Professional Documents
Culture Documents
AQUA 2011 - Machine
Uploaded by
Portia ShilengeOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AQUA 2011 - Machine
Uploaded by
Portia ShilengeCopyright:
Available Formats
AnnualQueenstownUpdateinAnaesthesia,2011 TheAnaestheticMachineTheNextGeneration
41
41
THE ANAESTHETIC MACHINE THE NEXT GENERATION
Dr Andrew Love
North Shore Hospital,
Auckland
In the last 10 to 15 years we have seen a move from pneumatically controlled, mechanical anaesthetic machines
and ventilators, to electronic control of gas flow, gas mixing, vapour delivery and ventilation. Closed loop control of
end tidal concentration of oxygen, nitrous oxide and anaesthetic agent has become a practical reality, and
software is available to predict the future. Closed loop control of other aspects of patient physiology using actual
and surrogate markers has also been trialled.
In parallel, there have been aviation accidents where it appears that a contributing factor has been the level of
automated control of the aircraft and the suppositions and algorithms which drive the response of the machine to
the control inputs from the aviator in unusual or abnormal conditions.
The presentation will cover
The origins of anaesthetic machines
Where we are now in terms of technology
Closed loop control of anaesthesia and its limitations
The regulatory environment now and in the future
Where Have We Come From?
The earliest anaesthesia administration system was the so called rag and bottle technique where ether or
chloroform was dripped into a handkerchief held over the patients nose and mouth. One of the early attempts to
produce a machine to deliver gases and vapours with an integrated ventilator was described by Sykes in 1962.
Early Electronic Machines
The PhysioFlex machine was introduced into clinical practice in the late 1980s. It was a fully closed circuit
anaesthesia machine with electronic gas flow control, direct injection of anaesthetic agent into the circuit with
closed loop control of end tidal agent, inspired oxygen concentration and circuit volume. While it was a
revolutionary concept, it apparently had problems with the stability of end tidal agent control system with a degree
of wobble. The control of nitrous oxide levels was said to be inadequate.
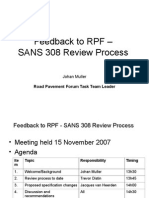
Figure 1. Change of inspired (solid line) and end-tidal (dashed line) sevoflurane in a PhysioFlex
TheAnaestheticMachineTheNextGeneration AnnualQueenstownUpdateinAnaesthesia,2011
42
closed circuit in seven patients when the end-tidal sevoflurane setting was changed from 1.0 to 3.0%
during maintenance of inhalational anaesthesia. Patients showing the slowest change indicated by
the light lines, patients showing the fastest change indicated by the heavy lines.
2
In the 1990s the Datex ADU was introduced with mechanical control of fresh gas flow, but with electronic
measurement of flow, and electronic control of agent delivery using the Aladdin Cassette. The availability of the
gas flow and vaporiser setting data, along with inspired and end tidal agent concentrations in the breathing
system, resulted in the development of a system which estimated the current effect site volatile concentration, and
provided predictions of future end tidal and effect site volatile concentrations.
Where Are We Now?
In parts of the third world, anaesthesia is administered using halothane delivered from draw over halothane
vaporisers with supplemental oxygen from oxygen concentrators, using ventilators designed to be driven by the
compressor of the concentrator. Volatile concentrations and anaesthetic depth is estimated using surrogate
markers such as pulse, blood pressure, movement and tearing.
In the developed world, anaesthesia is moving to automated control of a number of variables, including end tidal
agent concentration, inspired oxygen concentration, depth of anaesthesia, muscle relaxation, mean arterial
pressure (MAP).
Closed Loop Control in Anaesthesia
In open loop control of the anaesthetic agent or other variable, the anaesthetist takes information (variables) from
various monitors, and based on knowledge, experience and a mental model, adjusts the actuator (the vaporiser),
observes the results, and readjusts the actuator to bring the value(s) closer to the desired value, the set point.
