Professional Documents
Culture Documents
Letter To HDC Re Medical Code of Ethics by Roger Brooking
Uploaded by
Roger BrookingOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Letter To HDC Re Medical Code of Ethics by Roger Brooking
Uploaded by
Roger BrookingCopyright:
Available Formats
Health and Disability Commissioner PO Box 11934 Wellington 6142
26 July, 2013
Copies to the New Zealand Medical Association & the Ombudsman
Corrections Medicines Policy and the HDC report titled: Team Development Workshops for Prisons Nursing Services delivered by Dr Elizabeth Finn and Mr David Webber"
Dear Commissioner I am writing to you regarding the impact of paragraph 6.1.1 of Corrections Department Medicines Policy on the medical treatment of prisoners and the interpretation of this policy by the HDC. Paragraph 6.1.1 of the Medicines Policy says: "Prescribing medication that can be misused/abused or has some economic value in a prison environment (or example benzodiazepines, opioids, zopiclone) is actively discouraged. A clinically suitable alternative medication or treatment option is preferred. If however, there is no alternative, then a plan to safely manage the medication and/or the patient's treatment must be implemented. For example, giving a syrup or liquid formula instead of tablets." Henceforth, I shall refer to this as the Departments discouraged medication policy - which has detrimental consequences for prisoners, nurses and doctors. Prison inmates are known to experience a much higher prevalence of physical and mental health problems than those in the community - and often self-medicate with alcohol or drugs. New Zealand research suggests that 80% to 90% of those who end up in prison have problems with addiction and substance abuse. The result is that when sentenced to prison, offenders who are dependent are often forced into immediate withdrawal. Unless this is managed properly, it can lead to considerable distress; in the case of withdrawal from alcohol, it can lead to seizures and even death. Dr Wayne Cunningham, a senior lecturer at Otago Medical School, used to be the prison doctor at Otago Correctional Facility (OCF). Dr Cunningham told me that one of his greatest concerns was the lack of proper medical care offered to alcoholics and drug addicts forced into detoxing and pushed into withdrawing from addictive drugs in prison. He said that once his contract as prison doctor came to an end, he declined to renew it because he was concerned that eventually someone would die because of a lack of proper medical care. He was right. Soon after he left, two prisoners (Richard Barriball and Jai Davis) died within three months of each other. In both cases, inadequate medical care appears to have been a contributing factor; formal complaints have been made with the HDC about both cases. Dr Cunningham can be contacted at the Milton Health Centre on 03 417 8226. Corrections Department response The process of addressing addiction and withdrawal in prison is exacerbated by the Departments discouraged medication policy. Recently, I wrote to Corrections asking what other medications are discouraged besides opiates and benzodiazepines. I also asked for a list of clinically suitable alternatives that the Department recommends and what research or evidence exists indicating that 1
there are suitable alternatives. I received a confusing reply from Bronwyn Donaldson, Director of Offender Health, stating that there was no list of discouraged medications and no list of alternatives. However, Ms Donaldson went on to say: Corrections Operational Intelligence team analyses prison activities for any safety and security risks. At times they may find particular prescription drugs that are found to have gained currency and are being traded within prison. Releasing a list of these medicines may threaten the good order and security of the prison as it would inform prisoners of tradable items and potentially increase criminal behaviour within prison. Therefore, I am withholding this information under section 6(c) of the OIA" (copy attached). Whether there is a list or not, the upshot is that Corrections management believe they are entitled to discourage prison doctors from prescribing any medication that has potential currency in the prison. I have written to the Ombudsman asking that Corrections be persuaded to disclose this secret list of medications. Currently, because Corrections refuses to disclose the list, no one, including prison doctors, actually knows which medications are discouraged besides opiates and benzodiazepines. From previous correspondence with the Department I am aware that Ritalin and other drugs used to treat ADHD are also discouraged. From time to time medication used to treat other mental health problems may also be traded in prison and then be discouraged. Breaching human rights and other legislation Denying patients clinically appropriate medication, especially when they are in severe pain or have mental health disorders, is fundamentally inhumane and a breach of human rights. The denial of opiates to inmates experiencing severe pain contributes to depression and even to suicide. In my view, the systematic denial of opiates and other clinically appropriate medication is akin to an enhanced torture technique; it causes serious distress to the prisoner without leaving any visible evidence of the harm and suffering it causes. This policy is also a breach of Regulation 73 of the Corrections Amendment Regulations 2013 which describes the Duties of a Health Centre Manager as follows. Section 73(1) says: The health centre manager of a prison must take all practicable steps to maintain the physical and mental health of prisoners to a satisfactory standard. Section 73(2)(c) says the Health Centre Manager must: ensure that medicine is administered to a prisoner in accordance with his or her medical needs. The Departments discouraged medication policy is incompatible with this legislation. The denial of medication also appears to breach Section 151 of the Crimes Act requiring anyone who has actual care or charge of a person who is a vulnerable adult to (a) provide that person with necessaries; and (b) to take reasonable steps to protect that person from injury. The policy also appears to breach Section 75 of the Corrections Act 2004 which states: A prisoner is entitled to receive medical treatment that is reasonably necessary and the standard of healthcare that is available to prisoners in a prison must be reasonably equivalent to the standard of healthcare available to the public. Although caution has to be taken with potentially addictive medication, members of the public are not generally denied opiates, or mental health medications, just because they are open to abuse and potentially tradable. But prisoners are - so this discouraged medication policy negates any possibility that prisoners can receive an equivalent level of care to patients in the community.
