Professional Documents
Culture Documents
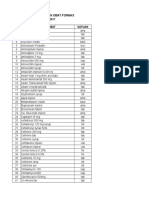
CDC Diphtheria Surveillance Worksheet
Uploaded by
Luna WhiteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CDC Diphtheria Surveillance Worksheet
Uploaded by
Luna WhiteCopyright:
Available Formats
DIPHTHERIA REPORTING INFORMATION Class A: Report immediately via telephone the case or suspected case and/or a positive laboratory
y result to the local public health department where the patient resides. If patient residence is unknown, report immediately via telephone to the local public health department in which the reporting health care provider or laboratory is located. Reporting Form(s) and/or Mechanism: Immediately via telephone. The CDC Diphtheria Surveillance Worksheet is available for use to assist local health department disease investigation and contact tracing activities. Additional reporting information, with specifics regarding the key fields for the Ohio Disease Reporting System (ODRS) Reporting can be located in Section 7. AGENT Corynebacterium diphtheriae; two strains, one toxigenic and one non-toxigenic, each can cause disease. CASE DEFINITION Clinical Description An upper respiratory tract illness with an adherent membrane of the nose, pharynx, tonsils, or larynx. Laboratory Criteria for Diagnosis Isolation of Corynebacterium diphtheriae from the nose or throat, or Histopathologic diagnosis of diphtheria. Case classification Probable: a clinically compatible case that is not laboratory confirmed and is not epidemiologically linked to a laboratory-confirmed case. Confirmed: a clinically compatible case that is either laboratory confirmed or epidemiologically linked to laboratory-confirmed case. Not a Case: This status will not generally be used when reporting a case, but may be used to reclassify a report if investigation revealed that it was not a case. Comment Cutaneous diphtheria should not be reported. Respiratory disease caused by non-toxigenic C. diphtheriae should be reported as diphtheria. SIGNS AND SYMPTOMS Diphtheria is often described according to the site of membrane involvement: nasal; tonsillar and pharyngeal; laryngeal; and non-respiratory, which includes skin wounds, conjunctival and genital lesions. Respiratory diphtheria has a gradual onset and is characterized by a mild fever (rarely >101 F or >38.3 C), sore throat, difficulty in swallowing, malaise, loss of appetite, and if the larynx is involved, hoarseness may occur. The hallmark of respiratory diphtheria is the presence of a membrane that appears within 23 days of illness over the mucous membrane of the tonsils, pharynx, larynx, or ODH-IDCM DIPTHERIA Page 1/Section 3 Revised 7/2013
nares, and which can extend into the trachea. The membrane is firm, fleshy, grey, and adherent, and bleeds following attempts to remove or dislodge it. Tonsillar and pharyngeal diphtheria begins with malaise, anorexia, sore throat and low-grade fever. Within 24 hours a whitish-grey or bluish-white membrane begins forming in the throat. When completely formed, the membrane may include one or both tonsils, uvula, soft palate and pharyngeal wall. Various degrees of cervical adenitis and periadenitis may be observed. In mild cases the membrane sloughs off in seven to ten days, and recovery is uneventful. Severe disease is characterized by increased toxemia and can result in death within six to ten days. Laryngeal diphtheria is generally an extension of pharyngeal infection. It can also result from separate involvement. Onset is characterized by fever, hoarseness and cough. Obstruction of the airway is increased. In mild cases the membrane is coughed up in six to ten days. Occasionally the membrane extends downward and involves the tracheobronchial tree. DIAGNOSIS The initial diagnosis of diphtheria should be made on the basis of clinical findings because any delay in therapy poses a serious risk to the patient. In patients, suspect cases and contacts, cultures should be taken from the nasopharynx as well as the throat, since 20% of positive cultures can be missed when only one site is cultured. Nasopharyngeal cultures should be obtained with a flexible alginate swab that reaches deep into the posterior nares. Throat cultures are taken with a cotton swab which is firmly applied to any area with a membrane or inflammation. For asymptomatic patients, the tonsillar fossae, posterior pharynx and retrouvular areas should be sampled as well as the nasopharynx. Before cultures of wounds are taken, the lesions should be cleansed with sterile, normal saline and crusted material should be removed. A cotton-tipped applicator is then firmly applied to the base of the wound. Contact the ODH Immunization Program at 614-466-4643 for specimen coordination with the CDC laboratory. EPIDEMIOLOGY Source Humans. Occurrence Considered a disease of colder months. Most cases are seen in inadequately or unimmunized children <15 years of age and also in adults with inadequate immunization. Rarely found in infants. Mode of Transmission The disease is contracted through contact with an infected individual or a carrier. Bacteria are spread person-to-person through oral or respiratory droplets by coughing, sneezing or even talking close physical contact. Period of Communicability Communicability varies, but is usually two weeks or less and seldom more than four weeks. Chronic carriers (which are rare) might shed organisms for six months or ODH-IDCM DIPTHERIA Page 2/Section 3 Revised 7/2013
