Professional Documents
Culture Documents
Shige LL
Uploaded by
Drashua AshuaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Shige LL
Uploaded by
Drashua AshuaCopyright:
Available Formats
Shigellosis infections case definition summary
Public Health Laboratory Network case definitions PHLN0006 Version: 1 Consensus Date: 29 May 2000 Authorisation: PHLN
1. Introduction
Shigella causes bloody diarrhoea (dysentery) and non-bloody diarrhoea. Shigellosis often begins with watery diarrhoea accompanied by fever and abdominal cramps but may progress to classical dysentery with scant stools containing blood mucus and pus. All four species of Shigella are capable of causing dysentery, but Sh.dysenteriae 1 has been associated with a particularly severe form of the illness thought to be related to its production of Shiga toxin. In 1998, 527cases of shigellosis were notified to the National Enteric Pathogens Surveillance Scheme (Anonymous. 1999). The dominant types were Sh.sonnei and Sh.flexneri 2a. Reference Anonymous, 1999 NEPSS Human Annual Report 1998, 3/99
2. Laboratory diagnosis/tests
2.1 Culture for Shigella species
While shigellae are classed as non-fastidious organisms, because of the nature of the specimens for culture, Shigella detection is still highly dependent on employing appropriate culture media. 2.1.1 Media For optimal isolation of Shigella, two different selective media should be used: a general - purpose plating medium of low selectivity ( e.g., MacConkey-MAC) and a more selective agar medium (e.g. xylose lysine desoxycholate agar-XLD). Salmonella -shigella agar (SS) should be used with caution because it inhibits some strains of Sh.dysenteriae There is no reliable effective enrichment medium for all types of Shigella, but gram-negative (GN) broth and Selenite broth are frequently used (Murray et.al. 1999).
2.1.2 Suitable specimens Faeces/rectal swab. Faeces collected in an appropriate sterile container, transported to the laboratory ASAP (if longer than 2h keep at 4 C), may be stored at 4 C for 24 hours before culture. Rectal swabs put into a tube transport medium containing modified Stuart's medium, transported to the laboratory ASAP. May be stored at RT for 24 hours before culture. 2.1.3 Test sensitivity No mathematical data available. Depends on the quality of the specimen, the type of media chosen, the number of organisms and the time of collection after the onset of diarrhoea. Antibiotic treatment may inhibit growth of shigellae 2.1.4 Test specificity No mathematical data available. The isolation of a Shigella like organism, confirmed by specific biochemical and preliminary serological techniques. At this point it is a "presumptive Shigella" The isolation of a Shigella species is significant. 2.1.5 Predictive values A negative culture does not exclude the diagnosis of shigellosis. 2.1.6 Suitable acceptance criteria. On MAC, XLD or SS a non-lactose fermenting, non-spreading colonies which biochemically fit a Shigella species. 2.1.7 Suitable internal controls Properly documented, relevant, quality control program for each type and batch of medium used. Use of a control Shigella with each batch of cultures is not recommended because of the risk of cross contamination of the test organisms. 2.1.8 Suitable test validation criteria Isolation of a Shigella species, confirmed by both biochemical and serological parameters, is the gold standard. 2.1.9 Suitable external QC programme Royal College of Pathologists of Australia Quality Assurance Programs Pty. Ltd. (RCPA) 2.1.10 Special considerations Based on DNA-DNA hybridization studies the genera Escherichia and Shigella are very
closely related are essentially the same genus. For practical and historical reasons both groups are still treated separately. It is essential therefore, before a final designation of Shigella is made the organism must conform to both recognised biochemical and serological parameters. Preferably, the isolate identity should be confirmed by a designated enteric reference laboratory. 2.1.11 References Ewing,W.H. 1986 Edwards and Ewing's Identification of Enterobacteriaceae. 4Th Edition, Elsevier Publishing Company, New York. Murray,P.R., Baron,E.J., Pfaller,M.A., Tenover,F.C. and Yolken,R.H. 1999. Manual of Clinical Microbiology, ASM Press, Washington, D.C.
