Professional Documents
Culture Documents
Lap Cholecystectomy Better Than OC
Uploaded by
mydewyboyOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lap Cholecystectomy Better Than OC
Uploaded by
mydewyboyCopyright:
Available Formats
ORIGINAL ARTICLES
Laparoscopic Surgery Is Associated With a Lower Incidence of Venous Thromboembolism Compared With Open Surgery
Ninh T. Nguyen, MD, Marcelo W. Hinojosa, MD, Christine Fayad, BS, Esteban Varela, MD, MPH, Viken Konyalian, MD, Michael J. Stamos, MD, and Samuel E. Wilson, MD
Background: Although laparoscopy now plays a major role in most general surgical procedures, little is known about the relative risk of venous thromboembolism (VTE) after laparoscopic compared with open procedures. Objective: To compare the incidence of VTE after laparoscopic and open surgery over a 5-year period. Patients and Interventions: Clinical data of patients who underwent open or laparoscopic appendectomy, cholecystectomy, antireux surgery, and gastric bypass between 2002 and 2006 were obtained from the University HealthSystem Consortium Clinical Database. The principal outcome measure was the incidence of venous thrombosis or pulmonary embolism occurring during the initial hospitalization after laparoscopic and open surgery. Results: During the 60-month period, a total of 138,595 patients underwent 1 of the 4 selected procedures. Overall, the incidence of VTE was signicantly higher in open cases (271 of 46,105, 0.59%) compared with laparoscopic cases (259 of 92,490, 0.28%, P 0.01). Our nding persists even when the groups were stratied according to level of severity of illness. The odds ratio (OR) for VTE in open procedures compared with laparoscopic procedures was 1.8 95% condence interval (CI) 1.32.5. On subset analysis of individual procedures, patients with minor/moderate severity of illness level who underwent open cholecystectomy, antireux surgery, and gastric bypass had a greater risk for developing perioperative VTE than patients who underwent laparoscopic cholecystectomy (OR: 2.0; 95% CI: 1.23.3; P 0.01), antireux surgery (OR: 24.7; 95% CI: 2.6 580.9; P 0.01), and gastric bypass (OR: 3.4; 95% CI: 1.8 6.5; P 0.01). Conclusions: Within the context of this large administrative clinical data set, the frequency of perioperative VTE is lower after laparoscopic compared with open surgery. The ndings of this study can
From the Department of Surgery, University of California, Irvine Medical Center, Orange, CA. Presented at the 78th annual meeting of The Pacic Coast Surgical Association in Kohala Coast, Hawaii, on February 18, 2007. The information contained in this article was based on the clinical database provided by the University HealthSystem Consortium. Ninh T. Nguyen, Michael J. Stamos, and Samuel E. Wilson are the members of PCSA. Reprints: Ninh T. Nguyen, MD, Department of Surgery, 333 City Building West, Suite 850, Orange, CA 92868. E-mail: ninhn@uci.edu. Copyright 2007 by Lippincott Williams & Wilkins ISSN: 0003-4932/07/24606-1021 DOI: 10.1097/SLA.0b013e31815792d8
provide a basis to help surgeons estimate the risk of VTE and implement appropriate prophylaxis for patients undergoing laparoscopic surgical procedures. (Ann Surg 2007;246: 10211027)
enous thromboembolism (VTE) is a major cause of morbidity and mortality in patients undergoing gastrointestinal surgery. It is estimated that 600,000 patients developed pulmonary embolism (PE) each year in the United States.1 The incidence of fatal PE ranges from 0.1% to 0.8% in patients undergoing elective general surgical procedures.2 Since the early 1990s, laparoscopy has revolutionized the eld of gastrointestinal surgery. The acceptance rate for laparoscopic surgery has been overwhelming for general surgical procedures such as cholecystectomy, appendectomy, solid organ removal, antireux surgery, and even Roux-en-Y gastric bypass for the treatment of morbid obesity. Although well accepted as the procedure of choice for many general surgical procedures, the incidence of VTE after laparoscopic gastrointestinal procedures is not well dened. Certain factors associated with laparoscopic surgery, such as early ambulation and a reduction in postoperative hypercoagulability, may reduce the risk of VTE.3,4 However, intraoperative factors associated with laparoscopic surgery have been shown to possibly increase the risk of VTE. The use of intraoperative pneumoperitoneum and reverse Trendelenburg position are independent factors for reduction of femoral venous ow and, combined with prolonged operative times associated with laparoscopic procedures, may increase the risk for VTE.5,6 Although the true incidence of VTE after laparoscopic compared with open surgery is unknown, most investigators recommend that thromboprophylaxis in laparoscopic surgery should be the same as those for conventional open surgery.7 Understanding the relative risk for development of VTE after laparoscopic compared with open surgery will help surgeons with the selection of appropriate thromboprophylaxis for their laparoscopic procedures. There have been no large studies examining the incidence of VTE after laparoscopic compared with open surgery. The objective of this study was to determine the incidence of clinically evident
Annals of Surgery Volume 246, Number 6, December 2007
1021
Nguyen et al
Annals of Surgery Volume 246, Number 6, December 2007
VTE during the initial hospitalization after laparoscopic compared with open surgery for 4 commonly performed gastrointestinal surgical proceduresappendectomy, cholecystectomy, antireux surgery, and Roux-en-Y gastric bypass.
