Professional Documents
Culture Documents
Medication Error: Technological Advances
Uploaded by
VictorLeiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medication Error: Technological Advances
Uploaded by
VictorLeiCopyright:
Available Formats
Running Head: MEDICATION ERROR: TECHNOLOGICAL ADVANCES
MEDICATION ERROR: TECHNOLOGICAL ADVANCES Victor J. Lei Northeastern University
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
Abstract Technological advances have changed the way many hospitals and pharmacies operate over the years. It is important to note that the change has come from thorough observation and analysis of current systems. In the healthcare field, medication errors are an important area of focus that needs constant improvement. Studies have been produced to measure the relative improvements on how technology has decreased the amount of medication errors made. Technology within the hospital and outpatient setting includes all levels of medication handling. It is important to see and observe the growth of such systems to help better understand how to further improve.
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
Introduction Healthcare professionals try their best to provide the most optimal care to their patients. Whether this comes from a thorough diagnosis or reduced wait times in the emergency rooms, improving patient care is a critical responsibility in healthcare field. Unfortunately, people make mistakes. It is unrealistic to expect healthcare professionals to have a zero percent margin of error, especially when healthcare professionals are being asked to work faster and increase patient volume. Thus, it is important for them to reduce their error as much as possible. Within the pharmacy department, there are many avenues where patient care can be affected. Pharmacists must worry about drug safety and medication errors. Technology has responded to this concern with new methods that have helped decrease medication dispensing times and increasing drug location tracking. Corporations like Pyxis and Omnicell, which focus on medication management, have changed the way pharmacy departments operate entirely. They have introduced carousel fill machines, and automated dispensing cabinets and drawers. Including the previous mentioned machines, technology has advanced to help significantly decrease the amount of medication error. With an in-depth discussion of what are medication errors, the technological advancements and pitfalls give insight on how one must operate and be aware of for the healthcare professional. Types of Medication Errors A Medication Error is an overarching term that describes a discrepancy between the patient and the correct drug intended for the patient. From that, medication errors can be broken down into 4 categories: prescribing, dispensing, administration, and monitoring (Lombardi 2000). For the first, prescribing errors occur when there are hard to read or wrong drugs
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
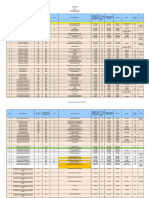
prescribed to a patient. Other issues include transcription errors from pharmacists and technicians. In dispensing errors, the mistake occurs between the handling of the drugs from the pharmacy side. As Figure 1 show, there are many occasions where a drug can be mishandled.
Figure 1 (Cheung, Bouvy, De Smet 2009) It is important for pharmacy workers to understand where these errors can occur and how to deal with them when they occur. If left untreated, serious drug adverse reactions could occur to patients if dispensed and administered the incorrect drug. This leads to a third potential error, administration error, which occurs while the drug is handled for the nurses or physicians who give the medication to the patient. It is important for healthcare workers to make sure they are administering the right drug to the right person. The final fourth type of medication error is monitoring, which is the last checks to see if the patient is receiving the correct dose and medicine.
