Professional Documents
Culture Documents
Kidney Stones
Uploaded by
Roanne LaguaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kidney Stones
Uploaded by
Roanne LaguaCopyright:
Available Formats
Nephrolithiasis is a common disease that is estimated to produce medical costs of $2.1 billion per year in the United States.
[4] Nephrolithiasis specifically refers to calculi in the kidneys, but this article discusses both renal calculi (see the first image below) and ureteral calculi (ureterolithiasis; see the second image below). Ureteral calculi almost always originate in the kidneys, although they may continue to grow once they lodge in the ureter.
Small renal calculus that would likely respond to extracorporeal
shockwave lithotripsy. Distal ureteral stone observed through a small, rigid ureteroscope prior to ballistic lithotripsy and extraction. The small caliber and excellent optics of today's endoscopes greatly facilitate minimally invasive treatment of urinary stones.
Urinary tract stone disease has been a part of the human condition for millennia; in fact, bladder and kidney stones have even been found in Egyptian mummies. Some of the earliest recorded medical texts and figures depict the treatment of urinary tract stone disease. Acute renal colic is probably the most excruciatingly painful event a person can endure. Striking without warning, the pain is often described as being worse than childbirth, broken bones, gunshot wounds, burns, or surgery. Renal colic affects approximately 1.2 million people each year and accounts for approximately 1% of all hospital admissions. Most active emergency departments (EDs) manage patients with acute renal colic every day, depending on the hospitals patient population. Initial management consists of proper diagnosis, prompt initial treatment, and appropriate consultations, but concurrently efforts should be directed towards patient education, including initial preventive therapy measures. Although nephrolithiasis is not a common cause of renal failure, certain problems, such as preexisting azotemia and solitary functional kidneys, clearly present a higher risk of additional renal damage. Other high-risk factors include diabetes, struvite and/or staghorn calculi, and various hereditary diseases such as primary hyperoxaluria, Dent disease, cystinuria, and polycystic kidney disease. Spinal cord injuries and similar functional or anatomical urological anomalies also predispose patients with kidney stones to an increased risk of renal failure.
Recurrent obstruction, especially when associated with infection and tubular epithelial or renal interstitial cell damage from microcrystals, may activate the fibrogenic cascade, which is mainly responsible for the actual loss of functional renal parenchyma. For other discussions on urolithiasis and nephrolithiasis, see Pediatric Urolithiasis, as well as Imaging Urinary Calculi, Hypercalciuria, Hyperoxaluria, andHypocitraturia.
Pathophysiology
Formation of stones
Urinary tract stone disease, depicted below, is likely caused by two basic phenomena. The first phenomenon is supersaturation of the urine by stone-forming constituents, including calcium, oxalate, and uric acid. Crystals or foreign bodies can act as nidi, upon which ions from the supersaturated urine form microscopic crystalline structures. The resulting calculi give rise to symptoms when they become impacted within the ureter as they pass toward the urinary bladder. The overwhelming majority of renal calculi contain calcium. Uric acid calculi and crystals of uric acid, with or without other contaminating ions, comprise the bulk of the remaining minority. Other, less frequent stone types include cystine, ammonium acid urate, xanthine, dihydroxyadenine, and various rare stones related to precipitation of medications in the urinary tract. Supersaturation of the urine is likely the underlying cause of uric and cystine stones, but calcium-based stones (especially calcium oxalate stones) may have a more complex etiology. The second phenomenon, which is most likely responsible for calcium oxalate stones, is deposition of stone material on a renal papillary calcium phosphate nidus, typically a Randall plaque (which are always composed of calcium phosphate). Evan et al recently proposed this model based on evidence accumulating from several laboratories. [5] Calcium phosphate precipitates in the basement membrane of the thin loops of Henle, erodes into the interstitium, and then accumulates in the subepithelial space of the renal papilla. The subepithelial deposits, which have long been known as Randall plaques, eventually erode through the papillary urothelium. Stone matrix, calcium phosphate, and calcium oxalate gradually deposit on the substrate to create a urinary calculus.
Development of renal colic pain and renal damage
The colicky-type pain known as renal colic usually begins in the upper lateral midback over the costovertebral angle and occasionally subcostally. It radiates inferiorly and anteriorly toward the groin. The pain generated by renal colic is primarily caused by the dilation, stretching, and spasm caused by the acute ureteral obstruction. (When a severe but chronic obstruction develops, as in some types of cancer, it is usually painless.) In the ureter, an increase in proximal peristalsis through activation of intrinsic ureteral pacemakers may contribute to the perception of pain. Muscle spasm, increased proximal peristalsis, local inflammation, irritation, and edema at the site of obstruction may contribute to the development of pain through chemoreceptor activation and stretching of submucosal free nerve endings. The term "renal colic" is actually a misnomer, because this pain tends to remain constant, whereas intestinal or biliary colic is usually somewhat intermittent and often comes in waves. The pattern of the pain depends on the individuals pain threshold and perception and on the speed and degree of the changes in hydrostatic pressure within the proximal ureter and renal pelvis. Ureteral peristalsis, stone migration, and tilting or twisting of the stone with subsequent intermittent obstructions may cause exacerbation or renewal of the renal colic pain.
