Professional Documents
Culture Documents
Ebp
Uploaded by
Jharene BasbañoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ebp
Uploaded by
Jharene BasbañoCopyright:
Available Formats
I.
EVIDENCE-BASED NURSING
Present Practice Treating Anemia with Red Blood Cell Transfusions When anemia becomes severe, generally when hemoglobin drops to or below 7-8 g/dL transfusions are often used to quickly raise hemoglobin levels to a normal range and reduce symptoms like significant fatigue and dizziness. Blood transfusions, however, do come with some risks. For instance transfused blood can introduce pathogens directly into the blood stream, can lead to possibly fatal reactions, or can cause changes in the patients immune system that may lead to other serious reactions and infections. Additionally, several studies have shown that patients who receive transfusions, on average, stay in the hospital longer, have higher hospital bills, and are generally more ill than patients who did not receive a transfusion.
Evidenced-Based Nursing New drug to treat anemia The name of the drug is FG-2216, and its designed to stimulate production of the hormone erythropoietin (EPO) in dialysis patients. In fact, its the worlds first oral drug for the treatment of kidney disease-related anemia; its a hypoxia inducible factor prolyl hydroxylase inhibitor (HIF-PHI) that stabilizes the "master switch," which normally tells the body to produce EPO in response to low oxygen levels. Anemia, one of the more common blood disorders, is caused by low production of EPO, which has been assumed to result from damage to the kidney cells that produce EPO. "Our study clearly shows that this may not be the case, and that the kidneys of patients on dialysis retain significant ability to produce erythropoietin," which Wanja M. Bernhardt, MD, Department of Nephrology, University hospital Erlangen, Germany, was quoted as saying. "Renal anemia seems to result from disturbed regulation rather than lost production capacity of the hormone. Treatment with FG-2216 considerably increased EPO production in dialysis patients, in addition to healthy people with normal kidneys. The utmost
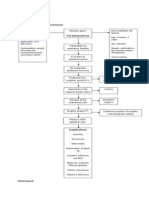
Recommendations to Present Practice Because of the risks present in blood transfusion the nurse should perform the following:
Verify that an order for the transfusion exists. Conduct a thorough physical assessment of the patient (including vital signs) to help identify later changes. Document findings. Confirm that the patient has given informed consent. Teach the patient about the procedures associated risks and benefits, what to expect during the transfusion, signs and symptoms of a reaction, and when and how to call for assistance. Check for an appropriate and patent vascular access. Make sure necessary equipment is at hand for administering the blood product and managing a reaction, such as an additional free I.V. line for normal saline solution, oxygen, suction, and a
increase in EPO production occurred in dialysis patients whose kidneys were still present, but no longer functioning. FG-2216 additionally stimulated EPO production in dialysis patients with no kidneys. These are individuals whose kidneys had been removed at surgery for cancer or other diseases. The significant increase in EPO production in patients devoid of kidneys was approximately as high as in people with normally functioning kidneys. In patients with no kidneys, FG-2216 in fact stimulated production of EPO by the liver. The studys outcome questions the standard knowledge that dialysis-related anemia occurs for the reason that patients with advanced kidney disease can no longer make their own EPO. "Our results confirm that both the liver and the kidneys retain a significant production capacity for erythropoietin in end-stage renal disease patients," adds Bernhardt. Presently, patients with dialysisrelated anemia are given EPO replacement therapy with drugs called erythropoiesis-stimulating agents (ESAs). Regardless of nearly two decades of use, there remains a constant debate related to the safety, appropriate clinical use, and in due course high costs of ESAs. If the latest results are borne out by future studies, then use of prolyl-hydroxylase inhibitors such as FG-2216 to help the body make its own EPO might provide a new-fangled alternative to ESAs.
hypersensitivity kit. Be sure you're familiar with the specific product to be transfused, the appropriate administration rate, and required patient monitoring. Know what personnel will be available in the event of a reaction, and how to contact them. Resources should include the oncall physician and a blood bank representative. Before hanging the blood product, thoroughly doublecheck the patients identification and verify the actual product. Check the unit to be transfused against patient identifiers, per facility policy. Infuse the blood product with normal saline solution only, using filtered tubing.
