Professional Documents
Culture Documents
Teaching Plan On Wound Care
Uploaded by
Franco ObedozaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Teaching Plan On Wound Care
Uploaded by
Franco ObedozaCopyright:
Available Formats
LEARNING CONTENT ON WOUND CARE WOUND CARE Wound care is the process in which preventing wound complications are
e being done. It involves the assessment and cleaning the wound. Wound care is done in every wound to prevent infection and other complications. DIFFERENT COMPLICATIONS
B. Fever: It is often accompanied by feeling chilled. This fever may because of the inflammatory process and due to toxins that the microorganism produced.
C. Hot Incision: This happens as the body sends infection fighting blood cells to the site of infection. Some of these may be leukocytes, histamines and others.
D. Swelling/Hardening of the Incision: infected incision may begin to harden as the 1. INFECTION main causes of post-operative morbidity in abdominal surgery most common form is superficial wound infection occurring within the first week presenting as localized pain, redness and slight discharge usually caused by skin staphylococci (Staphylococcus arues) Wound infection results from microbes flourishing in the surgical site because of poor preoperative preparation, wound contamination, poor antibiotic selection, or the inability of an immunocompromised patient to fight off infection. F. Drainage From the Incision: Foul-smelling drainage or pus may begin to appear on an infected incision. It can range in color from blood-tinged to green, white or yellow. The drainage from an infected wound may also be thick, and in rare cases, WHAT ARE THE SIGNS AND SYMPTOMS OF INFECTION chunky. E. Redness: An incision that gets red, or has red streaks radiating from it to the surrounding skin may be infected. Some redness is normal at the incision site, but it should decrease over time, rather than becoming more red as the incision heals. tissue underneath are inflamed. The incision itself may begin to appear swollen or puffy as well.
A. Malaise: One of the most common symptoms of a systemic infection, or an infection that is moving through your body. Patient may feel generalized body weakness. Feeling to be tired easily even without exerting effort.
G. Pain: the pain should slowly and steadily diminish as you heal. If pain level at the surgery site increases for no apparent reason, it may be developing an infection in the wound. It is normal for increased pain if increase with activity or decrease with pain medication, but a significant and unexplained increase in pain should be discussed with the surgeon
Fully soaked dressing THINGS TO DO: 1) Report immediately to the physician 2) Comply to antibiotic regimen strictly, Right dose and Right time 3) Do not expose further the wound Pallor Delayed capillary refill Rapid respiratory rate Rapid pulse rate Confusion Restlessness PREVENTION OF WOUND INFECTION a) Comply to antibiotic regimen strictly b) Do not rub, scratch, of play the wound c) Do not put lotion and powder unto the wound d) Clean the wound from inner to outer e) Do not let the dressing to be soiled PREVENTION 2. BLEEDING/HEMMORHAGE Severe bleeding from a wound can be life-threatening, depending on the amount of blood loss, how difficult the bleeding is to control, how long the bleeding goes unchecked and other injuries that may be present. The term hemorrhage refers specifically to blood being lost at a rapid rate. 1. For the first day or two, do not move the affected area too much in order to avoid causing bleeding. The pressure of the bandage should help to prevent bleeding. 2. A small amount of blood on the dressing is normal. If bleeding seems persistent, apply pressure firmly and steadily over the dressing for 10 to 15 minutes. This will usually stop the bleeding but if it does not, call the doctor promptly. 3. Dot expose directly to sunlight 4. do not take a bath under hot water 5. do not rub, scrub, and remove clots SIGNS AND SYMPTOMS Low urine output 3. WOUND DEHISENCE THING TO DO IF THIS HAPPENS a) Apply pressure directly on the wound b) Use clean clothe to cover if possible c) Seek medical attention immediately
Dehiscence is a surgical complication where the edges of a wound no longer meet. It is also known as wound separation.
come out of the incision (evisceration). Evisceration is an emergency and should be treated as such.