In contrast to open loop systems, a closed loop controller (eg of end tidal agent) consists of a number of parts
1. The system which is controlled (the patient)
2. A sensor which measures the controlled variable (vapour analyser and end tidal agent)
3. A set point for the variable (the desired end tidal concentration, chosen and set by the anaesthetist)
4. An actuator which controls the administration of the agent (the vaporiser)
5. A controller (the brain), which contains an algorithm which converts the information received from the
sensor(s), the entered set point, and alters the actuator
6. A user interface, which allows input from the anaesthetist, and displays the controlled variable(s) and
possibly actuator setting
7. Some models may include an adaptor, which updates the model based on the response of the system to
initial control inputs
Examples of controller types
1. Proportional integral derivative (PID) controller
a. The difference between the set point and the measured variable is calculated. The output of the
controller is proportional to the difference, to the integral of the difference against time, and to the rate
of change of the difference (the differential)
b. These are commonly used in industry to control relatively simple systems
c. PID controller can be made to adapt to specific patient characteristics
2. Model based
a. Using knowledge of the pharmacokinetics and pharmacodynamics of a drug, a mathematical model
can be constructed which predicts physiological responses
b. Because of inter-patient variation, these models need to be designed to adapt to patient responses
3. Knowledge based using fuzzy logic or neural networks
Limitations of closed loop controllers
1. The variable controlled may be
a. Direct end tidal agent
AnnualQueenstownUpdateinAnaesthesia,2011 TheAnaestheticMachineTheNextGeneration
43
43
b. Surrogate marker - BIS for depth of anaesthesia
2. The controller needs to be stable under extreme conditions
3. There needs to be an ability to reject signal artefacts or noise in the monitored variable signal
4. The controller needs to be stable and not cause the variable controlled to oscillate around the set point, or
deviate from the set point
5. There must be limits to the output of the actuator to prevent over dosage
Advantages of closed loop control
1. Reduced anaesthetist work load
2. Better control of physiological variables
3. Decreased agent consumption using end tidal control
4. Possibly more rapid recovery
Disadvantages
1. Over reliance on automation and decreased vigilance
2. Unexpected and unusual response of the controller to unusual circumstances
3. There is a need for those using these automated systems to understand fully
a. The functional logic of the controller
b. Its limitations
c. Its behaviour in unusual or extreme circumstances
d. The need to maintain vigilance in spite of being on auto pilot
Current examples of closed loop control in anaesthesia
1. GE Aisys with control of end tidal agent and inspired oxygen as it relatively new in clinical use there is
relatively little in the literature on the Aisys. Intuitively it should decrease agent concentration in the hands
of those not used to closed circuit or very low flow anaesthesia, but in its present iteration it has a
mandatory minimum flow of 500ml, which is not true closed circuit anaesthesia
2. Drager Zeus with control of end tidal agent and inspired oxygen there is more literature on the Zeus,
and some studies suggest that its use in closed loop mode decreases agent consumption
Where Are We Going?
1. In the literature there are examples of the use of closed loop control for
a. Depth of anaesthesia including sedation
b. Analgesia
c. Muscle relaxation
d. Arterial pressure
e. Ventilation
2. Integrated Automated Control McSleepy is an experimental closed loop control system that monitors
depth of anaesthesia, nocioception and muscle relaxation, and administers doses of the appropriate
drugs as necessary
3. Predicting the future. Many of you will be aware of the work of Ross Kennedy and Richard French of
Christchurch in developing a system to guide volatile agent administration. Using data from the ADU of
fresh gas flow and vaporiser setting, and inspired and end tidal agent from the gas analyser of the S/5
monitor, it estimates effect site agent concentration and predicts end tidal agent concentrations for the
next 10 to 20 minutes. The introduction of the model has coincided with significant reductions in fresh gas
flow settings. It has also proved useful in teaching the practice of inhalational kinetics and low flow
The Regulatory Environment
The Government
Those of you who deal with the purchase of equipment will be aware of the necessity for WAND and TGA
certification. WAND is the Web Assisted Notification of Devices program run by Medsafe which requires all
TheAnaestheticMachineTheNextGeneration AnnualQueenstownUpdateinAnaesthesia,2011
44
medical devices to be notified. TGA is the Australian Therapeutic Goods Administration which serves a similar
function across the Tasman.
