Professional Documents
Culture Documents
Scandinavian Guidelines For Initial Management of Minimal, Mild and Moderate Head Injuries in Adults: An Evidence and Consensus-Based Update
Uploaded by
Desy RusianaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Scandinavian Guidelines For Initial Management of Minimal, Mild and Moderate Head Injuries in Adults: An Evidence and Consensus-Based Update
Uploaded by
Desy RusianaCopyright:
Available Formats
ulscharge wlLh oral and wrlLLen lnsLrucLlons
Some paLlenLs may need admlsslon for reasons oLher Lhan Lhelr head ln[ury
es
All adulL paLlenLs wlLh mlnlmal, mlld and moderaLe head ln[ury (CCS 9-13) wlLhln 24 hours of ln[ury
es
M|n|ma|
CCS 13
Admlsslon for observaLlon >24 hours
Conslder consulLaLlon wlLh neurosurgeon
8epeaL C1 lf neurologlcal and/or CCS (>2 polnLs) deLerloraLlon
No
5ee belp sbeet fot exploootloos ooJ mote Jetolls
< 0.10
g]L
C1 abnorma|
C1
norma|
C1
abnorma|
C1
norma|
or
abnorma|
C1
norma|
C1
|
C1
Conslder admlsslon for observaLlon >12
hours afLer ln[ury as an alLernaLlve opLlon
C1
z 0.10
g]L
C1 C1 C11
C1
Conslder admlsslon for observaLlon >12
hours afLer ln[ury as an alLernaLlve opLlon
es es
M||d
medlum-rlsk
CCS 14-13 ooJ
8C1P age >63 years
ANu anLl-plaLeleL
medlcaLlon
8C
AN
me
No
C1
C1
es es
< 0.
g]
z 0.10
g]L
0 10
S1008
lf <6 hrs afLer ln[ury, sample serum for S1008
analysls
lf >6 hrs, exLracranlal ln[ury or lf S1008 ls
unavallable, do C1
S1008
es
No
es
M||d
hlgh-rlsk
CCS 14-13 ooJ
osLLraumaLlc selzures
local neurologlcal deflclLs
Cllnlcal slgns of depressed or
basal skull fracLure
ShunL-LreaLed hydrocephalus
1herapeuLlc anLlcoagulaLlon
or coagulaLlon dlsorders
No
es
M||d
low-rlsk
CCS 14
ot
CCS 13 ooJ
SuspecLed/conflrmed
loss of consclousness
8epeaLed vomlLlng (>2
eplsodes)
es
Moderate
CCS 9-13
o
CC
Su
los
No
lo
Cl
ba
Sh
No
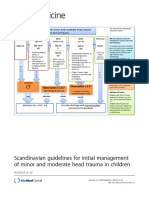
Scandinavian guidelines for initial management
of minimal, mild and moderate head injuries in
adults: an evidence and consensus-based update
Undn et al.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50 (25 February 2013)
GUI DELI NE Open Access
Scandinavian guidelines for initial management
of minimal, mild and moderate head injuries in
adults: an evidence and consensus-based update
Johan Undn
1*
, Tor Ingebrigtsen
2
and Bertil Romner
3
, for the Scandinavian Neurotrauma Committee (SNC)
See related commentary article here http://www.biomedcentral.com/1741-7015/11/51
Abstract
Background: The management of minimal, mild and moderate head injuries is still controversial. In 2000, the
Scandinavian Neurotrauma Committee (SNC) presented evidence-based guidelines for initial management of these
injuries. Since then, considerable new evidence has emerged.
Methods: General methodology according to the Appraisal of Guidelines for Research and Evaluation (AGREE) II
framework and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system.
Systematic evidence-based review according to Preferred Reporting Items for Systematic Reviews and Meta-
Analyses (PRISMA) methodology, based upon relevant clinical questions with respect to patient-important
outcomes, including Quality Assessment of Diagnostic Accuracy Studies (QUADAS) and Centre of Evidence Based
Medicine (CEBM) quality ratings. Based upon the results, GRADE recommendations, guidelines and discharge
instructions were drafted. A modified Delphi approach was used for consensus and relevant clinical stakeholders
were consulted.
Conclusions: We present the updated SNC guidelines for initial management of minimal, mild and moderate head
injury in adults including criteria for computed tomography (CT) scan selection, admission and discharge with
suggestions for monitoring routines and discharge advice for patients. The guidelines are designed to primarily
detect neurosurgical intervention with traumatic CT findings as a secondary goal. For elements lacking good
evidence, such as in-hospital monitoring, routines were largely based on consensus. We suggest external validation
of the guidelines before widespread clinical use is recommended.
Keywords: computed tomography, GRADE, guidelines, head/brain injury/trauma, management, prediction rule,
routines, S100/S100B/S100BB
Background
Traumatic brain injury (TBI) is one of the most common
reasons for emergency department (ED) care [1]. Cases
of TBI account for over 1 million visits per year in both
the USA and the UK [2,3] and are responsible for two-
thirds of all trauma deaths [4]. Only a small proportion
of these are classed as severe head injury [1], with a Glas-
gow Coma Scale (GCS) score of 3 to 8. The majority of
patients are instead classed as minimal, mild and
moderate head injuries [5] and are generally conscious in
the ED with varying degrees of neurological symptoms. A
minority of these patients will have intracranial pathology
on computed tomography (CT) scanning and an even
smaller proportion will need neurosurgical intervention
[6,7]. In particular, the intermediate risk group of mild
head injury (MHI) has been notoriously difficult to man-
age as these patients have a very low, but not negligible,
risk of needing neurosurgical intervention [7,8].
