Professional Documents
Culture Documents
Endometriosis
Uploaded by
banyenye25Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endometriosis
Uploaded by
banyenye25Copyright:
Available Formats
[DISORDERS OF THE REPRODUCTIVE SYSTEM] October 5, 2013
ENDOMETRIOSIS
A. Definition - It refers to the presence of the endometrial tissue in extrauterine sites. The most common sites for endometriosis includes the ovary, fallopian tubes, uterine ligaments, rectovaginal septum, umbilicus, vagina, vulva and in the hernial sac. B. Etiology and Risk Factors It has NO single, clearly identifiable cause THEORIES OF CAUSATION: Hormonal influence - The initial genesis of endometriosis, its further development depends on the presence of hormones, mainly estrogen. Endometriosis is rarely seen before puberty and it regresses after menopause. Hormones with antiestrogenic activity also suppress endometriosis and are used therapeutically. Retrograde Menstruation backward movement of endometrial cells through the fallopian tubes out into the abdomen Lymphatic or Vascular spread Immunological factor - The peritoneal fluid in endometriosis shows the presence of macrophages and natural killer (NK) cells. Impaired T cell and NK cell activity and altered immunology. Risk factors include: Age 30-40 Family History One or more relatives (The mother, aunt, sister) had endometriosis Early menarche Short menstrual cycles (< 27 days) Heavy bleeding during menses Delayed childbearing Infertility Defects in the uterus or fallopian tubes C. Epidemiology a. Incidence and Prevalence Endometriosis is estimated to affect over one million women (estimates range from 3% to 18% of women) in the United States. Between 20% to 50% of women being treated for infertility have endometriosis Up to 80% of women with chronic pelvic pain may be affected. Endometriosis is rare in postmenopausal women. b. Age
[DISORDERS OF THE REPRODUCTIVE SYSTEM] October 5, 2013
Most cases of endometriosis are diagnosed in women aged around 25 to 35 years c. Race Endometriosis is more commonly found in white women as compared with African American and Asian women Studies further suggest that endometriosis is most common in taller, thin women with a low body mass index (BMI) D. Symptoms The primary symptom of endometriosis is pelvic pain. Painful periods (dysmenorrhea). Pelvic pain and cramping may begin before and extend several days into your period and may include lower back and abdominal pain. Pain with intercourse (dyspareunia). Pain during or after sex is common with endometriosis. Pain with bowel movements or urination. Most likely to experience these symptoms during your period. Excessive bleeding. May experience occasional heavy periods (menorrhagia) or bleeding between periods (menometrorrhagia). Infertility. Endometriosis is first diagnosed in some women who are seeking treatment for infertility. Other symptoms. You may also experience fatigue, diarrhea, constipation, bloating or nausea, especially during menstrual periods. The severity of the pain isn't necessarily a reliable indicator of the extent of the condition. Some women with mild endometriosis have extensive pain, while others with advanced endometriosis may have little pain or even no pain at all. Based on the history and presenting signs and symptoms Tests to check for physical clues of endometriosis include: Pelvic exam. During a pelvic exam, your doctor manually feels (palpates) areas in your pelvis for abnormalities, such as cysts on your reproductive organs or scars behind your uterus. Often it's not possible to feel small areas of endometriosis, unless they've caused a cyst to form. Ultrasound. This test uses high-frequency sound waves to create images of the inside of your body. To capture the images, a device called a transducer is either pressed against your abdominal skin or inserted into your vagina (transvaginal ultrasound). Both types of ultrasound may be done to get the best view of your reproductive organs. Ultrasound imaging won't definitively tell your doctor
E. Diagnosis
[DISORDERS OF THE REPRODUCTIVE SYSTEM] October 5, 2013
