of oral transmucosal fentanyl citrate: potent, rapid and noninvasive opioid analgesia. J Palliat Med. 1998;1:55-63. Abstract 13. Simpson RK Jr, Edmondson EA, Constant CF, Collier C. Transdermal fentanyl as treatment for chronic low back pain. J Pain Symptom Manage. 1997;14:218-224. Abstract 14. Ahmedzai S, Brooks D. Transdermal fentanyl versus sustained-release oral morphine in cancer pain: preference, efficacy, and quality of life. The TTS-Fentanyl Comparative Trial Group. J Pain Symptom Manage. 1997;13:254-261. Abstract 15. Clark AJ, Ahmedzai SH, Allan LG, et al. Efficacy and safety of transdermal fentanyl and sustained-release oral morphine in patients with cancer and chronic non-cancer pain. Curr Med Res Opin. 2004;20:1419-1428. Abstract 16. Gourlay GK, Kowalski SR, Plummer JL, et al. The efficacy of transdermal fentanyl in the treatment of postoperative pain: a double-blind comparison of fentanyl and placebo systems. Pain. 1990;40:21-28. Abstract 17. Duragesic [package insert]. Raritan, NJ: Ortho-McNeil, Inc. 18. Sinatra R. The fentanyl HCl patient-controlled transdermal system (PCTS): an alternative to intravenous patient-controlled analgesia in the postoperative setting. Clin Pharmacokinet. 2005;44(suppl1):1-6. 19. Chelly JE. An iontophoretic, fentanyl HCl patient-controlled transdermal system for acute postoperative pain management. Expert Opin Pharmacother. 2005;6:1205-1214. Abstract 20. Mystakidou K, Katsouda E, Parpa E, Tsiatas ML, Vlahos L. Oral transmucosal fentanyl citrate for the treatment of breakthrough pain in cancer patients: an overview of its pharmacological and clinical characteristics. Am J Hosp Palliat Care. 2005;22:228-232. Abstract 21. Hanks GW, Nugent M, Higgs CM, Busch MA; OTFC Multicentre Study Group. Oral transmucosal fentanyl citrate in the management of breakthrough pain in cancer: an open, multicentre, dose-titration and long-term use study. Palliat Med. 2004;18:698-704. Abstract 22. Lichtor JL, Sevarino FB, Joshi GP, Busch MA, Nordbrock E, Ginsberg B. The relative potency of oral transmucosal fentanyl citrate compared with intravenous morphine in the treatment of moderate to severe postoperative pain. Anesth Analg. 1999;89:732-738. Abstract 23. Weinberg DS, Inturrisi CE, Reidenberg B, et al. Sublingual absorption of selected opioid analgesics. Clin Pharmacol Ther. 1988;44:335-342. Abstract 24. Streisand JB, Zhang J, Niu S, McJames S, Natte R, Pace NL. Buccal absorption of fentanyl is pH-dependent in dogs. Anesthesiology. 1995;82:759-764. Abstract 25. Sevarino FB, Ginsberg B, Lichtor JL, et al. Oral transmucosal fentanyl citrate (OTFC) compared with IV morphine for acute pain in patients following abdominal surgery. Anesth Analg. 1997;84:S330. 26. Streisand JB, Varvel JR, Stanski DR, et al. Absorption and bioavailability of oral transmucosal fentanyl citrate. Anesthesiology. 1991;75:223-229. Abstract
Funding Inform ation
www.medscape.org/viewarticle/518441_print 4/5
6/9/13
The Pharmacology of Fentanyl and Its Impact on Pain Management (printer-friendly)
Supported by an independent educational grant from Cephalon. Medscape Neurology. 2005;7(2) 2005 Medscape
www.medscape.org/viewarticle/518441_print
5/5
You might also like
- Medicine 18 Edition. Mcgraw Hill. 2012Document1 pageMedicine 18 Edition. Mcgraw Hill. 2012Diamond DustNo ratings yet
- Elbow Joint AnatomyDocument4 pagesElbow Joint AnatomyDiamond DustNo ratings yet
- Book List AlphaDocument3 pagesBook List AlphaDiamond DustNo ratings yet
- Intravenous ParacetamolDocument4 pagesIntravenous ParacetamolDiamond DustNo ratings yet
- Characteristics of GravesDocument4 pagesCharacteristics of GravesDiamond DustNo ratings yet
- Postoperative AnalgesiaDocument6 pagesPostoperative AnalgesiaDiamond DustNo ratings yet
- 12.management of PterygiumDocument3 pages12.management of PterygiumDiamond DustNo ratings yet
- Famona - Sezampro.rs Medifiles Otohns Scott Scott511Document43 pagesFamona - Sezampro.rs Medifiles Otohns Scott Scott511Diamond DustNo ratings yet
- InTech-Ultrasound Imaging of The Fetal PalateDocument13 pagesInTech-Ultrasound Imaging of The Fetal PalateDiamond DustNo ratings yet
- Skin CareDocument4 pagesSkin CareDiamond DustNo ratings yet
- Glomus TumourDocument5 pagesGlomus TumourDiamond DustNo ratings yet
- All New Sorento PDFDocument2 pagesAll New Sorento PDFDiamond DustNo ratings yet