The Medical Code of Ethics In addition to potential breaches of human rights, the Crimes Act and the Corrections Act, this policy also appears to be incompatible with doctors medical ethics. For instance, the preliminary statement in the New Zealand Medical Code of Ethics states: Standard treatises on medical ethics cite four moral principles: autonomy, beneficence, nonmaleficence, and justice. Autonomy recognises the rights of patients to make decisions for themselves. Beneficence requires a doctor to achieve the best possible outcome for an individual patient Non-maleficence implies a duty to do no harm. Justice incorporates notions of equity and of the fair distribution of resources. In New Zealand today there is also an increasingly wide recognition of the principle of partnership - between doctor and patient. If the Department does not allow prison doctors to prescribe opiates or other discouraged medications when appropriate, all four of these principles are being negated prison doctors are not allowing patients to make decisions for themselves; they are not achieving the best possible outcome for their patients; they are actively discriminating against this particular client group on the basis of the fact that they are in prison and they are inadvertently doing harm. If it is true that there is an increasingly wide recognition of the principle of partnership between doctor and patient in New Zealand, this is clearly not the case for those in prison. In addition to these introductory comments, the New Zealand Medical Code also contains 12 Principles and 44 Professional Responsibilities or Responsibilities to the Patient. The first principle is Consider the health and well-being of the patient to be your first priority. When doctors are not allowed to prescribe clinically appropriate medication because of the Departments concern that medicines may be traded, then prison security has become the doctors first priority - not the wellbeing of the patient. Recommendation number 7 states: When a patient is accepted for care, doctors should render medical service to that person without discrimination (as defined by the Human Rights Act). When prisoners in severe pain are not allowed certain medication simply because they are in prison, that constitutes discrimination. Professional responsibility number 37 states: Doctors should not countenance, condone or participate in the practice of torture or other forms of cruel, inhuman, or degrading procedures, whatever the offence of which the victim of such procedures is suspected, accused or guilty. Denial of appropriate painkilling medication for patients in severe pain is inherently cruel, inhuman and degrading. The point has already been made that the discouraged medication policy is tantamount to torture. Involvement of the HDC What is especially concerning is that the HDC appears to endorse this policy. The evidence for this appears in the report titled Team Development Workshops for Prisons Nursing Services delivered by Dr Elizabeth Finn and Mr David Webber". In 2009 Dr Finn and Mr Webber conducted workshops at 13 prisons and identified a number of issues of concern with the management of prison health services. Despite their concerns, the authors endorsed the view that prison doctors should be discouraged from prescribing certain medication. On page 4, it says:
It appears that some doctors are not sufficiently aware of the context of the prison environment and the particular challenges it presents. For example, some medications are inappropriate in this environment because of their potential for use as currency. Lack of national consistency with respect to provision of medications to patients who are prisoners may lead to stand-over tactics and abuse directed towards doctors in the first instance, and also towards nurses. A robust induction programme for doctors would be helpful. On page 5, the report even reprimands doctors in hospital Emergency Departments apparently for not doing what they are told by prison nurses. It says: EDs may not cooperate with advice from nurses that certain medications are not allowable in prisons, and still prescribe these (codeine, morphine). These statements suggest the HDC wholeheartedly endorses Corrections policy that prisoners should not be allowed opiates or other potentially tradable medications. The reality is that prisoners often have to be taken to ED with serious medical problems or injuries and may be in severe pain. For acute pain, opiates are likely to be the medication of choice. For patients with chronic pain problems, opiates may well be appropriate in the long term as well. However, the Finn/Webber