Professional Documents
Culture Documents
Metabolic Functions of The Liver
Uploaded by
Aizat KamalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metabolic Functions of The Liver
Uploaded by
Aizat KamalCopyright:
Available Formats
Metabolic Functions of the Liver (Biochemistry)
Hepatocytes are metabolic super-achievers in the body. They play critical roles in synthesizing molecules that are utilized elsewhere to support homeostasis, in converting molecules of one type to another, and in regulating energy balances. If you have taken a course in biochemistry, you probably spent most of that class studying metabolic pathways of the liver. At the risk of damning by faint praise, the major metabolic functions of the liver can be summarized into several major categories: Carbohydrate Metabolism It is critical for all animals to maintain concentrations of glucose in blood within a narrow, normal range. Maintenance of normal blood glucose levels over both short (hours) and long (days to weeks) periods of time is one particularly important function of the liver. Hepatocytes house many different metabolic pathways and employ dozens of enzymes that are alternatively turned on or off depending on whether blood levels of glucose are rising or falling out of the normal range. Two important examples of these abilities are:
Excess glucose entering the blood after a meal is rapidly taken up by the liver and sequestered as the large polymer, glycogen (a process called glycogenesis). Later, when blood concentrations of glucose begin to decline, the liver activates other pathways which lead to depolymerization of glycogen (glycogenolysis) and export of glucose back into the blood for transport to all other tissues.
When hepatic glycogen reserves become exhausted, as occurs when an animal has not eaten for several hours, do the hepatocytes give up? No! They recognize the problem and activate additional groups of enzymes that begin synthesizing glucose out of such things as amino acids and non-hexose carbohydrates (gluconeogenesis). The ability of the liver to synthesize this "new" glucose is of monumental importance to carnivores, which, at least in the wild, have diets virtually devoid of starch.
Fat Metabolism Few aspects of lipid metabolism are unique to the liver, but many are carried out predominantly by the liver. Major examples of the role of the liver in fat metabolism include:
The liver is extremely active in oxidizing triglycerides to produce energy. The liver breaks down many more fatty acids that the hepatocytes need, and exports large quantities of acetoacetate into blood where it can be picked up and readily metabolized by other tissues.
A bulk of the lipoproteins are synthesized in the liver. The liver is the major site for converting excess carbohydrates and proteins into fatty acids and triglyceride, which are then exported and stored in adipose tissue. The liver synthesizes large quantities of cholesterol and phospholipids. Some of this is packaged with lipoproteins and made available to the rest of the body. The remainder is excreted in bile as cholesterol or after conversion to bile acids.
Protein Metabolism The most critical aspects of protein metabolism that occur in the liver are:
Deamination and transamination of amino acids, followed by conversion of the nonnitrogenous part of those molecules to glucose or lipids. Several of the enzymes used in these pathways (for example, alanine and aspartate aminotransferases) are commonly assayed in serum to assess liver damage. Removal of ammonia from the body by synthesis of urea.Ammonia is very toxic and if not rapidly and efficiently removed from the circulation, will result in central nervous system disease. A frequent cause of such hepatic encephalopathy in dogs and cats are malformations of the blood supply to the liver called portosystemic shunts. Synthesis of non-essential amino acids. Hepatocytes are responsible for synthesis of most of the plasma proteins. Albumin, the major plasma protein, is synthesized almost exclusively by the liver. Also, the liver synthesizes many of the clotting factors necessary for blood coagulation .
PHYSIOLOGY OF BILIRUBIN PRODUCTION
Bilirubin is a bile pigment produced by the breakdown of haem and reduction of biliverdin. Unconjugated bilirubin is insoluble in plasma unless bound to protein, mainly albumin. Salicylates, sulphonamides, non-esterified fatty acids and reduced pH levels result in decreased protein-binding of unconjugated bilirubin. Normally, 95% of the circulating bilirubin is unconjugated. The bilirubin-albumin complex is dissociated by receptors on hepatocytes. The albumin remains in the plasma. The bilirubin is taken into the hepatocyte and conjugated by the enzyme bilirubin UDP-glucuronyl transferase to form bilirubin diglucuronide. It is this water-soluble glucuronate derivative which is excreted into the biliary system. In the gut, principally the colon, bilirubin glucoronides are degraded by bacteria and converted into a mixture of compounds, known as urobilinogen or stercobilinogen; these are water soluble.