Affects about 2% of mid-line laparotomy wounds. Serious complication with a mortality of up to 30%. Due to failure of wound closure technique. Usually occurs between 7 and 10 days post-operatively. Often heralded by serosanguinous discharge from wound. Should be assumed that the defect involves the whole of the wound. I. II. WHAT TO DO IF THIS HAPPENS: Call an emergency response team or bring patient tonearest hospital Cover the opening and organs with the cleanest sheet or bandage material you have, after wetting it thoroughly. If you have been bandaging your wound, you should have the supplies to cover the tissue with sterile bandages. The fabric/bandage needs to be moist, to prevent it from adhering to tissue. If you have sterile saline, use it to saturate the bandage or towel. If not, bottled or tap water can be used.
sudden increase in abdominal pressure, due to coughing, sneezing, vomiting, bearing down to have a bowel movement or lifting a heavy object, causes an abdominal wound to open it may also caused by infection
UNDER NO CIRCUMSTANCES should you attempt to push the organs back Symptoms of post operative wound dehiscence include: Failure of the staples or stitches Separation of the wound edges Wound swelling Fluid draining from the wound Tissue protruding from the wound How to Prevent Dehiscence and Evisceration: 4. WOUND EVISCERATION Evisceration is a rare but severe surgical complication where the surgical incision opens (dehiscence) and the abdominal organs then protrude or Bracing - When doing any activity that increases abdominal pressure (sneezing, coughing, vomiting, laughing, bearing down for a bowel movement) hold pressure over your incision using your hands or a pillow. This can both prevent dehiscence and minimize pain during activity. in to the abdominal cavity. If the worst case scenario has happened and loops of intestine have pushed out of the incision, gather them in the wet sheet or bandage and keep the patient calm and seated or lying down.
Prevent Constipation - Constipation is common after surgery, and straining to have a bowel movement puts unnecessary stress on your incision. Prevent constipation with proper nutrition after surgery, or if you are already constipated, ask your surgeon for medication to help. Proper Incision Care - Proper incision care will not only speed healing, but it helps prevent infection, which can weaken the incision and increase the chances of dehiscence. Prevent coughing and sneezing - If youve had surgery and your allergies are acting up or you have a cough, be proactive about keeping sneezing and coughing to a minimum. Repetitive coughing and sneezing can slowly weaken your incision, which can slow healing and (in some cases) lead to dehiscence. Avoid Lifting If your doctor says you are not allowed to lift anything heavier than 5 pounds for 2 weeks after surgery, he isnt kidding. Lifting objects can place stress on your incision that can cause it to open.
http://www.patient.co.uk/doctor/common-post-operative-complications http://surgery.about.com/od/aftersurgery/ss/DehiscenceEvisc_5.htm http://surgery.about.com/od/aftersurgery/ss/DehiscenceEvisc_4.htm
http://surgery.about.com/od/aftersurgery/qt/SignsInfections.htm http://www.mdguidelines.com/wound-infection-postoperative
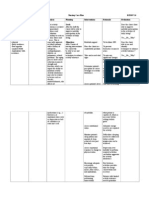
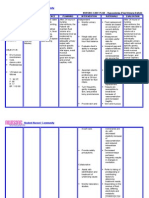
TEACHING PLAN ON WOUND COMPLICATION AND MANAGEMENT I. DESCRIPTION OF THE LEARNER: He is a 30 year old, male, and a resident of Ucab, Itogon, Benguet. He is an elementary graduate and able to read, speak, write and understand English, Tagalog, Ilocano, Kankanaey, and Ibaloi. He is a Roman catholic and a father of my patient who undergone Emergency exploratory laparotomy. It was his first time to have a child with exploratory laparotomy or and surgery. II. LEARNING NEED: Wound complication and management III. LEANING DIAGNOSIS: Readiness for enhance knowledge: wound care related to lack of exposure IV. TIME ALLOTMENT: 20 minutes V. LEANING PLAN BLOS LEARNING CONTENT TEACHING STRATEGY AND MATERIALS NEEDED After teaching the father of client on wound care, he will able to 1. Define wound care properly using his own words Definition wound care One-on-one teaching Picture analysis -pamphlet Instant oral feedback: ask the client to define wound care properly using his own words EVALUATION CRITERIA
2.
