Professional Documents
Culture Documents
Content of A Complete Routine Second Trimester Obstetrical Ultrasound Examination and Report
Uploaded by
bel4ronaldoeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Content of A Complete Routine Second Trimester Obstetrical Ultrasound Examination and Report
Uploaded by
bel4ronaldoeCopyright:
Available Formats
SOGC CLINICAL PRACTICE GUIDELINE
SOGC CLINICAL PRACTICE GUIDELINE No. 223, March 2009 (Replaces No. 103, May 2001)
Content of a Complete Routine Second Trimester Obstetrical Ultrasound Examination and Report
This clinical practice guideline has been reviewed by the Diagnostic Imaging Committee and approved by the Executive and Council of the Society of Obstetricians and Gynaecologists of Canada. The Society of Obstetricians and Gynaecologists of Canada acknowledges advisory input from the Canadian Association of Radiologists pertaining to imaging guidelines in the creation of this document. PRINCIPAL AUTHORS Yvonne Cargill, MD, Ottawa ON Lucie Morin, MD, Montreal QC DIAGNOSTIC IMAGING COMMITTEE Lucie Morin (Chair), MD, Montreal QC Stephen Bly, PhD, Ottawa ON Kimberly Butt, MD, Fredericton NB Yvonne Cargill, MD, Ottawa ON Nanette Denis, RDMS, CRGS, Saskatoon SK Robert Gagnon, MD, Montreal QC Marja Anne Hietala-Coyle, RN, Halifax NS Kenneth Lim, MD, Vancouver BC Annie Ouellet, MD, Sherbrooke QC Marie-Hlne Racicot, MD, Montreal QC Shia Salem, MD, Canadian Association of Radiologists, Toronto ON Disclosure statements have been received from all members of the committee. Screening were reviewed. PubMed and the Cochrane Database were searched using the words routine second trimester obstetrical ultrasound. Values: The evidence was evaluated using the guidelines developed by the Canadian Task Force on Preventive Health Care. Benefits, Harms, and Costs: A routine complete second trimester ultrasound between 18 and 22 weeks and a complete ultrasound report will provide the best opportunity to diagnose fetal anomalies and to assist in the management of prenatal care. It will also reduce the number of ultrasound examinations done during the second trimester for completion of fetal anatomy survey. The costs are those involved with the performance of obstetrical ultrasound. Validation: This is a revision of previous guidelines; information from other consensus reviews from medical publications has been used. Sponsors: The Society of Obstetricians and Gynaecologists of Canada. Recommendations 1. Pregnant women should be offered a routine second trimester ultrasound between 18 and 22 weeks gestation. (II-2B) 2. Second trimester ultrasound should screen for the number of fetuses, the gestational age, and the location of the placenta. (II-1A) 3. Second trimester ultrasound should screen for fetal anomalies. (II-2B) J Obstet Gynaecol Can 2009;31(3):272275
SECOND TRIMESTER ULTRASOUND
Abstract
Objective: To review the benefits of and requirements for a complete second trimester ultrasound and the documentation needed. Outcomes: A complete second trimester ultrasound provides information about the number of fetuses, the gestational age, the location of the placenta, and fetal and maternal anatomy. Evidence: In the production of this document, the American Institute of Ultrasound in Medicines Practice Guideline for the Performance of Obstetric Ultrasound Examinations, the American College of Obstetricians and Gynecologists practice bulletin, Ultrasound in Pregnancy, and the Royal College of Obstetricians and Gynaecologists Working Party Report, Ultrasound Key Words: Routine second trimester ultrasound, ultrasound report
n ultrasound scan performed between 18 and 22 weeks gestation provides the pregnant woman and her care provider with information about multiple aspects of her pregnancy.14 The obstetrical ultrasound will inform them of and/or confirm the number of fetuses present, the gestational age, and the location of the placenta. It will present an opportunity to diagnose congenital anomalies and/or to detect soft markers of aneuploidy and to identify maternal pelvic pathology.