Recently our government and their Australian counterparts have announced a joint scheme for the regulation of
therapeutic goods (medicines, medical devices), the Australia New Zealand Therapeutic Products Agency, which
will absorb the current regulators Australia's Therapeutic Goods Administration and New Zealand's Medsafe
(ANZTPA; yet another MLA to remember). The aim is to create, over time, a joint regulatory scheme across both
countries [which] will safeguard public health and safety, while encouraging economic integration and benefitting
industry in both countries which will be absorb the two current regulators, Medsafe and the Australian TGA.
Whether this will make matters simpler remains to be seen.
The Australian and New Zealand College of Anaesthetists (ANZCA)
The College has published a new document Minimum Safety Requirements for Anaesthetic Machines for Clinical
Practice 2011 T3 (2011). It has recognised the hazards inherent in electronic anaesthetic machines in adding
point 4.3.1
4.3 An on/off switch, if present, must be protected from unintended activation.
4.3.1 Switching off an electronic anaesthetic machine during normal operation should require a
confirmatory step and/or the machine should display a warning of imminent shut-down.
The provisions with regard to machine obsolescence are also powerful tools in dealing with management who are
reluctant to replace aging and failing equipment.
Conclusion
We are in a time of interesting developments in the technology of anaesthesia delivery, and it is unclear which of
the innovations will become accepted into clinical practice. Some of these innovations may not add safety or
efficacy in proportion to their costs. We may well be developing more and more expensive ways of doing what we
do, and we need to retain a degree of scepticism with regard to innovations being presented to us, and avoid the
view that everything new is necessarily a good thing.
References
1. Sykes MK. The East-Radcliffe Ventilator adapted for Anaesthesia. BJA 1962; 34: 203a
2. Suzuki A et al, Evaluation of the PhysioFlex closed-circuit anaesthesia machine. European Journal of
Anaesthesiology 2000; 17: 359-363
3. Tenbrinck R, Hahn MR, Gltuna I, Hofland J, van Dijk G, Baumert J, Hecker K, Erdmann W. The first
clinical experiences with xenon. Int Anesthesiol Clin. 2001; 39(2): 29-42.
4. Gentilini A, Frei CW, Glattfedler AH, Morari M, Sieber TJ, Wymann R, Schnider TW, Zbinden AM.
Multitasked Closed-Loop Control in Anesthesia. IEEE Engineering In Medicine And Biology;