Over the past decade, initial management strategies have
become focused on selective CT use based upon presence
or absence of specific aspects of patient history and/or
clinical examination [6,9-11], in order to effectively use
* Correspondence: dr.johan.unden@gmail.com
1
Department of Intensive Care and Perioperative Medicine, Institute for
Clinical Sciences, Sdra Frstadsgatan 101, 20502 Malm, Sweden
Full list of author information is available at the end of the article
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
2013 Undn et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
health care resources. This selective management has
received more attention following reports of increased
cancer risks from CT scans, estimated at 1 in 5,000 to
10,000 for a single head CT scan in young adults [12].
Following a normal CT scan after mild head injury,
consensus is generally to discharge patients from the hos-
pital [13,14], although subgroups of patients may still be
at risk of developing delayed intracranial complications
of varying significance [15,16].
In 2000, the Scandinavian Neurotrauma Committee
(SNC) presented evidence-based guidelines for the initial
management of minimal, mild and moderate head inju-
ries [5]. Although external and independent validation
has shown the guidelines to function favorably [17,18], it
is likely that new evidence exists which needs to be con-
sidered. The SNC has therefore mandated an update of
the guidelines. The aim of the present report is to present
these updated guidelines for adults, including the metho-
dology and considerations behind the workflow.
Methods
The overall policy was to follow the Appraisal of Guide-
lines for Research and Evaluation (AGREE) II guideline
development framework [19], complemented by the
Grading of Recommendations Assessment, Development
and Evaluation (GRADE) system [20]. Consensus was that
these two aids would result in a transparent and systematic
methodology and the best possible workflow from available
evidence to guideline construction and implementation.
The overall workflow process is shown in Figure 1.
Task force, working group and stakeholders
The SNC consists of neurosurgeons and anesthesiologists
from Scandinavia with expertise in neurotrauma. A task
force was initiated within the SNC, consisting of three
authors with experience within the field (JU, TI, BR), to
propose evidence-based recommendations and a draft for
the updated guidelines. For the consensus stage of devel-
opment, a working group was formed consisting of SNC
members. Important stakeholders from general surgery,
emergency medicine and orthopedics were also involved
in this process. These specialties initially manage the vast
majority of head injury patients in Scandinavia. We also
considered including members of the public in the pro-
cess but unanimously decided against this as we did not
believe it would facilitate optimal guideline development
in the present scenario.
Scope, purpose and target population
The objective of the guidelines created in the present
work would be to assist ED physicians with initial (the
first 24 h) management of all adult patients with minimal,
mild and moderate head injury, specifically to decide
which patients are to receive CT scanning, admission or
discharge (or combinations of these) from the ED. Head
injury severity was predefined according to the Head
Injury Severity Score (HISS [21]) where minimal repre-
sents patients with a GCS score of 15 and no risk factors,
mild is a GCS score of 14 or 15 with risk factors (such as
amnesia or loss of consciousness (LOC)) and moderate is
a GCS score of 9 to 13.
The rationale was primarily to identify all patients
needing neurosurgical intervention, including medical
intervention for high intracranial pressure (assigned a
critical level with regard to patient-important outcomes).
The secondary goals (assigned important, but not criti-
cal, with regard to patient-important outcomes) were
identification of non-neurosurgical intracranial trau-
matic complications and also strong consideration of
resource use with minimization of unnecessary (normal)
CT scans and/or admission.
The task force decided a priori to make an attempt to
keep the guidelines applicable to the complete patient
spectrum within EDs, that is, to ensure that all adult
patients with minimal, mild and moderate head injury
can be managed according to the guidelines.
Certain assumptions were also made a priori concern-
ing aspects of management that were deemed unneces-
sary for critical review. The task force all agreed that
magnetic resonance imaging (MRI) would not be con-
sidered in these guidelines concerning initial manage-
ment and that in-hospital observation, instead of CT,
would be regarded only as a secondary management
option. The use of plain skull films was addressed and
rejected in the previous guidelines. Additionally, we
chose not to consider later aspects of management, such
as detection and treatment of post-concussion syndrome
(PCS) and chronic subdural hematomas. We also agreed
that all pathological findings on head CT should lead
to hospital admission. Finally, we would not address
the surgical or medical management of intracranial
complications.
The task force was unclear concerning the selection of
patients for CT scanning or discharge, following minimal,
mild and moderate head injuries. We were also unclear
concerning which patients, irrespective of initial CT scan
results, should have hospital admission for clinical obser-
vation, a repeat CT scan, or both. Therefore, consensus
was achieved to address two important clinical questions
that would require systematic review of evidence and
would form the basis of the updated guidelines, shown
below.
Clinical question 1: Which adult patients with mini-
mal, mild and moderate head injury need a head CT
and which patients may be directly discharged?.
Clinical question 2: Which adult patients with mini-
mal, mild and moderate head injury need in-hospital
observation and/or a repeat head CT?.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 2 of 13
Search strategy
In order to address the clinical questions we performed
two separate systematic reviews of the literature, in
accordance to the Preferred Reporting Items for Systema-
tic Reviews and Meta-Analyses (PRISMA) statement [22].
Both utilized broad searches of the MEDLINE and
EMBASE databases, from 1985 until January 2010 and
then complemented to July 2012, using prespecified
Medical Subject Headings (MeSH) terms and key words
depicted by the task force. MeSH terms were pretested
for validity through identification of several key articles.
It was deemed unlikely that studies prior to 1985 would
be useful considering the wide-scale introduction of CT
scanning around this period. We did not apply any other
limitations to the search.
