Professional Documents
Culture Documents
Dental Assistant
Uploaded by
Almehey NaderCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dental Assistant
Uploaded by
Almehey NaderCopyright:
Available Formats
Knowledge for Clinical Practice
WWW.DENTALLEARNING.NET
A PEER-REVIEWED PUBLICATION
DENTAL LEARNING
DentalLearning.net is an ADA CERP Recognized Provider. ADA
CERP is a service of the American Dental Association to assist
dental professionals in identifying quality providers of continu-
ing dental education. ADA CERP does not approve or endorse
individual courses or instructors, nor does it imply acceptance
of credit hours by boards of dentistry. DentalLearning.net des-
ignates this activity for 3 continuing education credits.
Approved PACE Program Provider FAGD/MAGD Credit Approval
does not imply acceptance by a state or provincial board of
dentistry or AGD endorsement. (2/1/2012) to (1/31/2016)
AGD Code: 148
Instrument Processing
for Infection Prevention
Fiona M. Collins, BDS, MBA, MA
Inside earn
3 CE Credits
Written for dentists,
hygienists and assistants
DENTAL LEARNING
2
www.dentallearning.net
President
ALDO EAGLE
CE Content Manager
MONIQUE TONNESSEN
Creative Director
MICHAEL HUBERT
Art Director
MICHAEL MOLFETTO
Copyright 2012 by Dental Learning, LLC. No part of this publication
may be reproduced or transmitted in any form without prewritten
permission from the publisher.
10106 E. 79th St., Suite A, Tulsa, OK 74133
DENTAL LEARNING
EDUCATIONAL OBJECTIVES
The overall objective of this article is to provide the reader
with information on instrument processing. On completing
this article, the reader will be able to do the following:
1. Defne the elements of the chain of infection
2. Delineate and describe the differences in the processing
of critical, semicritical and noncritical instruments
3. Review the use of presoaks and cleaning of instruments
4. List and describe heat sterilization options and appropri-
ate sterilization packaging
5. Review the uses and purposes of chemical and biological
indicators
SPONSOR/PROVIDER: This is a Dental Learning, LLC continuing education activity. DESIGNATION STATEMENTS: Dental Learning, LLC is an ADA CERP recognized provider. ADA CERP is a service of the American Dental
Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by
boards of dentistry. Dental Learning LLC designates this activity for 3 CE credits. Dental Learning is also designated as an Approved PACE Program Provider by the Academy of General Dentistry. The formal continuing education
programs of this program provider are accepted by AGD for Fellowship, Mastership, and membership maintenance credit. Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement. The
current term of approval extends from 2/1/2012 - 1/31/2016. Provider ID: # 346890 Dental Learning, LLC is a Dental Board of California CE provider. The California Provider number is RP5062. This course meets the Dental Board
of Californias requirements for 3 units of continuing education. EDUCATIONAL METHODS: This course is a self-instructional journal and web activity. Information shared in this course is based on current information and evidence.
REGISTRATION: The cost of this CE course is $49.00 for 3 CE credits. PUBLICATION DATE: June, 2012. EXPIRATION DATE: May, 2015. REQUIREMENTS FOR SUCCESSFUL COMPLETION: To obtain 3 CE credits for this
educational activity, participants must pay the required fee, review the material, complete the course evaluation and obtain a score of at least 70%. AUTHENTICITY STATEMENT: The images in this course have not been altered.
SCIENTIFIC INTEGRITY STATEMENT: Information shared in this continuing education activity is developed from clinical research and represents the most current information available from evidenced-based dentistry. KNOWN
BENEFITS AND LIMITATIONS: Information in this continuing education activity is derived from data and information obtained from the reference section. EDUCATIONAL DISCLAIMER: Completing a single continuing education
course does not provide enough information to result in the participant being an expert in the feld related to the course topic. It is a combination of many educational courses and clinical experience that allows the participant to
develop skills and expertise. PROVIDER DISCLOSURE: Dental Learning does not have a leadership position or a commercial interest in any products that are mentioned in this article. No manufacturer or third party has had any
input into the development of course content. CE PLANNER DISCLOSURE: The planner of this course, Monique Tonnessen, does not have a leadership or commercial interest in any products that are mentioned in this article or
any other products or services discussed in this educational activity. She can be reached at mtonnessen@dentallearning.net. TARGET AUDIENCE: This course was written for dentists, dental hygienists, and assistants, from novice
to skilled. CANCELLATION/REFUND POLICY: Any participant who is not 100% satisfed with this course can request a full refund by contacting Dental Learning, LLC, in writing. Go Green, Go Online to www.dentallearning.net
take your course. Please direct all questions pertaining to Dental Learning, LLC or the administration of this course to mtonnessen@dentallearning.net.
ABOUT THE AUTHOR
Dr. Fiona M. Collins has authored and presented CE
courses to dental professionals and students in the
United States and internationally, and has been an ac-
tive consultant in the dental industry for several years.
She is a member of the American Dental Association
and the Organization for Safety, Asepsis and Preven-
tion, and has been a member of the British Dental As-
sociation, Dutch Dental Association, the International
Assocation for Dental Research and the Academy of
General Dentistry Foundation Strategy Board. Fiona
earned her dental degree from Glasgow University
and holds an MBA and MA from Boston University.
AUTHOR DISCLOSURE: Dr. Collins does not have
a leadership position or a commercial interest with
products and services discussed in this educational
activity. Dr. Collins can be reached at onacollins@
comcast.net
Safe and effective instrument processing is a key element of
the infection prevention cycle. This process must meet CDC
guidelines and OSHA requirements. The steps in instru-
ment processing include cleaning and sterilizing the instru-
ments. Their treatment depends on whether they are critical,
semicritical or noncritical. Critical and heat-resistant critical
instruments must be heat-sterilized, and handpieces must
be autoclaved. Prior to heat sterilization, instruments are
wrapped in appropriate FDA-cleared sterilization packaging,
which must include chemical indicators. Sterilization process-
es must be tested for sterility assurance and all sterilization
records maintained.
ABSTRACT
3
JUNE 2012
Introduction
I
nfection prevention is one of the key mandates in the
dental offce, required to protect clinicians and other
dental healthcare workers, patients, dental laboratory
personnel and, at a macrolevel, the community. In order to
prevent cross-contamination and disease transmission, the
chain of infection must be broken and a rigorous infec-
tion prevention protocol followed. The chain of infection
consists of fve elements: the presence of a pathogen at a
suffciently high concentration to cause disease, a source/
reservoir for that pathogen, a mode of transmission, an
entry portal in the host and a susceptible host. (Figure 1)
The tenet Do no harm is as applicable to the infection
prevention cycle as to any other aspect of clinical care. This
cycle consists of steps repeated sequentially during the day
prior to individual patient care, during patient care, im-
mediately following patient care and at the end of the day
after the last patient has been seen. Examples include the
use of protective barriers on clinical contact surfaces and
donning of personal protective equipment prior to patient
care, and the use of single-use disposables and instrument
cassettes during patient care. The focus of this article is on
instrument processing and the associated protocols that
must be followed.
Instrument Processing
Instrument processing is a key component of the infec-
tion prevention cycle, addressed in the Centers for Disease
Control and Prevention (CDC) 2003 guidelines for infec-
tion control in dental healthcare settings.
1
Although the
CDC later expanded the standard precautions in its isola-
tion guidelines for healthcare settings to address highly
transmissible diseases and specifc pathogens,
2
this did not
introduce any additional procedures with respect to instru-
ment processing in the dental setting.
3
The overall goal of instrument processing is to provide
sterile instruments for all patient care. Used instruments
are relevant to every element of the chain of infection.
They may contain a suffciently high level of a given patho-
gen to transmit disease, may serve as sources/reservoirs for
pathogens, offer multiple modes of transmission through
indirect and direct contact, are relevant to several portals
of entry and then only require a susceptible host to com-
plete the chain. Inadequately processed instruments place
patients, dental professionals and other dental healthcare
workers at risk.
Instrument processing involves a number of pre-
scribed, systematic steps that consider occupational
safety, types of instruments, required instrument process-
ing equipment and supplies, sterilization assurance, and
instrument inventory management. Instrument process-
ing should occur in a specifc location that is segregated
into dirty and clean areas, with instruments being
received in the dirty area and moving unidirectionally
Instrument Processing
for Infection Prevention
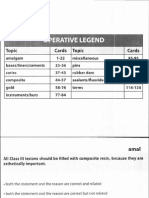
Figure 1. Chain of infection
The
Chain of
Infection
Reservoir
(source)
Pathogen at
a Suffcient
Level
Susceptible
Host
Portal of
Entry
Mode of
Transmission
DENTAL LEARNING
4
www.dentallearning.net
as they are processed. Designating dirty and clean areas
with a unidirectional fow avoids the risk of confus-
ing sterile and contaminated instruments, which could
result in recontamination of sterile instruments by newly
received contaminated instruments.
Safe Instrument Processing
Occupational safety must be ensured during instrument
processing to protect the operator from the risk of sharps
injuries and contact with contaminated instruments, spat-
ter and chemicals. Wearing heavy-duty utility gloves,
4
a
face mask and protective eyewear is required during opera-
tory cleanup and instrument processing. (Figure 2) Medical
and surgical gloves are never indicated; the person per-
forming cleanup and instrument processing must remove
and discard any medical or surgical gloves worn, perform
hand hygiene and don heavy-duty utility gloves to reduce
the risk of injury.