January/February 2001
5. Struys MM, De Smet T, Mortier EP. Closed-loop control of anaesthesia. Curr Opin Anaesthesiol. 2002
Aug; 15(4): 421-5
6. Struys MM, De Smet T, Mortier EP. Closed loops in anaesthesia. Best Practice and Research Clinical
Anaesthesiology 2006; 20(1): 211-20
7. Hemmerling TM. Automated anesthesia. Curr Opin Anaesthesiol 2009; 22: 757-63
8. O'Hara DA, Bogen DK, Noordergraaf A. The use of computers for controlling the delivery of anesthesia.
Anesthesiology 1992; 77: 563-81
9. Fields AM, Fields KM, Cannon JW. Closed-loop systems for drug delivery. Current Opinion in
Anesthesiology 2008; 21: 446-51
10. Kennedy RR, French RA. The development of a system to guide volatile anaesthetic administration.
Anaesth Intensive Care 2011; 39: 182-90
11. Medsafe. Medical Devices User Guide for NZ WAND (Web Assisted Notification of Devices) Version 2; 1
February 2010
12. Australian and New Zealand College of Anaesthetists (ANZCA) 2011; T3: Minimum Safety Requirements
for Anaesthetic Machines for Clinical Practice
AnnualQueenstownUpdateinAnaesthesia,2011 TheAnaestheticMachineTheNextGeneration
45
45
13. Bureau dEnqutes et dAnalyses pour la scurit de laviation civile. Report: Accident on 27 November
2008 off the coast of Canet-Plage (66) to the Airbus A320-232 registered D-AXLA operated by XL
Airways Germany 2011
TheAnaestheticMachineTheNextGeneration AnnualQueenstownUpdateinAnaesthesia,2011
46
You might also like
- Suitable Pumps For GasolineDocument5 pagesSuitable Pumps For GasolinePortia ShilengeNo ratings yet
- UOP Reforming Solutions For .Improved Profits PaperDocument32 pagesUOP Reforming Solutions For .Improved Profits PaperstevemetroNo ratings yet
- 12 Chapter3 Section4 Oil Refining Industry Page193 220Document26 pages12 Chapter3 Section4 Oil Refining Industry Page193 220Muhammad FarooqNo ratings yet
- Fluid Mechanics PresentationDocument158 pagesFluid Mechanics PresentationPortia ShilengeNo ratings yet
- 7 Flow of Compressible FluidsDocument27 pages7 Flow of Compressible FluidsPortia ShilengeNo ratings yet
- Caracteristicas Normas ASME B31Document3 pagesCaracteristicas Normas ASME B31darthneoNo ratings yet
- Presentations Oil Refinery ProcessesDocument36 pagesPresentations Oil Refinery ProcessesGururaj SreepatharaoNo ratings yet
- Fluid Mechanics PresentationDocument158 pagesFluid Mechanics PresentationPortia ShilengeNo ratings yet
- 2011-03 Head Losses Calculations PDFDocument44 pages2011-03 Head Losses Calculations PDFAnastasia Monica KhunniegalshottestNo ratings yet
- ECO2SA W2E Facility Draft Scoping Report For PPP 30 May 2012Document99 pagesECO2SA W2E Facility Draft Scoping Report For PPP 30 May 2012Portia ShilengeNo ratings yet
- Non Newtonian FluidsDocument12 pagesNon Newtonian FluidsPortia ShilengeNo ratings yet
- Solved Problems Samples in Fluid Flow PDFDocument10 pagesSolved Problems Samples in Fluid Flow PDFRichard Obinna100% (1)
- Cive1400 2000 01 - v2Document14 pagesCive1400 2000 01 - v2naefmubarakNo ratings yet
- Chapter 11Document36 pagesChapter 11Hamza FayyazNo ratings yet
- Lecture 6Document42 pagesLecture 6Anonymous 9R53UyNo ratings yet
- 2014 Nua301t Assessment 1 - MemoDocument4 pages2014 Nua301t Assessment 1 - MemoPortia ShilengeNo ratings yet
- 4 Flow MeasurementsDocument19 pages4 Flow MeasurementsPortia ShilengeNo ratings yet
- Conservation Laws: Control-Volume Approach: M Total Mass (KG) of A Within The System at Any TimeDocument8 pagesConservation Laws: Control-Volume Approach: M Total Mass (KG) of A Within The System at Any TimePortia ShilengeNo ratings yet
- Assignment 1-2013Document3 pagesAssignment 1-2013Portia ShilengeNo ratings yet
- Cive1400 200304 PDFDocument17 pagesCive1400 200304 PDFMohd Nazri SalimNo ratings yet
- Milestones Achieved: Viscous Flow in Pipes ??Document74 pagesMilestones Achieved: Viscous Flow in Pipes ??Portia ShilengeNo ratings yet
- Fluid PropertiesDocument32 pagesFluid Propertiesjmartinezmo100% (1)
- 2016 Heat and Mass Transfer Practical ManualDocument8 pages2016 Heat and Mass Transfer Practical ManualPortia ShilengeNo ratings yet
- Laminar Flow and Frictional Pressure DropDocument35 pagesLaminar Flow and Frictional Pressure DropsyedmuhammadtariqueNo ratings yet
- 15 Johan MullerDocument22 pages15 Johan MullerPortia ShilengeNo ratings yet