State at least 3 out of 4 surgical wound complication correctly
Wound complications
One-on-one teaching -pamphlet
Instant oral feedback: ask the client to state at least 3 out of 4 surgical wound complication correctly
3. Define each wound complications included in
Definition of each wound complications
One-on-one teaching -pamphlet
Instant oral feedback: ask the client to define each wound complications included in the discussion using his own words
the discussion using his own words correctly 4. Identify properly at least 2 signs and symptoms of each complications 5. Enumerate correctly at least 2 preventions of each complications 6. State at least 2 things to do if the wound complications happens correctly Things to do if wound complications happens Preventions of each complications One-on-one teaching pamphlet One-on-one teaching pamphlet Signs and symptoms of each complications One-on-one teaching Pamphlet
correctly
Instant oral feedback: ask the client identify properly at least 2 signs and symptoms of each complications
Instant oral feedback: ask the client to enumerate correctly at least 2 preventions of each complications Instant oral feedback: ask the client to state at least 2 things to do if the wound complications happens correctly
You might also like
- Case Solutions For Personality Theories Workbook 6th Edition by AshcraftDocument7 pagesCase Solutions For Personality Theories Workbook 6th Edition by AshcraftMonikaNo ratings yet
- Delayed Surgical Recovery Nursing Care PlanDocument3 pagesDelayed Surgical Recovery Nursing Care PlanMichala100% (3)
- Teaching Plan Wound CareDocument3 pagesTeaching Plan Wound CareAdrian Savastita82% (11)
- NCP LymphedemaDocument1 pageNCP Lymphedemayasira50% (2)
- Nursing Diagnosis of Prostate CancerDocument3 pagesNursing Diagnosis of Prostate CancerSyafiqAzizi100% (1)
- 8 Sample Care Plans For ACDFDocument11 pages8 Sample Care Plans For ACDFacasulla98No ratings yet
- Health Teaching Plan - Wound Care and DressingDocument6 pagesHealth Teaching Plan - Wound Care and Dressingp_dawg100% (2)
- Nursing Care Plans: Nursing Diagnosis and Assessment, Nursing Interventions GuideFrom EverandNursing Care Plans: Nursing Diagnosis and Assessment, Nursing Interventions GuideRating: 5 out of 5 stars5/5 (4)
- Teaching Plan On Wound CareeeDocument2 pagesTeaching Plan On Wound Careeeaambroce100% (1)
- Infection Control - Teaching PlanDocument3 pagesInfection Control - Teaching Planアンナドミニク100% (4)
- Actual Nursing Care Plan 2Document16 pagesActual Nursing Care Plan 2Alyanna Evangelista100% (2)
- Teaching Plan On Wound CareDocument6 pagesTeaching Plan On Wound CareFranco Obedoza100% (1)
- CF27 Ad 01Document2 pagesCF27 Ad 01Eka NovigustinaNo ratings yet
- HESI Study Guide Psychiatric NursingDocument26 pagesHESI Study Guide Psychiatric NursingDean Winchester100% (4)
- Nursing Care Plan For CellulitisDocument6 pagesNursing Care Plan For CellulitisChander Kanta100% (3)
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionDiane ReyNo ratings yet
- NCP Imapired Skin IntegrityDocument5 pagesNCP Imapired Skin IntegrityAno BaItoNo ratings yet
- Nursing Diagnosis: AdvertisementsDocument7 pagesNursing Diagnosis: AdvertisementsJamea TumbagaNo ratings yet
- NCP - Fluid Volume DeficitDocument2 pagesNCP - Fluid Volume DeficitPatrice LimNo ratings yet
- Copd Case StudyDocument5 pagesCopd Case StudyJake Yvan DizonNo ratings yet
- CHN NCPDocument2 pagesCHN NCPIna Marie Calungcaguin Castro100% (1)
- 3 Intraoperative PhaseDocument28 pages3 Intraoperative Phaseada_beer100% (2)
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegritySharewin PulidoNo ratings yet
- NCPDocument4 pagesNCPAndrea BroccoliNo ratings yet
