Professional Documents
Culture Documents
Pharmacy Care
Uploaded by
mysrskCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacy Care
Uploaded by
mysrskCopyright:
Available Formats
Section I
PHARMACEUTICAL CARE AND THE SCOPE OF PHARMACY PRACTICE
I. INTRODUCTION
1. The Practice of Pharmacy embraces a variety of settings, patient populations, and specialist as well as generalist pharmacists. Central to the practice of pharmacy, however, is the provision of clinical services directly to, and for the benefit of patients. 2. Definition. The term Pharmaceutical care describes specific activities and services through which an individual pharmacist cooperates with a patient and other professionals in designing, implementing and monitoring a therapeutic plan that will produce specific therapeutic outcomes for the patient.
II. SCOPE OF PRACTICE WITHIN PHARMACEUTICAL CARE
1. Role. Pharmaceutical care has evolved from an emphasis on prevention of drug- related problems (basically drug management) to extend roles of pharmacists in the Triage of patients, treatment of routine acute illnesses, management of chronic diseases, and primary disease prevention. 2. Function. The provision of pharmaceutical care does not imply that the pharmacist is no longer responsible for dispensing functions. In many instances, however, implementation of pharmaceutical care services necessitates a redesign of the professional work flow, with assignment of technical functions to technical personnel under the direct supervision and responsibility of the pharmacist.
III. UNIQUENESS OF PHARMACEUTICAL CARE
Provision of pharmaceutical care overlaps somewhat with other aspects of pharmacy practice (Table 1). However, pharmaceutical care is not the same as these other areas, which include: 1. Clinical Pharmacy 1. Patient counseling 2. Pharmaceutical services; when the activities of a pharmacy or pharmacy department are performed for faceless patients or charts, the activity is one of pharmacy service, not pharmaceutical care (e.g., chart or drug profile reviews without input from the patient or care giver is not pharmaceutical care).
1
Table 1 UNIQUENESS OF PHARMACEUTICAL CARE Traditional Pharmacy Prescription order or OTC request Upon Demand Obey Drug product Clinical Pharmacy Physicians or other health professionals Discontinuous Find fault or prevention Process Pharmaceutical Care Patient Continuous Anticipate or improve Outcomes
Primary Focus Continuity Strategy Orientation
IV. ESSENTIAL COMPONENTS OF PHARMACEUTICAL CARE A. Pharmacist patient relationship
The importance of putting a face and personality with the clinical picture is a key component of pharmaceutical care. A pharmacist can have a caring relationship with a patient but not with a chart or drug profile. A pharmacist cannot have empathy for words on a page or on a computer screen. Pharmaceutical care is based upon a collaborative effort between pharmacist and patient. B. Pharmacists workup of drug therapy (PWDT) The provision of pharmaceutical care is often centered around process described as the PWDT. Although the forms or methods used for this process may vary, the components are essentially the same. 1. Data collection. Collect, synthesize, and interpret relevant information such as: 1. Patient demographic data: age, sex, and race. 2. Pertinent medical information (1) Current and past medical history (2) Family history (3) Social history (4) Dietary history (5) Medication history ( prescription , OTC, social drugs and allergies) (6) Physical findings (e.g., weight, height, blood pressure, edema) (7) Laboratory or other test results (e.g., serum drug levels,potassium level, serum creatinine as relevant to drug therapy) 3. Patient complaints, symptoms, signs.
2. Develop or identify the CORE Pharmacotherapy Plan 1. C Condition or patient need 2. O Outcomes desired for that condition 3. R Regimen selected (prescribed) to achieve that outcome 4. E Evaluation parameters to assess outcome achievement 3. Identify the PRIME pharmacotherapy problems or indications for pharmacist interventions. The goal is to identify actual or potential problems that could compromise the desired patient outcomes (Table 2). 1. P Pharmaceutical based problems 2. R - Risks to patient 3. I Interactions 4. M Mismatch between medication and condition or patient needs. 5. E Efficacy issues 4. Formulate a FARM progress note to describe and document the interventions intended or provided by the pharmacist. 1. F Findings: the patient specific information that gives a basis for, or leads to, the recognition of a pharmacotherapy problem or indication for pharmacist intervention. 2. A Assessment: the pharmacists evaluation of the findings, including a statement of: (1) Any additional information that is needed to best assess the problem in order to make recommendations. (2) The severity, priority, or urgency of the problem. (3) The short-term and long-term goals of the intervention proposed or provided 1. Examples of short-term goals include: eliminate symptoms, lower blood pressure (BP) to 140/90 within 6 weeks, manage acute asthma flare up without requiring hospitalization. b. Examples of long-term goals include: prevent recurrence, maintain BP at less than 135/80, prevent progression of diabetic nerve disease. c. R- Resolution (including prevention): the intervention plan includes actual or proposed actions by pharmacist or recommendation to other health care professionals. The rationale for choosing a specific intervention should be stated. Intervention options may include: (1) Observation, reassessing, or following: no intervention necessary at this time. If no action was taken or recommended, the FARM note serves as a record of the event and should constitute part of the patients pharmacy chart or database.