proval for the use of the UHC patient-level data in this study was obtained from the Institutional Review Board of the University of California, Irvine Medical Center and the UHC.
Study Cohort
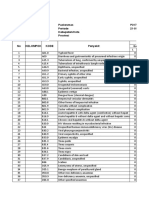
We analyzed the UHC hospital discharge records of all patients who were 18 years or older and who underwent 1 of 4 commonly performed gastrointestinal proceduresappendectomy, cholecystectomy, antireux surgery, and Rouxen-Y gastric bypass. Hospital discharge records for appendectomy and cholecystectomy were reviewed between January 1, 2002 and December 31, 2006 and records for antireux surgery and gastric bypass cases were reviewed between October 1, 2004 and December 31, 2006. The specic ICD-9 procedure code for laparoscopic gastric bypass only rst became available on October 1, 2004. All procedures were performed on an inpatient basis. Unfortunately, there is no information available on the use or nonuse of thromboprophylaxis or about the type (mechanical or antithrombotics) and duration of prophylaxis. Analysis of the 4 gastrointestinal procedures required the use of appropriate diagnosis and procedural codes as specied by the International Classication of Diseases, 9th Revision, Clinical Modication (ICD-9-CM). These 4 procedures were selected because they have both the laparoscopic and open ICD-9 procedural codes for their respective procedures. The ICD9-CM diagnosis and procedure codes for the 4 procedures are listed in Table 1. For appendectomy, the principal ICD-9 diagnosis codes for acute appendicitis and perforated appendicitis were used. Perforated appendicitis included a subcategory for generalized peritonitis or peritoneal abscess. For cholecystectomy, the principal ICD-9 diagnosis codes for cholelithiasis, acute cholecystitis, and chronic cholecystitis were used. We analyzed elective and urgent/emergent procedures for appendectomy and cholecystectomy groups. For antireux surgery, the principal ICD-9 diagnosis codes for esophagitis, esophageal reux, and Barrett esophagus were used. For gastric bypass, the principal ICD-9 diagnosis codes for obesity and morbid obesity were used, which included a subcategory of obesity and a subclassication of morbid
MATERIALS AND METHODS Discharge Data Set
The University HealthSystem Consortium (UHC) database is an administrative, clinical, and nancial database that provides benchmark measures on the utilization of health care resources for the purpose of comparative data analysis between academic institutions. The UHC database is a collection of patient-level, discharge-abstracted data from academic health centers and afliate community hospitals. It contains discharge information on inpatient hospital stay including patient characteristics, length of stay, overall and specic postoperative morbidity, and observed and expected (riskadjusted) in-hospital mortality. One of the benets of the UHC Clinical Database is the risk-adjusted data for comparison of institutions. To accomplish risk adjustment, the UHC uses regression-modeling techniques in combination with 3M Health Information Systems, Agency for Healthcare Research and Quality comorbidity software, and the UHC complication proler to assign a severity of illness level, and assign an expected length of stay, costs, and probability of mortality to every patient in the database. The assignment of severity of illness level is based on a combination of principal and secondary diagnoses to dene different levels of severity and complexity of treatment. The 4 severity of illness categories are minor, moderate, major, and extreme severity. For example, comorbidities such as diabetes would be categorized as moderate severity and recent myocardial infarction as extreme severity. Complication is dened as the percentage of patients who developed the particular complication before being discharged from the hospital. The UHC database has no information available on complications occurring after discharge, even if the complication occurred within 30 days from the date of surgery. Length of stay was dened as the period from the index procedure to hospital discharge. Ap-
TABLE 1. ICD-9-CM Diagnosis and Procedure Codes Used to Define Laparoscopic and Open Procedures
Principal Diagnosis Acute appendicitis Perforated appendicitis Cholelithiasis Acute cholecystitis Chronic cholecystitis Esophageal reux Esophagitis Barrett esophagus Morbid obesity ICD-9-CM 540, 540.9, 541, 542 540.0, 540.1 574.2, 574.20, 574.2 574.0, 574.00, 574.01, 575.0, 571.2 574.10, 575.11, 574.1 530.81 530.10, 530.11, 530.12, 530.19 530.85 278.0, 278.01, 278.00 Principal Procedure Laparoscopic appendectomy Open appendectomy Laparoscopic cholecystectomy Open cholecystectomy ICD-9-CM 47.01 47.0, 47.09 51.23 51.22, 51.21
Laparoscopic antireux surgery Open antireux surgery
44.67 44.65, 44.66
Laparoscopic gastric bypass Open gastric bypass
44.38 44.31, 44.39
1022
2007 Lippincott Williams & Wilkins
Annals of Surgery Volume 246, Number 6, December 2007
Incidence of Venous Thromboembolism After Surgery
obesity. The principal ICD-9 procedure codes for open Rouxen-Y gastric bypass included a subcategory of gastroenterostomy without gastrectomy and a subclassication of high gastric bypass and the principal ICD-9 procedure code for laparoscopic Roux-en-Y gastric bypass included a subcategory of gastroenterostomy without gastrectomy and a subclassication laparoscopic gastroenterostomy. To increase the homogeneity of the cohort, the diagnosis related group (DRG) for operative treatment of obesity (DRG 288) was also used to examine the data for gastric bypass. For antireux surgery and gastric bypass surgery, we only analyzed elective procedures; patients undergoing urgent and emergent procedures were excluded.
