Professional Documents
Culture Documents
Hiperbaric Oxygen Therapy in The Management of Chronic Nonhealing Ulcer
Uploaded by
Juan Jose LeonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hiperbaric Oxygen Therapy in The Management of Chronic Nonhealing Ulcer
Uploaded by
Juan Jose LeonCopyright:
Available Formats
70 Journal of Anaesthesiology Clinical Pharmacology | January-March 2012 | Vol 28 | Issue 1
Original Article
Evaluation of the efficacy of hyperbaric oxygen therapy in the
management of chronic nonhealing ulcer and role of periwound
transcutaneous oximetry as a predictor of wound healing
response: A randomized prospective controlled trial
Sarbjot Kaur, Mridula Pawar, Neerja Banerjee, Rakesh Garg
Department of Anaesthesiology and Intensive Care, Postgraduate Institute of Medical Education and Research and Dr. Ram Manohar Lohia
Hospital, New Delhi, India
Background: Hyperbaric oxygen therapy (HBOT) is a treatment option for chronic nonhealing wounds. Transcutaneous
oximetry (TCOM) is used for wound assessment. We undertook a randomized prospective controlled trial to evaluate the role
of HBOT in healing of chronic nonhealing wounds and to determine whether TCOM predicts healing.
Materials and Methods: This study was conducted in 30 consenting patients with nonhealing ulcer. The patients were
randomized into group HT (receiving HBOT in addition to conventional treatment) and group CT (receiving only conventional
treatment). Duration of treatment in both the groups was 30 days. Wound ulcer was analyzed based on size of the wound,
exudates, presence of granulation tissue, and wound tissue scoring. Tissue oxygenation (TcPO
2
) was measured on 0, 10
th
, 20
th
,
and 30
th
day.
Results: There was 59% reduction in wound area in group HT and 26% increase in wound area in group CT. Ten patients
in group HT showed improvement in wound score as compared to five patients in group CT. Complete healing was seen in
three patients in group HT as compared to none in group CT. Surgical debridement was required in 6 patients in group HT and
10 patients in group CT. One patient in group HT required amputation as compared to five patients in group CT. A positive
correlation was found between TcPO
2
value and various markers of wound healing.
Conclusion: HBOT has a definitive adjunctive role in the management of chronic nonhealing ulcers. It decreases the amputation
rate and improves patient outcome. Periwound TcPO
2
may be used as a predictor of response to HBOT and has a positive
correlation with wound healing.
Key words: Hyperbaric oxygen therapy, nonhealing wounds, transcutaneous oximetry
Abstract
Address for correspondence: Dr. Rakesh Garg,
Department of Anaesthesiology and Intensive Care, Postgraduate
Institute of Medical Education and Research and Dr Ram Manohar
Lohia Hospital, New Delhi, India.
E-mail: drrgarg@hotmail.com
Access this article online
Quick Response Code:
Website:
www.joacp.org
DOI:
10.4103/0970-9185.92444
Introduction
Chronic nonhealing wound are common and have a high
impact on the well-being of those affected.
[1]
They are often
associated with diabetes mellitus, arterial, and venous disease.
Increased oxygen demand, requiring sufficient supply of blood,
is there during ulcer healing.
[2]
Hyperbaric oxygen therapy
(HBOT) is a systemic treatment option, wherein a patient
breathes pure oxygen at greater than one atmospheric pressure
for a specified period of time. Therapeutic effects of HBOT
are due to an increase in dissolved oxygen in plasma and tissue
oxygen delivery. At 2.5 absolute atmosphere (ATA), partial
pressure of oxygen (PaO
2
) increases from 760 mmHg at room
air to 1900 mmHg, on breathing in 100% oxygen, and the
plasma content of oxygen increases from 0.3 to 5.62 volume-
percent. HBOT promotes healing in chronic nonhealing
wounds by means of its antiedema effect, augmenting
neovascularization, stimulating fibroblast proliferation and
differentiation, increasing collagen formation and cross linking,
and stimulating leukocyte microbial killing.
[2-4]
Although
HBOT has gained popularity as an adjunctive treatment for
[Downloadedfreefromhttp://www.joacp.orgonSaturday,May18,2013,IP:187.214.28.78]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Kaur, et al.: HBOT and TcPO
2
for nonhealing ulcer
Journal of Anaesthesiology Clinical Pharmacology | January-March 2012 | Vol 28 | Issue 1 71
problem wounds, there are only few randomized controlled
studies that support its efficacy.
Transcutaneous oximetry (TCOM) is a simple, reliable
noninvasive technique for the objective assessment of wound
perfusion and oxygenation.
[5]
Its definitive role in predicting
the wound healing has not yet been proven. We undertook
a randomized controlled trial to evaluate the role of HBOT
in healing of chronic nonhealing wounds and to determine
whether TCOM predicts healing.
Materials and Methods
This prospective randomized controlled study was
conducted after the approval of the institutional research
and ethical committee. Patients referred from surgical
specialties to the hyperbaric oxygen unit of the Department
of Anaesthesiology, with the complaint of chronic nonhealing
ulcer, were included in the study. Patients in the age group
of 1865 years of either sex with a nonhealing ulcer, despite
conventional therapy of more than 4 weeks duration, were
included in the study. Patients who were not willing for
HBOT, those with active upper respiratory tract infection,
with any active lung pathology or pregnancy were excluded
from the study. Written informed consent was obtained
from all the patients.
Investigations including complete hemogram, random blood
sugar, electrocardiogram, and X-ray chest were reviewed.