(2) (3) (4) (5) (6)
Counseling or educating the patient or care giver Making recommendations to the prescriber Informing the prescriber Making recommendation to the prescriber Withholding medication or advising against use
d. M Monitoring and follow-up: the parameters and timing of follow-up monitoring to assess the efficacy, safety, and outcome of the intervention. This portion of the FARM note should include: (1) The parameter to be followed (e.g., pain, depressed mood, serum potassium level) (2) The intent of the monitoring ?(e.g, efficacy, toxicity, adverse event) (3) How the parameter will be monitored (e.g, interview patient, serum drug level, physical examination) (4) Frequency of monitoring (e.g, weekly, monthly) (5) Duration of monitoring (e.g, until resolved, while on antibiotic, until resolved then monthly for one year) (6) Anticipated or desired finding (e.g, no pain, euglycemia, healing of lesion) (7) Decision point to alter therapy when or if outcome is not achieved (e.g., pain still present after 3 days, mild hypoglycemia more than 2 times a week)
Table 2 PRIME PHARMACOTHERAPY PROBLEM TYPES Pharmaceutical Assess for incorrect Dose Route Duration Form Frequency timing Assess for known contraindication patient medication allergy drug-induced problem improper utilization (i.e., risk is misused) common/serious adverse effects medication error considerations Assess for drug-drug drug-food drug-disease/ condition drug-lab Assess for medication used without indication indication, condition, or complaint untreated Assess for suboptimal selection of pharmacotherapy for indication minimal or no evidence of therapeutic effectiveness suboptimal utilization of pharmacotherapy (taking or receiving medications incorrectly) - patient preference consideration (e.g., undesirable prior experiences with medication , does not believe works) - medication availability considerations - compliance or administration considerations (e.g., inability to pay, unable to administer correctly or at all)
Risks to Patient
Interactions
Mismatch between medication and indications/ conditions/ complaints Efficacy issues
V. CLINICAL SKILLS AND PHARMACISTS ROLES IN PHARMACEUTICAL
CARE
The skills activities and services inherent in the provision of pharmaceutical care include, but are not limited to, the following: 1. Patient assessment 1. Physical assessment 2. Barriers to adherence 3. Psychosocial issues 2. Patient education and counseling 1. interview skills 2. communication skills (e.g., empathy, listening, speaking or writing at the patients level of understanding) 3. ability to motivate, inspire 4. develop and implement patient education plan based on an initial education assessment 5. identification and resolution of compliance barriers 3. Patient- specific pharmacist care plans 1. recognition, prevention, and management of drug interactions 2. pharmacology and therapeutic (innovative and conventional) 3. interpretation of laboratory tests 4. knowledge of community resources, professional referrals 5. communication and rapport with community medical providers 4. Drug Treatment protocols 1. develop and maintain (update) protocols 2. follow protocols as o pharmacist clinician 3. monitor aggregate adherence to treatment protocols (e.g., drug utilization evaluations {DUE} ) especially for managed care or health system facility. 5. Dosage adjustment 1. Identify patients at risk for exaggerated or subtherapeutic response. 2. Apply pharmacokinetic principles to determine patient-specific dosing 3. Order and interpret relevant tests at correct time intervals to assess dosage adjustment (e.g., plasma drug concentrations, blood glucose levels, blood pressure measurements) 6. Selection of therapeutic alternatives 1. use drug information resources effectively 2. review and critique drug literature 3. construct comparative analyses to support therapeutic decisions
7. Prescriptive authority in designated practice sites or positions H. Preventive services 1. Immunizations 2. Screenings 3. Health and wellness education I. Managerial skills 1. plan, direct and implement pharmaceutical care activities within various practice environments, such as community pharmacy, ambulatory care settings, managed or contractual care, home health services, long-term care facilities, inpatient hospital practice, and others. 2. Allocate resources.
