Professional Documents
Culture Documents
Decreased Cardiac Output
Uploaded by
Christine MatasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Decreased Cardiac Output
Uploaded by
Christine MatasCopyright:
Available Formats
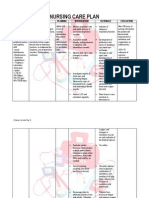
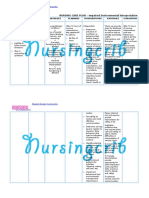
Assessment Subjective: Palaging mababa ang bp nya. As verbalized by his son.
Objectives: Increased heart rate (tachycardia), dysrhythmias, ECG changes Changes in BP (hypotension/hyp ertension) Extra heart sounds (S3, S4) Decreased urine output Diminished peripheral pulses Cool, ashen skin;
Diagnosis Decreased cardiac output related to decreased myocardial contractility
Planning Short Term: After 30 minutes of nursing intervention, the client will be able to: Patients lungs sounds will be clear to auscultation Patient will have no signs of dyspnea Patient will demonstrate an increase in activity intolerance Long Term: After 30 minutes of nursing intervention, the client will be able to: Patient will display hemodynamic stability (BP,
Intervention Assess patient respirations by observing respiratory rate and depth and use of accessory muscles Observe patient for restlessness, agitation, confusion and (late stages) lethargy
Rationale Increased respiratory rate and use of accessory muscles may be seen in patients with hypoxia Changes in behavior and mental status can be early signs of impaired gas exchange which will result from decreased cardiac output Crackles may indicate heart failure which can contribute to decreased cardiac output. Respiratory distress/failure often occurs as shock progresses. A positive hepatojugular reflex is indicative of rightsided heart failure Increasing lethargy, confusion, restlessness and / or irritability can be early signs of cerebral hypoxia from
Evaluation Goal Met. After 3 hours of nursing intervention the client will be able to: Patient has regular, even, non-labored respirations. Patient will be alert, oriented x 3 and calm Patients lungs sounds are clear to auscultation in all lobes Patient has normal hepatojugular reflex. Patient is awake, alert and oriented X3. Patient maintains baseline
Auscultate lungs for presence of normal or adventitious lung sounds
Assess patient for positive hepatojugular reflex
Assess for mental status changes.
diaphoresis Orthopnea, crackles, JVD, liver engorgement, edema Chest pain
cardiac output, urinary output and peripheral pulses WNL)
Weigh patient daily at same time with same clothing on same scale.
Observe patient for sleep apnea
Assess patient for chest pain or discomfort noting location, severity, duration, quality and radiation
Elevate legs when in sitting position and edematous extremities when at rest Monitor hourly urine output
decreased cardiac output Weight gain can be one of the earliest indicators of heart failure as a result of impaired ventricular pumping ability. An acute gain in weight of 1kg. can signal a l liter gain in fluid Sleep apnea is a common disorder in patients with chronic heart failure Chest pain is generally indicative of inadequate blood supply to the heart which can result in decreased cardiac output Improves venous return and increases cardiac output Decreased cardiac output results in decreased perfusion to the kidneys and decreased urine output.
weight or less daily Patient will have no episodes of sleep apnea Patient is free of chest pain. Patient will have decreased edema in legs Patient will have a minimum of 30ml/hr. urinary output Patient has normal heart sounds of S1 and S2 Patient will have normal sinus rhythm Patient will have strong, palpable peripheral pulses in all extremities
Urinary output < 30 ml/hr. indicates inadequate renal perfusion. Assess patient heart sounds Heart sounds may sound distant and have an S3 or S4 sound present with the presence of heart failure Heart irritability is common with conduction defects and/or ischemia from a poorly perfused heart (Tachycardia at rest, atrial fibrillation, bradycardia, or multiple dysrhythmias) Weak, thready peripheral pulses may reflect hypotension, vasoconstriction, shunting and venous congestion Pallor or cyanosis, cool moist skin and slow capillary refill time may be present from peripheral
Monitor patient for changes in heart rate and/or rhythm
Assess peripheral pulses
Observe patient for changes in skin color, moisture, temperature and capillary refill time
Patient will have normal skin color, be dry to touch and have capillary refill time of 3 seconds or less or 5 seconds or less (if patient is elderly) Patients oxygen saturation will remain at 93% or above at all times. Patient will get adequate rest in a stress-free environment. Patient and/or caregiver will verbalize an understandin g of patient medications
Administer supplemental Oxygen as indicated by cannula, mask, or ET/trach tube.