Duration of wound, associated medical illness including
history of smoking, diabetes mellitus (DM), hypertension
(HTN), and the type of treatment received and advised were
recorded. Ear, nose, throat examination was performed by
an Otorhinolaryngologist to rule out upper respiratory tract
infection and inflammation of tympanic membrane. Local
examination of the wound was done and the size (length and
width), number, site, color of the surrounding skin, type of
wound, discharge, vascular insufficiency, or associated varicose
vein were recorded. Doppler examination was performed to
confirm vascular insufficiency.
Thirty consenting patients were randomized by computer-
generated random numbers into two groups. Group HT
patients received HBOT in addition to conventional treatment,
while Group CT patients received only conventional treatment.
Duration of treatment in both the groups was 30 days. All
the patients received conventional therapy for the management
of wounds, i.e., wound debridement, treating infection, daily
dressing, etc., which was managed by the referring surgeon.
In group HT patients, HBOT was administered at 2.5ATA
in a monoplace chamber [Bara-Med monoplace hyperbaric
chamber, Biomedical systems, Environmental Tectonics
Corporation, Southampton, PA, USA) for 90 min, 6 days a
week. A total of 30 sessions were administered to each patient
along with conventional treatment.
Wound ulcer was analyzed on 0, 10th, 20th, and 30th day
and assessment of healing in both the groups was performed
on the basis of size of the wound [area of wound (sq cm) was
obtained by product of the greatest length (cm) and greatest
width (cm)], exudates (an estimate of ulcer was assessed on
the presence or absence of exudates), presence of granulation
tissue and wound tissue scoring [the wound (ulcer) bed was
scored on a score of 04] [Table 1].
TCM 400/TINA using Miniature Clark electrode (Tina
TCM 400 Transcutaneous pO
2
monitoring system,
Radiometer Copenhagen, Bronshoj, Denmark) was utilized
for measuring tissue oxygenation (TcPO
2
) in all the patients of
both groups. Measurements were recorded on noninflammed
skin 1 cm proximal to the upper margin of ulcer. TcPO
2
values
were recorded on 0, 10th, 20th, and 30th day. TcPO2 was
measured by an electrochemical transducer, which was fixed
to the skin with the help of an adhesive ring and contact
liquid supplied by the manufacturer. The measuring site was
cleaned carefully by a disinfectant (chlorhexidine-spirit). The
skin oxygen partial pressure was determined by measuring
the oxygen reduction current by means of a measuring cell.
To increase the permeability of the skin to oxygen molecules
at the measuring site, the transducer is heated to 44C. The
calibration period was on an average 10 min, and the TcPO
2
signal was continuously recorded.
Patients requiring surgical debridement/amputation were
noted. Any side effects related to HBOT were also noted.
Statistical analysis
The primary outcome variable was the wound size. Sample
size of 30 patients was based on the predicted difference
of 25% in the wound area in the two groups of treatment
modality. Data were analyzed using SPSS Version 15.0. For
quantitative variables, student t- test for independent samples
was applied to test the difference amongst the averages of
the quantitative data of the two groups. Paired t-test was
applied to compare the difference between the means. For
qualitative data, the chi square test, Fischer exact test, and
Wilcoxon signed rank test were applied to test the difference
amongst the two groups. Kendalls tau b test was applied
for correlating periwound TcPO
2
with various parameters
of wound healing. Nonparametric Mann Whitney U test
was applied for comparing duration of wound as it had non
Gaussian distribution.
[Downloadedfreefromhttp://www.joacp.orgonSaturday,May18,2013,IP:187.214.28.78]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Kaur, et al.: HBOT and TcPO
2
for nonhealing ulcer
72 Journal of Anaesthesiology Clinical Pharmacology | January-March 2012 | Vol 28 | Issue 1
Results
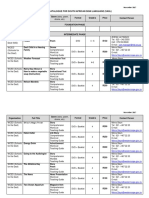
Forty-six patients were recruited for the study but only 30
patients fulfilled the study criteria and were randomized in the
two groups (Figure 1 consort chart). All patients completed
the study period and no patient was excluded from the study
analysis. The demographic profile was comparable in the two
groups [Table 1]. Both the groups were comparable in terms
of comorbid conditions [Table 2]. Of the comorbidities, three
patients had both DM and HTN and another three patients
had DM, HTN, and were smokers. Common sites of wound
were mid-foot (8 patients), leg (7 patients), fore-foot (6
patients), great toe (5 patients), other toes (1 patient), and
other sites (3 patients).
There was 59% reduction in wound area (median baseline
area of 24 cm
2
decreased to 6 cm
2
at 30 day of therapy,
P = 0.012) in group HT and 26% increase in wound
area (median baseline area of 16 cm
2
increased to 20 cm
2
at 30 day of therapy, P = 0.221) in group CT. This
difference in the two groups was statistically highly significant
(P = 0.001). Exudate resolved in 11 patients in group
HT as compared to 3 patients in group CT (P = 0.001).
There was significant improvement in exudates in group HT
(P = 0.006) as compared to group CT (P = 0.250) from
baseline exudates in the respective group. Granulation tissue
appeared in 12 out of 15 patients in group HT as compared
to 6 out of 15 patients in group CT (P = 0.02).