2.2 Identification of Shigella species
There are two levels of Shigella identification A. Diagnostic laboratories - identify the Shigella using biochemical parameters and may perform preliminary serology. B. Reference laboratories - both the state and Australian reference laboratories. 2.2.1 Conventional biochemical tests 2.2.1.1 Suitable specimen A pure culture on solid medium. 2.2.1.2 Media Various specific biochemical substrates 2.2.1.3 Test sensitivity Depends on the biochemical tests performed. "Any strain that blackens triple sugar iron, is urease positive, or is able to grow on Simmons' citrate or decarboxylates lysine, produces phenylpyruvic acid from phenylalanine, or is motile does not belong to the genus Shigella" (Ewing, 1986). Christensen's citrate sodium acetate and sodium mucate media are of considerable value in the differentiation of Shigella from Escherichia (Ewing, 1986). (Particularly from anaerogenic E.coli) 2.2.1.4 Test specificity Of 139 isolates submitted to an enteric laboratory as "probable Shigella species" eleven (7.9%) were not confirmed as a Shigella species (MDU unpublished data). Not all shigellae exhibit the same biochemical properties. The notable exception is Sh.sonnei which is the only Shigella serotype to ferment lactose. A few particular types produce gas in mannitol. 2.2.1.5 Predictive values A negative culture does not preclude a diagnosis of shigellosis.
2.2.1.6 Suitable test criteria An isolate which exhibits biochemical characteristics consistent with documented reactions for Shigella species. 2.2.1.7 Suitable internal controls Each batch of biochemical substrate tested with positive and negative control strains. Results of all testing recorded and the records maintained. 2.2.1.8 Suitable validation criteria Correct biochemical reactions exhibited by a standard Shigella strain. 2.2.1.9 Suitable external QC program RCPA Quality Assurance Programs Pty. Ltd. 2.2.1.10 Special consideration As indicated in 2.2.1.4 biochemical variants of shigellae occur. Even if an isolate is not biochemically typical of Shigella, serology may be performed on suspicious isolates. The major biochemical problem is the differentiation of Shigella from inactive or atypical E.coli. An isolate which biochemically resembles a Shigella must be confirmed by serotyping. 2.2.1.11 References Ewing,W.H. 1986. Edwards and Ewing's Identification of Enterobacteriaceae. 4th Edition, Elsevier Publishing Company, New York. 2.2.2 Kits/automated systems for biochemical identification Various kits and automated machines exist for the identification of Enterobacteriaceae Of the numerous kits available in Australia Microbact (Medvet Science Pty. Ltd., Adelaide, Australia, Micro - Id (Organon Teknika N.V. Belgium) and API would be the most commonly used. MicroScan (Baxter, Baxter Healthcare Corporation, West Sacramento, USA), Vitek (bioMerieux, Marcy- l'Etoile, France), MicroStation (Biolog, Heyward, USA) and Cobas (Becton Dickinson Instrument Systems, Sparks, USA) are the major systems. The information stated in sections 2.2.1.1 - 2.2.1.9 also applies to both kits and automated identification systems. 2.2.2.10 Special considerations For accurate results it is imperative to follow the manufactures procedure exactly. 2.2.3 Latex agglutination kit
A latex agglutination kit has been described for screening for shigellae from selenite enrichment broth (Wellcolex Color Shigella; Murex Diagnostics, Inc., Norcross, GA.) . This can also be used to screen individual colonies from primary plates. Suspect colonies may be inoculated into media to biochemically identify Shigella. This technique only identifies Shigella serological groups; it does not give a complete serological identification. NB Isolates must be sent to a designated reference centre for complete serological identification. "A preliminary report of suspect Shigella infection may be issued if biochemical or serologic screening tests are positive "(Murray et. al., 1999) 2.2.4 Molecular identification Probes for Shigella have been developed for the detection and identification of shigellae, however, to date they are not used routinely in clinical laboratories.