VI. PHARMACEUTICAL CARE AS THE MODEL FOR PHARMACY PRACTICE
The concepts, activities,, and services of pharmaceutical care form the basis for provision of clinical services directly to, and for the benefit of patient in all pharmacy practice settings. These settings include home health, hospital, ambulatory care, primary care, consultation, long term care, and community pharmacy practice. Workflow, staffing patterns, processes, and pharmacy programs might differ, but the core approach to patient care remains pharmaceutical care in all settings. Figure 1 & Figure2 illustrate pharmaceutical care models in the institutional and community pharmacy settings.
VII. Documentation of Pharmaceutical Care
Documentation of pharmaceutical care is integral to continuity of care, demonstration of clinician competence, communication among health care providers, evidence of contributions to patient care, and reimbursement of professional services. 1. Pharmaceutical care, including the Pharmaceutical care plan process (CORE, PRIME & FARM), is a systematic method for recording the pharmacists examination of a patient pharmacotherapy and subsequent identification of medication-related problems. 2. In most practice settings, computer software programs maintain patient data and drug profile records. Thus, after documentation of the initial pharmaceutical care plan, patient data or drug regimens are included in subsequent FARM notes only if a change occurs that is relevant to the therapeutic issue being addressed in the note.
3. Forms that summarize pharmacists interventions using a unified coding system are useful for processing reimbursement of billing forms, but these forms are not adequate documentation of pharmaceutical care. These forms do not communicate to other health professionals the depth and quality of pharmacist interventions or the pharmacists plan for ongoing pharmaceutical care.
VIII. Pharmaceutical Care : An ongoing process The patient profile is revised and re-assessed each time a new drug is added to or deleted from the medication regimen, a new disease or condition is diagnosed, or the patient undergoes other clinical intervention, such as surgery. When the patient returns to the pharmacy or is readmitted to the health system facility, the pharmacist uses the patient profile, PWDT, and FRAM notes (maintained in the patient pharmacy chart or in the medical chart) as the basis for ongoing pharmacists-patient interactions. XI. IMPORTANCE OF PHARMACEUTICAL CARE IN TODAYS PHARMACY PRACTICE
1. The potential for medication errors is growing, and one professional group must assume a primary role in addressing this issue rather than fragmented efforts by various groups or individuals. The pharmacist is trained specifically to address these therapeutic issues. 1. The use of prescription and nonprescription medications is growing and now constitutes the primary therapeutic modality available to health care practitioners and patients. 2. The number, complexity, and potency of prescription and non prescription drug products is increasing. 2. The need for pharmaceutical care secures an enduring role for the pharmacist in the American health care system. Every encounter with patients, regardless of practice setting, provider pharmaceutical care. 3. Pharmaceutical care activities integrate pharmacists into the health care system of the future.
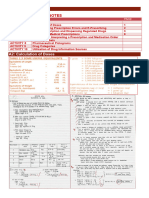
Figure 1 - TEMPLATE FOR PHARMACEUTICAL CARE : INSTITUTIONAL
PRACTICE
Data Collection 1. Review patient medical record 2. Review medication profile 3. Interview patient