nous thrombosis (classied according to DRG) were excluded.
Statistical Analysis
We compared patient characteristics (age, sex, race, and severity class), length of hospital stay, overall rate of VTE after laparoscopic versus open surgery, and the individual rate of VTE after laparoscopic versus open appendectomy, cholecystectomy, antireux surgery, and gastric bypass. The rate of VTE after laparoscopic versus open surgery was also examined according to the level of severity of illness. Data are expressed as mean SD. Differences in patient characteristics and VTE between laparoscopic versus open group were analyzed using Fisher exact test or the Pearsons 2 test. Univariate analysis was performed and the 95% condence interval (CI) of the odds ratio (OR) was obtained. Continuous variables were compared using Student t tests. Statistical analysis was performed using Epi Info statistical software, version 3.3.2 (CDC, Atlanta, GA). A P value of less than 0.05 was considered signicant.
Definition of Outcomes
The overall rate of venous thrombosis and PE after laparoscopic and open surgery for the 4 surgical procedures and the individual rate of VTE after appendectomy, cholecystectomy, antireux surgery, and gastric bypass were examined. The diagnosis of venous thrombosis and PE during the hospitalization for laparoscopic and open surgery was based on the presence of a secondary diagnosis of an ICD-9 CM code for venous thrombosis and/or PE. Patients with primary diagnosis of phlebitis, thrombophlebitis, PE, or ve-
RESULTS
From 2002 to 2006 a total of 138,595 patients, 84,650 of whom were female (61%), underwent 1 of the 4 selected
TABLE 2. Summary of Demographics of Patients Undergoing Open Versus Laparoscopic Appendectomy, Cholecystectomy, Antireflux Surgery, and Gastric Bypass Operations, 2002 to 2006
Open Procedure* Total No. cases Female gender, No. (%) Age, No. (%) 1830 yr 3150 yr 5164 yr 65 yr Race, No. (%) White African American Severity of illness, No. (%) Minor Moderate Major Extreme Admission status, No. (%) Elective Urgent Emergency Length of hospital stay (days) Appendectomy Cholecystectomy Antireux surgery Gastric bypass 46,105 22,342 (48.5) 12,180 (26.3) 17,799 (38.4) 9530 (20.5) 6857 (14.8) 26,951 (58.1) 6211 (13.4) 22,729 (49.0) 18,415 (39.7) 3876 (8.4) 1347 (2.9) 11,265 (24.3) 7452 (16.1) 27,650 (59.6) 3.4 3.0 7.2 6.9 3.9 5.0 4.2 6.9 Laparoscopic Procedure* 92,490 62,308 (67.4) 22,868 (24.7) 38,963 (42.0) 18,799 (20.3) 12,089 (13.0) 55,292 (59.6) 12,001 (12.9) 54,660 (59.0) 32,065 (34.6) 5058 (5.5) 935 (1.0) 32,451 (35.0) 12,640 (13.6) 47,628 (51.4) 2.2 2.5 3.3 4.3 2.2 2.3 2.7 3.0 P 0.01 0.01 0.01 0.2 0.01 0.01 0.02 0.01 0.01 0.01 0.01 0.01 0.01 0.01 0.01 0.04 0.01 0.01
*Includes appendectomy, cholecystectomy, antireux surgery, and gastric bypass. 2 , Fisher exact test, or Student t tests, where applicable. Includes appendectomy and cholecystectomy only.
