Professional Documents
Culture Documents
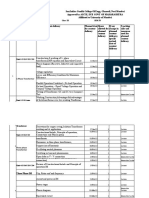
Assessment, Images Background
Uploaded by
sunkissedchiffonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment, Images Background
Uploaded by
sunkissedchiffonCopyright:
Available Formats
working with imagery: background
(this handout is based on a couple of blog posts on www.stressedtozest.com dated 6 & 8.03.13) A high percentage of chronic pain sufferers seem to be affected by recurrent imagery that is linked to and aggravates their pain. Often the imagery's occurrence only emerges with careful questioning. "Rescripting" these images is associated with impressive short term improvements in pain and distress. What's exciting is the potential for longer term benefits from this kind of rescripting approach ... not only for chronic pain sufferers but also for people suffering from other persistent distressing states like depression and anxiety. Clare Philips, a researcher at the Rehabilitation Centre in Richmond, Canada, has written a couple of fascinating research papers on this topic. The first - published in 2011 - is entitled "Imagery and pain: The prevalence, characteristics, and potency of imagery associated with pain" . Its abstract reads "The images of 59 pain sufferers were assessed by means of a semi-structured interview. The emotional, cognitive, behavioural, and pain-inducing properties (potency) of their index images were assessed by an image induction procedure and self-report scales of anxiety, depression and trauma symptoms. Results: The results showed a remarkably high incidence of images in pain sufferers, with 78% of participants reporting one or more repetitive images when in pain. Exposure to their most powerful/distressing image (Index image) resulted in significant increases in negative emotions, negative cognitive appraisals, and in pain levels. In a sub-group of sufferers with significant levels of trauma symptoms, the index images elicited significantly higher levels of emotion and pain increment than did those respondents in a low/no trauma group. Conclusion: It was concluded that imagery is a prevalent, often "unobserved" but potent cognition in pain sufferers. The implications for CBT approaches to chronic pain, including image rescripting, are considered." The pain sufferers assessed in this trial had all been referred to an 8 to 10 week programme at a Canadian Occupational Rehabilitation Centre through a Workers Compensation Board or insurance companies. Philips commented "These sources refer only those people whom they feel will be returning to work after the program of supervised exercise and work-hardening. People with psychological problems (i.e. alcoholism, drug dependence, post-traumatic stress disorder, anxiety disorders) are referred to (other) specialized clinics." So these patients, described by Philips below, were probably troubled by fewer comorbid psychological difficulties than many other groups of pain sufferers. The research paper noted "The mean age of the participants was 45.6 (SD = 10.5) ... Most (88%) reported pain onset directly linked to a work-related accident, while 8.5% reported a motor vehicle accident. Average pain levels in the preceding 2 weeks (0-10 scale, where 10 = unendurable pain) were estimated by participants as 4.99 (SD = 1.67) and peak pain was estimated at 7.1 (SD = 2.1). The chronicity of their current pain problem was 37.4 weeks (SD = 2.97) ... Litigation was ongoing for only 5 of 59 participants." The trauma history is interesting here, although it seems that those diagnosed as suffering from full PTSD were referred elsewhere. It's well worth noting that Philips found she needed to be careful how she asked about pain associated imagery. Some patients apparently became upset by these questions, feeling that the researcher was suggesting that they were in some way "imagining" their pain. Philips wrote "To clarify the presence and content of any mental imagery, two open-ended questions were used. (The first question was used merely as a smooth transition into an enquiry about imagery. The replies to this first
