Professional Documents
Culture Documents
Strategies For Working With Delusions
Uploaded by
Hannah Grace Protasio LumongsodOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Strategies For Working With Delusions
Uploaded by
Hannah Grace Protasio LumongsodCopyright:
Available Formats
1
STRATEGIES FOR WORKING WITH DELUSIONS Toni Rose G. Gimenez, RN 1. Establish a trusting, interpersonal relationship. Do not reason, argue, or challenge the delusion. Attempting to disprove the delusion is not helpful. Assure the person that it is safe and no harm will come. Do not leave the person alone, use openness and honesty at all times. Encourage the person to verbalize feelings of anxiety, fear and insecurity. Offer concern and protection to prevent injury to self and others. Convey acceptance of the need for the false belief. It is more helpful to talk about the experience that may have triggered the delusion. Center on the patient as a person, rather than on the need to control symptoms. Remain calm. 2. Identify the content or type of delusion. Assist in understanding the patient and the purpose of delusion. Clarify any confusion about the verbalization by asking what the patient is saying. If you do not attempt to clarify confusion, the result may be even greater confusion, anxiety and reaffirmed delusion. Identify the presence of a central topic. Identify the presence of a central feeling tone. 3. Investigate the meaning of the delusion. Assess areas in the persons life he can no longer manage, control or participate in. Assess the concrete ways the delusion interferes with functioning or may explain malfunctioning to the person. Ask whether the person has taken action based on the delusion. Without agreeing or arguing, question
the logic or reasoning behind the delusion. 4. Assess the intensity, frequency and duration of the delusion. Fleeting delusions are able to be worked with in a short time frame. Fixed delusions that have endured over a long time may have to be temporarily avoided in order to prevent them from becoming stumbling blocks in the relationship. Does the person always greet you with the delusion? If so, quietly listen and then give direction for the task at hand. If it appears the patient cannot stop talking about the delusion, ask gently if he recalls what you have been doing and that its time to resume that activity. If the patient is very intent on telling the delusion, just quietly listen until there is no need to discuss it any further. Remember, it is helpful to give the person reassurance during the delusion that he as a person is okay. 5. Identify what triggered the delusion. Assess for a change in the persons ability to manage activities of daily living, since delusions can be triggered by minor changes such as alterations in the daily schedule. Anything that is potentially disruptive to the person can trigger delusions. 6. Identify current major stresses. Assess if the person is under exaggerated stress (financial, family or job difficulties). 7. Correlate the onset of the delusion with the onset of the stress. Help the patient connect the false beliefs to time of increased anxiety; if the person is able to interrupt escalating anxiety, delusional thinking may be prevented.
Becoming anxious and avoiding the person. 8. If the patient asks you directly if you believ the delusion, respect that this is the patients experience. Always present reality to the patient who is delusional, without listening or invalidating his perceptions. Reinforce and focus on reality. Talk about real events and real people using real situations to divert the patient away from a long, rambling conversation. 9. Identify emotional needs the delusion may be meeting. Respond to the underlying feelings rather than the illogical nature of the delusion. This will encourage discussions of fears, anxieties, or anger without assuming the delusion is right. The person generally attaches the emotional tone of the first experience of the delusion to each successive experience with that particular delusion. Use the process of the conversation rather than the content by reflecting the feeling the feeling back to the patient. 10. Promote activities that require attention, physical skills, or action. When a persons energy is diverted, pathological thinking is interrupted, satisfying activities will help the person give up time used in delusional thinking. 11. Recognize healthy aspects of the patients personality. This will help the patient to doubt own delusional perceptions. 12. Structure situations so it is difficult to spend time in a delusional system, this encourages alternative methods of meeting needs. BARRIERS TO SUCCESSFUL INTERVENTION FOR DELUSION This leads to annoyance, anger, a sense of hopelessness and failure, feelings of inadequacy, and potential laughing at the patient. Reinforcing the delusion. Do not go along with the delusion, especially to get cooperation of the patient. Attempting to prove the person is wrong. Do not attempt a logical explanation. Setting unrealistic goals. Do not underestimate the power of a delusion and the patients need for it. Becoming incorporated into the delusional system. This will cause greater confusion for the person and make it possible to establish boundaries of the therapeutic relationship. Failing to clarify confusion surrounding the delusion. If the nurse does not clearly understand the complexity and many intricacies of the delusion, the delusion will become more elaborate. Being inconsistent in intervention. The intervention plan must be firmly adhered to. Try anything approaches lead to inconsistency and the person is less able to identify reality. Seeing the delusion first and the person second. Avoid saying the person who thinks hes being poisoned. STRATEGIES FOR WORKING WITH PATIENTS WITH HALLUCINATIONS 1. Establish a trusting, interpersonal relationship.