A significant improvement in wound score was observed
in group HT as compared to group CT after 20 days of
treatment [Table 3]. Significant improvement in wound
score was observed after every 10 sittings of HBOT in
Group HT [Table 4]. After 30 days of treatment in both
the groups, 10 patients out of 15 in group HT (P = 0.006)
showed improvement in wound score (decrease in tissue
grade) as compared to 5 out of 15 patients in group CT
(P = 0.52). Complete healing was seen in 3 out of 15 patients
in group HT as compared to none in group CT after 30 days
(P = 0.07). Surgical debridement was required in 6 out of 15
patients in group HT and 10 out of 15 patients in group CT
(P = 0.14). One patient in group HT required amputation
as compared to 5 patients in group CT (P = 0.06).
Table 4: Comparison of wound tissue score from baseline at different time intervals of therapy
Improvement in wound
score (n)
No change in wound
score (n)
Deterioration in wound
score (n)
P value
Group HT (n = 15)
After 10 days 9 6 0 0.005
After 20 days 10 5 0 0.004
After 30 days 10 4 1 0.006
Group CT (n = 15)
After 10 days 3 12 0 0.08
After 20 days 5 9 1 0.31
After 30 days 5 8 2 0.52
Table 1: The wound (ulcer) bed scoring
Score Tissue type in the
wound (ulcer) bed
Description
4 Necrotic tissue (eschar) Black, brown or tan tissue that
adheres firmly to the wound
bed or ulcer edges and may be
either firmer or softer than the
surrounding skin.
3 Slough Yellow or white tissue that adheres
to the ulcer bed in strings or thick
clumps or is mucinous.
2 Granulation tissue Pink or beefy red tissue with a
shiny, moist, granular appearance.
1 Epithelial tissue For superficial ulcer, new pink or
shiny tissue skin that grows in from
the edges or islands on the ulcer
surface.
0 Closed/resurfaced The wound is completely covered
with epithelium (new skin).
Table 2: Patient characteristics
Parameters Group HT
(n = 15)
Group CT
(n = 15)
P value
Age (years) 46.9 11.8* 47.4 12.5* 0.91
Sex (M/F) 12/03 13/02 0.78
Comorbidities
Diabetes mellitus 5 5 1
Hypertension 6 6 1
Varicose vein 2 2 1
Vascular insufficiency 2 2 1
Smoking 7 6 0.71
Wound duration (months),
median (range)
2 (160) 2.5 (136) 0.6
*Values are expressed as mean + standard deviation
Table 3: Assessment of wound tissue score
Tissue grading
(Grade 0: 1: 2: 3: 4)
Group HT
(n = 15)
Group CT
(n = 15)
P value
Baseline 0:0:5:7:3 0:1:1:9:4 0.25
On 10
th
day 0:3:8:3:1 0:1:3:8:3 0.08
On 20
th
day 0:7:5:2:1 0:0:5:6:4 0.01
On 30
th
day 2:6:4:1:2 0:0:6:3:6 0.02
[Downloadedfreefromhttp://www.joacp.orgonSaturday,May18,2013,IP:187.214.28.78]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Kaur, et al.: HBOT and TcPO
2
for nonhealing ulcer
Journal of Anaesthesiology Clinical Pharmacology | January-March 2012 | Vol 28 | Issue 1 73
After 30 days, periwound TcPO
2
(at room air) improved
by 11.8 mmHg in group HT (P = 0.01) and decreased
by 5.7 mmHg from baseline value in group CT (P = 0.2)
[Table 5]. On monitoring periwound TcPO
2
at regular
intervals in both the groups, an increasing trend in TcPO
2
values were observed in group HT (P = 0.09 at 10 days,
0.008 at 20 days, and 0.012 at 30 days as compared to
baseline), while a falling trend was observed in group CT
(P = 0.68 at 10 days, 0.49 at 20 days, and 0.22 at 30 days
as compared to baseline).
A positive correlation was found between TcPO
2
value and various markers of wound healing, such as
decrease in area of the wound, decrease in exudate
amount, and improvement in wound score [Table 6]. A
negative correlation was found between TcPO
2
value and
amputation rate. Periwound TcPO
2
values were monitored
at regular intervals in both the groups and a positive
correlation was found between TcPO
2
values and various
markers of wound healing, such as decrease in area of
the wound (P = 0.004), decrease in exudate amount
(P = 0.001), and improvement in wound score
(P = 0.01). A negative correlation of 0.53 was found
between TcPO
2
values and amputation rate (P = 0.004).
Higher the periwound TcPO
2
levels, lesser is the amputation
rate (P 0.05). Higher the periwound TcPO
2
levels more
are the chances of wound healing. Individually, correlations
were significant in group HT and not in group CT.
Common adverse effects seen with HBOT were pressure
related ear discomfort/pain (3 patients), claustrophobia (2
patients), headache (1 patient), and tinnitus (1 patient).
Discussion
We found that HBOT helps in nonhealing ulcer by decreasing
exudate and promoting granulation tissue. The wound size
decreases and wound tissue type is improves. A positive
correlation was found between TcPO
2
values and various
markers of wound healing, such as decrease in area of the
wound, decrease in exudate amount, and improvement in
wound score. A negative correlation was found between
TcPO
2
values and amputation rate.
Our results are in agreement with other studies showing
positive effects of adjunctive HBOT on chronic non healing
ulcer. Oriani et al., Zamboni et al., Faglia et al., Baroni et al.,
and Kalani et al. reported better healing and lower amputation
rate after HBOT as compared to conventional therapy in
patients with nonhealing ulcer.
[6-11]
Measurement of TcPO2 during inhalation of pure oxygen
or HBO exposure has been used to select patients for
HBOT
[10]
and values under 40 mmHg were associated with
poor ulcer healing in diabetic patients.