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
Technological Advancements Medication management companies have focused by looking at the many avenues where medication errors may be reduced. Some have focused on the transcribing of prescriptions. Others have focused on the dispensing and administration tracking machines. One of the most influential developments in medication management is Computerized Physician Order Entry (CPOE), which was created to help eliminate difficult to read handwriting, transcription errors, and ensure right prescriptions were paired with the right patients. Software would be utilized by mainly nurses and doctors, while being reinforced by pharmacists. Information input would then relay over to pharmacy information systems. Research indicates, computerized physician-order entry has been shown to reduce the incidence of serious medication errors by 55% (Poon et al. 2010). By keeping many of the interactions on an electronic media, healthcare workers can consistently see and understand where the order is in the process. This helps keep healthcare workers up to date on the handling of their medication to the respective patient. Such CPOE systems usually do not act alone. They in fact, often are paired with other information systems to help keep the information on a digital level and at all levels track medication from point a to point b. With this the development of barcodes has been essential. Barcodes on medications became mandatory by the Food and Drug Administration in 2006. Hospitals have, since then, begun implementing bar-code technology into their dispensing workflow (Poon et al. 2005). Barcode technology has had tremendous influence on the way healthcare practice operates. It permeates many levels of medication handling. From the beginning, prescriptions entered through a CPOE are given unique prescriptions that are specific to the prescription and patient. Medication management companies like, Omnicell and Pyxis,
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
utilize this in combination to the drug barcodes to help picking and dispensing of drugs. Machines with implemented software can categorize and identify if the correct drug is picked for the specific prescriptions. In the realm of dispensing, drugs can be scanned with prescription labels to make sure that they match up. This can go further when automated dispensing machines are stocked and drugs are required to be rescanned again to make sure the right drug is in the right location in the machine. From there, nurses and doctors can enter the machines and receive the correct drug for the correct patient. However, once the drug leaves the machine and enters the hands of the nurse or doctor, there leads to a potential error in administration. Error in administration would often occur with incorrect dosing or incorrect patient with the respective drug upon patient receiving the drug. Point-of-Administration (POA) systems were created as a result. POA systems ensured the right dose of the right drug was administered via the right route at the right time to the right patient (ASHP 2004). Verification would be created at specific checkpoints were drug or patient information could be mishandled. Barcodes were applied to patient wristbands and their specific code would entail the correct information about their list of approved medications. Electronic prescriptions would also have their own set of barcodes that would check if the barcodes on the drug and the prescription match, when they were delivered, and when they were administered. The pitfalls of the technological advancements and common mistakes made With the advancements, new problems arise in the implementation of the systems. Bar code technology has definitely decreased the amount of errors, but the system is not perfect. Often times, there are instances of unreadable drug barcodes or human error in scanning the drugs. Other times, some prescriptions would involve dispensing multiple vials of a drug where
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
only one drug would be scanned rather than all. Such limitations can cause mistakes in the dispensing of drugs. CPOE still is in a developmental phase and requires immense amounts of intervention. James Carptener, R.Ph., breaks down the difficulties of CPOE implementation and development, Implementing CPOE is challenging because of the complexities of medication orders and the clinical decision support that is required. Every possible type of order must be accommodated. Order communication channels are complex and communication is not necessarily linear. Professional knowledge and information are not discrete bits of data that can be stored and retrieved at will and they do not map in a simple manner onto other schemata. (ASHP 2004) The difficulties of implementation alone make utilizing CPOEs cumbersome, but also increase the amount of potential medication errors. It would be expected for hospitals upon first few months to have more errors, but eventually for the errors to decrease with the increased experience and knowledge of the system. Such problems can even leak into the dispensing realm. When an order is entered into a CPOE the information is carried to the appropriate machines that allow for the pharmacy to pick and dispense the entered drugs. Dispensing errors can occur even with the new technology implemented. Simple errors include the wrong drug restocked in the wrong location. Others could be dispensing a higher dose than what is prescribed due to limited stock of the drug within a pharmacy. One of the most important limitations would be caused from barcode technology. As pharmacists note, Pharmacy staff are frequently interrupted to address scanning problems and other unresolved issues. A variety of different bar-code formats are in development and reading the newer formats will require updated scanning equipment. Decisions also were made
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
about scanning procedures for certain products (e.g., bulk items, such as
topical
medications and inhalers and floor stock items, such as heparin flushes). In addition, education is necessary because nurses often do not recognize that floor stock is a medication, the administration of which needs to be documented. (ASHP 2004) Technology, though helpful, often include little hindrances like the previously describe. Barcode technology does have limitations in the parameters that set. For improvement to occur, such systems including that of CPOE and on other levels of medication handling, one must view the process systematically. Six Sigma as an Approach to Improvement Technological advancements come with their own set of problems. One interesting way of tackling some of these common problems is to utilize Six Sigma. Six Sigma is a set of strategies and techniques that are used for process efficiency and reducing defects in policy and procedure. It can be used to help dispensing errors when utilizing the multiple machines and software within a hospital pharmacy department. For this to work, it requires heavy statistical analysis. This process can be broken up into 3 sections: measurement phase, analyze phase, and improvement phase. One hospital was able to decrease their errors by 230 errors per million. The implementation of Six Sigma also helped pharmacists realize and understand the workflow that they utilize and where errors could occur. They became more open to tackling medication error problems and understood the importance of them (Chan 2004).