whether you have endometriosis, but it can identify cysts associated with endometriosis (endometriomas). Laparoscopy. Laparoscopy is the most common and the golden standard surgical procedure for the diagnosis of endometriosis. Medical management is usually tried first. But to be certain you have endometriosis, your doctor may refer you to a surgeon to look inside your abdomen for signs of endometriosis using a surgical procedure called laparoscopy. While you're under general anesthesia, your surgeon makes a tiny incision near your navel and inserts a slender viewing instrument (laparoscope), looking for endometrial tissue outside the uterus. He or she may take samples of tissue (biopsy). Laparoscopy can provide information about the location, extent and size of the endometrial implants to help determine the best treatment options. F. Treatment PHARMACOLOGIC MANAGEMENT: Nonsteroidal anti-inflammatory drugs or NSAIDs (such as ibuprofen or naproxen sodium) are commonly prescribed to help relieve pelvic pain and menstrual cramping. If they work to control pain, no other procedures or medical treatments are needed. If they do not relieve the pain, additional evaluation and treatment generally occur. Gonadotropin-releasing hormone analogs (GnRH analogs) Gonadotropin-releasing hormone analogs (GnRH analogs) have been effectively used to relieve pain and reduce the size of endometriosis implants. These drugs suppress estrogen production by the ovaries by inhibiting the secretion of regulatory hormones from the pituitary gland. As a result, menstrual periods stop, mimicking menopause. Nasal and injection forms of GnRH agonists are available. Oral contraceptive pills - Oral contraceptive pills (estrogen and progesterone in combination) are also sometimes used to treat endometriosis. The most common combination used is in the form of the oral contraceptive pill (OCP). Continuous use in this manner will free a woman of having any menstrual periods at all. Occasionally, weight gain, breast tenderness, nausea, and irregular bleeding are mild side effects. Oral contraceptive pills are usually well-tolerated in women with endometriosis. Progestins - Progestins [for example, medroxyprogesterone acetate (Provera, Cycrin, Amen), norethindrone acetate, norgestrel acetate (Ovrette)] are more potent than birth control pills and are recommended for women who do not obtain pain relief from or cannot take a birth control pill.
[DISORDERS OF THE REPRODUCTIVE SYSTEM] October 5, 2013
Side effects are more common and include: breast tenderness, bloating, weight gain, irregular uterine bleeding, and depression. Since the absence of menstruation (amenorrhea) induced by high doses of progestins can last many months after cessation of therapy, these drugs are not recommended for women planning pregnancy.
Danazol (Danocrine) Danazol (Danocrine) is a synthetic drug that creates a high androgen (male type hormone) and low estrogen hormonal environment by interfering with ovulation and ovarian production of estrogen. Eighty percent of women who take this drug will have pain relief and shrinkage of endometriosis implants, but up to 75% of women develop side effects from the drug. Side effects can include: weight gain, edema, decreased breast size, acne, oily skin, hirsutism (male pattern hair growth), deepening of the voice, headache, hot flashes, changes in libido, and mood changes. All of these changes are reversible, except for voice changes; but the return to normal may take many months. Danazol should not be taken by women with certain types of liver, kidney, and heart conditions. Aromatase inhibitors A newer approach to the treatment of endometriosis has involved the administration of drugs known as aromatase inhibitors (for example,anastrozole [Arimidex] and letrozole [Femara]). These drugs act by interrupting local estrogen formation within the endometriosis implants themselves. They also inhibit estrogen production in the ovary, brain, and other sources, such as adipose tissue. Research is still ongoing to characterize the effectiveness of aromatase inhibitors in the management of endometriosis. Aromatase inhibitors cause significant bone loss with prolonged use
[DISORDERS OF THE REPRODUCTIVE SYSTEM] October 5, 2013
and cannot be used alone without other medications such as GnRH agonists or combination of oral contraceptives in premenopausal women because they stimulate development of multiple follicles at ovulation. G. Surgical Management Surgery. Surgery is usually the best choice for women with severe endometriosis many growths, a great deal of pain, or fertility problems. There are both minor and more complex surgeries that can help. The doctor might suggest one of the following:
Laparoscopy can be used to diagnose and treat endometriosis. During this surgery, doctors remove growths and scar tissue or burn them away. The goal is to treat the endometriosis without harming the healthy tissue around it. Women recover from laparoscopy much faster than from major abdominal surgery. Laparotomy or major abdominal surgery that involves a much larger cut in the abdomen than with laparoscopy. This allows the doctor to reach and remove growths of endometriosis in the pelvis or abdomen. Hysterectomy is a surgery in which the doctor removes the uterus. Removing the ovaries as well can help ensure that endometriosis will not return. This is done when the endometriosis has severely damaged these organs. A woman cannot get pregnant after this surgery, so it should only be considered as a last resort.