[12]
Diabetic patients
with local hypoxic foot ulcer (TcPO2 < 40 mmHg) benefit
from HBOT when TcPO2 value increases to >100 mmHg
and/or at least three times basal value during inhalation
of pure oxygen.
[10]
TcPO
2
measured in chamber under
hyperbaric conditions provides the best single discriminator
between success and failure of HBOT, using a cut-off
score of 200 mmHg.
[13]
These data supported the use of
in-chamber TcPO
2
as a screening tool.
[14]
HBOT may be
added to conventional treatment of diabetic foot ulcers if
periwound TcPO
2
in 2.5 ATA HBO is over 200 mmHg.
[14]
In our study, periwound TcPO
2
levels at room air were also
monitored in both the groups in order to assess the role of
TcPO
2
in predicting wound healing. Periwound TcPO
2
Table 5: Periwound TcPO
2
values
Group HT
(n = 15)
Group CT
(n = 15)
P value
Baseline 22.5 13.4 27.1 15.9 0.407
Day 10 28.1 17.2 25.9 10 0.663
Day 20 33.3 18.5 24.7 9.9 0.122
Day 30 34.3 14.8 21.4 9.5 0.008
Table 6: Correlation of periwound TcPO
2
and various parameters of wound healing
Group Improvement in
TcPO
2
Improvement in
tissue grading
(decrease in wound
score)
Improvement in
exudates (decrease in
exudates)
Change in wound
size (decrease in
wound area)
Amputation rate
Total (n = 30) Correlation 0.473* 0.675** 0.535** -0.535**
Coefficient significance
(2-tailed)
0.011 0.001 0.004 0.004
Group HT (n = 15) Correlation 0.612* 0.739** 0.784** -0.535*
Coefficient significance
(2-tailed)
0.022 0.006 0.003 0.046
Group CT (n = 15) Correlation 0.213 0.294 -0.237 -0.426
Coefficient significance
(2-tailed)
0.425 0.271 0.376 0.111
*Correlation is significant at the 0.05 level (2-tailed)., **Correlation is significant at the 0.01 level (2-tailed)
[Downloadedfreefromhttp://www.joacp.orgonSaturday,May18,2013,IP:187.214.28.78]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Kaur, et al.: HBOT and TcPO
2
for nonhealing ulcer
74 Journal of Anaesthesiology Clinical Pharmacology | January-March 2012 | Vol 28 | Issue 1
levels were also measured inside the chamber in group HT
and the highest reading inside the chamber was recorded.
Wyss et al. measured TcPO
2
in patients with wounds and
found an increasing probability of failure with decreasing
TcPO
2
.
[15]
We also found a positive correlation between
TcPO
2
values and various markers of wound healing, while
a negative correlation of 0.53 was found between TcPO
2
values and amputation rate. Initial (room air) TCOM
values do not predict outcome however patients who go on
to heal have a higher TCOM value after breathing 100%
oxygen than those who do not heal.
[16]
Better results can be
obtained by combining information about sea-level air and
in-chamber oxygen measurement.
[13]
A sea-level air TcPO
2
<15 mmHg combined with an in-chamber TcPO
2
< 400
mmHg predicts failure of HBOT. Only one patient in
our study had in-chamber TcPO
2
< 400mmHg and this
patient (from group HT) had vascular insufficiency. He did
not respond to treatment and had to undergo amputation.
Statistical significance of this could not be calculated, and
therefore, we cannot comment upon the in-chamber TcPO
2
values as a predictor of response.
10 out of 15 patients in group HT showed signs of healing
compared to 5 out of 15 patients in group CT which
corroborates with the findings of the study by Kalani et al.
[10]
Complications reported in patients treated with HBOT
include ear pain (17%) and generalized seizures (0.5%).
[17]
In our study, the most common adverse effect with HBOT
was pressure related ear discomfort/pain (20%), followed by
claustrophobia (13%). No cases of seizure or pneumothorax
were observed in our study.
The limitations of our study were that long-term impact of
HBOT on wound healing was not studied beyond 30 days
and that we included patients having ulcers due to different
causes. However, the two groups were comparable.
We conclude that HBOT has a definitive adjunctive role in
the management of chronic nonhealing ulcers. Problem wounds
require multidisciplinary, aggressive, and a combined approach
including administration of HBOT. Administration of HBOT
along with conventional treatment decreases the amputation
rate and improves patient outcome. Periwound TcPO
2
values
may be used as a predictor of response to HBOT and have a
positive correlation with respect to wound healing. No serious
adverse effects have been observed with HBOT.
Figure 1: Consort chart
Assessed for eli gibility (n=46)
Excluded (n=16)
Not meeting inclusion criteri a (n=15)
Declined to participate (n= 1)
Other reasons (n=0)
Analysed (n=15)
Excluded from analysis (gi ve reasons) (n=0)
Lost to follow-up (gi ve reasons) (n=0)
Discontinued intervention (gi ve reasons) (n=0)
Allocated to intervention (n=15)
Recei ved allocated intervention (n=15)
Did not recei ve all ocated i ntervention (gi ve
reasons) (n=0)
Lost to follow-up (gi ve reasons) (n=0)
Discontinued intervention (gi ve reasons) (n=0)
Allocated to intervention (n=15)
Recei ved allocated intervention (n=15)
Did not recei ve all ocated i ntervention (gi ve
reasons) (n=0)
Analysed (n=15)
Excluded from analysis (gi ve reasons) (n=0)
Allocation
Analysis
Follow-Up
Randomized (n=30)
Enrollment
[Downloadedfreefromhttp://www.joacp.orgonSaturday,May18,2013,IP:187.214.28.78]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Kaur, et al.: HBOT and TcPO
2
for nonhealing ulcer
Journal of Anaesthesiology Clinical Pharmacology | January-March 2012 | Vol 28 | Issue 1 75
References
1. Lipsky BA, Berendt AR. Hyperbaric oxygen therapy for diabetic foot
wounds. Has hope hurdled hype? Diabetes Care 2010;33:1143-5.