If you want the person to open up, you must express feelings in an open, honest and direct manner. You will elicit the behavior you emit- if you are frightened, the individual will be frightened. Have as consistent a routine as possible. Be patient, show acceptance, and listen. Always remember the individual is experiencing anxiety, fear, loneliness, and low self-esteem, and the brain is not processing stimuli accurately. 2. Assess for symptoms of hallucination. Look at and listen to the person for clues the hallucination is in the beginning level of intensity. Behavioral clues include grinning or laughing inappropriately, moving lips without speaking, rapid blinking, slow verbal responses, silence, or making frequent telephone calls. Be Patient and listen when the patient is ready to talk. 3. Focus on the symptom and ask the person to describe what is happening. The goal is to empower the person by helping understand the symptoms experienced or demonstrated. This helps the person gain control of the illness, seek help, and hopefully prevent the hallucination from reaching a greater level of intensity. Be patient and use active listening techniques.
manage symptom intensity. The combination of brain disease and drugs or alcohol may cause irreparable harm and promote a long relapse. 6. Help the person describe and compare the present and recently past hallucination. You need to find out what the person is seeing, hearing, tasting, touching, or smelling to begin to discover if a pattern exists. Encourage the person to remember when hallucinations first began. This process is similar to taking medical history regarding any other symptoms. It is nearly impossible to understand the present without a clear understanding of the past.
4. Identify if drugs and/or alcohol has been used. You need to find out if the person is using street drugs and/or alcohol. You need to teach that this is extremely dangerous and a general rule of thumb is that one beer will act like a six-pack. Many persons turn to illicit drugs or alcohol as a coping mechanism or as a quick means to
7. Encourage the person to observe and describe thoughts, feelings, and actions, both present and past, as they relate to the hallucination. Frequently, people with schizophrenia appear to be able to turn their symptoms on and off. Many have learned how to survive this illness by covering up symptoms to appear normal. It takes tremendous energy and concentration to control the illness. If you listen for at least 15 minutes, the person will usually be able to talk about their cognitive and perceptual symptoms and provide clues to the underlying psychosis. Remember not to imply blame, since everyone involved in patient care shares in the responsible management of this illness. 8. Help the person describe needs that may be reflected in the content of the hallucination. Emotional needs can be categorized into four: a. ability to express anger b. having power and control of decisions that affect daily life
c. feeling ego syntonic(attuned to) with sexuality d. experiencing positive self-esteem
human
8. Help the person describe needs that may be reflected in the content of the hallucination. If one or more of these needs are not met for any of us(family members, consumers, providers) we also will experience emotional distress. Try to step into the shoes of an individual with brain disease who is already impaired in the ability to accurately interpret reality. Then add the effects of extra stress of unmet needs. For survival of the self, hallucinations may partially reflect these unmet needs.
11. Identify how other symptoms of psychosis have affected the persons ability to carry out activities of daily living. This means sharing your concerns and providing feedback regarding persons general behavioral responses. By assisting the person with the symptom identification and recognition of the effect of symptoms on ADL, self esteem will be increased, anger will be diffused, and the person will feel in control of the symptoms instead of feeling that the symptoms are in control.
9. Help the person identify if there is a correlation between the hallucination and the needs it may be reflecting. Focus on the unmet emotional need the person may be experiencing and discuss if there is a relationship with the appearance of hallucinations. Encourage the person to keep a chart or calendar of when hallucinations occur and how long they last in an effort to identify the trigger.
10 . Suggest and reinforce the use of interpersonal relationships in meeting the need. It is important to find one individual who will give honest feedback to help the person sort out reality from the hallucination. This individual must be readily accessible to the patient. Remember that anxiety reduction is the key intervention to interrupting hallucinations.
