Professional Documents
Culture Documents
Pseudomonas
Uploaded by
ajgondalCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pseudomonas
Uploaded by
ajgondalCopyright:
Available Formats
Eur J Clin Microbiol Infect Dis (2003) 22:2834 DOI 10.
1007/s10096-002-0852-8
A RT I C L E
G. Manno E. Ugolotti M. L. Belli M. L. Fenu L. Romano M. Cruciani
Use of the E test to Assess Synergy of Antibiotic Combinations Against Isolates of Burkholderia cepacia-Complex from Patients with Cystic Fibrosis
Published online: 25 January 2003 Springer-Verlag 2003
Abstract Treatment of Burkholderia cepacia-complex infections in cystic fibrosis patients is problematic, since the microorganism is often resistant to most antimicrobial agents. In this study, the Epsilometer test, or E test, was used to assess the activity of antimicrobial combinations against Burkholderia cepacia-complex. In a preliminary evaluation, the E test was compared to the checkerboard method using 10 test organisms. Synergy testing by the E test was then performed on 131 clinical isolates of Burkholderia cepacia-complex using various combinations of antimicrobial agents. Agreement between the E test and the checkerboard method was 90%. The rate of resistance to individual agents ranged from 48% for meropenem to 100% for tobramycin, chloramphenicol, and rifampin. In 71.6%, 15.6%, and 12.6% of the test evaluations performed, the combinations tested resulted in additivity/indifference, synergism, and antagonism, respectively. The highest rates of synergy were observed with combinations of ciprofloxacin-piperacillin (44%), rifampin-ceftazidime (33%), chloramphenicolceftazidime (22%), cotrimoxazole-piperacillin/tazobactam (22%), and ciprofloxacin-ceftazidime (21%). Rates of antagonism for cotrimoxazole and chloramphenicol in combination with -lactam agents were higher than those observed for ciprofloxacin plus -lactam agents. These results suggest that the E test is a valuable and
G. Manno () E. Ugolotti M. L. Belli M. L. Fenu Department of Paediatrics, Infectious Diseases Research and Diagnosis Laboratory, Gaslini Research Institute-Childrens Hospital, University of Genoa, Largo G. Gaslini 5, 16147 Genoa, Italy e-mail: graziana@unige.it Tel.: +39-010-5636780, Fax: +39-010-3773210 L. Romano Department of Paediatrics, Cystic Fibrosis Centre, 2nd Paediatric Clinic, Gaslini Research InstituteChildrens Hospital, University of Genoa, Genoa, Italy M. Cruciani Center of Preventive Medicine, USL 20, Verona, Italy
practical method to be considered for improving the identification of possible therapeutic options in cystic fibrosis patients infected with organisms belonging to the Burkholderia cepacia-complex.
Introduction
Although Burkholderia cepacia-complex is virtually nonpathogenic in healthy hosts, it is commonly associated with colonisation and pulmonary infection in cystic fibrosis patients [1, 2, 3, 4, 5]. Variable clinical courses have been reported in cystic fibrosis patients after the acquisition of Burkholderia cepacia [6, 7, 8, 9]. Antibiotic resistance appears to be a critical factor in the virulence of this microorganism [7]. Optimal antibiotic therapy of Burkholderia cepacia infection in cystic fibrosis patients is often problematic since most strains are resistant to the majority of individual antibiotics. Therefore, the concomitant use of two or more antimicrobial agents is often deemed necessary for the treatment of Burkholderia cepacia infections. Routine susceptibility testing of antibiotic combinations would be a valuable addition to the processing of Burkholderia cepacia isolates from cystic fibrosis patients. However, laboratory methods used to assess the activity of antimicrobial combinations are often time-consuming and relatively laborious to perform. The Epsilometer (E test) is an agar diffusion method for the quantitative determination of susceptibility to antimicrobial agents. The E test has also been used to evaluate the activity of antimicrobial combinations against mycobacteria and gram-positive and gram-negative microorganisms, including Pseudomonas spp. [10, 11, 12, 13]. Results from these studies suggest that the E test may provide an alternative method for studying the activity of antimicrobial combinations. In the present study, we evaluated the results of synergy testing using the E test on a total of 131 isolates of Burkholderia cepacia-complex recovered from cystic fibrosis patients in a large childrens hospital.