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
Figure 2 (Chan 2004) Process flow maps are important to help view and analyze where errors can occur. From these maps, information can be extrapolated to try to piece together potential solutions to improve on reducing medication errors. Conclusion There is no doubt that medication errors have been reduced by technological advancements, but it is important to not forget the common pitfalls that can attribute to many errors. A technological system is only as good as the compliance of the team utilizing the technology. So education and communication should be implemented between all healthcare workers to be able to utilize the new technological advances and continue to decrease the amount of medication errors that can occur.
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
10
Reflection This paper was very difficult for me to organize and break down. I found myself trying to discuss/argue too many things. However, I hope I was able to break down the information in a relative cohesive manner. I did notice that I found myself pulling a great deal of information for the ASHP mid year continuing education piece. I was hard pressed to believe it is a popular source but had difficulties citing it all. I would place this in my portfolio because it relates to how technology has changed the many aspects of medication handling and errors.
MEDICATION ERROR: TECHNOLOGICAL ADVANCES
11
References ASHP (2004). Improving medication safety in health systems through innovations in automation technology. ASHP. http://www.hospitalrx.com/pdf/ASHP%20Smart%20Pumps.pdf Lombardi, T. P. (2000). Closing the loop implementing quality improvement processes and advances in technology to decrease medication errors. Medscape. http://www.medscape.com/viewarticle/408564_4 Chan, Agnes L. F. (2004). Use of six sigma to improve pharmacist dispensing errors at an outpatient clinic. American Journal of Medical Quality, 19(3). http://ajm.sagepub.com/content/19/3/128.full.pdf Cheung, K., Bouvy, M. L., De Smet, P. A. G. M. (2009). Medication errors: the importance of safe dispensing. Br J Clin Pharmacol. 67(6). doi: 10.1111/j.1365-2125.2009.03428.x Poon, E. G., Cina, J. L., Churchill, W. W., Mitton, P., McCrea, M. L., Featherstone, E., Keohane, C. A., Rothschild, J. M., Bates, D. W., Gandhi, T. K. (2005). Effect of bar-code technology on the incidence of medication dispensing errors and potential adverse drug events in a hospital pharmacy. AMIA Annual Symposium Proceedings. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1560475/#__ffn_sectitle Poon, E. G., Keohan, C. A., Yoon, C. S., Ditmore, M., Bane, A., Levtzion-Korach, O., Moniz, T., Rothschild, J. M., Kachalia, A. B., Haynes, J., Churchill, W. W., Lipsitz, S., Whittemore, A. D., Bates, D. W., Gandhi, T. K., (2010) Effect of bar-code technology on the safety of medication administration. NEJM, doi: 10.1056/NEJMsa0907115
You might also like
- Phresh Pharmacy: New Ideas for the Business of Community PharmacyFrom EverandPhresh Pharmacy: New Ideas for the Business of Community PharmacyNo ratings yet
- The Role of Technology in The Medication Use ProcessDocument6 pagesThe Role of Technology in The Medication Use Processhadukenryu9761No ratings yet
- Newman's Certified Electronic Health Records Technician Study GuideFrom EverandNewman's Certified Electronic Health Records Technician Study GuideNo ratings yet
- Figure 1. Indicator Framework of The Medication Error (Nerich Et Al., 2010)Document3 pagesFigure 1. Indicator Framework of The Medication Error (Nerich Et Al., 2010)balqiswulanNo ratings yet