The occurrence of twins undiagnosed at delivery is extremely rare when women have received a second trimester ultrasound, and the likelihood of postdates induction and intrauterine growth restriction significantly decreases.1 In the last two decades, the infant death rate from congenital
This document reflects emerging clinical and scientific advances on the date issued and is subject to change. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed. Local institutions can dictate amendments to these opinions. They should be well documented if modified at the local level. None of these contents may be reproduced in any form without prior written permission of the SOGC.
272
l MARCH JOGC MARS 2009
Content of a Complete Routine Second Trimester Obstetrical Ultrasound Examination and Report
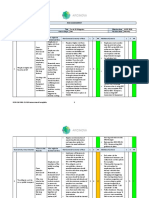
Table 1. Content of a Complete Obstetrical Ultrasound Report
Category Patient demographic information Required Information
Patient name, second patient identifier (birth date, hospital identifier, health insurance number) Indication for consultation Requesting physician/caregiver (preferably with contact information) Starting date of last normal menstrual period (LNMP) Examination date Date of written report Name of interpreting physician Presence of cardiac activity for each fetus
If multiple gestation: chorionicity and amnionicity should be reported Should be reported all in millimetres or in centimetres along with equivalent estimated gestational age for:
Number of fetuses and indications of life Biometry
Biparietal diameter Head circumference Abdominal circumference Femur length
Should be reported in millimetres if abnormal
Nuchal fold Cisterna magna Cerebellar diameter
Fetal anatomy
Lateral ventricle width Should be reported as: normal OR abnormal (with details) OR not seen, with explanation
Should be reported for:
Cranium Cerebral ventricles, cavum septi pellucidi, the midline falx, the choroid plexus Posterior fossa: cisterna magna, cerebellum Face: orbits, lips Spine Chest Cardiac four-chamber view Cardiac outflow tracts Heart axis Cardiac situs Stomach Bowel Kidneys Bladder Abdominal cord insertion Number of cord vessels Upper extremities and presence of hands
Amniotic fluid amount Placenta Maternal anatomy uterus, ovaries, cervix, bladder
Lower extremities and presence of feet Should be reported as: normal OR increased OR decreased OR absent Position should be reported as well as relationship to the cervical os Should be reported as: normal OR abnormal with details OR not seen
MARCH JOGC MARS 2009 l
273
SOGC CLINICAL PRACTICE GUIDELINE
Table 2. Key to evidence statements and grading of recommendations, using the ranking of the Canadian Task Force on Preventive Health Care
Quality of Evidence Assessment* I: Evidence obtained from at least one properly randomized controlled trial Classification of Recommendations A. There is good evidence to recommend the clinical preventive action B. There is fair evidence to recommend the clinical preventive action C. The existing evidence is conflicting and does not allow to make a recommendation for or against use of the clinical preventive action; however, other factors may influence decision-making D. There is fair evidence to recommend against the clinical preventive action E. There is good evidence to recommend against the clinical preventive action L. There is insufficient evidence (in quantity or quality) to make a recommendation; however, other factors may influence decision-making
II-1: Evidence from well-designed controlled trials without randomization II-2: Evidence from well-designed cohort (prospective or retrospective) or case-control studies, preferably from more than one centre or research group II-3: Evidence obtained from comparisons between times or places with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of treatment with penicillin in the 1940s) could also be included in this category III: Opinions of respected authorities, based on clinical experience, descriptive studies, or reports of expert committees
*The quality of evidence reported in these guidelines has been adapted from The Evaluation of Evidence criteria described in the Canadian Task Force on Preventive Health Care.11 Recommendations included in these guidelines have been adapted from the Classification of Recommendations criteria described in the The Canadian Task Force on Preventive Health Care.11
anomalies has decreased by 50% in infants born after 24 weeks.5 This is likely at least partially related to early diagnosis of congenital anomalies leading to either pregnancy termination or better neonatal care. Second trimester diagnosis of congenital anomalies also provides the opportunity for fetal therapy. The literature includes descriptions of anatomical surveys being performed before 18 weeks6 but other studies have repeatedly shown that more anomalies are diagnosed if the scan is done after 18 weeks.1,2 A study done by Lantz and Chisolm7 found that in normal sized and in overweight patients, a fetal anatomy survey for the detection of congenital anomalies was more likely to be incomplete if performed before 18 weeks than if performed at a later gestational age. In underweight patients, no difference was found. The Royal College of Obstetricians and Gynaecologists recommends that the second trimester fetal anatomical scan be performed between 20 and 23 weeks.8 We recommend that the second trimester ultrasound be performed after 18 weeks and before 22 weeks gestation.9 This will allow pregnancy options if an anomaly is diagnosed and avoid the added cost and unnecessary ultrasound exposure of a repeat scan related to incomplete fetal anatomy survey. This is a growing concern, as patients are increasingly likely to have a high BMI. When an ultrasound is performed at 18 to 22 weeks gestation, the maternal organs that should be screened are the cervix, uterus, and adnexa. Any abnormality of these structures should be documented.