For the first clinical question, the MeSH terms and key-
words were; ((head trauma) OR (brain injury) OR (head
injury) OR (traumatic head injury) OR (traumatic brain
injury)) AND (minimal OR mild OR minor OR moder-
ate) AND (management OR predictors OR predictor).
For the second clinical question we used; ((head trauma)
OR (brain injury) OR (head injury) OR (traumatic head
injury) OR (traumatic brain injury)) AND (minimal OR
mild OR minor OR moderate) AND (hospitalization OR
hospitalisation OR observation OR admission OR dis-
charge OR delayed OR ((normal OR negative OR repeat
Literature search
Final Guideline
Literature Selection
Evidence Grading
Evaluation of Clinical
Predictors
Evidence Summary and Draft
Recommendation
Recommendation and
Guideline development
Step in work process Method Description/Result
PRISMA In text
In text Figures 2 and 3
CEBM Additional files 2 and 4: Tables S2 and S4
QUADAS Additional files 3 and 5: Tables S3 and S5
In text Additional file 1: Table S1
GRADE Table 1
Deplhi process Tables 2, and
In text Additional files 6-7: Figures S1-2
Figure 1 Flow diagram showing the overall work process.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 3 of 13
OR multiple OR serial OR follow-up) AND (CT OR CCT
OR computed tomography)).
Additional papers were identified by hand-searching
bibliographies of retrieved studies.
Selection criteria and study eligibility
Titles were examined by one author (JU) and borderline
titles were included. Titles that were obviously not rele-
vant were excluded. Abstracts were examined indepen-
dently by two authors (JU, BR) and the third (TI) was
consulted when discrepancies arose. Selected full papers
were independently reviewed by all authors (JU, TI, BR)
and discrepancies were resolved through discussion.
Review articles, letters, expert opinion and editorials
could be retrieved for examination of bibliographies but
were excluded from the analysis. Papers reporting only
children (<18 years) were excluded in both searches. In
cases where essential data was missing or unclear, we
made an attempt to contact corresponding authors for
clarification. Studies including patients with all severities
of head injury were only included if at least 50% of
patients were within the GCS 9 to 15 range.
For the first clinical question, we included studies
reporting patients with admission/initial GCS scores 9
and that included one or more predictive risk factors for
the reference standards of CT findings, intracranial
injury (ICI) and/or neurosurgical intervention. We
decided a priori to only include studies where informa-
tion concerning true positives (TP), false positives (FP),
true negatives (TN) and false negatives (FN) could be
extracted. This information would be necessary to fully
appreciate the possible clinical effect and role of a risk
factor, allowing consideration of other effects than the
positive predictive power. Studies reporting less than 50
patients were excluded. Definitions for risk factors were
defined a priori.
For the second clinical question, we included studies
reporting patients with admission/initial GCS scores 9
with an initial CT scan (normal or abnormal) and con-
tained information regarding clinical characteristics that
were associated with a positive or worsening repeat CT
scan, ICI and/or neurosurgical intervention within 1
week following trauma.
CT findings were defined as any traumatic finding on
head CT. ICI was defined as any intracranial (isolated
non-depressed cranial fractures not included) traumatic
finding on CT. Also, since not all patients can be sub-
jected to CT, absence of ICI was defined as relevant and
robust clinical follow-up suggestive of normal neurologi-
cal functioning (with the exception of classical PCS
symptoms). The decision to consider any CT findings
and ICI as separate reference standards was due to the
difference in clinical importance of these measures. This
approach should also stratify reference standards in a
more homogenous selection compared to a combined
definition. Finally, neurosurgical intervention was
defined as any neurosurgical procedure for a cranial or
intracranial injury within the first week following
trauma. Medical treatment for elevated intracranial pres-
sure, within the first week following trauma, was also
included in this group since some patients with diffuse
brain injury cannot be managed surgically.
Data extraction and quality assessment
Data was extracted by one author (JU) and checked by
another (BR). Data was entered into a predefined protocol
and then inputted into Excel (Microsoft; Redmond, WA,
USA). Evidentiary tables were constructed to summaries
the studies. We decided to address the quality of papers in
different phases, due to the nature of the studies and the
phase of assessment. Firstly, all retrieved studies were
independently graded by all authors in the task force (JU,
TI, BR) according to the Centre of Evidence Based Medi-
cine (CEBM) diagnosis criteria [23]. Discrepancies in grad-
ing were resolved through discussion. Quality ratings
ranged from 1 (strongest evidence, for instance reports of
clinical decision rules and high quality validation studies)
to 5 (weakest evidence, often expert opinion). Studies
receiving CEBM scores of 5 were excluded.
Studies were then graded according to the Quality
Assessment of Diagnostic Accuracy Studies (QUADAS)
tool [24], which was modified for the purpose of the
review. This tool considers 14 criteria relevant to diagnos-
tic studies accounting for bias (items 3 to 7, 10 to 12),
variability (items 1 and 2) and reporting (items 8 and 9).
Items 4 (regarding the time period between index and
reference test) and 7 (regarding the independency of the
reference test) were omitted with regard to the selection
criteria and the previously applied CEBM criteria. Addi-
tionally, item 3 (regarding the ability of the reference test
to correctly classify the target condition) was applied to
CT findings, ICI and neurosurgery separately.