29
Materials and Methods
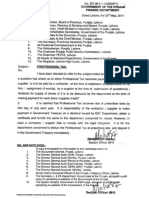
Bacterial Strains One hundred thirty-one isolates of Burkholderia cepacia complex were studied. They were recovered from sputum of 53 cystic fibrosis patients (23 males, 30 females) attending the cystic fibrosis center of the Gaslini Childrens Hospital in Genoa, Italy. Specimens were processed according to techniques regularly used in our laboratory for cystic fibrosis patients [14]. Strains were collected prospectively during a 7-year period (19932000). Multiple isolates from the same patient were differentiated on the basis of colony morphology and antibiotic susceptibility testing. Strains were isolated with the use of a medium selective for Burkholderia cepacia-complex (oxidation fermentation polymyxin B lactose [OFPBL] medium, Becton-Dickinson, USA). Strains were assigned to the Burkholderia cepacia-complex by polyphasic analysis employing the following conventional phenotypic tests: the API 20 E and API NE systems (bioMrieux, France), production of six sugars using OF basal medium (Difco, USA), the oxidase test, growth at 42C, production of pigment, and haemolysis. In addition, genus- and species-specific polymerase chain reaction assays were performed as described previously [15]. Ten isolates, recovered from different cystic fibrosis patients, were chosen for comparative evaluation of the checkerboard method and the E test. No common random amplified polymorphic DNA (RAPD) profiles were identified among these isolates (unpublished data). Preliminary Comparative Evaluation of the Checkerboard Method and the E Test The minimal inhibitory concentrations (MICs) of piperacillin, ciprofloxacin, and ceftazidime were determined by broth macrodilution and the E test for 10 test organisms. For broth macrodilution, we used Mueller-Hinton broth supplemented with calcium and magnesium; the final inoculum used was approximately 5105 cfu/ml. Stock solutions of antibiotics were prepared from standard laboratory powders in accordance with the guidelines of the National Committee for Clinical Laboratory Standards (NCCLS) [16]. The results were read after 1824 h of incubation in ambient air at 35C. The checkerboard method was performed in the same way, using two combinations of antibiotics: piperacillin plus ciprofloxacin, and ceftazidime plus ciprofloxacin. Both combinations were prepared as double-dilution concentrations ranging from 0.06 to 32 g/ml for ciprofloxacin and from 0.5 to 256 g/ml for piperacillin and ceftazidime. For the E test, Mueller-Hinton agar plates were inoculated with swabs saturated with suspensions of the test organism equivalent to a 0.5 McFarland standard, and the plastic strip (AB Biodisk, Sweden) was placed on a plate. For evaluation of synergy, one antibiotic strip was placed onto an agar plate for 1 h as described previously [17] and then removed, and a second antibiotic strip was placed on top of the gradient of the first agent. The MIC was interpreted as the value at which the inhibition zone intersected the scale on the E strip (Fig. 1). MIC results obtained by both methods were converted to qualitative categories (susceptible, intermediate, and resistant) using NCCLS guidelines [16] and compared. A reference strain, Pseudomonas aeruginosa ATCC 27853, was used as a quality control strain [18]. To evaluate the effect of the combination, the fractional inhibitory concentration (FIC) was calculated for each antibiotic in each combination as follows: FIC index=FIC of drug A+FIC of drug B, where FIC of drug A=MIC of drug A in combination/MIC of drug A alone; and FIC of drug B=MIC of drug B in combination/MIC of drug B alone [19]. Synergism was defined as an FIC index of 0.5, additivity as an FIC index of 0.510.99, indifference as an FIC index of 12, and antagonism as an FIC index of >2.
Fig. 1 Interpretation of the E test combination study, showing MICs of antibiotics A and B, used individually and in superimposed combinations at fixed ratios (concentration maxA:concentration maxB). FIC index=FIC of drug A + FIC of drug B, where FIC of drug A=MIC of drug A in combination/MIC of drug A alone; and FIC of drug B=MIC of drug B in combination/MIC of drug B alone
Evaluation of Drug Combinations by the E Test The following antibiotics were used singly and in various combinations: ceftazidime, ciprofloxacin, piperacillin, piperacillin-tazobactam, meropenem, trimethoprim-sulfamethoxazole (TMP-SMX; cotrimoxazole), chloramphenicol, minocycline, and rifampin. The antimicrobial concentrations or ranges tested were as follows: 0.016250 g/ml for ceftazidime, piperacillin, piperacillin/tazobactam (4 g/ml), cotrimoxazole (1/9), chloramphenicol, rifampin, and minocycline; 0.00232 g/ml for ciprofloxacin and meropenem; and 0.12564 g/ml for tobramycin. MIC and synergy testing were performed and interpreted as described above. Statistical Analysis Data were assessed for statistical significance using the chisquared2 test or Fishers two-tailed exact test.
Results
The MIC results obtained with the broth macrodilution method and the E test for the 10 test isolates are shown in Table 1. The results were variant by greater than 2 twofold dilutions for two isolates for ciprofloxacin. Five minor discrepancies (an intermediate result obtained by only one of the methods) occurred: three for ceftazidime and two for piperacillin and ciprofloxacin. One very major discrepancy (an isolate susceptible by the E test and resistant by broth dilution method) was noted for ciprofloxacin. Comparative results of synergy testing obtained with the checkerboard method and the E test for the 10 test strains are shown in Table 2. Overall, the results agreed in 18 of 20 instances (10 strains, 2 antibiotic combinations). The two discrepant results occurred with combinations of piperacillin and ciprofloxacin; in each of these cases the checkerboard method indicated synergy, while the E test indicated indifference.