report suggests HDC policy is that prisoners in severe pain should not have it relieved, even in emergency situations? Apparently, they should continue to suffer - even when the pain is so bad they need to be taken to hospital? That the HDC would endorse this deliberate abuse of prisoners is hard to believe. But the only alternative to this interpretation is that HDC agrees with Corrections that prisoners should be given clinically suitable alternatives. However, it seems there is no list of suitable alternatives especially in acute or crisis situations. Indeed if there were effective non-addictive alternatives, opiates would no longer be prescribed. For long-term or chronic pain, psychological or cognitive approaches to pain management may be effective. But these options are not available in prison and not part of Corrections Medicines Policy. This brings us back to the disturbing reality - which is that the HDC appears to be endorsing a policy that prisoners in severe pain should be denied opiate medication and (by virtue of medical neglect) should continue to suffer. And not just prisoners in pain. This applies to any and all prisoners who may become victims of the Departments discouraged medication policy which extends well beyond opiates. This appears to indicate a remarkable lack of understanding of doctors ethical responsibilities to their patients and an extraordinary lack of compassion for patients in prison. It actually suggests the HDC is complicit in Corrections strategy to breach the human rights of prisoners, deny them appropriate medical care and subject them to cruel and inhumane treatment. Concerns about the integrity of HDC investigations into prison healthcare For an agency responsible for promoting safe medical practices, this is truly disturbing. It raises serious questions about the integrity of investigations into complaints by prisoners who need these medications. If the HDC has already made up its mind that inmates should not receive them, then an inherent bias is brought to any investigation where pain management, addiction, withdrawal or mental health issues are a factor in the complaint because prisoners with these issues are being denied appropriate medication/treatment.
Unfortunately, the problem goes even deeper that. The workshops run by Dr Finn and Mr Webber were conducted at the request of the Corrections Department specifically because of concerns about bullying and poor management in prison health centres. Dr Finn and Mr Webber described what was happening as horizontal bullying. But it seems the authors failed to realise that the discouraged medication policy actually contributes to a nursing culture where bullying is legitimized. This is because prescribing is supposed to be the domain of qualified doctors or nurse practitioners who are licenced to prescribe. However, Bronwyn Donaldson makes it clear that Corrections management wants nurses to have a say in this process. In response to my query about how doctors are supposed to know which medications are actively discouraged (since there is no written list), Ms Donaldson wrote: Medical Officers (i.e. doctors) work closely with Health Centre Managers (i.e. nurses) who are made aware of the potential risks with the prescription of particular drugs in a prison setting If a Health Centre Manager has concern over the prescription of a specific medication they can raise this with the Medical Officer and discuss the patients clinical requirements. Prisoners tell me it is not just the Health Centre Managers who tell the doctors what to prescribe - so do other nurses. This manifests in different ways. Commonly, nurses will manufacture excuses (usually that the patient was attempting to divert the medication) in order to persuade the doctor into stopping his medication. I have also heard of cases where prisoners who are deemed difficult have been denied prescribed medication by a nurse without consultation with the prison doctor. The doctor may not even be informed that the prisoners medication has been stopped. In other words, there is confusion about who is in charge which puts both nurses and doctors into a difficult position. Nurses are being told to perform a task they are not qualified to undertake and doctors are expected to do as they are told - including doctors who dont even work for the Corrections Department (i.e. those in hospital EDs). Underlying this behaviour, it seems some nurses identify so closely with the Departments policies, they lose sight of their nursing ethics. They come to believe their primary role is to manage prisoners and the dispensation and denial of medication then becomes a mechanism