Professional Documents
Culture Documents
Acr Auim PDF
Uploaded by
dgina8800Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acr Auim PDF
Uploaded by
dgina8800Copyright:
Available Formats
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists,
and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice guidelines and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice guidelines and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice guideline and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review, requiring the approval of the Commission on Quality and Safety as well as the ACR Board of Chancellors, the ACR Council Steering Committee, and the ACR Council. The practice guidelines and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice guideline and technical standard by those entities not providing these services is not authorized .
Revised 2010 (Resolution 30)*
ACR-AIUM-SRU PRACTICE GUIDELINE FOR THE PERFORMANCE OF PERIPHERAL ARTERIAL ULTRASOUND USING COLOR AND SPECTRAL DOPPLER
PREAMBLE These guidelines are an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. They are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care. For these reasons and those set forth below, the American College of Radiology cautions against the use of these guidelines in litigation in which the clinical decisions of a practitioner are called into question. The ultimate judgment regarding the propriety of any specific procedure or course of action must be made by the physician or medical physicist in light of all the circumstances presented. Thus, an approach that differs from the guidelines, standing alone, does not necessarily imply that the approach was below the standard of care. To the contrary, a conscientious practitioner may responsibly adopt a course of action different from that set forth in the guidelines when, in the reasonable judgment of the practitioner, such course of action is indicated by the condition of the patient, limitations of available resources, or advances in knowledge or technology subsequent to publication of the guidelines. However, a practitioner who employs an approach substantially different from these guidelines is advised to document in the patient record information sufficient to explain the approach taken. The practice of medicine involves not only the science, but also the art of dealing with the prevention, diagnosis, alleviation, and treatment of disease. The variety and complexity of human conditions make it impossible to always reach the most appropriate diagnosis or to predict with certainty a particular response to treatment. Therefore, it should be recognized that adherence to these guidelines will not assure an accurate diagnosis or a successful outcome. All that should be expected is that the practitioner will follow a reasonable course of action based on current knowledge, available resources, and the needs of the patient to deliver effective and safe medical care. The sole purpose of these guidelines is to assist practitioners in achieving this objective. I. INTRODUCTION
The clinical aspects contained in specific sections of this guideline (Introduction, Indications, Specifications of the Examination, and Equipment Specifications) were developed collaboratively by the American College of Radiology (ACR), the American Institute of Ultrasound in Medicine (AIUM), and the Society of Radiologists in Ultrasound (SRU). Recommendations for physician requirements, written request for the examination, procedure documentation, and quality control vary among the three organizations and are addressed by each separately. These guidelines are intended to assist practitioners performing noninvasive evaluation of the peripheral arteries using color and spectral Doppler ultrasound. The sonographic examination of patients with peripheral vascular disease will, in general, complement the use of other physiologic tests, such as pressure measurements, pulse volume recordings, and continuous wave Doppler.
PRACTICE GUIDELINE
Peripheral Arterial Ultrasound / 1
In selected cases a tailored examination is used to answer a specific diagnostic question. While it is not possible to detect every abnormality, adherence to the following guidelines will maximize the probability of detecting most of the abnormalities that occur in the extremity arteries. II. INDICATIONS FOR PERIPHERAL ARTERIAL EXAMINATIONS ultrasound
See the ACRSPRSRU Practice Guideline for Performing and Interpreting Diagnostic Ultrasound Examinations. IV. WRITTEN REQUEST FOR THE EXAMINATION
Each organization will address this section in its document. ACR language is as follows: The written or electronic request for a peripheral arterial ultrasound examination should provide sufficient information to demonstrate the medical necessity of the examination and allow for its proper performance and interpretation. Documentation that satisfies medical necessity includes 1) signs and symptoms and/or 2) relevant history (including known diagnoses). Additional information regarding the specific reason for the examination or a provisional diagnosis would be helpful and may at times be needed to allow for the proper performance and interpretation of the examination. The request for the examination must be originated by a physician or other appropriately licensed health care provider. The accompanying clinical information should be provided by a physician or other appropriately licensed health care provider familiar with the patients clinical problem or question and consistent with the states scope of practice requirements. (ACR Resolution 35, adopted in 2006) V. SPECIFICATIONS OF THE EXAMINATION
The indications for peripheral arterial examination include, but are not limited to: 1.
