Professional Documents
Culture Documents
Cardiovascular Disorders Notes
Uploaded by
Perrilyn PereyOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular Disorders Notes
Uploaded by
Perrilyn PereyCopyright:
Available Formats
Aug 13, 2012
Cardiovascular Disorders
Anatomy and Physiology - HEART Center of the thorax 300 g in weight; cone shaped and tilted forward and to the left o Size and weight are influenced by Age Gender Body weight Physical condition Heart condition (disease) Pumps blood to the tissues and supplies them with oxygen and other nutrients Size of a fist Location: mediastinum o In a rotated position o Right ventricle > lies anteriorly, beneath the sternum o Left ventricle > situated posteriorly o Close proximity to chest wall > pulsation created by the normal ventricular contraction is easily detected = Apical Pulse / Point of Maximum Impulse (PMI) Layers: o Pericardium Thin, fibrous sac which encases the heart Layers: Visceral o Adheres to the epicardium Parietal o Envelops the visceral pericardium o Tough fibrous tissue that attaches to the great vessels, diaphragm, sternum and vertebral column o Supports the heart in the mediastinum The space between visceral and parietal is called pericardial space o Filled with about 20 ml of fluid o Lubricates the surface of the heart o Reduces friction during systole Pericardial space (between; consist the fluid) o Epicardium Exterior layer o Myocardium Heart muscle Responsible for the contractility (pumping action) and function of the heart Made up of muscle fibers Composed of specialized cells called Myocytes > which form an interconnected network of muscle fibers Fibers encircle the heart in a figure-of-eaight pattern, forming a spiral from the base (top_ of the heart to the apex (bottom) during contraction facilitates a twisting and compressive movement of the heart that begins in the atria and moves to the ventricles Sequential and rhythmic pattern of contraction + muscle fibers relaxation =maximizes the volume of blood ejected with each contraction. Controlled by the conduction system o Endocardium Innermost layer Consist of endothelial tissue and lines the inside of the heart and valves Pumping action > accomplished by the rhythmic relaxation and contraction of the four chambers muscular walls o Diastole Relaxation phase All four chambers relax simultaneously Allows the ventricles to fill in preparation for contraction. Period of Ventricular Filling o Systole Refers to the events in the heart during contraction of the two top chambers (atria systole) o Occurs first, just at the end of diastole Two bottom chambers (ventricular systole)
o Follows the atria systole o The process allows the ventricles to completely fill prior to ejection of blood from the chambers Heart Chambers o Right Side Right Atrium and Right Ventricle Distributes venous blood (deoxygenated blood) to the lungs via the pulmonary artery (pulmonary circulation) for oxygenation. Right Atrium Receives blood returning from the o Inferior vena cava o Superior vena cava o Coronary sinus cardiac vein Right ventricle o Contracts against a low pressure system within the pulmonary arteries and capillaries o Left Side Left atrium and left ventricle Distributes oxygenated blood to the remainder of the body via the aorta Left Atrium Receives oxygenated blood from the pulmonary circulation via four pulmonary veins. Left ventricle 2 times more muscular than the right ventricle To overcome the high aortic and arterial pressure o Valves Four valves Permit blood to flow in only one direction Composed of thin leaflets of fibrous tissue Open and close in response to the movement of blood and pressure changes within the chambers Types: Atrioventricular Valves o Separate the atria from the ventricles o Tricuspid Valve Composed of 3 cusps or leaflets Separate the right atrium from the right ventricle o Mitral / Bicuspid Valve Composed of 2 cusps Lies between the left atrium and the left ventricle o During diastole Tricuspid + Mitral = open >allowing blood in the atria to flow freely into the relaxed ventricles. o Ventricular systole starts Ventricles contract Blood flows upward into the cusps or the tricuspid and mitral valves > T + M = closes T and M pressure increase = the papillary muscles and the chordae tendineae maintain valve closure. Papillary muscles o located on the sides of the ventricular walls o Connected to the valve leaflets buy thin fibrous bands called Chordae Tendineae Contraction of papillary muscles Causes the chorea tendineae to become taut, keeping the valve leaflets approximated and closed. Prevents backflow of blood into the artia (regurgitation) as blood is ejected out into the pulmonary artery and aorta
Semilunar Valves o Composed of three leaflets which are shaped like half-moons. o Pulmonic Valve Valve between right ventricle and pulmonary artery o Aortic Valve Valve between the left ventricle and aorta o Closed during diastole Pressure in the pulmonary artery and orta decreases
o o
Causing blood to flow back toward the semilunar valves o Fills the cusps with blood and closes the valves Forced open during ventricular systole as blood is ejected from the R and L ventricles into the pulmonary artery and aorta.