of control, or a means to punish. This creates tension between those doctors and nurses who would rather ignore the discouraged medication policy (because they follow their ethics and want prisoners to receive the best care possible) and those nurses who advocate for it. When the nurses who enjoy power and control dominate this debate, the well-being of prisoners is ignored and nursing and medical ethics go out the window. This appears to be what happened at Otago prison in 2010/11 when two prisoners died within three months of each other (Richard Barriball and Jai Davis). (This confusion of roles has now been compounded by section 19A of the Corrections Amendment Act 2013 which removes statutory responsibility for the health care of prisoners from Medical Officers and gives it entirely to Heath Centre Managers. This will almost inevitably increase the tension between prison doctors and nurses who are now legally in control.) The point is that by endorsing the discouraged medication policy, the HDC has failed to appreciate that this policy is actually one of the key factors contributing to internal tension and horizontal 5
bullying the very issue the HDC was asked to address. The HDCs willingness to deny prisoners appropriate medication calls into question the integrity of its investigations into complaints from prisoners about their medical treatment. It also calls into question the HDC's ability to investigate complaints by prisoners concerning rude or bullying behaviour by nurses (and abusive responses from prisoners) when this behaviour is part and parcel of the discouraged medication policy. Consistent protocols Despite the existence of the discouraged medication policy, there is considerable variation in the way it is implemented. In some prisons, codeine is allowed but tramadol is not. In other prisons, tramadol is allowed but codeine is not. In response to this inconsistency, the HDC recommends: National policies regarding the availability of medicines and health services in prisons are (put) in place and complied with by all staff to ensure consistent services over all prison sites. Instead of a national policy denying prisoners certain medication, the protocols that need to be implemented nationally are those that ensure prisoners take/swallow their medication. These protocols already exist; they just need to be implemented more consistently. Will these protocols always prevent medication from being diverted or traded? Of course not. But illicit drug use is at an all-time low because the Department has an effective random drug testing policy which picks up opiates and benzodiazepines as well as illicit drugs. The point is, risk can be minimised, but it cannot be eliminated. Surely, it is better that a prisoner occasionally diverts medication than hundreds of prisoners live in pain, and hundreds with mental health problems suffer unnecessarily because they are denied appropriate medication. Further questions The other day, I received a letter from Chief Legal Advisor, Katie Elkin advising that in 2012, the HDC received only 36 complaints concerning prisoners health care. The letter from Ms Elkin indicated that none of these complaints were formally investigated by the Commissioner. 1) Did whoever investigated each of these 36 complaints make any enquiries (either of the prisoner or the prison health service) to ascertain whether or not the prisoner who made the complaint had been denied a discouraged medication. 2) Given that the HDC presumably endorses the use of clinically suitable alternatives to replace discouraged medications, when investigating complaints about medical treatment, what steps does the HDC take to determine whether the prescribed alternatives are indeed clinically suitable? 3) If the HDC does not know exactly what medications are discouraged or what is a suitable alternative, how can it evaluate whether or not a complaining prisoner received an acceptable standard of treatment - and whether or not the prisoners complaint is worthy of formal investigation?
4) Given that the discouraged medication policy appears to be incompatible with doctors medical ethics; given that the policy also appears to be incompatible with prisoners entitlement to an equivalent standard of medical care to that in the community; given that the HDC (through its investigative role) is responsible for ensuring that doctors and nurses deliver clinically appropriate medical treatment to patients; what does this say about the integrity of HDC investigations into complaints by prisoners about their medical treatment? 5) Does the HDC still endorse or condone this discouraged medication policy?