[DISORDERS OF THE REPRODUCTIVE SYSTEM] October 5, 2013
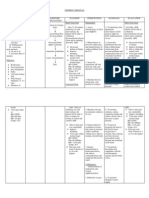
PATHOPHYSIOLOGY OF ENDOMETRIOSIS
RISK FACTORS: Family History One or more relatives (The mother, aunt, sister) had endometriosis Early menarche Short menstrual cycles (< 27 days) Heavy bleeding during menses Delayed childbearing Infertility Defects in the uterus or fallopian tubes
ETIOLOGY: UNKNOWN THEORIES:
Hormonal influence Retrograde Menstruation Lymphatic or Vascular spread Immunological factor
MENSTRUAL CYCLE: ESTROGEN LEVEL HORMONAL INFLUENCE
Thickening of the endometrial lining in preparation for the fertilization of egg
If the egg is not fertilized, it disintegrates causing the hormones to drop
Levels of Estrogen and Progesterone
Shedding of endometrial lining in the form of menstrual blood
Regurgitation from the fallopian tubes
RETROGRADE MENSTRUATION
[DISORDERS OF THE REPRODUCTIVE SYSTEM] October 5, 2013
Vascular
/ dissemination of
the endometrial tissue Endometrial cells deposited outside the uterus implant on structures within the cavity
LYMPHATIC OR VASCULAR SPREAD
Endometrium build up
Continuously responds to menstrual cycle stimulation More cells attach to pelvic structures
BLEEDING
INFLAMMATION
SCARRING
Infertility
ADHESION PHARMACOLOGIC MNGT: Nonsteroidal antiinflammatory drugs or NSAIDs Gonadotropin-releasing hormone analogs (GnRH analogs) Danazol (Danocrine) Aromatase inhibitors S/SX: Dysmenorrhea Chronic pelvic pain Dyspareunia Dysuria
PAIN
You might also like
- Clinical Instructor Cover LetterDocument1 pageClinical Instructor Cover Letterbanyenye25No ratings yet
- Pathophysiology of Congestive Heart Failure: Cardiovascular SystemDocument3 pagesPathophysiology of Congestive Heart Failure: Cardiovascular Systembanyenye25No ratings yet
- Virginia Henderson TheoryDocument6 pagesVirginia Henderson Theorybanyenye25No ratings yet
- Patho MIDocument2 pagesPatho MIbanyenye25100% (2)
- Com Epi PaperDocument25 pagesCom Epi Paperbanyenye25No ratings yet
- Acute Bronchitis PathoDocument3 pagesAcute Bronchitis Pathobanyenye25No ratings yet
- Patho MIDocument2 pagesPatho MIbanyenye25100% (2)
- Nursing Interventions CHFDocument3 pagesNursing Interventions CHFbanyenye25100% (1)
- Laboratory Assessment CHFDocument3 pagesLaboratory Assessment CHFbanyenye25No ratings yet
- Electro Cardiograph yDocument14 pagesElectro Cardiograph ybanyenye25No ratings yet
- NCP BurnDocument9 pagesNCP Burnbanyenye2533% (3)
- A G E - PathoDocument1 pageA G E - Pathoranee dianeNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation SubjectiveDocument6 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjectivebanyenye25No ratings yet
- Principles of BioethicsDocument5 pagesPrinciples of Bioethicsbanyenye25No ratings yet
- Philippines Population Pyramid For 2010Document4 pagesPhilippines Population Pyramid For 2010banyenye25No ratings yet
- NCPDocument4 pagesNCPbanyenye25No ratings yet
- Nursing Care for Fracture PatientDocument2 pagesNursing Care for Fracture Patientbanyenye25No ratings yet
- Philippine healthcare laws overviewDocument5 pagesPhilippine healthcare laws overviewbanyenye25100% (2)
- NURSING CARE PLAN For Myocardial InfarctionDocument13 pagesNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- NCP Risk For InfectionDocument3 pagesNCP Risk For Infectionbanyenye25No ratings yet
- Pa Tho PhysiologyDocument2 pagesPa Tho Physiologybanyenye25No ratings yet