more. Incubation Period Generally 2 to 5 days, but may range from 1 to 10 days. PUBLIC HEALTH MANAGEMENT Case Watch for any suspect cases in the same geographic area among those who are inadequately immunized. Treatment Antitoxin should be given immediately, preferably intravenously, after testing to rule out hypersensitivity. The dosage depends upon the duration of symptoms, area of involvement and severity of the disease. Both penicillin and erythromycin are effective against the organism but should be administered only after cultures are taken, in conjunction with, but not as a substitute for antitoxin. Following recovery, approximately 50% of patients will show immunity for at least a year. Second attacks, although rare, are a possibility. Therefore, appropriate immunization should be carried out following recovery. Isolation According to the Ohio Administrative Code (OAC 3701-3-13, (I)), a person with diphtheria shall be isolated until two cultures, from both throat and nose, and additionally, in the case of cutaneous diphtheria, a culture from skin lesions, are negative for diphtheria bacilli. Cultures shall be taken not less than twenty-four hours apart, and not less than twenty-four hours after cessation of antimicrobial therapy. If culturing is unavailable or impractical, isolation may be ended after fourteen days of effective antimicrobial therapy. Contacts Intimate and household contacts need to be identified immediately. Others with direct exposure history should be identified, such as healthcare staff exposed to the patients nasopharyngeal secretions and children care for by the infected individual. Regardless of their immunization status, contacts should be 1) under surveillance for 7 days for evidence of disease; 2) cultured for C. diphtheriae; 3) given antimicrobial prophylaxis with either oral erythromycin for 10 days or a single intramuscular injection of penicillin G. Contacts previously immunized should be given a booster disease of DTaP, DT, Td, or Tdap as age appropriate. (Please note that Tdap is currently only licensed for use in a single booster dose.) Prevention and Control The most effective prevention and control of diphtheria is accomplished through widespread routine immunization. For details consult the ODH Vaccine Protocol Manual. Children should be vaccinated against diphtheria with the DTaP (diphtheria toxoid in combination with tetanus toxoid and acellular pertussis) vaccine. This vaccine should be given at 2, 4, 6 and 15 to 18 months of age, and between 4 and 6 years of age. Adults with uncertain histories of a complete primary vaccination series with diphtheria and tetanus toxoid-containing vaccines should begin or complete a primary vaccination series. Older children and adults who have completed the primary series should receive Td (tetanus and diphtheria toxoid) boosters every 10 years to maintain immunity. One lifetime dose of Tdap (tetanus, diphtheria, and ODH-IDCM DIPTHERIA Page 3/Section 3 Revised 7/2013
acellular pertussis) is recommended for people 11 years of age and older as one of these boosters to provide protection against pertussis. Pregnancy is an exception to the one-dose recommendation (see below). In February 2013, the Advisory Committee on Immunization Practices (ACIP) published updated recommendations for pregnant women, stating that: A dose of Tdap should be given to a pregnant woman during each pregnancy, regardless of the patients previous history of receiving Tdap. The optimal timing of this dose is between 27 and 36 weeks of gestation but it may be given at any time during the pregnancy. This dose should be given regardless of the interval since any previous dose of Tdap. A woman who did not get a dose of Tdap during her pregnancy, and has never received a dose of Tdap in the past, should get a dose of Tdap immediately post-partum. Women previously vaccinated with Tdap should not get this dose. A pregnant woman who is due for a routine 10-year Td booster, or for whom tetanus toxoid is indicated for wound management, should receive Tdap. Please see the Centers for Disease Control and Prevention (CDC) website for the most current ACIP recommendations: http://www.cdc.gov/vaccines/. Ohio School Requirement: All children entering school must have received a minimum of four doses of the DTaP vaccination series with a minimum of 4 doses if the last dose was received after the fourth birthday. A Tdap booster dose is required prior to entry to 7th grade.