The detection of hemodynamically significant stenoses or occlusions in specified segment(s) of the peripheral arteries in symptomatic patients with suspected arterial occlusive disease. These patients could present with recognized clinical indicators, including claudication, rest pain, ischemic tissue loss, or suspected arterial embolizations [1-8]. The monitoring of sites of previous surgical interventions, including sites of previous bypass surgery with either synthetic or autologous vein grafts [9,10]. The monitoring of sites of various percutaneous interventions, including angioplasty, thrombolysis/thrombectomy, atherectomy, or stent placements [11]. The evaluation of suspected vascular and perivascular abnormalities, including such entities as masses, aneurysms, pseudoaneurysms [12], or arteriovenous fistulae. Mapping of arteries interventions [1,13]. prior to surgical
2.
3.
4.
5.
6.
Clarifying or confirming the presence of significant arterial abnormalities identified by other imaging modalities.
Additional uses of Doppler ultrasound can include preoperative mapping for dialysis access and postoperative follow-up (see the ACRAIUMSRU Practice Guideline for the Performance of Ultrasound Vascular Mapping for Preoperative Planning of Dialysis Access and the ACRAIUM Practice Guideline for the Performance of Vascular Ultrasound for Postoperative Assessment of Dialysis Access) [14]. III. QUALIFICATIONS AND RESPONSIBILITIES OF THE PHYSICIAN
The initial examination for determining the presence of arterial occlusive disease remains the determination of blood pressures in the extremities being studied. Blood pressure measurement at different levels should be reported as a ratio (e.g., ankle/brachial index) where appropriate. The sonographic examination consists of grayscale imaging and the evaluation of the spectral Doppler waveforms in the corresponding arterial segments. Color Doppler should be used to improve detection of arterial lesions and guide placement of the sample volume for spectral Doppler assessment [15]. A. Appropriate Techniques and Diagnostic Criteria Specific sonographic techniques must be tailored to the different arterial segments studied and to the specific pathology being evaluated. Established imaging, Doppler, and pressure criteria may be used to identify arterial stenoses and occlusions, identify graft abnormalities, detect abnormal arteriovenous communications, and evaluate suspected soft tissue abnormalities in proximity to an artery. PRACTICE GUIDELINE
Each organization will address this section in its document. ACR language is as follows: 2 / Peripheral Arterial Ultrasound
B. Arterial Occlusive Disease For arterial occlusive disease, the following general considerations apply. The full length of the arterial segment(s) of interest should be evaluated with color Doppler. Suspected abnormalities should also be imaged with grayscale ultrasound. Representative spectral Doppler waveforms with velocity measurements should be obtained and documented along the length of the arterial segment(s) and at any area of color or grayscale abnormality. A spectral Doppler waveform with velocity measurements in the arterial segment 2 to 4 cm proximal (upstream) to any stenosis should be documented. The location and the length of any diseased or nonvisualized segment(s) should also be documented. Every attempt should be made to acquire spectral Doppler waveforms with velocity measurements with the angle between the direction of moving blood and the direction of the ultrasound beam kept at less than or equal to 60 degrees. Velocity estimates made with larger angles are less reliable. An evaluation of the following arterial segments should generally be performed as indicated below. However, a focused or limited examination may be appropriate in certain clinical situations. At a minimum an angle corrected spectral Doppler waveform with velocity measurements should be obtained from the following sites: 1. Lower extremity a. Common femoral artery. b. Proximal superficial femoral artery. c. Mid superficial femoral artery. d. Distal superficial femoral artery. e. Popliteal artery. If clinically appropriate, imaging of the iliac, deep femoral, tibio-peroneal, and dorsalis pedis arteries can be performed. 2. Upper extremity a. Subclavian artery. b. Axillary artery. c. Brachial artery. If clinically appropriate, imaging of the innominate, radial, and ulnar arteries and/or the palmar arch can be performed. C. Evaluation Interventions 1. of Surgical and Percutaneous 3.