2007 Lippincott Williams & Wilkins
1023
Nguyen et al
Annals of Surgery Volume 246, Number 6, December 2007
procedures. As shown in Table 2, 92,490 patients (67%) had laparoscopic surgery and 46,105 patients underwent open surgery. The proportion of females was higher in the laparoscopic group (67% vs. 48%, P 0.01), as was the proportion of patients with a minor severity of illness level (59% vs. 49%, P 0.01). The age distribution was highest for patients grouped between 31 and 50 years (42% for laparoscopic and 38% for open). The proportion of white was higher for the laparoscopic group whereas the proportion of African Americans was higher in the open group. The length of stay was signicantly shorter for laparoscopic operations compared with open operations for all 4 procedures. Overall, VTE was diagnosed during the index hospitalization in 259 of 92,490 (0.28%) laparoscopic cases and 271
of 46,105 (0.59%) open cases (Fig. 1). Univariate analysis showed that open surgery was a signicant factor for development of VTE even when stratied according to different level of severity of illness; for minor/moderate severity of illness level the OR was 1.83 (95% CI: 1.322.54) and for major/extreme severity of illness level the OR was 1.31 (95% CI: 1.06 1.62). The incidence of VTE after laparoscopic and open appendectomy is listed in Figure 2. Laparoscopic appendectomy was associated with a lower rate of VTE compared with open appendectomy (0.11% vs. 0.28%, P 0.01); however, the association did not persist when the analysis was performed according to different level of severity of illness. The incidence of VTE after laparoscopic and open cholecystectomy is listed in Figure 3. Laparoscopic cholecys-
FIGURE 1. Overall incidence of VTE in patients who underwent open versus laparoscopic appendectomy, cholecystectomy, antireflux surgery, and gastric bypass operations, and stratified by severity of illness level, 2000 2006. *P 0.01; odds ratio (95% confidence interval) for overall group was 2.09 (95% CI: 1.76 2.49), for minor/moderate severity of illness level the OR was 1.83 (95% CI: 1.322.54), and for major/extreme severity of illness level the OR was 1.31 (95% CI: 1.06 1.62).
FIGURE 3. Incidence of VTE in patients who underwent open versus laparoscopic cholecystectomy, overall, and by severity of illness level, 20022006. *P 0.01; P 0.02; odds ratio (95% confidence interval) for cholecystectomy group was 2.89 (95% CI: 2.313.56), for minor/moderate severity of illness level the OR was 1.99 (95% CI: 1.20 3.27), and for major/extreme severity of illness level the OR was 1.35 (95% CI: 1.04 1.74).
FIGURE 2. Incidence of VTE in patients who underwent open versus laparoscopic appendectomy, overall, and by severity of illness level, 20022006. *P 0.05; odds ratio (95% confidence interval) for appendectomy group was 2.44 (95% CI: 1.54 3.87), for minor/moderate severity of illness level the OR was 1.79 (95% CI: 0.823.97), and for major/extreme severity of illness level the OR was 1.60 (95% CI: 0.89 2.90).
FIGURE 4. Incidence of VTE in patients who underwent open versus laparoscopic antireflux surgery, overall, and by severity of illness level, 2004 2006. *P 0.01; odds ratio (95% confidence interval) for antireflux surgery group was 11.78 (95% CI: 1.86 92.66), for minor/moderate severity of illness level the OR was 24.66 (95% CI: 2.61580.87), and for major/extreme severity of illness level the OR was 0.0 (95% CI: 0 24.88). 2007 Lippincott Williams & Wilkins
1024
Annals of Surgery Volume 246, Number 6, December 2007
Incidence of Venous Thromboembolism After Surgery
FIGURE 5. Incidence of VTE in patients who underwent open versus laparoscopic gastric bypass, overall, and by severity of illness level, 2004 2006. *P 0.01; odds ratio (95% confidence interval) for gastric bypass group was 2.58 (95% CI: 1.68 3.94), for minor/moderate severity of illness level the OR was 3.37 (95% CI: 1.76 6.45), and for major/ extreme severity of illness level the OR was 0.87 (95% CI: 0.48 1.58).