Sharps disposal
Disposing of sharps chairside, prior to transporting
instruments in closed cassettes/trays to the process-
ing area, reduces the risk of sharps injuries, which is
well-documented.
5
The sharps container must be color-
coded and puncture-resistant, have a rigid base and
walls, and be capable of being securely closed.
6
Capped
syringe needles, disposable all-in-one syringes, dispos-
able scalpels, blades, suture needles and broken glass
carpules should all be placed in the sharps container.
The container should be closed, sealed and disposed of
in accordance with the Occupational Safety and Health
Administration (OSHA), state, local and municipal
regulations. A tabletop device that melts and compresses
sharps into small, discrete sterile blocks is also avail-
able, after which the block may be disposed of in the
Figure 2. Use of heavy-duty utility gloves
Attributes of safe instrument processing
Use of heavy-duty utility gloves, masks and
protective eyewear
Disposal of sharps chairside
Use of a sharps container
Use of closed cassettes and instrument cages
Separate dirty and clean processing areas
Use of automated cleaning devices and
ultrasonic baths
Figure 3. Perforated cassette and sterilization cages for instruments
Instrument Processing for Infection Prevention
5
JUNE 2012
general trash. This device meets OSHA requirements in
many states. If you are considering using such a device,
frst consult state and local regulations to ensure that it
is permissible in your location.
Using closed cassettes - safety and transport
Using closed instrument cassettes contributes to the
safety of patient care and instrument processing. Contami-
nated instruments transported in closed cassettes to the
instrument processing area pose less risk of sharps injury
than do instruments transported while loose on a tray.
7
In
addition, closed cassettes can be placed in presoaks and
ultrasonic cleaners or washers/disinfectors prior to pack-
aging and sterilization, further reducing the risk of injury
and disease transmission. Closed cassettes used for instru-
ment processing must be perforated (Figure 3) if they are
being used in an autoclave, to allow steam to penetrate
the cassette and reach the instruments. Closed containers
and nonperforated closed cassettes must not be used for
autoclaving of instruments.
Using automated cleaning devices and ultrasonic baths
Using automated cleaning devices and ultrasonic baths
increases safety during instrument processing compared
with manual scrubbing.
Effective Instrument Processing
The sequential steps involved in instrument process-
ing must be properly executed each time.
1
These steps are:
1) disposal of sharps; 2) transportation of contaminated
instruments/cassettes/trays to the dirty receiving area of
the instrument processing location; 3) sorting of instru-
ments and devices; and 4) further processing of different
categories of instruments, for which the process involves
presoaking, cleaning, preparation/packaging, sterilization
and storage.
1,8
Figure 4. Sequential steps in effective instrument processing
Handpieces:
Remove burs,
wipe exterior of
handpiece.
Pre-sterilization
cleaning and
maintenance.
Follow
manufacturers
instructions.
Pouch handpieces
and autoclave
Remove damaged
instruments from
service
High-level
liquid disinfectant/
sterilant for
heat-sensitive
instruments.
Store in dry,
closed area
Dispose of sharps chairside; dispose of single-use items
Transport multiple use instruments to the
processing area
Segregate instruments by heat-resistant,
heat-sensitive and handpieces
Presoak instruments as required
(except handpieces)
Clean and inspect instruments; if visible debris,
clean again
Pouch/package critical and semi-critical
heat-resistant instruments
Heat-sterilize
Store, unopened, in a dry storage area until next use
DENTAL LEARNING
6
www.dentallearning.net
Disposal
The disposal of sharps must occur chairside. The
disposal of single-use items such as disposable air/water
syringes, bibs and bib holders, and saliva ejectors and the
disposal of waste may occur chairside or in the instru-
ment processing area. Regulated medical waste (hazardous
waste) must be discarded separately (or, if appropriate,
frst treated to render it nonhazardous), in keeping with
OSHA, state, local and municipal regulations.
Transport precautions
Impressions and other materials that will be trans-
ported to the dental laboratory must frst be disinfected ac-
cording to the material involved and following the manu-
facturers recommendations. Instructions regarding how
long a chemical disinfectant should be in contact with a set
impression should be carefully followed to avoid the risk
of altering the surface characteristics of the impression.
9
Sorting and Soaking
Contaminated cassettes/trays with instruments are
sorted on arrival in the instrument processing area, and
handpieces are removed for separate preparation accord-
ing to the material type and sterilization procedure (see
page 9). Instruments that will remain in the processing
area for a period of time prior to cleaning and steriliza-
tion should be presoaked in a presoak solution or spray to
help prevent debris from drying on the instruments, which
would make its removal more diffcult during cleaning.
10
If debris has already dried on by the time instruments
are received from the operatory, these instruments should
also be soaked before cleaning.
The closed perforated cassettes (or loose instruments)
should frst be placed in a soak container and then the
presoak solution or enzymatic spray added to fully coat
the instruments. If a foam product is being used, suff-
cient foam must be sprayed over the instruments to allow
for complete coverage after shrinkage of the foam. In
addition to preventing debris from drying on and wetting
(softening) debris that has already dried on, enzymatic
foam sprays begin dissolving blood, protein, carbohy-
drates, fat and other organic tissue, and help to break
down bioburden. Some foams that are marketed as non-
enzymatic have a near-neutral pH (slightly alkaline), and
are formulated to also break down bioburden. In general,
however, nonenzymatic foams and solutions do not help
to break down bioburden. If necessary, check with the
manufacturer. Foams are easier to use than solutions, are
less likely to result in spillage, and obviate the need to
store bulky solutions or dilute liquid concentrates. On the
other hand, liquid solutions do not dissipate. Solutions
and foams are now available that help to remove debris
Figure 5a. Presoaking in container with foam
Figure 5b. Pre-soak tub
Instrument Processing for Infection Prevention
7
JUNE 2012
and bioburden but with less wear on instruments.
Liquid solutions are available that can be used as
presoaks, in ultrasonic cleaners and instrument wash-
ers/disinfectors, and for evacuation lines. In deciding
what to use, factors to consider include whether a
presoak product is able to break down bioburden, how
instrument-friendly (i.e., nonaggressive) it is, whether
it is a concentrate or ready to use (consider inventory
requirements, storage space, and risk of spillage and
chemical exposure), ease of use, pH and, specifcally for
foam, how quickly it will dissipate and whether it will
maintain coverage over instruments. Presoaking togeth-
er with ultrasonic cleaning was found in one series of
tests to result in more effective cleaning than ultrasonic
cleaning alone. Presoaking should be relatively brief
and the manufacturers instructions followed to reduce
the possibility of corrosion/rusting of non-stainless steel
metal instruments (e.g., burs).
Cleaning Instruments
Instruments should be cleaned prior to sterilization.
1
The objective is to remove debris and bioburden prior to
preparation/packaging of instruments for sterilization;
debris can act as a barrier that protects microorganisms
and thereby prevents sterilization. The available options
are manual cleaning or mechanical cleaning (i.e., the use of
ultrasonic cleaners, instrument washers or washers/disinfec-
tors). The CDC recommends using an automated cleaner.
Mechanical cleaning by ultrasonic cleaners and instrument
washers or washers/disinfectors is superior to manual clean-
ing for debris removal and reduces handling.
11,12
Manual
cleaning/scrubbing of contaminated instruments should be
avoided where possible to reduce the risk of the operator
sustaining percutaneous injuries or being exposed to splash/
splatter that could result in disease transmission. If manual
scrubbing is required for example, if debris remains on an
instrument following mechanical cleaning this should be
performed at arms length, low in the sink using a long-han-
dled brush and underwater (and while wearing heavy-duty
utility gloves, a mask and protective eyewear).
Ultrasonic cleaning
Ultrasonic cleaning requires the use of an ultrasonic
cleaning machine and solution. During cleaning, the
machine generates sound waves which are introduced
into the solution, causing it to bubble. The action of the
bubbles imploding against the surfaces of the instru-
ments cleans them. This is called cavitation. Ultrasonic
machines with intermittent sound waves are considered
superior to those with continuous sound waves and
offer more consistent activity throughout the cleaning
solution. Other factors in choosing cleaning machines
include their volume (size) and design, which will
be based on the anticipated size of instrument loads,
processing-area space requirements, and whether the
space is countertop or under the counter. Additional
factors are the cleaners power and noise levels, test-
ing and reliability, and ease of use i.e., whether the
cleaning solution must be emptied manually (requiring
user handling) or can be drained through a hose. All
manufacturers instructions must be followed for a given
ultrasonic cleaner.
Closed cassettes should be placed on a tray or rack
inside the machine and not placed in contact with the
bottom of the ultrasonic cleaner. Similarly, loose instru-
ments should be placed in a basket and not be loose or
bundled in contact with the bottom of the ultrasonic
cleaner. Only one or two layers should be stacked in
the ultrasonic cleaner; failure to load the cleaner ap-
propriately can result in areas of instruments not being
cleaned because imploding bubbles may be unable to
reach some areas. After loading the ultrasonic cleaner,
the lid should be closed before the cleaner is turned
on to ensure no ultrasonic solution sprays out into the
surrounding environment. Instruments should not be
added to batches of instruments already being ultrasoni-
cally cleaned. After treatment, cleaned instruments are
removed and rinsed under running water to remove the
cleaning solution (prevents instrument spotting, stain-
ing and pitting) and then allowed to dry before being
prepared/packaged for sterilization.