2.3 Serological identification of Shigella species
2.3.1 Suitable specimen Pure bacterial culture. 2.3.2 Materials Verified polyvalent and monovalent somatic Shigella antisera. Many enteric (salmonella) reference laboratories raise their own antisera in rabbits. Prior to use each serum is titred for the specific antigen and for cross reactions to any other Shigella antigens. It is imperative to do this on all sera used in the reference section. All testing/titres must be fully documented. The production of Shigella antisera is more complex compared to the production of Salmonella antisera. Commercial antisera are available, but it is recognised that not all brands of antisera are reliable. For reference laboratories, which test large numbers of isolates, commercial antisera are expensive and not as useful because of cross-reactions and lack of information about the antigen titres. 2.3.3 Test sensitivity Unless an isolate is rough, most Shigella isolates will serotype. 2.3.4 Test specificity No data available. 2.3.5 Predictive values Failure to completely serotype a strain does not mean it cannot be serotyped. Using a different batch of antisera, using a younger subculture or another isolate from the patient may achieve serotyping of the Shigella infecting the patient. Occasionally a culture will not give a satisfactory serotype. This may indicate that the culture is mixed. 2.3.6 Suitable test acceptance criteria
Agglutination, to the specified titre, with specific Shigella antisera. 2.3.7 Suitable internal controls Regular serotyping of a Shigella type strain. 2.3.8 Suitable validation criteria Unequivocal demonstration of a recognised serotype. 2.3.9 Suitable External QC program None 2.3.10 Special considerations Because members of the genus Enterobacteriaceae are closely related there is antigenic cross over. Therefore it is imperative that been confirmed biochemically as a Shigella and only properly quality controlled antisera is used for serotyping. Very occassionally an isolate will be biochemically indistinguishable from Shigella species but no agglutination with the standard antisera is observed. This isolate may represent a new serotype. The isolate must be sent to the WHO designated Shigella Reference Centre at CDC, Atlanta, USA. for verification. 2.3.11 References Ewing,W.H. 1986 Edwards and Ewing's Identification of Enterobacteriaceae. 4th Edition Elsevier Publishing Company, New York.
2.4 Further subtyping
Biotyping and colicin typing (particularly for Sh.sonnei), plasmid profiling and various other molecular typing techniques may be used for the subtyping of shigellae, however to date they are not in use routinely.
2.5 Rapid methods
Commercial rapid diagnostic tests have been developed, but currently these techniques are not being used in the clinical diagnostic laboratories.
2.6 Serodiagnosis
"Several groups have developed serodiagnostic assays based on several antigens possessed by Shigella. These assays are practical only in research settings for seroepidemiology surveys and are not currently used for the diagnosis of infection in individual patients who are acutely ill" (Murray et .al., 1999).
