Professional Documents
Culture Documents
TB Micros
Uploaded by
Degee GonzalesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TB Micros
Uploaded by
Degee GonzalesCopyright:
Available Formats
TB MICROSCOPY DIRECTLY OBSERVED TREATMENT SHORT-COURSE (DOTS) recommended tuberculosis control strategy by the World Health Organization (WHO)
) which is used worldwide developed by Dr. Karel Styblo in 1980s composed of five elements: 1. Political commitment with increased and sustained financing 2. Case detection through quality-assured bacteriology 3. Standardized treatment with supervision and patient support 4. An effective drug supply and management system 5. Monitoring and evaluation system and impact measurement Introduced in the Philippines in 1996 using the Revised National Tuberculosis Control Program (NTP) guidelines NATIONAL TUBERCULOSIS CONTROL PROGRAM (NTP) IN THE PHILIPPINES: Goal : Detect 70% of cases and achieve 80% cure rate Objective : To cut the chain of transmission by detecting and treating infectious TB cases (source of infection) Priority : Sputum smear-positive cases (Active TB) Primary Diagnostic Tool: Direct Sputum Smear Examination DIRECT SPUTUM SMEAR MICROSCOPY (DSSM) Principal diagnostic method adopted by the NTP because: o It provides a definitive diagnosis of active TB o The procedure is simple o Economical o A microscopy center could be put up even in remote areas DSSM Results serve as bases for categorizing TB symptomatics according to standard case definition and are used to : o Monitor progress of patient with sputum smear-positive TB while they are receiving anti-TB treatment; and o Confirm cure at the end of treatment -----------------------------------------------------------------------------------------------------------------------------------------TB Symptomatics any person with cough for two or more weeks with or without the following symptoms: fever, chest and/or back pains not referable to any musculo-skeletal disorders; hemoptysis or recurrent blood-streaked sputum; significant weight loss; and other symptoms, such as sweating, fatigue, body malaise, shortness of breath.
-----------------------------------------------------------------------------------------------------------------------------------------THE PATHOGENESIS OF TUBERCULOSIS: AN OVERVIEW TB is spread from one person to person through the air by droplet nuclei containing TB bacilli (stays in the air for 1 hour) Droplet nuclei containing tubercle bacilli are inhaled, enter the lungs, and travel to the alveoli Tubercle bacilli multiply in the alveoli
A small number of tubercle bacilli enter the bloodstream and spread throughout the body. The bacilli may reach any part of the body, including areas where TB disease is more likely to develop (such as the lungs, kidneys, brain, or bone). Within 2-10 weeks, the immune system produces special immune cells called Macrophages that surround that surround the tubercle bacilli. The cells form a hard shell that keeps the bacilli contained and under control (TB Infection). If the Immune system cannot keep the bacilli under control, the bacilli begin to multiply rapidly (TB disease). As part of the bodys defense mechanism, the body expels (cough out) the TB bacilli from the lungs through the sputum.
ACID FAST BACILLI (AFB) SPUTUM SMEAR EXAMINATION Sputum Collection Sputum - Mucoid material from the lungs brought out by means of coughing which is made-up of 95% fluids (water, mucoprotein) and 5% cellular components (e.g. squamous cells, columnar cells, alveolar macrophage) - Specimen of choice in the bacteriological examination of Pulmonary Tuberculosis Ideal Sputum Specimen o Visual Appearance: Purulent or mucopurulent Cheese-like Yellowish 3 5 ml in quantity o Microscopic Indicators: Presence of at least 25 WBCs/LPO or 4-5 WBCs/OIO Presence of alveolar macrophages or dust cells ---------------------------------------------------------------------------------Alveolar Macrophage/Dust Cell A large, irregularly shaped, phagocytic cell in the alveoli which is mainly responsible in maintaining sterility in the lungs.
--------------------------------------------------------------------------------- 2 Types of Collection According to Purpose of Examination: o Three (3) Sputum Specimens Required from a TB symptomatic to establish a case of TB (For Diagnosis) Should be collected within 2 days Sputum Collection Schedule: Day 1 - SPOT (Random) Collection 1st specimen collected at the time of consultation or as soon as TB symptomatic is identified
Day 2
- EARLY MORNING Collection o 2nd specimen collected in the morning (2-3 hours after wakingup) by the TB symptomatic when he/she is due to submit the specimen to the health facility o Will yield a high percentage of detecting (+) AFB compared to SPOT - SPOT (Random) Collection 3rd specimen collected at the time the TB symptomatic comes back to the health facility to submit the 2nd specimen.