Develop or identify the CORE Pharmacotherapy Plan Key Points 1. Focus on outcomes, not interventions Identify drug related problems or patient needs (PRIME) 2. Daily pharmacy rounds are important Pharmacists can make rounds without medical team 3. Use this approach with all clinical Formulate a Pharmaceutical Care Plan pharmacokinetic dosing, disease management clinics, Communicate Plan with patient, health care team, etc programs, as 1. 2. 3. 4. 5. 6. 7. 8. 9. Individual dosing Medication without indication Indication without medication Potential or actual allergy or ADR Drug-drug/ lab/ food interaction Optimal drug selection Pharmacokinetics Education Potential cost saving (IV or PO, etc) Plan includes Findings Assessment Resolution/ recommendation Monitoring such
clinical pathways, etc
Document actions taken in patient medical record
You might also like
- Fundamentals of Clinical Pharmacy PracticeFrom EverandFundamentals of Clinical Pharmacy PracticeRating: 4.5 out of 5 stars4.5/5 (2)
- Chapter 5 - Instructor's Guide To Pharmacotherapy Casebook 5eDocument11 pagesChapter 5 - Instructor's Guide To Pharmacotherapy Casebook 5eRina Mai Saroh63% (8)
- Pharmacy Care PlanDocument20 pagesPharmacy Care PlanIsrar Qureshi100% (2)
- Community Pharmacy: Basic Principles and ConceptsFrom EverandCommunity Pharmacy: Basic Principles and ConceptsRating: 3 out of 5 stars3/5 (2)
- Dispensing and Medication CounselingDocument12 pagesDispensing and Medication CounselingLei100% (3)
- Social and Administrative Aspects of Pharmacy in Low- and Middle-Income Countries: Present Challenges and Future SolutionsFrom EverandSocial and Administrative Aspects of Pharmacy in Low- and Middle-Income Countries: Present Challenges and Future SolutionsRating: 1 out of 5 stars1/5 (1)
- Farm NoteDocument3 pagesFarm NoteSreya Sanil50% (2)
- Clinical Pharmacy Education, Practice and Research: Clinical Pharmacy, Drug Information, Pharmacovigilance, Pharmacoeconomics and Clinical ResearchFrom EverandClinical Pharmacy Education, Practice and Research: Clinical Pharmacy, Drug Information, Pharmacovigilance, Pharmacoeconomics and Clinical ResearchRating: 4 out of 5 stars4/5 (3)
- Prime Pharmacotherapy ProblemsDocument1 pagePrime Pharmacotherapy Problemsjp100% (3)
- Hospital Pharmacy - LECTURE 8Document34 pagesHospital Pharmacy - LECTURE 8Anish Kumar A100% (1)
- Generic DispensingDocument30 pagesGeneric Dispensingshervintancruzado83% (6)
- Pharmacy InformaticsDocument4 pagesPharmacy InformaticsMaharlika EgminNo ratings yet
- Handbook of Drug Interaction and the Mechanism of InteractionFrom EverandHandbook of Drug Interaction and the Mechanism of InteractionRating: 1 out of 5 stars1/5 (1)
- I. Pharmacist's Workup of Drug Therapy For Bronchial AsthmaDocument7 pagesI. Pharmacist's Workup of Drug Therapy For Bronchial AsthmaDave Cabuyadao0% (1)
- Pharmacy Practice Research Case StudiesFrom EverandPharmacy Practice Research Case StudiesRating: 5 out of 5 stars5/5 (1)
- Chapter 5 Hospital FormularyDocument6 pagesChapter 5 Hospital Formularyiamgerardgarces100% (15)
- History of Hospital PharmacyDocument41 pagesHistory of Hospital PharmacyLovely Ann Ayapana69% (16)
- Dispensing & Medical CounselingDocument25 pagesDispensing & Medical CounselingNik Ferandos100% (1)
- FOREIGN PHARMACY GRADUATES EQUIVALENCY EXAMINATION (FPGEE): Passbooks Study GuideFrom EverandFOREIGN PHARMACY GRADUATES EQUIVALENCY EXAMINATION (FPGEE): Passbooks Study GuideNo ratings yet
- Clinical Pharmacy - A Definition: Fahad Hussain 9/20/2010Document4 pagesClinical Pharmacy - A Definition: Fahad Hussain 9/20/2010Tawhida Islam100% (1)
- Hospital Pharmacy: Mae Quenie A. Tiro, RPHDocument100 pagesHospital Pharmacy: Mae Quenie A. Tiro, RPHRonan Keanlor Tiro Llaguno82% (22)
- Briefer On RA 10918Document3 pagesBriefer On RA 10918Eugene UC100% (1)
- Clinical PharmacyDocument16 pagesClinical Pharmacyblossoms_diyya299850% (6)
- Databook for Clinical PharmacologyFrom EverandDatabook for Clinical PharmacologyRating: 5 out of 5 stars5/5 (1)
- Pharmacy Ethics and Jurisprudence in The PhilippinesDocument18 pagesPharmacy Ethics and Jurisprudence in The PhilippinesMeg Gutierrez100% (6)