ODH-IDCM
DIPTHERIA Page 4/Section 3
Revised 7/2013
Disease Fact Sheet
Diphtheria
What is diphtheria? Diphtheria is a disease caused by the bacteria Corynebacterium diphtheriae that affects the tonsils, throat, nose or skin. It is the toxin (poison) produced by the bacteria that causes the severe disease problems. Who gets diphtheria? The disease is often found among adults whose immunization was neglected, and is most severe in unimmunized or inadequately immunized individuals. How is diphtheria spread? Diphtheria is transmitted to others through close contact with the discharges from an infected persons nose, throat, eyes and skin lesions. Rarely transmission may occur after contact with articles soiled by the discharges from the nose, throat or skin lesions. What are the symptoms of diphtheria? Infection of the nose and throat causes symptoms such as fever, sore throat, and tiredness. The infection in the throat may cause a membrane to develop on the tonsils that could making breathing difficult for the individual. If significant toxin is produced by the bacteria, the individual can develop other complications, such as myocarditis (inflammation of heart muscle) and neuritis (inflammation of nerves). A diphtheria infection in the skin causes a scaling rash or ulcerative lesions. Generally the diphtheria bacteria found in recent cases of diphtheria skin infections has not produced the harmful toxin. How soon do symptoms appear? Symptoms usually appear 2 to 5 days after infection, with a range of 1 to 10 days. What are the complications associated with diphtheria? The diphtheria bacteria can produce a toxin that can spread from the primary site of infection (the throat) throughout the body. The toxin can cause complications such as myocarditis (inflammation of heart muscle), neuritis (inflammation of nerves), and blood disorders. Death occurs in 5 to 10% of infected individuals. When and for how long is a person able to spread diphtheria? Unless treated with antibiotics, people who are acutely infected with the diphtheria bacteria may be contagious for up to two weeks, but seldom more than four weeks. If the patient is treated with appropriate antibiotics, this can quickly stop the spread of the bacteria. Does past infection with diphtheria make a person immune? Recovery from diphtheria is not always followed by lasting immunity. Is there a vaccine for diphtheria? Yes. Children should be vaccinated against diphtheria with the DTaP (diphtheria toxoid in combination with tetanus toxoid and acellular pertussis) vaccine. This vaccine should be given at 2, 4, 6 and 15 to 18 months of age, and between 4 and 6 years of age. Adults with uncertain histories of a complete primary vaccination series with diphtheria and tetanus toxoid-containing vaccines should begin or complete a primary vaccination ODH-IDCM DIPTHERIA Page 5/Section 3 Revised 7/2013
series. Older children and adults who have completed the primary series should receive Td (tetanus/diphtheria) boosters every 10 years to maintain immunity. One lifetime dose of Tdap (tetanus, diphtheria, and acellular pertussis) is recommended for people 11 years of age and older as one of these boosters to provide protection against pertussis. Pregnancy is an exception to the one-dose recommendation. Please see the CDC for the most current Advisory Committee on Immunization Practices (ACIP) recommendations at the following website: http://www.cdc.gov/vaccines/. How can diphtheria be prevented? The single most effective control measure for diphtheria is maintaining the highest possible level of immunization in the community. Other methods of control include the prompt treatment of cases and surveillance for cases. What is the treatment for diphtheria? Certain antibiotics, such as penicillin and erythromycin, can be prescribed for the treatment of diphtheria. A diphtheria antitoxin is also used for treatment. What can be the effect of not being treated for diphtheria? If diphtheria goes untreated, serious complications such as paralysis, heart failure and blood disorders may occur. Death occurs in approximately 5 to 10% of all cases.