2. Gill AL, Bell CA. Hyperbaric oxygen: Its uses, mechanisms of action
and outcomes. QJ Med 2004;97:385-95.
3. Niinikoski J. Hyperbaric oxygen therapy of diabetic foot ulcers,
transcutaneous oximetry in clinical decision making. Wound Rep
Reg 2003;11:458-61.
4. Eskes AM, Ubbink DT, Lubbers MJ, Lucas C, Vermeulen H.
Hyperbaric oxygen therapy: Solution for difficult to heal acute
wounds: Systemic review. World J Surg 2011;35:535-42.
5. Niinikoski J. Clinical hyperbaric oxygen therapy, wound perfusion,
and transcutaneous oximetry. World J Surg 2004;28:307-11.
6. Oriani G, Meazza D, Favales F, Pizzi GL, Aldeghi A, Faglia
E. Hyperbaric oxygen in diabetic gangrene. J Hyperb Med
1990;5:171-5.
7. Zamboni WA, Wong HP, Stephenson LL, Pfeifer MA. Evaluation
of hyperbaric oxygen for diabetic wounds: A prospective study. J
Hyperb Med 1997;24:175-9.
8. Faglia E, Favales F, Aldeghi A, Calia P, Quarantiello A, Oriani G,
et al. Adjunctive systemic hyperbaric oxygen therapy in treatment
of severe prevalently ischemic diabetic foot ulcer. Diabetic Care
1996;19:1338-43.
9. Baroni G, Porro T, Faglia E, Pizzi G, Mastropasqua A, Oriani G,
et al. Hyperbaric oxygen in diabetic gangrene treatment. Diabetes
Care 1987;10:81-6.
10. Kalani M, Jorrneskog G, Nazanin N, Lind F, Brismar K. Hyperbaric
oxygen (HBO) therapy in the treatment of diabetic foot ulcers.
Long term follow-up. J Diabetes Compl 2002;16:153-8.
11. Goldman RJ. Hyperbaric oxygen therapy for wound healing and
limb salvage: A systemic review. PM R 2009;1:471-89.
12. Quigley FG, Faris IB. Transcutaneous oxygen tension measurements
in the assessment of limb ischemia. Clin Physiol 1991;11:315-20.
13. Fife CE, Buyukcakir C, Otto GH, Sheffield PJ, Warriner RA, Love
TL, et al. The predictive value of transcutaneous oxygen tension
measurement in diabetic lower extremity ulcers treated with
hyperbaric oxygen therapy: A retrospective analysis of 1144
patients. Wound Rep Reg 2002;10:198-207.
14. Wattel F, Mathieu D, Fossati F, Nevie`re R, Coget JM. Hyperbaric
oxygen in the treatment of diabetic foot. Undersea Biomed Res
1990;17:160-1.
15. Wyss CR, Harrington RM, Burgess EM, Matsen FAIII. Transcutaneous
oxygen tension as a predictor of success after an amputation. J
Bone Joint Surg 1988;70:203-7.
16. Grolman RE, Wilkerson DK, Taylor J, Allinson P, Zatina MA.
Transcutaneous Oxygen measurements predict a beneficial
response to hyperbaric oxygen therapy in patients with non healing
wounds and critical limb ischemia. Am Surg 2001;67:1072-9.
17. Plafki C, Peters P, Almeling M, Welslau W, Busch R. Complications
and side effects of hyperbaric oxygen therapy. Aviat Space Environ
Med 2001;72:150.
How to cite this article: Kaur S, Pawar M, Banerjee N, Garg R. Evaluation
of the effcacy of hyperbaric oxygen therapy in the management of chronic
nonhealing ulcer and role of periwound transcutaneous oximetry as a predictor
of wound healing response: A randomized prospective controlled trial. J
Anaesth Clin Pharmacol 2012;28:70-5.
Source of Support: Nil, Confict of Interest: None declared.
Announcement
Android App
A free application to browse and search the journals content is now available for Android based
mobiles and devices. The application provides Table of Contents of the latest issues, which
are stored on the device for future offline browsing. Internet connection is required to access the
back issues and search facility. The application is compatible with all the versions of Android. The
application can be downloaded from https://market.android.com/details?id=comm.app.medknow.
For suggestions and comments do write back to us.