- Pharmacy Informatics NotesDocument3 pagesPharmacy Informatics NotesSmoi Liver100% (2)
- The Role of Technology MedicationsDocument10 pagesThe Role of Technology MedicationsMeccanazaren Susvilla BojorqueNo ratings yet
- Running Head: Computerized Provider Order Entry 1Document9 pagesRunning Head: Computerized Provider Order Entry 1api-509672908No ratings yet
- Evidence Paper JpeacottricardosDocument7 pagesEvidence Paper Jpeacottricardosapi-302415380No ratings yet
- Bar Coded Medication AdministrationDocument2 pagesBar Coded Medication AdministrationJoan TemplonuevoNo ratings yet
- Preventing Medication ErrorsDocument26 pagesPreventing Medication ErrorsmrkianzkyNo ratings yet
- Computerized Provider Order Entry: by Jyotirmoy Roy (3 Year, 6 Sem) Guided by Avishek ChatterjeeDocument12 pagesComputerized Provider Order Entry: by Jyotirmoy Roy (3 Year, 6 Sem) Guided by Avishek ChatterjeeAndrey VadylaNo ratings yet
- Medication ErrorsDocument7 pagesMedication ErrorsNelly CheptooNo ratings yet
- Health Information TechnologyfinalDocument8 pagesHealth Information TechnologyfinalFranzia Izandra Alkuino Mojica100% (1)
- Case Study 1-Statistical Thinking in HealthcareDocument6 pagesCase Study 1-Statistical Thinking in HealthcareRoxana Aguilar100% (2)
- Medication Errors:: Don't Let Them Happen To YouDocument6 pagesMedication Errors:: Don't Let Them Happen To YouPhuong Tran100% (1)
- Applying Lewins Change Management Theory To The Implementation of Bar-Coded Medication AdministrationDocument6 pagesApplying Lewins Change Management Theory To The Implementation of Bar-Coded Medication AdministrationgergisNo ratings yet
- Computer System in Hospital Pharmacy 1Document9 pagesComputer System in Hospital Pharmacy 1Sreya Sanil100% (4)
- Medication Safety Alerts: David UDocument3 pagesMedication Safety Alerts: David UVina RulinaNo ratings yet
- My First Presentation - SabaDocument20 pagesMy First Presentation - SabaSaba Abu FarhaNo ratings yet
- Running Head: Analysis of Automated Dispensing Cabinets 1Document16 pagesRunning Head: Analysis of Automated Dispensing Cabinets 1api-413318865No ratings yet
- Trabalho e HealthDocument14 pagesTrabalho e Healthgabriel_ferreria89No ratings yet
- RoilsDocument4 pagesRoilsapi-568855135No ratings yet
- Week 3 HandoutsDocument22 pagesWeek 3 HandoutsAlbert Ey BubanNo ratings yet
- Information Technology: Medical ScienceDocument17 pagesInformation Technology: Medical ScienceKimochi SenpaiiNo ratings yet
- Hospital Reduces Medication Errors Using DMAICDocument9 pagesHospital Reduces Medication Errors Using DMAICdrustagiNo ratings yet
- Literature Review On Medication ErrorsDocument7 pagesLiterature Review On Medication Errorsqyptsxvkg100% (1)
- Final WhitepaperDocument15 pagesFinal Whitepaperapi-488096711No ratings yet
- IAA Assignment 1Document10 pagesIAA Assignment 1Chai MichelleNo ratings yet
- Applying Lewins Change Management Theory To The Implementation of Bar-Coded Medication AdministrationDocument6 pagesApplying Lewins Change Management Theory To The Implementation of Bar-Coded Medication AdministrationMohamed IrshaNo ratings yet
- Computerized Provider Order Entry: by Jyotirmoy Roy (3 Year, 6 Sem) Guided by Avishek ChatterjeeDocument12 pagesComputerized Provider Order Entry: by Jyotirmoy Roy (3 Year, 6 Sem) Guided by Avishek ChatterjeeAli El AttarNo ratings yet
- Medication Errors in The United States and How To Improve Simple Mistakes 1Document7 pagesMedication Errors in The United States and How To Improve Simple Mistakes 1api-681331537No ratings yet
- 10 Changing PharmacyDocument1 page10 Changing Pharmacyjatanagurmaan06No ratings yet