DENTAL LEARNING
8
www.dentallearning.net
Ultrasonic cleaning solutions
Ultrasonic cleaning solutions or dissolving ultrasonic
tablets are essential. Water is not an ultrasonic cleaning
solution. Both enzymatic and nonenzymatic options are
available for instrument processing. As with presoaks,
preferred ultrasonic cleaning solutions are those that help
to break down bioburden and can help remove organic
tissue, blood and material debris such as plaster and
oxides stuck to instruments. A solutions cleaning abil-
ity and instrument compatibility are important. Anti-
corrosive ultrasonic cleaners help protect non-stainless
steel metal instruments and increase their useful life,
while noncorrosive products will not damage them.
Other factors to consider are the form of the solution
(i.e., concentrate versus a prepared solution or tablets),
cost-effectiveness and scent. It is essential that ultrasonic
solutions are discarded and replaced at least once a day.
If bacterial loads are higher due to more heavily contami-
nated instruments or heavier/more-frequent instrument
loads, then the solution must be changed more frequently.
Ultrasonic solutions should not under any circumstances
be topped off in lieu of full replacement of the solution.
Instrument washers and washers/disinfectors
Instrument washers and washers/disinfectors are more
automated compared with ultrasonic cleaners, requiring
less handling of contaminated instruments and therefore
reducing exposure to contamination and the risk of injury.
Both washer and washer/disinfector cycles provide for
cleaning, rinsing and drying. The difference lies in the use
of high-temperature water and disinfectants in washers/
disinfectors compared with the hot water and detergent
used in washers, which results in cleaned and disinfected
instruments with less debris. The detergent/disinfectant
recommended by the manufacturer should be used and
the manufacturers instructions followed. Note that these
cleaners are medical devices regulated by the FDA; regular
dishwashers are not regulated as medical devices and are
not a suitable substitute for an instrument washer or wash-
er/disinfector. After cleaning, rinsing and drying, instru-
ments are ready for inspection to ensure that they are free
of damage and debris before entering the next phase of
instrument processing. For cleaning endodontic fles, ultra-
sonic cleaners have been found to be superior to washers/
disinfectors, which may have been due to the shape of the
instrument holder or complexity of the fles surface area.
13
Instrument Sterilization
The sterilization process for instruments is based on
their classifcation. Spauldings classifcation categorizes
Tips for Effective Ultrasonic Cleaning
Place cassettes on a tray or rack in the machine
Place loose instruments in a basket
Place only one or two layers of cassettes in the
ultrasonic cleaner
Avoid overloading the ultrasonic cleaner
Use an ultrasonic cleaning foam or solution
that is gentle on instruments while being able to
reduce bioburden
Keep the lid on the ultrasonic cleaner while it is
in use
Rinse all cleaned instruments under running
water and allow to dry
Discard and replace ultrasonic cleaning solution
at least daily and more often if bacterial loads
are high or if visibly dirty
Do not add instruments to others already being
cleaned
Do not place cassettes or loose instruments in
the base of the ultrasonic bath
Never top off ultrasonic cleaning solutions
Instrument Processing for Infection Prevention
9
JUNE 2012
instruments as critical, semicritical or noncritical. Critical
instruments are those that penetrate soft tissues (e.g., oral
mucosa) and contact or enter bone and other normally
sterile tissues. Semicritical instruments contact mucous
membrane or nonintact (i.e., broken) skin but do not
penetrate these or contact or penetrate other tissues. Lastly,
noncritical instruments are those that contact only intact
skin and do not penetrate tissues. Instruments in each of
these categories are treated differently. (Table 1)
All critical instruments, and semicritical instruments
that are heat-resistant, as well as handpieces, must be
heat-sterilized. Semicritical instruments that are heat-sen-
sitive with the exception of handpieces and noncritical
instruments may be sterilized with a high-level sterilant/
disinfectant.
1,8
The majority of instruments in service today
are heat-tolerant (and therefore can be heat-sterilized), or
are single-use disposable which means they may not be
reprocessed and must be disposed of after a single use. In
fact, recent studies have shown that, even after precleaning
and sterilization, sterilization of complex-surface instru-
ments such as dental burs and endodontic fles was not
always successful, with failure ranging from 15% (bur set)
to 58% (endodontic fles).
14
The CDC recommends the use
of single-use disposable items whenever possible.
With more advanced devices being used chairside, it
is critical to understand which instruments can undergo
mechanical cleaning, tolerate use of disinfectant/sterilant
or need to be disassembled for processing. For example,
autoclaving was found to result in signifcantly less change
in the transmitted light intensity of curing lights in one
study of 2,100 sterilization cycles when compared with
use of a 2% glutaraldehyde liquid disinfectant/sterilant
for curing light tips.
15
Another example is lasers, some of
which have been designed with fully autoclavable tips,
spools and sleeves, while others may have disposable tips
and other components that are autoclavable. These attri-
butes are considerations when purchasing equipment, and
the protocol for an instrument must be known to ensure
appropriate processing.
Handpieces
For handpieces, the burs should be removed and
the external surface of the handpiece wiped to remove
debris. Handpieces must not be immersed in solution or
placed in an ultrasonic bath, as doing so would damage
the bearings and result in premature failure. After clean-
ing, handpieces must be heat-sterilized in accordance
with the processing described below. Handpieces that
cannot be heat-sterilized must be removed from service.
1
Although handpieces were highly vulnerable to heat
associated with sterilization when heat-sterilization frst
became a requirement, developments in O-rings and tur-
bines have resulted in a signifcant improvement in the
life of heat-sterilized handpieces. In one study assessing
TABLE 1. Classifcation of instruments
Critical Penetrate soft tissues, bone, normally sterile tissues Heat-sterilize
Semi-critical Contact mucous membranes, nonintact skin
Do not penetrate hard or soft tissues
Heat-sterilize if heat-resistant
Heat-sterilize handpieces
If heat-sensitive:
High-level disinfectant/sterilant
Noncritical Contact intact skin High-level disinfectant
Sources: Guidelines for infection control in dental healthcare settings2003 (CDC); Guideline
for disinfection and sterilization in healthcare facilities2008 (CDC).
DENTAL LEARNING
10
www.dentallearning.net
high-speed air turbine handpieces after 300 cycles, no
abnormalities were noted in the turbines ball bear-
ings.
16
A newly completed study found that tested tur-
bines failed after 560 cycles, with longevity infuenced
by lubrication, corrosion protection and maintaining
usage at low loads. It was concluded that although
autoclaving reduces the life of handpieces, lubrication
increases their life, and the greatest negative infuence
on the turbines was running at high load.
17
In addition
to following the CDC guidelines, it is essential to follow
the handpiece manufacturers instructions for cleaning,
sterilization and lubrication.
Heat-Sensitive Semicritical and Noncritical
Instruments
For heat-sensitive semicritical instruments (except handpiec-
es) and noncritical instruments, high-level disinfectants/steril-
ants (not surface disinfectants) may be used instead of heat
sterilization. High-level disinfectants/sterilants are germicidal
chemicals that have been cleared by the FDA for this use and
can destroy all microorganisms (including spores) in a given
length of time. Soaking trays are also available for use with
high-level disinfectants/sterilants. A number of chemicals meet
the requirements of a high-level disinfectant/sterilant, includ-
ing 7.5% hydrogen peroxide solution (sterilizes in six hours of
immersion), 3.4% buffered glutaraldehyde solution (sterilizes
in 10 hours at 77F). Other chemicals include phenol solu-
tions and 8% periacetic acid. The manufacturers instructions
must be followed and compatibility with instrument materi-
als verifed. Sterilized instruments should be dried, segregated
and stored in a dry, enclosed area. Note that tests cannot be
performed to assure sterility with high-level disinfectants/steril-
ants. Tests are however available for some high-level disinfec-
tant/sterilants that show whether the solution is still active and
above the minimum effective concentration.
Heat-Sterilization: Instrument and Closed-
Cassette Sterlization Packaging
Cleaned, dry instruments and closed cassettes should
be packaged before being heat-sterilized. In all situa-
tions, only FDA-cleared sterilization packaging may be
used. Properly packaging instruments and cassettes prior
to sterilization serves several functions: 1) packaging has
external and internal indicators that verify sterilization
parameters (see below); 2) the risk of confusing contami-
nated with sterilized instruments is removed; and 3) sterile
instruments will remain uncontaminated in intact packag-
ing post-sterilization, provided they are handled and stored
correctly, until they are again used chairside.
18
In contrast,
unpackaged loose instruments are handled immediately
after sterilization and therefore are subject to contamina-
tion from then onward.
Sterilization packaging must be strong enough for
routine use without tearing, must allow penetration of the
sterilant and must remain intact post-sterilization during
storage to prevent contamination.
