Professional Documents
Culture Documents
Abscesses:: Liver Needle Aspi Ration Versus Catheter Drainage
Uploaded by
Muhammad FadillahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abscesses:: Liver Needle Aspi Ration Versus Catheter Drainage
Uploaded by
Muhammad FadillahCopyright:
Available Formats
Percutaneous
Treatment
Abscesses:
Catheter
Chaturbhuj Sanjay Yogesh Madhu Sudha La) Rajak1
OBJECTIVE.This ically guided percutaneous of liver abscesses.
Needle Drainage
study was designed needle aspiration
Liver Aspi ration Versus
of
to determine
and compare catheter
the efficacy drainage
of sonograph-
Sanjay Gupta
Jam2 Chawla3 Gulati1
and percutaneous
in the treatment and 12 fepyogenic. or catheter
Sun1
SUBJECTS AND METHODS. In a randomized study, males; age range, 2-72 years; average age, 35 years) with liver 1 1 ; indeterminate, 19) underwent either percutaneous needle
50 patients
abscesses aspiration
(38 males
(amebic.
(ii
=
20; 25)
drainage
(n
25) along with appropriate
antimicrobial
therapy.
In patients
assigned
to the needle
aspiration group, an 18-gauge needle was used to aspirate the abscess cavity. was attempted only once in each patient not responding to the first aspiration: second
drainage drainage,
Repeated aspiration nonresponse to the were group).
using
aspiration (however,
8- to
was considered these patients
catheters 1 2-French
failure were
were
of treatment,
introduced into
and these patients drainage
cavity the abscess
given
the
catheter
Seldinger
not included
in the catheter
For catheter
technique. In patients with multiple abscesses group), all the abscesses except those smaller ment. Patients were followed hospital stay, and development during hospitalization. After
(seven in aspiration group and five in catheter than 3 cm were subjected to percutaneous treat-
up to assess the outcome of the percutaneous treatment, length of of any complications. Sonography was performed every third day discharge of the patient, periodic clinical and sonographic in only examinaof the in all 25
tions were done until total resolution of abscesses was achieved. RESULTS. Although percutaneous needle aspiration was successful
25 patients
15 (60%)
after
one (n
1 1) or two (n
4) aspirations.
catheter
drainage
was curative
patients (100%) (p < .05). Among the successfully treated patients, the average time for clinical improvement and the mean hospital stay were similar in the two treatment groups. Although the average time
taken
needed
in the
for a 50%
aspiration
reduction
than
in the size of the abscess
in the catheter was was the group
cavity
was significantly versus
and
(p the aver-
<
.05)
age
greater time
group
( 1 1 days
S days).
for total
resolution
which
of abscess No relapse
ranged
same ( I S weeks)
on
in both groups.
No major ex-
complications
amination during
were encountered.
follow-up,
documented 8 to 37 weeks.
clinical
sonographic
from
CONCLUSION. Our results show that percutaneous catheter drainage is more effective than needle aspiration in the treatment of liver abscesses. Needle aspiration. if limited to two attempts, has a high failure rate.
Received July 29, 1997; accepted October22, 1997.
1 Department
after revision Postgraduate Chandigarh, to S. Sun. PGIMER, Chandigarh, Institute of
L
Pin. 160012
iver
abscesses,
pyogenic, portant mortality
mode medical; abscesses
both amebic and continue to be an imof morbidity The liver
as to
13, 4].
ated
However,
operative (10-47%)
drainage
is associ-
with
significant
morbidity
and
of Radio-Diagnosis, and Research, Medicine,
cause of amebic
as many refractory
and primary is
ther-
mortality
[4-61.
In
recent
years,
imaging-
Medical
Education
in tropical of treatment
however, may be
countries.
India. Address 2Department 3Department
correspondence of Internal
abscess
guided percutaneous drainage has been increasingly used to treat liver abscesses. with reported 100% placement method
abscesses
15% of amebic
medical
success
rates 1].
an
ranging Although
from
catheter
70%
is
to
the
Pin. 160 012 India. of Hepatology, PGIMER. Chandigarh.
Pin. 160 012 India. AJR 1998:170:1035-1039 0361-803X/98/1704-1 035
Ray Society
apy may
scesses
[I I. Also,
complicate
[2]. In
[5,
of
7-1
percutaneous to drain
have
secondary bacterial 20% of amebic
such
infection liver ab-
indwelling
most
widely
preferred
studies
liver
shown
with
pyogenic
the
liver
patients and in patients abscesses, surgical drainmode of treatment
[8-131,
recent
American
Roentgen
age has been
traditional
therapeutic less costly,
needle aspiration to be a simpler. and equally effective mode of
AJR:17O, April 1998
1035
Rajak
et al.
treatment
I 14,
the relative
1 SI. We
conducted in 50 patients
and efficacy needle
a prospecto deterof the two
lf:1Patient
and
Abscess
Characteristics
in the Two
Treatment
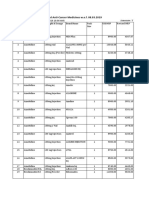
Treatment Group Catheter 4-65 (35.6) l9maIe,6female 23 patients 25 patients 3 patients
20 patients 32 (31b) 20 patients
Groups
tive randomized
mine procedures
study
safety (percutaneous
and
percutaneous
catheter
aspiration drainage) in the
Characteristic
Needle Aspiration Patient age (average) Sex Fever >37.2#{176}C Pain and tenderness
abdomen
(n
25)
Drainage
(n
25)
treatment
of liver abscesses.