- Module 13 - Cystoclysis (Student)Document4 pagesModule 13 - Cystoclysis (Student)Raymond Edge100% (2)
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- Cues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalDocument4 pagesCues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalKei Cruz100% (1)
- NCP Impaired Skin IntegrityDocument2 pagesNCP Impaired Skin IntegrityAshley Kate SantosNo ratings yet
- Skin Grafting Surgical NursingDocument21 pagesSkin Grafting Surgical NursingHEMMA100% (1)
- Impaired Physical Mobility...Document3 pagesImpaired Physical Mobility...Christy BerryNo ratings yet
- Breast Cancer Risk For InfectionDocument6 pagesBreast Cancer Risk For Infectionam peNo ratings yet
- Bladder Irrigation (Cystoclysis)Document4 pagesBladder Irrigation (Cystoclysis)CJ Angeles100% (2)
- Risk For InfectionDocument5 pagesRisk For InfectionRochelle Corneta JoreNo ratings yet
- Acute Biologic Crisis-ArDocument71 pagesAcute Biologic Crisis-ArJayvee Novenario CasaljayNo ratings yet
- Lung Cancer (Nursing Care)Document5 pagesLung Cancer (Nursing Care)heiyuNo ratings yet
- DM Health Teaching PlanDocument5 pagesDM Health Teaching PlancamilatanNo ratings yet
- Nursing DiagnosisDocument10 pagesNursing DiagnosisZaty ChaiyOkk100% (1)
- Nursing Care Plan GuideDocument4 pagesNursing Care Plan Guidemarie99% (134)
- Nursing Care Plan For "DYSRHYTHMIAS"Document12 pagesNursing Care Plan For "DYSRHYTHMIAS"jhonroks79% (14)
- FILARIASISDocument2 pagesFILARIASIShaoc0425No ratings yet
- Cues Problem Physiologic Behavioral: Nutrition: Less Than Body Requirements Acute Pain Altered ADLDocument3 pagesCues Problem Physiologic Behavioral: Nutrition: Less Than Body Requirements Acute Pain Altered ADLAya BolinasNo ratings yet
- Wound Care Teaching Plan Sample PDFDocument1 pageWound Care Teaching Plan Sample PDFcatislandbigredNo ratings yet
- Discharge Plan For Dengue Fever 1Document4 pagesDischarge Plan For Dengue Fever 1Cecille Ursua0% (1)
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityBesael BaccolNo ratings yet
- Deficit)Document2 pagesDeficit)Lee DeeNo ratings yet
- Icu NCPDocument4 pagesIcu NCPdrsabuegNo ratings yet
- How To Prevent Evisceration:: Bracing - When Doing Any Activity That Increases Abdominal Pressure (Sneezing, CoughingDocument5 pagesHow To Prevent Evisceration:: Bracing - When Doing Any Activity That Increases Abdominal Pressure (Sneezing, Coughingcyrilcarinan100% (1)
- PE1Document23 pagesPE1abbynoreen2No ratings yet
- Instructionsheet Abscessundertheskinid512 PDFDocument1 pageInstructionsheet Abscessundertheskinid512 PDFNik UrlaubNo ratings yet
- Infected WoundDocument23 pagesInfected WoundMohamed FarahatNo ratings yet
- Incision & Drainage of Abscess Group 9 4bDocument5 pagesIncision & Drainage of Abscess Group 9 4bGUDISELA ramyaNo ratings yet
- How Is A Wound Infection Treated?Document5 pagesHow Is A Wound Infection Treated?Haider JulailiNo ratings yet
- How Is A Wound Infection Treated?Document5 pagesHow Is A Wound Infection Treated?Haider JulailiNo ratings yet
- CD DressingDocument11 pagesCD DressingPATEL NEHAKUMARI VIMALBHAINo ratings yet
- First AidDocument10 pagesFirst AidavielavenderNo ratings yet
- Basics of Wound Care: TH e HELP Guide ToDocument16 pagesBasics of Wound Care: TH e HELP Guide TomatentenNo ratings yet
- Appendicitis&AppendectomyDocument5 pagesAppendicitis&AppendectomyJestine Joy CustodioNo ratings yet
- Wound InfectionDocument2 pagesWound InfectionMary Anjeanette Ramos VardeleonNo ratings yet
- Case Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara SabriDocument19 pagesCase Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara Sabrifarzaneh yeganehNo ratings yet
- Abscess Case Pre FinalDocument41 pagesAbscess Case Pre FinalDavid DueñasNo ratings yet
