Professional Documents
Culture Documents
What Is Dysautonomia
Uploaded by
jo_jo_maniaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
What Is Dysautonomia
Uploaded by
jo_jo_maniaCopyright:
Available Formats
What is Dysautonomia? Dysautonomia refers to a disorder of autonomic nervous system (ANS) function.
Most physicians view dysautonomia in terms of failure of the sympathetic or parasympathetic components of the ANS, but dysautonomia involving excessive ANS activities also can occur. Dysautonomia can be local, as in reflex sympathetic dystrophy, or generalized, as in pure autonomic failure. It can be acute and reversible, as in Guillain-Barre syndrome, or chronic and progressive. Several common conditions such as diabetes and alcoholism can include dysautonomia. Dysautonomia also can occur as a primary condition or in association with degenerative neurological diseases such as Parkinson's disease. Other diseases with generalized, primary dysautonomia include multiple system atrophy and familial dysautonomia. Hallmarks of generalized dysautonomia due to sympathetic failure are impotence (in men) and a fall in blood pressure during standing (orthostatic hypotension). Excessive sympathetic activity can present as hypertension or a rapid pulse rate. Is there any treatment? There is no cure for dysautonomia. Secondary forms may improve with treatment of the underlying disease. In many cases treatment of primary dysautonomia is symptomatic and supportive. Measures to combat orthostatic hypotension include elevation of the head of the bed, frequent small meals, a high-salt diet, and drugs such as fludrocortisone, midodrine, and ephedrine. What is Holmes-Adie syndrome ? Holmes-Adie syndrome (HAS) is a neurological disorder affecting the pupil of the eye and the autonomic nervous system. It is characterized by one eye with a pupil that is larger than normal and constricts slowly in bright light (tonic pupil), along with the absence of deep tendon reflexes, usually in the Achilles tendon. HAS is thought to be the result of a viral or bacterial infection that causes inflammation and damage to neurons in the ciliary ganglion, an area of the brain that controls eye movements, and the spinal ganglion, an area of the brain involved in the response of the autonomic nervous system. HAS begins gradually in one eye, and often progresses to involve the other eye. At first, it may only cause the loss of deep tendon reflexes on one side of the body, but then progress to the other side. The eye and reflex symptoms may not appear at the same time. People with HAS may also sweat excessively, sometimes only on one side of the body. The combination of these 3 symptoms abnormal pupil size, loss of deep tendon reflexes, and excessive sweating is usually called Rosss syndrome, although some doctors will still diagnosis the condition as a variant of HAS. Some individuals will also have cardiovascular abnormalities. The HAS symptoms can appear on their own, or in association with other diseases of the nervous system, such as Sjogrens syndrome or migraine. It is most often seen in young women. It is rarely an inherited condition.
Is there any treatment? Doctors may prescribe reading glasses to compensate for impaired vision in the affected eye, and pilocarpine drops to be applied 3 times daily to constrict the dilated pupil. Thoracic sympathectomy, which severs the involved sympathetic nerve, is the definitive treatment for excessive sweating. Babinski's sign I A pathological reflex where the great toe extends and flexes toward the top of the foot and the other toes fan out when the sole of the foot is firmly stroked. Normally, the great toe is flexed when the sole of the relaxed foot is stroked. Babinskis reflex is normal in children up to about two years of age. The persistence in older people is a sign of damage to the corticospinal tract. Because this tract is right- and left-sided, a Babinskis reflex can occur on one side or on both sides. An abnormal Babinskis reflex can be temporary or permanent. The test for Babinskis sign, called Babinskis test, is running a pointed instrument up the lateral border of the foot and crossing to the medial side over the metatarsal pads. The term Babinskis sign also refers to a reflex of the forearm and indicates a lesion of the spinal cord. Flix Alfred Vulpian, neuropathologist at the Hpital de Salptrire in Paris, half a century before Babinski had observed the extension of the great toe in certain types of brain damage. The sign had also been reported three years before by Ernst Julius Remak (1849-1911), but it was Babinski who first realized its diagnostic significance. In 1896, at a meeting of the Socit de Biologie, Babinski first reported his discovery that while the normal reflex of the sole of the foot consists of a plantar reflex of the toes; an injury to the pyramidal tract will show up in an isolated dorsal flexion of the great toe. In 1903 he completed his report with another article containing a description of the fanning of the other toes.