You might also like
- CV Vivek Benegal 0610Document16 pagesCV Vivek Benegal 0610bhaskarsg0% (1)
- Recreational Therapy: Ms. Priyanka Kumari F.Y. M.Sc. NursingDocument22 pagesRecreational Therapy: Ms. Priyanka Kumari F.Y. M.Sc. NursingHardeep KaurNo ratings yet
- Depressive Disorders Social Isolation/Impaired Social InteractionDocument5 pagesDepressive Disorders Social Isolation/Impaired Social InteractionYannesa S. Bantilan - Balbin100% (2)
- G CBT For DelusionDocument23 pagesG CBT For DelusionIoana DarjanNo ratings yet
- Psychology Assignment 3Document5 pagesPsychology Assignment 3sara emmanuelNo ratings yet
- Issues Faced by TherapistDocument2 pagesIssues Faced by TherapistMarianne DalmacioNo ratings yet
- P.Vijayalakshmi Reddy, MSN NimhansDocument51 pagesP.Vijayalakshmi Reddy, MSN NimhansVijaya LakshmiNo ratings yet
- Bernard Gallagher Cap. 5 Sociology of Mental IllnessDocument16 pagesBernard Gallagher Cap. 5 Sociology of Mental IllnessLaura CristinaNo ratings yet
- Causes and Risk Factors For Attention-Deficit Hyperactivity DisorderDocument8 pagesCauses and Risk Factors For Attention-Deficit Hyperactivity DisorderFranthesa LayloNo ratings yet
- The Suicidal ClientDocument18 pagesThe Suicidal ClientReet_paed100% (2)
- Internet Addiction (TLE)Document25 pagesInternet Addiction (TLE)April PalamosNo ratings yet
- Stages of Psychotherapy Process: Zsolt UnokaDocument15 pagesStages of Psychotherapy Process: Zsolt UnokaNeil Retiza AbayNo ratings yet
- Transformational AssertivenessDocument13 pagesTransformational AssertivenessPanchali_rNo ratings yet
- MSE and History TakingDocument17 pagesMSE and History TakingGeetika Chutani18No ratings yet
- Psychosocial Theory of SchizophreniaDocument16 pagesPsychosocial Theory of SchizophreniaJona JoyNo ratings yet
- Indian Mental Disability ActDocument78 pagesIndian Mental Disability ActVinit YadavNo ratings yet
- WHODAS2.0 36itemsPROXYDocument5 pagesWHODAS2.0 36itemsPROXYJarmy BjNo ratings yet
- Short Michigan Alcohol Screening Test (Smast) : NAME: - DateDocument2 pagesShort Michigan Alcohol Screening Test (Smast) : NAME: - DateKrithika MalhotraNo ratings yet
- Introduction To Psychological InterventionsDocument26 pagesIntroduction To Psychological InterventionsJay Mark Cabrera100% (1)
- Substance Related Disorders - UpdatedDocument24 pagesSubstance Related Disorders - Updatedapi-334763728No ratings yet
- FRAMES CounsellingDocument2 pagesFRAMES CounsellingLIDIYA MOL P V100% (1)
- Dissociation DisorderDocument33 pagesDissociation DisorderVaibhav KrishnaNo ratings yet
- Suicide Risk and Assessment of Suicide-1Document33 pagesSuicide Risk and Assessment of Suicide-1Omeerul RafieNo ratings yet
- Mental Health Self CareDocument34 pagesMental Health Self CareRALLIEGH VIZCARRA100% (1)
- Schema TherapyDocument5 pagesSchema TherapyATHINA METAXANo ratings yet
- Legal and Ethical Issues in PsychotherapyDocument69 pagesLegal and Ethical Issues in PsychotherapyRhea Andrea UyNo ratings yet
- Assisted Outpatient Treatment in New York State: The Case For Making Kendra's Law PermanentDocument16 pagesAssisted Outpatient Treatment in New York State: The Case For Making Kendra's Law PermanentManhattan InstituteNo ratings yet
- Psychotherapy ReportDocument7 pagesPsychotherapy ReportEileen Medina CostoNo ratings yet
- Chapter 10 Basic Features of Clinical InterventionDocument3 pagesChapter 10 Basic Features of Clinical InterventionKathleenNicole De Castro EnfectanaNo ratings yet