Promote rest
Educate patient and caregivers about the importance of taking prescribed medications at prescribed times
vasoconstriction and decreased oxygen saturation Supplemental oxygen helps to improve cardiac function by increasing available oxygen and reducing oxygen consumption. Rest and a quiet environment reduces a catecholamine-induced stress response and decreases cardiac workload thus increasing cardiac output Patient is often on multiple medications which can be difficult to manage, thus increasing the likelihood that medications can be missed or incorrectly used
and dosing schedule.
You might also like
- OCAMPO, Maria Cecilia R. BSN 3d2 - 8i / MS Nursing Care Plan Related To Hypercalcemia Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesOCAMPO, Maria Cecilia R. BSN 3d2 - 8i / MS Nursing Care Plan Related To Hypercalcemia Assessment Diagnosis Planning Intervention Rationale Evaluationchurva_freak433533% (9)
- Tachycardia NCPDocument2 pagesTachycardia NCPRemita Hutagalung50% (4)
- Ncp-Ineffective Tissue Perfusion (Aortic Stenosis)Document2 pagesNcp-Ineffective Tissue Perfusion (Aortic Stenosis)Daniel Vergara Arce67% (3)
- NCP: DysrhythmiasDocument12 pagesNCP: DysrhythmiasJavie100% (3)
- Nutrition NCPDocument3 pagesNutrition NCPMarielle Adrienne Bitancor100% (1)
- Ate Gara NCP (Activity Intolerance)Document2 pagesAte Gara NCP (Activity Intolerance)Kimsha ConcepcionNo ratings yet
- Nursing Care Plan 2Document2 pagesNursing Care Plan 2Isabel Barredo Del MundoNo ratings yet
- Decreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To CardiomyopathyDocument2 pagesDecreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To Cardiomyopathywen_pil75% (8)
- NCP 2 and Soapie 1Document5 pagesNCP 2 and Soapie 1narsD100% (1)
- Nursing Care Plan2 CVADocument4 pagesNursing Care Plan2 CVAhermesdave1No ratings yet
- Nursing Care Plan HF FinalDocument10 pagesNursing Care Plan HF FinalCristina L. JaysonNo ratings yet
- Maternal NursingDocument130 pagesMaternal NursingChristine MatasNo ratings yet
- Initiatives of FSSAIDocument27 pagesInitiatives of FSSAIAshok Yadav100% (2)
- NCPDocument9 pagesNCPTracy Camille EscobarNo ratings yet
- NCP PROPER Pain and Decreased Cardiac OutputDocument3 pagesNCP PROPER Pain and Decreased Cardiac OutputErienne Lae Manangan - CadalsoNo ratings yet
- NCP HypertensionDocument1 pageNCP HypertensionCharisse VillanuevaNo ratings yet
- CRF Fluid Volume Excess NCPDocument3 pagesCRF Fluid Volume Excess NCPchubbielitaNo ratings yet
- NCP For CTTDocument1 pageNCP For CTTJen Rhae LimNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanJayalakshmi David50% (2)
- Decreased Cardiac OutputDocument2 pagesDecreased Cardiac OutputEdrianne J.100% (2)
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue Perfusionsyderman999No ratings yet
- Hypertonic SolutionsDocument4 pagesHypertonic SolutionsVanessa PaguiriganNo ratings yet
- Decreased Cardiac OutputDocument2 pagesDecreased Cardiac OutputDheza Rodis Santos0% (1)
- NCP - Ineffective Airway ClearanceDocument4 pagesNCP - Ineffective Airway ClearanceKim Gabrielle Exene LeeNo ratings yet
- Student Nurses’ Community NURSING CARE PLAN – Renal FailureDocument2 pagesStudent Nurses’ Community NURSING CARE PLAN – Renal FailureAldrein GonzalesNo ratings yet