The severity of the pain depends on the degree and site of the obstruction, not on the size of the stone. A patient can often point to the site of maximum tenderness, which is likely to be the site of the ureteral obstruction (see the image below).
Nephrolithiasis: acute renal colic. Distribution of renal and ureteral pain.
A stone moving down the ureter and causing only intermittent obstruction actually may be more painful than a stone that is motionless. A constant obstruction, even if high grade, allows for various autoregulatory mechanisms and reflexes, interstitial renal edema, and pyelolymphatic and pyelovenous backflow to help diminish the renal pelvic hydrostatic pressure, which gradually helps reduce the pain. The interstitial renal edema produced stretches the renal capsule, enlarges the kidney (ie, nephromegaly), and increases renal lymphatic drainage. (Increased capillary permeability facilitates this edema.) It may also reduce the radiographic density of the affected kidneys parenchyma when viewed on a noncontrast CT scan. Distention of the renal pelvis initially stimulates ureteral hyperperistalsis, but this diminishes after 24 hours, as does renal blood flow. Peak hydrostatic renal pelvis pressure is attained within 2-5 hours after a complete obstruction. Within the first 90 minutes of a complete ureteral obstruction, afferent preglomerular arteriolar vasodilation occurs, which temporarily increases renal blood flow. Between 90 minutes and 5 hours after the obstruction, renal blood flow starts to decrease while intraureteral pressure continues to rise. By 5 hours after a complete obstruction, both renal blood flow and intraluminal ureteral pressure decrease on the affected side. Renal blood flow decreases to approximately 50% of normal baseline levels after 72 hours, to 30% after 1 week, to 20% after 2 weeks, and to 12% after 8 weeks. By this point, intraureteral pressures have returned to normal, but the proximal ureteral dilation remains and ureteral peristalsis is minimal. Interstitial edema of the affected kidney actually enhances fluid reabsorption, which helps to increase the renal lymphatic drainage to establish a new, relatively stable, equilibrium. At the same time, renal blood flow increases in the contralateral kidney as renal function decreases in the obstructed unit. In summary, by 24 hours after a complete ureteral obstruction, the renal pelvic hydrostatic pressure has dropped because of (1) a reduction in ureteral peristalsis; (2) decreased renal arterial vascular flow, which causes a corresponding drop in urine production on the affected side; and (3) interstitial renal edema, which leads to a marked increase in renal lymphatic drainage. Additionally, as the ureter proximal to the stone distends, some urine can sometimes flow around the obstruction, relieving the proximal hydrostatic pressure and establishing a stable, relatively painless equilibrium. These factors explain why severe renal colic pain typically lasts less than 24 hours in the absence of any infection or stone movement. Whether calyceal stones cause pain continues to be controversial. In general, in the absence of infection, how a renal stone causes pain remains unclear, unless the stone also causes obstruction. Arguably, proving that a calyceal stone is causing an obstruction can be difficult. However, a stone trapped in a calyx plausibly could block the outflow tract from that calyx, causing an obstruction and subsequent pain.
Experimental studies in animals have suggested that renal damage may begin within 24 hours of a complete obstruction and that permanent kidney deterioration starts within 5-14 days. Whereas some practitioners wait several months for a stone to pass in an asymptomatic patient, others argue that permanent damage is occurring as long as intervention is delayed. Based on personal experience and anecdotal cases, the author recommends waiting no longer than 4 weeks for a stone to pass spontaneously before considering intervention. Convincing asymptomatic patients of the need for surgical intervention may be difficult in the absence of a clear consensus in the urological community about the length of time to wait before surgical stone removal, fragmentation, or bypass. If only a partial obstruction is present, the same changes occur, but to a lesser degree and over a longer period. Proximal ureteric and renal pelvic hydrostatic pressures tend to remain elevated longer, and ureteral peristalsis does not diminish as quickly. If the increased pressure is sufficient to establish a reasonable flow beyond the obstructing stone, glomerular filtration and renal blood flow approximates reference range baseline levels, although pain may be ongoing.
Anatomy
The basic anatomy of the ureter is as follows (see the image below).
Nephrolithiasis: acute renal colic. Anatomy of the ureter.