(yr)
2-72 (35.44) l9male,6female 25 patients
Subjects Subjects
Fifty
and Methods
in upper
25 patients 3 patients
patients
with
liver
abscesses
referred
to the for 1994 The nonof
Jaundice
Leukocytosis (>10,000/mm3)a
Department percutaneous
and Febmary indications
of Radio-Diagnosis
at our institution
22 patients
management
1997 were for percutaneous
between
included interventions
February
in this study. were
Number of abscesses
Solitary
43 (37b)
l8patients
response to medical therapy and imminent rupture abscess [9. 1 1 1. Patients who did not res)nd
medical show signs derness therapy any clinical of deterioration and enlarging included (i.e.. 22 patients or increasing who who pain did and improvement showed
Multiple Location
Right
7 patientsc of abscesses 17 patients 3 patients 5 patients 10-847 ml (221.86 205.49 ml) 16 abscesses 11 patients 6 patients 8patients
six in aspiration
group
5 patientsd 17 patients 4 patients 4 patients 33-1834 ml (335.74 376.72 ml) 14 abscesses 9 patients 5 patients 11 patients
and one in catheter groupl measuring <3 cm in their
to
not ten-
lobe
Left lobe Both lobes Volume of percutaneously treated abscesses e (mean SO)
abscess size on serial sonogra-
phy while on medical therapy). Patients with imminent rupture of abscess included 28 patients in whom sonography showed a thin (<I cm) rim or no discernible hepatic parenchyma around any part of the circumference of the abscess. Patients with already ruptured abscesses were not included in this study. The patients were randomly assigned to undergo either percutaneous needle aspiration (n = 25) or percutaneous catheter drainage (n = 25) along
with appropriate included antimicrobial 38 males therapy. and The patient who population 12 females
Signs of impending
Cause of abscesses Amebic Pyogenic Indeterminate
rupture
alotal leukocyte count. bIn patients with multiple abscesses, abscesses largest dimension were not treated percutaneously.
ciwo
to six abscesses:
mean, 3.57.
x
were 2-72 years old (mean age. 35 years old). The patient characteristics in the two treatment groups are summarized in Table I . The two groups were similar in all respects except for the volume of
abscesses; the average volume of abscesses (336 ml)
dTwo to three abscesses; mean, 2.4. eVolume of abscesses was calculated using the formula of an ellipse: 0.523 x length
breadth
height.
was larger in the catheter drainage group than the average volume (222 ml) in the needle aspiration group. Amebic abscesses were diagnosed in 20 of the 50 patients on the basis of positive findings on an mdirect hemagglutination test (titer, l : 128). In I I of the
50 patients, the abscesses were pyogenic as sug-
received appropriate blood products for correction to acceptable levels of coagulation factors. The percutaneous treatment procedures were performed under local anesthesia (2% lignocaine)
with IV analgesia and sedation when required. The
4600 kee, sector Systems.
(General WI) and Issaquah.
Electric Sonoline WA)
Medical 51-450 systems were was
Systems. (Siemens used.
MilwauMedical
and 3.5- or 5-MHz aspiration into the in an In the
or convex transducers In the patients assigned
an I 8-gauge needle cavity
to the needle advanced were the
were performed under continuous realtime sonographic guidance using the freehand technique. For sonographic guidance. RT 3600 and RT
procedures
S Of
group. abscess attempt
and the contents evacuate
aspirated cavity.
to completely
gested
of the aspirated pus. The specific organisms cultured were Staphylococcus aureus in five patients and a-hemolytic streptococcus. hemolytic streptococcus, Klebsie!k, pneunioniae, Escherichia coli. Acinetobacter anitratus, and Enterococcus faecalis
by the culture
Percutaneous
Ur Ac.u.s
Needle
Asplration
and Catheter
Drainage
In 50
ots
in one
patient
each.
In the other
although the abscess cavity aspirates were frankly purulent on visual inspection and showed the
19 patients, presence cytes of innumerable polymorphonuclear leuko-
on cytologic examination. no organisms were identified and the findings of both amebic serology and pus cultures were negative: hence. the cause of these abscesses could not be definitely established.
Methods
Informed
consent determined
was taken
from
all the patients
undergoing
factors were
percutaneous
treatment.
in all patients
Coagulation
before the Note-NA
=
not applicable.
group) showed small residual cavities -3 cm) at 10-12 weeks
scheduled procedure to rule out any bleeding disorder. Three patients with evidence of coagulopathy
#{149}Three patients (one in aspiration group and two in catheter but were lost to further follow up.
1036
AJR:17O, April 1998
Percutaneous
Treatment
of Liver
Abscesses longed
gram
seven abscesses sion) dle
patients (which were aspiration
with were was
multiple to needle attempted
abscesses. aspiration; in 37
all but largest of thus. the
six nee43
<3 cm in their
dimen-
subjected in this group
normalized, follow-up imaging showed resolution of the abscess (total resolution or reduction in size to <3 cm), and no evidence of relapse or recurrence
was seen during follow-up.