[Downloadedfreefromhttp://www.joacp.orgonSaturday,May18,2013,IP:187.214.28.78]||ClickheretodownloadfreeAndroidapplicationforthisjournal
You might also like
- 10 36516-Jocass 1240290-2908682Document5 pages10 36516-Jocass 1240290-2908682yyyyx842No ratings yet
- IAEA HPFX 2015Document6 pagesIAEA HPFX 2015Johana PatiñoNo ratings yet
- J. Antimicrob. Chemother. 2011 Xu 1687 95Document9 pagesJ. Antimicrob. Chemother. 2011 Xu 1687 95novia khairulbariaNo ratings yet
- A Study On Newer Dressing Materials Versus Conventional Dressing Materials in Ulcer HealingDocument5 pagesA Study On Newer Dressing Materials Versus Conventional Dressing Materials in Ulcer HealingratnaNo ratings yet
- The Efficacy of Daily Chlorhexidine Bathing For Preventing Healthcare-Associated Infections in Adult Intensive Care UnitsDocument12 pagesThe Efficacy of Daily Chlorhexidine Bathing For Preventing Healthcare-Associated Infections in Adult Intensive Care UnitsKanameMizumiNo ratings yet
- Stroids Meta 2023Document14 pagesStroids Meta 2023Sachin KumarNo ratings yet
- Appropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortDocument5 pagesAppropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortSiti Annisa NurfathiaNo ratings yet
- Comparison of The Short-Term Outcomes of Using DST and PPH Staplers in The Treatment of Grade Iii and Iv HemorrhoidsDocument7 pagesComparison of The Short-Term Outcomes of Using DST and PPH Staplers in The Treatment of Grade Iii and Iv HemorrhoidsdianisaindiraNo ratings yet
- Management of Peritoneal Metastases- Cytoreductive Surgery, HIPEC and BeyondFrom EverandManagement of Peritoneal Metastases- Cytoreductive Surgery, HIPEC and BeyondAditi BhattNo ratings yet
- Herrera Briones2013Document10 pagesHerrera Briones2013Fernando Lopez EncisoNo ratings yet
- Analisa Jurnal Stase MaternitasDocument11 pagesAnalisa Jurnal Stase MaternitasDedeDhazrekaNo ratings yet
- Nej Mo A 1414882Document9 pagesNej Mo A 1414882Corina Hagiu-RaduNo ratings yet
- Nej Mo A 1000067Document13 pagesNej Mo A 1000067Jorg AiNo ratings yet
- Hyerbaric Oxygenation - Final DraftDocument17 pagesHyerbaric Oxygenation - Final Draftapi-542958465No ratings yet
- 1471 2334 11 278Document6 pages1471 2334 11 278Dwi WirastomoNo ratings yet
- Annotated BibDocument16 pagesAnnotated Bibapi-542958465No ratings yet
- Pressure Ulcer ManagmentDocument16 pagesPressure Ulcer ManagmentRosalía Arroyo Flores100% (1)
- Factors Associated With Short-Term Mortality After Surgical Oncologic EmergenciesDocument12 pagesFactors Associated With Short-Term Mortality After Surgical Oncologic EmergenciesErinda SafitriNo ratings yet
- Health Related Quality of Life Following Open VersDocument8 pagesHealth Related Quality of Life Following Open Versevelynmoreirappgcmh.ufpaNo ratings yet
- UntitledDocument26 pagesUntitledAounAbdellahNo ratings yet
- Cancer Mucositis 6Document7 pagesCancer Mucositis 6arbfilmsNo ratings yet
- Nejmoa 1112088Document11 pagesNejmoa 1112088Med MedNo ratings yet
- Steroids in Chronic Subdural Hematomas SUCRE TrialDocument8 pagesSteroids in Chronic Subdural Hematomas SUCRE TrialEdward Arthur IskandarNo ratings yet
- Bisa 1Document8 pagesBisa 1justforuroNo ratings yet
- Corticosteroids in The Treatment of Severe Sepsis and Septic Shock in AdultsDocument14 pagesCorticosteroids in The Treatment of Severe Sepsis and Septic Shock in AdultsTatiana Salvatierra RiosNo ratings yet
- Ventosa Na Dor LombarDocument7 pagesVentosa Na Dor Lombarmauricio da silva barbosaNo ratings yet
- Blood 2012 LudwigDocument43 pagesBlood 2012 LudwigRaquel LopesNo ratings yet
- tmpFB45 TMPDocument6 pagestmpFB45 TMPFrontiersNo ratings yet
- Fiber TreatmentDocument8 pagesFiber TreatmentLana AdilaNo ratings yet
- 2018 Article 6554Document8 pages2018 Article 6554Raíla SoaresNo ratings yet
- Tese SnotDocument16 pagesTese SnotCaio GonçalvesNo ratings yet
- Project MoralesDocument6 pagesProject MoralesDiane Krystel G. MoralesNo ratings yet
- Dosimetric Comparison of AcurosBV With AAPMDocument19 pagesDosimetric Comparison of AcurosBV With AAPMBruno MendesNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Choudhury 2021 Lancet Onc BC2001 BCON Hypofrac Meta AnalysisDocument10 pagesChoudhury 2021 Lancet Onc BC2001 BCON Hypofrac Meta AnalysiszanNo ratings yet
- Fsurg 10 1151327Document7 pagesFsurg 10 1151327theomnagarowner2811No ratings yet
- Mertens2021 Article TransthoracicVersusTranshiatalDocument9 pagesMertens2021 Article TransthoracicVersusTranshiatalDr Shiv ChopraNo ratings yet
- The Effect of Clinical Pathway in Patients With Acute Complicated AppendicitisDocument6 pagesThe Effect of Clinical Pathway in Patients With Acute Complicated AppendicitisEko arya setyawanNo ratings yet