The groundwork has been set with this study, which moreover evaluated merely the response to a single dose of FG-2216. Although there were no harmful effects, the results and long-term safety of activation of HIF by prolylhydroxylase inhibitors remain uncertain. Additional research will furthermore be required to find out why HIF is evidently not stabilized in response to decreased oxygen concentrations in patients with kidney disease but responds to treatment with prolyl-hydroxylase inhibitors. SOURCE: Journal of the American Society of Nephrology, November 29, 2010
Reference: http://www.ivanhoe.com/channels/ p_channelstory.cfm?storyid=2583 1
You might also like
- Influence of Dry Weight Reduction On Anemia in Patients Undergoing HemodialysisDocument12 pagesInfluence of Dry Weight Reduction On Anemia in Patients Undergoing HemodialysisFajar JarrNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyFrom EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyNo ratings yet
- Adult Onset Hypophosphatasia Before and After Treatment With AsfotaseDocument12 pagesAdult Onset Hypophosphatasia Before and After Treatment With AsfotaseCaro ErazoNo ratings yet
- Treatment of Anemia in CKD: Pathophysiology and Potential New TherapiesDocument14 pagesTreatment of Anemia in CKD: Pathophysiology and Potential New TherapiesDesi MeliaNo ratings yet
- Research Paper Kidney FailureDocument7 pagesResearch Paper Kidney Failurexfeivdsif100% (3)
- Ncologist: Erythropoiesis-Stimulating Agents in Renal MedicineDocument6 pagesNcologist: Erythropoiesis-Stimulating Agents in Renal MedicineSergio RodriguezNo ratings yet
- Lack of Nephrotoxicity by 6% Hydroxyethyl Starch 130/0.4 During Hip ArthroplastyDocument11 pagesLack of Nephrotoxicity by 6% Hydroxyethyl Starch 130/0.4 During Hip ArthroplastyKarina Mega WNo ratings yet
- Ebora - Meta AnalysisDocument29 pagesEbora - Meta AnalysisISRAEL JULIANO SALGADONo ratings yet
- Literature Review Demographics of The End-Stage Renal Disease PopulationDocument22 pagesLiterature Review Demographics of The End-Stage Renal Disease PopulationSriMathi Kasi Malini ArmugamNo ratings yet
- 1271 HSP .FullDocument8 pages1271 HSP .FulldonkeyendutNo ratings yet
- Anemia in Kidney Disease and DialysisDocument6 pagesAnemia in Kidney Disease and DialysiscopiimeiNo ratings yet
- Anemia 1Document8 pagesAnemia 1Pablo AlvarezNo ratings yet
- Erectile Dysfunction and HypertensionDocument8 pagesErectile Dysfunction and HypertensionILham SyahNo ratings yet
- 857 1857 1 PBDocument4 pages857 1857 1 PBJesselle LasernaNo ratings yet
- Article ReviewDocument8 pagesArticle Reviewwjohnson_3No ratings yet
- Sciencedaily (June 10, 2010) - A Drug Commonly Used To Treat Gout May Help MaintainDocument4 pagesSciencedaily (June 10, 2010) - A Drug Commonly Used To Treat Gout May Help MaintainAmbbiga AmirthamNo ratings yet
- Changes in Urine Volume and Serum Albumin in Incident Hemodialysis PatientsDocument12 pagesChanges in Urine Volume and Serum Albumin in Incident Hemodialysis Patientsmelda lestari haidirNo ratings yet
- Febuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go ToDocument9 pagesFebuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go ToAnadi GuptaNo ratings yet
- 2008 Anemia in Children With Chronic Kidney DiseaseDocument11 pages2008 Anemia in Children With Chronic Kidney DiseaseFabiana RaimundoNo ratings yet
- A C A D e M I C S C I e N C e SDocument5 pagesA C A D e M I C S C I e N C e SApacetech IluvbNo ratings yet
- Jurnal KimiaDocument9 pagesJurnal KimiaTeguh DesmansyahNo ratings yet
- Otero Et Al 2011 Elevated Alkaline Phosphatase in Children An Algorithm To Determine When A Wait and See Approach IsDocument4 pagesOtero Et Al 2011 Elevated Alkaline Phosphatase in Children An Algorithm To Determine When A Wait and See Approach IsmokgabisengNo ratings yet