30 Table 1 MICs of ceftazidime, piperacillin, and ciprofloxacin as determined by the E test and broth macrodilution for test 10 strains of Burkholderia cepacia complex Strain no. MIC (g/ml) Ceftazidime E test 1 2 3 4 5 6 7 8 9 10 Median 32 (R) 128 (R) 16 (I) 16 (I) 16 (I) 16 (I) 16 (I) 24 (I) 16 (I) 32 (R) 24 Broth macrodilution 32 (R) 128 (R) 16 (I) 16 (I) 16 (I) 16 (I) 32 (R) 32 (R) 16 (I) 16 (I) 16 Piperacillin E test >256 (R) 128 (R) >256 (R) 16 (S) >256 (R) 8 (S) >256 (R) >256 (R) 16 (S) >256 (R) >256 Broth macrodilution >256 (R) 128 (R) 128 (R) 64 (I) 256 (R) 8 (S) 128 (R) 128 (R) 64 (I) >256 (R) >256 Ciprofloxacin E test >32 (R) >32 (R) >32 (R) 2 (I) 32 (R) 8 (R) >32 (R) >32 (R) 1 (S) >32 (R) >32 Broth macrodilution >16 (R) 16 (R) 16 (R) 1 (S) 2 (I) 4 (R) 8 (R) 4 (R) 4 (R) 4 (R) 4
I, intermediately susceptible; R, resistant; S, susceptible
Table 2 Comparison of results of synergy testing for 10 test strains of Burkholderia cepacia complex Antibiotic combination No. of isolates showing synergism(FIC <0.5) Checker-board Piperacillin + ciprofloxacin Ceftazidime + ciprofloxacin Total (%) 6 5 55 E test 4 5 45 No. of isolates showing indifference (FIC 12) Checker-board 3 5 40 E test 5 5 50 No. of isolates showing antagonism (FIC >2) Checker-board 1 0 5 E test 1 0 5
Table 3 MICs as determined by the E test for 131 isolates of Burkholderia cepacia-complex Antibiotic MIC (g/ml) MIC50 Piperacillin Ceftazidime Ciprofloxacin Meropenem Minocycline Cotrimoxazole Chloramphenicol Tobramycin Rifampin 256 32 16 8 16 32 256 >64 32 MIC90 >256 >256 >32 >32 >256 >32 >256 >64 >32 Percent resistance 78 60 89 48 58 89 100 100 100
Evaluation of the E test Using 131 Strains of Burkholderia cepacia Results of the E test for individual antimicrobial agents are shown in Table 3. Among the -lactam agents, meropenem had the best inhibitory activity (52% of strains susceptible), followed by ceftazidime (40%). Among the non -lactam agents, minocycline had the best antimicrobial activity (42% of strains susceptible). All strains tested were resistant to chloramphenicol tobramycin and rifampin, while only 11% of strains were susceptible to ciprofloxacin and cotrimoxazole.
The results of synergy testing by the E test are shown in Tables 4 and 5. Overall, indifference or additivity was observed in 522 of 728 (71.6%) instances, synergism in 114 (15.6%), and antagonism in 92 (12.6%). On the whole, the proportion of isolates that demonstrated synergism, additivity, or indifference did not differ when tested against combinations of -lactam agents plus ciprofloxacin, -lactam agents plus cotrimoxazole, -lactam agents plus tobramycin, and -lactam agents plus rifampin (Table 5). There was, however, a wide range of rates of synergy found with each combination (Table 4). The most effective antibiotic combinations were ciprofloxacin plus piperacillin, rifampin plus ceftazidime, chloramphenicol plus ceftazidime, cotrimoxazole plus piperacillin-tazobactam, and ciprofloxacin plus ceftazidime, which were associated with synergy in 44%, 33%, 22%, 22%, and 21% of the isolates tested, respectively. In contrast, combinations of tobramycin plus -lactam agents and tobramycin plus ciprofloxacin were not associated with synergism in any of the isolates tested. Moreover, combinations of ciprofloxacin and -lactam agents showed a statistically significant lower percentage of antagonism (19 of 339 [5.6%]) when compared with the combination of cotrimoxazole and -lactam agents (26 of 139 [18.7%], P=0.001) and with the combination of chloramphenicol and -lactam agents (24 of 91 [26.3%], P<0.0001).