Most of the urobilinogen is excreted in the faeces where it is oxidised to urobilin which is brown. Some is reabsorbed into the liver where it is re-excreted. When the amount of urobilinogen is increased, some passes into the systemic circulation and is excreted in the urine.
You might also like
- Treatment of Cardiac Arrest in The Hyperbaric Environment - Key Steps On The Sequence of Care - Case ReportsDocument8 pagesTreatment of Cardiac Arrest in The Hyperbaric Environment - Key Steps On The Sequence of Care - Case Reportstonylee24No ratings yet
- Managing obstetric emergenciesDocument9 pagesManaging obstetric emergenciesSnurah Idris100% (1)
- Medications and Antidotes ChartDocument2 pagesMedications and Antidotes ChartkNo ratings yet
- Oman New Health Application FormDocument3 pagesOman New Health Application FormAravind AlavantharNo ratings yet
- American River Cycling Club: W M H R ?Document1 pageAmerican River Cycling Club: W M H R ?Jotaro KujoNo ratings yet
- United Home Whitfield's OintmentDocument5 pagesUnited Home Whitfield's OintmentWalidur Rahman MridulNo ratings yet
- Digestion and Absorption of Lipids: A Comprehensive GuideDocument28 pagesDigestion and Absorption of Lipids: A Comprehensive GuideEng Matti Ur RehmanNo ratings yet
- Distal Radius Fractures in AdultsDocument35 pagesDistal Radius Fractures in AdultsNicolás OpazoNo ratings yet
- Chapter Iii AnaphysioDocument3 pagesChapter Iii AnaphysiojakerzNo ratings yet
- Impact of Job Related Factors On Turn Over Intention SrilankaDocument8 pagesImpact of Job Related Factors On Turn Over Intention Srilankatedy hermawanNo ratings yet
- MidtermDocument2 pagesMidtermDiane JulianNo ratings yet
- Hyporeninemic HypoaldosteronismDocument12 pagesHyporeninemic HypoaldosteronismCésar Augusto Sánchez SolisNo ratings yet
- Acute Vs Chronic Renal FailureDocument7 pagesAcute Vs Chronic Renal FailurePellan Rhey CapuyanNo ratings yet
- Colles FractureDocument32 pagesColles FractureAndi KurniawanNo ratings yet
- Anatomy and Physiology of The BrainDocument4 pagesAnatomy and Physiology of The BraineriannajNo ratings yet
- Diabetes MilletusDocument31 pagesDiabetes MilletusMary Joy SumandaNo ratings yet
- Addison's Disease: Adrenal Insufficiency and Adrenal CrisisDocument15 pagesAddison's Disease: Adrenal Insufficiency and Adrenal CrisisMaryONo ratings yet
- Page 35-52 (Drug Study Gyne)Document20 pagesPage 35-52 (Drug Study Gyne)Ivan Chester de GuzmanNo ratings yet
- Gestational DiabetesDocument21 pagesGestational DiabetesRiko Sampurna SimatupangNo ratings yet
- Mineral MetabolismDocument12 pagesMineral MetabolismPavan Kumar RNo ratings yet
- Update On Cancer CachexiaDocument4 pagesUpdate On Cancer CachexiaIyanNo ratings yet
- Endocrine Pancreas & Fuel Homeostasis: Learning ObjectivesDocument7 pagesEndocrine Pancreas & Fuel Homeostasis: Learning ObjectivesMaggieLockeNo ratings yet
- c2Document37 pagesc2LuisAngelPonceTorresNo ratings yet
- TBI Understanding TBI Part 1Document4 pagesTBI Understanding TBI Part 1LindseyRae ParkerNo ratings yet
- Fluids & Electrolytes Disorders: Ariano Marcos State UniversityDocument13 pagesFluids & Electrolytes Disorders: Ariano Marcos State UniversityClements galiza100% (1)
- Nutritional Support of Stroke Patients: ESPEN Congress Lisbon 2015Document40 pagesNutritional Support of Stroke Patients: ESPEN Congress Lisbon 2015Risma SaroyaNo ratings yet