(35 days) in only one patient; obtained and
with
a cavitorevealed This disbe-
in with three
catheters
this more
patient patients
communication patient
the biliary
in situ
system. were
they when
abscesses
of patients.
For percutaneous catheter drainage, appropriatesized catheters (8- to I 2-French pigtail or Malecot
drainage introduced Seldinger scesses, catheter: and each two catheter: into technique. abscess catheters Cook, the Bloomington, abscess In patients was were drained used cavity with with IN) using multiple were the ab-
The chi-square test with Yates correction was used to analyze the success rates of the two treatment techniques. A nonpaired Students t test was used to assess periods the statistical significance and of differences in the
charged
came drainage
clinically
from the
stable
catheter;
but
had
the
persistent
patients at-
a separate patients
in four
one patient needed three catheters. The cathetens were connected to a completely closed collecting system
A daily
the time needed for clinical improvement, 50% reduction in size of abscess cavity, and total or near-total resolution of the abscess after percutaneous treatment. A p value of less than .05 was considered statistically significant.
of hospitalization
the outpatient department on alternate days until catheter removal. Among the successfully treated patients, the average time needed for clinical relief (detended
fervescence)
and the time
mean needed
hospital groups
stays (Table
were 2). of the
similar Although Results The results of percutaneous in Table 2.
aspiration
in the two treatment
and routine estimate
catheter fluid sterile was saline
care
was
instituted. Irrigation daily removed symptoms counts), to
of the amount,
with
color, and consisrecorded. was done were local
for reduction
tency avoid
of the drainage catheter defervescence normalization blockage.
of the catheter
needle
aspira-
Catheters
tion and percutaneous
catheter drainage
in the
when
(i.e.. and
the patients
showed
and relief of elevated
clinical
from
improvement
50 patients are given
Percutaneous needle
abscess cavity to 50% of its original size was significantly more in the needle aspiration group than in the percutaneous catheter drainage group ( I I days versus 5 days), the average
time taken for total or near total resolution of the abscess was similar in both groups of patients (Table 2). In three patients, small (2-3 cm) 10-12 were residual weeks lost cavities after were drainage; still present patients at these
was successpaThe
leukocyte
the catheter output dropped to less than 10 ml/24 hr for 2 consecutive days, and follow-up sonography
showed tests negligible pus residual was cavity. and microbiologic oran day Aspirated examined
ful in 15 (60%) of the 25 patients. Eleven tients responded to a single aspiration. other
piration
14 patients were subjected to a second as2-7 days (average, 3 days) later for one
were performed to determine the causative ganism. Broad spectrum antibiotics, including
aminoglycoside (cloxacillin at 150 mg/kg per
or both of the following fever lation and leukocytosis
reasons: persistence of
(n as
=
to further
follow-up.
No relapse (range, 8-37
1 1) and reaccumuby follow-up
was documented
on clinical
and sonographic
of the
(n
abscess
=
shown
IV and gentamicin at 4.5 mg/kg per day IV) with metronidazole (500 mg IV or 800 mg orally three times a day) and chloroquine. were initiated. Once the lalxwatory results were available, antibiotics were changed on the basis of sensitivity tests. However, patients in whom pus culture findings were negative were continued on the same broad spectrum antibiotics and antiamebic drugs. The antibioticy and
sonography
I 2). Only
four of these 14 pa-
examination during follow-up weeks; mean, 20 weeks).
tients responded to a second aspiration. Percutaneous needle aspiration was considered cause unsuccessful they failed in to 10 patients improve (40%) clinically aspiration evacuate beor
No major complications were encountered. Three patients, two in the catheter group and
radiologically even after a second In three of these patients, needle
(both
aspiration.
one in the aspiration group, had minor complications. One patient complained of severe pain at the catheter entry site that was relieved
with oral analgesic. with of the
within
A pericatheter debris;
leak devel-
metronidazole and 14 days, in the
were dosage
given of 600
for a duration Chloroquine mg daily for
of was 2
attempts)
failed
to completely
oped in another patient because ofblockage
the catheter the leak stopped
of
after
10 days given days
respectively.
orally
followed
by 300 mg daily
for 19 days.
the abscess cavity because of the thick viscous nature of the pus. Rapid reaccumulation in the abscess cavity was seen in eight of these 10
patients within 3-6 days after the second
in whom needle
flushing
Hemorrhage
catheter with sterile the abscess cavity
during needle
saline.
develaspira-
All patients were followed up to assess the time needed for clinical improvement. length of hospital
stay. odic and development size until of any the patients complications. were hospitalized. Pen-
aspia.spira-
oped
in the third patient
ration. The average volume
ml) in the 10 patients
of abscesses (425
significantly volume (p
<
sonography
was done every
third day to assess
tion was
.05)
unsuccessful than
was
tion, as suggested by the sudden appearance of echogenic foci within the homogeneously hypoechoic abscess cavity and the mixture of
blood with the aspirated
the cavity
larger
the average
( 178 ml) who reHowever, were Subse-
Patients in the percutaneous needle aspiration group who did not improve clinically after the first aspiration and continued to have leukocytosis or showed refilling of the abscess cavity on follow-up
sonography were subjected to a second aspiration.