31 Table 4 Synergy, additivity, indifference, or antagonism of antibiotic combinations against clinical isolates of Burkholderia cepacia-complex as determined by the E test Antibiotic combination No. of strains tested 129 49 76 85 65 38 27 9 45 40 42 20 36 9 14 15 5 6 6 6 6 728 No. (%) of strains Synergism CIP+CAZ CIP+PIP CIP+TMP CIP+MEM SXZ+CAZ SXZ+MEM SXZ+TMP SXZ+PIP SXZ+CIP CHL+MEM CHL+TMP CHL+SXZ CHL+MIN CHL+CAZ RIF+PIP RIF+CAZ RIF+MEM TOB+CAZ TOB+PIP TOB+MEM TOB+CIP Total no. of evaluations 27 (21) 22 (44) 9 (11) 6 (12) 9 (14) 3 (8) 6 (22) 0 (0) 5 (11) 5 (12) 5 (12) 1 (5) 6 (17) 2 (22) 3 (21) 5 (33) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 114 (15.6) Additivity 33 (25) 7 (14) 11 (14) 25 (29) 12 (18) 8 (21) 3 (11) 2 (22) 8 (18) 7 (17) 6 (14) 0 (0) 11 (31) 1 (11) 3 (21) 4 (27) 2 (40) 0 (0) 0 (0) 0 (0) 0 (0) 143 (19.6) Indifference 63 (49) 18 (37) 52 (68) 47 (55) 33 (55) 18 (47) 12 (44) 7 (78) 20 (44) 17 (42) 21 (50) 15 (75) 15 (42) 3 (33) 8 (57) 5 (33) 1 (20) 6 (100) 6 (100) 6 (100) 6 (100) 379 (52.0) Antagonism 6 (5) 2 (4) 4 (5) 7 (8) 11 (17) 9 (24) 6 (22) 0 (0) 12 (27) 11 (27) 10 (24) 4 (20) 4 (11) 3 (33) 0 (0) 1 (7) 2 (40) 0 (0) 0 (0) 0 (0) 0 (0) 92 (12.6)
CAZ, ceftazidime; CHL, chloramphenicol; CIP, ciprofloxacin; MEM, meropenem; MIN, minocycline; PIP, piperacillin; RIF, rifampin; SXZ, sulfamethoxazole; TOB, tobramycin; TMP, trimethoprim
Table 5 Synergy, additivity, or antagonism of the most frequent antibiotic combinations tested against clinical isolates of Burkholderia cepacia-complex as determined by the E test Antibiotic combination No. of evaluations 339 139 91 24 34 No. (%) of strains showing synergism 64 (18.8) 18 (12.9) 12 (13.1) 0 (0) 8 (23.5) No. (%) of strains showing additivity or indifference 256 (75.4) 95 (68.2) 55 (60.4) 24 (100) 23 (67.5) No. (%) of strains showing antagonism 19 (5.6) 26 (18.7)* 24 (26.3)** 0 (0) 3 (8.8)
Ciprofloxacin + -lactam agents Cotrimoxazole + -lactam agents Chloramphenicol + -lactam agents Tobramycin + -lactam agents Rifampin + -lactam agents
* P=0.0001 by comparison to ciprofloxacin + -lactam agents ** P<0.0001 by comparison to ciprofloxacin + -lactam agents Table 6 Patterns of susceptibility to -lactam agents alone and in combination with various antibiotics showing synergistic interaction by the E test Antimicrobial combination -lactam agents + ciprofloxacin -lactam agents + cotrimoxazole -lactam agents + chloramphenicol -lactam agents + rifampin No. (%) of strains susceptible to both drugs in combination 18/64 (28.1) 12/18 (88.8) 4/12 (33.3) 2/8 (25) No. (%) originally susceptible to single antibiotics alone ciprofloxacin, 1/64 (1.5%) -lactams, 5/64 (7.8%) cotrimoxazole, 17/18 (94.4%) -lactams, 0/18 (0%) chloramphenicol, 1/12 (8.3%) -lactams, 0/12 (0%) rifampin, 0/8 (0%) -lactams, 0/8 (0%) No. (%) susceptible to single antibiotics when combined ciprofloxacin, 27/64 (42.1%)* -lactams, 50/64 (78.1%)* cotrimoxazole, 8/8 (100%) -lactams, 11/18 (61.1%)* chloramphenicol, 4/12 (25%) -lactams, 7/12 (58.3%)** rifampin, 2/8 (25%) -lactams, 6/8 (75%)***
* P<0.0001, **P=0.002, ***P=0.003 by comparison to original susceptibility to single antibiotic
Furthermore, there was a significant increase in the proportion of strains susceptible to -lactam agents in any of the synergistic combinations tested (Table 6). Likewise, there was a significant increase in the proportion of strains susceptible to ciprofloxacin when it was combined with piperacillin (P=0.02) or with ceftazidime (P=0.001).