You might also like
- Donordarah PDFDocument1 pageDonordarah PDFjo_jo_maniaNo ratings yet
- Efficacy and Safety of Tigecycline - A Systematic Review and Meta-AnalysisDocument8 pagesEfficacy and Safety of Tigecycline - A Systematic Review and Meta-Analysisjo_jo_maniaNo ratings yet
- Canadian Contraception ConsensusDocument14 pagesCanadian Contraception Consensusjo_jo_maniaNo ratings yet
- Case Report: Pulmonary Sequestration: A Case Report and Literature ReviewDocument4 pagesCase Report: Pulmonary Sequestration: A Case Report and Literature Reviewjo_jo_maniaNo ratings yet
- 111992518Document6 pages111992518jo_jo_maniaNo ratings yet
- Dystocia SOGCDocument16 pagesDystocia SOGCAdhitia NugrahantoNo ratings yet
- Bioethic MetaphysicDocument6 pagesBioethic Metaphysicjo_jo_maniaNo ratings yet
- ContentServer 37.ASPaaaaaDocument6 pagesContentServer 37.ASPaaaaaAchmad Deza FaristaNo ratings yet
- Donor DarahDocument1 pageDonor Darahjo_jo_maniaNo ratings yet
- Chlamydial Infection Can Cause Disease in Many Organ SystemsDocument22 pagesChlamydial Infection Can Cause Disease in Many Organ Systemsjo_jo_maniaNo ratings yet
- Case Studies Module 1 - A Case of PcosDocument9 pagesCase Studies Module 1 - A Case of PcosBobNo ratings yet
- Sunday, 26/09 /2010 PT/LN/MG:: Consultant DR Mas Putra SPMDocument6 pagesSunday, 26/09 /2010 PT/LN/MG:: Consultant DR Mas Putra SPMjo_jo_maniaNo ratings yet
- AnyelirDocument2 pagesAnyelirjo_jo_maniaNo ratings yet
- Structure Content: 1. EXERCISE 1 (Skill 1-2) 2. Toefl Review Exercise (Skill 1-2) 3. Answer KeysDocument3 pagesStructure Content: 1. EXERCISE 1 (Skill 1-2) 2. Toefl Review Exercise (Skill 1-2) 3. Answer Keysjo_jo_mania0% (1)
- IBT Q4 03 ReadingonlyDocument1 pageIBT Q4 03 Readingonlyjo_jo_maniaNo ratings yet
- HiResOligonucleoutide ACGH Analysis Under24Hrs AppNote5991-0643ENDocument8 pagesHiResOligonucleoutide ACGH Analysis Under24Hrs AppNote5991-0643ENjo_jo_maniaNo ratings yet
- Yg Belum Masuk IpadDocument1 pageYg Belum Masuk Ipadjo_jo_maniaNo ratings yet
- Induction of Labour Versus Expectant Monitoring ForDocument11 pagesInduction of Labour Versus Expectant Monitoring Forjo_jo_maniaNo ratings yet
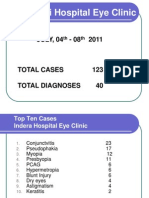
- BARUPoliklinik Wangaya 4-8 Juli 2011Document14 pagesBARUPoliklinik Wangaya 4-8 Juli 2011jo_jo_maniaNo ratings yet
- NEW Weekly Indra 04-08 July 2011Document13 pagesNEW Weekly Indra 04-08 July 2011jo_jo_maniaNo ratings yet
- International Centre For Eye Health Teaching Set 2 The Eye in Primary Health CareDocument25 pagesInternational Centre For Eye Health Teaching Set 2 The Eye in Primary Health Carejo_jo_maniaNo ratings yet
- TOEFL Speaking - Question 1&2 TopicsDocument8 pagesTOEFL Speaking - Question 1&2 TopicsSiddharthaSidNo ratings yet
- Cancer RiskDocument1 pageCancer Riskjo_jo_maniaNo ratings yet
- Prediction Reccurence Prostat CADocument9 pagesPrediction Reccurence Prostat CAjo_jo_maniaNo ratings yet
- OrtoDocument61 pagesOrtojo_jo_maniaNo ratings yet
- Arterial Blood Gas: DR - Made Widia, Sp.A (K)Document19 pagesArterial Blood Gas: DR - Made Widia, Sp.A (K)jo_jo_mania100% (1)
- Laser Iridotomy and GlaucomaDocument2 pagesLaser Iridotomy and Glaucomajo_jo_maniaNo ratings yet
- Migraine Prophylaxis: Pharmacotherapy PerspectivesDocument11 pagesMigraine Prophylaxis: Pharmacotherapy Perspectivesjo_jo_maniaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Corrode Four Horsemen Book 3 by SarahDocument323 pagesCorrode Four Horsemen Book 3 by SarahSaoirse ZherineNo ratings yet