- Research Paper On Renal FailureDocument8 pagesResearch Paper On Renal Failurefapavelyfel2100% (3)
- Hepatic EncephalopathyDocument5 pagesHepatic EncephalopathyRobert G. Gish, MDNo ratings yet
- Ijnrd 10 129Document6 pagesIjnrd 10 129Erick Rivera SainzNo ratings yet
- Research Paper On Liver DiseaseDocument5 pagesResearch Paper On Liver Diseaseefjem40q100% (1)
- Reproduction Women ESRDDocument4 pagesReproduction Women ESRDInomy Claudia Katherine ImbiriNo ratings yet
- Neonatal and Pediatric Transfusion Practice: Cassandra D. Josephson, MD, and Erin Meyer, DO, MPHDocument28 pagesNeonatal and Pediatric Transfusion Practice: Cassandra D. Josephson, MD, and Erin Meyer, DO, MPHpro earnerNo ratings yet
- ESA in CKD - Review ArticleDocument27 pagesESA in CKD - Review ArticleBhavani KirthiNo ratings yet
- Ultrafiltration Therapy for Cardiorenal Syndrome Physiologic Basis and Contemporary OptionsDocument9 pagesUltrafiltration Therapy for Cardiorenal Syndrome Physiologic Basis and Contemporary Optionsfernando.suarez.mtzNo ratings yet
- GoutDocument14 pagesGoutElisa KartikaNo ratings yet
- Mcvary 2007Document15 pagesMcvary 2007abhijeet abhijeetNo ratings yet
- Treatment of Orthostatic and Postprandial HypotensionDocument13 pagesTreatment of Orthostatic and Postprandial HypotensionRebeca RiveraNo ratings yet
- Polycythemiawith Hydronephrosis:a Rare CaseDocument5 pagesPolycythemiawith Hydronephrosis:a Rare CaseIJAR JOURNALNo ratings yet
- Chronic Kidney Disease: PathophysiologyDocument8 pagesChronic Kidney Disease: Pathophysiologyaryati yayaNo ratings yet
- (Osborn) Chapter 47: Osborn, Et Al., Test Item File For Medical-Surgical Nursing: Preparation For PracticeDocument19 pages(Osborn) Chapter 47: Osborn, Et Al., Test Item File For Medical-Surgical Nursing: Preparation For PracticeKittiesNo ratings yet
- WJH 14 670Document13 pagesWJH 14 670juliomenimssNo ratings yet
- Reducción de Uratos y ERC NEJM 2020Document2 pagesReducción de Uratos y ERC NEJM 2020Gabriel VargasNo ratings yet
- Multiple Myloma AneamiaDocument3 pagesMultiple Myloma AneamiaShafiq Ahmad KhanNo ratings yet
- Nursing Care for Hepatic EncephalopathyDocument14 pagesNursing Care for Hepatic EncephalopathyClarisse AcacioNo ratings yet
- Blood Conservation in Pediatric Cardiac SurgeryDocument5 pagesBlood Conservation in Pediatric Cardiac Surgerymohanakrishna007No ratings yet
- NIH Public Access: Author ManuscriptDocument8 pagesNIH Public Access: Author ManuscriptAlexisUrielMontesNo ratings yet
- Ed Hypog DR BarkinDocument6 pagesEd Hypog DR BarkinMohankummar MuniandyNo ratings yet
- American Heart American Heart American Heart American Heart AssociationDocument11 pagesAmerican Heart American Heart American Heart American Heart Associationmubarak19855No ratings yet
- Nursing Care Plan for Ineffective Myocardial Tissue PerfusionDocument5 pagesNursing Care Plan for Ineffective Myocardial Tissue PerfusionTin DuapaNo ratings yet
- Normal Protein Diet and L-Ornithine-L-Aspartate For Hepatic EncephalopathyDocument4 pagesNormal Protein Diet and L-Ornithine-L-Aspartate For Hepatic EncephalopathyElisa SalakayNo ratings yet
- Clinical Update: Upper Gastrointestinal BleedingDocument4 pagesClinical Update: Upper Gastrointestinal BleedingSNo ratings yet
- Erythropoietin CASE STUDYDocument2 pagesErythropoietin CASE STUDYVVBNo ratings yet
- Anemia Management in Peritoneal Dialysis: Perspectives From The Asia Paci Fic RegionDocument7 pagesAnemia Management in Peritoneal Dialysis: Perspectives From The Asia Paci Fic RegionSwingly ThineNo ratings yet
- Dissert. AnisimovDocument7 pagesDissert. AnisimovcamiloNo ratings yet
- Albumin Transfusion Guidelines Following ParacentesisDocument3 pagesAlbumin Transfusion Guidelines Following ParacentesisVlad IonutNo ratings yet