Data analysis
Although extracted data regarding the first clinical ques-
tion, predictors of CT findings, ICI and neurosurgery,
could theoretically be summarized in a meta-analysis, the
task force decided a priori not to perform such an analysis
for the purpose of development of the guidelines, indepen-
dent of heterogeneity between studies. We felt combining
the data in this way could mislead the working group in
the consensus process and opted to instead present
uncombined data for studies including their quality assess-
ment. We therefore calculated individual positive likeli-
hood ratios (PLR) and negative likelihood ratios (NLR) for
each risk factor with respect to the corresponding refer-
ence test (CT, ICI or neurosurgery) and the prevalence
of both the reference test and the risk factor in the
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 4 of 13
population. We felt that these indices would represent the
most relevant clinical applications for the working group
when considering the recommendations. For the second
clinical question, we presented only descriptive analysis.
Evidence summary and recommendations draft
Recommendations were formed by the task force (JU, TI,
BR) based upon the evidence in accordance with the
GRADE system [20,25]. This system is increasingly been
used in the development of recommendations and allows
consideration of aspects other than level of evidence in
determining the strength of a recommendation [25].
Clinical predictors were chosen based upon the summar-
ized evidence (see Additional file 1, Table S1). Focus was
put on the more severe outcome variables (need for neu-
rosurgery being of critical importance), but ICI and any
CT findings were also considered, especially in cases
where the evidence concerning neurosurgery was poor
and/or inconsistent. We also considered the prevalence
of the risk factors in the studied cohorts. Risk factors
relatively common in a population would lead to many
CT scans and these risk factors would therefore need to
show high predictive abilities to be included.
The summarized quality of evidence, from studies
forming the basis of a recommendation, was graded from
high quality to very low quality, see Table 1. Evidence
was initially considered high quality when derived from
cohort studies reporting patients with diagnostic uncer-
tainty and appropriate reference standards, as described
earlier. Evidence could be downgraded due to risk of bias
(selection (population indirectness), verification, observer
and reporting), outcome indirectness (balance between
the presumed influence on patient outcome of the test
result (combination of risk factors) in relation to the
complications and resource use of the test), inconsistency
(large differences in prevalence of reference tests, preva-
lence of risk factors, PLR or NLR) or differing general
results between studies), impreciseness (studies with
small number of patients and few positive CT, ICI or
neurosurgery events) and suspicion of publication bias
(small number of studies, industry funding).
Recommendations, relating to the clinical questions,
were classed as strong (we recommend...), weak (we
suggest...) or uncertain (we cannot recommend...) (see
Table 1). For this process, careful consideration was again
made to risk/benefit aspects of patient-important outcomes
(need for neurosurgery was classed as the most important)
in relation to test results, including assumptions for pretest
probabilities (different magnitudes of risk for a positive
reference result of CT, ICI or neurosurgery) for different
patients, quality of evidence, uncertainty of the preferences
and values for outcomes and the use of health care
resources. Therefore, it is theoretically possible to achieve a
strong recommendation despite low quality evidence or vice
versa.
Recommendations and guideline development
Based upon the recommendations, a draft for the updated
guidelines was constructed by the task force. Following
this, a modified Delphi process was used [26], involving
the working group previously described, consisting of at
least two rounds of consensus. The a priori criteria to
determine acceptance, rejection or lack of consensus are
shown in Table 2. In the first round, the recommenda-
tions, including data from included studies with CEBM,
QUADAS and GRADE evaluations together with a guide-
line draft were sent via email to the working group.
Ratings, including feedback, were anonymously collected.
The task force adjusted the recommendations and draft
based upon these responses. Then, in conjunction with a
2-day SNC meeting in September 2012 outside Copenha-
gen, Denmark, results were discussed and suggestions for
improvements made. Following this, the second round of
Delhi was completed via email. Additional rounds would
be undertaken if necessary. The task force and working
group were urged to consider the GRADE aspects pre-
viously mentioned, especially health risk/benefit aspects
including resource use, as well as side effects and risks
(misclassification of patients), at all stages of development.
The final guidelines were evaluated, independently of
the task force and working group, in the ED of Skane
University Hospital, Malmo, Sweden, to judge clarity of
presentation and ease of use. Simultaneously, the guide-
lines were evaluated by important stakeholders from
specialties directly involved in the everyday management
of these patients. Feedback was documented and appro-
priate changes were made, if necessary, but only to con-
sensus aspects. Finally, the working group reapproved
the guidelines after presentation of changes and feed-
back from the evaluation.
Implementation, monitoring and future updates
Guidelines will only be successful if they are used correctly
and on a wide scale. Previous experience with the 2000
Scandinavian guidelines has shown poor compliance and
varying degrees of implementation success [27,28]. Imple-
mentation and monitoring strategies were discussed within
the working group in order to facilitate long-term successful
use of the guidelines in Scandinavia. Focus was put on over-
coming barriers to application and effectively using available
resources. The working group also outlined a procedure
and approximate time period for updating the guidelines.
Results
The search and selection process is shown in Figures 2
and 3 for the two clinical questions.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 5 of 13
For the first clinical question, we found 72 studies that
adhered to our inclusion criteria (see Additional File 2,
Table S2 for evidentiary information). These studies
included 226,606 individual patients. The level of evidence
according to CEBM was variable and overall judged to be
moderate (see Additional file 2, Table S2). Quality assess-
ment with the QUADAS tool (see Additional file 3, Table
S3) showed substantial bias in the studies, particularly
concerning the representativeness of the studied popula-
tion (selection bias, criteria 1), blinding of the index test
(criteria 8) and withdrawals (criteria 12). Studies scored
better regarding the reporting of selection criteria (criteria
2) and most had acceptable reference standards (criteria
3), although they were often described poorly.
Clinical predictors, with according source study, PLR,
NLR, reference test prevalence and risk factor preva-
lence are shown in Additional file 1, Table S1.