Roger Brooking, P.O.Box 29-075, Ngaio, Wellington
You might also like
- Medical Errors and Adverse Events: Managing the Aftermath: Managing the AftermathFrom EverandMedical Errors and Adverse Events: Managing the Aftermath: Managing the AftermathNo ratings yet
- The Slim Book of Health Pearls: The Prevention of Medical ErrorsFrom EverandThe Slim Book of Health Pearls: The Prevention of Medical ErrorsNo ratings yet
- Mantilla-Neil, EssayDocument7 pagesMantilla-Neil, EssayJohn ManaloNo ratings yet
- Legal Aspects of Psychiatric Nursing: Linda Funk Barloon, MS, RN, APRN, CS, CPNP, BCDocument11 pagesLegal Aspects of Psychiatric Nursing: Linda Funk Barloon, MS, RN, APRN, CS, CPNP, BCpadmaNo ratings yet
- Responding To Patient Requests For Assisted Dying Guidance For DoctorsDocument12 pagesResponding To Patient Requests For Assisted Dying Guidance For DoctorsDavid BenbowNo ratings yet
- Letter To Ombudsman Re The HDC by Roger BrookingDocument2 pagesLetter To Ombudsman Re The HDC by Roger BrookingRoger BrookingNo ratings yet
- Psychiatry & The Law: Forensic Psychiatry Forensic PsychiatryDocument15 pagesPsychiatry & The Law: Forensic Psychiatry Forensic PsychiatryWinfrey PangestuNo ratings yet
- Best Interests DecisionDocument4 pagesBest Interests Decisiondknorsyafinaz pgadnanNo ratings yet
- Pharmacology For Canadian Health Care Practice, 3rd Canadian Edition: Chapter 03 - Legal and Ethical Considerations Chapter SummaryDocument4 pagesPharmacology For Canadian Health Care Practice, 3rd Canadian Edition: Chapter 03 - Legal and Ethical Considerations Chapter SummaryNadine MahadeoNo ratings yet
- The Cost of Conscience CQDocument14 pagesThe Cost of Conscience CQmiguel5628No ratings yet
- Principles of BioethicsDocument5 pagesPrinciples of Bioethicsshadrack mungutiNo ratings yet
- Eol 5 - Arihan Gupta 1Document5 pagesEol 5 - Arihan Gupta 1api-529369011No ratings yet
- Ethical Aspects of Withholding and Withdrawing Life Sustaining TreatmentDocument15 pagesEthical Aspects of Withholding and Withdrawing Life Sustaining TreatmentwakldNo ratings yet
- Dr. Abdirahman Moalim Hassan: Green Hope UniversityDocument29 pagesDr. Abdirahman Moalim Hassan: Green Hope UniversityabdirahmanNo ratings yet
- PCEP-PC Module 3 NotesDocument22 pagesPCEP-PC Module 3 NotesMan MedNo ratings yet
- Analysis On Medical Law and Ethics in India - Assignment 2Document6 pagesAnalysis On Medical Law and Ethics in India - Assignment 2Niyati SrivastavaNo ratings yet
- Case Study On Ethical Issue Faced by PhysiansDocument5 pagesCase Study On Ethical Issue Faced by PhysiansClash WolfNo ratings yet
- Affirmative November - DecemberDocument2 pagesAffirmative November - DecemberJamie ParkerNo ratings yet
- 2-3 Samillano-SamontegeronDocument19 pages2-3 Samillano-SamontegeronLance_Joshua_7907No ratings yet
- Medical Ethics and Case Studies ReportDocument29 pagesMedical Ethics and Case Studies ReportMARC B. DE PERALTANo ratings yet
- Report On Legal Medicine PowerpointDocument31 pagesReport On Legal Medicine PowerpointEdwin VillaNo ratings yet
- Contemporary-Ethico-Legal Issues FromDocument36 pagesContemporary-Ethico-Legal Issues FromtisuchiNo ratings yet
- Ethics in OBGDocument36 pagesEthics in OBGManinder SekhonNo ratings yet
- 00-3 Legal PrescriptionDocument1 page00-3 Legal PrescriptionMarc Angelo Villalobos BantugNo ratings yet
- Letter To The Editor - Substance AbuseDocument2 pagesLetter To The Editor - Substance Abuserapannika100% (2)
- LivingWill TexasDocument3 pagesLivingWill TexasAmesNo ratings yet
- Principles of BioethicsDocument7 pagesPrinciples of BioethicsNuronnisah Kalinggalan PadjiriNo ratings yet