Coronary Arteries L and R arteries and the branches > supply arterial blood to the heart Arteries > originate from the aorta just above he aortic valve leaflets Heart > high metabolic requirements, extracting approximately 70% to 80% of the Oxygen delivered Are perfused during diastole Heart rate increases = diastole time is shortened > may not allow adequate time for myocardial perfusion. Result > patient at risk for myocardial ischemia (HR>100), esp. patient with CAD L Coronary Artery Has three branches o Left main coronary artery Artery from the point of origin to the first major branch Two branches arises Left anterior descending artery o Courses down the anterior wall of the heart Circumflex artery o Circles around to the lateral left wall of the heart Three Vessels involved in ASHD CAD 3: 1. R Coronary Artery 2. Left Anterior Descending Artery 3. Left Circumflex Right Coronary Artery Leads to the inferior wall of the heart Posterior wall > receives blood supply by an additional branch from the R coronary artery call posterior descending artery Coronary Veins Superficial to the coronary arteries Venous blood returns to the heart primarily through the coronary sinus (located posteriorly in R atrium)
Coronary Circulation Needs a constant supply of O2 and nutrients to contract efficiently and conduct impulses Major blood vessels Blood flow through myocardium is greatest during relaxation (diastole) and reduced during contraction (systole) Rapid/prolonged contractions interfere with blood supply to the heart Anastomoses (connections) btw RCA and LCA Potential to open up and provide collateral circulation Collateral circulation alternative source of blood When obstruction develops gradually, other capillaries tend to enlarge to meet metabolic needs RCA supplies R side of heart and inferior part of LV SV node, AV node anterior descending anterior wall of ventricles, anterior septum, bundle branches L Circumflex L atrium, lateral and posterior walls of LV Implications o RCA blockage -> conduction disturbances of AV node (arrhythmias) o LCA - > Impair pumping ability of LV (CHF ) Cardiac Cycle Refers to the alternating sequence of diastole (relaxation) and systole (contraction) coordinated by the conduction system Cycle o 2 atria relaxed and filing with blood o AV valves open because of pressure and ventricles are relaxed o Blood flows into ventricles almost emptying atria o Conductions system stimulates atrial muscle to contract forcing any blood into the ventricles o Atria relax o 2 ventricles contract and pressure increases in V o AV valves closed o (Brief moment) all valves closed, ventricular myocardium continues to contract building up pressure (isovulmetric phase) o Increasing pressure opens up the semilunar valves(blood forced into pulmonary and aorta)
o o o Pulse -
Contraction needs to be strong to overcome opposing pressure in the artery Atria fills again, ventricles relax Start the cycle again
The pulse indicated the heart rate During ventricular systole, it expands the arteries Weakness or irregularity is in a peripheral pulse (radial) indicates a problem Apical pulse rate measures at the heart itself Pulse deficit difference between apical and radial Common causes: coartation of aorta / stenosis
Cardiac Output Blood ejected from L ventricle / minutes Ave: 5.6 L / min CO = stroke vol x HR o Stroke volume: blood ejected / heartbeat o Increased amt of blood returns to the heart (SNS stimulation), heart stretched more and force of contraction increases proportionately o Preload: venous return o Afterload: resistance to L Ventricular ejections (peripheral resistance) Vascular System Arteries Arterioles (smallest) Capillaries (site of diffusion, O/CO2 exchange, supply of nutrients) Venules Veins Valves Lymphatics drains the lymph fluids Arteries and Veins 3 Layers o Tunica Intima Endothelial cells secretes substances that can adjust the dilatation and constriction of blood vessels o Tunica Media Smooth muscle that controls the diameter and lumen size of the blood vessels o Tunica Adventitia Outermost Autoregulation Localized vasodilation and vasoconstriction regulated by reflex and adjustment Decrease in pH and O and increased CO2 and release of chemical mediators > vasodilation Norepinephrine / Epinephrine, angiotensin > systemic vasoconstriction (Alpha 1 receptions) Blood Pressure Pressure of blood against systemic arterial walls Systolic pressure pressure exerted by the blood when ejected by the LV Diastolic pressure pressure that occurs when the ventricles are relaxed BP = CO x PR Peripheral resistance: o Decrease lumen o Vasoconstriction o Obstruction of blood vessels Blood Pressure Controls o Baroreceptors (Pressoreceptors) aortic arch and carotid sinus o Stretch Receptors vena cava and right atrium o Anti-diuretic hormone o Aldosterone: primary fx: Na Reabsorption with Water o Renin-Angiotensin System Properties of Cardiac Muscle Automaticity Excitability Conductivity Contractility Cardiac Conduction System Conduction system