of the other
similar
abscesses in the 15 patients sponded to one or two aspirations. patient and abscess two groups
with
was treated conservatively
IV fluids.
material; this patient with bed rest and
characteristics of patients.
in these
treated (however, included
Failure of the patient to improve after a second aspiration was considered as failure of aspiration therapy. After discharge, all patients were followed up with periodic clinical and sonographic examinations to assess for any recurrence of the disease and
quently, fully
drainage are not
all of these 10 patients
percutaneous in our study, in the
were successcatheter
Discussion In recent ous
drainage) years, imaging-guided
these
patients
drainage
treatment
(needle
aspiration
surgical
percutaneor catheter
as
catheter
has replaced
intervention
group). these
A cavitogram
was obtained because the communication was successful
for two of fluid was seen in all 25 catheter
to monitor the size of the abscess cavity. The patients were examined weekly for I month, monthly for the next 3 months. and at two monthly intervals thereafter until complete resolution of the abscess
was achieved.
10 patients
drainage
the primary treatment for liver abscesses [5, 7-1 1 ]. The main advantages of needle aspiration over catheter drainage include the foland
was bilious; biliary in both patients. Catheter patients drainage (100%)
lowing: Needle less expensive; follow-up
nursing care
aspiration
is less
invasive
it avoids care,
is required;
problems so less
and multiple
related medical
cavities
to or
Treatment was considered successful if all of the following criteria were met: The patients improved
clinically and (i.e.. subsidence elevated of fever leukocyte and local counts signs were symptoms).
of the percutaneous
catheter
drainage group. In most patients (n = 24), duration of catheter drainage varied from 3 to 15 days (average, 7 days). The duration was pro-
can be aspirated However,
in the same session [14, 15].
shows, needle aspira-
as our study
AJR:170, April 1998
1037
Rajak
et al.
tion,
cantly
if limited
lower
to two attempts,
success rate
has a signifithan catheter
In contrast tion, percutaneous catheter
accumulation
to percutaneous placement continuous
are
needle aspiraof an indwelling
may
ally
persist
for years.
Such from
cavities simple
are usuhepatic Singh and
indistinguishable
drainage (60% versus 100%). The success rate of percutaneous needle aspiration in the various series reported in the literature varies from 79% to
provides
drainage; evacuation
hence, and re-
cysts [20]. In a series of 30 patients,
the problems
drainage,
of incomplete
100% rate in our
[14-18].
accounting
not associated with catheter for the high success rates
reported in most of the
Kashyap [9] noted much faster and more complete resolution of abscess cavity after percutaneous
The
relatively
lower
needle
success aspiration
(60%)
study
of
is
of catheter earlier
drainage
percutaneous
possibly
ration
dure
related to the fact that repeated aspiwas attempted only once in cases of
to the first aspiration;
in which repeated aspirations this
studies [7, 9-1 1, 19] and also seen in our series. The only reasons for failure of percutaneous catheter drainage, as reported in some
taneous
catheter drainage than after percutaneous needle aspiration. However, the results of our study suggest that although mitial collapse earlier of the abscess undergoing cavity is achieved drainin patients catheter
nonresponse studies,
procewere
of the earlier
drainage (this
series
problem
[10,
can
19], have
is in contrast
to that in most of the other
been either thick pus not amenable
come
premature
to percube over-
age than in those undergoing needle aspiration, the time needed for total resolution of the
abscesses is similar in the two groups. have been
(12%
done up to three or four times [9, 14, 15, 17, 18]. In our study also, the success rate after
one aspiration was only 44%; it increased success if multiHowneedle of aspi[9,
5 to from
by using
removal
larger
of the
bore
catheters)
catheter
or
both
Complications
drainage
catheter
drainage
reported with in the series of
to
(strict
adherence occurred
to the criteria
60% after rate would ple repeated aspirations rations
14-18]) 14 days
two aspirations. A higher likely have been achieved aspirations (with attempted. the patients to multiple the average ranging
period
removal
recurrence Our
can prevent
this problem
for catheter [1 1]). No
Lambiase et al. [21]) and needle aspiration (4% in the series of Baek et al. [14]). Baek et al. and Giorgio lower incidence
as one
in any of our cases dur-
et al. [15]
describe
the much
with
were
ing the follow-up
study
period.
no meaningful differ-
of complications
of the major
percu-
ever, subjecting
per patient
over [14-17]
suggests
taneous
drainage
needle aspiration
than with
catheter
of
number
varying
from
1.4 to five
ence in either the time taken for defervescence or the duration of hospitalization among the
patients successfully treated with either tech-
advantages
a short
needle aspiration. However, our study and some recent reports suggest that both procedures,
safe if properly performed, are essentially
is a traumatic
and unpleasant
experience
ceptable
tempts
14-18].
for the patients and may not be acto many. Moreover, even multiple atdo not guarantee a 100% cure rate [9,
For
nique. In keeping with the findings of earlier reports [7, 9-1 1, 14-19], both treatment techniques resulted in rapid clinical relief, with
most patients showing resolution of fever, local symptoms, of the procedure.
procedures with minimal [5, 7-15]. Singh and Kashyap
15%
complications [9] reported bacterial conaspirations;
incidence
after
of secondary
multiple needle
these
reasons,
we
preferred aspiration.
to
and leukocytosis
within
3 days
tamination
subject drainage
the patients
after failure
to percutaneous
by second
catheter
however, countered bacterial possibility complication abscesses
other this infection with
workers problem.