- Psych Case StudyDocument14 pagesPsych Case StudySmridhi Seth100% (1)
- Bullying Is An Ongoing and Deliberate Misuse of Power in Relationships Through Repeated VerbalDocument4 pagesBullying Is An Ongoing and Deliberate Misuse of Power in Relationships Through Repeated VerbalAngelNo ratings yet
- Family TherapyDocument8 pagesFamily TherapyManoj NayakNo ratings yet
- Apsy 603 Dual Relationship Assignment 4Document18 pagesApsy 603 Dual Relationship Assignment 4api-161848380100% (1)
- Out of the Silence: My Journey into Post-Traumatic Stress Disorder and BackFrom EverandOut of the Silence: My Journey into Post-Traumatic Stress Disorder and BackNo ratings yet
- Cns 6161 Treatment Plan - WalterDocument7 pagesCns 6161 Treatment Plan - Walterapi-263972200No ratings yet
- MHN: Unit XV: Adjustment and Impulse Control Disorders Adjustment DisordersDocument12 pagesMHN: Unit XV: Adjustment and Impulse Control Disorders Adjustment Disordersmadhurima kunduNo ratings yet
- Neuropsychiatric Complications of Alcohol Dependence SyndromeDocument54 pagesNeuropsychiatric Complications of Alcohol Dependence Syndromedrkadiyala2100% (2)
- Disruptive Impulse Control and Conduct Disorders 2Document120 pagesDisruptive Impulse Control and Conduct Disorders 2Sana100% (1)
- Counselling Pschology UNIT-1Document7 pagesCounselling Pschology UNIT-1NehaNo ratings yet
- Conduct DisordersDocument17 pagesConduct DisordersMamta PooniaNo ratings yet
- Interpersonal PsychotherapyDocument21 pagesInterpersonal PsychotherapyDr. Jayesh PatidarNo ratings yet
- Impulsive DisordersDocument21 pagesImpulsive DisordersAli B. SafadiNo ratings yet
- Healing Inside Out And Outside In: Finding Zen through Spriritual HealingFrom EverandHealing Inside Out And Outside In: Finding Zen through Spriritual HealingNo ratings yet
- From Nope to Hope: How I Overcame My Suicidal Thoughts (and How You Can Too)From EverandFrom Nope to Hope: How I Overcame My Suicidal Thoughts (and How You Can Too)No ratings yet
- Diagnostic FormulationDocument8 pagesDiagnostic FormulationAnanya ReddyNo ratings yet
- SchizophreniaDocument4 pagesSchizophreniaVin Grace Tiqui - GuzmanNo ratings yet
- Counselling TheoriesDocument15 pagesCounselling TheoriesPranavi KhandekarNo ratings yet
- The General Well-Being Scale PDFDocument5 pagesThe General Well-Being Scale PDFMyOdysseyNo ratings yet
- Bipolar Disorder Bipolar DisorderDocument3 pagesBipolar Disorder Bipolar DisorderJorgeNo ratings yet
- Mood Disorders - DepressionDocument58 pagesMood Disorders - Depressionmaha abdallahNo ratings yet
- Informed Consent DocumentDocument4 pagesInformed Consent Documentapi-600986693No ratings yet
- NOTES Groups HepworthDocument4 pagesNOTES Groups Hepworthejanis39No ratings yet
- Growth and Development: Yarsi School of MedicineDocument32 pagesGrowth and Development: Yarsi School of MedicineLia Noor AnggrainiNo ratings yet
- Case Study Jared Tacey Youngstown State UniversityDocument13 pagesCase Study Jared Tacey Youngstown State Universityapi-402076669100% (1)
- Renal Physio #1 - Fluid and Electrolyte Notes (Dr. Nobleza)Document3 pagesRenal Physio #1 - Fluid and Electrolyte Notes (Dr. Nobleza)Hannah Grace Protasio LumongsodNo ratings yet
- Basic Mycology For PGIsDocument260 pagesBasic Mycology For PGIsHannah Grace Protasio LumongsodNo ratings yet