Atrial contraction depolarization in the P wave Ventricular contraction depolarization in the ventricles (QRS) T-Wave ventricular repolarization
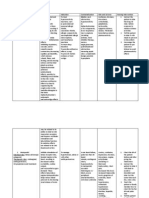
ECG Control of Heart Heart rate and force of contraction controlled cardiac control center (medulla) Baroreceptor (aorta and carotid) changes in BP > cardiac center > SNS/PNS SNS increase heart rate and contractility and vasoconstrictions PNS vagus nerve stimulation slows heart rate Beta receptors in the heart Nursing History Non modifiable o Age o Gender o Race o Heredity Modifiable o Stress o Diet o Exercise o Cigarette o Alcohol o HPN o Hyperlipidaemia o DM o Obesity o Contraceptive pill o Personality type Physical Examination Inspection o Skin color o JV distention o Respiration o PMI o Edema Palpate o Peripheral pulses o Apical pulse Auscultate o Heart sounds (s1-apex, AV closure, s2-base, semilunar valve closure, s3, s4) o Murmurs o Pericardial friction rub Percussion o Note: dullness (heart is a solid organ) Common clinical manifestation o Dyspnea Dyspnea on exertion Orthopnea Paroxysmal dyspnea o Chest pain o Edema o Syncope caused by narrowing of blood vessels; common carotids supply the brain (anterior part of the brain) o Palpitation because of the abnormality of the conduction and contractility of the heart o Fatigue - related to Oxygen hypoxemia Diagnostic Tests Cardiac Enzymes Enzyme CPK MB LDH Troponin Myoglobin
Onset 4-5 hours Within 24 hours Within 3 hours 1 hour
Peek 18-24 hours 48-72 hours Up to 7 days 4-6 hours
Normal Values 0 4.7 ng/ml 70-200 IU / L Less than 0.6 ng/ml 0-85 g / ml
Complete Blood Count Serum Lipids
o Cholesterol o Triglycerides o HDL/LDL Electrolytes o Any imbalance can result to arrhythmias and dysrhythmias Increase Decrease Potassium Vent dysrhythmia Vent dysrhythmia assystole Sodium Calcium H20 Toxicity AV block/Tachycardia Shortened at interval Muscle weakness Hypotension Prolonged PR interval Wide QRS complex BUN o Diuretics use / HF Prolonged of interval vent tachycardia
MG
Fibrillation
Renal fx Creatinine Chest X-Ray o Silhouette of the heart o Left ventricular hypertrophy image retrosternal fullness o Right ventricular hypertrophy image retrocardia fullness ECG o 0.04 sec and 0.1 millivolt 1 box o 6 chest leads V1-V6 V1-V3 Septal defect Septal Wall (Atrium or Ventricular = multiple vessels) V1-v4 Anterior Defects V5-V6 Lateral Wall Defects 2-3 ABF Inferior wall ischemia/infarction Right coronary Artery 1 ABL High lateral wall infarction Left Coronary Artery o Initial dx and monitoring of arrhythmias o Non invasive o Holter-monitor worn to record ECG changes while pursuing daily activities; what activities of the px can induce arrhythmia o Echocardiagraphy reflected sound waves records the image of the heart and valve movements; Heart structure and valve movement Invasive Hemodynamic Monitoring o Central Venous Pressure Monitors right side of the heart The tip of the catheter is inside the Right atrium Common with px with hypervolemia Nursing responsibility Consent Explain the procedure Patient must be relaxed o The reading will be altered if patient is tachypnic or brachydic 0 point of manometer at level of R atrium Record initial reading must be done in the same position Concurrent reading must be done in the same position Change dressing, IV fluid bag, manometer and tubing every 24 hours Hold breath when cath is changed Check daily for infection o Pulmonary Artery Pressure (PAP) / Pulmonary Capillary Wedge Pressure (PCWP) For patients with Cor Pulmonale Nursing responsibility Consent Explain procedure Check baseline VS or attach to ECG monitor Position: Supine Adjust transducer at phlebostatic axis or sternal notch Observe insertion site for information, swelling and bleeding Deflate balloon after reading o If a balloon is left inflated, no blood will enter from the R ventricle to enter the pulmonary circulation o Cardiac Catheterization Passing a catherter to the blood vessel to:
o o