[14-1
8] have not ensecondary theoretic this in liver catheter, reported
The average size of the abscess in our study was larger than in other series 14, 15, 18]. In
contrast
to some the ultimate abscesses
of the earlier outcome are more
reports
that show
that the initial size of the abscess cavity did not
affect
[15, 16], we believe difficult to evacurenecessitating
The average hospital stay ( 1 1 days) of the who underwent percutaneous catheter drainage in our study was shorter than that reported in two earlier series [7, 19]. One possible explanation is that all the patients in those series had pyogenic liver abscesses and
patients
continued to be hospitalized for the definitive
Although a distinct
remains
an indwelling
has been rarely [7, 9-1 1, 19]. of our study
One limitation
is that the pa-
that large
peated
tients included
with abscesses
formed
of both
a heterogeneous
amebic
group
ate completely abscesses neous
in one attempt,
treatment
of the predisposing
conditions
such
and pyogenic
aspirations. The average volume of in the 10 patients in whom percutaneedle aspiration larger was unsuccessful volume
responded who
as diverticulitis, cinoma, and
gall stones, gall bladder carso forth even after removal of
causes existing in both groups. Also, many abscesses (n = 19) were of indeterminate cause. Because our institution is a referral many of these patients had been treated counts study. had this of these with antibiotics and antiamebic hospital, partially drugs
was of
catheter and resolution
No such predisposing
nized
of the abscess [7, 19].
conditions were recog-
significantly
than the average
the abscesses in the 15 patients to one or two aspirations.
One important reason for
failure
of needle
aspiration
is the inability viscous
to completely
evacu-
ate the thick
pus that may be present
in some of the abscesses [9, 15]; this pus was seen in three of our patients. Rapid reaccumulation another and seen In some of the abscess after needle aspiration is
in the small number (n = 1 1) of patients with proven pyogenic liver abscesses encountered in our study. The shorter hospital stay could also be related to the fact that, unlike the practice in previous studies, we did not wait for total radiologic resolution of abscess cavity before discharge; the average volume
before being referred
for the high
to us; this probably
percentage researchers [10, 17]. Hence,
ac-
of abscesses
with negative
Some cases This
findings
previous does
on pus cultures
have
in our
also analysis
experience outcome
of abscess Also, with
at the time of discharge
was 70 ml.
successful
scesses. from
not allow prediction of a based on the cause of abcould be obtained a larger
cause.
problem,
described
by Dietrick
[17]
in 12 of our patients of the patients (two
after first aspiraaspiration. in our series), this due to biliary no existed, and the
tion and eight patients rapid refilling
communication; obvious continuing
after second
been
could have
however,
in most patients
four of our patients were discharged catheters in situ when they became clinically stable but had persistent drainage from the catheter. The time required for complete sonographic resolution of abscess cavities after
percutaneous treatment
information
a prospective
abscesses
study that included
of a single
number of
needle
In conclusion, aspiration
although and
both
percutaneous drainage are
catheter
predisposing
factor
ranges
from
2 weeks
sale methods for the nonsurgical liver abscesses, catheter drainage
treatment
is more
of
ef-
inflammatory process itself probably contributed to the reaccumulation of fluid.
to 9 months [9, 18]. In fact, total resolution may not occur, and small residual cavities
fective
than needle aspiration,
attempts, is associated
which,
with
if lim-
ited to two
a high
1038
AJR:170, April 1998
Percutaneous
Treatment
of Liver
Abscesses
failure
rate, especially with thick
in large viscous
abscesses pus.
and
4.
Satani
provement
in abscesses
However,
B, Davidson ED. Hepatic abscesses: in mortality with early diagnosis
Am J Sung 1978:135:647-650
imand DC.
genic hepatic abscess: ment. Am Sung 1995:61 14. Back SY. Lee
results of current :407-41 1 percutaneous
manage-
the results also with appropriate many
patients,
indicate that antimicrobial
result in
needle aspiration therapy will, in
Also, among
treatment.
MG, Cho KS, Lee effectiveness
SC, Sung aspiration
KB,
of
AiR
5. GerzofSG,
JohnsonWC,
Robbins
AH, Nabseth
Auh YH. Therapeutic
hepatic abscesses: 1993; 160:799-802 15. Giorgio A, Tarantino genic abscesses: percutaneous needle liver
a cure.