with color Doppler. Suspected abnormalities should also be imaged with grayscale ultrasound. Spectral Doppler waveforms and velocity measurements should be documented in the native artery proximal to the graft anastomosis, at the proximal anastomosis, at representative sites along the graft, at the distal anastomosis, and in the native artery distal to the anastomosis. Angle corrected spectral Doppler waveforms and velocity measurements should also be obtained in regions of suspected flow abnormalities noted on grayscale or color Doppler imaging. 2. Sites having interventions undergone percutaneous
An attempt should be made to sample the site of selective arterial interventions as well as the segment immediately proximal (upstream) and distal (downstream) to the site of intervention. Spectral Doppler waveforms and velocity measurements should be documented. D. Other 1. Suspected soft tissue abnormalities in proximity to arteries The entire area of a suspected soft tissue abnormality should be imaged. If appropriate, spectral and color Doppler may be performed to determine the presence and nature of blood flow in the region of the suspected abnormality. 2. Pseudoaneurysms The size of the pseudoaneurysm, the residual lumen, and the length and width of the communicating channel should be documented. Spectral Doppler waveforms should be obtained in the communicating channel to demonstrate to-and-fro flow. In case of therapeutic intervention, color and/or spectral Doppler may be used as a guide to therapy and as a means of documenting therapeutic success [12,16-18]. Abnormal communication between artery and vein Color and spectral color Doppler may be used to document the location of abnormal vascular communications. Angle corrected spectral Doppler waveforms should be documented from within vessels proximal to, in the area of, and distal to abnormal communications. Color Doppler is particularly useful for identifying the level of such communications and resultant
Bypass grafts An attempt should be made to sample the full length of any bypass graft whenever possible
PRACTICE GUIDELINE
Peripheral Arterial Ultrasound / 3
transmitted soft tissue vibrations secondary to the flow disturbances produced by abnormal vascular communications. VI. DOCUMENTATION
Safety, Infection Control, and Patient Education on the ACR web page (http://www.acr.org/guidelines). Equipment performance monitoring should be in accordance with the ACR Technical Standard for Diagnostic Medical Physics Performance Monitoring of Real Time Ultrasound Equipment. ACKNOWLEDGEMENTS
Each organization will address this section in its document. ACR language is as follows: Adequate documentation is essential for high-quality patient care. There should be a permanent record of the ultrasound examination and its interpretation. Comparison with prior relevant imaging studies may prove helpful. Images of all appropriate areas, both normal and abnormal, should be recorded. Variations from normal size should generally be accompanied by measurements. Images should be labeled with the patient identification, facility identification, examination date, and image orientation. An official interpretation (final report) of the ultrasound examination should be included in the patients medical record. Retention of the ultrasound examination images should be consistent both with clinical need and with relevant legal and local health care facility requirements. Reporting should be in accordance with the ACR Practice Guideline for Communication of Diagnostic Imaging Findings. VII. EQUIPMENT SPECIFICATIONS
This guideline was revised according to the process described under the heading The Process for Developing ACR Practice Guidelines and Technical Standards on the ACR web page (http://www.acr.org/guidelines) by the Guidelines and Standards Committee of the Commission on Ultrasound in collaboration with the AIUM and the SRU. Collaborative Committee ACR Michelle L. Robbin, MD, FACR, Chair John S. Pellerito, MD Joseph F. Polak, MD, MPH AIUM M. Robert De Jong, RDMS, RVT Laurence Needleman, MD, FACR Leslie M. Scoutt, MD SRU Edward G. Grant, MD, FACR Janis G. Letourneau, MD ACR Guidelines and Standards Committee Ultrasound Mary C. Frates, MD, FACR, Chair Debra L. Acord, MD Marcela Bohm-Velez, MD, FACR Helena Gabriel, MD Ruth B. Goldstein, MD Robert D. Harris, MD, MPH, FACR Beverly E. Hashimoto, MD, FACR Leann E. Linam, MD Laurence Needleman, MD, FACR Maitray D. Patel, MD Philip W. Ralls, MD, FACR Michelle L. Robbin, MD, FACR Robert M. Sinow, MD Deborah Levine, MD, FACR, Chair, Commission REFERENCES 1. Avenarius JK, Breek JC, Lampmann LE, van Berge Henegouwen DP, Hamming JF. The additional value of angiography after colour-coded duplex on decision making in patients with critical limb ischaemia. A prospective study. Eur J Vasc Endovasc Surg 2002;23:393-397.
