Professional Documents
Culture Documents
14 - Uveitis
Uploaded by
Spislgal PhilipCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
14 - Uveitis
Uploaded by
Spislgal PhilipCopyright:
Available Formats
1
UVEITIS
Anatomy/Background
The iris regulates the amount of light that enters the eye, the ciliary body produces aqueous humor and supports the lens, and the choroid provides oxygen and nourishment for the retina.
Definition (Mayoclinic.com)
Uveitis is inflammation of the uvea, the middle layer of the eye. The uvea consists of the iris, choroid and ciliary body. The choroid is sandwiched between the retina and the white of the eye (sclera), and it provides blood flow to the deep layers of the retina. The most common type of uveitis is an inflammation of the iris called iritis (anterior uveitis).
Classifications (Brunner & Suddarth pg1790, Lippincott pg596, Medscape.com)
By Location: Anterior uveitis inflammation of the iris (iritis) and ciliary body (iridocyclitis) IS THE MOST COMMON Intermediate uveitis inflammation of the structures posterior to the lens (pars plantis or peripheral uveitis) Posterior uveitis inflammation of the choroid (choroiditis), retina (retinitis), or vitreous near the optic nerve and macula After anatomical classification, uveitis is further described by the following: Onset (sudden or non-granulomatous) vs. (insidious or granulomatous) Duration (limited less than 3 months in duration, or persistent greater than 3 months in duration) Course (acute, recurrent, or chronic) Laterality (unilateral vs. bilateral)
Incidence (Medscape.com)
1. United States - The estimated annual incidence is approximately 12 cases per 100,000 persons. 2. International - Uveitis is more common in Finland, where the annual incidence is approximately 23 cases per 100,000 persons. This is probably because of high frequency of the gene HLA-B27 in the population. 3. Mortality/Morbidity
No deaths due to iritis or uveitis have been reported. Morbidity results from posterior synechiae formation (adhesions between the iris and the lens) that may lead to high intraocular pressure and subsequent optic nerve loss.
2 4. The majority of patients are aged 20-50 years.
Etiology ((Brunner & Suddarth pg1790, Lippincott pg596, Medscape.com + Mayoclinic.com)
Sometimes, the specific cause of uveitis isn't clear (idiopathic/unknown). However, in some people, uveitis is associated with: (1)Inflammatory (2) Traumatic (3) Infections (4) Drug induced (5) Genetic Possible risk factors for uveitis include: A genetic predisposition - people with changes in certain genes may be more likely to develop uveitis. Having an infection - a number of infections, such as toxoplasmosis, cat-scratch fever, tuberculosis, herpes, syphilis and West Nile virus, can increase the risk of uveitis. Having an autoimmune or inflammatory disorder such as ankylosing spondylitis, sarcoidosis, Behcet's disease, ankylosing spondylitis, sarcoidosis, psoriatic arthritis, Crohn's disease and ulcerative colitis. A history of eye injury - trauma to the eye can cause uveitis. It's even possible for uveitis to develop in the eye that wasn't injured. Certain cancers, such as lymphoma, that can directly or indirectly affect the eye Drugs such as : rifabutin, cidofovir, sulfonamides, pamidronate
Pathophysiology
Will depend on the cause 1. The mechanism for trauma is believed to be a combination of microbial contamination and accumulation of necrotic products at the site of injury, thereby stimulating proinflammatory processes. For infectious etiologies of uveitis, it is postulated that the immune reaction directed against foreign molecules or antigens may injure the uveal tract vessels and cells. 2. When uveitis is found in association with autoimmune disorders, the mechanism may be a hypersensitivity reaction involving immune complex deposition within the uveal tract.
Clinical Manifestations/Signs & Symptoms
Diseases that predispose a patient to uveitis and are likely to present to the emergency department include inflammatory bowel disease, rheumatoid arthritis, systemic lupus erythematosus (SLE), sarcoidosis, tuberculosis, syphilis, and AIDS.
Complications (Mayoclinic.com)
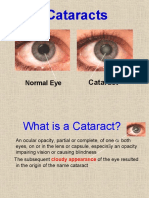
If left untreated, uveitis can cause the following complications: Abnormally high pressure inside the eye (glaucoma) Damage to the optic nerve Clouding of the lens (cataract) or cornea Retinal problems, such as fluid within the retina or retinal detachment Vision loss
Diagnostic Evaluation
If the uveitis is recurrent, a careful history should be initiated to discover any underlying causes.