- Daphne Goodsby - Before Another Tragedy Strikes-Address Bullying in Our SchoolsDocument4 pagesDaphne Goodsby - Before Another Tragedy Strikes-Address Bullying in Our Schoolsapi-327329006No ratings yet
- Lesson Plan: Learning OutcomesDocument4 pagesLesson Plan: Learning OutcomesJoshua AgucoyNo ratings yet
- Summary New Black Beauty Level 2Document23 pagesSummary New Black Beauty Level 2merinaNo ratings yet
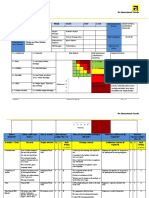
- Ergonomic Risk Identification and Assessment - Identification and Assessment ToolDocument54 pagesErgonomic Risk Identification and Assessment - Identification and Assessment Toolhitm357No ratings yet
- Breech PresentationDocument85 pagesBreech Presentationwidya vannesaNo ratings yet
- Art of Fitness BrochureDocument62 pagesArt of Fitness Brochureprotein47No ratings yet
- Toolbox Talk Chemical GlovesDocument6 pagesToolbox Talk Chemical GlovesBomber Man100% (1)
- Wrist Anatomy and Surgical Approaches: Roy Cardoso, MD, Robert M. Szabo, MD, MPHDocument22 pagesWrist Anatomy and Surgical Approaches: Roy Cardoso, MD, Robert M. Szabo, MD, MPHMd Ahsanuzzaman PinkuNo ratings yet
- Plexo BraquialDocument26 pagesPlexo BraquialXavier RiveraNo ratings yet
- Epov EclipseDocument12 pagesEpov EclipseShivani JaiswalNo ratings yet
- Investigation of An Animal Mutilation Injuries in Cache County, UtahDocument33 pagesInvestigation of An Animal Mutilation Injuries in Cache County, UtahLionel Elyansun100% (1)
- New Power Cabinet Installation ManualDocument59 pagesNew Power Cabinet Installation ManualHerianto UntasNo ratings yet
- Jeopardy CPRDocument51 pagesJeopardy CPRapi-273870175No ratings yet
- Lec 11 UL Forarm Anterior CompartmentDocument32 pagesLec 11 UL Forarm Anterior CompartmenthusseinNo ratings yet
- What Are The Benefits of Chiropractic CareDocument2 pagesWhat Are The Benefits of Chiropractic CaretomNo ratings yet
- MRI REPORT OF LEFT KNEE (Tushar Singh)Document2 pagesMRI REPORT OF LEFT KNEE (Tushar Singh)Tushar SinghNo ratings yet
- Kinesiotaping TechniquesDocument26 pagesKinesiotaping TechniquesSuhana hidayat100% (1)
- Dtx10 SDocument60 pagesDtx10 Sлюбовь инжинирингNo ratings yet
- Ecto-Meso-Endo-Dermal LayersDocument3 pagesEcto-Meso-Endo-Dermal LayersCarissa NicholsNo ratings yet
- Risk Assessment - Window and Glass Partition InstallationDocument4 pagesRisk Assessment - Window and Glass Partition Installationburak80% (5)
- LungeDocument6 pagesLungeKaiNo ratings yet
- Iotn Training SlidesDocument38 pagesIotn Training SlidesAchini LiyanageNo ratings yet
- ATI Radially-Compliant Robotic Deburring Tools Flexdeburr™: Installation and Operation ManualDocument28 pagesATI Radially-Compliant Robotic Deburring Tools Flexdeburr™: Installation and Operation ManualAndrei JilaNo ratings yet
- 100 Opthalmology Questions For PracticeDocument37 pages100 Opthalmology Questions For Practicekyonaboy85% (13)
- SkullmethodDocument3 pagesSkullmethodJoeriz BartolomeNo ratings yet
- Assessment (1) Diagnosis: LT Knee OsteoarthritisDocument13 pagesAssessment (1) Diagnosis: LT Knee OsteoarthritisDounia A OdehNo ratings yet
- The Americans 1x01 - Pilot PDFDocument75 pagesThe Americans 1x01 - Pilot PDFDaniel GreenspanNo ratings yet
- NCLEX - Review (6514)Document51 pagesNCLEX - Review (6514)whereswaldo007yahooc100% (1)
- Panch Tantra Stories Part TwoDocument144 pagesPanch Tantra Stories Part TwoKrupal VithlaniNo ratings yet