Peripheral arterial sonography should be performed with a real-time scanner with a linear array or curved array transducer equipped with pulsed Doppler and color Doppler capability. (Power or energy Doppler may be used if needed.) The transducer should operate at the highest clinically appropriate frequency, recognizing that there is a trade-off between resolution and penetration. This should usually be at a frequency of 3.5 MHz or greater, with the occasional need for a lower frequency transducer. Evaluation of the flow signals originating from within the lumen of the vessel should be conducted with a carrier frequency of 2.5 MHz or greater. VIII. QUALITY CONTROL AND IMPROVEMENT, SAFETY, INFECTION CONTROL, AND PATIENT EDUCATION
Each organization will address this section in its document. ACR language is as follows: Policies and procedures related to quality, patient education, infection control, and safety should be developed and implemented in accordance with the ACR Policy on Quality Control and Improvement, Safety, Infection Control, and Patient Education appearing under the heading Position Statement on QC & Improvement,
4 / Peripheral Arterial Ultrasound
PRACTICE GUIDELINE
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
Kohler TR, Nance DR, Cramer MM, Vandenburghe N, Strandness DE, Jr. Duplex scanning for diagnosis of aortoiliac and femoropopliteal disease: a prospective study. Circulation 1987;76:1074-1080. Mulligan SA, Matsuda T, Lanzer P, et al. Peripheral arterial occlusive disease: prospective comparison of MR angiography and color duplex US with conventional angiography. Radiology 1991;178:695700. Polak JF. Arterial sonography: efficacy for the diagnosis of arterial disease of the lower extremity. AJR 1993;161:235-243. Polak JF, Karmel MI, Mannick JA, O'Leary DH, Donaldson MC, Whittemore AD. Determination of the extent of lower-extremity peripheral arterial disease with color-assisted duplex sonography: comparison with angiography. AJR 1990;155:10851089. Ranke C, Creutzig A, Alexander K. Duplex scanning of the peripheral arteries: correlation of the peak velocity ratio with angiographic diameter reduction. Ultrasound Med Biol 1992;18:433-440. Talbot SR, Zwiebel WJ. Assessment of upper extremity arterial occlusive disease. In: Zwiebel WJ, Pellerito JS, ed. Introduction to Vascular Ultrasonography. 5th ed. New York, NY: Elsevier; 2005. Letourneau J, Beidel, T. Arm Swelling. In: Bluth E, Benson C, Ralls P, Siegel M, ed. Ultrasound: A Practical Approach to Clinical Problems. 2nd ed. New York, NY: Thieme; 2008:613-626. Fasih T, Rudol G, Ashour H, Mudawi A, Bhattacharya V. Surveillance versus nonsurveillance for femoro-popliteal bypass grafts. Angiology 2004; 55:251-256. Ferris BL, Mills JL, Sr., Hughes JD, Durrani T, Knox R. Is early postoperative duplex scan surveillance of leg bypass grafts clinically important? J Vasc Surg 2003;37:495-500. Gerhard-Herman M, Gardin JM, Jaff M, Mohler E, Roman M, Naqvi TZ. Guidelines for noninvasive vascular laboratory testing: a report from the American Society of Echocardiography and the Society for Vascular Medicine and Biology. Vasc Med 2006;11:183-200. Paulson EK, Sheafor DH, Kliewer MA, et al. Treatment of iatrogenic femoral arterial pseudoaneurysms: comparison of US-guided thrombin injection with compression repair. Radiology 2000;215:403-408. Koelemay MJ, Legemate DA, de Vos H, et al. Duplex scanning allows selective use of arteriography in the management of patients with severe lower leg arterial disease. J Vasc Surg 2001;34:661-667. Robbin ML, Lockhart MR. Ultrasound assessment before and after hemodialysis access. In: Zwiebel WJ, Pellerito JS, ed. Introduction to Vascular Ultrasonography. 5th ed. New York, NY: Elsevier; 2005.