With regard to the second clinical question, we found
21 studies adhering to our inclusion criteria (see Addi-
tional file 4, Table S4 for evidentiary information and
relevant results). The CEBM rating was generally low,
with several studies reporting non-independent reference
standards (see Additional file 4, Table S4). QUADAS
assessment showed selection bias in most studies (criteria
1). Other consistent weaknesses of the studies were a lack
of reference test description and blinding (see Additional
file 5, Table S5 for details).
Recommendations
Based upon the evidence, drafts for recommendations,
guidelines and written discharge advice were constructed
by the task force. These, with according presentation of
the evidence (Additional files 1, 2, 3, 4, 5, Tables S1-S5),
were reviewed by the working group using the predefined
Delphi process. Following round 1 (see Table 3), discus-
sion in the working group concerned points 4 and 7. Since
point 7 regarded the overall guidelines, minor adjustments
were also made to other points. Only consensus points
were changed (the risk factors shunt-treated hydrocepha-
lus and the combination of age >65 and antiplatelet medi-
cation were added, discharge advice was simplified,
monitoring routines were adjusted and the graphical lay-
out of the guidelines was improved).
Following round 2 (see Table 4), consensus was achieved
in favor of all recommendations, the guidelines and the
discharge instructions. One recommendation, concerning
Table 1 Grading of Recommendations Assessment, Development and Evaluation (GRADE) system [24] for rating
quality of evidence and strength of recommendation
Factor Description
Evidence:
High quality Considerable confidence of the estimate of effect. Further research is very unlikely to change our confidence in the
estimated effect.
Moderate quality Confidence that the estimate is close to the truth. Further research is likely to have an important impact on our
confidence in the estimate effect and may change the estimate.
Low quality Limited confidence in the effect. Further research is likely to have an important impact on our confidence in the
estimate effect and is likely to change the estimate.
Very low quality Little confidence in the effect estimate. Any change of effect is uncertain.
Recommendation:
Strong: We recommend... A strong recommendation indicates that most well informed people will make the same choice
Weak: We suggest... A weak recommendation indicates that the majority of well informed people will make the same choice but a
substantial minority will not
Uncertain: We cannot
recommend...
No specific recommendation for or against
Factors influencing the strength of the recommendation include evidence quality, risk/benefit aspects of presumed patient-important outcomes, costs and
uncertainty concerning values and preferences.
Table 2 A priori established seven-point response scale and criteria to determine acceptance, rejection or lack of
consensus for recommendations and guidelines for the working group using a modified Delphi process [25]
Level of agreement
Strongly
disagree
Disagree Moderately
disagree
Neither agree or disagree Moderately
agree
Agree Strongly
agree
Score 1 2 3 4 5 6 7
Criteria 75% of respondents score 3 on the 7-point scale All other situations 75% of respondents score 5 on the 7-
point scale
Result Consensus against No consensus Consensus in favor
Action Reject recommendation Indicates no consensus has been
reached
Accept recommendation
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 6 of 13
clinical question 1, was removed due to the working group
finding the information irrelevant, despite consensus. This
recommendation was an uncertain recommendation (we
cannot recommend...) for risk factors not included in the
other recommendations (such as headache, intoxication,
nausea and amnesia). The working group felt this recom-
mendation was unnecessary and confusing, shifting focus
from the important recommendations below.
The final recommendations, based purely on evidence,
are presented below.
Clinical question 1: Which adult patients with minimal,
mild and moderate head injury need a head CT and
which patients may be directly discharged?
(1) We recommend that adult patients after mild and
moderate head injury with GCS 14, loss of consciousness,
repeated (2) vomiting, anticoagulant therapy or coagula-
tion disorders, clinical signs of depressed or basal skull
fracture, post-traumatic seizures or focal neurological defi-
cits should have a CT scan (moderate quality, strong
recommendation).
Excluded by title
n=3295
Abstracts
n=401
Titles initially screened
n=3696
Full-text papers
n=201
Additional papers from
reference lists of retrieved
papers
n=27
Excluded by abstract
n=200
Papers included in review
n=72
Excluded by full-text n=156
Not relevant n=79
No data n=24
Reporting only
children n=43
<50 patients n=6
Duplicate data n=4
Full-text papers
n=228
Figure 2 Adapted Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram showing the review
process with reference to the clinical question: Which adult patients with minimal, mild and moderate head injury need a head CT
and which patients may be directly discharged?.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 7 of 13
The evidence was initially of high quality but was down-
graded due to limitations in study design (mostly selection
bias), indirectness (outcomes were rarely reported) and
impreciseness (different magnitudes of predictive power of
risk factors between studies). However, the strength of the
recommendation was view as strong by the working
group, considering the seriousness of the complication
and health/economic impact of missing a patient with a
neurosurgical lesion. The working group also discussed
older age (60 years and 65 years) as well as antiplatelet
medication as risk factors of importance, partly due to the
presence of these criteria in other guidelines and decision
rules. However, the predictive ability was only moderate
and these individual risk factors would lead to an unaccep-
table CT increase and so consensus was not to include
these in our recommendation.