3. PHLN laboratory definition
3.1 Condition Shigellosis 3.1.1 Tests Definitive Criteria: Isolation of a Shigella species.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
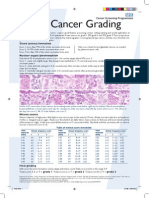
- Breast Cancer Grading PDFDocument1 pageBreast Cancer Grading PDFDrashua AshuaNo ratings yet
- ABO in The Context ofDocument21 pagesABO in The Context ofDrashua AshuaNo ratings yet
- Keys CardiologyDocument1 pageKeys CardiologyDrashua AshuaNo ratings yet
- DM CardiologyDocument39 pagesDM CardiologyDrashua AshuaNo ratings yet
- Application PDFDocument2 pagesApplication PDFDrashua AshuaNo ratings yet
- Bio Medical Rules PDFDocument28 pagesBio Medical Rules PDFDrashua AshuaNo ratings yet
- Post Graduate Medical Admission Test (Pgmat) - 2014 For MD/MS/PGD, MDS & MD (Ayurveda)Document1 pagePost Graduate Medical Admission Test (Pgmat) - 2014 For MD/MS/PGD, MDS & MD (Ayurveda)Drashua AshuaNo ratings yet
- Bence Jones Protein-UrineDocument16 pagesBence Jones Protein-UrineDrashua Ashua100% (2)
- Post Graduate Medical Admission Test (Pgmat) - 2015 For MD/MS/PGD, MDS & MD (Ayurveda)Document2 pagesPost Graduate Medical Admission Test (Pgmat) - 2015 For MD/MS/PGD, MDS & MD (Ayurveda)Drashua AshuaNo ratings yet
- Bihar PG15 ProspectusDocument37 pagesBihar PG15 ProspectusDrashua AshuaNo ratings yet
- Telephone Directory EngDocument8 pagesTelephone Directory EngDrashua AshuaNo ratings yet
- Hilgendorf Bio 07Document52 pagesHilgendorf Bio 07Drashua AshuaNo ratings yet
- Post Graduate Medical Admission Test (Pgmat) - 2015 For MD/MS/PGD, MDS & MD (Ayurveda)Document2 pagesPost Graduate Medical Admission Test (Pgmat) - 2015 For MD/MS/PGD, MDS & MD (Ayurveda)Drashua AshuaNo ratings yet
- Compliance rate study of bio-medical waste segregationDocument50 pagesCompliance rate study of bio-medical waste segregationAman Dheer Kapoor100% (2)
- CBD FullDocument5 pagesCBD FullDrashua AshuaNo ratings yet
- Muscle Origins and InsertionsDocument9 pagesMuscle Origins and Insertionsnoisytaost92% (12)
- Shigella in Child-Care SettingsDocument2 pagesShigella in Child-Care SettingsDrashua AshuaNo ratings yet
- SHIGELLOSISDocument1 pageSHIGELLOSISDrashua AshuaNo ratings yet
- Ecp Shigella InfectionDocument4 pagesEcp Shigella InfectionDrashua AshuaNo ratings yet
- ID 20i2.1Document12 pagesID 20i2.1Drashua AshuaNo ratings yet
- HematologyDocument58 pagesHematologyAchmad DainuriNo ratings yet
- Shigella BackgroundDocument2 pagesShigella BackgroundDrashua AshuaNo ratings yet
- P 133-1430Document11 pagesP 133-1430Drashua AshuaNo ratings yet
- P 133-1430Document11 pagesP 133-1430Drashua AshuaNo ratings yet
- 420 079 Guideline ShigellosisDocument7 pages420 079 Guideline ShigellosisDrashua AshuaNo ratings yet
- Shigellosis: Frequently Asked QuestionsDocument2 pagesShigellosis: Frequently Asked QuestionsDrashua AshuaNo ratings yet
- ShigellaDocument1 pageShigellaDrashua AshuaNo ratings yet
- ShigellaDocument2 pagesShigellaDrashua AshuaNo ratings yet
- 0314Document6 pages0314Drashua AshuaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Depression and Anxiety Among College StudentsDocument2 pagesDepression and Anxiety Among College StudentsAnonymous 5WUUQijWNo ratings yet
- Burkitt's Lymphoma: A Guide to Diagnosis and TreatmentDocument51 pagesBurkitt's Lymphoma: A Guide to Diagnosis and TreatmentDee100% (2)
- 3 MBBS Part I Routine (Theory) Department of Pediatrics Total: 20 Duration: 1hrDocument12 pages3 MBBS Part I Routine (Theory) Department of Pediatrics Total: 20 Duration: 1hrGaurav BatniNo ratings yet