- NCP PTBDocument2 pagesNCP PTBMack Jhed AnarconNo ratings yet
- Multi Noduar Colloid GoiterDocument1 pageMulti Noduar Colloid GoiterVincent John Faller100% (1)
- Ncp-Impaired Verbal CommunicationDocument4 pagesNcp-Impaired Verbal CommunicationEzra TuanNo ratings yet
- NCPDocument2 pagesNCPsphinx809100% (2)
- NCPDocument2 pagesNCPDidith AbanNo ratings yet
- Managing Urinary Tract Obstruction Nursing InterventionsDocument8 pagesManaging Urinary Tract Obstruction Nursing Interventionsjyaba0% (1)
- Acute Pain Related To Tissue Trauma and InjuryDocument4 pagesAcute Pain Related To Tissue Trauma and Injuryprickybiik50% (2)
- Care Plan ExampleDocument2 pagesCare Plan Exampleincess27100% (1)
- NURSING CARE PLAN Decreased Cardiac Output FnaDocument2 pagesNURSING CARE PLAN Decreased Cardiac Output FnaAce Dioso Tubasco100% (1)
- NCP For CTTDocument2 pagesNCP For CTTKay D. BeredoNo ratings yet
- Assessment Diagnosis Planning Intervention Evaluation for Impaired Gas ExchangeDocument2 pagesAssessment Diagnosis Planning Intervention Evaluation for Impaired Gas ExchangeCharissa Magistrado De LeonNo ratings yet
- Altered Renal Perfusion CRFDocument4 pagesAltered Renal Perfusion CRFKristel Anne Nillo ZepolNo ratings yet
- Nursing Care PlanDocument5 pagesNursing Care Planruggero07100% (2)
- Nursing Care Plan For Impaired Environmental Interpretaion NCPDocument4 pagesNursing Care Plan For Impaired Environmental Interpretaion NCPderic100% (2)
- Nursing Interventions for Ineffective Breathing PatternDocument1 pageNursing Interventions for Ineffective Breathing PatternnikkilyceeNo ratings yet
- Hyperthermia NCPDocument3 pagesHyperthermia NCPJayr DiazNo ratings yet
- Nursing Care Plan 1 DiagDocument4 pagesNursing Care Plan 1 Diagguysornngam100% (1)
- Nursing Care PlanDocument13 pagesNursing Care PlanCris Solis33% (3)
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- Cardiovascular Disease NCPDocument5 pagesCardiovascular Disease NCPShyla ManguiatNo ratings yet
- NCP PTBDocument2 pagesNCP PTBKath TalubanNo ratings yet
- NCP Ch31 p991-992Document2 pagesNCP Ch31 p991-992Ala'a Abd Mansor100% (2)
- NCP LocDocument2 pagesNCP LocMel RodolfoNo ratings yet
- Knowledge Deficit Related To HypertensionDocument2 pagesKnowledge Deficit Related To HypertensionChenee Mabulay100% (1)
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionDiane ReyNo ratings yet
- NCP For Ears Nose ThroatDocument1 pageNCP For Ears Nose ThroatMcmac YangoNo ratings yet
- NCP For OxygenationDocument6 pagesNCP For OxygenationChriz LechNo ratings yet
- NCP Impaired Gas Exhange Related To Alveolar Wall Destruction EMPHYSEMADocument5 pagesNCP Impaired Gas Exhange Related To Alveolar Wall Destruction EMPHYSEMAMa. Elaine Carla Tating50% (2)
- Assessment Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationDocument4 pagesAssessment Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationKrisha Miel DomedeNo ratings yet
- Reflective Journaling 1Document12 pagesReflective Journaling 1Nosheen ShahNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Respiratory Failure Results From Inadequate Gas ExchangeDocument7 pagesRespiratory Failure Results From Inadequate Gas ExchangeJiezl Abellano AfinidadNo ratings yet