(2) We recommend that adult patients after mild head
injury with GCS 14 and no risk factors (anticoagulant
therapy or coagulation disorders, post-traumatic seizures,
clinical signs of depressed or basal skull fracture, focal
Excluded by title
n=2795
Abstracts
n=131
Titles initially screened
n=2926
Full-text papers
n=33
Additional papers from
reference lists of retrieved
papers
n=12
Excluded by abstract
n=98
Papers included in review
n=21
Excluded by full-text n=24
Not relevant n=20
No data n=2
Reporting only
children n=2
Full-text papers
n=45
Figure 3 Adapted Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram showing the review
process with reference to the clinical question: Which adult patients with minimal, mild and moderate head injury need in-hospital
observation and/or a repeat head CT?.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 8 of 13
neurological deficits), or GCS 15 with loss of conscious-
ness or repeated (2) vomiting and no other risk factors,
be sampled for analysis of S100B if less than 6 h have
elapsed following trauma. If S100B is less than 0.10 g/l,
the patient may be discharged without a CT (moderate
quality, strong recommendation).
The evidence was initially of high quality but was
downgraded due to study design (mostly selection bias)
and indirectness (outcomes were rarely reported). How-
ever, studies consistently show that low S100B levels
can be used to select patients who do not need a CT
scan and, hence, may save valuable resources. Of the
few missed patients in the literature, almost all are non-
neurosurgical lesions. Some studies include risk factors
such as GCS 13, anticoagulation and focal neurological
deficits in the inclusion criteria. The working group,
however, found these risk factors to be too predictive of
intracranial injury.
This recommendation may seem conflicting with
recommendation 1, above. However, S100B is recom-
mended as an option for reducing unnecessary CT
scans in a subgroup of Mild head injury patients with
low risk for intracranial complication and/or neurosurgi-
cal intervention.
(3) We recommend that adult patients after minimal
and mild head injury with GCS 15 and without risk fac-
tors (loss of consciousness, repeated (2) vomiting,
anticoagulation therapy or coagulation disorders, post-
traumatic seizures, clinical signs of depressed or basal
skull fracture, focal neurological deficits) can be dis-
charged from the hospital without a CT scan (moderate
quality, strong recommendation).
The evidence was initially of high quality but was
downgraded due to limitations in study design (mostly
selection bias), indirectness (outcomes were rarely
reported) and impreciseness (different magnitudes of
predictive power of risk factors between studies). The
working group felt, however, that the large proportion
of patients with head injury would fall into this category
and that a CT policy in all these patients would not be
health/economically viable considering the very low risk
of intracranial injury, and even lower risk of neurosur-
gery, in this patient group. As previously discussed,
older age and antiplatelet medication was again consid-
ered but rejected by the working group.
Clinical question 2: Which adult patients with minimal,
mild and moderate head injury need in-hospital
observation and/or a repeat head CT?
(1) We suggest that all adult patients after head injury
with GCS 13, clinical signs of depressed or basal skull
fracture, anticoagulation therapy or coagulation disorder,
post-traumatic seizure or focal neurological deficit
should have a CT scan and be admitted to hospital for
observation, irrespective of CT findings (low quality,
weak recommendation).
The evidence was sparse and also of low quality due to
study limitations (selection bias) and inconsistency in
findings. The working group felt that it would not be
good clinical practice to discharge patients with any of
these risk factors, despite the low quality of evidence.
(2) We recommend that repeat CT scans should be per-
formed in patients with neurological and/or GCS (2
points) deterioration (low quality, strong recommendation).
The evidence was of moderate quality and was down-
graded due to serious limitations in study design and
some inconsistency. Most of the evidence indicates that
routine repeat CT of these patients with or without CT
findings is unnecessary in the absence of clinical deteriora-
tion, specifically deterioration of GCS >2 points and/or
Table 3 Results of the modified Delphi process, round 1
Delphi point Working group member Result Cf/nC/Ca
1 2 3 4 5 6 7 8 9 10
1 6 6 6 6 2 6 6 5 7 7 90% Cf
2 6 6 6 - 3 6 6 6 4 7 78% Cf
3 7 6 7 6 3 6 6 7 1 7 80% Cf
4 5 4 4 6 2 6 6 6 6 2 60% nC
5 6 5 6 6 7 6 6 7 6 6 100% Cf
6 6 6 7 4 7 6 6 6 7 7 90% Cf
7 6 6 5 6 2 6 6 - 4 3 67% nC
8 5 5 6 6 6 6 6 7 - 3 89% Cf
9 5 - 5 6 6 6 6 6 - 5 100% Cf
Delphi points 1 to 3 refer to recommendations 1 to 3 concerning clinical
question 1, point 4 refers to a recommendation that was dropped due to
irrelevance (see main text), points 5 and 6 refer to recommendations 1 and 2
concerning clinical question 2, point 7 refers to the guideline draft including
the help sheet, point 8 refers to the written discharge advice and point 9 to
the in-hospital monitoring routines.
Ca = consensus against; Cf = consensus in favor; nC = no consensus.
Table 4 Results of the modified Delphi process, round 2
Delphi point Working group member Result Cf/nC/Ca
1 2 3 4 5 6 7 8 9 10
1 7 6 3 6 7 7 6 7 88% Cf
2 - 6 4 6 6 6 6 7 86% Cf
3 7 6 3 6 6 6 7 7 88% Cf
4 7 6 6 6 6 3 7 6 88% Cf
5 7 6 7 6 7 - 6 7 100% Cf
6 7 7 7 6 7 - - 7 100% Cf
7 7 6 7 6 6 7 5 7 100% Cf
8 7 6 4 - - - 6 7 80% Cf
9 7 6 6 5 7 - 6 7 100% Cf
Two members did not reply. Delphi points 1 to 3 refer to recommendations 1
to 3 concerning clinical question 1, point 4 refers to a recommendation that
was finally dropped due to irrelevance (see main text), points 5 and 6 refer to
recommendations 1 and 2 concerning clinical question 2, point 7 refers to the
guideline draft including the help sheet, point 8 refers to the written
discharge advice and point 9 to the in-hospital monitoring routines.