tectomy was associated with a lower rate of VTE compared with open cholecystectomy (0.36% vs. 1.03%, P 0.01) and persisted when stratied according to different severity of illness level; for minor/moderate severity of illness level the OR was 1.99 (95% CI: 1.20 3.27) and for major/extreme severity of illness level the OR was 1.35 (95% CI: 1.04 1.74). The incidence of VTE after laparoscopic and open antireux surgery is listed in Figure 4. Laparoscopic antireux surgery was associated with a lower rate of VTE compared with open antireux surgery (0.09% vs. 1.1%, P 0.01) and persisted when stratied according to minor/moderate severity of illness level with an OR of 24.66 (95% CI: 2.61580.87). The higher incidence of VTE in the laparoscopic antireux surgery group within the category of major/ extreme severity of illness did not reach statistical signicance between groups because of the small number of patients within this category (n 21 for open and n 29 for laparoscopic). The incidence of VTE after laparoscopic and open gastric bypass is listed in Figure 5. Laparoscopic gastric bypass was associated with a lower rate of VTE compared with open gastric bypass (0.30% vs. 0.78%, P 0.01) and persisted when stratied according to minor/moderate severity of illness level with an OR of 3.37 (95% CI: 1.76 6.45). Although the incidence of VTE seems to be higher in the laparoscopic gastric bypass group within the category of major/extreme severity of illness, we were not able to nd statistical signicance between groups (4.90% for laparoscopic vs. 4.28% for open, OR 0.86).
DISCUSSION
The relative risk of VTE after laparoscopic surgery compared with open surgery is unknown. Certain investigators suggest that the risk for venous thrombosis and PE after laparoscopic surgery may be higher than after open surgery because of the intraoperative use of pneumoperitoneum with its effects on femoral venous ow.6 To date, there have been
2007 Lippincott Williams & Wilkins
no large studies examining the incidence of VTE after laparoscopic compared with open surgery.7,8 In this study, we used the UHC Clinical Database to analyze the incidence of VTE in a large cohort of patients who underwent laparoscopic compared with open appendectomy, cholecystectomy, antireux surgery, and Roux-en-Y gastric bypass. These 4 gastrointestinal procedures were selected because of the availability of ICD-9 codes for open and laparoscopic procedures. We found an overall lower incidence of VTE after laparoscopic compared with open procedures (0.28% vs. 0.59%, respectively). Although there are differences in the severity of illness level between the 2 groups, the incidence of VTE after laparoscopic surgery continues to be lower than that of open surgery even when the data are stratied according to the level of severity of illness. On examination of each of the 4 specic operations, the incidence of VTE is again lower after the laparoscopic operation compared with the open operation, although these differences were not signicant for appendectomy. We conclude from this study that laparoscopic operation is associated with a lower incidence of VTE compared with open operation and that laparoscopy in itself should not be viewed as an additional risk factor during risk assessment for venous thrombosis. Factors predisposing to VTE during open surgical procedure include deciency of Antithrombin III, protein C and S, and dysbrinogenemia. Other risk factors include advanced age, obesity, previous history of VTE, cancer, lengthy operation (2 hours) and immobility.9 In addition, laparoscopic procedures have additional risk factors for development of VTE, which include the use of pneumoperitoneum, reverse Trendelenburg position, and possibly a prolonged operative time during the learning curve of the procedure. Consideration of these possible risk factors has led some investigators to hypothesize that patients undergoing laparoscopic surgery may be at higher risk for development of VTE compared with open surgery.10,11 Results from our study, however, do not support this hypothesis. Ours result conclusively show that laparoscopic surgery is not associated with a higher incidence of clinically symptomatic venous thrombosis or PE compared with open surgery during the hospitalization. In fact, comparison of the 2 groups even after risk adjustment showed that the odds of development of an inpatient VTE is 1.8 times higher after open operation compared with laparoscopic operation. The ndings from our study can be used by surgeons to assess more accurately the individual patients risk for perioperative VTE. A common risk assessment method has been reported by Caprini.9 In this risk assessment model, Caprini stratied the patients into 4 categories, low, moderate, high, and highest, based on multiple factors. One of the listed risk factors is laparoscopic surgery (45 minutes), which receive 2 points. Our study examined antireux surgery and Rouxen-Y gastric bypass, which normally have an operative time longer than 45 minutes. Despite the longer operative time, laparoscopic gastric bypass and antireux surgery were associated with a lower incidence of VTE. According to Caprini thrombosis risk factor assessment,9 a hypothetical case study of a 39-year-old morbidly obese female undergoing