This evaluation should include a complete history, physical examination, and diagnostic tests, including a complete blood cell count, erythrocyte sedimentation rate, antinuclear antibodies, and Venereal Disease Research Laboratory (VDRL) and Lyme disease titers
Nursing Assessment
((Brunner & Suddarth pg1790, Lippincott pg596, Medscape.com + Mayoclinic.com)
Hx Taking Questions to be asked When did you first begin experiencing symptoms? Have your symptoms been continuous or occasional? How severe are your symptoms? Have they gotten worse? Does anything seem to improve your symptoms? What, if anything, appears to worsen your symptoms? Have you ever had uveitis before? Do you have any other medical problems? Do you have arthritis? Do you have back problems? Have you had any recent skin rashes? Have you had any ulcerated sores in your mouth or on your genitalia? Have you had a recent upper respiratory infection or cold symptoms?
Medical Management
1. Wear dark glasses outdoors to help manage photophobia 2. Ciliary spasms and synechia are managed by mydriasis cyclopentolate (Cyclogyl) and atropine are used 3. Anti-inflammatory medication. Your doctor may prescribe anti-inflammatory medication, such as a corticosteroid, to treat your uveitis. This medication may be given as eye drops. Or, you may be given corticosteroid pills or an injection into the eye.
a. Local corticosteroid drops, such as Pred Forte 1% and Flarex 0.1%, instilled four to six times a day are also used to decrease inflammation. In very severe cases, systemic corticosteroids, as well as intravitreal corticosteroids, may be used. b. For people with difficult-to-treat posterior uveitis, a device that's implanted in your eye may be an option. This device slowly releases corticosteroid medication into your eye for about 2 1/2 years.
4. Antibiotic or antiviral medication. If uveitis is caused by an infection, antibiotics, antiviral medications or other medicines may be given with or without corticosteroids to bring the infection under control. 5. Immunosuppressive or cell-destroying (cytotoxic) medication. Immunosuppressive or cytotoxic agents may be necessary if your uveitis doesn't respond well to corticosteroids or becomes severe enough to threaten your vision. 6. Surgery. Vitrectomy surgery to remove some of the jelly-like material in your eye (vitreous) may be necessary both for diagnosis and management of your uveitis. A small sample of the vitreous can help identify a specific cause of eye inflammation, such as a virus, bacterium or lymphoma. The procedure may also be used to remove developing scar tissue in the vitreous.
Nursing Diagnosis, Interventions, and Expected Outcome
Family Education and Health Maintenance Discharge Planning
You might also like
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Case Presentation: by Michael ArmstrongDocument21 pagesCase Presentation: by Michael ArmstrongWirawan Amirul BahriNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Anal Canal: Fissure in Ano HaemorrhoidsDocument37 pagesAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNo ratings yet
- Chronic Suppurative Otitis MediaDocument11 pagesChronic Suppurative Otitis MediaaditiarrtuguNo ratings yet
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- Examination of A Comatose PatientDocument13 pagesExamination of A Comatose PatientReinaldy BasraNo ratings yet
- Anal and Perianal ConditionsDocument58 pagesAnal and Perianal ConditionsYonas YemidiralemNo ratings yet
- Otitis MediaDocument8 pagesOtitis MediamuhammadridhwanNo ratings yet
- Phimosis and ParaphimosisDocument3 pagesPhimosis and ParaphimosisJoshua PowersNo ratings yet
- Foreign Body in The NoseDocument32 pagesForeign Body in The NoseLady350zNo ratings yet