Ca = consensus against; Cf = consensus in favor; nC = no consensus.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 9 of 13
neurological status. A strong recommendation was chosen
in spite of weak evidence due to the seriousness of the
condition. Clinical aspects such as anticoagulation and
persistent neurological findings were discussed but the
working group could not reach consensus on a recom-
mendation for follow-up scans in these patients.
Guidelines
Based upon the recommendations, guidelines were con-
structed. The addition of shunt-treated hydrocephalus
was based upon consensus in the working group with
little evidence to support this. The working group dis-
cussed risk factors relating to trauma mechanism and
multitrauma injuries but found these difficult to recom-
mend, mainly due to practical issues with clinical appli-
cation. We considered serious extracranial injuries
(defined as Abbreviated Injury Score (AIS) >3 to any
organ system, for instance large (for example, femur)
fractures or serious thoracic or abdominal injuries) as a
risk factor due to the probability of a higher magnitude
of trauma, need for extracranial CT and the poorer
prognosis of brain injury in these patients. However, we
finally decided to omit this as a risk factor primarily due
to the difficulty of classifying this risk factor in a busy
clinical scenario. Additionally, predictive ability was gen-
erally only moderate for these risk factors. Also, loss of
consciousness was expanded to suspected/confirmed
loss of consciousness, as it is often difficult to confirm
this finding in the clinical setting. Patients who could
not clearly deny any loss of consciousness should be
classed as suspected. Finally, the working group could
not recommend older age or antiplatelet medication as
individual risk factors due to the unacceptable CT
increase such a recommendation would cause, in combi-
nation with only moderate predictive abilities. However,
consensus was reached to combine these into one risk
factor, namely age 65 years and antiplatelet medication.
Written instructions for patients being discharged were
adapted from the 2000 guidelines with consideration of
the National Institute of Clinical Excellence (NICE)
instructions [29] and a proposal for evidence-based
instructions from Fung et al. [30], (see Additional file 6,
Figure S1). With the Scandinavian setting in mind, the
discharge sheet was heavily simplified for clarity. Obser-
vation and monitoring routines for admitted patients
were based on consensus in the working group. We dis-
cussed the intensity of monitoring routines in relation to
the severity of the complications and burden on hospital
wards and finally decided that these should be relatively
frequent shortly after trauma (the first 4 h) with de-esca-
lation over time. Reasonably, most admitted patients will
arrive to a ward after at least 4 h and hence already have
passed the 15-minute interval period. Also, these moni-
toring routines will only be used in small minority of
patients as moderate and high-risk patients are relatively
uncommon and other patients should preferentially have
a CT.
Feedback from ED evaluation and from stakeholders
resulted in minor changes to wording and general
appearance of the guidelines. All stakeholders and the
working group approved the final version, see Additional
file 7, Figure S2.
Implementation, monitoring and future updates
The working group decided on implementation by SNC
members in their respective countries. This would be
performed through a combination of written and oral
presentations in national medical journals and national
meetings, respectively. We discussed barriers to imple-
mentation and decided that the most important of these
was probably the absence of sufficient education con-
cerning head injury management in Scandinavia. We
would attempt to further facilitate implementation by
printing flyers and placards with the guidelines and to
send these to Scandinavian hospitals. We would also
initiate national training initiatives within the respective
Scandinavian countries.
With respect to monitoring aspects, the working group
decided to plan a questionnaire to Scandinavian physi-
cians treating head injury to determine the present use of
guidelines, similar to previous efforts [31]. At 1 year fol-
lowing implementation, a follow-up questionnaire will be
sent out to establish changes in management routines.
We will also initiate studies examining compliance with
the guidelines, as previously established in Norway
[27,28], and attempt to improve insufficient use of the
guidelines depending on these results. Finally, we will
initiate a prospective validation study, also comparing the
performance of our guidelines with other guidelines,
decision rules and, importantly, unstructured physician
judgment [32].
The working group decided that an update of the
guidelines would be necessary in 2015. This would
include evidence updates concerning the clinical ques-
tions addressed in the present update and would further
examine the observation and monitoring routines for
admitted patients.
Discussion
Since 2000, considerable evidence has emerged concern-
ing the initial management, particularly risk factors for
CT selection, of minimal, mild and moderate head injury.
The work presented here is, in contrast to our previous
guidelines, confined to adults but a similar effort regard-
ing management of children is underway. Although these
guidelines can theoretically be used in any setting, they
were designed with the Scandinavian emergency care set-
ting in mind. They are also designed to primarily identify
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 10 of 13
patients needing neurosurgical or medical intervention,
with traumatic CT findings being the secondary identifi-
cation goal.
In summary, the evidence was of reasonable quality
referring to the predictive ability of risk factors for compli-
cations following head injury in these patients. Unsurpris-
ingly, many of the risk factors included here are also
found in other guidelines and decision rules [6,9-11,29,33].
However, several differences can be noted. We found that
the predictive power of amnesia was too low to be
included. This risk factor was present in the SNC guide-
lines from 2000, mostly due to the difficultly in ruling out
loss of consciousness in some patients. For this reason, we
include suspected loss of consciousness as a risk factor.
Risk factors such as intoxication, trauma above the cla-
vicles, nausea, vertigo and headache were not included
due to poor predictive ability combined with a high pre-
valence of these factors in the head injury population.
The working group found injury mechanisms compli-
cated to use practically in initial management and
decided not to include these as risk factors.