15. Pellerito JS. Current approach to peripheral arterial sonography. Radiol Clin North Am 2001;39:553-567. 16. Kang SS, Labropoulos N, Mansour MA, Baker WH. Percutaneous ultrasound guided thrombin injection: a new method for treating postcatheterization femoral pseudoaneurysms. J Vasc Surg 1998;27:1032-1038. 17. Khoury M, Rebecca A, Greene K, et al. Duplex scanning-guided thrombin injection for the treatment of iatrogenic pseudoaneurysms. J Vasc Surg 2002;35:517-521. 18. Paulson EK, Nelson RC, Mayes CE, Sheafor DH, Sketch MH, Jr., Kliewer MA. Sonographically guided thrombin injection of iatrogenic femoral pseudoaneurysms: further experience of a single institution. AJR 2001;177:309-316. Suggested Reading (Additional articles that are not cited in the document but that the committee recommends for further reading on this topic) 19. Carrol B. Pulsatile groin mass in the postcatherterization patient. In: Bluth E, Benson C, Ralls P, Siegel M, ed. Ultrasound: A Practical Approach to Clinical Problems. 2nd ed. New York: Thieme; 2008:588-601. 20. Zweibel W. Painful legs after walking. In: Bluth E, Benson C, Ralls P, Siegel M, ed. Ultrasound: A Practical Approach to Clinical Problems. 2nd ed. New York, NY: Thieme; 2008:602-612.
*Guidelines and standards are published annually with an effective date of October 1 in the year in which amended, revised or approved by the ACR Council. For guidelines and standards published before 1999, the effective date was January 1 following the year in which the guideline or standard was amended, revised, or approved by the ACR Council. Development Chronology for this Guideline 1993 (Resolution 7) Amended 1995 (Resolution 53) Revised 1997 (Resolution 29) Revised 2001 (Resolution 35) Revised 2006 (Resolution 41, 35) Revised 2010 (Resolution 30)
PRACTICE GUIDELINE
Peripheral Arterial Ultrasound / 5
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Cases CX CarcinomaDocument2 pagesCases CX Carcinomadgina8800No ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Rush Echo Massive Air EmbolismDocument3 pagesRush Echo Massive Air Embolismdgina8800No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Target Marketing: Target Marketing Is "The Process of Identifying Market Segments, Selecting OneDocument7 pagesTarget Marketing: Target Marketing Is "The Process of Identifying Market Segments, Selecting Onedgina8800No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- 44 Traditional Medicine FINALDocument72 pages44 Traditional Medicine FINALdgina8800No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Echocardiography AdvanceDocument8 pagesEchocardiography Advancedgina88000% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- E Learn CAE - ICCU - LoRes PDFDocument8 pagesE Learn CAE - ICCU - LoRes PDFdgina8800No ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- 4 Print Form Cardiac - USDocument1 page4 Print Form Cardiac - USdgina8800No ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Echo Case Ao RegurgDocument3 pagesEcho Case Ao Regurgdgina8800No ratings yet
- 4P Fellowship Pros & Cons & Focus On Ultrasound Fellowship GaspariDocument5 pages4P Fellowship Pros & Cons & Focus On Ultrasound Fellowship Gasparidgina8800No ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- New Brochure FTTE 11-2-2010Document4 pagesNew Brochure FTTE 11-2-2010dgina8800No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Standardized Echo Report Rev1Document38 pagesStandardized Echo Report Rev1dgina8800100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Medical Terminology On CPC Exam2 - YouTubeDocument2 pagesMedical Terminology On CPC Exam2 - YouTubedgina8800No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- A FEEL@Chelmers Flyer 02 14Document1 pageA FEEL@Chelmers Flyer 02 14dgina8800No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Ocr Graphics Gcse CourseworkDocument6 pagesOcr Graphics Gcse Courseworkzys0vemap0m3100% (2)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- A Study On Mistakes and Errors in Consecutive Interpretation From Vietnamese To English. Dang Huu Chinh. Qhf.1Document38 pagesA Study On Mistakes and Errors in Consecutive Interpretation From Vietnamese To English. Dang Huu Chinh. Qhf.1Kavic100% (2)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Ant Colony AlgorithmDocument11 pagesAnt Colony Algorithmjaved765No ratings yet