question were not analyzed in this study.) Q1: People experiencing pain think about many things. Tell me about some of the thoughts that keep coming back into your mind when you are in pain. Once their thoughts had been noted, the key question for this study was asked. Q2: Do you also sometimes see picture thoughts? Thoughts which you picture to yourself when you are in pain? . . . that pop in to your mind when you are in pain? (An alternative [Cont] question was used if the participants appeared not to understand the initial question: "Do you visualize your thoughts when in pain? Tell me some of your picture thoughts associated with pain that pop in to your mind when you are in pain.")" Fascinatingly and probably importantly Philips found that "the pain thoughts were easily, quickly and unemotionally disclosed. The descriptions were general and without personal or idiosyncratic content (such as, when will I ever get better?). However, participants found the pain images difficult to articulate, and they were frequently accompanied by high levels of emotional response (i.e. tears, weeping, loss of eye-contact, flushing). The images were replete with personal details." This dovetails very well with the general finding that imagery tends to be more linked with emotions than verbal thoughts are, and that this often makes imagery particularly important and helpful to work with therapeutically. Apparently "Frequently the occurrence of imagery was not reported initially by participants but once the type of cognition was clarified (if necessary with an example: seeing a pink elephant), imagery reports were obtained. Participants were given time to consider the questions, as the phenomenon of image cognitions appeared novel to them. Few participants made a distinction between thoughts and mental images prior to the interview. Only visual images were investigated in this study. Once the image(s) had been recorded, the participants were asked which of their images they felt was the most powerful/disturbing. This became the "Index" image that was used exclusively for the subsequent questions regarding characteristics and effects of the image." I have a query here about selecting only one image to work with if one was using this approach as a treatment ... although I can see the sense in keeping things simple for the purposes of this exploratory research study. In an earlier post about the treatment of posttraumatic stress disorder, I wrote "In a typical severe trauma there are likely to be several "hot spots" of particularly intense emotion. These hot spots are crucial therapeutic targets as they are often sections of memory that are most disorganized and that are key sources of self-damaging misunderstanding." Philips noted that "The average number of images reported was 2.47 (range 1-6)." In a thera-peutic setting I would ask about the frequency of and level of distress associated with the differ-ent images and I would certainly consider rescripting all of the more severely upsetting images. In Clare Philips' research study "Imagery and pain: The prevalence, characteristics, and potency of imagery associated with pain" she wrote "the characteristics of the Index image were assessed (frequency, similarity, persistence and clarity of image). Once the Index image had been fully described, respondents were asked about image meaning: What does this picture mean to you, your future or your life?" Links between the images and actual memories were discussed. Then participants took part in a "Voluntary Image Exposure procedure" where they were asked to form the image and then answer questions about them. They could do so with eyes open or closed. All formed their index image within seconds of the request, and were able to answer questions about image characteristics as well as their emotions, pain and behavioural response to the image, using "analogue scales ... from 0 (none) to 10 (maximum levels) of anxiety, sadness, anger, happiness, and calm. The cognitive scales of believed threat and physical and/or emotional fragility (defined as easily broken, weak) were assessed using analogue scales from 0 (no belief) to 10 (maximum belief/conviction). The pain scale used was from 0 (no pain) to 10