- Stevens Johnson DiseaseDocument5 pagesStevens Johnson DiseaseShammy RNNo ratings yet
- Liver Function Test: AssignmentDocument6 pagesLiver Function Test: Assignmentsaud100% (2)
- Grp.10 DiabetesDocument15 pagesGrp.10 DiabetesVanessa JanneNo ratings yet
- Acute Limb IschemiaDocument21 pagesAcute Limb IschemiaHina BatoolNo ratings yet
- Protein Malnutrition: Understanding Kwashiorkor and MarasmusDocument19 pagesProtein Malnutrition: Understanding Kwashiorkor and MarasmusJanine Kristine ManaoisNo ratings yet
- Hyperlipidemia Guide: Causes, Symptoms and TreatmentDocument17 pagesHyperlipidemia Guide: Causes, Symptoms and Treatmentbent alfay7a2No ratings yet
- Myocardialinfarction 150223043527 Conversion Gate02 PDFDocument22 pagesMyocardialinfarction 150223043527 Conversion Gate02 PDFBhavika Aggarwal100% (1)
- Immunity: Immunity Is The Balanced State ofDocument1 pageImmunity: Immunity Is The Balanced State ofCarolina GasperNo ratings yet
- Atherosclerosis PathophysiologyDocument11 pagesAtherosclerosis PathophysiologyCandice ChengNo ratings yet
- Obesity and DiabetesDocument7 pagesObesity and DiabetesJuliana Taemy OkimotoNo ratings yet
- Glycogen Storage Disease, Type II (Pompe Disease) : BackgroundDocument7 pagesGlycogen Storage Disease, Type II (Pompe Disease) : Background201111000No ratings yet
- Immunodeficiency DisordersDocument8 pagesImmunodeficiency Disordersbpt2No ratings yet
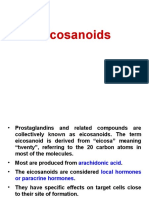
- Eicosanoids: 20-Carbon Compounds That Mediate InflammationDocument22 pagesEicosanoids: 20-Carbon Compounds That Mediate InflammationKifayat Kamal NowshinNo ratings yet
- TOEFL Essay 011 - 020Document9 pagesTOEFL Essay 011 - 020hungdn2121No ratings yet
- Eating DisordersDocument9 pagesEating DisordersFatin Nurina Mohd NazemiNo ratings yet
- Inborn Errors of MetabolismDocument4 pagesInborn Errors of Metabolismcurly perkyNo ratings yet
- T B E P: I W B E: Online Continuing Education For NursesDocument41 pagesT B E P: I W B E: Online Continuing Education For NursesAlagappan ThiyagarajanNo ratings yet
- 14 DyslipidemiaDocument45 pages14 DyslipidemiaSaniNo ratings yet
- Lower Urinary Tract Symptoms (LUTS)Document26 pagesLower Urinary Tract Symptoms (LUTS)Ayi Abdul BasithNo ratings yet
- 01 Serpentina Presentation PDFDocument27 pages01 Serpentina Presentation PDFabcNo ratings yet
- Bowel Obstruction Surgery: Causes, Risks, and RecoveryDocument12 pagesBowel Obstruction Surgery: Causes, Risks, and RecoveryDivya JoyNo ratings yet
- Diamond-Blackfan Anemia Is A DisorderDocument22 pagesDiamond-Blackfan Anemia Is A DisorderDarem SoNo ratings yet
- Osteogenesis ImperfectaDocument27 pagesOsteogenesis Imperfectacode212No ratings yet
- Anemia in ChildrenDocument4 pagesAnemia in ChildrenTeslim Raji100% (1)
- Truncus ArteriosusDocument4 pagesTruncus ArteriosuskemalahmadNo ratings yet
- Anti Diabetic DrugsDocument58 pagesAnti Diabetic DrugsDaniel WangNo ratings yet
- Biochemistry of GlycoproteinDocument6 pagesBiochemistry of GlycoproteinMahathir Mohmed100% (7)
- Cancer Prevention - The Causes and Prevention of Cancer Volume 1 (Cancer Prevention-Cancer Causes) (PDFDrive) PDFDocument338 pagesCancer Prevention - The Causes and Prevention of Cancer Volume 1 (Cancer Prevention-Cancer Causes) (PDFDrive) PDFtheresaNo ratings yet