Visualize the inside of the heart Measure pressures Asses valve and heart function Right Sided Catheterization Antecubital or femoral vein Measures R atria and ventricle pressure Left Sided Catheterization Retrograde catheterization Transseptal Catheterization Nursing Responsibilities Pre procedure: o Consent o Explain procedure o Asses allergies to seafoods and iodine o Document wt and ht o Baseline VS o Inform of fluttery feeling / warm, flushed feeling and desire to cough Post procedure o VS q 30 mins for 2 hours o Asses for chest pain or dysrhythmias o Monitor for bleeding and hematoma o Keep extremely extended for 4-6 hours o CBR for 6-12 hours o Increase fluid intake Cardiac angiography Contrast dye injection to visualize blood flow and any obstructions Blood flow in peripheral vessels can be assessed with Doppler studies (microphone that records the sound of blood flow)
HEART DISEASES Coronary Artery Disease (CAD) o Narrowing or obstruction of one or more coronary arteries as result of Atherosclerosis Dyslepedemia Arteriorsclerosis immune defects o Common with narrowing of arteriosclerosis Signs and symptoms Chest pain Palpitation Difficulty in breathing / dyspnea Syncope / loss of consciousness Cough or hemoptysis Excessive fatigue o Management Nitrates Antiplatelets Antilipemics Beta adrenergic blockers Calcium Channel Blockers Surgery PTCA Atherectomy CABG o Nursing Management Encourage to reduce the risk by modifying lisfestyle Admin prescribed meds Diet: low fat, low cholesterol, low Na Angina Pectoris o Types: Stable Unstable Prinzmetal exposure to cold weather Intractable unrelieved by any type of meds; very suggestive of MI o Causes: Exertion Emotion Exposure to cold Excessive smoking Excessive eating o Assessment: Pain patterns
Mild to moderate Retrosternal choking, heartburn, pressing, bursing squeezing Radiating to neck, jaw, shoulder, arms L 3-5 minutes Relieved by rest and nitroglyceride Pallor, diaphoresis, dizziness, palpitation ECG change ST depression, T wave inversion o Medications Vasodilators Nitroglycerine, amyl nitrate, isosorbide B-Adrenergic Propranolol, metoprolol Ca channel blocker Verapamil, nifedipine, diltiazem Pit aggregating inhibitors ASA, dypiridamole, ticlopidine Anticoagulants Heparin Na, Warfarin NA (Coumadin), dicumarol Thrombus thrombolytics o Nursing Responsibilities Anticipate postural hypotension Take max of 3 doses at 5 min interval SL prep has nursing or stinging sensation Avoid OH - tachycardia Advise client to carry 3 tabs in his pocket; store nitroglycerine in a cool, dry, dark placel replace stock every 3-6 months Nitropatch applied OD in AM, rotating sites Do not give NTG if px took Viagra or any drug for erectile dysfunction Evaluate effectiveness (if not MI) o Interventions Beta blockers, calcium channel blockers Myocardial Infarction o Sudden dec of oxygenation due to absence of coronary blood flow that results to destruction of myocardial tissue in regions of the heart o Right coronary -> arrhythmia o Left Coronary -> DEAD; comprises the cardiac output immediately o Causes: Thrombus Emboli Atherosclerosis o Location L anterior descending artery anterior or septal wall MI or both Circumflex artery - posterior wall MI or lateral wall MI Right coronary artery inferior wall MI o Diagnostic Studies Total CK levels Cardiac enzymes AST ECG T wave inversion zone of hypoxia ST elevation zone of injury Pathologic Q wave zone of infarction o Assessment Pain pattern: sever crushing substernal pain; knife like, viselike May radiate to jaw, back and left arm Fever N/V Anxiety Crushing chest pain Dyspnea Pallor o Nursing responsibilities Admin prescribed meds Morphine, Nitrogen, Oxygen, Aspirates Lidocaine Xylocaine Beta blockers propranolol, timolol Thrombolytics risk for bleeding; streptokinase and uroinase Anticoagulants heparin, warfarin/Coumadin Oxygen at 2-4 L/min Stool softeners and soft diet to avoid valsalva
Diet: liquid / small frequent meals; low fat, cholesterol and Na Pos: semi fowlers to promote lung expansion Emotional rxns: anxiety, denial, depression Monitor thrombolytic therapy Check for signs of bleeding Used within 3-4 hours after onset of Sxs 6 hours golden period Following acute episode: Maintain CPR Provide ROM o Progressive Cardiac rehab Progress to ambulation Rehabilitation: Early activity o 1-2 metabolic act on tas (MET) th o Hospitals discharge: 14 day o ADLs: 6 weeks after o Sex: 4-8 weeks after Guidelines Resume if bale to climb 2 flights of stairs Before: rest is impt / avoid large meals/ wear loose fitting clothes/ nitro before sex / usual envi / sex at rm temp/ foreplay During: comfortable position Female position: side lying Male position: sitting position o Usual complications Cardiogenic shock pumping ability of the LV severely impaired Cardiac Arrhythmias lack of O causes conduction problems CHF Cardiac Dysrhythmias o Abnormal cardiac rhythms that can be due to abnormal automaticity of conduction or both o Most common complications and major cause of MI o Most common dysrhythmia in MI is PVCs o PVC of >6/min is life threatening o Predisposing factors are Tissue ischemia Hypoxemia CNS and PNS influences Lactic acidosis Hemodynamic abnormalities Drug toxicities Electrolyte imbalance o Types Sinus Atrial Ventricular Conduction o Bradycardia regular, slower rate <60 o Tachycardia regular, faster rate >100 o Atrial flutter 160-350 / min, less filling time o Atrial fibrillation rate >300, uncoordinated, muscle contractions, no output carding standstill, no filling o PVCs may induce fibrillation o Bundle branch block delayed conduction to BB st o 1 degree Heart Block delayed conduction AC node nd o 2 degree HB some beats go to AV, some dont rd o 3 degree HB no conduction to AV node, ventricles slowly contract, some independent atrial contractions Sinus Dysrhythmias o Types Sinus Tachycardia Digitalis Sinus Bradycardia Atropine Atrial Dysrhythmias o Premature Atrial Contaction (PAC) o Paroxysmal Atrial Tachycardia o Atrial Flutter o Atrial Fibrilation o Meds
Quinidine Ca Channel Blockers Cardioversion The electrical impulse waits for the R wave at the peak of the QRS complex Pacemaker Long term management Ventricular Dysrhythmia o Premature Ventricular Contraction o Vantricular Tachycardia Widen QRS Rapid firing o Ventricular Fibrillation Chaotic discharge rate >300 May result to clinical death Tx: immediate defibrillation then CPR Epinephrine o Pacemakers Electronic device that causes cellular depolarization and cardiac contraction It initiates and maintains HR Pacing modes Demand Fixed Rate Precautions DO NOT MRI Nursing interventions Monitor ECG ff implantation, include VS Make sure all the equipment in the clients unit is grounded Observe for signs of pacemaker failure o Cardioversion / Defibrillation Cardioversion Synchronous application of shock during R wave Defib Asynchronized electric shock to terminate VF or V tachycardia without pulse Nursing intervention Client in firm, flat surface Apply interface materials to the paddle Grasp paddle only by insulated handles Give command to STAND clear rd Apply one of the paddles at precordium, other R parasternal area 3 ICS For defibrillation, release 200-360 joule; for cardioversion, lower energy is required Defibrillation is done prior to CPR Diazepam sedative CPR Indications o CP Arrest / clinical death (breathlessness / pulselessness) o CPR should be started < 5 mins after arrest Types o Basic Life Support use of mouth, hands o Advance Cardiac Support BLS and equipment When to stop? o When the client is revived o When EMS has been activated o When the rescuer is exhausted o When client is dead CHF o Causes Hypervolemia Arteriosclerosis MI Valvular problems o Types Right sided CHF (Systemic Sx) Fatigue o Distended jugular veins Ascites Left side heart failure (Pulmonary Sx) Cardiomegaly o Blood tinged sputum Chronic cough
o Acute pulmo edema Exertional dyspnea o Cyanosis Orthopnea o Weight loss
Managements Rest minimize O2 consumption High fowlers or sitting Decrease fluids and Na Medications Cardiac glycosides (+) inotropy / (-) chronotropy Digitalis / digozin (Lanoxin) / digitoxin (Crystodigin)/ Lanatoside o Guidelines Check HR ^ K intake Normal level: 0.5-2 ng/ml Toxicity o Antidote Digoxin Immune Fab (Digibind) = Antibodies that bind to digoxin Diuretics = H2O and Na + excretion Loop Diuretics Furosemide (Lasix) Potassium sparing spironolactone (Aldactone) Guidelines: Give in the AM Monitor IO S/E: Hypoalemia / hyponatremia/ dehydration/hypotension o Rotating Tourniquet Principles: Apply 3 tourniquet Inflate cuff 10 mm above diastolic pressure Rotate q 15 Check distal pulses Remove 1 at a time q 15 mins interval Inflammatory Disease of the Heart o Pericarditis Acute or chronic inflammation of the pericardium Assessments Precordial pain Pain (inspiration, coughing, and swallowing) Pain worse when supine Pericardial friction rub Fever and chills Management Pos: side liying, high fowlers, upright or leaning forward Admin: analgesic, corticosteroids, NSAIDs Avoid aspirin and anticoagulants Antibiotics Diuretics and digoxin Monitor for complications: cardiac tamponade o Over accumulation of pericardial fluid o Pericardial effusion occurs when the space bet. The parietal and visceral layers of the pericardium fill with fluid o Etiology Stab wound Effusion Heart surgery o Assessment Becks triad: Distended neck veins o Compressed heart due to the cardiac tamponade, no space to accommodate the blood coming from the venous system, cannot enter the R atrium Muffled heart sounds o Interface of the fluid not good conductor of sound Hypotension o Inability of the heart to contract Paradoxical Pulse More than 10 mm