Most of the pain receptors of the upper urinary tract responsible for the perception of renal colic are located submucosally in the renal pelvis, calices, renal capsule, and upper ureter. Acute distention seems to be more important in the development of the pain of acute renal colic than spasm, local irritation, or ureteral hyperperistalsis. Stimulation of the peripelvic renal capsule causes flank pain, while stimulation of the renal pelvis and calices causes typical renal colic (see the image below). Mucosal irritation can be sensed in the renal pelvis to some degree by chemoreceptors, but this irritation is thought to play only a minor role in the perception of renal or ureteral colic.
Nephrolithiasis: acute renal colic. Renal colic and flank pain.
Renal pain fibers are primarily preganglionic sympathetic nerves that reach spinal cord levels T11 to L-2 through the dorsal nerve roots (see the images below). Aortorenal, celiac, and inferior mesenteric ganglia are also involved. Spinal transmission of renal pain signals occurs primarily through the ascending spinothalamic tracts.
Nephrolithiasis: acute renal colic. Nerve supply of the kidney.
Nephrolithiasis: acute renal colic. Nerve supply of the kidney.
In the lower ureter, pain signals are also distributed through the genitofemoral and ilioinguinal nerves (see the image below). The nervi erigentes, which innervate the intramural ureter and bladder, are responsible for some of the bladder symptoms that often accompany an intramural ureteral calculus.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Drummond Methods For The Economic Evaluation of Health Care Programmes PDFDocument461 pagesDrummond Methods For The Economic Evaluation of Health Care Programmes PDFGerman Camilo Viracacha Lopez80% (10)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Nails Diagnosis, Therapy, Surgery Richard K Scher MD, C Ralph DanielDocument319 pagesNails Diagnosis, Therapy, Surgery Richard K Scher MD, C Ralph DanieldrNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Case Study On BurnsDocument16 pagesCase Study On BurnsRoanne Lagua100% (2)
- Case Study On BurnsDocument16 pagesCase Study On BurnsRoanne Lagua100% (2)
- Form 1 - HEARS Field Report As of Jan 25 - 0Document1 pageForm 1 - HEARS Field Report As of Jan 25 - 0Roanne Lagua100% (1)
- Associate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and GynecologyDocument31 pagesAssociate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and Gynecologyivan0% (1)
- MUNICIPALITY OF PENABLANCA HEALTH REPORTDocument4 pagesMUNICIPALITY OF PENABLANCA HEALTH REPORTRoanne LaguaNo ratings yet
- Field Health Information System PDFDocument36 pagesField Health Information System PDFBarbie Beronio100% (1)
- Presentation in Ovarian New GrowthDocument29 pagesPresentation in Ovarian New GrowthRoanne Lagua0% (1)
- Music and Art TherapyDocument21 pagesMusic and Art TherapyRoanne LaguaNo ratings yet
- Jeros 2Document298 pagesJeros 2Roanne LaguaNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanRoanne LaguaNo ratings yet
- Electroconvulsive TherapyDocument9 pagesElectroconvulsive TherapyRoanne LaguaNo ratings yet
- Penicillin-resistant Staphylococcal Infections TreatmentDocument2 pagesPenicillin-resistant Staphylococcal Infections TreatmentRoanne LaguaNo ratings yet
- Afpmc Casafpe FinalDocument18 pagesAfpmc Casafpe FinalRoanne LaguaNo ratings yet
- Uterine Bleeding-A Case StudyDocument4 pagesUterine Bleeding-A Case StudyRoanne Lagua0% (1)
- Medical Surgical Nursing ExamsDocument4 pagesMedical Surgical Nursing ExamsRoanne LaguaNo ratings yet
- Case of Romualdez Vs COMELECDocument126 pagesCase of Romualdez Vs COMELECRoanne LaguaNo ratings yet
- Myocardial IschemiaDocument7 pagesMyocardial IschemiaRoanne LaguaNo ratings yet
- Leadership DefinitionsDocument2 pagesLeadership DefinitionsRoanne LaguaNo ratings yet
- Case Analysis On Abnormal Uterine BleedingDocument9 pagesCase Analysis On Abnormal Uterine BleedingRoanne LaguaNo ratings yet
- Nlex For Endocrine SystemDocument6 pagesNlex For Endocrine SystemRoanne LaguaNo ratings yet
- Nclex ReviewerDocument5 pagesNclex ReviewerRoanne LaguaNo ratings yet