- Phase I Oncology Drug DevelopmentFrom EverandPhase I Oncology Drug DevelopmentTimothy A. YapNo ratings yet
- Negative Pressure Wound Therapy The Experience of Our Surgery DepartmentDocument10 pagesNegative Pressure Wound Therapy The Experience of Our Surgery DepartmentAthenaeum Scientific PublishersNo ratings yet
- Management of Chronic Pressure Ulcers: An Evidence-Based AnalysisDocument6 pagesManagement of Chronic Pressure Ulcers: An Evidence-Based AnalysisdevaNo ratings yet
- Vrijland Et Al-2002-British Journal of SurgeryDocument5 pagesVrijland Et Al-2002-British Journal of SurgeryTivHa Cii Mpuzz MandjaNo ratings yet
- Arm 23058Document10 pagesArm 23058drsadafrafiNo ratings yet
- Artikel TreatmentDocument8 pagesArtikel TreatmentFaiz MubarokNo ratings yet
- Effect of Chamomilla Recutita in The Oncology Patient With Oral Mucositis 2021Document13 pagesEffect of Chamomilla Recutita in The Oncology Patient With Oral Mucositis 2021emmanuelle leal capelliniNo ratings yet
- Precision Medicine Oncology: A PrimerFrom EverandPrecision Medicine Oncology: A PrimerLorna Rodriguez-RodriguezNo ratings yet
- Characteristics of Chinese Herbal Medicine Usage and Its Effect On Survival ofDocument9 pagesCharacteristics of Chinese Herbal Medicine Usage and Its Effect On Survival ofu106023406No ratings yet
- CC 9312Document10 pagesCC 9312Fitrianto Dwi UtomoNo ratings yet
- Classification of Masseter Hypertrophy For.11Document10 pagesClassification of Masseter Hypertrophy For.11alinutza_childNo ratings yet
- 2009hetrase CCMDocument12 pages2009hetrase CCMgiseladelarosa2006No ratings yet
- Clinical Applications of Nuclear Medicine Targeted TherapyFrom EverandClinical Applications of Nuclear Medicine Targeted TherapyEmilio BombardieriNo ratings yet
- A Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerDocument9 pagesA Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerOtoyGethuNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryLouis HutahaeanNo ratings yet
- Mitomycin C in The Endoscopic Treatment of Laryngotracheal Stenosis Systematic Review and Proportional Meta-AnalysisDocument12 pagesMitomycin C in The Endoscopic Treatment of Laryngotracheal Stenosis Systematic Review and Proportional Meta-AnalysisImam Taqwa DrughiNo ratings yet
- 1 s2.0 S0422763815301023 MainDocument4 pages1 s2.0 S0422763815301023 MainEghar EverydayishellNo ratings yet
- A Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerDocument9 pagesA Randomized Trial of Laparoscopic Versus Open Surgery For Rectal CancerFarizka Dwinda HNo ratings yet
- Steroid PaperDocument16 pagesSteroid PaperkhyatisethiaNo ratings yet
- Diagnostic Value of Candida Mannan Antigen and Anti-Mannan Igg, Igm Antibodies For Candida InfectionDocument18 pagesDiagnostic Value of Candida Mannan Antigen and Anti-Mannan Igg, Igm Antibodies For Candida Infectionmagda SiraitNo ratings yet
- 3avijeet EtalDocument9 pages3avijeet EtaleditorijmrhsNo ratings yet
- Gist NiñosDocument9 pagesGist NiñosJuan Jose LeonNo ratings yet
- PtFE Vs Cierre de PilaresDocument4 pagesPtFE Vs Cierre de PilaresJuan Jose LeonNo ratings yet
- 2005 - EMCNA - Disorders of PotassiumDocument25 pages2005 - EMCNA - Disorders of PotassiummagnavlerNo ratings yet
- Esplen Ecto MiaDocument6 pagesEsplen Ecto MiaJuan Jose LeonNo ratings yet
- CA Gastrico y CirugiaDocument5 pagesCA Gastrico y CirugiaDiego Bedón AscurraNo ratings yet
- Biopsia Hepatica para El CHCDocument5 pagesBiopsia Hepatica para El CHCJuan Jose LeonNo ratings yet
- Esplenomegalia Ind QXDocument5 pagesEsplenomegalia Ind QXJuan Jose LeonNo ratings yet
- Bypass Gastrico AbiertoDocument5 pagesBypass Gastrico AbiertoJuan Jose LeonNo ratings yet
- Ultrasonography in Diagnosis of Acute AppendicitisDocument6 pagesUltrasonography in Diagnosis of Acute AppendicitisJuan Jose LeonNo ratings yet
- Laparoscopia DiagnosticaDocument8 pagesLaparoscopia DiagnosticaJuan Jose LeonNo ratings yet
- 11-cm Lap-Band® System Placement After History ofDocument4 pages11-cm Lap-Band® System Placement After History ofJuan Jose LeonNo ratings yet
- Apendicectomia Laparos Vs AbiertaDocument12 pagesApendicectomia Laparos Vs AbiertaJuan Jose LeonNo ratings yet
- 11-cm Lap-Band® System Placement After History ofDocument4 pages11-cm Lap-Band® System Placement After History ofJuan Jose LeonNo ratings yet
- Abdomianl EmergenciesDocument15 pagesAbdomianl EmergenciesJuan Jose LeonNo ratings yet
- Arco Axilar de LangerDocument3 pagesArco Axilar de LangerJuan Jose LeonNo ratings yet
- Dialisis y Lapartomia 67-7-615Document4 pagesDialisis y Lapartomia 67-7-615Juan Jose LeonNo ratings yet
- Abscesos INtraabdominales ApendicectomiaDocument4 pagesAbscesos INtraabdominales ApendicectomiaJuan Jose LeonNo ratings yet