Intrahepatic pyogenic abscesses: treatment by percutaneous drainage. Am JSurg 1985:149:487-494
6.
in 25 patients.
the successfully
difference tion, abscess
exists
treated patients, no significant
in the time required for clini-
Lee JF, Block
GE. The changing
clinical
pattern
of
L, Marmniello
N. et al. Pyo-
cal improvement, and the time cavity
the duration needed in the two
of hospitalizaof the groups. to treatment
hepatic abscesses. Arc-h Sung 1972:104:465-470 7. Artar B, Levendoglu H, Cuasay NS. CT-guided percutaneous aspiration and catheter drainage pyogenic liver abscesses. Am J Gasimenteml
of
13 years of experience in aspiration with US guidance. HW. PyoArch Surg
for resolution
Radiology
16. Stain genic
1995;l95: 122-124 SC. Yellin AE, Donovan AJ, Brien liver abscess:
Unfortunately,
our data do not allow us to prelikely to respond
1986;8:550-555
8. Seeto change
Medicine
modem
with
treatment.
RK,
Rockey
DC.
Pyogenic
liver and
abscess: outcome. of ame-
dict the type of abscesses
in etiology,
management.
1991:126:991-996 17. Dietrick RB. Experience
Surg 1984:147:288-291
liver abscess.
Am
needle aspiration
randomized ration cally alone address studies
alone. Further
investigating warranted
prospective,
needle aspito specifi-
9. Singh
1996:75:99-I 12 JP, Kashyap A. A comparative catheter drainage
evaluation
are therefore this problem.
percutaneous
for resistant
18. Giorgio guided
tmintest 19.
A. Amoroso percutaneous tool
Radio!
P. Francica G, et al. Echopuncture: a safe and valuable liver abscess.
Gas-
bic liver abscesses. Am J Surg 1989;l58:58-62 10. vanSonnenberg E. Muller PR, Schiffman results
ogv
therapeutic HR. et al. Bertel
for amebic 1988;l3:336-340
Intrahepatic amebic abscesses: indications for and of percutaneous catheter drainage. Radio!1985:156:631-635 VA, Agarwal DK, Baijal 55, et al. Percucatheter drainage of amoebic liver ab1992:45:187-189 D, Ambroseui P. Khoury review
Surg Gyneco!
CK, vanHeerden JA. Sheedy PF II. Treatment of pyogenic hepatic abscess. Arch Sung
1986;121:554-558
References
1 . Thompson abscess: 2. Sherlock
.cv.cIen:.
JE, Forlenza a therapeutic S. DooleyY.
9th ed. Oxford:
S, Verma approach.
R. Amebic
Rev Inftct
liver
Dis
I I. Saraswat taneous
20.
RaIls PW, Quinn
MF, Boswell
WD Jr, Calletti
PM.
1985:7:171-179
Disease
scesses. C/in Radio! 12. Robert JH, Miresew Greenstein treatment
Obstet
Radin DR. Halls J. Pattern of resolution in successfully treated hepatic amebic abscess: sonographic
evaluation. 21
.
G,
Radiology
1983;l49:541-543 L Cronan L Cronan JJ, Dorfdrainage of 335 consecutive drainage 167-179 with I -year 1992;l84:
of the liver and
1993:471-502
btharv
Blackwell,
Al. Rohner A. Critical of pyogenic liver abscess. R, Broniatowski
of the
Lambiase RE, Deyoe man GS. Percutaneous abscesses: results
Radiology
3. Theron
P. Surgical
aspects
ofamoebiasis.
BrMedJ
1947:2:123-126
1992;l74:97-l02 13. Hashimoto L. Hermann
of primary
5G. Pyo-
follow-up.
AJR:170, April 1998
1039
You might also like
- D1747 PDFDocument4 pagesD1747 PDFMahmoud FlefilNo ratings yet
- 2.2.49. Falling Ball Viscometer MethodDocument2 pages2.2.49. Falling Ball Viscometer MethodDheeraj Shukla100% (1)
- Academia-Cat en HRDocument616 pagesAcademia-Cat en HRetsimo100% (1)
- Gkf3000s enDocument6 pagesGkf3000s enPiotrSikoraNo ratings yet
- Iq of SFPDocument25 pagesIq of SFPKrishna PalNo ratings yet
- EP1374874A2 Liquid Antacid CompositionsDocument6 pagesEP1374874A2 Liquid Antacid CompositionsKevin Alexander Campos De León100% (1)
- Rubber Surgical Gloves: Standard Specification ForDocument4 pagesRubber Surgical Gloves: Standard Specification ForRaya TahomaNo ratings yet
- F - DataDocument6,411 pagesF - DatapadmaNo ratings yet
- Design Guide For CleanroomsDocument1 pageDesign Guide For CleanroomsJeffNo ratings yet
- CPCB - Pollution Control Acts - (p1-660)Document660 pagesCPCB - Pollution Control Acts - (p1-660)Rajit VasudevNo ratings yet
- Healthcare: Dow Corning Pharma TubingDocument4 pagesHealthcare: Dow Corning Pharma TubingkajukafrisNo ratings yet
- Sticking and Picking in Pharmaceutical Tablet CompressionDocument1 pageSticking and Picking in Pharmaceutical Tablet CompressionKangal PothikNo ratings yet