Chest pain Cardiogenic shock Increased CVP
Management CC for hemodynamic monitoring PERICARDIOCENTESIS o Spinal needle will enter the medistianum and aspirate the pericardial fluid Admin IV fluid as prescribed Myocarditis Acute/chronic inflammation of the myocardium Etiology: Bacterial o Staphylococcus /pneumococcal Viral o Mumps / influenza Parasitic: o Toxoplasmosis Radiation / Lead exposure Assessment Fever Pericardial friction rub Gallop rhythm Murmur o Infective endocarditis S/S of HF Chest pain Management Pos: bed rest/ sitting up or leaning forward Monitor the pulse rate and rhythm o Can result to arrhythmia Admin of NSAID / analgesics / salicylates for fever and pain Limit activities o Prevent fatigue Admin digoxin / antidysrhythmic / antibiotics as prescribed Endocarditis Inflammation of the inner lining of the heart Expect valvular problem Assessment Fever Anorexia Wt loss Fatigue Cardiac murmur Janeways lesions Osslers Nodes Petechiae Splinter haemorrhages in nail beds Splenomegaly Rheumatic heart fever (valve) Management Balance activity with intermitted rest Antiembolic stockings Monitor emboli o Splenic sudden abd pain radiating to L shoulder / rebound tenderness on palpitation o Renal flank pain radiating to the groin, hematuria and pyuria Cardiomyopathy Myocardium around left ventricle becomes flabby, altering cardiac function > decreased CO2 Inc HR and inc muscle mass compensate in early but later stage > HF Types Dilated (congestive) o Dilated chambers contract poorly causing blood to pool and reducing CO Hypertrophic (Obstructive) o Hypertrophied LV cant relax and fill properly Assessment Chest pain Dyspnea
Enlarged heart Crackles Dependent putting edema Enlarge liver Jugular vein distension Murmur Gallops Syncope Management Low Na diet Dual chamber pacing Surgery Heart transplant Cardiomyoplasty o Valvular Heart disease 3 types of mechanical disruption from VHD Stenosis or narrowing o Doesnt open the valve Insufficiency o Incomplete Mitral insufficiency o Same + peripheral edema Tricuspid insufficiency o R sided HF Treatment Na restrictions Open heart surgery using CP bypass for valve replacement Medications Anticoagulants Nursing management Monitor for sign of HF or pulmo edema and monitor for adverse rxns from drug therapy Place in upright position to relieve dyspnea Maintain bed rest If patient undergoes surgery, watch for hypotension Peripheral Arterial and Venous Disease o Arterial Disease Buergers Disease o Occlusive disease of the median and small arteries and veins accompanied by clot formation Etiology Unknown Smoking Males Assessment Intermittent claudication Ischemic pain occurring in the digits while at rest Cool number tingling sensation Diminished pulse at distal extremitiy Ulceration o Lower extremity Management Amputation Removal of the thrombus / clot supplying the area Instruct to stop smoking Monitor pulses Avoid injury to extremities Admin vasodilators ad prescribed o Reynauds Disease Vasospasm of the arterioles and arteries of extremities Etiology: Cold Stress Smoking Management Stop smoking Vasodilators Avoid precipitating factors Warm clothing Avoid injuries to hands and fingers
Venous Diseases Thrombophlebitis Clots lead to vein inflammation Phlebothrombus A thrombus w/o inflammation Common in the antecubital area Phlebitis Vein inflammation usually assoc. with invasive procedures Deep Vein Thrombosis Pain (calf or groin tenderness) Positive Homans sign Warm skin and tender to touch Varicose Veins Distended protruding veins that appear darkened and tortuous; vein wall weaken and dilate, the valves become incompetent Etiology o Prolonged standing o Pregnancy o Obesity o Congenital Incidence o female o 35-40 y/o
Assessment (in comparison with arterial diseases) Arterial Intermittent claudication Cyanosis Coldness Absent pulse Loss of sensation Gangrene ulcers Decreased capillary refill
Venous Heaviness and leg cramps Redness Warmth Unpalpable pulse due to edema No loss of sensation Venous stasis ulcers (+) Trendelenburg test