19
The choice of packag-
ing depends on what type of heat sterilizer will be used,
20
what is being packaged and personal preference. Options
include FDA-cleared paper wrap, paper pouches, paper/
plastic pouches, plastic pouches and tubing. Paper wrap
is used routinely for cassettes, with an internal indicator
and heat-sensitive tape for closure. Note that staples, pins
and other objects that close the packaging by piercing it
may not be used because they compromise the packaging
and permit recontamination of processed instruments once
they have been removed from the sterilizer. Plastic and
plastic/paper pouches and plastic tubing are used for cas-
settes, instruments and handpieces. These enable identifca-
tion of both the contents and the status of internal indica-
tors. Self-sealing pouches are also available, offering ease
of use. The seal on any packaging must be adequate and
not compromised.
Paper and paper/plastic pouches are contraindicated
for sharp instruments that are not contained in cassettes,
because the points of the instruments can pierce these. In
addition, plastic/paper pouches may separate, scorch or
melt during exposure to the high temperatures reached in
dry-heat sterilizers and are therefore contraindicated for
that purpose.
21
If dry-heat sterilization is being performed,
packaging that is FDA-cleared specifcally for this purpose
Instrument Processing for Infection Prevention
11
JUNE 2012
must be used. If in doubt, check with the manufacturer on
the intended use of specifc sterilization packaging.
All sterilization packaging must include an internal in-
dicator; if the internal indicator is not visible (for example,
in a paper wrap), then an external indicator must also be
used. Sterilization packaging should have FDA clearance,
use medical-grade paper and/or plastic, be easy to use (e.g.,
self-sealing), be reliable and be available in multiple sizes.
Chemical indicators
There are six classes of chemical indicators used with
sterilization packaging/processing. These indicate whether
malfunctioning occurred during sterilization (including as a
result of operator error); they do not indicate if sterilization
was achieved. Class I and II indicators are external indica-
tors. A Class I indicator is required if an internal indicator
is present but not visible. It indicates only that the package
was exposed to the process. Class II indicators are required
specifcally for dynamic air removal (Class B) sterilizers.
This is the Bowie-Dick (air-removal) test and must be
performed in a test pack at the beginning of each day in an
otherwise-empty sterilizer, in conformance with standards.
22
Class III, IV, V and VI indicators are internal. The Class
VI, known as an emulating indicator, reacts to all variables
(time, temperature and presence of saturated steam) for a
specifc sterilization cycle and verifes the cycle; Class V in-
tegrating indicators react to all variables (time, temperature
and presence of saturated steam) over a range of tempera-
tures. The main difference between a Class III and Class IV
internal indicator is that the Class IV is designed to react
to two or more variables rather than to only one, at stated
values for the given variables. These also meet the packag-
ing internal indicator requirement and are built into some
sterilization pouches. Sterilization packaging with built-in
indicators saves time and inventory and avoids the risk that
placement of an indicator may be forgotten. If any in-use in-
dicator fails, the load must be repackaged and reprocessed.
When using internal indicators, these should be placed
next to the instruments to ensure that they are measuring
the parameters where the instruments are located. This is
especially important for larger sterilization packages. No
chemical indicators indicate sterility has been achieved, only
that the process met the parameters being measured.
Heat Sterilization
Heat sterilization of dental instruments is achieved by au-
toclaving, dry-heat sterilization or chemical sterilization using
a chemclave. All are effective at killing microorganisms when
used correctly, and cycle times vary depending on the method
of sterilization, cycle selected and the specifc sterilizer. Instru-
ment loads placed in sterilizers should not be placed on top
of, in contact with or overlapping one another. They must be
placed with suffcient space between them to allow sterilant
Figure 6a. Sterilization packaging
Figure 6b. Sterilization packaging over cassette
DENTAL LEARNING
12
www.dentallearning.net
contact and penetration of the sterilant through sterilization
packaging. The sterilizer must not be overloaded, and the
manufacturers instructions must be followed.
Autoclaves
Autoclaves use a combination of heat and pressure to
generate steam that penetrates the sterilization packaging
to sterilize instruments. Sterilization occurs by denatur-
ation of microbes proteins. Cassette racks are available for
horizontal or vertical loading, thereby helping to prevent
overloading. All autoclaves require the use of distilled water
to prevent potential spotting on instruments or cassettes and
the buildup of mineral deposits from regular tap water in-
cluding calcium on the autoclave chamber and in its pipes.
Autoclaves operate in two distinct ways, using dynamic
air-removal or gravity displacement. Dynamic air-removal
autoclaves (vacuum autoclaves) work by frst removing air
using a vacuum pump or a valve that is controlled elec-
tronically, after which steam enters the chamber. Com-
pared with the gravity displacement autoclave, this process
removes more air and improves the steams penetration
into the turbines of dental handpieces.
23
With the gravity
displacement autoclave, steam enters the chamber from
the sides and top of the chamber and pushes air out of the
chamber through the base using a vent.
After autoclaving, the load must remain in the auto-
clave with the door still closed until depressurization and
drying of the packaging has been completed. Packaging
removed prematurely from an autoclave while still damp
can wick and become contaminated, at which point instru-
ment processing must begin anew for that load. Typical
cycle times and temperatures for gravity displacement and
dynamic air-removal autoclaves are, respectively, 15 to 30
minutes at 250F (121C) and 3.5 to 10 minutes at 270F
(132C). This does not include warm-up pressurization
time or the time required for depressurization and the dry-
ing cycle.
Dry-heat sterilizers
Dry-heat static and convection (forced-air) sterilizers
utilize higher temperatures compared with autoclaves to
achieve sterilization. As with autoclaves, the cycle time var-
ies, ranging from six minutes to up to two hours. Unlike
with autoclaves, the packaged instruments are then ready
for removal and storage since no drying cycle is necessary.
Typical cycle times and temperatures for static and convec-
tion dry-heat sterilizers are, respectively, 60 to 120 minutes
at 320F (160C) and 6 to 12 minutes at 375F (190C).
Chemclaves
Chemclaves use temperatures similar to those used
in autoclaves. They have a fast cycle time of around 20
minutes, and the instruments are dry after the cycle.
Chemclaves use proprietary formaldehyde-alcohol-based
chemicals. Although chemclaves are faster than autoclaves
and use lower temperatures than those used in dry-heat
sterilization, their use of chemicals reduces their attractive-
ness and increases exposure to chemicals in the offce. The
typical cycle time and temperature for chemclaves are 20
minutes at 270F (132C).
Each category of heat sterilizer has advantages and
disadvantages. Autoclaving can result in corrosion/pitting
of non-stainless steel metals carbon-steel instruments/
devices can be treated with rust inhibitors to help prevent
this. In comparison, chemclaves reduce the risk of corro-
sion/pitting, and dry-heat sterilization eliminates the risk
completely (because only dry heat is used) and reduces
dulling of the instruments. On the other hand, dry-heat
sterilizers utilize the highest temperatures and are more
likely than autoclaves to damage instrument O-rings (con-
tained in dental handpiece turbines) and other plastics and
lead to their deterioration.
All sterilizers are medical devices regulated by the FDA,
and all must pass rigorous testing before being cleared
as medical devices. Mechanical indicators on sterilizers
confrm that a specifc parameter was reached. These may
be mechanical gauges or electronically controlled gauges.
Examples of mechanical indicators include the gauges on
autoclaves indicating that a given temperature or pres-
sure has been reached in the chamber. In some devices,
Instrument Processing for Infection Prevention
13
JUNE 2012
these parameters can be printed; when this capability is
present, the printout for each cycle should be kept in the
sterilization log. Mechanical indicators provide immediate
feedback; however, even if all parameters are met, they in-
dicate only that the sterilizer was functioning, not whether
sterilization has occurred.
Biological indicators (spore tests)
Only biological indicators give any assurance that ste-
rility has actually been achieved. The necessity of perform-
ing biological indicator tests (spore tests) is highlighted
by results from several studies in Europe and North
America demonstrating fail rates ranging from 2.3% up to
33% when spore tests were performed in autoclaves.
24-28
Biological indicators should be used at least weekly and
every time an implantable device is being sterilized before
implantation.
8
Spore levels are tested because spores are the most
resistant microorganism if they are killed by steriliza-
tion, then so are all other less-resistant microorganisms. To
ensure that a successful test result stems from sterilization
having actually occurred rather than from spores that were
not viable even without sterilization, both test and control
biological indicators are used. The test indicator is placed
inside the sterilizer, while the control one is left outside the
sterilizer. The test is deemed valid if the spores outside the
sterilizer are still alive and the sterilized ones are not.
Spore tests differ in the type of spore they use for
different modes of heat sterilization: Geobacillus stearo-
thermophilus for autoclaves and chemclaves, and Bacillus
subtilis for dry-heat sterilization. Spore tests may be per-
formed in-offce using standard kits that include the spore
test vials and incubators, or the spore test can be sent to a
laboratory for verifcation of sterility assurance following
its use in the sterilizer. Regardless of which method is used,
all data must frst be recorded before the spore test is per-
formed, including the load number, sterilizer number and
processing date. This data should be placed on the spore
test vial label as well as in the record book, together with
the results of the test.
Control and failed spore tests (live spores) must be
autoclaved at 250F/121C for at least 30 minutes prior
to disposal. For failed tests, a repeat test should be per-
formed before using the sterilizer again for instrument
processing. The loads that were treated at the time of the
frst failed test must also be reprocessed, as must implant-
able devices (which must always be accompanied by a
spore test in the sterilizer). If the sterilizer fails to inac-
tivate spores in a second (repeat) test, then the sterilizer
must be examined by a specialist before being used again.