ODH-IDCM
DIPTHERIA Page 6/Section 3
Revised 7/2013
You might also like
- MDCH Diphtheria Guidelines Revise 2014Document5 pagesMDCH Diphtheria Guidelines Revise 2014TriponiaNo ratings yet
- Microlife GP - FINAL - Oct 2012Document2 pagesMicrolife GP - FINAL - Oct 2012HeartofEnglandNo ratings yet
- WHO Operational Protocols Diphtheria PDFDocument25 pagesWHO Operational Protocols Diphtheria PDFAnonymous hETtEBkk7No ratings yet
- DiphtheriaDocument18 pagesDiphtheriaShishir ShresthaNo ratings yet
- Diphtheria HandoutsDocument8 pagesDiphtheria HandoutsRachelle Mae DimayugaNo ratings yet
- By-Dr. Samarjeet Kaur JR-II BRD Med. College GKPDocument17 pagesBy-Dr. Samarjeet Kaur JR-II BRD Med. College GKPSamarjeet Kaur100% (1)
- Patofisiologi DifteriDocument11 pagesPatofisiologi DifteriicorrrNo ratings yet
- Nursing Care for Measles and DiphtheriaDocument5 pagesNursing Care for Measles and DiphtheriaChristian Eduard de DiosNo ratings yet
- What Is PlagueDocument3 pagesWhat Is Plagueanon_959000253No ratings yet
- Diphtheria Investigation GuidelineDocument20 pagesDiphtheria Investigation GuidelineIslammiyah Dewi YuniantiNo ratings yet
- East Africa University Bosaso, Puntland Somalia Faculty of Medicine Communicable Disease MR Buruj Ali SaladDocument42 pagesEast Africa University Bosaso, Puntland Somalia Faculty of Medicine Communicable Disease MR Buruj Ali SaladShaimaa AbdulkadirNo ratings yet
- Tetanus: Acute Communicable Disease Control Manual (B-73) Revision - February 2012Document2 pagesTetanus: Acute Communicable Disease Control Manual (B-73) Revision - February 2012Hisashi Ren MinamotoNo ratings yet
- Chickenpox, Diphtheria, Measles, Pertussis and PolioDocument17 pagesChickenpox, Diphtheria, Measles, Pertussis and PolioJennifer Alojado TunaNo ratings yet
- Treatment of Acute PharyngitisDocument4 pagesTreatment of Acute PharyngitisZafira Ananda RaishaNo ratings yet
- DIPHTHERIADocument6 pagesDIPHTHERIAblack_knight118No ratings yet
- Diphtheria Pertussis TetanusDocument43 pagesDiphtheria Pertussis TetanusPURVI BARIANo ratings yet
- Good Health in the Tropics: Advice to Travellers and SettlersFrom EverandGood Health in the Tropics: Advice to Travellers and SettlersNo ratings yet
- Case Study On Communicable DiseaseDocument15 pagesCase Study On Communicable DiseaseThiradevi BalakrisnanNo ratings yet
- Diptheria Converted 200726175940Document44 pagesDiptheria Converted 2007261759407dbnf4stjyNo ratings yet
- Diphtheria and Pertussis: Causes, Symptoms and PreventionDocument30 pagesDiphtheria and Pertussis: Causes, Symptoms and Preventioneman khammasNo ratings yet
- Diphtheria SlideDocument11 pagesDiphtheria Slideandre andreNo ratings yet
- NR 224 Week 1 Instuctor Unit 1 Questions and AnswersDocument7 pagesNR 224 Week 1 Instuctor Unit 1 Questions and AnswersJesse JohnsonNo ratings yet
- Timeout PosterDocument2 pagesTimeout Posterapi-138096780100% (1)
- Manage Seasonal FluDocument7 pagesManage Seasonal FluAJEET KUMAR PANDEYNo ratings yet