- Exudative Pleural Effusions - UpToDateDocument2 pagesExudative Pleural Effusions - UpToDateAsif IqbalNo ratings yet
- Chp9 Sclera DiseasesDocument23 pagesChp9 Sclera DiseasesUchyIntamNo ratings yet
- ConjunctivitisDocument52 pagesConjunctivitisFiona H.D.100% (2)
- Typhoid FeverDocument13 pagesTyphoid FeverSuhas Ingale0% (1)
- Final Hernioplasty Compilation RevisedDocument58 pagesFinal Hernioplasty Compilation RevisedRaidis PangilinanNo ratings yet
- Hyphema 2Document7 pagesHyphema 2heidyNo ratings yet
- PterygiumDocument3 pagesPterygiumtri_budi_20No ratings yet
- Anatomy and Physiology of The Conjunctiva: Presented by Arundhati Hatikakoty Bachelor of Optometry 3 Year Roll No-302Document43 pagesAnatomy and Physiology of The Conjunctiva: Presented by Arundhati Hatikakoty Bachelor of Optometry 3 Year Roll No-302Vincentius Okta VidiandickaNo ratings yet
- Amblyopia: Glomarie Hope A. Paquera Danica Ilah M. SincoDocument39 pagesAmblyopia: Glomarie Hope A. Paquera Danica Ilah M. SincoJan IrishNo ratings yet
- Parapneumonic Pleural Effusions and Empyema Thoracis - Background, Pathophysiology, EpidemiologyDocument4 pagesParapneumonic Pleural Effusions and Empyema Thoracis - Background, Pathophysiology, EpidemiologyLorentina Den PanjaitanNo ratings yet
- Anatomy and Diseases of The UveaDocument102 pagesAnatomy and Diseases of The UveaVishakh IsloorNo ratings yet
- AdenoidsDocument6 pagesAdenoidsIfeanyichukwu OgbonnayaNo ratings yet
- Renal Cell CarcinomaDocument10 pagesRenal Cell Carcinoma'asyura Mohd RezaNo ratings yet
- DB13 - Pathophysiology of AtherosclerosisDocument2 pagesDB13 - Pathophysiology of Atherosclerosisi_vhie03No ratings yet
- Orbital and Ocular TumorsDocument13 pagesOrbital and Ocular TumorsstarlytexpressNo ratings yet
- Running Head: A Patient Who Has Glaucoma 1Document10 pagesRunning Head: A Patient Who Has Glaucoma 1Alonso LugoNo ratings yet
- Nephrotic Syndrome: Dinesh Kumar PDocument42 pagesNephrotic Syndrome: Dinesh Kumar PRiya Sweetsolitude100% (1)
- Pemphigus vulgarisPPTDocument23 pagesPemphigus vulgarisPPTSiti HanisaNo ratings yet
- BlepharitisDocument20 pagesBlepharitisNorshahidah IedaNo ratings yet
- Best Aid To Ophthalmology - Pramod TK - 318Document3 pagesBest Aid To Ophthalmology - Pramod TK - 318Danielle SangalangNo ratings yet
- Case Studies - Tetralogy of FallotDocument16 pagesCase Studies - Tetralogy of FallotKunwar Sidharth SaurabhNo ratings yet
- Short Case 1 PterygiumDocument15 pagesShort Case 1 PterygiumAnmol KhadkaNo ratings yet
- Cataract: Mohd Roslee Bin Abd GhaniDocument46 pagesCataract: Mohd Roslee Bin Abd GhaniSaha DirllahNo ratings yet
- Management of OliguriaDocument14 pagesManagement of OliguriaAhmed El-MalkyNo ratings yet
- Malaria: Dr. Shree Narayan Yadav Internal Medicine Resident NamsDocument40 pagesMalaria: Dr. Shree Narayan Yadav Internal Medicine Resident Namsasyanadhikary18No ratings yet
- Carbolic Acid & Oxalic AcidDocument46 pagesCarbolic Acid & Oxalic AcidImteaz ahamadNo ratings yet
- Brain TumorDocument50 pagesBrain TumorbudiNo ratings yet
- Lateral Neck SwellingDocument62 pagesLateral Neck Swellingசுபத்ரா சந்திரசேகர்No ratings yet
- Acute Suppurative Otitis MediaDocument19 pagesAcute Suppurative Otitis MediaRajesh Sharma100% (1)
- NCP DIarrheaDocument8 pagesNCP DIarrheakamini ChoudharyNo ratings yet
- Nephrotic SyndromeDocument56 pagesNephrotic SyndromeMurugesan100% (1)
- Infective EndocarditisDocument58 pagesInfective EndocarditisTok KeawkaewNo ratings yet
- CataractDocument35 pagesCataractyusufharkianNo ratings yet
- Vitamin A and XerophthalmiaDocument29 pagesVitamin A and XerophthalmiaJayashree IyerNo ratings yet
- CataractDocument5 pagesCataractcarls burg a. resurreccionNo ratings yet