- Tamsulosina + DutasterideDocument13 pagesTamsulosina + DutasterideJavier Hernandez100% (1)
- APSSSR, 96 AtthapuDocument64 pagesAPSSSR, 96 AtthapuAtthapu ThirupathaiahNo ratings yet
- Department: Quality Assurance: Surface Area Calculation SheetDocument4 pagesDepartment: Quality Assurance: Surface Area Calculation SheetDarlenis RodriguezNo ratings yet
- Operating Manual of SFPDocument14 pagesOperating Manual of SFPKrishna Pal0% (1)
- ASEAN TMHS GMP Training Chapter 2 Personnel FD1Document24 pagesASEAN TMHS GMP Training Chapter 2 Personnel FD1Abou Tebba SamNo ratings yet
- Article WJPR 1467266667Document10 pagesArticle WJPR 1467266667Atthapu ThirupathaiahNo ratings yet
- PharmexcilAnnualReport 2017 18Document86 pagesPharmexcilAnnualReport 2017 18Vu HauNo ratings yet
- Multidimensional Component Inspection DevicesDocument81 pagesMultidimensional Component Inspection DevicesMiltos BoboulosNo ratings yet
- Highlights of IP Addendum 2012Document4 pagesHighlights of IP Addendum 2012NitinPrachiJainNo ratings yet
- Filter Testing PDFDocument23 pagesFilter Testing PDFamol1321No ratings yet
- Drugs Standard Rules 2041 - NepalDocument38 pagesDrugs Standard Rules 2041 - NepalAbhishek Man ShresthaNo ratings yet
- PM AutoClave Vertical ManualDocument50 pagesPM AutoClave Vertical ManualAndre Fikas0% (1)
- Generation and Validation of Standard Operating Procedure For Dissolution ApparatusDocument18 pagesGeneration and Validation of Standard Operating Procedure For Dissolution ApparatusAbhishek JhaNo ratings yet
- Glad OSDDocument32 pagesGlad OSDYose RizalNo ratings yet
- Dewpoint Compressed Air Application NoteDocument4 pagesDewpoint Compressed Air Application NoteKarthick Velayutham100% (1)
- List APOTIKDocument17 pagesList APOTIKAtuq MudhaNo ratings yet
- Laporan Igd 2018Document216 pagesLaporan Igd 2018Rahma watiNo ratings yet
- Operation and Calibration of The AutoclaveDocument6 pagesOperation and Calibration of The Autoclaveemje pebeNo ratings yet
- PV SDF 2 FdaDocument84 pagesPV SDF 2 FdaLien Hong0% (1)
- HPLC Verification - Pic Added &shortendDocument40 pagesHPLC Verification - Pic Added &shortendMD Fahad MiajiNo ratings yet
- GMP LabDocument40 pagesGMP Labsudar1477No ratings yet
- Propofol - Injectable Injection - RLD 19627 - RC06-16 PDFDocument3 pagesPropofol - Injectable Injection - RLD 19627 - RC06-16 PDFAhmed SalehinNo ratings yet
- Results and Discussion: Table 1. Diffusivities at 50 CDocument7 pagesResults and Discussion: Table 1. Diffusivities at 50 CMichelle HutamaresNo ratings yet
- PFP Alt Spi Maf Elc Gen 0004Document6 pagesPFP Alt Spi Maf Elc Gen 0004dhanu_lagwankarNo ratings yet
- List of Cytotoxic MedicinesDocument1 pageList of Cytotoxic Medicinesempr404100% (1)
- Usp 797GCDocument61 pagesUsp 797GCAwni1989No ratings yet
- Limit Test For Heavy MetalsDocument19 pagesLimit Test For Heavy MetalsnutrimakeNo ratings yet
- Validation of Coating Equipment Ketik UlangDocument6 pagesValidation of Coating Equipment Ketik UlangSatish Hiremath100% (2)
- Guidelines For Registration of Pharmaceutical Premises in Nigeria by Pharm Saidu BurjiDocument10 pagesGuidelines For Registration of Pharmaceutical Premises in Nigeria by Pharm Saidu BurjiYPS NetworkNo ratings yet
- Antacid Suspension PDFDocument3 pagesAntacid Suspension PDFvenishetty0% (1)
- Cleaning Validation Approach 1Document19 pagesCleaning Validation Approach 1Dharmesh PatelNo ratings yet
- Anti Cancer List TotalDocument23 pagesAnti Cancer List Totalsampath seshadri100% (1)
- Norma Astm Dd1338Document3 pagesNorma Astm Dd1338Manuel ContrerasNo ratings yet
- List of Guidelines 1679795815Document3 pagesList of Guidelines 1679795815Rezha AmaliaNo ratings yet
- KluberDocument20 pagesKluberJako MishyNo ratings yet
- Compression Machine AlarmsDocument2 pagesCompression Machine AlarmsJc NaveenNo ratings yet
- Safe Management of Wastes From Healthcare ActivitiesDocument330 pagesSafe Management of Wastes From Healthcare Activitiesrsia mitra husada100% (1)
- 〈665〉 Plastic Components and Systems Used to Manufacture PharmaceuticalDocument9 pages〈665〉 Plastic Components and Systems Used to Manufacture Pharmaceuticalmehrdarou.qaNo ratings yet