- Medication Errors Their Causative and Preventive Factors2.Doc 1Document11 pagesMedication Errors Their Causative and Preventive Factors2.Doc 1Mary MannNo ratings yet
- Role of Technology in Medication Use ProcessDocument31 pagesRole of Technology in Medication Use Processgctv0491100% (5)
- Applications of Computers in Hospital Pharmacy PracticeDocument12 pagesApplications of Computers in Hospital Pharmacy Practicepatil dewanshi kNo ratings yet
- Module 1 Lab-1Document27 pagesModule 1 Lab-1k kkkNo ratings yet
- QualityDocument8 pagesQualityjadema14No ratings yet
- Research Article: A New Visual Cryptography-Based QR Code System For Medication AdministrationDocument10 pagesResearch Article: A New Visual Cryptography-Based QR Code System For Medication Administrationtimehealing056No ratings yet
- Informatics RaveloDocument4 pagesInformatics RaveloKyle Isidro MaleNo ratings yet
- Medication Safety Issues - 1: Keywords: Medication Safety, Errors, Patients Care, Prevention, Safe PracticeDocument4 pagesMedication Safety Issues - 1: Keywords: Medication Safety, Errors, Patients Care, Prevention, Safe PracticeErnda PutrNo ratings yet
- His Essays Lesson 9 15Document6 pagesHis Essays Lesson 9 15Raymund Vincent OmayaoNo ratings yet
- Nurs 218 - AssignmentDocument6 pagesNurs 218 - Assignmentapi-354434651No ratings yet
- Application of Computers in Hospital and Clinical PharmacyDocument13 pagesApplication of Computers in Hospital and Clinical PharmacyAmmarah Taimur11% (9)
- Running Head: Health Informatics 1Document6 pagesRunning Head: Health Informatics 1Vishal VijNo ratings yet
- Unit 3 Computer Applications in PharmacyDocument8 pagesUnit 3 Computer Applications in PharmacyHiba MohammedNo ratings yet
- MMICC 2015 - Appendix BookletDocument20 pagesMMICC 2015 - Appendix BookletBen LeeNo ratings yet
- Ucs 17609Document4 pagesUcs 17609Abubakar SadiqNo ratings yet
- Medication ErrorDocument7 pagesMedication ErrorLenny SucalditoNo ratings yet
- Medication Errors Prevention and Reduction GuidelinesDocument18 pagesMedication Errors Prevention and Reduction GuidelinesasgbalajiNo ratings yet
- Fs 2Document13 pagesFs 2Muhamad Taufiq AliNo ratings yet
- Drug Procurement and Institution Tracking SystemDocument78 pagesDrug Procurement and Institution Tracking SystemLatifa AmeirNo ratings yet
- Evidence Based Practice Medication ErrorsDocument6 pagesEvidence Based Practice Medication Errorsapi-302591810No ratings yet
- Reducing Medication Risks of Electronic Medication Systems: Laura A. FinnDocument9 pagesReducing Medication Risks of Electronic Medication Systems: Laura A. FinnASHISH KUMAR YADAVNo ratings yet
- Comp14 Unit4 Audio TranscriptDocument7 pagesComp14 Unit4 Audio TranscriptP D SpencerNo ratings yet
- The Impact of Health Information Technology On Patient SafetyDocument13 pagesThe Impact of Health Information Technology On Patient SafetySaba Abu FarhaNo ratings yet
- Implementation of Physician Order Entry: User Satisfaction and Self-ReportedDocument14 pagesImplementation of Physician Order Entry: User Satisfaction and Self-ReportedAditya Pratap SinghNo ratings yet
- 35521Document12 pages35521Kyle MaogNo ratings yet
- Applications of Computer Science in PharmacyDocument33 pagesApplications of Computer Science in PharmacyPaul DavidNo ratings yet
- Use of Computer in Medical Field: Pharmacy Practice-IiiDocument4 pagesUse of Computer in Medical Field: Pharmacy Practice-IiiZaid RazaNo ratings yet
- Preventing Medication ErrorsDocument24 pagesPreventing Medication Errorsn100% (1)