(unendurable pain)." Philips noted that "In response to an open-ended question, participants found it difficult to articulate a single or predominant meaning of their index image. Few had considered meaning prior to the question being asked by the investigator. The result was frequently a number of answers with respect to image meaning. Presenting them with a discrete number of meaning categories to choose from also had limita-tions. Often more than one category was chosen, as in the following example. "I see myself sitting alone in my wheelchair. I am old and unable to care for myself ". When asked about the meaning of her image, the 35-year old women replied it meant she would be a burden to her children in the future. Presented with a number of meaning categories, she chose five: future catastrophe, physical disability, absence of control, unhappiness, and dependence. In addition to the [Cont.] openended and categorical approaches to defining image meaning, the experimenter classified participant responses into the predominant categories. Nearly 1/4 (23%) gave negative self-appraisals (i.e. "I am a loser"). A future catastrophe was described by 28.2% and a past cata-strophe (accident or other past trauma) was described by 12.8% ... The relation of the image to past memories was assessed using categories: 34.1% reported the image was connected to their memory of the causative accident that had led to their pain problem; 18.2% felt the image came from memories of family worries, and 13.6% identified memories of their work situation. As can be seen in the examples below, this classification does not do justice to the complexities and details of many of the reported images. - "I see my mother needing me. She is upset and I can not help. She can't get out of a dark dungeon." (classified by participant as: Memories of family concern/worries). - "My body is crying, and I feel it. I can't move and it is solid and tight. Others look at me wanting to help ... their eyes look at me." (classified by participant as: Memories idiosyncratic). - "I see the ugly faces of the irresponsible management ... the unethical things they are doing ... the threats and intimidation. The pictures open like an umbrella". (classified by participant as: Memories of work situation). - "I see an old woman with a cane ... curved over. I look under her hood - it is ME!" (image of a women in her 20s) (classified by participant as Memories idiosyncratic)." Philips went on to write "The causal event is not always present in the image. The past event may have occurred sometime before, even a memory from childhood 40 years earlier. One catastr-ophic event (causal accident) appears not infrequently to lead to memories/images of a previous trauma event. Catastrophic consequences (not experienced by the participant) may be elaborated in the memory of the causative accident. Catastrophic future worries may also be visualized ... In summary, imagery was found to be a common though even if "unobserved" form of cognition in these pain sufferers. When assessing their index image, participants reported frequent, clear, brief and unchanging content. The appraisal of the image meaning proved complex. Participants appeared perplexed, and endorsed a number of meaning categories. However, categorization of meaning statements showed that the majority were focused upon negative self-appraisal and predicted catastrophe." Using simple 0 (0 = none) to 10 (10 = maximum levels) scales, assessment was made of changes in mood and pain brought on when the pain sufferers visualised their most upsetting image. The effects were dramatic on all the measured emotions and on the pain too. So average increases in anxiety, sadness & anger were 48%, 68% & 103% respectively. Average decreases in happiness & calm were 66% & 46%. And in the few brief minutes of stationary visualisation, pain levels increased