- Erythropoietin (EPO) : Dr. Zulfkar Qadrie SR., PharmacologyDocument28 pagesErythropoietin (EPO) : Dr. Zulfkar Qadrie SR., PharmacologyZulfkar Latief QadrieNo ratings yet
- 13 JCR 015 Neki PhenytoinDocument6 pages13 JCR 015 Neki PhenytoinAnis ThohirohNo ratings yet
- Manejo de La Sepsis 2Document5 pagesManejo de La Sepsis 2Rachmi Pratiwi Febrita PartiNo ratings yet
- Laporan MRDocument6 pagesLaporan MRParahmitaNo ratings yet
- 50 Years Old Male With Non Hodgkin Lymphoma and Vincristine Induced Unilateral PtosisDocument1 page50 Years Old Male With Non Hodgkin Lymphoma and Vincristine Induced Unilateral PtosisArya BrunoNo ratings yet
- Case Report PUBS V6Document8 pagesCase Report PUBS V6Kevin RengelNo ratings yet
- Risk Factors and Management of Acute Kidney Injury in the ElderlyDocument15 pagesRisk Factors and Management of Acute Kidney Injury in the ElderlySiti NcitNo ratings yet
- PEAK Drug Therapy During Pregnancy Implications For Dental PracticeDocument8 pagesPEAK Drug Therapy During Pregnancy Implications For Dental PracticeAmalia KautsariaNo ratings yet
- Anesthesia Care PlanDocument2 pagesAnesthesia Care PlanMedShare100% (10)
- Study Notes SurgeryDocument56 pagesStudy Notes SurgeryMedShare83% (12)
- Epinephrine Generic and Brand Names, Mechanism of Action, Indications, Adverse Effects and Nursing ResponsibilitiesDocument23 pagesEpinephrine Generic and Brand Names, Mechanism of Action, Indications, Adverse Effects and Nursing ResponsibilitiesJharene BasbañoNo ratings yet
- Evidence-Based NursingDocument3 pagesEvidence-Based NursingJharene BasbañoNo ratings yet
- Case Abstract GrandcaseDocument2 pagesCase Abstract GrandcaseJharene BasbañoNo ratings yet
- Drugs ICUDocument4 pagesDrugs ICUJharene BasbañoNo ratings yet
- Drugs GCDocument7 pagesDrugs GCJharene BasbañoNo ratings yet
- Amitriptyline HydrochlorideDocument1 pageAmitriptyline HydrochlorideJharene BasbañoNo ratings yet
- Abruptio Placenta Nursing Care PlanDocument2 pagesAbruptio Placenta Nursing Care PlanJharene Basbaño100% (5)
- PathoDocument1 pagePathoJharene BasbañoNo ratings yet
- Laboratory ResultsDocument6 pagesLaboratory ResultsJharene BasbañoNo ratings yet
- Patho MeaslesDocument2 pagesPatho MeaslesJharene BasbañoNo ratings yet
- Drugs ICUDocument4 pagesDrugs ICUJharene BasbañoNo ratings yet
- EnvironmentalDocument1 pageEnvironmentalJharene BasbañoNo ratings yet
- URTI Sample ChartingDocument1 pageURTI Sample ChartingJharene BasbañoNo ratings yet
- Health Teaching Plan: Iron-Rich Foods BenefitsDocument1 pageHealth Teaching Plan: Iron-Rich Foods BenefitsJharene BasbañoNo ratings yet
- Nursing Law and EthicsDocument14 pagesNursing Law and Ethicsaleth joyce cubacub96% (25)
- OngoingDocument2 pagesOngoingJharene BasbañoNo ratings yet
- Nursing Leadership and Management Effects Work EnvironmentsDocument2 pagesNursing Leadership and Management Effects Work EnvironmentsJharene BasbañoNo ratings yet
- Nursing Leadership and Management Effects Work EnvironmentsDocument2 pagesNursing Leadership and Management Effects Work EnvironmentsJharene BasbañoNo ratings yet
- Epinephrine Generic and Brand Names, Mechanism of Action, Indications, Adverse Effects and Nursing ResponsibilitiesDocument23 pagesEpinephrine Generic and Brand Names, Mechanism of Action, Indications, Adverse Effects and Nursing ResponsibilitiesJharene BasbañoNo ratings yet
- Abruptio Placenta Nursing Care PlanDocument2 pagesAbruptio Placenta Nursing Care PlanJharene Basbaño100% (5)
- Nursing Care Plan for Postpartum HemorrhageDocument4 pagesNursing Care Plan for Postpartum HemorrhageJharene BasbañoNo ratings yet
- Epinephrine Generic and Brand Names, Mechanism of Action, Indications, Adverse Effects and Nursing ResponsibilitiesDocument23 pagesEpinephrine Generic and Brand Names, Mechanism of Action, Indications, Adverse Effects and Nursing ResponsibilitiesJharene BasbañoNo ratings yet