- TB Guidance Chapter 2Document15 pagesTB Guidance Chapter 2dindaNo ratings yet
- DynamedDocument41 pagesDynamedkaren AlvaradoNo ratings yet
- Local Media3061431616755544477Document42 pagesLocal Media3061431616755544477Kim Harold SalasNo ratings yet
- Pertussis: 1. Disease ReportingDocument18 pagesPertussis: 1. Disease Reportingzenagit123456No ratings yet
- Fresh H1N1 Guidelines 1 - 1-18Document15 pagesFresh H1N1 Guidelines 1 - 1-18Shahid IqbalNo ratings yet
- Tuberculosis Diagnosis, Causative Agent, TransmissionDocument58 pagesTuberculosis Diagnosis, Causative Agent, TransmissionMazinNo ratings yet
- Diphtheria: Prepared By: Patricia Johanna A. Tan, BSN 3ADocument18 pagesDiphtheria: Prepared By: Patricia Johanna A. Tan, BSN 3ApatriciaNo ratings yet
- Name: Carlo M. Yao Bachelor of Science in NursingDocument33 pagesName: Carlo M. Yao Bachelor of Science in Nursingcarlo24_briggsNo ratings yet
- Emergency MedDocument4 pagesEmergency MedbencleeseNo ratings yet
- Expanded Program For Immunization (EPI)Document70 pagesExpanded Program For Immunization (EPI)Erwin Jake Taguba100% (1)
- Trachoma; Tetanus; Leprosy (1)Document40 pagesTrachoma; Tetanus; Leprosy (1)Osama adel Mohamed SmadiNo ratings yet
- Diphtheria, Tetanus and PoliomyelitisDocument11 pagesDiphtheria, Tetanus and PoliomyelitisPriyanka SinghNo ratings yet
- Diphtheria Disease Reporting and Surveillance GuidelinesDocument10 pagesDiphtheria Disease Reporting and Surveillance GuidelinesAgustin IskandarNo ratings yet
- Infectious Pertusis-6 (Muhadharaty)Document5 pagesInfectious Pertusis-6 (Muhadharaty)dr.salam.hassaniNo ratings yet
- tetanusDocument6 pagestetanusImmelda Stella Medessoh DohoNo ratings yet
- 2 Review Diphtheria Results April2017 Final Clean PDFDocument20 pages2 Review Diphtheria Results April2017 Final Clean PDFchameleonNo ratings yet
- Journal Reading Tonsilitis Akut PDFDocument6 pagesJournal Reading Tonsilitis Akut PDFTaufiq HidayatNo ratings yet
- Lecture 5 - Whooping CoughDocument37 pagesLecture 5 - Whooping CoughShaimaa AbdulkadirNo ratings yet
- Swine Flu Swine Flu: Ministry of Health and Family Welfare Government of IndiaDocument19 pagesSwine Flu Swine Flu: Ministry of Health and Family Welfare Government of IndiagirismgNo ratings yet
- COMMUNICABLE DISEASES PREVENTIONDocument136 pagesCOMMUNICABLE DISEASES PREVENTIONCharmaine BonifacioNo ratings yet
- Management of PharyngotonsylitisDocument6 pagesManagement of PharyngotonsylitisAmeenu Isah HasheemNo ratings yet
- Australia Covid PpeDocument5 pagesAustralia Covid PpeAbidi HichemNo ratings yet
- Annexure-XX Clinical Management Protocol: (Novel Influenza A H1N1)Document3 pagesAnnexure-XX Clinical Management Protocol: (Novel Influenza A H1N1)Ramadi PrameelaNo ratings yet
- 420 052 Guideline DiphtheriaDocument12 pages420 052 Guideline DiphtheriaLeo RinaldiNo ratings yet
- Update On Covid 19Document3 pagesUpdate On Covid 19Savitha NarayanNo ratings yet