- DMSF Apa FormatDocument1 pageDMSF Apa FormatHannah Grace Protasio LumongsodNo ratings yet
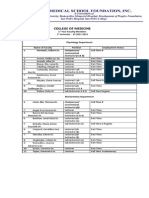
- College of Medicine: 1 Year Faculty Members 1 Semester - SY 2011-2012Document3 pagesCollege of Medicine: 1 Year Faculty Members 1 Semester - SY 2011-2012Hannah Grace Protasio LumongsodNo ratings yet
- Angel Lord Soul Family GoodDocument1 pageAngel Lord Soul Family GoodHannah Grace Protasio LumongsodNo ratings yet
- NRES Seminar CertificateDocument10 pagesNRES Seminar CertificateHannah Grace Protasio LumongsodNo ratings yet
- Breast Self ExamDocument6 pagesBreast Self ExamHannah Grace Protasio LumongsodNo ratings yet
- Course in The HospDocument1 pageCourse in The HospHannah Grace Protasio LumongsodNo ratings yet
- Laboratory Study: Determinants Actual Values Normal Values Interpretation Clinical Significance Nursing ResponsibilitiesDocument1 pageLaboratory Study: Determinants Actual Values Normal Values Interpretation Clinical Significance Nursing ResponsibilitiesHannah Grace Protasio LumongsodNo ratings yet
- Bse, Pap, DreDocument13 pagesBse, Pap, DreHannah Grace Protasio LumongsodNo ratings yet
- SchizophreniaDocument2 pagesSchizophreniaHannah Grace Protasio LumongsodNo ratings yet
- Laboratory Study: Determinants Actual Values Normal Values Interpretation Clinical Significance Nursing ResponsibilitiesDocument1 pageLaboratory Study: Determinants Actual Values Normal Values Interpretation Clinical Significance Nursing ResponsibilitiesHannah Grace Protasio LumongsodNo ratings yet
- NCM 207 Midterm No.2Document4 pagesNCM 207 Midterm No.2Hannah Grace Protasio LumongsodNo ratings yet
- Hydrocephalus FinalDocument10 pagesHydrocephalus FinalHannah Grace Protasio LumongsodNo ratings yet
- Clinical Chemistry: Determinants Actual Values Normal Values Interpretation Clinical Significance Nursing ResponsibilityDocument2 pagesClinical Chemistry: Determinants Actual Values Normal Values Interpretation Clinical Significance Nursing ResponsibilityHannah Grace Protasio LumongsodNo ratings yet
- NCM 207aDocument16 pagesNCM 207aHannah Grace Protasio LumongsodNo ratings yet
- Smoking CessationDocument10 pagesSmoking CessationLakshmipriya NagarajanNo ratings yet
- Incomplete AbortionDocument193 pagesIncomplete AbortionHannah Grace Protasio Lumongsod100% (1)
- Stop Smoking Start Living - BookletDocument22 pagesStop Smoking Start Living - BookletHannah Grace Protasio LumongsodNo ratings yet
- Cognitive DisordersDocument9 pagesCognitive DisordersHannah Grace Protasio LumongsodNo ratings yet
- RRL1Document11 pagesRRL1Hannah Grace Protasio LumongsodNo ratings yet
- Cognitive DisordersDocument9 pagesCognitive DisordersHannah Grace Protasio LumongsodNo ratings yet
- Age PeriodsDocument1 pageAge PeriodsHannah Grace Protasio LumongsodNo ratings yet
- Moving From Campus To CorporateDocument27 pagesMoving From Campus To CorporatepriyannthuNo ratings yet
- Pom - Evolution of MGMT ThoughtDocument27 pagesPom - Evolution of MGMT ThoughtMuhammadFaheemNo ratings yet
- Eng 22 Lesson 2Document48 pagesEng 22 Lesson 2Sopphia CalopeNo ratings yet
- Cultural Genogram Hardy Laszloffy 1995 PDFDocument11 pagesCultural Genogram Hardy Laszloffy 1995 PDFSasha GiseleNo ratings yet
- Communication Skills of Practicing Pharmacists and Pharmacy StudentsDocument6 pagesCommunication Skills of Practicing Pharmacists and Pharmacy StudentsAshraf KhanNo ratings yet