- Salpingitis: Sumber: 1. Dorland 2. Williams Gynecology 3. Better Health Channel Fact Sheet - SalpingitisDocument6 pagesSalpingitis: Sumber: 1. Dorland 2. Williams Gynecology 3. Better Health Channel Fact Sheet - Salpingitisearthbend_tophNo ratings yet
- Chronic Suppurative Otitis Media A Model Case Sheet by DrtbaluDocument2 pagesChronic Suppurative Otitis Media A Model Case Sheet by DrtbaluMaria Arifuddin0% (1)
- Peri TonsilLar AbscessDocument6 pagesPeri TonsilLar Abscessrivan90No ratings yet
- Lower Respiratory Tract Diseases - KeyDocument45 pagesLower Respiratory Tract Diseases - KeyYugmaPandyaNo ratings yet
- Infective EndocarditisDocument68 pagesInfective EndocarditisDr. Rajesh PadhiNo ratings yet
- Thesis Protocol For M.S. Degree (Ophthalmology)Document31 pagesThesis Protocol For M.S. Degree (Ophthalmology)zebaNo ratings yet
- Mounika G1Document8 pagesMounika G1pandem soniyaNo ratings yet
- PUK Vs Mooren Ulcer Presentasi FinalDocument35 pagesPUK Vs Mooren Ulcer Presentasi FinalRaissaNo ratings yet
- Chronic Tonsillitis PDFDocument27 pagesChronic Tonsillitis PDFAnanta Ayu WulansariNo ratings yet
- Cataract InformationDocument25 pagesCataract Informationvasanth_1515No ratings yet
- Meniere's DiseaseDocument50 pagesMeniere's DiseaseRaisa CleizeraNo ratings yet
- STDDocument78 pagesSTDKrupa KarnikNo ratings yet
- Nursing Care of The ElderlyDocument11 pagesNursing Care of The ElderlySpislgal PhilipNo ratings yet
- Antibiotics and Their Types, Uses, Side EffectsDocument4 pagesAntibiotics and Their Types, Uses, Side EffectsSpislgal PhilipNo ratings yet
- TrachomaDocument6 pagesTrachomaSpislgal PhilipNo ratings yet
- PressureUlcer GradingToolDocument1 pagePressureUlcer GradingToolSpislgal PhilipNo ratings yet
- Maintaining Health in The Geriatric PatientDocument10 pagesMaintaining Health in The Geriatric PatientSpislgal PhilipNo ratings yet
- Legal Issues - Practice EssaysDocument1 pageLegal Issues - Practice EssaysSpislgal PhilipNo ratings yet
- Biochemistry Study Guide - CarbohydratesDocument4 pagesBiochemistry Study Guide - CarbohydratesSpislgal PhilipNo ratings yet
- A Woman of StrengthDocument1 pageA Woman of StrengthSpislgal PhilipNo ratings yet
- Theories On Aging - Partial Notes From ScribdDocument2 pagesTheories On Aging - Partial Notes From ScribdSpislgal PhilipNo ratings yet
- Common Lab ValuesDocument7 pagesCommon Lab ValuesSpislgal PhilipNo ratings yet
- Emergency NursingDocument5 pagesEmergency NursingSpislgal PhilipNo ratings yet
- Study LikeDocument1 pageStudy LikeSpislgal PhilipNo ratings yet
- God's Gift: My Prayers Have Been AnsweredDocument1 pageGod's Gift: My Prayers Have Been AnsweredSpislgal PhilipNo ratings yet
- Biochemistry Study Guide - Electron TransportDocument7 pagesBiochemistry Study Guide - Electron TransportSpislgal PhilipNo ratings yet
- OsteomyelitisDocument4 pagesOsteomyelitisSpislgal PhilipNo ratings yet
- Cranial Nerve Function TestDocument1 pageCranial Nerve Function TestSpislgal PhilipNo ratings yet
- Study Guide - The Nervous SystemDocument2 pagesStudy Guide - The Nervous SystemSpislgal PhilipNo ratings yet
- What Is Epidemiology - A General OverviewDocument2 pagesWhat Is Epidemiology - A General OverviewSpislgal PhilipNo ratings yet
- HIV and SpermDocument2 pagesHIV and SpermSpislgal PhilipNo ratings yet
- Chalazion ConditionDocument6 pagesChalazion ConditionSpislgal Philip100% (1)
- Professionalism in NursingDocument4 pagesProfessionalism in NursingSpislgal Philip100% (6)
- 1 - MyopiaDocument9 pages1 - MyopiaSpislgal PhilipNo ratings yet
- Medical Surgical Exam Part 1Document16 pagesMedical Surgical Exam Part 1api-382250888% (42)
- Nurse CartoonsDocument3 pagesNurse CartoonsSpislgal PhilipNo ratings yet
- Primary Health Care Presentation - Dr. Rasha SalamaDocument40 pagesPrimary Health Care Presentation - Dr. Rasha SalamaSpislgal PhilipNo ratings yet