- PlagiarismDocument3 pagesPlagiarismRoanne LaguaNo ratings yet
- Life of Rizal in LondonDocument7 pagesLife of Rizal in LondonRoanne LaguaNo ratings yet
- Coping With The Environment: Danish Companies and Their Experiences With ISO 14001/EMASDocument10 pagesCoping With The Environment: Danish Companies and Their Experiences With ISO 14001/EMASRoanne LaguaNo ratings yet
- Exam in Jose RizalDocument1 pageExam in Jose RizalRoanne Lagua50% (2)
- The Philippine LiteratureDocument35 pagesThe Philippine LiteratureRoanne Lagua100% (1)
- Accoplishment ReportDocument2 pagesAccoplishment ReportRoanne LaguaNo ratings yet
- In Medias Res Flashbacks TrumpetDocument3 pagesIn Medias Res Flashbacks TrumpetRoanne LaguaNo ratings yet
- ResearchDocument6 pagesResearchRoanne LaguaNo ratings yet
- She's My Personal Slave (Finished)Document355 pagesShe's My Personal Slave (Finished)renzeiaNo ratings yet
- E.2 Bipolar PPT 2017Document42 pagesE.2 Bipolar PPT 2017abrihamNo ratings yet
- SickLeaveCertificate With and Without Diagnosis 20240227 144109Document2 pagesSickLeaveCertificate With and Without Diagnosis 20240227 144109Sawad SawaNo ratings yet
- Atopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)Document289 pagesAtopic Dermatitis - The Epidemiology, Causes and Prevention of Atopic Eczema (PDFDrive)NguyenDinh NinhNo ratings yet
- Tall StatureDocument24 pagesTall StaturedianmutiaNo ratings yet
- NP 5 Set BBBBBDocument31 pagesNP 5 Set BBBBBGo IdeasNo ratings yet
- Seminar ON: Birth InjuriesDocument38 pagesSeminar ON: Birth Injuriesvishnu100% (1)
- 155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Document8 pages155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Verico PratamaNo ratings yet
- Clinical Nursing Skills & TechniquesDocument6 pagesClinical Nursing Skills & TechniquesTimi BCNo ratings yet
- Orthopaedic Surgery Fractures and Dislocations: Tomas Kurakovas MF LL Group 29Document13 pagesOrthopaedic Surgery Fractures and Dislocations: Tomas Kurakovas MF LL Group 29Tomas Kurakovas100% (1)
- Aesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Document60 pagesAesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Drhisham AttiaNo ratings yet
- Cytotoxins Pose Risks for Healthcare WorkersDocument2 pagesCytotoxins Pose Risks for Healthcare WorkersMaria Nesen NuezNo ratings yet
- Four Humors Theory in Unani MedicineDocument4 pagesFour Humors Theory in Unani MedicineJoko RinantoNo ratings yet
- New Technologies Related To Public Health Electronic InformationDocument22 pagesNew Technologies Related To Public Health Electronic InformationKhams TolentinoNo ratings yet
- Amanita PhalloidesDocument15 pagesAmanita PhalloidesJair Carrillo100% (1)
- Patient'S Peripheral Arterial Disease Risk FactorsDocument2 pagesPatient'S Peripheral Arterial Disease Risk FactorsKrystel BatinoNo ratings yet
- Classification of FracturesDocument26 pagesClassification of FracturesHoney May Rollan VicenteNo ratings yet
- Dialog Convincing, Consoling, Persuading, Encouraging, Apologizing, Disclaiming, RequestingDocument4 pagesDialog Convincing, Consoling, Persuading, Encouraging, Apologizing, Disclaiming, RequestingmeliaNo ratings yet
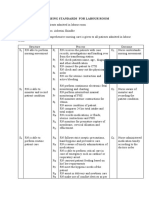
- Nursing Standards for Labour RoomDocument3 pagesNursing Standards for Labour RoomRenita ChrisNo ratings yet
- Teaching Plan for HypertensionDocument2 pagesTeaching Plan for HypertensionAno BaIto100% (1)
- Detailed drug study of metronidazole for anaerobic infectionsDocument5 pagesDetailed drug study of metronidazole for anaerobic infectionsKarl Vincent SosoNo ratings yet
- Perioperative Management of Hyperglycemia and Diabetes in Cardiac Surgery PatientsDocument24 pagesPerioperative Management of Hyperglycemia and Diabetes in Cardiac Surgery PatientsRudi HaryantoNo ratings yet
- Miliaria Pustulosa (Infetrop)Document11 pagesMiliaria Pustulosa (Infetrop)Muhammad mukramNo ratings yet
- Human DrugsDocument1,620 pagesHuman DrugsMohamed GameelNo ratings yet
- Aiims Hospital Disaster PlanDocument6 pagesAiims Hospital Disaster PlanSujatha J JayabalNo ratings yet
- Cali Naturals CBDDocument7 pagesCali Naturals CBDSomya MishraNo ratings yet