Professional Documents
Culture Documents
Preop HO
Uploaded by
apocruCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Preop HO
Uploaded by
apocruCopyright:
Available Formats
PREOPERATIVEMEDICALEVALUATION I. PreoperativeMedicalEvaluation: primarycarephysicianbeingaskedto: 1.) Establishbaselinehistoryandphysical. 2.) Identifypreviouslyundetecteddisease. 3.) Assessoperativerisk.Shouldthepatientproceedwithelectivesurgery? 4.) Makespecificrecommendationsregardingpreoperativetreatment thatmightlowertheriskofsurgery. 5.) Givesuggestionsregardingintraoperativeandpostoperativecare. II.
History: Age seelabalgorithmforadditionalstudies(page2) CC whattypeofoperation whattypeofanesthesia
HarryColt 8/26/09
PMHx surg problemswithanesthesia,DVT,PE med diabetes,COPD,bleedingdisorders,cardiac,sleepapnea,H/Otraumaor surgerytoback,?needforantibioticprophylaxis OB LMP allergies meds prescription OTC Herbal(seereference#2) SHx tobacco,ETOH,druguse FHx malignanthyperthermia(autosomaldominant),bleedingdisorders, diabetes,ASCVD ROS thorough,esp.LMP,cardiovascular,pulmonary,functionalstatus Advanceddirectives/CodeStatus III. P.E.: Thoroughesp.examinationofairwayandmouth,ROMofneck,cardiovascular pulmonary. IV. Lab: (MedClinNorthAm 77:289307) routineornonselectivelabtestingnotjustifiable screeningshouldbebasedonage,coexistentillness,typeofsurgery severalfactorsimportanttoconsiderwhendecidingwhethertoorderlab testsinasymptomaticindividuals 1.) Istheresignificantlikelihoodtestwillbeabnormal? 2.) Willdiscoveryofabnormaltestresultleadtotreatmentsor investigationsthatreducethepatient'ssurgicalrisk? 3.) Isitimportanttogetabaselinetestforteststhatmayberepeatedafter surgery? LabTestinginAsymptomaticLowRiskPatients: and
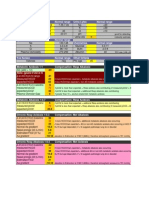
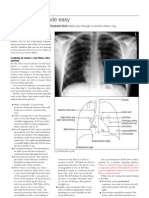
Hgb/HCT recommendedinpatientsbeforemajorsurgeryexpectedtohave highbloodloss notrecommendedforminorsurgeryinasymptomaticindividuals WBC notrecommended Platelets notrecommended Lytes notrecommended Renalfunction asymptomaticrenalinsufficiencymorecommonwithage, andisrelatedtoperioperativemorbidity.Management decisionsbasedonrenalfunction.Therefore,recommended inpatientover50*scheduledformajorelectivesurgery. Glucose notrecommended* LFTs notrecommended Coags abnormalitiesrareinpatientswithoutcluesonHxorPx notrecommended UA notrecommended CXR debatable.Somerecommendinpatients>60.Otherssuggest CXRonlyifHx+Pxsuggestsitorintrathoracicsurgeryplanned EKG EKGformalepatient>45*,femalepatient>50* Pregnancytestanyquestionofpregnancy Otherthoughts: Ifdementiaorhistoryinadequate,routinetestingmorejustifiable. Somestudiessuggestpriortestresults(<4monthsold*)adequate,ifpriortest normalandnochangeinstatus. InSummary: Routinepreoperativetestingbeforeelectivesurgerynotjustified,becausethe frequencyofunexpectedabnormalitiesthatchangemanagementissolow. Onepossiblealgorithm: Test/Age H&P CXR EKG:Males Females Cr/BUN HCT PT/PTT 040 X 4045 X 4549 X X* 5059 X 60+ X X* X* X
X* X* X* beforemajorsurgeryexpectedtohavehighbloodloss notindicatedinotherwisehealthypatients
V. PreoperativePulmonaryEvaluation: Pulmonarycomplicationsareimportantcauseofpostoperativemorbidity