- Health Teaching Plan: Iron-Rich Foods BenefitsDocument1 pageHealth Teaching Plan: Iron-Rich Foods BenefitsJharene BasbañoNo ratings yet
- Post Appendectomy NCPDocument1 pagePost Appendectomy NCPJharene BasbañoNo ratings yet
- Emergency DrugsDocument6 pagesEmergency DrugsJharene BasbañoNo ratings yet
- Emergency DrugsDocument6 pagesEmergency DrugsJharene BasbañoNo ratings yet
- Nursing Care Plan for Postpartum HemorrhageDocument4 pagesNursing Care Plan for Postpartum HemorrhageJharene BasbañoNo ratings yet
- Patho MeaslesDocument2 pagesPatho MeaslesJharene BasbañoNo ratings yet
- Basic Science and Sructure of Skin MCQsDocument92 pagesBasic Science and Sructure of Skin MCQsDr.Tawheed88% (16)
- DepresijaDocument6 pagesDepresijaChristopher PhillipsNo ratings yet
- Pressure HazardsDocument4 pagesPressure HazardsABDulNafeNo ratings yet
- CH 3 - Study GuideDocument13 pagesCH 3 - Study Guide2688gieNo ratings yet
- Cysteine, Methionine, ProlineDocument3 pagesCysteine, Methionine, ProlineRio BurlazaNo ratings yet
- Review of System Done... 1Document2 pagesReview of System Done... 1Dheng EsquijoNo ratings yet
- Biological Level of Analysis Research GuideDocument45 pagesBiological Level of Analysis Research GuidePhiline Everts100% (2)
- CK-MB production method reportDocument1 pageCK-MB production method reportOkura JoshuaNo ratings yet
- New European Guidelines Address Hyponatremia ManagementDocument5 pagesNew European Guidelines Address Hyponatremia ManagementGherciuChirilaLarisaNo ratings yet
- How The Circadian Rhythm Affects Sleep, Wakefulness, and Overall HealthDocument62 pagesHow The Circadian Rhythm Affects Sleep, Wakefulness, and Overall HealthRosemarie Fritsch100% (1)
- 1.13.2 Clinical Localization and History in NeurologyDocument42 pages1.13.2 Clinical Localization and History in Neurologyfikrah sharifNo ratings yet
- UQU SLE CORRECTED FILE by DR Samina FidaDocument537 pagesUQU SLE CORRECTED FILE by DR Samina Fidaasma .sassi100% (1)
- Chapter 9 &10 - Gene ExpressionDocument4 pagesChapter 9 &10 - Gene ExpressionMahmOod GhNo ratings yet
- Endocrine - FRCEM SuccessDocument110 pagesEndocrine - FRCEM SuccessskNo ratings yet
- Pathophysiology PneumoniaDocument2 pagesPathophysiology PneumoniaSheila Mae Escalante67% (3)
- Microsoft Word - Endodontic - MishapsDocument20 pagesMicrosoft Word - Endodontic - MishapsShufeiNo ratings yet
- Surya NamaskarDocument2 pagesSurya NamaskarDipkumar Patel100% (2)
- Hypertension ControlDocument7 pagesHypertension ControlXyla CullenNo ratings yet
- Blood ? Summary PDFDocument10 pagesBlood ? Summary PDFmanar aleneziNo ratings yet
- Removable Partial Denture ComponentsDocument128 pagesRemovable Partial Denture ComponentsVikas Aggarwal50% (2)
- Kurukshetra University Date-Sheets for BA/BSc Part ExamsDocument12 pagesKurukshetra University Date-Sheets for BA/BSc Part ExamsabhishekNo ratings yet
- Medico Legal Aspects of DeathDocument206 pagesMedico Legal Aspects of Deathrosana f.rodriguez83% (12)
- U04 Fxs of Humeral ShaftDocument88 pagesU04 Fxs of Humeral Shaftadrian_mogosNo ratings yet
- BLOCK II LMS Quiz AnatomyDocument27 pagesBLOCK II LMS Quiz AnatomyAshley BuchananNo ratings yet
- Use of Vasopressors and Inotropes - UpToDateDocument25 pagesUse of Vasopressors and Inotropes - UpToDateVictor Mendoza - MendezNo ratings yet
- Postpartum HemorrhageDocument25 pagesPostpartum HemorrhageaKmaL67% (3)
- DNA/RNA Extraction Guide - Isolate Nucleic Acids From CellsDocument27 pagesDNA/RNA Extraction Guide - Isolate Nucleic Acids From CellsSahilKulkarniNo ratings yet
- In This Issue: Wound Infection and ColonisationDocument7 pagesIn This Issue: Wound Infection and ColonisationSeftiana WahyuniNo ratings yet
- Q and A DactylosDocument56 pagesQ and A DactylosJUNN REE MONTILLA100% (2)
- Rajeev Kumar Talakayala CVDocument37 pagesRajeev Kumar Talakayala CVSanjeev KumarNo ratings yet