- Research Paper - Eating DisordersDocument14 pagesResearch Paper - Eating DisordersJason OrrNo ratings yet
- Hyperosmolar HyperglycemicDocument8 pagesHyperosmolar HyperglycemicCésar Augusto Sánchez SolisNo ratings yet
- Parkinsonism PDFDocument3 pagesParkinsonism PDFNerissaArvianaShintaraNo ratings yet
- Diabetes NotesDocument10 pagesDiabetes Notestripj33No ratings yet
- Amyotrophic Lateral SclerosisDocument6 pagesAmyotrophic Lateral SclerosisJohnjohn MateoNo ratings yet
- Case Study 1 (Muscular) - ALSDocument5 pagesCase Study 1 (Muscular) - ALSSamantha AquinoNo ratings yet
- Metabolic Syndrome Lecture Explains Insulin Resistance and InflammationDocument34 pagesMetabolic Syndrome Lecture Explains Insulin Resistance and InflammationMuhammad Riandy Lukman Tanjung100% (1)
- Complete Guide to Cirrhosis of the LiverDocument12 pagesComplete Guide to Cirrhosis of the LiverherlindaNo ratings yet
- Other Foreign Substances These Substances Have Entered The Blood Supply EitherDocument15 pagesOther Foreign Substances These Substances Have Entered The Blood Supply EitherAnis Assila Mohd RohaimiNo ratings yet
- The Liver and Hepatobiliary SystemDocument11 pagesThe Liver and Hepatobiliary SystemYonathanHasudunganNo ratings yet
- Scope of Knowledge For Master of Radiology MedexDocument1 pageScope of Knowledge For Master of Radiology MedexAizat KamalNo ratings yet
- Kee MRI PDFDocument17 pagesKee MRI PDFNoura RoseNo ratings yet
- Surgical Management of PterygiumDocument5 pagesSurgical Management of PterygiumAizat KamalNo ratings yet
- Revisited: Amoebic Liver AbscessDocument3 pagesRevisited: Amoebic Liver AbscessBarudak Theris BadeurNo ratings yet
- Radiological Anatomy For FRCRDocument29 pagesRadiological Anatomy For FRCRAizat KamalNo ratings yet
- Amoebic Liver Abscess: Clinical MedicineDocument5 pagesAmoebic Liver Abscess: Clinical MedicineAizat KamalNo ratings yet
- FRCR Part 1 Anatomy Mock Examinations Download Free BookDocument4 pagesFRCR Part 1 Anatomy Mock Examinations Download Free BookAizat KamalNo ratings yet
- NUCLEAR MEDICINE POLICY 2018 (Edited)Document100 pagesNUCLEAR MEDICINE POLICY 2018 (Edited)Aizat KamalNo ratings yet
- Phenylephrine Is A Noncatecholamine With PredominaDocument2 pagesPhenylephrine Is A Noncatecholamine With PredominaAizat KamalNo ratings yet
- Standards of Medical Care in Diabetes 2015Document99 pagesStandards of Medical Care in Diabetes 2015Juan Carlos Sánchez Suárez100% (1)
- Case Report: Primary AnetodermaDocument3 pagesCase Report: Primary AnetodermaAizat KamalNo ratings yet
- Standards of Medical Care in Diabetes 2015Document99 pagesStandards of Medical Care in Diabetes 2015Juan Carlos Sánchez Suárez100% (1)
- Allgulander CDocument1 pageAllgulander CAizat KamalNo ratings yet
- South African Family PracticeDocument5 pagesSouth African Family PracticeAizat KamalNo ratings yet
- Acute Diarrhea Long FINAL 120604Document24 pagesAcute Diarrhea Long FINAL 120604Aizat KamalNo ratings yet
- Threatened Abortion PDFDocument3 pagesThreatened Abortion PDFAizat KamalNo ratings yet
- New Ballard Score for Premature InfantsDocument1 pageNew Ballard Score for Premature InfantsAizat KamalNo ratings yet
- MorphineDocument3 pagesMorphineAizat KamalNo ratings yet
- MELOXICAMDocument4 pagesMELOXICAMAizat KamalNo ratings yet