274 l MARCH JOGC MARS 2009
The number of fetuses and the presence of cardiac activity should be recorded. If a multiple gestation is diagnosed, the chorionicity and amnionicity should be assessed and documented. The fetal biometric measurements should include at least the following: biparietal diameter, head circumference, abdominal circumference, and femur length. Absolute biometric measurements with their estimated gestational age should be documented and reported. A composite estimated gestational age should also be reported, taking into consideration measurement errors arising from abnormal fetal body parts. Moreover, the gestational age/size should be interpreted in correlation with any previous obstetrical ultrasound if available. This will allow the care provider to confirm if fetal growth has been appropriate. Due date should not be adjusted if it has been established by an earlier ultrasound.
Fetal Anatomy Survey to Be Performed During a Complete Obstetrical Routine Second Trimester Ultrasound
The standard fetal brain anatomical survey should include an assessment and documentation of the following anatomical landmarks: the shape of the fetal skull, the cavum septi pellucidi, the midline falx, the choroid plexus, the lateral cerebral ventricles, the cerebellum, the cisterna magna, and the nuchal fold. The face should be scanned to assess and document the orbits and lips. In the thorax, the heart and lungs should be examined. Examination of the fetal heart includes its relationship with the chest (axis, size, and position) as well as the assessment
Content of a Complete Routine Second Trimester Obstetrical Ultrasound Examination and Report
of the four chamber view and the relationships of the outflow tracts. The fetal cardiac motion should be observed and a fetal heart rate recorded. The lungs should be examined for their echogenicity. In the fetal abdomen, the anatomical survey should include the position, presence, and situs of the stomach, and visualization of the bowel, bladder, kidneys, cord insertion, and number of cord vessels. The fetal spine should be viewed throughout its length in sagittal, coronal, and transverse planes if possible. The skin line should be seen away from the uterine wall. This cannot always be documented with still images. An attempt should be made to assess the fetal genitalia. All four limbs to the level of the hands and feet should be visualized, and the presence of hands and feet should be noted. Subjective assessment of bone size, shape, and density should be done. This cannot always be documented with still images. The placenta should be examined for position, appearance, and presence or absence of abnormalities. The placental location and its relationship to the internal cervical os should be assessed and documented. A qualitative assessment of the amniotic fluid volume should be made. It should be reported as normal, increased, decreased, or absent. Table 1 shows the recommended content of the report, but other information may be provided in such consultations. The ultrasound report should include all ultrasound information necessary for appropriate management of the pregnancy. It needs to include the date the scan was performed and the composite gestational age based on fetal biometric measurements. The number and size of fetuses and the measurements obtained to determine them should be noted. If a structure was not seen, this should be reported, along with the reason it was not seen. If fetal or maternal abnormalities are reported, a differential diagnosis and, when appropriate, a recommendation for further investigation should be provided. The report should comment on any significant technical difficulty of the examination. The