- Páginas Desdepharmacotherapy Casebook 10th Ed.Document61 pagesPáginas Desdepharmacotherapy Casebook 10th Ed.Glo VsNo ratings yet
- Unit I: Introduction To Pharmacy InformaticsDocument24 pagesUnit I: Introduction To Pharmacy InformaticsLynette Evangelista100% (1)
- Hospital and Clinical Pharmacy Answer Key-RED PACOPDocument75 pagesHospital and Clinical Pharmacy Answer Key-RED PACOPArk Olfato Parojinog100% (3)
- Community Pharmacy PracticeDocument18 pagesCommunity Pharmacy Practiceكسلان اكتب اسميNo ratings yet
- Jurisprudence and EthicsDocument22 pagesJurisprudence and EthicsRozamae Magnanao100% (1)
- Dispensing, Incompatibility & Adr Page 1 of 19Document19 pagesDispensing, Incompatibility & Adr Page 1 of 19Yishka ZaireahNo ratings yet
- Hypertensive Crisis: Instructor'S Guide To Changes in This EditionDocument6 pagesHypertensive Crisis: Instructor'S Guide To Changes in This Editionnurmaliarizky100% (1)
- Internship 9 10Document26 pagesInternship 9 10Desa Refuerzo100% (1)
- Community Pharmacy InternshipDocument12 pagesCommunity Pharmacy InternshipSun Shines50% (2)
- Pharmaceutical Care PlanDocument91 pagesPharmaceutical Care PlanYuliusDenisChrismaajiNo ratings yet
- Preventing Dispensing ErrorsDocument39 pagesPreventing Dispensing ErrorsMark RevertNo ratings yet
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesZen HeartNo ratings yet
- DISPENSING 1 - Module 1Document68 pagesDISPENSING 1 - Module 1Precious Faith SabalaNo ratings yet
- Patient ScriptingDocument1 pagePatient ScriptingKarren ReyesNo ratings yet
- Community PharmacyDocument13 pagesCommunity PharmacyVikrant Saluja100% (2)
- FormularyDocument32 pagesFormularyAnonymous U4JLHU9e3100% (1)
- Classification of Organic Medicinals and Pharmaceuticals-FinalsDocument4 pagesClassification of Organic Medicinals and Pharmaceuticals-FinalsEzra Linn Navacilla100% (1)
- Pharmacy and Therapeutic CommitteDocument23 pagesPharmacy and Therapeutic CommitteLp Dhq Teaching100% (1)
- Hospital Pharmacy Internship 2020Document7 pagesHospital Pharmacy Internship 2020Buenconsejo Gelo100% (1)
- Dose and IntervalDocument37 pagesDose and IntervalRosel Ann BontiaNo ratings yet
- INCOMPATIBILITIESDocument27 pagesINCOMPATIBILITIESArk Olfato Parojinog100% (1)
- HospiDocument8 pagesHospiYvana Dela CruzNo ratings yet
- Systematic Approaches in Answering A Drug Information QueryDocument4 pagesSystematic Approaches in Answering A Drug Information Queryabirami p100% (2)
- 3-Pharmacy, Its Organization and PersonnelDocument27 pages3-Pharmacy, Its Organization and PersonnelHaseeba Khan100% (4)
- Hospital Pharmacy Management Manual CORETEXTDocument25 pagesHospital Pharmacy Management Manual CORETEXTpharmaebooks88% (8)
- Hospital and Clinical Pharmacist PDFDocument23 pagesHospital and Clinical Pharmacist PDFmajd67% (6)
- DISPLABPreps1 20 2Document21 pagesDISPLABPreps1 20 2Alexa Joy C. InguilloNo ratings yet
- Pacop Pink Pharmacology ReviewerDocument100 pagesPacop Pink Pharmacology Reviewer;'SiLeNt';100% (1)
- TuberculosisDocument24 pagesTuberculosismysrskNo ratings yet
- Imtehanat Ki Tayari Ka TarikaDocument33 pagesImtehanat Ki Tayari Ka TarikamysrskNo ratings yet
- Project ManagementDocument7 pagesProject ManagementmysrskNo ratings yet
- Antimicrobial Guideline 2009 2010Document78 pagesAntimicrobial Guideline 2009 2010Lalalala Gabriella KristianiNo ratings yet
- WazaifDocument8 pagesWazaifmysrsk100% (1)
- Viscometer:-: Standard Laboratory Viscometers For LiquidsDocument6 pagesViscometer:-: Standard Laboratory Viscometers For LiquidsmysrskNo ratings yet
- Full Medical Examination Form For Foreign Workers: Work Pass DivisionDocument1 pageFull Medical Examination Form For Foreign Workers: Work Pass Divisionkarthik.swamyNo ratings yet
- Conduction Blocks in Acute Myocardial Infarction: A Prospective StudyDocument6 pagesConduction Blocks in Acute Myocardial Infarction: A Prospective StudyJack JacksonNo ratings yet