- Pilonidal Sinus: Information For PatientsDocument12 pagesPilonidal Sinus: Information For PatientsAliyah Tofani PawelloiNo ratings yet
- MergeResult 2023 11 05 02 20 37Document232 pagesMergeResult 2023 11 05 02 20 37Russel John MunarNo ratings yet
- Wound Case Study AssessmentDocument7 pagesWound Case Study Assessmentcass1526100% (2)
- First AidDocument13 pagesFirst AidJasier Sahagun0% (1)
- Drug StudyDocument10 pagesDrug StudyFranco ObedozaNo ratings yet
- National Telehealth CenterDocument5 pagesNational Telehealth CenterFranco ObedozaNo ratings yet
- Teaching Plan On CoughDocument3 pagesTeaching Plan On CoughFranco Obedoza67% (3)
- Teaching Plan On CoughDocument3 pagesTeaching Plan On CoughFranco Obedoza67% (3)
- OBEDOZA, Franco Obedoza II CDocument1 pageOBEDOZA, Franco Obedoza II CFranco ObedozaNo ratings yet
- Teaching PlanDocument8 pagesTeaching PlanFranco Obedoza100% (1)
- Teaching Plan Breast Feeding 270Document8 pagesTeaching Plan Breast Feeding 270Franco ObedozaNo ratings yet
- Rao 2017Document5 pagesRao 2017drzana78No ratings yet
- Bracket PositionDocument10 pagesBracket PositionBarsha ThapaNo ratings yet
- Renal Trauma by Mohammad Shaar, M.D.Document42 pagesRenal Trauma by Mohammad Shaar, M.D.atef shaar100% (1)
- David BurnsDocument2 pagesDavid Burnspsic7loga7martos100% (1)
- The Counselling Process and Attributes of An Effective CounsellorDocument17 pagesThe Counselling Process and Attributes of An Effective CounsellorKeishailla MenonNo ratings yet
- IABPDocument88 pagesIABPNavojit Chowdhury100% (1)
- Foundations of QigongDocument7 pagesFoundations of QigongAudrygodwynNo ratings yet
- EVM500019 Inspiration I Series Service Manual Rev E PDFDocument200 pagesEVM500019 Inspiration I Series Service Manual Rev E PDFMIGUEL ANGEL75% (4)
- When People Are Dying: Palliative CareDocument17 pagesWhen People Are Dying: Palliative Carenerlyn100% (1)
- NCP Acute PainDocument3 pagesNCP Acute PainAngel HernandezNo ratings yet
- CoNcept of CounsellingDocument14 pagesCoNcept of CounsellingKool KattyNo ratings yet
- Adhd New ContentDocument9 pagesAdhd New ContentAsha jiluNo ratings yet
- HypoglicemiaDocument4 pagesHypoglicemiayeniNo ratings yet
- Kalkstein Dissertation2005Document76 pagesKalkstein Dissertation2005Petruța MarianNo ratings yet
- Training Program: By: Rahul AhujaDocument17 pagesTraining Program: By: Rahul Ahujakei HoinaNo ratings yet
- Playful Integration - Resource List On Gender Expansive Kids in The PlayroomDocument3 pagesPlayful Integration - Resource List On Gender Expansive Kids in The PlayroomSana UmarNo ratings yet
- How Did I As A Student Music Therapist, Use Songwriting Techniques To Facilitate Self-Expression With Adolescents in A Mental Health School Setting?Document63 pagesHow Did I As A Student Music Therapist, Use Songwriting Techniques To Facilitate Self-Expression With Adolescents in A Mental Health School Setting?Earh AngelNo ratings yet
- Microincision Cataract SurgeryDocument20 pagesMicroincision Cataract SurgeryviticodocNo ratings yet
- Three Years of H CL TherapyDocument50 pagesThree Years of H CL TherapyVíctor ValdezNo ratings yet
- PsmsformsDocument1 pagePsmsformsapi-261670650No ratings yet
- Document-Dikonversi Sms Dan EmsDocument4 pagesDocument-Dikonversi Sms Dan EmsAORI BEAUTY OFFICIALNo ratings yet
- Retinal DetachmentDocument21 pagesRetinal Detachmentณัช เกษมNo ratings yet
- Soul Link PDFDocument8 pagesSoul Link PDFCr HtNo ratings yet
- Professional Quality of Life ScaleDocument2 pagesProfessional Quality of Life ScaleCyntia PopaNo ratings yet
- Drug KenalogDocument1 pageDrug KenalogSrkocherNo ratings yet
- Non Steroidal Anti Inflammatory DrugDocument21 pagesNon Steroidal Anti Inflammatory DrugRanganath NagarajNo ratings yet