- PE1 ReviewerDocument4 pagesPE1 ReviewerZoe BeatrizNo ratings yet
- Abdominal Wall HerniaDocument100 pagesAbdominal Wall Herniaintandiahningrum100% (1)
- Nursing Care Plan for Hiatal Hernia ReliefDocument3 pagesNursing Care Plan for Hiatal Hernia ReliefLalaine Nadulpit100% (2)
- Cicatricial Atelectasis - Print Friendly - STATdxDocument2 pagesCicatricial Atelectasis - Print Friendly - STATdxmihaelaNo ratings yet
- A Laser Peripheral Iridotomy Would Most Likely Relieve AngleDocument2 pagesA Laser Peripheral Iridotomy Would Most Likely Relieve AngleGlaucoma UnhasNo ratings yet
- Oral Manifestations of Thyroid Disorders and Its MDocument4 pagesOral Manifestations of Thyroid Disorders and Its MNike WijayaNo ratings yet
- NCP AidsDocument16 pagesNCP AidstferdianingsihNo ratings yet
- Celluar and Neural Regulation StudentDocument52 pagesCelluar and Neural Regulation StudentCruz YrNo ratings yet
- Blood TransfusionDocument2 pagesBlood TransfusionKomal TomarNo ratings yet
- Obg MCQSDocument11 pagesObg MCQSShriyansh ChaharNo ratings yet
- Three Cases of Chronic Suppurative Otitis Media (CSOM) Caused by Kerstersia Gyiorum and A Review of The LiteratureDocument6 pagesThree Cases of Chronic Suppurative Otitis Media (CSOM) Caused by Kerstersia Gyiorum and A Review of The LiteraturealdaNo ratings yet
- Kanker ServiksDocument17 pagesKanker Serviksvenia endah tamaraNo ratings yet
- Acute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFDocument9 pagesAcute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFSai Khin Aung TintNo ratings yet
- ModuleIV RespiratoryEmergencies CHF COPD AsthmaDocument96 pagesModuleIV RespiratoryEmergencies CHF COPD AsthmaSaiKiranNo ratings yet
- Perioperative Fluid Management in ChildrenDocument31 pagesPerioperative Fluid Management in ChildrenRashmi SahaNo ratings yet
- Adenosine Therapy for Supraventricular TachycardiaDocument17 pagesAdenosine Therapy for Supraventricular TachycardiaKirsten Padilla Chua0% (1)
- Globemed FormDocument4 pagesGlobemed Formangeloriondo1217No ratings yet
- Ayurvedic Diabetes CureDocument13 pagesAyurvedic Diabetes CureYassine KrineNo ratings yet
- Evolve Resources For Goulds Pathophysiology For The Health Professions 6th Edition Hubert Test BankDocument9 pagesEvolve Resources For Goulds Pathophysiology For The Health Professions 6th Edition Hubert Test Bankhungden8pne100% (26)
- Nursing Care Plan Colorectal CancerDocument2 pagesNursing Care Plan Colorectal Cancerderic88% (34)
- Gastroenterology - Lower GI Bleeding - SOAP Note - Maitreyi RamanDocument4 pagesGastroenterology - Lower GI Bleeding - SOAP Note - Maitreyi RamanFrancieudo Sampaio100% (1)
- Asking-Filling in Medical ReportDocument5 pagesAsking-Filling in Medical ReportMiss Hanay VinnyNo ratings yet
- Akapulko or Acapulco in English Is A Shrub Found Throughout The PhilippinesDocument6 pagesAkapulko or Acapulco in English Is A Shrub Found Throughout The PhilippinesJon Adam Bermudez SamatraNo ratings yet
- Hematology Topics Objectives References: Our Lady of Fatima University Department of Internal MedicineDocument7 pagesHematology Topics Objectives References: Our Lady of Fatima University Department of Internal MedicineAlmar NuñezNo ratings yet
- Tay-Sachs Disease I. What Is Tay-Sachs Disease?Document2 pagesTay-Sachs Disease I. What Is Tay-Sachs Disease?DBA MurialdoNo ratings yet
- Activity IntoleranceDocument4 pagesActivity IntoleranceDianne MacaraigNo ratings yet
- Multiple Organ Failure As A Cause of DeaDocument6 pagesMultiple Organ Failure As A Cause of DeaEliza DiaconescuNo ratings yet