- As 4369.2-1996 Surgical Dressings General Purpose Single-Use Woven Gauze SwabsDocument6 pagesAs 4369.2-1996 Surgical Dressings General Purpose Single-Use Woven Gauze SwabsSAI Global - APACNo ratings yet
- Fabtech Granulation SystemsDocument16 pagesFabtech Granulation SystemsRam SantoshNo ratings yet
- 2013-12 QP Template Imp PDFDocument3 pages2013-12 QP Template Imp PDFMarcM77No ratings yet
- Solitaire Pharmacia Pvt. LTD.: Restricted Circulation Authorised Persons OnlyDocument8 pagesSolitaire Pharmacia Pvt. LTD.: Restricted Circulation Authorised Persons OnlyNgoc Sang HuynhNo ratings yet
- Pilot Plant Scale-Up TechniquesDocument62 pagesPilot Plant Scale-Up TechniquesVaseline Robinson100% (2)
- Bosch GKF 2000Document105 pagesBosch GKF 2000Chris WoltzNo ratings yet
- Liver A BSC DrainDocument8 pagesLiver A BSC DrainAngelica AmesquitaNo ratings yet
- Jurnal Reading Abses HeparDocument5 pagesJurnal Reading Abses Heparika nur utamiNo ratings yet
- Appropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortDocument5 pagesAppropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortSiti Annisa NurfathiaNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Or JournalDocument2 pagesOr JournalNathaniel PulidoNo ratings yet
- Synopsis DR - VasundhraDocument8 pagesSynopsis DR - Vasundhraprince395No ratings yet
- Siddha Quest Siddha Medicine Practitioners Can Also Practice Modern MedicineDocument5 pagesSiddha Quest Siddha Medicine Practitioners Can Also Practice Modern MedicineDr.Santhosh SelvamNo ratings yet
- Jurnal Bumil Pingsan 3Document4 pagesJurnal Bumil Pingsan 3rina astutiNo ratings yet
- Aroma N Masase KakiDocument5 pagesAroma N Masase KakiAsmawati NadhyraNo ratings yet
- Guide To Dental Implants Cost and ProcedureDocument11 pagesGuide To Dental Implants Cost and Procedureawideman22No ratings yet
- AMC Batch 47Document3 pagesAMC Batch 47noha darwishNo ratings yet
- Ringer Asetat Pada AnakDocument72 pagesRinger Asetat Pada Anaknanda surastyo100% (1)
- Larry Wheels God Delts PDFDocument2 pagesLarry Wheels God Delts PDFYagesh0% (1)
- Thanatologi International 2007Document37 pagesThanatologi International 2007Paul LeeNo ratings yet
- PET/CT TechnologistDocument3 pagesPET/CT Technologistapi-79302631No ratings yet
- Structure and Function of HaemoglobinDocument21 pagesStructure and Function of HaemoglobinSonam JoshiNo ratings yet
- Review of SystemsDocument3 pagesReview of SystemsCarrboro Family Medicine100% (1)
- MCN Lec QuizzesDocument22 pagesMCN Lec QuizzesRaquel Monsalve67% (3)
- ACOG Guidelines For Exercise During PregnancyDocument13 pagesACOG Guidelines For Exercise During Pregnancypptscribid100% (1)
- Pemicu 2 Blok KGD Jovian LutfiDocument77 pagesPemicu 2 Blok KGD Jovian LutfiJovian LutfiNo ratings yet
- To Whom It May ConcernDocument2 pagesTo Whom It May ConcernIrina PapucNo ratings yet
- Abnormal LaborDocument20 pagesAbnormal Laborأ.م.د. إنعام فيصل محمدNo ratings yet
- Afra Sulthana M V: Submitted byDocument40 pagesAfra Sulthana M V: Submitted byjafir8shangmail.com shanNo ratings yet
- PreTest Obstetrics & Gynecology, Fifteenth EditionDocument255 pagesPreTest Obstetrics & Gynecology, Fifteenth EditionDr. Faeba JosephNo ratings yet
- Zimmer Trabecular Metal Femoral Cone Augment Surgical TechniqueDocument12 pagesZimmer Trabecular Metal Femoral Cone Augment Surgical TechniqueTudor MadalinaNo ratings yet
- Enigma 1 Trial 2007Document11 pagesEnigma 1 Trial 2007Jason TiongNo ratings yet
- Carboprost Drug StudyDocument3 pagesCarboprost Drug StudyAjay SupanNo ratings yet
- Easa Caa Class 1Document2 pagesEasa Caa Class 1A0938746599273927No ratings yet
- Abnormal Uterine ContractionDocument75 pagesAbnormal Uterine ContractionNishaAhsin90% (20)
- Obstetric SBAs MCQDocument5 pagesObstetric SBAs MCQCofeelovesIronman Javier100% (1)
- AbbreviationsDocument3 pagesAbbreviationsJade Hemmings100% (1)
- Prelacrimal Approach To Maxillare SinusesDocument5 pagesPrelacrimal Approach To Maxillare SinusesBagus Sofian AdhatamaNo ratings yet
- Mnemonic S NSGDocument18 pagesMnemonic S NSGohsnapitsleiNo ratings yet
- The Grand MultiparaDocument5 pagesThe Grand MultiparaIndhumathiNo ratings yet