- BMJ BMJ: British Medical Journal: This Content Downloaded From 103.25.55.252 On Mon, 23 May 2016 05:18:53 UTCDocument5 pagesBMJ BMJ: British Medical Journal: This Content Downloaded From 103.25.55.252 On Mon, 23 May 2016 05:18:53 UTCNurul BariyyahNo ratings yet
- Diphtheria JellyDocument23 pagesDiphtheria JellyRexaurus EncarriosusNo ratings yet
- Diphtheria Pertussis TetanusDocument43 pagesDiphtheria Pertussis Tetanuspnalinl108No ratings yet
- Tetanus: HistoryDocument15 pagesTetanus: HistorydanielleNo ratings yet
- Pertusis 2Document21 pagesPertusis 2AbhishekNo ratings yet
- Dr. Nadia Aziz C.A.B.C.M Baghdad Medical CollegeDocument39 pagesDr. Nadia Aziz C.A.B.C.M Baghdad Medical CollegeMazinNo ratings yet
- Immunization EPI Huda 201212Document5 pagesImmunization EPI Huda 201212Aerish TupazNo ratings yet
- Pulmonary Tuberculosis (PTB)Document6 pagesPulmonary Tuberculosis (PTB)carls burg a. resurreccion100% (2)
- AIRBORNE DISEASESDocument25 pagesAIRBORNE DISEASESAyro Business CenterNo ratings yet
- Control of Viral Diseases: Derek WongDocument43 pagesControl of Viral Diseases: Derek WongAyioKunNo ratings yet
- Health Advice and Immunizations for TravelersFrom EverandHealth Advice and Immunizations for TravelersNo ratings yet
- Buku UKDIDocument247 pagesBuku UKDILuna WhiteNo ratings yet
- Smart AttackDocument1 pageSmart AttackLuna WhiteNo ratings yet
- HIV Infection and The CNS: Stephen J. Gluckman, M.DDocument36 pagesHIV Infection and The CNS: Stephen J. Gluckman, M.DLuna WhiteNo ratings yet
- Chest Imaging and Anatomy (2010)Document47 pagesChest Imaging and Anatomy (2010)Luna WhiteNo ratings yet
- What Is Diphtheria?Document2 pagesWhat Is Diphtheria?Luna WhiteNo ratings yet
- Radiological Feature of Patien TB With HIV POSTIVE and HIV NEGATIVEDocument4 pagesRadiological Feature of Patien TB With HIV POSTIVE and HIV NEGATIVELuna WhiteNo ratings yet
- BONE SCAN - Chest Imaging (2010)Document38 pagesBONE SCAN - Chest Imaging (2010)Luna WhiteNo ratings yet
- Introduction For CXRDocument53 pagesIntroduction For CXRLuna WhiteNo ratings yet
- Introduction For CXRDocument53 pagesIntroduction For CXRLuna WhiteNo ratings yet
- CXR (2010 C1)Document103 pagesCXR (2010 C1)anaskabahaNo ratings yet
- Everything You Need To Know About AllergiesDocument26 pagesEverything You Need To Know About AllergiesGiuliana FloresNo ratings yet
- ASTD PRODUCT LIST 2020Document2 pagesASTD PRODUCT LIST 2020midoNo ratings yet
- 10 Communicable DiseasesDocument3 pages10 Communicable DiseasesPauline de VeraNo ratings yet
- Metoprolol and AmiodaroneDocument5 pagesMetoprolol and AmiodaroneNolte BombayNo ratings yet
- Invasive Group A Streptococcal Disease Fact SheetDocument2 pagesInvasive Group A Streptococcal Disease Fact SheetCityNewsTorontoNo ratings yet
- Integrated Management of Childhood Illness: Child Aged 2 Months Up To 5 YearsDocument44 pagesIntegrated Management of Childhood Illness: Child Aged 2 Months Up To 5 YearsJulio Iñigo López100% (22)