- NCP Risk For InfectionDocument3 pagesNCP Risk For Infectionbanyenye25No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Managing Twin Pregnancy Risks and ComplicationsDocument66 pagesManaging Twin Pregnancy Risks and ComplicationsEkta Rajput100% (1)
- Sop Eclampsia KNH 2009Document11 pagesSop Eclampsia KNH 2009adammzjinNo ratings yet
- 28 April - 1 MEI 2021: Enhancing Patient's Experience in Urogynecology ServicesDocument10 pages28 April - 1 MEI 2021: Enhancing Patient's Experience in Urogynecology ServicesUNS KAMERA BELAKANGNo ratings yet
- Female and Male Reproductive SystemsDocument5 pagesFemale and Male Reproductive SystemsPol HuelarNo ratings yet
- Abortion: PathophysiologyDocument3 pagesAbortion: PathophysiologyEdmund Lominoque LamelaNo ratings yet
- MCNDocument13 pagesMCNJoseph Wilson MacasaNo ratings yet
- Cryopreservation and Ivf: What Can Be Stored?Document2 pagesCryopreservation and Ivf: What Can Be Stored?Deepanshu ShakargayeNo ratings yet
- C. Anovulation: C. Dysfunctional Uterine BleedingDocument18 pagesC. Anovulation: C. Dysfunctional Uterine BleedingJan Mikhail Frasco100% (1)
- Efektifitas Pemberian Wedang Jahe terhadap Frekuensi Mual dan Muntah pada Ibu Hamil Trimester IDocument11 pagesEfektifitas Pemberian Wedang Jahe terhadap Frekuensi Mual dan Muntah pada Ibu Hamil Trimester IrohyatiNo ratings yet
- Ojsadmin, 993Document6 pagesOjsadmin, 993pondyNo ratings yet
- Obstetrics Case History by S.P.kamthankarDocument7 pagesObstetrics Case History by S.P.kamthankarMd Ali0% (1)
- Dr. Kee OngDocument2 pagesDr. Kee OngDr. Kee OngNo ratings yet
- Postpartum Haemorrhage Causes and ManagementDocument51 pagesPostpartum Haemorrhage Causes and ManagementBasudev chNo ratings yet
- Genital Tract InjuriesDocument16 pagesGenital Tract InjuriesNadiya Rashid100% (4)
- How To Diagnose PROM & PPROM - Cahara AdhiDocument20 pagesHow To Diagnose PROM & PPROM - Cahara AdhiAmarendra Wardhana100% (1)
- How to Perform a Monthly Breast Self-ExamDocument4 pagesHow to Perform a Monthly Breast Self-ExamPriyanka SheoranNo ratings yet
- Fetal Growth DisorderDocument100 pagesFetal Growth Disorderwidia iryuzzaNo ratings yet
- Eming Report Precipitous LaborDocument11 pagesEming Report Precipitous LaborJudeLaxNo ratings yet
- ADH Risk Factor & ScreeningDocument6 pagesADH Risk Factor & ScreeningpgalamilloNo ratings yet
- Continuing Professional Development Questions and Answer For FSRH Guideline Progestogen-Only Pill (March 2015, Amended April 2019)Document2 pagesContinuing Professional Development Questions and Answer For FSRH Guideline Progestogen-Only Pill (March 2015, Amended April 2019)Sarumathy AshokNo ratings yet
- CERVICAL DILATORSDocument5 pagesCERVICAL DILATORSTomy SaputraNo ratings yet
- ST. Mary Maternity HospitalDocument8 pagesST. Mary Maternity HospitalgajendraNo ratings yet
- PROM Management and OutcomesDocument6 pagesPROM Management and OutcomesRayhan AlatasNo ratings yet
- EINC Protocol Skills for Newborn CareDocument3 pagesEINC Protocol Skills for Newborn CareAngelika Padawan100% (1)
- Nurse 320 Hawaiian PaperDocument6 pagesNurse 320 Hawaiian Paperapi-302588274No ratings yet
- Speech of Queen About ContraceptiveDocument3 pagesSpeech of Queen About ContraceptiveNimrad LavapiezNo ratings yet
- Inserto Inmunoqimicas Bio RadDocument2 pagesInserto Inmunoqimicas Bio RadorthincoatzaNo ratings yet
- Printable - Thesis On Bishop ScoreDocument103 pagesPrintable - Thesis On Bishop Scoreanuaurv100% (3)
- Everything You Need to Know About Oral Contraceptive PillsDocument3 pagesEverything You Need to Know About Oral Contraceptive PillsbebytycoNo ratings yet