- Chapter 11Document36 pagesChapter 11Hamza FayyazNo ratings yet
- p2 Cyclone Eff ProjctDocument12 pagesp2 Cyclone Eff ProjctPortia ShilengeNo ratings yet
- Experiment Report: Characterizing Resonant Series RLC Circuits Using LabviewDocument15 pagesExperiment Report: Characterizing Resonant Series RLC Circuits Using LabviewPortia ShilengeNo ratings yet
- Optimization of Ball Mill Lifter Profiles and Determination of Top Ball SizeDocument15 pagesOptimization of Ball Mill Lifter Profiles and Determination of Top Ball SizePortia ShilengeNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Series C Fieldbus Interface Module Users Guide EPDOC X125 en 432Document490 pagesSeries C Fieldbus Interface Module Users Guide EPDOC X125 en 432TohidflaNo ratings yet
- Buck Converter Controlled by Arduino UnoDocument5 pagesBuck Converter Controlled by Arduino Unohamparan nightwatchNo ratings yet
- CV Dion Hendra Wisudana Sales EngineerDocument4 pagesCV Dion Hendra Wisudana Sales EngineerAri SuprayogiNo ratings yet
- Northwestern Polytechnical University Graduate Degree Dissertation Title Selection Report FormDocument14 pagesNorthwestern Polytechnical University Graduate Degree Dissertation Title Selection Report Formanna100% (1)
- DC Motor Speed Control - 2Document8 pagesDC Motor Speed Control - 2ravsreeNo ratings yet
- Water Level Control SytemDocument3 pagesWater Level Control SytemKaung Thant MinnNo ratings yet
- CSTR Temperature Control Using IMC-PIDDocument29 pagesCSTR Temperature Control Using IMC-PIDS Kiong TingNo ratings yet
- Performance Evaluation of Fuzzy Logic and PI Controller Based UPFC For Power Quality ImprovementDocument8 pagesPerformance Evaluation of Fuzzy Logic and PI Controller Based UPFC For Power Quality ImprovementSiraj PashaNo ratings yet
- Motion At005 - en PDocument112 pagesMotion At005 - en PNelsonNo ratings yet
- Pneumatic GripperDocument52 pagesPneumatic GripperretechNo ratings yet
- Gyro Position Control - Student ManualDocument55 pagesGyro Position Control - Student ManualBruno Martins Leite0% (1)
- LabVIEW HandoutDocument52 pagesLabVIEW HandoutYatheesh KaggereNo ratings yet
- Pid ProjectDocument5 pagesPid ProjectroydebopriyaNo ratings yet
- GS OverviewDocument51 pagesGS OverviewMuhammad AmjadNo ratings yet
- Control System Design Process by VisSimDocument6 pagesControl System Design Process by VisSimSreedhar MadichettyNo ratings yet
- EDC16 TranslDocument11 pagesEDC16 TranslFlorent Morel100% (1)
- Cn32Pt, Cn16Pt, Cn16Ptd, Cn8Pt, Cn8Ptd, Cn8Ept: Temperature & Process ControllersDocument79 pagesCn32Pt, Cn16Pt, Cn16Ptd, Cn8Pt, Cn8Ptd, Cn8Ept: Temperature & Process Controllerscraigorio616No ratings yet
- CDVR CommisioningDocument47 pagesCDVR CommisioningCandiano PopescuNo ratings yet
- Aluminium Alloy 3-Segment Soldering StationDocument4 pagesAluminium Alloy 3-Segment Soldering StationSyed Khawar MukhtarNo ratings yet
- Load Frequency Control of Hydro-Thermal System With Fuzzy Logic Controller Considering Boiler DynamicsDocument5 pagesLoad Frequency Control of Hydro-Thermal System With Fuzzy Logic Controller Considering Boiler DynamicsSudhir KumarNo ratings yet
- 450-4000 Ton Two-Platen Injection Molding MachinesDocument8 pages450-4000 Ton Two-Platen Injection Molding MachinesDenny BayuajiNo ratings yet
- 40 5456 - Books Catalog - 2016 WEBDocument40 pages40 5456 - Books Catalog - 2016 WEBJeanfranco Jordano Zarzosa OrtizNo ratings yet
- Prelab3 SolutionDocument8 pagesPrelab3 Solutionksajj100% (1)
- Electrical Operation Manual 2 ECS Control System Plant Name: Electrical Standard Contract NumberDocument22 pagesElectrical Operation Manual 2 ECS Control System Plant Name: Electrical Standard Contract NumberTuấnNo ratings yet
- Mm440 Parameter ListtDocument328 pagesMm440 Parameter ListtDjordje JovanovicNo ratings yet
- Sensorless BLDC Control With Back-EMF FilteringDocument28 pagesSensorless BLDC Control With Back-EMF FilteringRomeo Đạp Xíck LôNo ratings yet
- Udc 3300Document118 pagesUdc 3300chuyNo ratings yet
- Lynkurs Prosessregulering (Crash Course Process Control)Document20 pagesLynkurs Prosessregulering (Crash Course Process Control)tryanti sinambelaNo ratings yet
- Temp Control of ExtruderDocument15 pagesTemp Control of ExtruderMoksh PrasadNo ratings yet