- Whether or Not Euthanasia Is Being Practised in The CommunityDocument9 pagesWhether or Not Euthanasia Is Being Practised in The Communitygpy297No ratings yet
- The Ethics of AddictionDocument20 pagesThe Ethics of AddictionNicolas MartinNo ratings yet
- Dashboard Library Study Plans Qbank Analysis Account Help Center & Legal InfoDocument42 pagesDashboard Library Study Plans Qbank Analysis Account Help Center & Legal InfoGauri SurnerNo ratings yet
- CovertMedication-GoodPracticeGuide 2022Document25 pagesCovertMedication-GoodPracticeGuide 2022AMBNo ratings yet
- (Law of Evidence) Expert OpinionDocument12 pages(Law of Evidence) Expert OpinionKhairul Idzwan100% (3)
- Health Law Set 1Document15 pagesHealth Law Set 1Vijay Srinivas KukkalaNo ratings yet
- Module 15: Contemporary Issues in PsychopathologyDocument5 pagesModule 15: Contemporary Issues in PsychopathologyLiz EvermoreNo ratings yet
- Legal MedicineDocument9 pagesLegal MedicineEdwin VillaNo ratings yet
- Legal Aspects of NursingDocument9 pagesLegal Aspects of NursingleslyjoyNo ratings yet
- DNR and Medical FutilityDocument13 pagesDNR and Medical Futilityapi-216057141No ratings yet
- Argument Essay COM101KOODocument4 pagesArgument Essay COM101KOOMaliha MoriumNo ratings yet
- Ethics in Midwifery PracticeDocument42 pagesEthics in Midwifery PracticeDivya Grace95% (19)
- Forensic PsychiatryDocument56 pagesForensic PsychiatryRahelAdmasuNo ratings yet
- Consent Guidance Revised Jan2018Document12 pagesConsent Guidance Revised Jan2018mazin kenziNo ratings yet
- Medical EthicsDocument6 pagesMedical Ethicsdobuol gorNo ratings yet
- Principles of BioethicsDocument80 pagesPrinciples of BioethicsYashmine Castrence0% (1)
- Medical Ethics by The BookDocument4 pagesMedical Ethics by The BookFatima NaeemNo ratings yet
- The Underlying Principles of Ethical Patient CareDocument7 pagesThe Underlying Principles of Ethical Patient CareGulshanNo ratings yet
- The Principle of Non MaleficenceDocument1 pageThe Principle of Non MaleficenceClaire Esic PontanarNo ratings yet
- CPR Nurse LawDocument6 pagesCPR Nurse LawIpar DayNo ratings yet
- CONSENSUS-PAPER-PRISON-PSYCHIATRY Final Version (54175)Document5 pagesCONSENSUS-PAPER-PRISON-PSYCHIATRY Final Version (54175)dehamericoNo ratings yet
- Medical Ethics and Case Studies Part1Document12 pagesMedical Ethics and Case Studies Part1denver cayagaNo ratings yet
- Forensic PsychiatryDocument56 pagesForensic PsychiatryJeffrey RamosNo ratings yet
- Lymberis-Ethical and LegalDocument10 pagesLymberis-Ethical and LegalEmily PanganibanNo ratings yet
- Doctor and The LawDocument24 pagesDoctor and The LawEffah FestusNo ratings yet
- Health LawDocument9 pagesHealth LawayishaNo ratings yet
- Etika Hub DR - PasienDocument27 pagesEtika Hub DR - PasienJamali GagahNo ratings yet
- Deborah Bowman, John Spicer, Rehana Iqbal-Informed Consent - A Primer For Clinical Practice-Cambridge University Press (2012)Document107 pagesDeborah Bowman, John Spicer, Rehana Iqbal-Informed Consent - A Primer For Clinical Practice-Cambridge University Press (2012)Meliani R'KyMeyNo ratings yet
- Ethical Principles of PharmacistDocument6 pagesEthical Principles of Pharmacistvarmapharm100% (1)
- Health Law First DraftDocument10 pagesHealth Law First DraftNAYAN SINGHNo ratings yet
- Final Medical NegligenceDocument74 pagesFinal Medical NegligenceAabritti PaudyalNo ratings yet
- Unit 7 Mental Ill-Health Reading 2019-20Document25 pagesUnit 7 Mental Ill-Health Reading 2019-20Helen VlotomasNo ratings yet
- Debate: Euthanasia Posture: AgainstDocument5 pagesDebate: Euthanasia Posture: Againstapi-292542297No ratings yet