by an average of 25%. Although people suffering from diagnosed posttraumatic stress disorder (PTSD) were referred to other, more specialised clinics, even in this Rehabilitation Centre based study, pain sufferers who scored higher on PTSD scales tended to report more frequent and more upsetting pain images. Overall though, only about a third of all described images were actually of accidents leading to the pain. As a therapist my mind starts to whirl here. Repetitive intrusive images appear to be much more common amongst chronic pain sufferers than I would have guessed. How much is this also true for other distressed states like depression & anxiety? Fascinatingly the majority of these pain-associated images do not seem to be about the accident that caused the problem, and the mean- ings linked to the images particularly involved "negative self-appraisal and predicted catastrophe. Researchers have put in a lot of work on the relevance of images in depression & anxiety as well, but my strong impression is that the focus has been on traumatic experiences rather than the broader & more mixed picture highlighted by this pain research - see for example the 18 slides on "The importance of traumatic memories" that I put together for a talk I gave a few years ago on this subject and listed further down the "Good knowledge" page "Life review, traumatic [Cont.] memories & therapeutic writing" . The pain-linked images described in this research study are clearly therapeutically relevant. The severe worsening in symptoms triggered by bringing the images to mind shows that they are not just irrelevant, peripheral aspects of the sufferers' experience. In the next post I will describe Clare Philips' follow-on research demonstrating that altering the images powerfully alters the associated pain & distress. It will be fascinating to explore the potential clinical relevance of these findings for chronic pain sufferers and for other distressed states too. To help with this process I have put together an imagery assessment questionnaire and a frequency/severity assessment.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- BeGudd - Issue Nr. 6 2020Document80 pagesBeGudd - Issue Nr. 6 2020sunkissedchiffon38% (53)
- Assessment, Experiencing Scale - 1Document2 pagesAssessment, Experiencing Scale - 1sunkissedchiffonNo ratings yet
- Assessment, Experiencing Scale - 1Document2 pagesAssessment, Experiencing Scale - 1sunkissedchiffonNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Assessment, Iapt, Ph9, EtcDocument1 pageAssessment, Iapt, Ph9, EtcsunkissedchiffonNo ratings yet
- Assessment, Interpersonal Iip-48, TDocument3 pagesAssessment, Interpersonal Iip-48, TsunkissedchiffonNo ratings yet
- Appellants' Reply BriefDocument20 pagesAppellants' Reply BriefAnita Belle100% (1)
- STRUCTURAL EQUATION MODELING : DETERMINANTS OF ORGANIZATIONAL COMMITMENTS AND ITS IMPLICATION ON EMPLOYEE WORK PRODUCTIVITY OF MANAGERIAL LEVEL ASEP SUTARMAN, ANOESYIRWAN MOEINS AND RAHMAD EVAN PURNAWANDocument16 pagesSTRUCTURAL EQUATION MODELING : DETERMINANTS OF ORGANIZATIONAL COMMITMENTS AND ITS IMPLICATION ON EMPLOYEE WORK PRODUCTIVITY OF MANAGERIAL LEVEL ASEP SUTARMAN, ANOESYIRWAN MOEINS AND RAHMAD EVAN PURNAWANGSA publishNo ratings yet
- Moot MemorialDocument33 pagesMoot MemorialVivek Singh100% (1)
- The Shame Experiences of The Analysts-R Stein PDFDocument8 pagesThe Shame Experiences of The Analysts-R Stein PDFsunkissedchiffonNo ratings yet
- B08LT728MSDocument501 pagesB08LT728MSSandy FireNo ratings yet
- Assessment, Life HighlightsDocument1 pageAssessment, Life HighlightssunkissedchiffonNo ratings yet
- Assessment, Knee LequesneDocument2 pagesAssessment, Knee LequesnesunkissedchiffonNo ratings yet
- HDS Manual PDFDocument73 pagesHDS Manual PDFsunkissedchiffon100% (1)
- Assessment, Intrusive Memories - 0Document2 pagesAssessment, Intrusive Memories - 0sunkissedchiffonNo ratings yet
- Assessment, Expectancy & CredibilityDocument2 pagesAssessment, Expectancy & CredibilitysunkissedchiffonNo ratings yet
- Assessment, Images RescriptingDocument2 pagesAssessment, Images RescriptingsunkissedchiffonNo ratings yet
- Assessment, Images DetailsDocument3 pagesAssessment, Images DetailssunkissedchiffonNo ratings yet
- Assessment, Images TreatmentDocument4 pagesAssessment, Images TreatmentsunkissedchiffonNo ratings yet
- Assessment, Images WeekDocument2 pagesAssessment, Images WeeksunkissedchiffonNo ratings yet
- Assessment, Ibs Severity, TDocument3 pagesAssessment, Ibs Severity, TsunkissedchiffonNo ratings yet
- Assessment, Hip & Knee ScoreDocument1 pageAssessment, Hip & Knee ScoresunkissedchiffonNo ratings yet
- Hip Pain Assessment Form: Date Name Points I - Pain or DiscomfortDocument2 pagesHip Pain Assessment Form: Date Name Points I - Pain or DiscomfortsunkissedchiffonNo ratings yet