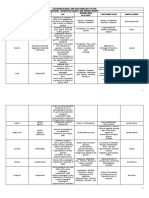
One (1) Sputum Specimen Required from a TB patient to monitor the status of the TB patient after initiation of treatment (For Follow-up) Preferable early morning specimen Sample Sputum Collection Schedule:
Towards the end of nd 2 Mo. Towards the end of rd 3 Mo. Towards the end of th 4 Mo. Towards the end of th 5 Mo. Beginning of th 6 Mo. Beginning of th 7 Mo.
Reg. I Reg. II Reg. III Reg. I
- from the time the patient was diagnosed as smear-positive after the submission of the 3 sputum specimen Reg. II -if smear-positive in 2nd month (follow-up exam), proceed to Reg. II all the way Reg. III - if smear-negative in the 2nd month (follow-up exam) Storage of Sputum Specimens o Should be kept in a cool, dark (away from sunlight) and dry place to avoid liquefaction o Can be stored at room temperature for up to 4 days only from the time of collection o When transport is needed, should be placed in a special box (sputum carrier) and stored in a cool place as possible until it is dispatched (an accompanying Laboratory Request Form which identifies the sputum specimens should be included with each transport box)
Labeling Yearly serial number and order number of sputum specimen on each side of the slide Smear Preparation 1. Fish-out enough yellowish mucopurulent or cheesy particle of the sputum with the flattened rough end of the coco midrib or the end of the wire loop 2. Spread the sputum evenly on a clean labeled glass slide o Standard size of smear is approximately 3cm. in length by 2cm. in width
3. Smear repeatedly in small, circular, coil-like pattern (must be uniform all the time) to allow penetration of the dye into the cell wall of the bacilli during staining. o Smear is considered even if sputum is fully and finely distributed in most of the smear area. o Presence of small circular coil-like pattern of smearing is an indication of an evenly spread smear.
4. Allow the smear to dry at room temperature (Do not dry it under the sun or over a flame) 5. Fix the smear by passing through the flame 2-3 times, about 2-3 seconds. Staining Ziehl-Neelsen Method for AFB Staining Leave enough space between the slides on the staining bridge to prevent the transfer of material from one smear to another. After heating the slide 2-3 times (covered with carbol fuchsin), leave the slide for 5 minutes to allow the waxy part of the bacilli to close. After staining, tilt and air-dry at room temperature using a slide rack (do not expose to sunlight) AFB is distinctly pink or red in color against a blue background Microscopic Examination Smear is of acceptable thickness if the whole depth of smear can be focused sharply, in most fields, under the microscope. Stained smear must be free from stain deposit, dirt, crystals and artifacts, which are commonly caused by overheating of stain and prolonged exposure of the slide to an open environment. Put one drop of immersion oil on the stained smear. Do not touch the smear with the dropper to avoid transfer of AFB from 1 slide to another.