- 2 Field Study Activities 1Document6 pages2 Field Study Activities 1jacky matoreNo ratings yet
- EAPP Midterm ExamDocument5 pagesEAPP Midterm ExamDA FT100% (2)
- Employee Performance Management Group Project (Finalized)Document50 pagesEmployee Performance Management Group Project (Finalized)Kauthamen AppuNo ratings yet
- Writing The College Essay: Undergraduate Admissions OfficerDocument12 pagesWriting The College Essay: Undergraduate Admissions OfficermortensenkNo ratings yet
- Dealing With Interpersonal Crisis: 1. in A Crisis Situation, It's Crucial To Do Something!Document3 pagesDealing With Interpersonal Crisis: 1. in A Crisis Situation, It's Crucial To Do Something!Swagat PradhanNo ratings yet
- Classroom Supervisory Practices and Teacher Effectiveness Fil AuthorDocument13 pagesClassroom Supervisory Practices and Teacher Effectiveness Fil AuthorLAGUIO ELEMENTARY SCHOOLNo ratings yet
- CONTOH RPH Bahasa Inggeris Tahun 1Document2 pagesCONTOH RPH Bahasa Inggeris Tahun 1Mohana SanthNo ratings yet
- Mus 177 SyllabusDocument6 pagesMus 177 Syllabusapi-260184492No ratings yet
- Personality and Individual Differences: Tara C. Marshall, Katharina Lefringhausen, Nelli FerencziDocument6 pagesPersonality and Individual Differences: Tara C. Marshall, Katharina Lefringhausen, Nelli FerencziAdamNo ratings yet
- Letter of Rec - Olivia Churchwell 2021Document2 pagesLetter of Rec - Olivia Churchwell 2021api-605017862No ratings yet
- Taking Your Leadership - Tom AlafatDocument29 pagesTaking Your Leadership - Tom AlafatFredSmith777No ratings yet
- Overrating or Dismissing The Value of Evidence-Based Practice+++Document7 pagesOverrating or Dismissing The Value of Evidence-Based Practice+++pig5evans30No ratings yet
- Nursing Science and Profession: As An ArtDocument45 pagesNursing Science and Profession: As An ArtHans TrishaNo ratings yet
- Anabolic Optimism PDFDocument42 pagesAnabolic Optimism PDFcomtrol100% (1)
- Submitted by Name-Muskan Singh Enrollment Number - A1506918455 Section - 3FDocument8 pagesSubmitted by Name-Muskan Singh Enrollment Number - A1506918455 Section - 3FMuskan SinghNo ratings yet
- Rationale All About MeDocument50 pagesRationale All About Meapi-224425581100% (2)
- Un Chien AndalouDocument3 pagesUn Chien AndalouBurcu Erdoğan100% (1)
- Single Subject Credential Program EDSC Lesson Plan Template: Precious Daileg, Estefani Bautista, Brit Brown BiologyDocument7 pagesSingle Subject Credential Program EDSC Lesson Plan Template: Precious Daileg, Estefani Bautista, Brit Brown Biologyapi-257666656No ratings yet
- How To Communicate Globally and EffectivelyDocument11 pagesHow To Communicate Globally and EffectivelyconniephuongNo ratings yet
- The Four Questions Great Leaders AskDocument3 pagesThe Four Questions Great Leaders AskajaynerkarNo ratings yet
- Developmental Characteristics of AdolescenceDocument1 pageDevelopmental Characteristics of Adolescenceapi-644447279No ratings yet
- Strategy - Repeated Writing StrategyDocument2 pagesStrategy - Repeated Writing Strategyapi-299634543100% (1)
- Soft Skills For EngineersDocument50 pagesSoft Skills For EngineersJorge Isaac OrtizNo ratings yet
- Dasari Sravani: Career ObjectiveDocument3 pagesDasari Sravani: Career ObjectiveSuriya GNo ratings yet
- BOOK - WEEK 6 - Chapter 10&11 - Seating & Grouping Ss - Techno 4 LearningDocument31 pagesBOOK - WEEK 6 - Chapter 10&11 - Seating & Grouping Ss - Techno 4 LearningPhương UyênNo ratings yet