After such an examination, for a dynamic air-removal
autoclave the Bowie-Dick test must be run in three con-
secutive cycles, together with CI and BI tests. The CI and
BI tests are also required in three consecutive cycles for
gravity displacement autoclaves.
Storage
Regardless of which heat-sterilization technique is used,
sterilized instruments and devices should be stored in their
unopened sterilization packaging in a dry, dust-free storage
area until needed. One study found no contamination of
test groups of autoclaved or dry-heat-sterilized instruments
that had been stored for six months in intact packaging
in a closed, dry area post-sterilization. Contamination oc-
curred where packaging had lost its integrity (was torn),
increasing with time.
29
Another study that ended at 124
days found no post-sterilization contamination of instru-
ments stored in their intact, unopened sterilization packag-
ing during the duration of the study.
30
Summary
Instrument processing is a key element of the infec-
tion prevention cycle. Its success depends on following
a standard protocol that meets the CDC guidelines and
OSHA requirements. The protocol must be reliable and
repeatable, and FDA-cleared devices and supplies, as well
as personal protective equipment, must be used appropri-
ately to ensure safe and effective instrument processing
for the protection of dental personnel, patients and the
general public.
DENTAL LEARNING
14
www.dentallearning.net
References
1. CDC. Guidelines for infection control in dental health-care set-
tings2003. MMWR 2003;52(RR-17):1-66.
2. Siegel JD, Rhinehart E, Jackson M, Chiarello L; Health Care Infection
Control Practices Advisory Committee. 2007 Guideline for isolation
precautions: preventing transmission of infectious agents in health care
settings. Am J Infect Control. 2007;35(10 suppl 2):S65-S164.
3. Harte JA. Standard and Transmission-Based Precautions: An Update
for Dentistry. J Am Dent Assoc. 2010;141;572-581. www.osha.gov/SLTC/
dentistry/index.html.
4. Cleveland JL, Barker LK, Cuny EJ, Panlilio AL. National Surveillance
System for Health Care Workers Group.
Preventing percutaneous injuries among dental health care personnel. J
Am Dent Assoc. 2007 Feb;138(2):169-178.
5. OSHA. Bloodborne pathogens standard. Available at: http://
www.osha.gov/pls/oshaweb/owadisp.show_document?p_
table=STANDARDS&p_id=10051.
6. Harte JA, Molinari JA. Instrument cassettes for offce safety and infec-
tion control. Compendium. November 2007;28(11):596-601.
7. Rutala WA, Weber DJ, Healthcare Infection Control Practices Advi-
sory Committee. Guideline for disinfection and sterilization in health-
care facilities. CDC2008. Available at: http://www.cdc.gov/hicpac/pdf/
guidelines/Disinfection_Nov_2008.pdf
8. Blalock JS, Cooper JR, Rueggeberg FA. The effect of chlorine-based
disinfectant on wettability of a vinyl polysiloxane impression material. J
Prosthet Dent. 2010 Nov;104(5):333-341.
9. Miller CH. Cleaning, sterilisation and disinfection: basics of microbial kill-
ing for infection control. J Am Dent Assoc. 1993;124:48-56.
10. Miller CH, Riggen SD, Sheldrake MA, Neeb JM. The presence
of microorganisms in used ultrasonic cleaning solutions. Am J Dent.
1993;6:27-31.
11. Miller CH, Palenik CJ. Infection Control & Management of Hazard-
ous Materials for the Dental Team. 3rd Edition, Elsevier Mosby, St.
Louis, Mo., 2005.
12. Perakaki K, Mellor AC, Qualtrough AJ. Comparison of an ultrasonic
cleaner and a washer disinfector in the cleaning of endodontic fles. J
Hosp Infect. 2007 Dec;67(4):355-359. Epub 2007 Nov 19.
13. Morrison A, Conrod S. Dental burs and endodontic fles: are routine
sterilization procedures effective? J Can Dent Assoc. 2009 Feb;75(1):39.
14. Kakaboura A, Tzoutzas J, Pitsinigos D, Vougiouklakis G. The effect
of sterilization methods on the light transmission characteristics and
structure of light-curing tips. J Oral Rehabil. 2004 Sep;31(9):918-923.
15. Nagai M, Takakuda K. Infuence of number of dental autoclave
treatment cycles on rotational performance of commercially available
air-turbine handpieces. J Med Dent Sci. 2006 Jun;53(2):93-101.
16. We M, Dyson J, Darvell B. Factors affecting dental air-turbine hand-
piece bearing failure. Oper Dent. 2012 Feb 16. [Epub ahead of print]
17. ADA Council on Scientifc Affairs and ADA Council on Dental Prac-
tice. Infection control recommendations for the dental offce and the
dental laboratory. J Am Dent Assoc. 1996;127:672-680.
18. Dunkelberg H, Fleitmann-Glende F. Measurement of the microbial
barrier effectiveness of sterilization containers in terms of the log reduc-
tion value for prevention of nosocomial infections. Am J Infect Control.
2006;34:285-289.
19. Association for the Advancement of Medical Instrumentation,
American National Standards Institute. Good hospital practice: steam
sterilization and sterility assurance. ANSI/AAMI ST46-1993. Arlington,
VA: Association for the Advancement of Medical Instrumentation, 1993.
20. Rutala WA, Weber DJ. Choosing a sterilization wrap for surgical
packs. Infect Cont Today. 2000;4:64-70.
21. OSAP. Infection Control in Practice. 2008;7(4):1-8.
22. Association for the Advancement of Medical Instrumentation. ANSI/
AAMI.2006;ST79-2006;A1,A2.
23. Andersen HK, Fiehn NE, Larsen T. Effect of steam sterilization inside
the turbine chambers of dental turbines. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 1999;87(2):184-188.
24. Palenik CJ, King TN, Newton CW, Miller CH, Koerber LG. A survey
of sterilisation practices in selected endodontic offces. J Endod.
1986;12:206-209.
25. Simonsen RJ, Schachtele CF, Joos RW. An evaluation of sterilisation
by autoclave in dental offces. J Dent Res. 1979;58:400.
26. Engelhardt FP, Fisvatin H. Hygiene in der ZahnartzpraxisWunsch
und Wirklichkeit. Dtsch Zahnarzd Z 1976; 31:277-281.
27. Scheutz F, Reinholdt J. Outcome of sterilisation by steam autoclaves
in Danish dental offces. Scand J Dent Res. 1988; 96:167-170.
28. Burke FJT, Coulter WA, Cheung SW, Palenik CJ. Autoclave perfor-
mance in and practitioner knowledge of autoclave use: a survey of selected
UK practices. Quintessence Int. 1998;29:231-238.
29. Rosa AC, Brusca MI, Manto MC, Mosca CO, Nastri N. Effects of han-
dling and storage on sterile dental instruments. Acta Odontol Latinoam.
2001;14(1-2):35-39.
30. Barker CS, Soro V, Dymock D, Fulford M, Sandy JR, Ireland AJ. Time-
dependent recontamination rates of sterilised dental instruments. Br
Dent J. 2011 Oct 21;211(8):E17.
Webliography
Centers for Disease Control and Prevention. Guidelines for infection
control in dental health-care settings2003. MMWR 2003;52(RR-
17):1-66. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/
rr5217a1.htm.
OSHA. Bloodborne pathogens standard. Available at: http://www.osha.
gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_
id=10051.
Rutala WA, Weber DJ, Healthcare Infection Control Practices Advisory
Committee. Guideline for disinfection and sterilization in healthcare
facilities. CDC2008. Available at: http://www.cdc.gov/hicpac/pdf/
guidelines/Disinfection_Nov_2008.pdf.
Instrument Processing for Infection Prevention
15
JUNE 2012
1. The chain of infection consists of __________ elements.
a. one
b. three
c. fve
d. seven
2. The CDC guidelines for infection control in dental healthcare
settings were published in __________.
a. 1993
b. 1998
c. 2003
d. 2008
3. The isolation guidelines for healthcare settings from the CDC
address __________.
a. specifc pathogens
b. all pathogens
c. highly-transmissible diseases
d. a and c
4. The overall goal of instrument processing is to provide _______.
a. a clean clinical setting
b. sterile instruments
c. an OSHA-compliant offce
d. all of the above
5. Instrument processing should occur in a specifc location that is
segregated into __________.
a. dirty and clean areas
b. cold and hot areas
c. the most convenient location
d. all of the above
6. The wearing of heavy-duty utility gloves, a face mask and pro-
tective eyewear is necessary during __________.
a. operatory clean-up
b. transportation of instruments
c. instrument processing
d. all of the above
7. Closed perforated cassettes __________.
a. can be placed in pre-soaks
b. can be placed in ultrasonic cleaners or washer/disinfectors
c. reduce the risk of injury
d. all of the above
8. __________ should be placed in the sharps container.
a. Suture needles and capped syringe needles
b. Disposables blades, scalpels and all-in-one syringes
c. Broken glass carpules
d. all of the above
9. __________, state, local and municipal regulations must be
followed when disposing of sharps containers.