- Apendicectomia Laparos Vs AbiertaDocument12 pagesApendicectomia Laparos Vs AbiertaJuan Jose LeonNo ratings yet
- Arterias Del Estomago Higado y BazoDocument1 pageArterias Del Estomago Higado y BazoJuan Jose LeonNo ratings yet
- Histologic Severity of Appendicitis Can Be Predicted by Computed TomographyDocument5 pagesHistologic Severity of Appendicitis Can Be Predicted by Computed TomographyJuan Jose LeonNo ratings yet
- The Lymphatics of The Lower ExtremityDocument2 pagesThe Lymphatics of The Lower ExtremityJuan Jose LeonNo ratings yet
- The Abdominal AortaDocument9 pagesThe Abdominal AortaJuan Jose LeonNo ratings yet
- Irrigación Miembros PelvicosDocument7 pagesIrrigación Miembros PelvicosJuan Jose LeonNo ratings yet
- Arterias Del Estomago Higado y BazoDocument1 pageArterias Del Estomago Higado y BazoJuan Jose LeonNo ratings yet
- Wound Healing 2008Document7 pagesWound Healing 2008Juan Jose Leon100% (1)
- Pathophysiology of Acute Wound HealingDocument10 pagesPathophysiology of Acute Wound HealingJuan Jose LeonNo ratings yet
- Advanced Wound Care Therapies UlcerDocument182 pagesAdvanced Wound Care Therapies UlcerJuan Jose Leon100% (1)
- Helicobacter Pylori and Ulcers:: A Paradigm RevisedDocument8 pagesHelicobacter Pylori and Ulcers:: A Paradigm RevisedNavdeep DhanoaNo ratings yet
- Wound Healing 2008Document7 pagesWound Healing 2008Juan Jose Leon100% (1)
- ICRASH Abstract Book 2023Document92 pagesICRASH Abstract Book 2023elba lincolnNo ratings yet
- Injuries Diseases & Disorders of The Muscular SystemDocument22 pagesInjuries Diseases & Disorders of The Muscular SystemAngeli LozanoNo ratings yet
- Salpingo OophorectomyDocument2 pagesSalpingo OophorectomyKasamapon Oak ChawanachitNo ratings yet
- Novel Approaches To Clinical Trial Design and ImplementationDocument7 pagesNovel Approaches To Clinical Trial Design and ImplementationEditor IJTSRDNo ratings yet
- DBE South African Sign Language National Catalogue 2018Document7 pagesDBE South African Sign Language National Catalogue 2018Anonymous ozd4aLKhNo ratings yet
- Planned Parenthood Response To DHHDocument5 pagesPlanned Parenthood Response To DHHKevin LittenNo ratings yet
- GHGK SDocument48 pagesGHGK SAnonymous Syr2mlNo ratings yet
- Digestive SystemDocument27 pagesDigestive SystemLealyn Martin BaculoNo ratings yet
- Blood Cells MorphologyDocument20 pagesBlood Cells MorphologyKevin MikeNo ratings yet
- CCC Breast Feeding PolicyDocument1 pageCCC Breast Feeding PolicyVictorNo ratings yet
- ACTIVITY DESIGN-first AidDocument4 pagesACTIVITY DESIGN-first AidShyr R Palm0% (1)
- Rimso 50Document1 pageRimso 50monloviNo ratings yet
- New IB Diploma Psychology Topic PostersDocument8 pagesNew IB Diploma Psychology Topic PostersRajat Palaswadikar100% (1)
- Pinnacle Tecnica Quirurgica 2Document49 pagesPinnacle Tecnica Quirurgica 2Saenz Guzman LauraNo ratings yet
- API 580 SG Part 1, Rev 4Document77 pagesAPI 580 SG Part 1, Rev 4Mukesh100% (8)
- Blood Component PreparationDocument24 pagesBlood Component PreparationLaiba ArshadNo ratings yet
- (HSO) Medical Examination FormDocument1 page(HSO) Medical Examination FormKrizel LagundiNo ratings yet
- Sudeep SrivastavaDocument202 pagesSudeep Srivastavasandeepsrivastava41No ratings yet
- 2011 Sewarage SystemDocument29 pages2011 Sewarage Systemceafalld CE AF100% (1)
- Appendix 26 - SSG Prejoining Ship Check ListDocument1 pageAppendix 26 - SSG Prejoining Ship Check ListEliza's Soothing SoundsNo ratings yet
- Dosis Ranitidin cw1Document5 pagesDosis Ranitidin cw1Cristine Indria Pieter IINo ratings yet
- American Architecture Began With Frank Lloyd WrightDocument8 pagesAmerican Architecture Began With Frank Lloyd WrightAdheith South NgalamNo ratings yet
- Lifeline Supreme BrochureDocument5 pagesLifeline Supreme BrochureSumit BhandariNo ratings yet
- Ofw Child Experience: An Analysis PaperDocument2 pagesOfw Child Experience: An Analysis PaperClark AbonadoNo ratings yet
- Edmond Locard: Written By: Haley FischerDocument2 pagesEdmond Locard: Written By: Haley FischerHaley MichelleNo ratings yet
- Anatomy of The Male Reproductive SystemDocument70 pagesAnatomy of The Male Reproductive SystemDaniel HikaNo ratings yet
- Sanofi Corporate Social Responsibility Reporting 2011Document761 pagesSanofi Corporate Social Responsibility Reporting 2011CSRmedia.ro NetworkNo ratings yet
- Ayahuasca GuideDocument27 pagesAyahuasca GuidedevoutoccamistNo ratings yet
- Vol. 12 No. 4 Doi: ISSN: 1829 - 7285 E-ISSN: 2040 - 881X: 10.20473/jkl.v12i4.2020.276-284Document9 pagesVol. 12 No. 4 Doi: ISSN: 1829 - 7285 E-ISSN: 2040 - 881X: 10.20473/jkl.v12i4.2020.276-284Mpth MpthNo ratings yet