- NAMA OBAT DAN HARGADocument59 pagesNAMA OBAT DAN HARGAtutikNo ratings yet
- IMPORTANT: The Original of This Form Is To Be Kept by The Seafarer. A Copy Must Be Kept by The ClinicDocument2 pagesIMPORTANT: The Original of This Form Is To Be Kept by The Seafarer. A Copy Must Be Kept by The ClinicTigreal MLNo ratings yet
- Refkas CondylomaAccuminataDocument18 pagesRefkas CondylomaAccuminatamichelle1945No ratings yet
- Lyme Disease Brochure TemplateDocument2 pagesLyme Disease Brochure Templatetburkle50% (2)
- Daftar Nama ObatDocument5 pagesDaftar Nama ObatGabriyah HamzahNo ratings yet
- Mapping Cempaka Ii Obstetri Selasa, 7 Juli 2020: HYS 207.2 SNR 207.3 DST 209.1 MGP 211.4 BYM 209.3Document4 pagesMapping Cempaka Ii Obstetri Selasa, 7 Juli 2020: HYS 207.2 SNR 207.3 DST 209.1 MGP 211.4 BYM 209.3Ayu Putri HitasariNo ratings yet
- BiodataDocument15 pagesBiodataRiris SihotangNo ratings yet
- Daftar Formulariumobat SementaraDocument26 pagesDaftar Formulariumobat SementarafarmasiNo ratings yet
- ImpetigoDocument1 pageImpetigoshailesh284No ratings yet
- EBM-Diagnosis & SkriningDocument37 pagesEBM-Diagnosis & SkriningIndah MaulidawatiNo ratings yet
- Sexually Transmitted DiseasesDocument120 pagesSexually Transmitted DiseasesGliza Jane100% (4)
- Newborn Growth Chart and Resuscitation GuidelinesDocument125 pagesNewborn Growth Chart and Resuscitation GuidelinesShelleyVanessaAgudoNo ratings yet
- Regimen for paediatric ALL risk groupsDocument5 pagesRegimen for paediatric ALL risk groupsGlobal cancerNo ratings yet
- Contraindications: DRUG STUDY: MetronidazoleDocument1 pageContraindications: DRUG STUDY: MetronidazoleKimberly OlarteNo ratings yet
- Stok 5 April 2021 Ogb Dexa: Stock Product - DescDocument8 pagesStok 5 April 2021 Ogb Dexa: Stock Product - DescBelza ChristianNo ratings yet
- Jurnal Vaksin HPVDocument9 pagesJurnal Vaksin HPVlitaayuningdyahNo ratings yet
- Unicom Product and Price ListDocument6 pagesUnicom Product and Price ListImanoelClousAndohNo ratings yet
- Child's Abdominal Pain Admitting ConferenceDocument24 pagesChild's Abdominal Pain Admitting ConferenceRaul MangrobangNo ratings yet
- Nahdi Pharma FileDocument477 pagesNahdi Pharma FileSarah JeanNo ratings yet
- Drug Summary Table: Chapter 37 Pharmacology of Cancer: Genome Synthesis, Stability, and MaintenanceDocument6 pagesDrug Summary Table: Chapter 37 Pharmacology of Cancer: Genome Synthesis, Stability, and MaintenanceRita GameiroNo ratings yet
- MCCQE - 1 - November 2003 1. For Nocturnal Enuresis How Long You ...Document71 pagesMCCQE - 1 - November 2003 1. For Nocturnal Enuresis How Long You ...Vinil SaratchandranNo ratings yet
- Penguins Medicine August-SeptumberDocument215 pagesPenguins Medicine August-SeptumberKhattabNo ratings yet
- Hypertension in Pregnancy: Executive SummaryDocument10 pagesHypertension in Pregnancy: Executive SummaryimeldaNo ratings yet
- Case Iron Deficiency AnemiaDocument11 pagesCase Iron Deficiency AnemiaNur Amaleeza Abdul MananNo ratings yet