1025
Nguyen et al
Annals of Surgery Volume 246, Number 6, December 2007
open gastric bypass would have a minimum risk factor score of 3 (1 for obesity and 2 for major surgery) whereas the same patient undergoing laparoscopic gastric bypass would have a minimum risk factor score of 5 (1 for obesity, 2 for major surgery, and 2 for laparoscopic surgery 45 minutes). Our study does not support the use of additional points for laparoscopy during the calculation of thrombosis assessment. Our conclusions are in agreement with a large clinical series of open and laparoscopic gastric bypass (Table 3), which showed that the incidence of VTE seems to be lower after laparoscopic compared with open gastric bypass (0.5% vs. 1.0%).1219 In a series of 380 patients who underwent laparoscopic gastric bypass without the use of anticoagulant prophylaxis, Gonzalez et al17 reported a 0.3% incidence of clinically evident deep venous thrombosis. We recognize that the limitations of data from administrative databases are the accuracy in coding and input of data. Nevertheless, VTE as represented by symptomatic venous thrombosis and/or PE is likely to be an accurate end point because this data point does not require subjective evaluation. Another weakness in comparing the outcome of laparoscopic versus open procedure is the limited use of risk-adjustment in most databases. An argument against the validity of our results is that open procedures were performed in higher risk patients with more comorbidity. Risk adjustment is the key for establishing a valid comparison between laparoscopic versus open procedures. The UHC database uses an extensive risk adjustment model and methodology to assign a severity of illness level. In our study, the rates of VTE between laparoscopic and open procedures were calculated according to severity of illness level. Within the subgroup analysis according to severity of illness level, the incidence of VTE continues to be lower after laparoscopic operation compared with open operation. Another limitation is that the data used in this study were obtained from an administrative database that does not have any information concerning the use or nonuse of thromboprophylaxis or the type and duration of the prophylaxis. Could it be that our nding of a lower incidence of VTE after laparoscopic surgery stems from the fact that a more aggressive VTE prophylaxis regimen is being used in this patient population? This is unlikely as the current guideline from SAGES states that the same thromboprophylaxis recommendations for open procedures should be followed when the same procedures are accomplished via laparoscopy.20 There is also lack of infor-
mation about the physiologic status of the patient and history for venous thrombosis or PE, and lack of body mass index for risk stratication in the morbidly obese patients. Additionally, the UHC database is compiled from discharge abstract data and is limited to in-hospital morbidity only without follow-up data. Therefore, VTE arising after discharge would not be captured in this database and we do not know the true incidence of VTE at follow-up for both groups. White et al8 showed, in an analysis of 1,653,275 cases using a large administrative database, that 56% of all VTE events were diagnosed after discharge from the hospital. Finally, the more extensive ambulation and earlier discharge after laparoscopic operations may be a major contributing factor for the lower incidence of VTE in the laparoscopic group. However, we theorize that the short differential in the length of stay ( 2 days) did not fully explain the large differences in VTE rate between the 2 groups. For example, although the length of stay in the open antireux surgery group was only 1.7 days longer than the laparoscopic group, the incidence of VTE was 10-fold higher in the open group (1.1% vs. 0.1%, respectively). Similarly, the length of stay in open gastric bypass was only 1.5 days longer than the laparoscopic group, whereas the incidence of VTE was almost 3-fold higher in the open group (0.8% vs. 0.3%, respectively). Nevertheless, whatever the reason, the observation of a decreased association of VTE with laparoscopic compared with open operations remains. Recognizing these limitations, this analysis of a large sample size is the rst to demonstrate that laparoscopic surgery is associated with a signicantly lower incidence of VTE compared with open surgery.
CONCLUSIONS
This study used a large administrative data set to determine the incidence of VTE after 4 commonly performed laparoscopic and open gastrointestinal operations. Overall, the incidence of VTE is lower after laparoscopic operations compared with open operations, even when stratied according to level of severity of illness. Compared with laparoscopic procedures, we found that open procedures were a signicant risk factor for development of VTE. The results from this study will help surgeons to appropriately estimate the risk of VTE associated with various laparoscopic operations and implementation of a thromboprophylaxis regimen accordingly.