Intervention (Peripheral) o Lower down legs o Wear warm socks o Beurger Allens Exercise o Avoid tight clothing o Avoid obesity o Avoid crossing legs o Avoid smoking and cold weather o Femoral artery bypass o Angioplasty o Amputation Intervention (Venous) o Elevate legs o Wear elastic stockings o Ankle push up o Avoid obesity o Avoid crossing legs o Avoid tight clothing o Avoid smoking and prolong standing o Vein striping and ligation o Post op care Elevate legs CBR for 24 hrs Elastic compression Check for haemorrhage Prevent thrombophlebitis
Aortic Aneurism Abnormal dilation of the arterial wall caused by localized weakness and stretching in the medial layer or wall of the artery Types According to morphology or form o Fusiform o Saccular o Dissecting o False (Pseudoanuerysm) According to location
Thoracic aortic aneurysm S/s Pain Syncope Dyspnea Inc pulse o Abdominal aortic aneurysm S/s Pulsating mass in the abd Systolic bruit over the aorta Tenderness on deep palpation Abdominal or lower back pain o Cerebral aneurysm s/s headache vomiting ^ICP Intervention o Prevent rupture Antihypertensive medications Modify risk factors o Surgery Resection of aneurysm with Teflon/Dacron Graft o Post Op Monitor for haemorrhage Flat pos / avoid SF pos O2 as ordered Coughing / breathing exercise Check distal pulses Avoid hip-knee flexion HYPERTENSION Abnormal elevation of BP above 140/90 mmHg based on at least 2 readings on same condition Brain o Cerebrovascular accidents Eyes o Hypertensive retinopathy Heart o L ventricular Hypertrophy resulting to HF or Cardiomyopathy (Hypertophic) Kidneys o Hypertensive Nephrosclerosis Types Primary / Essential / Idiopathic o Most common o 90-95 percent of cases o Unknown cause Secondary o With known cause o Endocrine Neochromocytoma Hyperthyroidism o Cardiovascular Artherosclerosis o Renal Secondary to activation of renin angiotensin system Renal artery stenosis o Pregnancy Increase in blood volume Vasospasm Preeclampsia Labile o Intermittenly elevated BO Malignant o Sever, rapidly progressing and sustained > leads to rapid end organ complication White coat o Elevation of BP only during clinical visits Assessments Signs and symptoms
o Headach o Depression o Dizziness o Nocturia o Unsteadiness o Tinnitus o Blurred vision o Memory loss Asymptomatic, L ventricular hypertrophy, cerebral ischemia, renal failure, visual disturbances including blindness, epistaxis Management Step care approach o Joint Committee on Detection, Evaluation and Treatment of High blood Pressure pp 898 Lifestyle modification Single Drug Therapy Mild hypertension diuretics (thiazide) beta blockers Multi Drug Therapy Add: ACE Inhibitors Inc Dosage of Beta Blockers Add beta blocker to diuretics (Thiazides) Substitute vasodilators All receptor blockers (sartans) Anti-lipemics (statins) Add: vasodilator or slow calcium channel blocker to current regimen Add: sympatholytic / Antiadrenergics central acting Major side effects Orthostatic hypertension Dizziness Cardiac rate alteration Sexual disturbance Drowsiness Health teachings Emphasize compliance Therapy is usually for life Monitor BP Do not increase of decrease dose without doctors order Do not abruptly discontinue meds
You might also like
- Open Chole and AdrenDocument8 pagesOpen Chole and AdrenPerrilyn PereyNo ratings yet
- Bubbles HeDocument39 pagesBubbles HePerrilyn PereyNo ratings yet
- Excess Fluid Volume PPT (Case Press)Document10 pagesExcess Fluid Volume PPT (Case Press)Perrilyn PereyNo ratings yet
- Calcium CarbonateDocument22 pagesCalcium CarbonatePerrilyn PereyNo ratings yet
- LaminectomyDocument6 pagesLaminectomyPerrilyn Perey100% (1)
- Lap Adrenalectomy NcaDocument9 pagesLap Adrenalectomy NcaPerrilyn PereyNo ratings yet
- Drug AnalysisDocument3 pagesDrug AnalysisPerrilyn PereyNo ratings yet
- Hematologic DiseasesDocument11 pagesHematologic DiseasesPerrilyn Perey100% (2)
- Acute Renal FailureDocument4 pagesAcute Renal FailurePerrilyn PereyNo ratings yet
- Arrest of DescentDocument5 pagesArrest of DescentPerrilyn PereyNo ratings yet
- Critcare PDFDocument20 pagesCritcare PDFPerrilyn PereyNo ratings yet
- Stages of LaborDocument30 pagesStages of LaborPerrilyn Perey100% (1)
- Pneumonia BIBLIODocument8 pagesPneumonia BIBLIOPerrilyn PereyNo ratings yet
- Nihms220210.pdf BibliographyDocument17 pagesNihms220210.pdf BibliographyPerrilyn PereyNo ratings yet
- Drug AnalysisDocument3 pagesDrug AnalysisPerrilyn PereyNo ratings yet
- 5 P - S of LaborDocument19 pages5 P - S of LaborPerrilyn PereyNo ratings yet
- Nihms220210.pdf BibliographyDocument17 pagesNihms220210.pdf BibliographyPerrilyn PereyNo ratings yet