Discussion
Since the mid-1980s, an increasing proportion of patients attending cystic fibrosis centers have been colonised with Burkholderia cepacia. Colonisation with Burkholderia cepacia is associated with an increased duration
32
of hospitalisation and reduced long-term survival [3, 4, 5, 6, 7, 8, 9]. Thus, the issue of effective antimicrobial therapy of such infections is of chief importance. Burkholderia cepacia is innately resistant to many antimicrobial agents, making effective treatment problematic and restricted to just a few antibacterial agents. The microorganism is intrinsically resistant to aminoglycosides, and rates of resistance to -lactam agents are frequently high. The in vitro susceptibility of Burkholderia cepacia to carbapenems, ciprofloxacin, cotrimoxazole, and other agents is variable [7, 20]. Consequently, the concomitant use of two or more antibiotics is a common practice in the treatment of cystic fibrosis patients infected with Burkholderia cepacia [7, 20, 21, 22]. In this context, however, convincing data supporting the use of combination therapy are lacking. Published results from trials in pulmonary exacerbations of cystic fibrosis comparing monotherapy and combination therapy are limited, controversial, and include only small numbers of patients [21]. The reasons for the use of antibiotic combinations include the achievement of antimicrobial synergism and the reduced probability of the emergence of resistant strains. Ideally, rather than empirical treatment, an effective antimicrobial combination regimen should be chosen on the basis of the results of in vitro tests. Unfortunately, laboratory methods used to assess the activity of antimicrobial combinations (e.g., checkerboard and timekill curves) are cumbersome, time-consuming, and require technical experience. In the present study, we used the E test method for evaluating antimicrobial combinations potentially synergistic against clinical isolates of Burkholderia cepacia. Antimicrobial combinations were tested by superimposing different antibiotic strips on the same agar plate. The prerequisite for creating superimposed antibiotic combination is an effective release of the antibiotic from the strip carrier into the agar matrix. Using a model similar to one we used, Bolstrom et al. [17] showed that most of the antibiotics tested were released within 30 min, and all were completely released within 1 h. As in previous reports [11, 12, 13], the results were compared with those of the checkerboard method. In our preliminary evaluation using 10 strains of Burkholderia cepaciacomplex, agreement between the E test and checkerboard was observed in 18 of 20 instances (10 strains, 2 antibiotic combinations). In another study that compared three different in vitro methods of detecting synergy, concordance between the E test and the checkerboard or time-kill curves method was present in 75% of cases [10]. In this study, however, synergy was evaluated by the E test using a different technique, and the plastic strips were crossed at a 90 angle on the plates. From the results of the E test method, no great optimism can be raised about the activity of any antimicrobial agents tested singly against the 131 Burkholderia cepacia isolates in our center. The MIC90 of piperacillin, ceftazidime, minocycline, and chloramphenicol was >256 g/ml, of tobramycin >64 g/ml, and of ci-
profloxacin, meropenem, and rifampin >32 g/ml. Only 52% of the isolates were susceptible to meropenem, and about 40% to minocycline and ceftazidime. Ciprofloxacin, ceftazidime, and cotrimoxazole showed poor activity, while chloramphenicol, tobramycin, and rifampin were not active against any Burkholderia cepacia isolate. On the basis of these susceptibility profiles, the choice of an effective antibiotic treatment can be considered problematic. To help us make optimal therapeutic choices, an E-test-based technique to evaluate antimicrobial combinations was performed on these 131 isolates. The results of the drug combination study show that, in 71.6% of the test evaluations performed, isolates were affected additively or indifferently by the combinations tested. However, isolates were affected by synergism in 15.6% of the evaluations and by antagonism in 12.6% of the evaluations. Synergism was more commonly observed with combinations of ciprofloxacin and -lactam agents (64 of 339 [18.8%] evaluations). Previous in vitro studies investigating the potential of the use of ciprofloxacin-lactam combinations against Burkholderia cepacia by checkerboard [7, 22, 23, 24, 25] or time-kill curves [26] methods gave variable results. The rate of synergy