- Ian Callinan ReportDocument148 pagesIan Callinan ReportRoger BrookingNo ratings yet
- Prof Phil Brindid Psychiatric Assessment of David BainDocument5 pagesProf Phil Brindid Psychiatric Assessment of David BainRoger BrookingNo ratings yet
- Familicide: Long Term AntecedentsDocument9 pagesFamilicide: Long Term AntecedentsRoger Brooking100% (1)
- Joe Karam Correspondance With Amy AdamsDocument55 pagesJoe Karam Correspondance With Amy AdamsRoger BrookingNo ratings yet
- Kim Workman - Submission On The Clean Slate Act 2004Document25 pagesKim Workman - Submission On The Clean Slate Act 2004Roger BrookingNo ratings yet
- Familicide SuicideDocument14 pagesFamilicide SuicideRoger Brooking100% (2)
- Familicide Why Children Are KilledDocument7 pagesFamilicide Why Children Are KilledRoger BrookingNo ratings yet
- Ian Binnie Report Appendices - Tab F To Tab JDocument233 pagesIan Binnie Report Appendices - Tab F To Tab JRoger BrookingNo ratings yet
- Joe Karam Media Statement 5 August 2016Document5 pagesJoe Karam Media Statement 5 August 2016Roger Brooking100% (1)
- Kenneth Palmer's Letter About Ian Binnie's ReportDocument1 pageKenneth Palmer's Letter About Ian Binnie's ReportRoger BrookingNo ratings yet
- Ian Binnie Report Appendices - Tab A To Tab EDocument143 pagesIan Binnie Report Appendices - Tab A To Tab ERoger BrookingNo ratings yet
- Dean Cottle's Statement About Laniet BainDocument3 pagesDean Cottle's Statement About Laniet BainRoger Brooking0% (1)
- New Zealand IPCA - Police Failure To Prosecute - Double StandardsDocument6 pagesNew Zealand IPCA - Police Failure To Prosecute - Double StandardsRoger BrookingNo ratings yet
- Kenneth Palmer Letter To EditorDocument2 pagesKenneth Palmer Letter To EditorRoger BrookingNo ratings yet
- Jai Davis - Inspector's Report Executive SummaryDocument6 pagesJai Davis - Inspector's Report Executive SummaryRoger BrookingNo ratings yet
- IPCA - Slow Investigation Into Death of Jai DavisDocument4 pagesIPCA - Slow Investigation Into Death of Jai DavisRoger BrookingNo ratings yet
- IPCA - Police Emails Re Jai DavisDocument9 pagesIPCA - Police Emails Re Jai DavisRoger BrookingNo ratings yet
- IPCA - Police Failure To Prosecute - Evidential TestDocument7 pagesIPCA - Police Failure To Prosecute - Evidential TestRoger BrookingNo ratings yet
- Litmus ReportDocument99 pagesLitmus ReportRoger BrookingNo ratings yet
- New Zealand IPCA - Police Failure To Prosecute - Double StandardsDocument6 pagesNew Zealand IPCA - Police Failure To Prosecute - Double StandardsRoger BrookingNo ratings yet
- Ombudsman's Special Investigation Into Management of Prisoner Arthur Taylor in Auckland Prison, New ZealandDocument34 pagesOmbudsman's Special Investigation Into Management of Prisoner Arthur Taylor in Auckland Prison, New ZealandRoger BrookingNo ratings yet
- Albuterol-Budesonide Fixed-Dose Combination Rescue Inhaler For AsthmaDocument13 pagesAlbuterol-Budesonide Fixed-Dose Combination Rescue Inhaler For AsthmaLydia ? Raposo MartinezNo ratings yet
- Green and White Corporate Technology Pitch Deck PresentationDocument13 pagesGreen and White Corporate Technology Pitch Deck PresentationPradeep PandeyNo ratings yet
- ED Report FinalDocument15 pagesED Report FinalA B M MoshiuddullahNo ratings yet
- Evaluation of Anti-Inflammatory Effect of Ashwagandha: A Preliminary Study in VitroDocument3 pagesEvaluation of Anti-Inflammatory Effect of Ashwagandha: A Preliminary Study in VitroAmmar Ali KhanNo ratings yet
- IRR Ra 9165 and AmendmentDocument35 pagesIRR Ra 9165 and AmendmentThessaloe B. FernandezNo ratings yet