- Lectura CardiologiaDocument8 pagesLectura CardiologiaNatalia Castellanos CoteNo ratings yet
- Case PresDocument6 pagesCase PresCharm TanyaNo ratings yet
- Heart Failure Care PlanDocument6 pagesHeart Failure Care PlanOlivia Winkler StuartNo ratings yet
- Elevated Blood PressureDocument3 pagesElevated Blood PressureSean MercadoNo ratings yet
- Cardiovascular System: AnatomyDocument19 pagesCardiovascular System: AnatomyStephanie MacVeighNo ratings yet
- Covid Compensation MatasDocument3 pagesCovid Compensation MatasChristine MatasNo ratings yet
- 5D4N Winter in Osaka Package 2022 PDFDocument3 pages5D4N Winter in Osaka Package 2022 PDFChristine MatasNo ratings yet
- ManagementDocument5 pagesManagementChristine MatasNo ratings yet
- FNCP Table, Intro..docxcDocument5 pagesFNCP Table, Intro..docxcChristine MatasNo ratings yet
- 5D4N Winter in Osaka Package 2022 PDFDocument3 pages5D4N Winter in Osaka Package 2022 PDFChristine MatasNo ratings yet
- Pink EyeDocument14 pagesPink EyeChristine MatasNo ratings yet
- Nutrion & Diet Therapy: Group 2A Charlene Mae B. Matas Charlene Mae B. MatasDocument3 pagesNutrion & Diet Therapy: Group 2A Charlene Mae B. Matas Charlene Mae B. MatasChristine MatasNo ratings yet
- OSCE Training and SupportDocument1 pageOSCE Training and SupportChristine MatasNo ratings yet
- Nursing Pharmacology Dosage Calculations GuideDocument101 pagesNursing Pharmacology Dosage Calculations GuideChristine Matas100% (1)
- Histograms Are Used To Show Numerical Information in Graphic FormDocument3 pagesHistograms Are Used To Show Numerical Information in Graphic FormChristine MatasNo ratings yet
- ManagementDocument5 pagesManagementChristine MatasNo ratings yet
- GROUPDocument2 pagesGROUPChristine MatasNo ratings yet
- Mental Status ExaminationDocument7 pagesMental Status ExaminationChristine MatasNo ratings yet
- English 113fDocument2 pagesEnglish 113fChristine MatasNo ratings yet
- EquilibriumDocument1 pageEquilibriumChristine MatasNo ratings yet
- Drug StudyDocument8 pagesDrug StudyChristine MatasNo ratings yet
- English 113fDocument2 pagesEnglish 113fChristine MatasNo ratings yet
- Drugs Part 1Document5 pagesDrugs Part 1Christine MatasNo ratings yet
- Case Pres - NCPDocument14 pagesCase Pres - NCPChristine MatasNo ratings yet
- A Sudden Redness of The Skin Is Known As: Flush: Place The Patient's Feet in DorsiflexionDocument1 pageA Sudden Redness of The Skin Is Known As: Flush: Place The Patient's Feet in DorsiflexionChristine MatasNo ratings yet
- Barriers and obstacles to adult learning in healthcareDocument2 pagesBarriers and obstacles to adult learning in healthcareChristine MatasNo ratings yet
- Significance of The StudyfDocument1 pageSignificance of The StudyfChristine MatasNo ratings yet
- F NCPDocument1 pageF NCPChristine MatasNo ratings yet
- Summary of The Seven Exchange ListsDocument9 pagesSummary of The Seven Exchange ListsChristine MatasNo ratings yet
- Principal Uses of NounsDocument18 pagesPrincipal Uses of NounsChristine Matas100% (1)
- General Survey TECHNIQUE Actual Findings Normal Findings AnalysisDocument21 pagesGeneral Survey TECHNIQUE Actual Findings Normal Findings AnalysisJerry Joseph B. AbordoNo ratings yet