for the ciprofloxacin--lactam combinations in the present study are lower than those reported in some of these studies [22, 23, 24, 25] but are in agreement with those of Burns and Saiman [7]; these authors reported a rate of synergism of 16% by the checkerboard method on 652 Burkholderia cepacia isolates using the combination of piperacillin-ciprofloxacin. The combination of -lactam agents and cotrimoxazole or chloramphenicol was synergistic in 12.9% (18 of 131) and 13.1% (12 of 91) of isolates, respectively. Of note, synergy between -lactam agents and rifampin was found in 23.5% of 34 isolates tested. In contrast, the combination of tobramycin and -lactam agents was not associated with synergy in any of the 24 isolates examined. These results are in disagreement with those of previous studies that have evaluated the combination of -lactam agents and aminoglycosides by the checkerboard method on Burkholderia cepacia isolates [7, 19, 27]. In those studies, variable rates of synergism were observed, and resistance to aminoglycosides did not preclude the positive result. This discrepancy might be explained by the very high level of resistance to tobramycin that characterises our strains, though a discordance between the E test and checkerboard methods to detect synergism cannot be excluded. For most isolates that were affected synergistically, the MICs of -lactam agents in any of these combinations and the MICs of ciprofloxacin in combination with piperacillin or ceftazidime dropped, often into the susceptibility range. Antagonism was observed in 92 of 728 (12.6%) evaluations. Rates of antagonism for cotrimoxazole (18.7%) and chloramphenicol (26.3%) in combination with -lactam agents were significantly higher than those observed
33
for ciprofloxacin and -lactam agents (5.6%). Antagonism between -lactam agents and chloramphenicol has been reported in various in-vitro studies, but the clinical relevance of these observations is not convincing [19]. The use of antibiotic combinations in the treatment of patients with cystic fibrosis is widely accepted. In the case of Burkholderia cepacia infection, an empirical choice of treatment is often problematic because most strains are panresistant to most individual agents [7, 20]. Practical and accurate methods to assess the activity of antimicrobial combinations should therefore be considered in order to ensure that the therapy chosen is optimal for the patient. The E test technique that we have applied allows us to rapidly screen multiple combinations of antibiotics against isolates of Burkholderia cepacia. The technique was chosen because it is both easy to perform and flexible. The modified technique for synergy studiessimple to use, time efficient, and reproducibleis now increasingly being used by others [28]. In the present study, the antibiotic gradients were superimposed at a fixed ratio corresponding to the maximal concentration. However, antibiotic combinations may be superimposed in different positions or crossed in order to achieve other ratios of the two components [10, 17]. Overall, the results of this study and those of previous studies support the further evaluation of the E test for improving our therapeutic options for pulmonary exacerbations of cystic fibrosis associated with Burkholderia cepacia or other microorganisms.
Acknowledgements We are grateful to Gaslini Research Institute and to the Ligurian Cystic Fibrosis Foundation for financial support.
References
1. Baltimore BJ, Radnay-Baltimore K, Graevenitz A von, Bolan TF (1982) Occurrence of non-fermentative gram-negative rods other thanPseudomonas aeruginosa in the respiratory tract of children with cystic fibrosis. Helv Paediatr Acta 37:547 554 2. Isles AI, Maclusky M, Corey M, Gold R, Prober C, Fleming P, Levison H (1984)Pseudomonas cepacia infection in cystic fibrosis: an emerging problem. J Pediatr 104:206210 3. Tablan OC, Martone WJ, Doershuk-Stern RC, Thomassen MJ, Klinger JD, White JW, Carson LA, Jarvis WR (1987) Colonisation of the respiratory tract withPseudomonas cepacia in cystic fibrosis. Chest 91:527532 4. Tablan OC, Chorba TL, Schidlow DV, White JW, Hardy KA, Gilligan PH, Morgan WM, Carson LA, Martone WJ, Jason JM et al (1985)Pseudomonas cepacia colonisation in patients with cystic fibrosis: risk factors and clinical outcome. J Pediatr 107:382387 5. Thomassen MJ, Demko CA, Klinger JD, Stern RC (1985) Pseudomonas cepacia colonisation among patients with cystic fibrosis. Am Rev Resp Dis 131:791-796 6. Brown P, Butler S, Nelson J (1993)Pseudomonas cepacia in adult cystic fibrosis: accelerated decline in lung function and increased mortality. Thorax 48:425429 7. Burns Jl, Saiman L (1999)Burkholderia cepacia infections in cystic fibrosis. Ped Infect Dis J 18:153156