Examine under 1000x objective with 10x eyepiece lens. o Standard Smear Scanning Horizontal Scanning = 150 visual fields
Vertical Scanning = 50 visual fields
Read at least 300 visual fields ( 2 Horizontal line or 6 vertical lines)
Storage of Smeared Slides Dip all examined slides in xylene for 30 minutes to remove immersion oil (separate smearpositive slides from smear-negative slides) Store in the same order of Laboratory register in the slide box Standard Reporting Scale
3+ 2+ 1+ +N 0
PHILIPPINE NATIONAL STANDARD REPORTING SCALE More than 10 AFB/OIO in at least 20 fields 1 10 AFB/OIO in at least 50 fields 10 99 AFB/100 OIO 1 9 AFB/100 OIO (Write actual no. of AFB seen) No AFB seen in 300 OIO
SPUTUM MICROSCOPY EXAMINATION LABORATORY DIAGNOSIS (Based on 3 Sputum Collection) POSITIVE - 2 out of 3 specimens or ALL specimens demonstrate AFB on stained smear NEGATIVE - NONE of the specimens demonstrate AFB on stained smear DOUBTFUL - 1 out of 3 specimens demonstrates AFB on stained smear (Collect another 3 sputum immediately
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Rite of Blessing of The Advent Wreath and CandlesDocument1 pageRite of Blessing of The Advent Wreath and CandlesDegee GonzalesNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Directory of Institutes of Consecrated Life Present in MindanaoDocument49 pagesDirectory of Institutes of Consecrated Life Present in MindanaoDegee GonzalesNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Holy Rosary GuideDocument9 pagesThe Holy Rosary GuideDegee GonzalesNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Food Microbiology Lecture Final PresDocument86 pagesFood Microbiology Lecture Final PresDegee GonzalesNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Alone With God: Grant That I May SeeDocument2 pagesAlone With God: Grant That I May SeeDegee GonzalesNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Lab DX of Fungal InfxnDocument110 pagesLab DX of Fungal InfxnDegee GonzalesNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Sacred Heart of Jesus and MaryDocument16 pagesSacred Heart of Jesus and MaryDegee GonzalesNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- 9 Day Novena To St. GerardDocument3 pages9 Day Novena To St. GerardDegee Gonzales50% (4)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- My Experience with the Missionaries of CharityDocument1 pageMy Experience with the Missionaries of CharityDegee GonzalesNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Morning & Evening and Holy Mass PrayersDocument12 pagesMorning & Evening and Holy Mass PrayersDegee GonzalesNo ratings yet
- Connectivity TroubleshootingDocument2 pagesConnectivity TroubleshootingDegee GonzalesNo ratings yet
- Histology Practice Test 2Document4 pagesHistology Practice Test 2Degee Gonzales100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Mycobacterium: Acid-Fast Bacteria Causing Tuberculosis and LeprosyDocument79 pagesMycobacterium: Acid-Fast Bacteria Causing Tuberculosis and LeprosyDegee GonzalesNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Communicative ActivitiesDocument15 pagesCommunicative ActivitiesSimona SingiorzanNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Tuberculosis Lecture Pres.Document24 pagesTuberculosis Lecture Pres.Degee GonzalesNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Mycobacteria-Part 1 LectureDocument77 pagesMycobacteria-Part 1 LectureDegee GonzalesNo ratings yet
- Mycobacterium LectureDocument39 pagesMycobacterium LectureDegee GonzalesNo ratings yet
- AFB Pictures From Dr. MesolaDocument39 pagesAFB Pictures From Dr. MesolaDegee GonzalesNo ratings yet
- Drug Resistant Tuberculosis in Southeast Asia-Status ReportDocument19 pagesDrug Resistant Tuberculosis in Southeast Asia-Status ReportDegee GonzalesNo ratings yet
- Protocol of TB TreatmentDocument15 pagesProtocol of TB TreatmentDegee GonzalesNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- New and Improved MethodsDocument16 pagesNew and Improved MethodsDegee GonzalesNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Training Module For Medical Practitioners 300309Document84 pagesTraining Module For Medical Practitioners 300309Vinoth ChellaiyanNo ratings yet
- How To Diagnosis TBDocument9 pagesHow To Diagnosis TBDegee GonzalesNo ratings yet
- Mycobacterium Africanum Subtype 1Document8 pagesMycobacterium Africanum Subtype 1Degee GonzalesNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Factsheet Tub TobDocument2 pagesFactsheet Tub TobDegee GonzalesNo ratings yet
