Professional Documents
Culture Documents
Chart 38-3
Uploaded by
MelissaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chart 38-3
Uploaded by
MelissaCopyright:
Available Formats
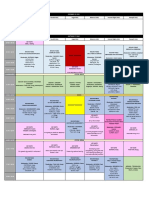
CHART 383
Procedure for Continuous ECG Monitoring
Choose an area to place the electrodes where there are no bony prominences, thick muscles, or skin folds, because these areas are prone to produce noncardiac waveforms and interference. Prepare the skin for electrode placement by making sure that it is clean, dry, and free of hair. It may be necessary to shave the chest area of male patients. Remove dead skin cells to improve electrical conductivity by rubbing the skin with the rough patch on the back of the electrode, a dry washcloth, or a gauze pad. The skin will become reddened with the rubbing; be careful not to cause skin breakdown. Wipe the skin with an alcohol sponge if skin is oily or a moist wipe; allow it to air dry. Make sure that the electrode pads are moistened with conducting gel prior to placing them on the chest to increase electrical conductivity. A dry electrode is not effective for conducting the electrical activity. When the electrode becomes dry or loose, it needs to be replaced. If the skin around the electrode becomes irritated the electrode must be removed and relocated. Position electrodes on the chest wall at prescribed locations depending on the lead or leads being monitored. Change electrodes when wet, poor contact, unclear tracing, and/or every 48 hours to avoid skin irritation.
Electrode Attachment
Lead Wire and Cable Connection
Connect the electrode to the lead wire, which is approximately 16 inches long. Typically a snap attaches the lead wire to the electrode. The lead wires are color coded to represent positive, negative, and ground leads. Attach the opposite end of the lead wire to the cable. The cable has individual color-coded receptacles or holes for each lead wire.
Monitor Connection and Adjustment
Attach the cable to the monitor. Adjust the monitor to increase the size of the PQRST complex for more accurate interpretation. Read the operating instructions for the specific brand of monitor prior to use. Always leave the alarm on. Recognize that the alarms have upper and lower heart rate limits. Set the alarm approximately 20 beats above and below the patients resting intrinsic heart rate. Follow institutional policy, if present, to determine different alarm limits. Be aware that when the alarm sounds, the first nursing responsibility is to check the patient. Recognize that movement by the patient may cause the alarm to sound falsely.
Alarm Setting
Documentation
Document lead used. Document PR interval, QRS width, QT interval, ectopic beats, and type of rhythm/dysrhythmia. Record ECG changes and patients response to changes.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- 3096 3113985 Flash Mobber Info 2024Document1 page3096 3113985 Flash Mobber Info 2024MelissaNo ratings yet
- CompPlan Certified US-ENDocument1 pageCompPlan Certified US-ENMelissaNo ratings yet
- 1 Patient FloatDocument2 pages1 Patient FloatMelissaNo ratings yet
- Keys To Nursing Success Chapter 2Document32 pagesKeys To Nursing Success Chapter 2MelissaNo ratings yet
- (Regular/Irregular) Location:: Cardiovascular: GenitourinaryDocument1 page(Regular/Irregular) Location:: Cardiovascular: GenitourinaryMelissaNo ratings yet
- Position on assisting with medicationsDocument2 pagesPosition on assisting with medicationsMelissaNo ratings yet
- Nursing Management Concept MapDocument1 pageNursing Management Concept MapXy-Za Roy Marie100% (1)
- 2023 R1 USEN ConsultantGuide 4webDocument28 pages2023 R1 USEN ConsultantGuide 4webMelissaNo ratings yet
- Benefits SummaryDocument27 pagesBenefits SummaryMelissaNo ratings yet
- 25 Psychiatric Nursing Mnemonics and Tricks - NurseBuffDocument24 pages25 Psychiatric Nursing Mnemonics and Tricks - NurseBuffMelissa100% (3)
- Keys To Nursing Success Chapter 3Document34 pagesKeys To Nursing Success Chapter 3MelissaNo ratings yet
- #2 CM Nursing DXDocument1 page#2 CM Nursing DXMelissaNo ratings yet
- The Complexities of Care: Nursing Reconsidered: Edited by Sioban Nelson and Suzanne GordonDocument0 pagesThe Complexities of Care: Nursing Reconsidered: Edited by Sioban Nelson and Suzanne GordonMelissaNo ratings yet
- Keys To Nursing Success Chapter 1Document42 pagesKeys To Nursing Success Chapter 1Melissa100% (2)
- hippocrateshipaaII PDFDocument8 pageshippocrateshipaaII PDFMelissaNo ratings yet
- PDFDocument6 pagesPDFMelissaNo ratings yet
- Personality Disorders - PartyDocument3 pagesPersonality Disorders - PartyMelissaNo ratings yet