andmortality.Includeaspiration,pneumonia,atelectasis,pulmonary edema,PE. Riskfactors: siteofoperation(mostimportant),durationofsurgeryand anesthesia,tobaccouse,chroniclungdisease,pulmonaryhypertension, obstructivesleepapnea. Siteofoperation: pulmonarycomplicationshigherassurgerynearsthediaphragm PPC1033%ofupperabdominalsurgery,010%lowerabdominalsurgery Generalanesthesiacauses10%dropinFRCduetoanestheticandmuscle relaxant Whenupperabdominalorganshandled,diminisheddiaphragmatic contractilitylastsfordays anestheticanddiaphragmaticparesistogethercause2050%decreasein FRCandexpiratoryflows.Maylastuptotwoweeks. Postoperatively:higherRR,lowerTV.Shallowrespirationscause atelectasis 1030%dropinp02believedduetoV/Qmismatches Innormalpatient,thesechangesunimportant.Incompromisedpatient, thesechangescanbecrucial. Whatcanwedotoreducepulmonarycomplications? Reductionofriskfactors(preoperatively) Tobaccoabuse stopsmoking8weekspriortosurgery. COPD smokingcessation,optimizelungfunction(Ipratrupiumortiotropium, betaagonistprn,steroidifindicated),lungexpansion Ifinfectedsputum,antibioticsanddelaysurgery. Inhighriskpatientsincentivespirometry15min.QIDpreoperatively. Reductionofriskfactors(postoperatively) deepbreathingexercisesorincentivespirometry paincontrol earlymobilization
AlgorithmforPreoperativePulmonaryEvaluation
4 Possiblepreoperativemeasurestoimprovepulmonaryfunction: 1) smokingcessation(8weeks) 2) bronchodilators 3) incentivespirometry
Postoperativemeasurestoimprovefunction: 1) incentivespirometry 2) earlymobilization 3) paincontrol Whoneedspreoperativepulmonaryfunctiontesting?(seebelow) Veryfew.Onlythosewith: 1) Unexplaineddyspneaorexercisetolerance 2) ThosewithCOPDorasthmaandunclearwhetherattheirbaseline 3) plannedlungresection
VI.
PreoperativeCardiovascularTesting: 1/3to1/2ofperioperativedeathsarecardiac. Manyrecentstudiesdevisedtolookathowwecanbetterpredictwhowill
developthesecardiacevents,sothatwecanintervenemedicallyor surgicallypreoperatively. A. MultifactorialRiskStudies: 1.) Goldman bestknown,mostwidelyused.Lookedat1,001patients whounderwentnoncardiacsurgeryinthelate70's.Cameupwith GoldmanCriteriaandriskcategories: GoldmanCriteria
S3galloporjugularvenousdistentiononpreoperative physicalexamination Transmuralorsubendocardialmyocardialinfarctioninthe previous6months Prematureventricularbeats,morethan5/mindocumented atanytime Rhythmotherthansinusorpresenceofprematureatrial contractionsonlastpreoperativeelectrocardiogram Ageover70years Emergencyoperation Intrathoracic,intraperitonealoraorticsiteofsurgery Evidenceofimportantvalvularaorticstenosis Poorgeneralmedicalcondition (K3,HCO320,BUN>50,Cr>3,pO2<60,pCO2>40 Abnormalliver(GOT),orbedridden) CardiacMorbidity ClassI(0to5points) ClassII(6to12points) ClassIII(12to25points) ClassIV(26ormore) 0.7% 5% 11% 22%
Points 11 10 7 7 5 4 3 3 3
CardiacDeath 0.2% 2% 2% 56%
Predictedcomplicationsofclass4well Lowsensitivityforidentifyinghighriskpatientintheintermediateriskgroups
2.) Detsky addedanginaclasses,remoteMI,andCHF B. FunctionalCapacity: canhelpassesscardiacriskbeforenoncardiacsurgery C. SugerySpecificRisk D. Algorithm(ACC/AHA)seebelow 1.)includesurgencyofsurgery,majoractivecardiacconditions,surgery specificrisk,andfunctionalcapacity
ACC/AHAGuidelines(seep6ofhandout)
5Keyquestions(steps) 1) Isthenoncardiacsurgeryurgent? 2) Isthereamajoractivecardiaccondition?(seetable2,p9) 3) Itthepatientundergoinglowrisksurgery?(seetable3,p10) 4) Doesthepatienthavegoodfunctionalcapacitywithoutsymptoms?