final report should be easy to read. It is acknowledged that even in the best of hands and circumstances, the 1822 week scan has limitations and cannot detect all fetal and maternal abnormalities.10 Any significant fetal or maternal abnormalities need to be reported promptly to the caregiver. The communication should be recorded in the patients file. An ultrasound report summary should provide: Estimation of gestational age according to ultrasound if this is the first obstetrical ultrasound, estimation of gestational age according to last menstrual period dates, and the expected date of confinement Appropriateness of the biometry, size, growth, and estimated gestational age
Summary of findings Differential diagnosis if indicated Recommendations for further investigations and
referral for tertiary centre assessment when necessary. Recommendations The evidence was evaluated using the guidelines developed by the Canadian Task Force on Preventive Health Care (Table 2). 1. Pregnant women should be offered a routine second trimester ultrasound between 18 and 22 weeks gestation. (II-2B) 2. Second trimester ultrasound should screen for the number of fetuses, the gestational age, and the location of the placenta. (II-1A) 3. Second trimester ultrasound should screen for fetal anomalies. (II-2B)
REFERENCES
1. Ecker JL, Green MF. Indications for diagnostic obstetrical ultrasound examination. UpToDate [web site] Version 15.1, December 2006. 2. Neilson JP. Ultrasound for fetal assessment in early pregnancy (Review). Cochrane Database Syst Rev 1998;Issue 4. Art. No.: CD000182. DOI: 10.1002/14651858.CD000182. 3. ACOG Committee on Practice Bulletins. ACOG Practice Bulletin, No. 58, October 2008. Ultrasonography in pregnancy. Obstet Gynecol 2004;104(6):144958. 4. Seeds JW. The routine screening obstetrical ultrasound examination. Clin Obstet Gynecol 1996;39(4):81430. 5. Liu S, Joseph KS, Wen SW. Trends in fetal and infant deaths caused by congenital anomalies. Semin Perinatol 2002;26(4):26876. 6. Souka AP, Pilalis A, Kavalakis I, Antsaklis P, Papantoniou N, Mesogitis S, et al. Screening for major structural abnormalities at the 11- to 14- week ultrasound scan. Am J Obstet Gynecol 2006;194(2):3936. 7. Lantz ME, Chisolm CA. The preferred timing of second-trimester sonography based on maternal body mass index. J Ultrasound Med 2004;23(8):101922. 8. Whittle MJ, Chitty LS, Neilson JP, Shirley, Smith IM, Ville YG, et al.; National Working Party, Royal College of Obstetricians and Gynaecologists. Ultrasound Screening. Supplement to Ultrasound Screening for Fetal Abnormalities. Royal College of Obstetricians and Gynaecologists Working Party Report. July 2000. Available at: http://www.rcog.org.uk/index.asp?PageID=1185. Accessed November 26, 2008. 9. Tjepkema M. Adult obesity in Canada: measured height and weight. Statistics Canada, 82620-MWE/2005001. 10. Ewigman BG, Crane JP, Frigoletto FD, LeFevre ML, Bain RP, McNellis D. Effect of prenatal ultrasound screening on perinatal outcome. RADIUS Study Group. N Engl J Med 1993;329(12):8217. 11. Woolf SH, Battista RN, Angerson GM, Logan AG, Eel W. Canadian Task Force on Preventive Health Care. New grades for recommendations from the Canadian Task Force on Preventive Health Care. CMAJ 2003;169(3):2078.
MARCH JOGC MARS 2009 l
275
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Medicine 2Document1 pageMedicine 2aasi121No ratings yet
- Doi:10.6323/Jocrp.2010.26.3.1: Meaning-Centered Group Psychotherapy-Introduction and CommentsDocument12 pagesDoi:10.6323/Jocrp.2010.26.3.1: Meaning-Centered Group Psychotherapy-Introduction and CommentsJoan ChuNo ratings yet
- The Clinician Role in Health Care Delivery and InnovationDocument21 pagesThe Clinician Role in Health Care Delivery and InnovationLuis Henrique SalesNo ratings yet