8. Frangolias DD, Mahenthiralingam E, Rae S, Raboud JM, Davidson AG, Wittmann R, Wilcox PG (1999)Burkholderia cepacia in cystic fibrosis. Variable disease course. Am J Respir Crit Care Med 160:15721577 9. Lewin L, Byard P, Davis P (1990) Effect ofPseudomas cepacia colonisation on survival and pulmonary function in cystic fibrosis patients. J Clin Epidemiol 43:125130 10. White RL, Burgess DS, Manduru M, Bosso JA (1996) Comparison of three different in vitro methods of detecting synergy: time-kill, checkerboard, and E test. Antimicrob Agents Chemother 40:19141918 11. Hofner SE, Klintz L, Olsson-Liljequist B, Carlson A, Bolmstrom A (1993) Rapid susceptibility testing of Mycobacterium chelonae and M. fortuitum to single and combined drug using E-test. In: Program and abstracts of the 18th International Congress of Chemotherapy, Stockholm, abstract no. 939 12. Bolmstrom A, Karlson A, Nordstrom U, Mills (1995) E-test for drug combination studies with mycobacteria. In: Program and abstracts of the 19th International Congress of Chemotherapy, Montreal, abstract no. 1142 13. Poupard J, Langan R, Utrup L, Rittenhouse S, Clark RB (1993) Use of the AB-BIODISK E-test as a screen for ticarcillin clavulanate-amikacin synergy with isolates ofXantomonas maltophilia. In: Program and abstracts of the 18th International Congress of Chemotherapy, Stockholm, abstract no. 366 14. Saiman L, Schidlow D, Smith A (eds) (1994) Concepts in care: microbiology and infectious diseases in cystic fibrosis, vol V. Cystic Fibrosis Foundation, Bethesda, MD, p S1 15. Bevivino A, Dalmastri C, Tabacchioni S, Chiarini L, Belli ML, Piana S, Materazzo A, Vandamme P, Manno G (2002) Burkolderia cepacia Complex bacteria of clinical and environmental source in Italy: genomovar status and distribution of traits related with virulence and trasmissibility. J Clin Microbiol 40:846851 16. National Committee for Clinical Laboratory Standards (1993) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A3. NCCLS, Villanova, PA 17. Bolstrom A, Ardvison S, Ericson M, Karlsonn A (1989) New in vitro models for studying antibiotic combination using predefined antibiotics gradient. In: Program and abstracts of the 16th International Congress of Chemotherapy, Jerusalem, abstract no. 011 18. Acar JF, Goldstein FW (1996) Disk susceptibility test. In: Lorian V (ed) Antibiotics in laboratory medicine, 4th edn. Williams & Wilkins, Baltimore, pp 52111 19. Eliopoulos GM, Moellering RC Jr (1996) Antimicrobial combination. In: Lorian V (ed) Antibiotics in laboratory medicine, 4th edn. Williams & Wilkins, Baltimore, pp 330396 20. Aaron SD, Ferris W, Henry DA, Speert DP, MacDonald NE (2000) Multiple combination bactericidal antibiotic testing for patients with cystic fibrosis infected withBurkholderia cepacia. Am J Respir Crit Care Med 161:12061212 21. Bosso JA, Saxon BA, Matsen JM (1987) In vitro activities of aztreonam combined with tobramycin and gentamicin against clinical isolates ofPseudomonas aeruginosa and Pseudomonas cepacia from patients with cystic fibrosis. Antimicrob Agents Chemother 31:14031405 22. Bosso JA, Saxon BA, Matsen JM (1990) In vitro activities of combinations of aztreonam, ciprofloxacin, and ceftazidime against clinical isolates ofPseudomonas aeruginosa and Pseudomonas cepacia from patients with cystic fibrosis. Antimicrob Agents Chemother 34:487488 23. Bosso JA, Saxon BA, Matsen JM (1991) Comparative activity of cefepime, alone and in combination, against clinical isolates ofPseudomonas aeruginosa and Pseudomonas cepacia from cystic fibrosis patients. Antimicrob Agents Chemother 35:783 784 24. Kumar A, Wofford-McQuenn R, Gordon RC (1989) Ciprofloxacin, imipenem and rifampicin: in-vitro synergy of two and three drug combinations againstPseudomonas cepacia. J Antimicrob Chemother 23:831835
34 25. Lu DCT, Chang SC, Chen YC, Luh KT, Hsieh WC (1997) In vitro activities of antimicrobial agents, alone and in combinations againstBurkholderia cepacia isolated from blood. Diagn Microbiol Infect Dis 28:187191 26. Bonacorsi S, Fitoussi F, Lhopital S, Bingen E (1999) Comparative in vitro activities of meropenem, imipenem, temocillin, piperacillin, and ceftazidime in combination with tobramycin, rifampin, or ciprofloxacin against Burkholderia cepacia isolates from patients with cystic fibrosis. Antimicrob Agents Chemother 43:213217 27. Aronoff SC, Klinger JD (1984) In vitro activities of aztreonam, piperacillin, and ticarcillin combined with amikacin against amikacin-resistantPseudomonas aeruginosa and Pseudomonas cepacia isolates from children with cystic fibrosis. Antimicrob Agents Chemother 25:279280 28. Lewis RE, Diekema DJ, Messer SA, Pfaller MA, Klepser ME (2002) Comparison of E test, checkerboard dilution and timekill studies for the detection of synergy or antagonism between antifungal agents tested againstCandida species. J Antimicrob Chemother 49:345351