- Maternal and Child Health Practice Test Part 1Document12 pagesMaternal and Child Health Practice Test Part 1Spislgal PhilipNo ratings yet
- Procedure - Assessment Body TemperatureDocument3 pagesProcedure - Assessment Body TemperatureSpislgal PhilipNo ratings yet
- Citric Acid CycleDocument1 pageCitric Acid CycleSpislgal PhilipNo ratings yet
- Ornithine or Urea CycleDocument1 pageOrnithine or Urea CycleSpislgal PhilipNo ratings yet
- Prinsip Prinsip SurveilansDocument30 pagesPrinsip Prinsip SurveilansYona TarunaNo ratings yet
- Possible Bacteria Pathogens Found in The Internal Surface of Ladies Handbags in Umuahia, Abia State, South-Eastern NigeriaDocument8 pagesPossible Bacteria Pathogens Found in The Internal Surface of Ladies Handbags in Umuahia, Abia State, South-Eastern NigeriaUMYU Journal of Microbiology Research (UJMR)No ratings yet
- History and Pathology of Vaccination by Edgar M. Crookshank, M.B. (1889)Document560 pagesHistory and Pathology of Vaccination by Edgar M. Crookshank, M.B. (1889)puckett33100% (1)
- Heamatology Dr. Osama PDFDocument94 pagesHeamatology Dr. Osama PDFRaouf Ra'fat Soliman80% (5)
- SCHITOSOMIASISDocument8 pagesSCHITOSOMIASISxteph04No ratings yet
- CPWP Orientation Manual - REWORKEDmarch 2011Document257 pagesCPWP Orientation Manual - REWORKEDmarch 2011habotugeunimNo ratings yet
- Ta Bo LaDocument65 pagesTa Bo LaFina RepitiyanaNo ratings yet
- HivrenewalformDocument3 pagesHivrenewalformkbl27No ratings yet
- Biochemistry MnemonicsDocument10 pagesBiochemistry MnemonicsEsam RiveraNo ratings yet
- 1 s2.0 S0944501322000507 MainDocument19 pages1 s2.0 S0944501322000507 Mainsalmanurani warodatuszaqiahNo ratings yet
- The Efforts of The Philippine Government in Preventing COVID-19 InfectionDocument2 pagesThe Efforts of The Philippine Government in Preventing COVID-19 InfectionLJ MermidaNo ratings yet
- s4 l3 Nematodes IIDocument14 pagess4 l3 Nematodes II2013SecB100% (1)
- Expanded Program On ImmunizationDocument4 pagesExpanded Program On ImmunizationcharmdoszNo ratings yet
- T CellDocument36 pagesT CellSurja DasNo ratings yet
- Fungal Dieases in PlantDocument9 pagesFungal Dieases in Plantsauravv7No ratings yet
- Nursing Case Study (Final) - ArchieDocument23 pagesNursing Case Study (Final) - ArchieArchie Astorga100% (2)
- Presented By:dr - Anita Chaudhari Roll No: 2Document22 pagesPresented By:dr - Anita Chaudhari Roll No: 2younismushtaq100% (1)
- Respiratory DisorderDocument2 pagesRespiratory DisorderMarkdanielRamiterreNo ratings yet
- Philippine NLE Board ExamDocument29 pagesPhilippine NLE Board ExamMarlo Valdez82% (28)
- MHC Class 1 and 2Document14 pagesMHC Class 1 and 2Ömer KhanNo ratings yet
- Blueberry Propagation SuggestionsDocument8 pagesBlueberry Propagation SuggestionsJovan Ličanin100% (1)
- Antibiotic GuidelineDocument60 pagesAntibiotic GuidelineNazmul Alam FarukiNo ratings yet
- Prepration of The Isolation UnitDocument43 pagesPrepration of The Isolation UnitGayatri MudliyarNo ratings yet
- Public Health Approaches To Malaria: Source: National Library of MedicineDocument24 pagesPublic Health Approaches To Malaria: Source: National Library of MedicineRahmalia Fitri RosaNo ratings yet
- Background of The StudyDocument11 pagesBackground of The StudyWaleed JaddiNo ratings yet
- BronchiolitisDocument17 pagesBronchiolitisRizky DarmawanNo ratings yet
- Multisystem & Genetic - BoardsDocument10 pagesMultisystem & Genetic - BoardsSoojung NamNo ratings yet
- HAI BrochureDocument6 pagesHAI BrochureNidia MaradiagaNo ratings yet
- Hooligans Contract of SaleDocument4 pagesHooligans Contract of Saleapi-245350059No ratings yet
- Lymph Ad en Op A ThyDocument24 pagesLymph Ad en Op A ThyAlyaa El SayedNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)