- Nematodes of The Turkey Meleagris Gallopavo (Galliformes: Phasianidae) From Al-Nasiryah, IraqDocument6 pagesNematodes of The Turkey Meleagris Gallopavo (Galliformes: Phasianidae) From Al-Nasiryah, IraqMd Ashikur RahmanNo ratings yet
- Delayed Homicides and The Proximate Cause.8Document5 pagesDelayed Homicides and The Proximate Cause.8rheanditahafsaNo ratings yet
- Sample ReportDocument3 pagesSample ReportRobeants Charles PierreNo ratings yet
- Perio QuestionsDocument32 pagesPerio QuestionsSoha Jan KhuhawarNo ratings yet
- Department of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseaseDocument84 pagesDepartment of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseasePatty ReyesNo ratings yet
- COPD CurrentDocument9 pagesCOPD Currentmartha kurniaNo ratings yet
- Pumpkin TakoshiDocument22 pagesPumpkin TakoshiSudhanshu NoddyNo ratings yet
- The Effect of Tobacco Smoking Among Third Year Student Nurse in The University of LuzonDocument6 pagesThe Effect of Tobacco Smoking Among Third Year Student Nurse in The University of LuzonNeil Christian TadzNo ratings yet
- Introduction of Magic Rose UpDocument21 pagesIntroduction of Magic Rose UpanggrainiNo ratings yet
- Dula-Tungkulin o Gampanin NG ProduksyonDocument12 pagesDula-Tungkulin o Gampanin NG ProduksyonBernadette DuranNo ratings yet
- Beauty Hankering For Memory: Marne L. KilatesDocument9 pagesBeauty Hankering For Memory: Marne L. KilatesKuya ReaGoNo ratings yet
- NW NSC GR 10 Life Sciences p1 Eng Nov 2019Document12 pagesNW NSC GR 10 Life Sciences p1 Eng Nov 2019lunabileunakhoNo ratings yet
- Riddhi Perkins College ResumeDocument3 pagesRiddhi Perkins College Resumeapi-3010303820% (1)
- 3E - Agustin, Anne Julia - Group 1 - Case 7,8Document5 pages3E - Agustin, Anne Julia - Group 1 - Case 7,8Anne Julia AgustinNo ratings yet
- Menstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleDocument6 pagesMenstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Resource Material - Day 1 Primary Register Activity - ANC Register - 0Document3 pagesResource Material - Day 1 Primary Register Activity - ANC Register - 0Ranjeet Singh KatariaNo ratings yet
- Cholecystitis BelgradeDocument52 pagesCholecystitis BelgradeLazar VučetićNo ratings yet
- Factsheet - Ectopic Heartbeats (160201)Document1 pageFactsheet - Ectopic Heartbeats (160201)RodiAdiNo ratings yet
- Punjab Municipal Corporation Act, 1976 PDFDocument180 pagesPunjab Municipal Corporation Act, 1976 PDFSci UpscNo ratings yet
- DOPR Vision 2030Document36 pagesDOPR Vision 2030Hendi HendriansyahNo ratings yet
- The Effects of The Concept of Minimalism On Today S Architecture Expectations After Covid 19 PandemicDocument19 pagesThe Effects of The Concept of Minimalism On Today S Architecture Expectations After Covid 19 PandemicYena ParkNo ratings yet
- Information On The Use of Domperidone To Increase Milk Production in Lactating WomenDocument3 pagesInformation On The Use of Domperidone To Increase Milk Production in Lactating WomenKhairul HananNo ratings yet
- Resveratrol and Its Effects On Human Health and LongevityDocument367 pagesResveratrol and Its Effects On Human Health and LongevityArnulfo Yu LanibaNo ratings yet
- Sino-Nasal Outcome Test (SNOT-22) Questionnaire: Patient's Name Date DOBDocument2 pagesSino-Nasal Outcome Test (SNOT-22) Questionnaire: Patient's Name Date DOBIchsanJuliansyahNo ratings yet
- Nclex Mnemonics 2020 2Document9 pagesNclex Mnemonics 2020 2Winnie OkothNo ratings yet
- Aac-Augmentative and Alternative CommunicationDocument35 pagesAac-Augmentative and Alternative Communicationrenuka aurangabadkerNo ratings yet
- DASH Questionnaire Disability Arm Shoulder HandDocument3 pagesDASH Questionnaire Disability Arm Shoulder HandChristopherLawrenceNo ratings yet
- GMO Pro Arguments (Gen-WPS OfficeDocument4 pagesGMO Pro Arguments (Gen-WPS OfficeFranchesca RevelloNo ratings yet