(seetable4, p10) 5) ClinicalRiskFactors(seetable5,p10) a) Noneproceedwithsurgery b) 1or2proceedwithsurgerywithBetaBlockers c) 3ormoreconsidercardiactestingifitwillchangemanagement;beta blockers E. ReducingPostoperativeCardiacComplications:BBlockers KEYPOINT Bblockersrecommendedforpatientswithknownorhighriskfor coronaryarterydisease.Canreducecardiaccomplicationsignificantly. aimforHR<55(seesampleMGHprotocol,page11) F.Possiblyreducingpostoperativecardiaccomplications 1.)statinsinstudy,theyreduceabsolutemortality1% startstatinsifindicatedlongterm G.Summary: Useperioperativebetablockersifpatienthighriskforheartdisease Considerpreoperativecardiactestingonlyifitwillchangemanagement VII. SpecificSituations: A. Diabetes littledataonperioperativecare Theoretically:elevatedglucosescancausediminishedleukocyte function,increasedinfectionrate,delayedwoundhealing. Aimforglucoses<200. 1.) DietControlled nodextroseorinsulin.Followglucose. 2.) OralAgents Holdoralhypoglycemicthedayofsurgery(holdmetformin for2days). Ifwellcontrolledandshortsurgery,maynotneedinsulin Ifpoorlycontrolled,variablerateIVinsulininfusion(seetable6,page12) Restartoralhypoglycemicwheneatingnormally. 3.) IDDM VariablerateIVinsulininfusion(seetable6,page12) Aimforglucoseof120180 B. Hypertension mildmoderatediastolicHTN(<110)adjustmedsduringtheseveral weekspriortosurgery.Acutecontrolnotadvisable. poorlycontrolledHTNpostponeelectivesurgeryuntilBP<180/110. Iftimeallows,bringBPto140/90overseveralweeks. Takemedsthemorningofsurgery(exceptdiuretic*). C. Anemia Noabsolutethresholdfortransfusions.Overallclinicalpictureiswhat
isimportant.Inhigherriskpatient,keepHgbabove9*, D. AdrenalInsufficiency If3weeksofsuppressivedoses(Prednisone>7.5QD)inpast6months, needstresssteroiddoses. E. Anticoagulation IfonCoumadin(INR23):stopCoumadinapproximately4daysbefore surgery Considerpreoperativeanticoagulation(LMWHorHeparin)forthoseat highestriskofthromboembolism(seeTable8,pg12).Postoperativelycan heparinize.DiscusstimingofstartingHeparinwithsurgeon. D/Cnonsteroidalsatleastoneweekbeforesurgery. D?CASAatleastoneweekpriortosurgery*(unlesscoronarystent). ifpriorPCI,seetable9,page14 F. DVT/PEProphylaxis Prophylaxis:Warfarin,LMWH,SQHeparin,externalpneumatic compression,earlyactivity. G. EndocarditisProphylaxis Efficacyofprophylaxisunproven. AHA2007Guidelines:antibioticsforhighriskcardiac abnormalities(prostheticheartvalves,priorendocanditis,certain congenitalheartdisease)undergoinghighriskprocedure(seeTable7, p.12). VIII. Summary: Preoperativemedicalevaluationismorethana"routine"H&P.Doboth thoroughandfocusedH&P,orderappropriatelabtests,decidewhether furthercardiovascularorpulmonarytestingindicated,makespecific recommendationsregardingpreoperativeandperioperativecare.
IX.
Cases: 1.) L.T.isa68yearoldmanwithdiabetes,COPD,osteoarthritis,whois scheduledforhipreplacementintwoweeks.Hehasa56packyear smokinghistory.Medsinclude:glyburide,albuterol,ibuprofen.On exam,hehasoccasionalwheezes,barrelshapedchest. 2.) D.R.isa71yearoldwomanwithahistoryofhypertensionscheduledfor carotidendarterectomy.Medsincludebenazepril.ExamnotableforBPof 160/100,rightcarotidbruit.EKGshowsQwavesinferiorly.LastEKG8 yearsagounremarkable.
Whatelsedoyouwanttoknow? Anyfurthertesting? Whatareyourrecommendations?
9 ForAdditionalInfo: 1.) ACC/AHAGuidelinesonPerioperativeCardiovascularEvaluation:ExecutiveSummary. Anesthesia&Analgesia106(3):685712,2008. 2.) AngLeeMKetall.HerbalMedicinesandPerioperativeCare.JAMA286(2):208216,2001. 3.) BepojeSRetal.PerioperativeEvaluationofthePatientwithPulmonaryDisease.Chest 132(5):16371645,2007. 4.) FloodC,FleisherLA.PreparationoftheCardiacPatientforNoncardiacSurgery.AmerFam Phys75(5):656665,2007. 5.) MarksJB.PerioperativeManagementofDiabetes.AmFamPhys67(1):93100,2003. 6.) MacphersonDS.PreoperativeLaboratoryTesting:ShouldanyTestbe"Routine"Before Surgery?MedClinNorthAm77(2):289207,1993.