- Allen Chao's Business StrategyDocument2 pagesAllen Chao's Business StrategyNapoleon Naufal Aziz100% (1)
- CS528-Medication Care Plan - ExampleDocument2 pagesCS528-Medication Care Plan - ExamplehdbundoNo ratings yet
- Project On Employees RetentionDocument48 pagesProject On Employees Retentionyogender83% (53)
- DownloadDocument27 pagesDownloadKHAIRUNNISA FADILANo ratings yet
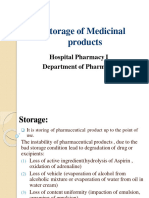
- Storage of MP (21-22)Document24 pagesStorage of MP (21-22)ranemabdo22No ratings yet
- Pharmacy Law - Terminology & PrinciplesDocument18 pagesPharmacy Law - Terminology & PrinciplesHIND MOHAMEDNo ratings yet
- Introductory Pharmacy Practice Experience ManualDocument26 pagesIntroductory Pharmacy Practice Experience ManualsarojiniNo ratings yet
- Death by 1000 Lawsuits: The Public Litigation in Response To The Opioid Crisis Will Mirror The Global Tobacco Settlement of The 1990s by Paul L. KeenanDocument26 pagesDeath by 1000 Lawsuits: The Public Litigation in Response To The Opioid Crisis Will Mirror The Global Tobacco Settlement of The 1990s by Paul L. KeenanNew England Law ReviewNo ratings yet
- Class Notes 6 Quality Assurance in The Pharmaceutical Supply ChainDocument11 pagesClass Notes 6 Quality Assurance in The Pharmaceutical Supply ChainNdatasha PambweNo ratings yet
- FPGEE Blueprint: Area 1 - Basic Biomedical Sciences - 21%Document12 pagesFPGEE Blueprint: Area 1 - Basic Biomedical Sciences - 21%Raafat A. Issaq100% (2)
- Mmas+kuesioner Kepatuhan Minum ObatDocument9 pagesMmas+kuesioner Kepatuhan Minum Obatdesti purnama sariNo ratings yet
- ISMP List of High-Alert Medications: in Acute Care SettingsDocument1 pageISMP List of High-Alert Medications: in Acute Care SettingsSafitri W100% (1)
- Gabapentin - The Most Dangerous Drug in America? - DentistryIQDocument11 pagesGabapentin - The Most Dangerous Drug in America? - DentistryIQdo leeNo ratings yet
- Telling A Stellar Story: Published by BS CentralDocument6 pagesTelling A Stellar Story: Published by BS CentralBS Central, Inc. "The Buzz"No ratings yet
- Biniam 2019 CVDocument5 pagesBiniam 2019 CVBiniam Abeelo TadeleNo ratings yet
- The Healing Power of Chinese Herbs and Medicinal RecipesDocument847 pagesThe Healing Power of Chinese Herbs and Medicinal RecipesCARLOS SMITH NINO QUINONEZ89% (9)
- Comhealth Lec 1Document24 pagesComhealth Lec 1Kiana SanchezNo ratings yet
- Chapter 1 Chapter 1 - Definition History Present Status and Scope of Pharmacognosy Notes PDF D.Pharma 1st Year Notes NoteskartsDocument4 pagesChapter 1 Chapter 1 - Definition History Present Status and Scope of Pharmacognosy Notes PDF D.Pharma 1st Year Notes NoteskartsManish BudhrajaNo ratings yet
- Taj Pharma Brochure API 2017Document6 pagesTaj Pharma Brochure API 2017Anonymous BVD7IKfNo ratings yet
- Current Situation On Nutrient-Drug Interactions in Health Care PracticeDocument3 pagesCurrent Situation On Nutrient-Drug Interactions in Health Care PracticeRijantono Franciscus MariaNo ratings yet
- 1534 - Prescription Audit Guidelines16042021Document52 pages1534 - Prescription Audit Guidelines16042021Rajender SinghNo ratings yet
- Alphabetic List of Iran Pharmaceutical CompaniesDocument11 pagesAlphabetic List of Iran Pharmaceutical Companiesvarunfdoxx50% (6)
- 3911 Human EnUserGuide Neurobion 1.3.3.2 English LeafletDocument1 page3911 Human EnUserGuide Neurobion 1.3.3.2 English LeafletNadia AfifahNo ratings yet
- Dr. BM RAO - Nitrosamine Impurities and NDSRIs UpdatesDocument5 pagesDr. BM RAO - Nitrosamine Impurities and NDSRIs UpdatesVinay PatelNo ratings yet
- Pharma Corner - Sample Study MaterilasDocument17 pagesPharma Corner - Sample Study MaterilasAmit PatelNo ratings yet