a. FDA
b. OSHA
c. AGD
d. all of the above
10. Medical and surgical gloves are __________ indicated for
operatory clean-up or instrument processing.
a. sometimes
b. never
c. always
d. none of the above
11. Using automated cleaning devices and ultrasonic baths
increases safety during instrument processing compared
with __________.
a. manual scrubbing
b. mechanical brushing
c. chemical scavenging
d. all of the above
12. Disposing of sharps chairside, prior to transporting
instruments in closed cassettes/trays to the processing
area, __________.
a. is compulsory
b. is essential
c. reduces the risk of sharps injuries
d. all of the above
13. Non-perforated closed cassettes __________used for
autoclaving of instruments.
a. must not be
b. may be
c. must be
d. none of the above
14. Impressions and other materials that will be transported
to the dental laboratory must frst be disinfected according
to __________.
a. the material involved
b. the time available
c. the manufacturers recommendations
d. a and b
15. Instruments are segregated by __________ after being
transported to the instrument processing area.
a. size
b. purpose
c. whether or not they are heat-resistant or handpieces
d. a and b
CEQuiz
DENTAL LEARNING
16
www.dentallearning.net
16. Instruments that will remain in the processing area for a
period of time prior to cleaning and sterilization should be
__________ to help prevent debris from drying on to the
instruments.
a. pre-soaked
b. ultrasonically treated
c. treated with high-level sterilants instead of heat sterilization
d. a and c
17. If debris has dried on instruments while being used in the
operatory, they must be __________ before cleaning.
a. dunked in hot water
b. placed in a pre-soak
c. placed in a vibrator to loosen the debris
d. none of the above
18. If a foam product is being used as a pre-soak, suffcient foam
must be sprayed over the cassette/loose instruments to allow
for complete coverage __________.
a. after removal of the instruments
b. after shrinkage of the foam
c. over the bottom layer of instruments
d. none of the above
19. Solutions and foams are now available that __________.
a. are less aggressive on instruments
b. help remove debris
c. help remove bioburden
d. all the above
20. Presoaking together with ultrasonic cleaning was found in
one series of tests to result in __________ cleaning than
ultrasonic cleaning alone.
a. less effective
b. more effective
c. unnecessary
d. none of the above
21. If manual scrubbing of instruments is required, this should be
performed __________.
a. at arms length
b. low in the sink and underwater
c. while wearing gloves, a mask and protective eyewear
d. all of the above
22. Instruments and cassettes should never be placed in contact
with the bottom of the ultrasonic bath as __________.
a. imploding bubbles may then not be able to reach all areas of
the instruments
b. this can result in inadequate cleaning of instruments
c. this will result in a high-pitched whine
d. a and b
23 Anti-corrosive ultrasonic cleaners help protect and increase
the useful life of __________.
a. stainless steel metal instruments
b. non-stainless steel metal instruments
c. plastic instruments
d. all of the above
24. If instruments are not rinsed with water after being in an
ultrasonic cleaning solution, this can result in instrument
__________.
a. spotting
b. staining
c. pitting
d. all of the above
25. If there is no longer enough ultrasonic cleaning solution
present, this can be __________.
a. topped up
b. replaced with water
c. diluted with saline
d. none of the above
26. Instruments washer/disinfectors use __________.
a. cold water and sterilant
b. hot water and detergent
c. high-temperature water and disinfectant
d. none of the above
27. Mechanical cleaning by ultrasonic cleaners and instruments
washers or washer/disinfectors is __________ to manual
cleaning for debris removal.
a. inferior to
b. superior to
c. the same as
d. none of the above
28. For processing of handpieces, __________.
a. the bur should be removed
b. the external surface of the handpiece should be wiped
c. the handpiece must be autoclaved
d. all of the above
29. __________ classifcation categorizes instruments as critical,
semi-critical or non-critical.
a. Spellings
b. Spauldings
c. Sporemans
d. none of the above
30. __________ must be heat-sterilized.
a. All critical instruments
b. All handpieces
c. Semi-critical instruments that are heat-resistant
d. all of the above
31. Precleaning and sterilization of complex-surface instruments
is __________ successful.
a. never
b. not always
c. always
d. extremely
32. High-level disinfectants/sterilants can __________ curing lights.
a. reduce the light transmission intensity of
b. improve the functioning of
c. soften
d. all of the above
CE QUIZ
Instrument Processing for Infection Prevention
17
JUNE 2012
33. High-level disinfectants/sterilants __________.
a. can destroy all microorganisms in almost no time
b. have been cleared by the FDA for use
c. are germiphobic chemicals
d. all of the above
34. 7.5% hydrogen peroxide solution sterilizes instruments
after __________ hours of immersion.
a. two
b. four
c. six
d. eight
35. Tests can be performed on high-level disinfectant/sterilants
that __________.
a. assure sterility
b. measure whether it is at the minimum effective concentration
c. take the place of indicators
d. none of the above
36. Paper and paper/plastic sterilization pouches __________.
a. are contraindicated for sharp instruments that are not contained
in cassettes
b. may separate during exposure to the high temperatures reached
in dry heat sterilizers
c. must be FDA-cleared for this use
d. all of the above
37. Paper wrap is used for cassettes, with __________.
a. heat-sensitive tape
b. an internal indicator
c. a biological indicator
d. a and b
38. All sterilization packaging must include use of __________.
a. an external indicator
b. an internal indicator
c. a biological indicator
d. none of the above
39. Sterilization packaging must __________.
a. be strong enough for routine use
b. allow penetration of the sterilant through it
c. remain intact post-sterilization during storage
d. all of the above
40. A __________ indicates only that the package was exposed
to the process.
a. Class I indicator
b. Class III indicator
c. Class VI indicator
d. all of the above
41. The main difference between a Class III and Class IV internal
indicator is that the Class IV is designed to react to __________.
a. single variables
b. multiple variables
c. specifc instruments
d. b and c
42. Heat sterilization of dental instruments is achieved by
__________.
a. autoclaving
b. dry-heat sterilization
c. chemical sterilization
d. all of the above
43. Instrument loads placed in sterilizers should not be placed
__________.
a. on top of each other
b. in contact with each other
c. overlapping each other
d. all of the above
44. Autoclaves __________.
a. use a combination of heat and pressure
b. denature microbes proteins
c. can be gravity displacement or dynamic air-removal
autoclaves
d. all of the above
45. After autoclaving, the load must remain in the autoclave
with the door still closed until __________.
a. depressurization has occurred
b. drying of the packaging has been completed
c. repressurization has occurred
d. a and b
46. Chemclaves are __________ than autoclaves.
a. slower
b. faster
c. less effective
d. b and c
47. Dry-heat sterilization __________.
a. eliminates the risk of instrument corrosion
b. increases the potential for damage to O-rings
c. reduces the dulling of instruments
d. all of the above
48. Mechanical indicators __________.
a. indicate if parameters were met
b. indicate whether sterilization occurred
c. indicate the weight of the instrument load
d. all of the above
49. Only __________ indicators give any assurance that sterility
was actually achieved.
a. external indicators
b. biological indicators
c. internal indicators
d. none of the above
50. Sterilized instruments and devices should be stored in their
unopened sterilization packaging __________.
a. above the autoclave
b. in the processing area
c. in a dry, dust-free storage area
d. none of the above
CE QUIZ
DENTAL LEARNING
18
www.dentallearning.net
EDUCATIONAL OBJECTIVES
Defne the elements of the chain of infection
Delineate and describe the differences in the processing of critical, semicritical and noncritical instruments
Review the use of presoaks and cleaning of instruments
List and describe heat sterilization options and appropriate sterilization packaging
Review the uses and purposes of chemical and biological indicators
Please direct all questions pertaining to Dental Learning, LLC or the administration of this course to mtonnessen@dentallearning.net. COURSE EVALUATION and PARTICIPANT FEEDBACK: We encourage participant feedback pertaining to all courses. Please be sure
to complete the survey included with the course. Please e-mail all questions to: mtonnessen@dentallearning.net. INSTRUCTIONS: All questions should have only one answer. Participants will receive confrmation of passing by receipt of a verifcation form. Verifcation
forms will be mailed within two weeks after taking an examination. EDUCATIONAL DISCLAIMER: The content in this course is derived from current information and evidence. Any opinions of effcacy or perceived value of any products mentioned in this course
and expressed herein are those of the author(s) of the course and do not necessarily refect those of Dental Learning. Completing a single continuing education course does not provide enough information to give the participant the feeling that s/he is an expert in
the feld related to the course topic. It is a combination of many educational courses and clinical experience that allows the participant to develop skills and expertise. COURSE CREDITS/COST: All participants scoring at least 70% on the examination will receive a
verifcation form verifying 3 CE credits. The formal continuing education program of this sponsor is accepted by the AGD for Fellowship/Mastership credit. Please contact Dental Learning, LLC for current term of acceptance. Participants are urged to contact their state
dental boards for continuing education requirements. Dental Learning, LLC is a California Provider. The California Provider number is RP5062. The cost for courses ranges from $29.00 to $110.00. Many Dental Learning, LLC self-study courses have been approved by
the Dental Assisting National Board, Inc. (DANB). To fnd out if this course or any other Dental Learning, LLC course has been approved by DANB, please RECORD KEEPING: Dental Learning, LLC maintains records of your successful completion of any exam. Please
contact our offces for a copy of your continuing education credits report. This report, which will list all credits earned to date, will be generated and mailed to you within fve business days of receipt. CANCELLATION/REFUND POLICY: Any participant who is not
100% satisfed with this course can request a full refund by contacting Dental Learning, LLC in writing or by calling 1-888-724-5230. 2012
PLEASE PHOTOCOPY ANSWER SHEET FOR ADDITIONAL PARTICIPANTS.