Table3. Cardiac Risk Stratification for Noncardiac Surgical Procedures**
10
Highrisk(reportedcardiacriskoften>5percent) Emergentmajoroperations,particularlyintheelderly Aorticandothermajorvascularsurgery Peripheralvascularsurgery Anticipatedprolongedsurgicalproceduresassociatedwithlargefluidshiftsand/orbloodloss Intermediaterisk(reportedcardiacriskgenerally<5percent) Carotidendarterectomy Headandnecksurgery Intraperitonealandinthrathoracicsurgery Orthopedicsurgery Prostatesurgery Low risk (reported cardiac risk generally < 1 percent) = Endoscopicprocedures Superficialprocedures Cataractsurgery Breastsurgery **Combinedincidenceofcardiacdeathandnonfatalmyocardialinfarction. =Donotgenerallyrequirefurtherpreoperativecardiactesting.
Table4. FunctionalCapacityAssessmentfromClinicalHistory Excellent(Activitiesrequiring>7METs) Carry24lbup8steps Carryobjectsthatweigh80lb Outdoorwork(shovelsnow,spadesoil) Recreation(ski,basketball,squash,handball,jog/walk5mph) Moderate(Activityrequiring>4METsbut<7METs) Havesexualintercoursewithoutstopping Walkat4mphonlevelground Outdoorwork(garden,rake,week) Recreation(rollerskate,dance,foxtrot) Poor(Activityrequiring<4METs) Shower/dresswithoutstopping,stripandmakebed,dusting,dishwashing Walkat2.5mphonlevelground Outdoorwork(cleanwindows) Recreation(playgolf,bowl)
Table5 ClinicalRiskFactors*CardiacRiskIndex HLoischemicheartdisease HLocompensatedorpriorheartfailure HLocerebrovasculardisease diabetesmellitus renalinsufficiency
11
12
13
14
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Clinical Examination in Surgery 3rd YearDocument4 pagesClinical Examination in Surgery 3rd YearapocruNo ratings yet
- Lego 2013 CarDocument45 pagesLego 2013 Carapocru100% (1)
- Fuck You ScribdDocument1 pageFuck You ScribdapocruNo ratings yet
- Breast BiopsyDocument2 pagesBreast BiopsyapocruNo ratings yet
- 05 22Document2 pages05 22apocruNo ratings yet
- Shipping Procedure and Measuring GuideDocument2 pagesShipping Procedure and Measuring GuideapocruNo ratings yet
- History Taking ExaminationDocument7 pagesHistory Taking ExaminationIndunil AnuruddhikaNo ratings yet
- Welcome Booklet 2013Document17 pagesWelcome Booklet 2013apocruNo ratings yet
- Acute PancreatitisDocument48 pagesAcute PancreatitisapocruNo ratings yet
- Otitis MediaDocument4 pagesOtitis MediaapocruNo ratings yet
- Application FormDocument1 pageApplication FormapocruNo ratings yet
- Acid Base EquationsDocument21 pagesAcid Base EquationsBen JonesNo ratings yet
- Surgery State Exam Questions 24Document11 pagesSurgery State Exam Questions 24apocruNo ratings yet
- 100 MeningitisDocument4 pages100 MeningitisapocruNo ratings yet
- March 2013 April 2013 : Feb 2013 Apr 2013 Mar 2013 May 2013Document1 pageMarch 2013 April 2013 : Feb 2013 Apr 2013 Mar 2013 May 2013apocruNo ratings yet
- Google Mother's DayDocument1 pageGoogle Mother's DayapocruNo ratings yet
- Acid Base EquationsDocument21 pagesAcid Base EquationsBen JonesNo ratings yet
- Abortionsource 100605123737 Phpapp01Document38 pagesAbortionsource 100605123737 Phpapp01Erina Erichan OtoNo ratings yet
- ShockDocument9 pagesShockapocruNo ratings yet
- Paediatric Basic Life Support: Resuscitation Council (UK)Document15 pagesPaediatric Basic Life Support: Resuscitation Council (UK)Wicaksono Sigit PNo ratings yet
- March 2013 : Sun Mon Tue Wed Thu Fri SatDocument4 pagesMarch 2013 : Sun Mon Tue Wed Thu Fri SatapocruNo ratings yet
- 2010 Resuscitation GuidelinesDocument157 pages2010 Resuscitation GuidelinesapocruNo ratings yet
- Conservative Management of Chronic Renal FailureDocument45 pagesConservative Management of Chronic Renal FailureapocruNo ratings yet
- STDDocument2 pagesSTDapocruNo ratings yet
- 2010 Resuscitation GuidelinesDocument157 pages2010 Resuscitation GuidelinesapocruNo ratings yet
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaNo ratings yet