TABLE 3. Incidence of VTE After Open Versus Laparoscopic Gastric Bypass From Selected Large Series With More Than 300 Operations
Open Gastric Bypass Capella and Capella12 (n 652) Obeid et al14 (n 925) Livingston et al16 (n 1067) Smith et al18 (n 451) Total (n 3095) No. DVT and PE (%) 2 (0.3) 14 (1.5) 9 (0.8) 7 (1.6) 32 (1.0) Laparoscopic Gastric Bypass Shikora et al13 (n 750) Biertho et al15 (n 456) Gonzalez et al17 (n 380) Smith et al18 (n 328) Higa et al19 (n 1500) Total (n 3414) No. DVT and PE (%) 5 (0.7) 4 (0.9) 1 (0.3) 1 (0.3) 6 (0.4) 17 (0.5)
1026
2007 Lippincott Williams & Wilkins
Annals of Surgery Volume 246, Number 6, December 2007
Incidence of Venous Thromboembolism After Surgery
REFERENCES
1. Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism: a statement for healthcare professionals from the council on thrombosis (in consultation with the council on cardiovascular radiology), American Heart Association. Circulation. 1996;93:22122245. 2. Colditz GA, Tuden RL, Oster G. Rates of venous thromboembolism after general surgery: combined results of randomized clinical trials. Lancet. 1986;1:143146. 3. Prisco D, De Gaudio AR, Carla R, et al. Videolaparoscopic cholecystectomy induces a hemostasis activation of lower grade than does open surgery. Surg Endosc. 2000;14:170 174. 4. Nguyen NT, Owings JT, Gosselin R, et al. Systemic coagulation and brinolysis after laparoscopic and open gastric bypass. Arch Surg. 2001;136:909 916. 5. Nguyen NT, Wolfe BM. The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg. 2005;241:219 226. 6. Nguyen NT, Cronan M, Braley S, et al. Duplex ultrasound assessment of femoral venous ow during laparoscopic open gastric bypass. Surg Endosc. 2003;17:285290. 7. Zacharoulis D, Kakkar AK. Venous thromboembolism in laparoscopic surgery. Curr Opin Pulm Med. 2003;9:356 361. 8. White RH, Zhou H, Romano PS. Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Throm Haemost. 2003;90:446 455. 9. Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51:70 78. 10. Patel MI, Hardman DT, Nicholls D, et al. The incidence of deep venous thrombosis after laparoscopic cholecystectomy. Med J Aust. 1996;164: 652 654.
11. Kopanski Z, Cienciala A, Ulatowski Z, et al. Comparison of thrombosis rate after laparoscopic and conventional interventions with the I (125) brinogen test. Wien Klin Wochenschr. 1996;108:105110. 12. Capella JF, Capella RF. An assessment of vertical banded gastroplastyRoux-en-Y gastric bypass for the treatment of morbid obesity. Am J Surg. 2002;183:117123. 13. Shikora SA, Kim JJ, Tarnoff ME, et al. Laparoscopic Roux-en-Y gastric bypass: results and high-volume academic program. Arch Surg. 2005; 140:362367. 14. Obeid F, Falvo A, Dabideen H, et al. Open Roux-en-Y gastric bypass in 926 patients without mortality. Am J Surg. 2005;189:352356. 15. Biertho L, Steffen R, Ricklin T, et al. Laparoscopic gastric bypass versus laparoscopic gastric banding: a comparative study of 1,200 cases. J Am Coll Surg. 2003;197:536 547. 16. Livingston EH, Huerta S, Arthur D, et al. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002;236:576 582. 17. Gonzalez QH, Tishler DS, Plata-Munoz J, et al. Incidence of clinically evident deep venous thrombosis after laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2004;18:10821084. 18. Smith SC, Edwards CB, Goodman GN, et al. Open vs. laparoscopic Roux-en-Y gastric bypass: comparison of operative morbidity and mortality. Obes Surg. 2004;14:7376. 19. Higa KD, Ho T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: technique and 3-year follow-up. J Laparoendosc Adv Surg Tech. 2001; 6:377382. 20. Global statement on deep venous thrombosis prophylaxis during laparoscopic surgery. SAGES position statement. Society of American Gastrointestinal Endoscopic Surgeons. Surg Endosc. 1999;13:200.
2007 Lippincott Williams & Wilkins
1027
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Ozone Therapy by Saul Pressman at Oxygen Therapies Support Forum, Topic 443552 PDFDocument15 pagesOzone Therapy by Saul Pressman at Oxygen Therapies Support Forum, Topic 443552 PDFHello MisterNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- IV Drip CalculationsDocument4 pagesIV Drip CalculationsmydewyboyNo ratings yet
- Bipolar 1 DisorderDocument11 pagesBipolar 1 DisorderGirlly AlcantaraNo ratings yet
- Hospital Grades January 2014: 18 Southey Road P O. Box 2026 Harare El/fax: +236 4 778896/778798/778724Document7 pagesHospital Grades January 2014: 18 Southey Road P O. Box 2026 Harare El/fax: +236 4 778896/778798/778724Tony Peterz Kurewa100% (1)