To obtain credits:
1. Read the entire course.
2. Complete this entire answer sheet in either pen or pencil.
3. Mark only one answer for each question.
4. A score of 70% will earn your credits.
5. Make check payable to Dental Learning, LLC.
OR
For Immediate results:
1. Read the entire course.
2. Go to www.dentallearning.net to take the tests online.
3. Answers can be submitted electronically or by fax at
732-303-0555 with credit card payment.
4. Answers can also be mailed to:
* Dental Learning, LLC
500 Craig Road, Floor One
Manalapan, NJ 07726
*If paying by credit card, please note:
Master Card | Visa | AmEx | Discover
*Account Number ______________________________
*Expiration Date _______________________________
The $49 charge will appear as Dental Learning, LLC
1. A B C D
2. A B C D
3. A B C D
4. A B C D
5. A B C D
6. A B C D
7. A B C D
8. A B C D
9. A B C D
10. A B C D
11. A B C D
12. A B C D
13. A B C D
14. A B C D
15. A B C D
16. A B C D
17. A B C D
18. A B C D
19. A B C D
20. A B C D
21. A B C D
22. A B C D
23. A B C D
24. A B C D
25. A B C D
26. A B C D
27. A B C D
28. A B C D
29. A B C D
30. A B C D
31. A B C D
32. A B C D
33. A B C D
34. A B C D
35. A B C D
36. A B C D
37. A B C D
38. A B C D
39. A B C D
40. A B C D
41. A B C D
42. A B C D
43. A B C D
44. A B C D
45. A B C D
46. A B C D
47. A B C D
48. A B C D
49. A B C D
50. A B C D
COURSE EVALUATION
Please evaluate this course using a scale of 5 to 1, where 5 is excellent and 1 is poor
1. To what extent were the course objectives accomplished overall? 5 4 3 2 1
2. Please rate your overall mastery of the educations objectives? 5 4 3 2 1
3. How would you rate the educational methods? 5 4 3 2 1
4. How do you rate the authors mastery of the topic? 5 4 3 2 1
5. Please rate the instructors effectiveness. 5 4 3 2 1
6. Do you feel the references were adequate? 5 4 3 2 1
7. Would you participate in a similar course? 5 4 3 2 1
8. Was any subject matter confusing please describe. 5 4 3 2 1
Fill in the circle of the appropriate answer that corresponds to the question on previous pages.
AGD Code: 148
If you have any questions,
please call Dental Learning,
LLC at 1-888-724-5230.
CE ANSWER FORM (E-mail address required for processing)
ALL FIELDS MARKED WITH
AN ASTERISK (*) ARE
REQUIRED
*Name: Title: Specialty:
*Address: *E-mail:
*City: *State: *Zip:
*Telephone: License renewal date: AGD Identifcation No.
Price: $49
To save $5 and get your verifcation form
immediately, go to www.dentallearning.net,
and type DLXXX, into the coupon feld.
Discounts will ONLY be applied to tests
taken online.
Save time and the environment by taking
this course online.
Instrument Processing for Infection Prevention
You might also like
- Dental AssistantDocument19 pagesDental AssistantMelissa Forbes80% (5)
- Dental Assisting Notes Dental Assistants Chairside Pocket GuideDocument188 pagesDental Assisting Notes Dental Assistants Chairside Pocket GuideIlhami GümüsNo ratings yet
- Review Questions and Answers For Dental Assisting PDFDocument275 pagesReview Questions and Answers For Dental Assisting PDFMansoor Malik92% (13)
- Managment of Medically Compromised PatientsDocument25 pagesManagment of Medically Compromised PatientsDemaagh seneNo ratings yet
- Dental Foundation Training Curriculum 2016Document46 pagesDental Foundation Training Curriculum 2016Rajitha Dilhan100% (1)
- DH Notes - Dental Hygienist's Chairside Pocket GuideDocument231 pagesDH Notes - Dental Hygienist's Chairside Pocket GuideHany L Hossainy100% (4)
- Certification Preparation For Dental Assisting B Bennett Et Al Lippincott 2012 BBSDocument178 pagesCertification Preparation For Dental Assisting B Bennett Et Al Lippincott 2012 BBSLeavatte100% (6)
- Dental Assistant Modules OverviewDocument62 pagesDental Assistant Modules OverviewReihan Kaur100% (1)
- Dental Assisting GuidelinesDocument22 pagesDental Assisting GuidelinestzuquinoNo ratings yet
- Dental Assisting ProgramsDocument4 pagesDental Assisting ProgramsJuan EstebanNo ratings yet
- Dental Assistant Practice ExamDocument5 pagesDental Assistant Practice ExamFaye Nervanna Alecha Alferez100% (8)
- Dental HygieneDocument56 pagesDental Hygienesohail shaikhNo ratings yet
- Periplus Education N0 Subject Isbn TitleDocument12 pagesPeriplus Education N0 Subject Isbn TitleMuhammad MuhammadNo ratings yet
- Ethics in Dentistry PDFDocument2 pagesEthics in Dentistry PDFEmilyNo ratings yet
- A Mindfulness Intervention For Children With Autism Spectrum DisorderDocument155 pagesA Mindfulness Intervention For Children With Autism Spectrum Disorderclaughlinsr4721No ratings yet
- Dental PersonnelDocument32 pagesDental PersonnelLucina San MateoNo ratings yet
- 16 Dental Instrument SetDocument6 pages16 Dental Instrument Setaang hilmiNo ratings yet
- Infection Prevention Control Manual For Dental Settinga1Document121 pagesInfection Prevention Control Manual For Dental Settinga1Almehey Nader0% (1)
- Infection Prevention Control Manual For Dental Settinga1Document121 pagesInfection Prevention Control Manual For Dental Settinga1Almehey Nader0% (1)
- Guidelines For Access CavityDocument8 pagesGuidelines For Access CavityAshri Ratnasari100% (2)
- Dental Assistant: Study GuideDocument22 pagesDental Assistant: Study GuideMansoor MalikNo ratings yet
- 13 Osha Infection ControlDocument78 pages13 Osha Infection ControlAnonymous c8G1bmIrNo ratings yet
- Professionalism and Ethics: A guide for dental care professionalsFrom EverandProfessionalism and Ethics: A guide for dental care professionalsNo ratings yet
- CHAPTER 1 Manual OperativeDocument27 pagesCHAPTER 1 Manual OperativeCassie Von PeenqNo ratings yet
- Dental Radiography 5th Iannucci Test BankDocument14 pagesDental Radiography 5th Iannucci Test BankSaifoqqNo ratings yet
- ABGD Written Study Questions 2007Document291 pagesABGD Written Study Questions 2007Almehey NaderNo ratings yet
- Test Bank For Pearsons Comprehensive Dental Assisting by TylerDocument10 pagesTest Bank For Pearsons Comprehensive Dental Assisting by Tylera254340512No ratings yet
- Intra Oral RadiographyDocument11 pagesIntra Oral RadiographyAnggreta Auriadini100% (1)
- OrthosisDocument35 pagesOrthosissinghmenkaNo ratings yet
- Dental Infection Control GuidelinesDocument77 pagesDental Infection Control GuidelinesMohamed KhaledNo ratings yet
- Dental Assistant Rev Jan 2016 v2Document7 pagesDental Assistant Rev Jan 2016 v2Netzao NetzaoNo ratings yet
- National Dental Hygiene Certification Examination Sample QuestionsDocument9 pagesNational Dental Hygiene Certification Examination Sample QuestionsJoyce Ann Laro Ola100% (2)
- Ethics Handbook For DentistsDocument14 pagesEthics Handbook For DentistsAlbert ArtandiNo ratings yet
- Dental Assistant Exam Content and References PDFDocument1 pageDental Assistant Exam Content and References PDFJashim Jumli II100% (1)
- Medical Emergencies in Dental OfficeDocument37 pagesMedical Emergencies in Dental Officeleozee100% (2)
- Dental Radiography & Infection Control QuizDocument12 pagesDental Radiography & Infection Control QuizFaye Nervanna Alecha AlferezNo ratings yet
- Exercises in Oral Radiographic InterpretationsDocument239 pagesExercises in Oral Radiographic InterpretationsSufaru Ciprian75% (4)
- Dental Assisting Sample TestDocument26 pagesDental Assisting Sample TestFaye Nervanna Alecha Alferez100% (1)
- Dental Assisting National Board (DANB) Exams Study GuideDocument20 pagesDental Assisting National Board (DANB) Exams Study GuideMcRee Learning CenterNo ratings yet
- Dental Practice AbbreviationsDocument52 pagesDental Practice AbbreviationsLee Redditt0% (2)
- Dental AssistingDocument3 pagesDental Assistingkenshinx100% (1)