- Nausea and VomittingDocument1 pageNausea and VomittingAizat KamalNo ratings yet
- Metabolic Functions of The LiverDocument3 pagesMetabolic Functions of The LiverAizat KamalNo ratings yet
- 2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFDocument555 pages2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFGiovana BarbosaNo ratings yet
- Annual Health Checkup (Executive) : Package Amt. Package Actual AmtDocument1 pageAnnual Health Checkup (Executive) : Package Amt. Package Actual AmtPAWAN KUMARNo ratings yet
- Physiology of the Pleural Space: Visceral Pleura, Parietal Pleura, and Fluid FormationDocument78 pagesPhysiology of the Pleural Space: Visceral Pleura, Parietal Pleura, and Fluid FormationAhmad RafiqiNo ratings yet
- Heart Disease Course PDALongDocument84 pagesHeart Disease Course PDALongArpanpatelNo ratings yet
- Choosing the Right PaediatricianDocument263 pagesChoosing the Right PaediatricianSuneethaVangala100% (1)
- ER Nurse CVDocument5 pagesER Nurse CVLopezDistrict FarmersHospitalNo ratings yet
- The Vanuatu Cooking Project ProposalDocument6 pagesThe Vanuatu Cooking Project ProposalBunga Melur MewangiNo ratings yet
- Article Dietschi VeenersDocument18 pagesArticle Dietschi VeenersRoberto PucNo ratings yet
- 2-Downer Cow and HypoMgDocument13 pages2-Downer Cow and HypoMgY.rajuNo ratings yet
- Protein and Amino Acid MetabolismDocument52 pagesProtein and Amino Acid MetabolismRisky OpponentNo ratings yet
- Comp ReviewDocument99 pagesComp ReviewTHAO DANGNo ratings yet
- Viral and Bacterial Infections of The SkinDocument200 pagesViral and Bacterial Infections of The SkinKarla Jane100% (1)
- Ramadan Fasting and Infectious Diseases: A Systematic ReviewDocument9 pagesRamadan Fasting and Infectious Diseases: A Systematic ReviewBasel SoudanNo ratings yet
- A Pain Education ProgrammeDocument13 pagesA Pain Education Programmeapi-244230664No ratings yet
- Air Traffic Controllers Warned on Sleeping on the JobDocument108 pagesAir Traffic Controllers Warned on Sleeping on the Jobeduardo juniorNo ratings yet
- Lecture 6 Cardiovascular: Vascular System - The HemodynamicsDocument61 pagesLecture 6 Cardiovascular: Vascular System - The HemodynamicsAndreea ŞtefănescuNo ratings yet
- Psychiatric Nursing Mastery Test Part 2Document16 pagesPsychiatric Nursing Mastery Test Part 2Rika MaeNo ratings yet
- Nursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationDocument10 pagesNursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationmalindaNo ratings yet
- Dengue AccomplishmentDocument4 pagesDengue AccomplishmentKylie GolindangNo ratings yet
- Inclusiveness: Prepared By: Dinke A. 2021Document131 pagesInclusiveness: Prepared By: Dinke A. 2021maria tafaNo ratings yet
- Dagim Firide YimenuDocument138 pagesDagim Firide Yimenugemu deribaNo ratings yet
- Rectal Cancer,: Clinical Practice Guidelines in OncologyDocument28 pagesRectal Cancer,: Clinical Practice Guidelines in OncologyRaíla SoaresNo ratings yet
- What Is Water PollutionDocument13 pagesWhat Is Water PollutiondumitrutudoranNo ratings yet
- Dangers of Excess Sugar ConsumptionDocument2 pagesDangers of Excess Sugar ConsumptionAIDEN COLLUMSDEANNo ratings yet
- Nume CNP Sex Varsta Dimensiune Pozitie PietreDocument12 pagesNume CNP Sex Varsta Dimensiune Pozitie PietreGabriel BurteaNo ratings yet