- Lab Diagnosis of MycobacteriaDocument56 pagesLab Diagnosis of MycobacteriaDegee GonzalesNo ratings yet
- TB Sero Test Policy 2011Document2 pagesTB Sero Test Policy 2011Degee GonzalesNo ratings yet
- Ethics in TB Factsheet 28jan11revDocument2 pagesEthics in TB Factsheet 28jan11revDegee GonzalesNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Drug Resistant Tuberculosis in Southeast Asia-Status ReportDocument19 pagesDrug Resistant Tuberculosis in Southeast Asia-Status ReportDegee GonzalesNo ratings yet
- The Concept of NeuropsychiatryDocument10 pagesThe Concept of NeuropsychiatryOscar Adrian Carmona NietoNo ratings yet
- 2020 Pickaway County Fair ReportDocument9 pages2020 Pickaway County Fair ReportWSYX/WTTENo ratings yet
- Nur 097 Sas 1 3Document9 pagesNur 097 Sas 1 3gekkonoojiNo ratings yet
- Medicine in Allen: Sensitive TouchDocument38 pagesMedicine in Allen: Sensitive TouchAyeshik ChakrabortyNo ratings yet
- Progestin-Only Injectables: Characteristics and Health BenefitsDocument11 pagesProgestin-Only Injectables: Characteristics and Health BenefitsRazaria DailyneNo ratings yet
- Group 2 Research G8Document24 pagesGroup 2 Research G8aurasaliseNo ratings yet
- Drugs Acting On Blood and Blood Forming OrgansDocument42 pagesDrugs Acting On Blood and Blood Forming OrgansNazmul NabilNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaAlmira PutriNo ratings yet
- MCQ in MedicineDocument18 pagesMCQ in MedicineEslamAlmassri75% (4)
- IAS CSAT Question Paper 2011 (General Studies IIDocument76 pagesIAS CSAT Question Paper 2011 (General Studies IIAadil AnsariNo ratings yet
- Aapi Ebook June 19 2017Document621 pagesAapi Ebook June 19 2017AAPIUSANo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bannock Awareness: Celebrating Aboriginal Culture Through RecipesDocument28 pagesBannock Awareness: Celebrating Aboriginal Culture Through RecipesMaggie SedgemoreNo ratings yet
- BBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Document2 pagesBBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Manam SiddiquiNo ratings yet
- 2023061-21 Seminar On The Development and Application of Mobile PaymentDocument3 pages2023061-21 Seminar On The Development and Application of Mobile PaymentMunkhuu NasaaNo ratings yet
- CU DFScience Notes Bacteria General Dairy Micro 06 10 PDFDocument10 pagesCU DFScience Notes Bacteria General Dairy Micro 06 10 PDFjoel osortoNo ratings yet
- GASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXDocument11 pagesGASTROINTESTINAL DRUGS FOR ULCERS AND REFLUXRhealyn LegaspiNo ratings yet
- Kirit P. Mehta School of Law, Mumbai: A Project Submitted ONDocument12 pagesKirit P. Mehta School of Law, Mumbai: A Project Submitted ONNikit BaryaNo ratings yet
- Family Case Study For HydrocephalusDocument9 pagesFamily Case Study For HydrocephalusjaegergranNo ratings yet
- Essential Health Services and PlansDocument4 pagesEssential Health Services and Planszahara mahalNo ratings yet
- Photosensitizing Agents and Their Applications in PhototherapyDocument26 pagesPhotosensitizing Agents and Their Applications in PhototherapyMagesh SNo ratings yet
- GAD Database DCFDocument26 pagesGAD Database DCFBaby Jane Dedase100% (1)
- Nursing Care Plan Neonatal PneumoniaDocument2 pagesNursing Care Plan Neonatal Pneumoniaderic93% (41)
- First International congress on clinical Hypnosis & Related Sciences programDocument91 pagesFirst International congress on clinical Hypnosis & Related Sciences programGolnaz BaghdadiNo ratings yet
- Neonatal Disease Severity Scoring SystemsDocument6 pagesNeonatal Disease Severity Scoring Systemsida ayu agung WijayantiNo ratings yet
- GEHC Brochure Senographe CareDocument7 pagesGEHC Brochure Senographe CareVremedSoluCionesNo ratings yet
- Yes, aside from the educational SMS intervention, the groups were treated equally as they both received routine trainingDocument54 pagesYes, aside from the educational SMS intervention, the groups were treated equally as they both received routine trainingYogiNo ratings yet
- Discussion Topics: Seafood Red ListDocument3 pagesDiscussion Topics: Seafood Red ListНадія ЛупійNo ratings yet
- Embryonic Development and OrganogenesisDocument33 pagesEmbryonic Development and OrganogenesisMariam QaisNo ratings yet
- Project Report For 9000Document10 pagesProject Report For 9000GOLLAVILLI GANESH100% (1)
- Gastrointestinal Tract Infections: General ConsiderationsDocument17 pagesGastrointestinal Tract Infections: General ConsiderationsDarpan GelalNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)