- The Dental Foundation Interview Guide: With Situational Judgement TestsFrom EverandThe Dental Foundation Interview Guide: With Situational Judgement TestsNo ratings yet
- Journal Hydrodynamic Theory by Brnnstrm1986Document5 pagesJournal Hydrodynamic Theory by Brnnstrm1986Fifth TsuchikageNo ratings yet
- Cuspid Volume 1: Clinically Useful Safety Procedures in DentistryFrom EverandCuspid Volume 1: Clinically Useful Safety Procedures in DentistryNo ratings yet
- Dental Clinic Requirements ChecklistDocument12 pagesDental Clinic Requirements ChecklistArchanaShenoy100% (1)
- Dental Hygiene - Manual - 2013 Adex ExamDocument76 pagesDental Hygiene - Manual - 2013 Adex ExamMaria Mercedes LeivaNo ratings yet
- NATIONAL DENTAL ASSISTANT BOARDS (DANB): Passbooks Study GuideFrom EverandNATIONAL DENTAL ASSISTANT BOARDS (DANB): Passbooks Study GuideRating: 4 out of 5 stars4/5 (1)
- Medical Imaging TechniquesDocument8 pagesMedical Imaging TechniquesCora DoranNo ratings yet
- Review Questions and Answers For Dental Assisting - Revised Reprint, 2e by Mosby, Betty Ladley Finkbeiner CDA Emeritus BS MSDocument266 pagesReview Questions and Answers For Dental Assisting - Revised Reprint, 2e by Mosby, Betty Ladley Finkbeiner CDA Emeritus BS MSroz nejadiNo ratings yet
- Dental AssistantDocument4 pagesDental Assistantpravijohn28100% (1)
- A5 Risk Assessment in DentistryDocument16 pagesA5 Risk Assessment in DentistryJimena Chavez100% (4)
- Cuspid Volume 2: Clinically Useful Safety Procedures in DentistryFrom EverandCuspid Volume 2: Clinically Useful Safety Procedures in DentistryRating: 3 out of 5 stars3/5 (1)
- MammographyDocument27 pagesMammographyRohmatullah Anas100% (1)
- Viral Exanthems: Sahara Tuazan AbonawasDocument75 pagesViral Exanthems: Sahara Tuazan AbonawasMarlon Cenabre Turaja100% (1)
- Infection ControlDocument83 pagesInfection ControlAlmehey NaderNo ratings yet
- Drug Prescribing For DentistsDocument84 pagesDrug Prescribing For Dentistsmoheen_khanNo ratings yet
- Chapter 4 - Dental Anatomy (Essentials of Dental Assisting)Document28 pagesChapter 4 - Dental Anatomy (Essentials of Dental Assisting)mussanteNo ratings yet
- DentalDocument29 pagesDentalJase Phan100% (2)
- A Dentists Guide To Implantology PDFDocument42 pagesA Dentists Guide To Implantology PDFRetno Kanthi NingsihNo ratings yet
- HND Dental Nurse AssignmentDocument18 pagesHND Dental Nurse Assignmentandreeal8950% (8)
- Questions and Answers for Diploma in Dental Nursing, Level 3From EverandQuestions and Answers for Diploma in Dental Nursing, Level 3No ratings yet
- Child Development Mannualfinal-SinhalaDocument250 pagesChild Development Mannualfinal-SinhalaAshhara FazalNo ratings yet
- DENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideFrom EverandDENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideNo ratings yet
- Dental Instruments CHDocument20 pagesDental Instruments CHAhmed Tarek El-ShanawanyNo ratings yet
- Dental Instrument Identification and Tray Setup GuideDocument69 pagesDental Instrument Identification and Tray Setup GuideIndrani Das100% (2)
- CH 35 Dental Handpieces and Accessories3641Document32 pagesCH 35 Dental Handpieces and Accessories3641Suvasish Suvasish50% (2)
- OTC COURSES 2020 Information Booklet PDFDocument38 pagesOTC COURSES 2020 Information Booklet PDFMuhammad SajidNo ratings yet
- Lauren ResumeDocument3 pagesLauren Resumeapi-504789913No ratings yet
- Emergency Endodontic Classifications and ManagementDocument66 pagesEmergency Endodontic Classifications and ManagementAlmehey NaderNo ratings yet
- Working Length DeterminationDocument23 pagesWorking Length DeterminationAlmehey NaderNo ratings yet
- HottoothDocument75 pagesHottoothsalman azizNo ratings yet
- Clinical Guide To Endodontics 1 (Update 2009)Document6 pagesClinical Guide To Endodontics 1 (Update 2009)Almehey NaderNo ratings yet
- Dento - Alveolar InjuriesDocument34 pagesDento - Alveolar InjuriesAlmehey NaderNo ratings yet
- Managing Dentin HypersensitivityDocument10 pagesManaging Dentin HypersensitivityAlmehey NaderNo ratings yet
- OperativeDocument249 pagesOperativeAlmehey NaderNo ratings yet
- Ic ManualDocument29 pagesIc ManualAlmehey NaderNo ratings yet
- Acid EtchingDocument64 pagesAcid EtchingAlmehey NaderNo ratings yet
- New Class IDocument6 pagesNew Class IAlmehey NaderNo ratings yet
- New Class IDocument6 pagesNew Class IAlmehey NaderNo ratings yet
- Bleaching of Ally Treated TeethDocument12 pagesBleaching of Ally Treated TeethAlmehey NaderNo ratings yet
- Balanced ForceDocument29 pagesBalanced ForceAlmehey NaderNo ratings yet
- Diastema 2Document4 pagesDiastema 2Almehey NaderNo ratings yet
- Endodontic Diagnosis: February 19, 2009 Brett NagataniDocument53 pagesEndodontic Diagnosis: February 19, 2009 Brett NagataniSama ShayneHolicNo ratings yet
- IFDEA Dental Anatomy Educational Teaching ResourceDocument38 pagesIFDEA Dental Anatomy Educational Teaching ResourceaerowongNo ratings yet
- Basic Load (Individual) Veterinarian Field PackDocument3 pagesBasic Load (Individual) Veterinarian Field PackJohn MillerNo ratings yet
- Strategic PlanDocument84 pagesStrategic PlanAurutchat VichaiditNo ratings yet
- AsfaDocument28 pagesAsfaBhakti MehtaNo ratings yet
- Lawsuit Against Small Smiles Dental Center Aka Alabany Access Dental Center Et. Al.Document52 pagesLawsuit Against Small Smiles Dental Center Aka Alabany Access Dental Center Et. Al.DebHgnNo ratings yet
- 05thjan Assignment Abroad TimesDocument8 pages05thjan Assignment Abroad TimesSameer ShaikNo ratings yet
- Akupuntur 7Document9 pagesAkupuntur 7Ratrika SariNo ratings yet
- Don't Steal My Mind!: Extractive Introjection in Supervision and TreatmentDocument2 pagesDon't Steal My Mind!: Extractive Introjection in Supervision and TreatmentMatthiasBeierNo ratings yet
- Arriving at The Scene: Initial Response/Prioritization of Efforts 2.safety ProceduresDocument2 pagesArriving at The Scene: Initial Response/Prioritization of Efforts 2.safety ProceduresSumit GuptaNo ratings yet
- ق 4Document36 pagesق 4Zainab HasanNo ratings yet
- Wallen Et Al-2006-Australian Occupational Therapy JournalDocument1 pageWallen Et Al-2006-Australian Occupational Therapy Journal胡知行No ratings yet
- Blood Pressure Log 30Document2 pagesBlood Pressure Log 30Yousab KaldasNo ratings yet
- Medical Certificate Guidelines June 2012Document3 pagesMedical Certificate Guidelines June 2012wudthipanNo ratings yet
- Biology Contents - RPSC FSO by Food TecKnowDocument35 pagesBiology Contents - RPSC FSO by Food TecKnowRahul JainNo ratings yet
- PDFDocument2 pagesPDFMohammed FasilNo ratings yet
- PTP1 - Reading Test 5Document17 pagesPTP1 - Reading Test 5Anh DucNo ratings yet
- Legumes - AnOverview PDFDocument6 pagesLegumes - AnOverview PDFMayuri JagtapNo ratings yet
- 3.pleural Effusion Imaging - Overview, Radiography, Computed TomographyDocument32 pages3.pleural Effusion Imaging - Overview, Radiography, Computed TomographyAchmadRizaNo ratings yet
- Basic Principles of Pediatric Mechanical VentilationDocument39 pagesBasic Principles of Pediatric Mechanical VentilationNav KovNo ratings yet
- Thyroid and Antithyroid Drugs - PPTX - 20231126 - 103419 - 0000Document11 pagesThyroid and Antithyroid Drugs - PPTX - 20231126 - 103419 - 0000Vaishnavi SheteNo ratings yet
- C.V AfayoDocument4 pagesC.V AfayoAfayo RobertNo ratings yet
- Fa14 Concept Map 10-26-14 2Document2 pagesFa14 Concept Map 10-26-14 2api-270415831No ratings yet
- Drug Release Kinetics ModelsDocument7 pagesDrug Release Kinetics ModelsSajid Khan SadozaiNo ratings yet
- Resume Jurnal-Dessy Dwi H 201720401011160Document3 pagesResume Jurnal-Dessy Dwi H 201720401011160Pratiwi UmbohNo ratings yet