- Quiz RenalDocument81 pagesQuiz RenalMedShare86% (14)
- Quiz Pharmacology Part 2 of 2Document54 pagesQuiz Pharmacology Part 2 of 2MedShare92% (25)
- Quiz PhysiologyDocument46 pagesQuiz PhysiologyMedShare78% (9)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2005 Magnetom Flash 1Document96 pages2005 Magnetom Flash 1Herick Savione100% (1)
- ItoprideDocument2 pagesItoprideLesValenzuelaNo ratings yet
- Model Paper ADocument7 pagesModel Paper AAndrewwwCheahNo ratings yet
- Bethesda 14Document12 pagesBethesda 14BegognaAnguloCruzado100% (1)
- Mergency Medicine, Second Edition: 60 Acid-Base DisordersDocument21 pagesMergency Medicine, Second Edition: 60 Acid-Base DisordersLukman NurfauziNo ratings yet
- Stroke (Brain Attack)Document16 pagesStroke (Brain Attack)Nhayr Aidol100% (1)
- Erotic CountertransferenceDocument3 pagesErotic CountertransferenceVictor Gan100% (2)
- Rehabilitation of Spinal Cord Injuries: Kemal Nas, MD, Professor, Series EditorDocument10 pagesRehabilitation of Spinal Cord Injuries: Kemal Nas, MD, Professor, Series EditorMuhammad AbduhNo ratings yet
- Health Assessment Portfolio Course SummaryDocument3 pagesHealth Assessment Portfolio Course Summaryapi-507520601No ratings yet
- SATO METHOD: Unique Qigong Originated in Japan (Part 1)Document18 pagesSATO METHOD: Unique Qigong Originated in Japan (Part 1)kkkanhaNo ratings yet
- Asuhan Keperawatan Pada Pasien Dengan Chronic Kidney DiseasesDocument24 pagesAsuhan Keperawatan Pada Pasien Dengan Chronic Kidney DiseasestidaktahudiriNo ratings yet
- Fundamentals of Nursing ReviewerDocument28 pagesFundamentals of Nursing ReviewerJamaica Manuel Iglesias100% (1)
- Special - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta StudentsDocument23 pagesSpecial - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta Studentsrizqi100% (1)
- Intertrigo Facts: Obesity ItchingDocument3 pagesIntertrigo Facts: Obesity Itchingyyfan98No ratings yet
- Lithoskop Product BrochureDocument20 pagesLithoskop Product BrochureJaseel AkNo ratings yet
- Serial Sampling of Serum Protein Biomarkers For Monitoring Human Traumatic Brain Injury Dynamics: A Systematic ReviewDocument23 pagesSerial Sampling of Serum Protein Biomarkers For Monitoring Human Traumatic Brain Injury Dynamics: A Systematic Reviewsatyagraha84No ratings yet
- Fundamentals of ICU Rehab: Christiane Perme, PT CCS Speaker BiographyDocument2 pagesFundamentals of ICU Rehab: Christiane Perme, PT CCS Speaker Biographyapi-250709992No ratings yet
- ParacetamolDocument24 pagesParacetamolFriné MirandaNo ratings yet
- Truncus ArteriosusDocument19 pagesTruncus ArteriosusHijaz Al-YamanNo ratings yet
- Viapath JobDocument6 pagesViapath JobRebeca UrseNo ratings yet
- DMNCP - Imbalanced Nutrition Less Than Body RequirementsDocument1 pageDMNCP - Imbalanced Nutrition Less Than Body RequirementsMel Izhra N. MargateNo ratings yet
- Structured Clinical Interview For DSM-IV Axis I DisordersDocument223 pagesStructured Clinical Interview For DSM-IV Axis I DisordersΕιρηνη Κουτσοδοντη100% (2)
- Erb's PalsyDocument18 pagesErb's PalsyMegha PataniNo ratings yet
- CCRN-PCCN-CMC Review Cardiac Part 2Document21 pagesCCRN-PCCN-CMC Review Cardiac Part 2Giovanni Mictil100% (1)
- Transnasal Esophagoscopy - Overview, Indications, Contraindications PDFDocument8 pagesTransnasal Esophagoscopy - Overview, Indications, Contraindications PDFRizqi Karima PutriNo ratings yet
- Assignment On PhototherapyDocument10 pagesAssignment On PhototherapyMital Patel100% (3)
- Ornap 2012Document2 pagesOrnap 2012Harby Ongbay AbellanosaNo ratings yet
- Sleep Disorders and Sleeping ProblemsDocument71 pagesSleep Disorders and Sleeping Problemsdeo2002No ratings yet
- Factors Influencing Bioavailability of Drugs PDFDocument2 pagesFactors Influencing Bioavailability of Drugs PDFRoy50% (2)