- Pathophysiology of Rheumatic Heart Disease to CardiomegalyDocument2 pagesPathophysiology of Rheumatic Heart Disease to CardiomegalyRj Avila100% (1)
- Seminar on Concepts and Foundations of RehabilitationDocument13 pagesSeminar on Concepts and Foundations of Rehabilitationamitesh_mpthNo ratings yet
- Indian ListenerDocument103 pagesIndian ListenerTareq Aziz100% (1)
- IP Sterility TestingDocument6 pagesIP Sterility TestingVarghese100% (3)
- WHO 1991 128 PagesDocument136 pagesWHO 1991 128 PagesLilmariusNo ratings yet
- 2017-18 Undergraduate Catalog PDFDocument843 pages2017-18 Undergraduate Catalog PDFguruyasNo ratings yet
- 6/27/2019 NO NAMA BARANG QTY UOM Batch EDDocument8 pages6/27/2019 NO NAMA BARANG QTY UOM Batch EDRedCazorlaNo ratings yet
- 4926-02 L2 Certificate Qualification Handbook v1 PDFDocument116 pages4926-02 L2 Certificate Qualification Handbook v1 PDFforumuse3bNo ratings yet
- Textbook of Clinical Occupational and Environmental MedicineDocument4 pagesTextbook of Clinical Occupational and Environmental MedicineAmos SiraitNo ratings yet
- Sefcik Ashley Resume 2018Document1 pageSefcik Ashley Resume 2018api-394215168No ratings yet
- BarryKuebler Lesson1 AssignmentDocument4 pagesBarryKuebler Lesson1 AssignmentBarry KueblerNo ratings yet
- KENCAP Changzhou 2013Document19 pagesKENCAP Changzhou 2013KencapchangzhouNo ratings yet
- Safety of Low-Dose Oral Minoxidil for Hair Loss: A Study of 1404 PatientsDocument8 pagesSafety of Low-Dose Oral Minoxidil for Hair Loss: A Study of 1404 PatientsLuisNo ratings yet
- Class III Cavity Treatment (Procedure, Materials)Document2 pagesClass III Cavity Treatment (Procedure, Materials)Manos KritikosNo ratings yet
- Pterygomandibular Space DepthDocument10 pagesPterygomandibular Space DepthBharathNo ratings yet
- Past PE Papers Viva TopicsDocument29 pagesPast PE Papers Viva TopicsLouis MasonNo ratings yet
- Kepler and AlchemyDocument13 pagesKepler and AlchemyMartha100% (1)
- Nutrition Care Process NoteDocument3 pagesNutrition Care Process Noteapi-242497565No ratings yet
- Cerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluidDocument5 pagesCerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluiderickNo ratings yet
- Phobic EncounterDocument1 pagePhobic EncounterEmanuel PeraltaNo ratings yet
- Ancient Indian yoga techniqueDocument12 pagesAncient Indian yoga techniqueRandhir SinghNo ratings yet
- Jubilant Life Sciences Receives ANDA Approval For Rosuvastatin Calcium Tablets (Company Update)Document3 pagesJubilant Life Sciences Receives ANDA Approval For Rosuvastatin Calcium Tablets (Company Update)Shyam SunderNo ratings yet
- Parallax Xray For Maxillary CanineDocument3 pagesParallax Xray For Maxillary Canineabdul samad noorNo ratings yet
- Hipraviar ClonDocument2 pagesHipraviar Clonst_richard04100% (2)
- Drug Study HydrocodoneDocument1 pageDrug Study HydrocodoneYlrenne DyNo ratings yet
- 515Document972 pages515solecitodelmarazul100% (6)
- Radial Club Hand TreatmentDocument4 pagesRadial Club Hand TreatmentAshu AshNo ratings yet
- Stress Dose SteroidsDocument4 pagesStress Dose SteroidsTitien fitria sholihati100% (1)