- What Is Peripheral Arterial Disease - (Printer-Friendly)Document7 pagesWhat Is Peripheral Arterial Disease - (Printer-Friendly)Diamond DustNo ratings yet
- What Is Peripheral Arterial Disease - (Printer-Friendly)Document7 pagesWhat Is Peripheral Arterial Disease - (Printer-Friendly)Diamond DustNo ratings yet
- 2010 9Document9 pages2010 9Diamond DustNo ratings yet
- P Cefalico Varones 0-36Document1 pageP Cefalico Varones 0-36RONALDNo ratings yet
- Daftar Pustaka HZDocument2 pagesDaftar Pustaka HZDiamond DustNo ratings yet
- Herpes ZosterDocument20 pagesHerpes ZosterDiamond DustNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Buffer Stock Maret1Document22 pagesBuffer Stock Maret1Selvi RatnasariNo ratings yet
- Professional Malpractice, Quackery and Healthcare FraudsDocument10 pagesProfessional Malpractice, Quackery and Healthcare FraudsAhmed HashmiNo ratings yet
- Cover LetterDocument2 pagesCover Letteralaa KassabNo ratings yet
- FDA LTO and CPR RequirementsDocument6 pagesFDA LTO and CPR RequirementsMylz MendozaNo ratings yet
- Sample Questions PharmacyDocument6 pagesSample Questions PharmacyfaisalnadeemNo ratings yet
- PRLB - Bpom - 8 - 2020 - enDocument14 pagesPRLB - Bpom - 8 - 2020 - enPT Java Teknologi FarmasiNo ratings yet
- STDTRT Guidelilne Essentialdruglist SA PHCDocument392 pagesSTDTRT Guidelilne Essentialdruglist SA PHCAvinash Rangarajan100% (1)
- Common Medical AbbreviationsDocument2 pagesCommon Medical AbbreviationsShahad HakimuddinNo ratings yet
- Cosmetic Product FormulationDocument6 pagesCosmetic Product FormulationNikko Nabasca GorneNo ratings yet
- Harga ObatDocument71 pagesHarga Obatklinik madaniyahNo ratings yet
- Drug Tariff March 2024Document1,245 pagesDrug Tariff March 2024piNo ratings yet
- Mahatma Gandhi Institute of Pharmacy, LucknowDocument3 pagesMahatma Gandhi Institute of Pharmacy, LucknowMukesh TiwariNo ratings yet
- Summary of Pharmacy Services NC III PDFDocument21 pagesSummary of Pharmacy Services NC III PDFArjay Plauta100% (1)
- Dice Hospital - Rules for a strategy dice game about healing patientsDocument7 pagesDice Hospital - Rules for a strategy dice game about healing patientsViktorNo ratings yet
- PharmaDocument1 pagePharmaIrene Soriano BayubayNo ratings yet
- AKTU B.Pharm 3rd Sem Exam Admit CardDocument2 pagesAKTU B.Pharm 3rd Sem Exam Admit CardAshu BhargavNo ratings yet
- List of Funding AgenciesDocument3 pagesList of Funding AgenciesRishavNo ratings yet
- HTTPS://WWW - Scribd.com/document/516867318/araling Panlipunan 10 Module 1 1st Quarter 1Document2 pagesHTTPS://WWW - Scribd.com/document/516867318/araling Panlipunan 10 Module 1 1st Quarter 1Aleckz MinaNo ratings yet
- FILE 28 June QDocument45 pagesFILE 28 June QHanan HejaziNo ratings yet
- Genotropin RefresherDocument4 pagesGenotropin RefresherJessica BascoNo ratings yet
- Pharmd Programme Handbook Faculty of Medical Sciences Entry Level Doctor of Pharmacy PDFDocument53 pagesPharmd Programme Handbook Faculty of Medical Sciences Entry Level Doctor of Pharmacy PDFJmv Velazquez100% (1)
- Pharmacy Endorsement LetterDocument2 pagesPharmacy Endorsement LetterShielo Marie CabañeroNo ratings yet
- TRW - pro.POL.1063.1 Supply Chain Inventory Management PolicyDocument27 pagesTRW - pro.POL.1063.1 Supply Chain Inventory Management PolicyCma Koshti100% (2)
- Full Programme FinalDocument4 pagesFull Programme FinalnosfarNo ratings yet
- Applied Pharmacology For The Dental Hygienist - Mosby 6 Edition (February 10, 2010)Document406 pagesApplied Pharmacology For The Dental Hygienist - Mosby 6 Edition (February 10, 2010)DrleoNo ratings yet
- Factors Associated With Patients' Incomplete Understanding of PrescriptionsDocument9 pagesFactors Associated With Patients' Incomplete Understanding of PrescriptionsCanlas John MichaelNo ratings yet
- DR Javier CAINTA MUNICIPAL HOSPITAL PATIENT OUTPUTDocument36 pagesDR Javier CAINTA MUNICIPAL HOSPITAL PATIENT OUTPUTLeah Grace Moreno-javierNo ratings yet
- Medication Adherence in The Real WorldDocument13 pagesMedication Adherence in The Real WorldCognizantNo ratings yet
- FDA Pharmaceutical Scientist Title 21 VacancyDocument8 pagesFDA Pharmaceutical Scientist Title 21 Vacancyashil R.No ratings yet
- New Medication Calculation PresentationDocument70 pagesNew Medication Calculation PresentationAna Luisa100% (1)