- Nursing ProcessDocument1 pageNursing ProcessMelissaNo ratings yet
- Chart 40-9Document1 pageChart 40-9MelissaNo ratings yet
- Chart 40-8Document1 pageChart 40-8MelissaNo ratings yet
- Causes of Intimal Vessel Wall Injury: CHART 40-2Document1 pageCauses of Intimal Vessel Wall Injury: CHART 40-2MelissaNo ratings yet
- Differential Diagnosis of Chest Pain ChartDocument1 pageDifferential Diagnosis of Chest Pain ChartMelissaNo ratings yet
- Chart 38-8Document1 pageChart 38-8MelissaNo ratings yet
- Chest Pain Causes ChartDocument1 pageChest Pain Causes ChartMelissaNo ratings yet
- Increased Oxygen Demand and Decreased Supply FactorsDocument1 pageIncreased Oxygen Demand and Decreased Supply FactorsMelissaNo ratings yet
- Nursing ProcessDocument1 pageNursing ProcessMelissaNo ratings yet
- Genetic Considerations For Hypercholesterolemia: Unit 8Document1 pageGenetic Considerations For Hypercholesterolemia: Unit 8MelissaNo ratings yet
- Laboratory Test Goals to Prevent CADDocument1 pageLaboratory Test Goals to Prevent CADMelissaNo ratings yet
- AV Block Dysrhythmias GuideDocument2 pagesAV Block Dysrhythmias GuideMelissaNo ratings yet
- Ventricular Dysrhythmias: Etiology, Physical Assessment, and TreatmentDocument2 pagesVentricular Dysrhythmias: Etiology, Physical Assessment, and TreatmentMelissaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Sonus CompleteDocument4 pagesSonus CompleteSonusNo ratings yet
- Comparative Study of Hepatoprotective Activity of Proprietary Polyherbal Preparations Against paraDocument5 pagesComparative Study of Hepatoprotective Activity of Proprietary Polyherbal Preparations Against paraassemNo ratings yet
- Manage High-Risk PregnanciesDocument33 pagesManage High-Risk PregnanciesDakshayini MbNo ratings yet
- Arogya KavachaDocument5 pagesArogya KavachaiamgodrajeshNo ratings yet
- Hormone Levels For Fertility Patients1Document4 pagesHormone Levels For Fertility Patients1Kunbi Santos-ArinzeNo ratings yet
- Controversias en El Manejo de Las Fracturas Abiertas (2014)Document7 pagesControversias en El Manejo de Las Fracturas Abiertas (2014)J. Adrian NogueraNo ratings yet
- OB Case Presentation Inforgraphic Garcia-GumbeDocument2 pagesOB Case Presentation Inforgraphic Garcia-GumbeLara GeeNo ratings yet
- Cwe Nephrotic SnydromeDocument12 pagesCwe Nephrotic SnydromeFariezuan HamidNo ratings yet
- Pre-Surgical Hand WashDocument2 pagesPre-Surgical Hand WashRatna LamaNo ratings yet
- Lip LesionsDocument4 pagesLip LesionsGhada AlqrnawiNo ratings yet
- 2019 International Symposium on Pediatric Audiology ScheduleDocument3 pages2019 International Symposium on Pediatric Audiology ScheduleEulalia JuanNo ratings yet
- Cleaning Allergen Polyurethane 1Document128 pagesCleaning Allergen Polyurethane 1Yudhi AdiNo ratings yet
- 3595 Article 14344 1 10 20230529Document4 pages3595 Article 14344 1 10 20230529ReendiIshqNo ratings yet
- Talk WslidesDocument43 pagesTalk WslidesraydonalNo ratings yet
- Pharmaceutical Assasination (Partial)Document14 pagesPharmaceutical Assasination (Partial)jamie_clark_2100% (2)
- The XbarM Control ProgramDocument7 pagesThe XbarM Control ProgramLaboratório Jofre CohenNo ratings yet
- Sonopuls 490 User ManualDocument57 pagesSonopuls 490 User ManualMaryam BushraNo ratings yet
- StomatitisDocument74 pagesStomatitisZahoor ZaidiNo ratings yet
- Heat Illness Types, Causes, Symptoms and TreatmentsDocument46 pagesHeat Illness Types, Causes, Symptoms and TreatmentsDewi Pertiwi Pertiwi0% (1)
- Prospect Frisium in EnglezaDocument4 pagesProspect Frisium in EnglezaTanasa AdrianNo ratings yet
- List of ReferencesDocument3 pagesList of ReferencesRave MiradoraNo ratings yet
- Gunshot Wound ScenariosDocument19 pagesGunshot Wound Scenariossweetwaffle50% (2)
- E-Poster PresentationDocument1 pageE-Poster PresentationOvamelia JulioNo ratings yet
- Problem SetDocument2 pagesProblem Sethlc34No ratings yet
- Drug Study NifedipineDocument3 pagesDrug Study NifedipineJanzelvine Lee MontenegroNo ratings yet
- Hip FractureDocument1 pageHip FractureHAILIE23100% (3)
- Porose Gravidez e Puerperio 2021Document15 pagesPorose Gravidez e Puerperio 2021Ben-Hur AlbergariaNo ratings yet
- Ecart Medications and EquipmentDocument9 pagesEcart Medications and EquipmentJan Philippe BelandoNo ratings yet
- Enterobacter QuizDocument8 pagesEnterobacter QuizDan Paolo Sanchez100% (2)
- 2019 - E Danse, Dragean, S Van Nieuwenhove Et Al - Imaging of Acute Appendicitis For Adult PatientsDocument10 pages2019 - E Danse, Dragean, S Van Nieuwenhove Et Al - Imaging of Acute Appendicitis For Adult PatientsdaniprmnaNo ratings yet