You might also like
- Form Sr. Instruction Instructions For Filling in Return Form & Wealth StatementDocument8 pagesForm Sr. Instruction Instructions For Filling in Return Form & Wealth StatementajgondalNo ratings yet
- Extensively Drug-Resistant Pseudomonas AeruginosaDocument6 pagesExtensively Drug-Resistant Pseudomonas AeruginosaajgondalNo ratings yet
- DentalPosterWeb8 5x11Document1 pageDentalPosterWeb8 5x11ajgondalNo ratings yet
- Fic CriterionDocument19 pagesFic CriterionajgondalNo ratings yet
- Pro TaxDocument1 pagePro TaxM Usman ChaudharyNo ratings yet
- MTBF MTFF Vol 1 by MTBF TeamDocument116 pagesMTBF MTFF Vol 1 by MTBF TeamajgondalNo ratings yet
- (Copy of The Same Is Also Available On Our Website) : IndicationDocument4 pages(Copy of The Same Is Also Available On Our Website) : IndicationajgondalNo ratings yet
- IIIDocument17 pagesIIIajgondalNo ratings yet
- IIIDocument17 pagesIIIajgondalNo ratings yet
- CGT On Stock ExchangesDocument2 pagesCGT On Stock ExchangesajgondalNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 4 - PaediatricsDocument121 pages4 - Paediatricsayeshafarooq60No ratings yet
- Cystic Fibrosis OutlineDocument3 pagesCystic Fibrosis OutlineDominique PorterNo ratings yet
- Paeds MCQs Part 1Document34 pagesPaeds MCQs Part 1SsNo ratings yet
- Song Review I Lived by OnerepublicDocument2 pagesSong Review I Lived by OnerepublicNur AdilaNo ratings yet
- D - 5answer KeyDocument15 pagesD - 5answer KeyJune DumdumayaNo ratings yet
- Pedia BulletsDocument2 pagesPedia BulletsDebbiearlNo ratings yet
- Scenarios DISEASES RELATED TO CELL ORGANELLEDocument5 pagesScenarios DISEASES RELATED TO CELL ORGANELLEShahnaz AhmedNo ratings yet
- Pharmacology Respiratory DrugsDocument51 pagesPharmacology Respiratory DrugsAngel DamoNo ratings yet
- Cystic FibrosisDocument35 pagesCystic Fibrosisvani reddyNo ratings yet
- Cystic Fibrosis Guidelines For ParentsDocument14 pagesCystic Fibrosis Guidelines For ParentsReine SalamounNo ratings yet
- RPN Post Review TestDocument69 pagesRPN Post Review Testdaljit chahalNo ratings yet
- Understanding Pathophysiology, Fifth Edition - Sue Huether PDFDocument1,187 pagesUnderstanding Pathophysiology, Fifth Edition - Sue Huether PDFmina mina97% (58)
- NCM 116 Medical SurgicalDocument9 pagesNCM 116 Medical SurgicalIvan A. EleginoNo ratings yet
- 1 s2.0 S1569199321019652 MainDocument1 page1 s2.0 S1569199321019652 MainAnita DewiNo ratings yet
- Chapter 53 - Introduction To The Respiratory SystemDocument13 pagesChapter 53 - Introduction To The Respiratory SystemJonathonNo ratings yet
- AQA GCSE Biology For Combined Science: Trilogy: Exam-Style Questions (Higher)Document8 pagesAQA GCSE Biology For Combined Science: Trilogy: Exam-Style Questions (Higher)OHNo ratings yet
- Clinical Cases: World Journal ofDocument16 pagesClinical Cases: World Journal ofRhotmy Raúl Escobar GuzmánNo ratings yet
- Cystic Fibrosis Fact SheetDocument6 pagesCystic Fibrosis Fact SheetAnggun SafariantiniNo ratings yet
- Head N Neck-MCQsDocument57 pagesHead N Neck-MCQsbhargavi pasagadaNo ratings yet
- Cystic Fibrosis PathophysiologyDocument5 pagesCystic Fibrosis PathophysiologyKim Enrico JumarangNo ratings yet
- Disorder Cause Treatment/Possible TreatmentDocument3 pagesDisorder Cause Treatment/Possible TreatmentNoval, SheanNo ratings yet
- 6th Chapter4 Section5 pt2Document11 pages6th Chapter4 Section5 pt2Angel TemelkoNo ratings yet
- Billy Ray A. Marcelo, BSN, RN Faculty Bataan Peninsula State UniversityDocument292 pagesBilly Ray A. Marcelo, BSN, RN Faculty Bataan Peninsula State UniversityDarell M. Book100% (1)
- Principles of Molecular Medicine - J. Larry Jamenson - Humana Press - 1998Document1,144 pagesPrinciples of Molecular Medicine - J. Larry Jamenson - Humana Press - 1998BOC100% (1)
- FQ, Probioticos - CochraneDocument80 pagesFQ, Probioticos - CochraneNoemi MartínezNo ratings yet
- The Salty Kiss (Sample PBL Case)Document9 pagesThe Salty Kiss (Sample PBL Case)c3624343No ratings yet
- Aiims Neet-Pg 2017 Pediatrics Mcqs 91-100Document4 pagesAiims Neet-Pg 2017 Pediatrics Mcqs 91-100DrHassan Ahmed Shaikh100% (1)
- PaedsDocument72 pagesPaedsOlivia Genevieve El JassarNo ratings yet
- Genetic DiseasesDocument2 pagesGenetic DiseasesDindaNo ratings yet
- Zheng Lixia 2020Document31 pagesZheng Lixia 2020Adin KerenNo ratings yet