- Ear Disorder Multiple Choice Questions-RationaleDocument5 pagesEar Disorder Multiple Choice Questions-Rationalemydewyboy83% (6)
- Cosmetic Surgery PDFDocument3 pagesCosmetic Surgery PDFDa Young Anna Choi100% (1)
- Pathognomonic Signs of DiseasesDocument4 pagesPathognomonic Signs of DiseasesmydewyboyNo ratings yet
- Arterial Line and Central LineDocument32 pagesArterial Line and Central LineOrachorn AimarreeratNo ratings yet
- Inflammatory Bowel Disease IBDDocument24 pagesInflammatory Bowel Disease IBDmydewyboyNo ratings yet
- Answer Key EXAM DRILL 1 - Community Health Nursing Nursing Practice Ii - CHN and Care of The Mother and ChildDocument11 pagesAnswer Key EXAM DRILL 1 - Community Health Nursing Nursing Practice Ii - CHN and Care of The Mother and Childbetiful100% (5)
- Umbilical Cord Care - Cord Detachment and Prevention of InfectionDocument2 pagesUmbilical Cord Care - Cord Detachment and Prevention of InfectionmydewyboyNo ratings yet
- JurnalDocument12 pagesJurnalIrara RaNo ratings yet
- IV Fluid CommonDocument1 pageIV Fluid CommonmydewyboyNo ratings yet
- DRUGS PoisoningDocument76 pagesDRUGS PoisoningmydewyboyNo ratings yet
- Xplore The World of Nursing in The ORDocument2 pagesXplore The World of Nursing in The ORmydewyboyNo ratings yet
- Summary of Vaccine Procurement, Donation Processing, and Approval (By The National Government)Document6 pagesSummary of Vaccine Procurement, Donation Processing, and Approval (By The National Government)December CoolNo ratings yet
- External Stressors: - Physical Environment - Social Interaction - Organisational - Major Life Events - Daily HasslesDocument71 pagesExternal Stressors: - Physical Environment - Social Interaction - Organisational - Major Life Events - Daily HasslesSara NaeemNo ratings yet
- E-Book C Arms-NewDocument9 pagesE-Book C Arms-NewHugoNo ratings yet
- 1 Revised Food Borne Illness Lecture 1Document5 pages1 Revised Food Borne Illness Lecture 1Tarequl Islam NishadNo ratings yet
- Global Quality Manual PDFDocument30 pagesGlobal Quality Manual PDFArief Prasetya HarahapNo ratings yet
- Femoral Block Vs Adductor Canal Block: Regional Analgesia For Total Knee ArthroplastyDocument10 pagesFemoral Block Vs Adductor Canal Block: Regional Analgesia For Total Knee ArthroplastyStanford AnesthesiaNo ratings yet
- Prevention of Pin Site Infection in External FixatioDocument11 pagesPrevention of Pin Site Infection in External FixatioKim Gabrielle Exene LeeNo ratings yet
- 222Document7 pages222Erl DrizNo ratings yet
- Laporan Bulanan Lb1: 0-7 HR Baru LDocument20 pagesLaporan Bulanan Lb1: 0-7 HR Baru LOla SarlinaNo ratings yet
- Reflexology Intake FormDocument1 pageReflexology Intake FormJael PistioNo ratings yet
- Clinical Examination and Record KeepingDocument3 pagesClinical Examination and Record Keepingsam paulNo ratings yet
- Fever in Children With ChemoteraphyDocument23 pagesFever in Children With ChemoteraphyImanuel Far-FarNo ratings yet
- First Aid / CPR: HSE Training 2005Document36 pagesFirst Aid / CPR: HSE Training 2005Martin griffinNo ratings yet
- CSOMDocument29 pagesCSOMsuciNo ratings yet
- OtoscopeDocument3 pagesOtoscopeVpjunaib JunaibNo ratings yet
- Paired Facial Treatment With 755nm Picosecond Laser With Diffractive Lens Array and 1060nm Laser Lipolysis of The Submentum - An Open-Label Prospective TriaDocument7 pagesPaired Facial Treatment With 755nm Picosecond Laser With Diffractive Lens Array and 1060nm Laser Lipolysis of The Submentum - An Open-Label Prospective TriaErik BrooksNo ratings yet
- Inflammatory Breast CancerDocument6 pagesInflammatory Breast CancerHafsa ShafiqueNo ratings yet
- Roles & Responsibilities of CRADocument26 pagesRoles & Responsibilities of CRANaresh Kumar RapoluNo ratings yet
- Case:chronic Constrictive Pericarditis - NicvdDocument44 pagesCase:chronic Constrictive Pericarditis - NicvdNavojit ChowdhuryNo ratings yet
- Chapter 10 Syringes and NeedlesDocument15 pagesChapter 10 Syringes and NeedlesTiffany FlorentNo ratings yet
- © Simtipro SRLDocument11 pages© Simtipro SRLMoncef PechaNo ratings yet
- Conference & Workshop ScheduleDocument5 pagesConference & Workshop ScheduleglmoningkaNo ratings yet
- Literature & MedicineDocument14 pagesLiterature & MedicineJoyce LeungNo ratings yet
- Catalog Tracoe 2014 PDFDocument94 pagesCatalog Tracoe 2014 PDFLiudmila RailescuNo ratings yet