- B2 First Unit 11 Test: Section 1: Vocabulary Section 2: GrammarDocument1 pageB2 First Unit 11 Test: Section 1: Vocabulary Section 2: GrammarNatalia KhaletskaNo ratings yet
- India Internet Goldman SachsDocument86 pagesIndia Internet Goldman SachsTaranjeet SinghNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- SDLC Review ChecklistDocument4 pagesSDLC Review Checklistmayank govilNo ratings yet
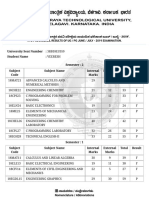
- VTU Result PDFDocument2 pagesVTU Result PDFVaibhavNo ratings yet
- Kepimpinan BerwawasanDocument18 pagesKepimpinan BerwawasanandrewanumNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- 3723 Modernizing HR at Microsoft BCSDocument14 pages3723 Modernizing HR at Microsoft BCSYaseen SaleemNo ratings yet
- NCLEX 20QUESTIONS 20safety 20and 20infection 20controlDocument8 pagesNCLEX 20QUESTIONS 20safety 20and 20infection 20controlCassey MillanNo ratings yet
- Paleontology 1Document6 pagesPaleontology 1Avinash UpadhyayNo ratings yet
- Tate J. Hedtke SPED 608 Assignment #6 Standard # 8 Cross Categorical Special Education/ Learning Disabilities Artifact SummaryDocument5 pagesTate J. Hedtke SPED 608 Assignment #6 Standard # 8 Cross Categorical Special Education/ Learning Disabilities Artifact Summaryapi-344731850No ratings yet
- Local Anesthesia For The Dental Hygienist 2nd Edition Logothetis Test BankDocument12 pagesLocal Anesthesia For The Dental Hygienist 2nd Edition Logothetis Test BankJessicaPorterfqmei100% (18)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Schmitt Allik 2005 ISDP Self Esteem - 000 PDFDocument20 pagesSchmitt Allik 2005 ISDP Self Esteem - 000 PDFMariana KapetanidouNo ratings yet
- Visual Impairments in Young Children: Fundamentals of and Strategies For Enhancing DevelopmentDocument13 pagesVisual Impairments in Young Children: Fundamentals of and Strategies For Enhancing Developmentfadil ahmadiNo ratings yet
- Superscope, Inc. v. Brookline Corp., Etc., Robert E. Lockwood, 715 F.2d 701, 1st Cir. (1983)Document3 pagesSuperscope, Inc. v. Brookline Corp., Etc., Robert E. Lockwood, 715 F.2d 701, 1st Cir. (1983)Scribd Government DocsNo ratings yet
- MathTextbooks9 12Document64 pagesMathTextbooks9 12Andrew0% (1)
- ECON266 Worksheet 8Document4 pagesECON266 Worksheet 8Oi OuNo ratings yet
- Operations Management and Operations PerformanceDocument59 pagesOperations Management and Operations PerformancePauline LagtoNo ratings yet
- Top Websites Ranking - Most Visited Websites in May 2023 - SimilarwebDocument3 pagesTop Websites Ranking - Most Visited Websites in May 2023 - SimilarwebmullahNo ratings yet
- BattleRope Ebook FinalDocument38 pagesBattleRope Ebook FinalAnthony Dinicolantonio100% (1)
- Unilateral Lower Limb SwellingDocument1 pageUnilateral Lower Limb SwellingLilius TangNo ratings yet
- Evaluation of The Performance of HRCT in The Diagnostic and Management of Covid-19Document7 pagesEvaluation of The Performance of HRCT in The Diagnostic and Management of Covid-19IJAR JOURNALNo ratings yet
- Ais Activiy Chapter 5 PDFDocument4 pagesAis Activiy Chapter 5 PDFAB CloydNo ratings yet
- Adobe Voice Assessment Tool-FinalDocument1 pageAdobe Voice Assessment Tool-Finalapi-268484302No ratings yet
- WaveDocument1 pageWavejimbieNo ratings yet
- U6 - S7 - Trabajo Individual 7 - Ficha de Aplicación INGLES 3Document2 pagesU6 - S7 - Trabajo Individual 7 - Ficha de Aplicación INGLES 3Antonio Andres Duffoo MarroquinNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- OITE - MCQ S QuestionsFinal2011Document67 pagesOITE - MCQ S QuestionsFinal2011KatKut99100% (7)
- FSR 2017-2018 KNL CircleDocument136 pagesFSR 2017-2018 KNL CircleparthaNo ratings yet
- Observation: Student: Liliia Dziuda Date: 17/03/21 Topic: Movie Review Focus: Writing SkillsDocument2 pagesObservation: Student: Liliia Dziuda Date: 17/03/21 Topic: Movie Review Focus: Writing SkillsLiliaNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)