- Assessment, Fatigue TirednessDocument2 pagesAssessment, Fatigue TirednesssunkissedchiffonNo ratings yet
- Assessment, Espie Diary FormDocument2 pagesAssessment, Espie Diary FormsunkissedchiffonNo ratings yet
- Assessment, Fatigue SeverityDocument1 pageAssessment, Fatigue SeveritysunkissedchiffonNo ratings yet
- Assessment, Espie Overall ProgressDocument1 pageAssessment, Espie Overall ProgresssunkissedchiffonNo ratings yet
- Assessment, Disability, 0-8 Five Areas, ScoringDocument1 pageAssessment, Disability, 0-8 Five Areas, ScoringsunkissedchiffonNo ratings yet
- Assessment, Diener Swls BackgroundDocument3 pagesAssessment, Diener Swls BackgroundsunkissedchiffonNo ratings yet
- Assessment, Erectile Dysfunction ScoringDocument1 pageAssessment, Erectile Dysfunction ScoringsunkissedchiffonNo ratings yet
- Assessment, Erectile Dysfunction ScaleDocument1 pageAssessment, Erectile Dysfunction ScalesunkissedchiffonNo ratings yet
- Assessment, Dyadic Adjustment ScoringDocument1 pageAssessment, Dyadic Adjustment ScoringsunkissedchiffonNo ratings yet
- Assessment, Diener SwlsDocument1 pageAssessment, Diener SwlssunkissedchiffonNo ratings yet
- Emailing PROG PINAGSAMA 3112 AT 3113 NAND2 EIN PERIODICAL PDFDocument2,600 pagesEmailing PROG PINAGSAMA 3112 AT 3113 NAND2 EIN PERIODICAL PDFNathaniele Lean CastroNo ratings yet
- Ethics PPT.3Document21 pagesEthics PPT.3Ronalyn CasanovaNo ratings yet
- Intro For Guest SpeakerDocument2 pagesIntro For Guest Speakerdatabasetechnology collegeNo ratings yet
- Answer Book: College of Management & TechnologyDocument6 pagesAnswer Book: College of Management & TechnologyOmar RafieNo ratings yet
- R.A. 9512Document11 pagesR.A. 9512Marc Keiron Farinas33% (3)
- Distinguishing Between Fact and OpinionDocument2 pagesDistinguishing Between Fact and OpinionnadiaNo ratings yet
- From Mass To Popular Culture - Short Ess PDFDocument1 pageFrom Mass To Popular Culture - Short Ess PDFHelmunthTorresContrerasNo ratings yet
- UnilabDocument6 pagesUnilabKim LaguardiaNo ratings yet
- Gyford Catalog 2015 enDocument164 pagesGyford Catalog 2015 enAnonymous NwnJNONo ratings yet
- Class Se Sem Iv Academic Year:2021-22Document55 pagesClass Se Sem Iv Academic Year:2021-22utkarsha sonekarNo ratings yet
- Jawaban Case 4Document5 pagesJawaban Case 4Friista Aulia Labiba100% (1)
- Tess Study QuestionsDocument3 pagesTess Study QuestionsIsrar KhanNo ratings yet
- Are Famous People Treated Unfairly by The MediaDocument1 pageAre Famous People Treated Unfairly by The MediaChu Thế AnhNo ratings yet
- Caltex Filipino Managers and Supervisors Assn vs. CIR GR No. L-30632-33Document6 pagesCaltex Filipino Managers and Supervisors Assn vs. CIR GR No. L-30632-33King KingNo ratings yet
- Consequences of Power Distance Orientation in Organisations: Vision-The Journal of Business Perspective January 2009Document11 pagesConsequences of Power Distance Orientation in Organisations: Vision-The Journal of Business Perspective January 2009athiraNo ratings yet
- Proforma Mte 3113 - Action Research I - Primary Mathematics Methodology)Document6 pagesProforma Mte 3113 - Action Research I - Primary Mathematics Methodology)MUHAMMAD RIDHUAN BIN HANAFINo ratings yet
- Auditing Theory Chapter 5Document13 pagesAuditing Theory Chapter 5Almira BesoniaNo ratings yet
- Honduras 2023. Constitutional CrisisDocument3 pagesHonduras 2023. Constitutional CrisismoracunaNo ratings yet
- SACCO, Rodolfo. Legal Formants. A Dynamic Approach To Comparative Law (Installment II)Document59 pagesSACCO, Rodolfo. Legal Formants. A Dynamic Approach To Comparative Law (Installment II)Federalist_PubliusNo ratings yet
- Case Study - 5Document11 pagesCase Study - 5krati123chouhanNo ratings yet
- A cn4 507Document109 pagesA cn4 507amallaNo ratings yet
- HSI-Safety Plan-2019Document8 pagesHSI-Safety Plan-2019Arvin Omboy100% (1)
- The Kindhearted SparrowDocument8 pagesThe Kindhearted Sparrowpjas0001No ratings yet
- GP Essay Skills 2012Document13 pagesGP Essay Skills 2012Audrey JongNo ratings yet
- SocratesDocument9 pagesSocratesKathHinlogNo ratings yet
- Domingo Roco Vs Hon. Contreras Rem - RevDocument2 pagesDomingo Roco Vs Hon. Contreras Rem - RevVanessa100% (1)
- The Enlightenment and The American RevolutionDocument8 pagesThe Enlightenment and The American RevolutionBevynNo ratings yet