- Medical Lay TermsDocument35 pagesMedical Lay TermsXuMengNo ratings yet
- Non CAT - Verbal ReasoningDocument9 pagesNon CAT - Verbal ReasoningPadmabati Roy ChoudhuryNo ratings yet
- HOME-VISIT Sir DeoDocument26 pagesHOME-VISIT Sir DeoWilma Nierva BeraldeNo ratings yet
- Sob Physician Services 20120401 Web VersionDocument874 pagesSob Physician Services 20120401 Web Versionpop99999No ratings yet
- Iio Ow Waa B Bo Oaarrd D O Off N Nu Urrssiin NG GDocument34 pagesIio Ow Waa B Bo Oaarrd D O Off N Nu Urrssiin NG GWichipirichiNo ratings yet
- Uterine Leiomyoma: Case ReportDocument16 pagesUterine Leiomyoma: Case Reportangie riveraNo ratings yet
- RA-EHS-047-E2 - Covid-19 Site Risk Assessment 002Document16 pagesRA-EHS-047-E2 - Covid-19 Site Risk Assessment 002Samsu RizalNo ratings yet
- Pregnancy ExaminationDocument11 pagesPregnancy ExaminationLisa KnappNo ratings yet
- NCD High-Risk Assessment (Community Case Finding Form) NCD High-Risk Assessment (Community Case Finding Form)Document1 pageNCD High-Risk Assessment (Community Case Finding Form) NCD High-Risk Assessment (Community Case Finding Form)Gen GenNo ratings yet
- Ese - Arbina JajiDocument6 pagesEse - Arbina JajiShenasiJajiNo ratings yet
- Chapter 10: Elimination Test Bank: 1. A. B. C. D. Ans: ADocument6 pagesChapter 10: Elimination Test Bank: 1. A. B. C. D. Ans: AMary SingletonNo ratings yet
- Farah Al Souheil, Pharmd, RPH Lebanese International University, SopDocument36 pagesFarah Al Souheil, Pharmd, RPH Lebanese International University, Sopعلي عويد جابر محمدNo ratings yet
- Group 1,2,4 QuizDocument221 pagesGroup 1,2,4 QuizPaulNo ratings yet
- The Impact of Nutrition Education On Knowledge, Attitude, and Practiceregarding Iron Deficiency Anemia Among Female Adolescent Studentsin JordanDocument7 pagesThe Impact of Nutrition Education On Knowledge, Attitude, and Practiceregarding Iron Deficiency Anemia Among Female Adolescent Studentsin JordanAppierien 4No ratings yet
- Margaret Sanger PresentationDocument4 pagesMargaret Sanger PresentationCarly Faith VanderkolkNo ratings yet
- Adjusted ContractDocument19 pagesAdjusted Contractmarsen100% (1)
- DineshPonraj 1808165 - 05 00 - 1Document4 pagesDineshPonraj 1808165 - 05 00 - 1revanth kumarNo ratings yet
- CMN 463 Lecture 2 Insurance Medicare and MedicaidDocument18 pagesCMN 463 Lecture 2 Insurance Medicare and MedicaidCarlos GuiterizNo ratings yet
- Network Lists in UAE - Mar 2015Document93 pagesNetwork Lists in UAE - Mar 2015Kamran KhanNo ratings yet
- Who BG PDFDocument21 pagesWho BG PDFAastha AroraNo ratings yet
- Basics of Medical Billing & CodingDocument86 pagesBasics of Medical Billing & CodingRic Sánchez100% (3)
- Department of Health - Knock Out Tigdas 2007 - 2011-10-19Document3 pagesDepartment of Health - Knock Out Tigdas 2007 - 2011-10-19daryl ann dep-asNo ratings yet
- Test Bank For Lemone and Burkes Medical Surgical Nursing 7th by BauldoffDocument5 pagesTest Bank For Lemone and Burkes Medical Surgical Nursing 7th by Bauldoffcosimalocu68xb1No ratings yet
- Spot 2023 Brochure - FinalDocument3 pagesSpot 2023 Brochure - FinalMontesqieu SilalahiNo ratings yet
- High-Risk Non-Small Cell Lung Cancer Treated With Active Scanning Proton Beam Radiation Therapy and ImmunotherapyDocument9 pagesHigh-Risk Non-Small Cell Lung Cancer Treated With Active Scanning Proton Beam Radiation Therapy and ImmunotherapyRaul Matute MartinNo ratings yet
- Oral Biopsy: Oral Pathologist's Perspective: Review ArticleDocument7 pagesOral Biopsy: Oral Pathologist's Perspective: Review ArticleRafa LopezNo ratings yet
- EMAH Patient Information Leaflet v3Document5 pagesEMAH Patient Information Leaflet v3SonaliNo ratings yet