- Chemical and Biological Considerations in The Treatment of Metal Intoxications by Chelating AgentsDocument11 pagesChemical and Biological Considerations in The Treatment of Metal Intoxications by Chelating AgentsaprilfitriaNo ratings yet
- The Interaction of Herbs and DrugsDocument17 pagesThe Interaction of Herbs and DrugsCarleta StanNo ratings yet
- EFRAC Drug BrochureDocument58 pagesEFRAC Drug BrochureEfracNo ratings yet
- Tabel Obat Kardiovaskuler Aulia Nurtafani Reforma (189296)Document9 pagesTabel Obat Kardiovaskuler Aulia Nurtafani Reforma (189296)Aulia Nurtafani ReformaNo ratings yet
- Particle Size Reduction ResearchDocument15 pagesParticle Size Reduction ResearchEman SaidNo ratings yet
- ONE Compartment Open ModelDocument29 pagesONE Compartment Open ModelNOORUDDINNo ratings yet
- Formulation DevelopmentDocument1 pageFormulation DevelopmentbilcareNo ratings yet
- University of The Immaculate Conception: Fr. Selga Street, Davao CityDocument2 pagesUniversity of The Immaculate Conception: Fr. Selga Street, Davao CitykarenbarnNo ratings yet
- 1.adverse Drug ReactionsDocument18 pages1.adverse Drug ReactionsVitalis MbuyaNo ratings yet
- Dispensing Lecture Reviewer - MidtermDocument26 pagesDispensing Lecture Reviewer - Midtermapi-306968266No ratings yet
- Pharmacology AssignmentDocument3 pagesPharmacology AssignmentmorphimistNo ratings yet
- Best Summary and Analogy QuestionsDocument8 pagesBest Summary and Analogy QuestionsvikrrantNo ratings yet
- Billing Rawat JalanDocument1 pageBilling Rawat Jalankhusnul astriNo ratings yet
- CHLDocument12 pagesCHLParthNo ratings yet
- Understanding Manganum Aceticum Through Hahnemann's Materia Medica PuraDocument12 pagesUnderstanding Manganum Aceticum Through Hahnemann's Materia Medica PuraHomoeopathic Pulse100% (1)
- Pharma Leader Series Top 50 Generic Drug Manufacturers 2013-2023Document30 pagesPharma Leader Series Top 50 Generic Drug Manufacturers 2013-2023VisiongainGlobal0% (1)
- E Tender 20-03-18Document132 pagesE Tender 20-03-18gomathi ShankarNo ratings yet
- Module 2Document3 pagesModule 2Esmareldah Henry SirueNo ratings yet
- Full Text of Results - Top 10, Performance of SchoolsDocument3 pagesFull Text of Results - Top 10, Performance of SchoolsTheSummitExpressNo ratings yet
- Pharmaceutical QBD (Final)Document41 pagesPharmaceutical QBD (Final)Tahsin AhmedNo ratings yet
- RhubarbDocument16 pagesRhubarbAN MarcosNo ratings yet
- Fixed Dose Combinations Approved by DCGI Upto August 2022Document5 pagesFixed Dose Combinations Approved by DCGI Upto August 2022SKC AMSTACRITNo ratings yet
- Amodiaquine HydrochlorideDocument31 pagesAmodiaquine HydrochlorideJulia TaranchukNo ratings yet
- Drug Related ProblemsDocument25 pagesDrug Related ProblemsChristine GanNo ratings yet
- CETIRIZINEDocument2 pagesCETIRIZINEAngelica Cassandra Villena100% (10)
- Lecture - 1 Introduction To PharmacologyDocument62 pagesLecture - 1 Introduction To PharmacologyAshique FarhadNo ratings yet
- Azathioprine DrugDocument18 pagesAzathioprine DrugteritohahaNo ratings yet
- Review Garlic (Allium Sativum L.) : Adverse Effects and Drug Interactions in HumansDocument12 pagesReview Garlic (Allium Sativum L.) : Adverse Effects and Drug Interactions in HumansRizkaa Harinii QuinshaNo ratings yet
- Dossier Common Technical Document CTD Index: (Sample Document Will Provide On Request)Document6 pagesDossier Common Technical Document CTD Index: (Sample Document Will Provide On Request)Karem EladweyNo ratings yet
- Biopharmaceutics Uos Past PapersDocument9 pagesBiopharmaceutics Uos Past PapersMr nobodyNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (6)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)