- Critcare PDFDocument20 pagesCritcare PDFPerrilyn PereyNo ratings yet
- Pathophysio For Late Onset SepsisDocument1 pagePathophysio For Late Onset SepsisPerrilyn PereyNo ratings yet
- Nihms281140.pdf BibliographyDocument13 pagesNihms281140.pdf BibliographyPerrilyn PereyNo ratings yet
- Leg or Foot Amputation Pref CardDocument2 pagesLeg or Foot Amputation Pref CardPerrilyn PereyNo ratings yet
- Anxiety Related 2010Document17 pagesAnxiety Related 2010Perrilyn PereyNo ratings yet
- BioethicsDocument12 pagesBioethicsPerrilyn PereyNo ratings yet
- OR TermsDocument1 pageOR TermsPerrilyn PereyNo ratings yet
- BreastfeedingDocument3 pagesBreastfeedingPerrilyn PereyNo ratings yet
- HTTADocument2 pagesHTTAPerrilyn PereyNo ratings yet
- Drug NameDocument1 pageDrug NamePerrilyn PereyNo ratings yet
- Drug NameDocument1 pageDrug NamePerrilyn PereyNo ratings yet
- MenstruationDocument1 pageMenstruationPerrilyn PereyNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Cambridge Primary Science Teacher's Resource Book 6 With CD-ROM, Fiona Baxter and Liz Dilley, Cambridge University Press - PublicDocument38 pagesCambridge Primary Science Teacher's Resource Book 6 With CD-ROM, Fiona Baxter and Liz Dilley, Cambridge University Press - PublicSaleha Shoaib68% (22)
- Electrocardiogram: By: Keverne Jhay P. Colas, RN, MANDocument72 pagesElectrocardiogram: By: Keverne Jhay P. Colas, RN, MANGaras AnnaBerniceNo ratings yet
- Circulatory System Revision WorksheetDocument4 pagesCirculatory System Revision WorksheetPoulomi Sengupta100% (1)
- Grade 10 12 Biology Revision Notes Transport in Plants and AnimalsDocument33 pagesGrade 10 12 Biology Revision Notes Transport in Plants and AnimalsMapalo ChirwaNo ratings yet
- 2023 AL Subject ReportDocument269 pages2023 AL Subject ReportSand FossohNo ratings yet
- Hempel 2020 Sci30 Bio Video SheetsDocument11 pagesHempel 2020 Sci30 Bio Video SheetsticoninxNo ratings yet
- Cardiovascular System: Dulay, Arjay SDocument21 pagesCardiovascular System: Dulay, Arjay SarjayNo ratings yet
- The Human Circulatory System by TariqDocument84 pagesThe Human Circulatory System by TariqMuhammad Tariq KhanNo ratings yet
- The Heart: Guyton Unit III Ch9 Dr. Ebaa AlzayadnehDocument9 pagesThe Heart: Guyton Unit III Ch9 Dr. Ebaa AlzayadnehEbaa Moh'd ZayadnehNo ratings yet
- Cardiovascular Physical TherapyDocument206 pagesCardiovascular Physical TherapyJuanitoCabatañaLimIII100% (2)
- Electrocardiography II StudentDocument20 pagesElectrocardiography II StudentArmando Valdez ZamoranoNo ratings yet
- Anatomy & Physiology of The Cardiovascular SystemDocument3 pagesAnatomy & Physiology of The Cardiovascular SystemluaNo ratings yet
- PDF Class 11 Body Fluids Circulation BiologyDocument92 pagesPDF Class 11 Body Fluids Circulation BiologyNiharika SharmaNo ratings yet
- Omron M6Document26 pagesOmron M6paninaro2011No ratings yet
- Transportation in Animals and PlantsDocument12 pagesTransportation in Animals and PlantssuvashreeNo ratings yet
- Markscheme Unit1WBI01 June2018 IAL Edexcel BiologyDocument23 pagesMarkscheme Unit1WBI01 June2018 IAL Edexcel BiologyitgggreNo ratings yet
- Biology C - Lesson 1 - Circulatory SystemDocument46 pagesBiology C - Lesson 1 - Circulatory SystemMuhammad Azrie0% (1)
- Avant Review Lesson 1-8 ECG Rhythm Strip InterpretationDocument28 pagesAvant Review Lesson 1-8 ECG Rhythm Strip InterpretationphoebjaetanNo ratings yet
- How Animals Survive (Circulation and GasDocument24 pagesHow Animals Survive (Circulation and GasJohn Ted BañezNo ratings yet
- TransportationDocument58 pagesTransportatione-SayutiNo ratings yet
- Cardiology 2: OutlineDocument5 pagesCardiology 2: Outlinevinnie0905No ratings yet
- PMLS 2 ReviewerDocument8 pagesPMLS 2 ReviewerNepoy Beltran Entendez100% (3)
- One Point Acupressure Treatment AllDocument23 pagesOne Point Acupressure Treatment AllPraveen Kumar100% (1)
- Ventricular TachycardiaDocument2 pagesVentricular TachycardiaKim TaeyeonNo ratings yet
- Siemens Imaging AllDocument24 pagesSiemens Imaging AllVishnu0049No ratings yet
- Constrictive Pericarditis - UpToDateDocument26 pagesConstrictive Pericarditis - UpToDateSebastian CastañedaNo ratings yet
- Blood Vessels and Circulation 1Document36 pagesBlood Vessels and Circulation 1Kuya RnJNo ratings yet
- Physiology-1st Year Topical Past Papers-1Document14 pagesPhysiology-1st Year Topical Past Papers-1HussnainNo ratings yet
- Ventricular Fibrillation 2010Document9 pagesVentricular Fibrillation 2010Aisya HumairaNo ratings yet
- Heart SoundsDocument56 pagesHeart SoundsBetsy Babilonia100% (1)