Older age, most often defined as 60 or 65 years, is
often included in other guidelines. The predictive ability of
this risk factor was only moderate and there was consider-
able uncertainty in the group with regard to patient
important outcomes and resource use. The number of
people in older age groups in industrialized countries is
increasing [34] and the increased CT rate that would be
associated with this risk factor was deemed unacceptable.
Also, the risk factor is common in the head injury cohorts,
with between 10% and 45% of patients being over 65 years
of age in reported cohorts of mild [10,35-38] and moder-
ate [39] TBI. Fabbri et al. recently presented results con-
sidering the combination of older age and antiplatelet
agents [40]. Despite the lack of good evidence for this
combination, consensus was reached to include age 65
years in combination with any antiplatelet agent as a risk
factor. It is reasonable to expect that the combination
would be more predictive of complications after head
injury and result in a smaller CT rate increase when com-
pared to the risk factors used individually. Additionally, it
has been suggested that antiplatelet medication may be at
least partly responsible for the higher risks for intracranial
complications seen after head injury in older patients [40].
Shunt-treated hydrocephalus was added purely based
on consensus, with evidence derived from expert opinion
in the group. We acknowledge the poor evidence-based
background to this decision but this patient group is
uncommon and will not lead to a noticeable increase in
CT scanning.
Evidence concerning repeat CT was reasonable but lack-
ing concerning both written discharge advice and observa-
tion routines. These aspects were therefore based heavily
upon consensus with special weight put on adaptation to
the Scandinavian health care system. Since in-hospital
observation consumes valuable resources, there is a need
for stronger evidence examining the need and magnitude
of these routines.
For the first time, a brain biomarker has been intro-
duced into clinical practice guidelines. Using a low cut-
off of 0.10 g/l, the biomarker has shown considerable
ability to predict the absence of CT pathology and neuro-
surgical intervention [36,41,42]. This negative prediction
is welcomed since all other risk factors are of positive
predictive nature. S100B allows for a safe reduction in
CT scans in a subpopulation of patients with mild head
injury. In order to maintain the theoretical safety and
cost-saving ability, the biomarker should primarily not
exhibit false negative results. Also, the biomarker should
only be taken in patients that would usually receive a CT
scan and the fraction of negative S100B results (below
cut-off) should be as large as possible. S100B is clinically
unspecific [43,44] and has a short half-life [45]. There-
fore, patients with extracranial injuries and those seeking
care more than 6 h after trauma are not good candidates
for S100B sampling due to a risk of false positives and
negatives, respectively. Some patients have risk factors
with higher predictive abilities and also factors that
would usually warrant admission irrespective of CT find-
ings. This group is therefore also not suitable for S100B
sampling. Despite the relatively good evidence for S100B
in this setting, biomarkers have historically had different
effects in actual management and the clinical impact and
health economic implications may alter future recom-
mendations. Based upon the current evidence and clinical
setting, however, this biomarker should safely reduce
resource use if used correctly since low levels are very
uncommon in patients needing neurosurgical interven-
tion in this setting.
There are limitations to the process outlined in this
paper. Although the recommendations are based upon
evidence, there were elements of consensus input to the
final guidelines. This is inevitable when dealing with
these injuries and we attempted to minimize the negative
effects of this through our stringent and extensive metho-
dology using the best available tools. Particularly, the
GRADE system [20] allows consideration of other impor-
tant aspects other than the level of evidence in recom-
mendations. The derivation and validation of predictive
risk factors as performed by other authors [6,10,18]
would hardly be feasible in Scandinavia and would only
account for one aspect of the management guidelines.
Our methodology was judged as the most feasible consid-
ering the target population. However, external clinical
validation of our guidelines is welcomed and would natu-
rally support successful implementation.
Finally, these guidelines are, by definition, guidelines
and should be utilized accordingly. They are primarily
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 11 of 13
designed as evidence and consensus-based guidance for
physicians who are not experts in the field. Physicians
who have considerable experience with these patients
should naturally be allowed to defer from the guidelines
according to clinical judgment.
Conclusions
We present guidelines for initial management of adults
with minimal, mild and moderate head injury based upon
a thorough evidence and consensus-based methodology.
The guidelines are primarily designed to detect complica-
tions after head injury needing either neurosurgical or
medical intervention. They can be applied to all adult
patients and include aspects such as CT and admission
selection, repeat CT selection, monitoring routines and
discharge aspects. However, we suggest external valida-
tion before they are widely implemented. Furthermore,
areas with poor evidence, such as clinical monitoring
routines for patients following head injury, should be
addressed in future studies.
Additional material
Additional file 1: Table S1. Predictive risk factors with according studies
derived from the clinical question: Which adult patients with minimal,
mild and moderate head injury need a head CT and which patients may
be directly discharged? showing corresponding positive likelihood ratio
(PLR), negative likelihood ratio (NLR), prevalence for the reference test
(CT findings (CT)), intracranial injury (ICI) and neurosurgery (NS)) and the
risk factor prevalence. CT = computed tomography.
Additional file 2: Table S2. Evidentiary table of studies with reference
to the clinical question: Which adult patients with minimal, mild and
moderate head injury need a head CT and which patients may be
directly discharged?. CT = computed tomography.
Additional file 3: Table S3. Modified Quality Assessment of Diagnostic
Accuracy Studies (QUADAS) grading of studies referring to the clinical
question: Which adult patients with minimal, mild and moderate head
injury need a head CT and which patients may be directly discharged?.
CT = computed tomography.
Additional file 4: Table S4. Evidentiary table of studies with reference
to the clinical question: Which adult patients with minimal, mild and
moderate head injury need in-hospital observation and/or a repeat head
CT?. CT = computed tomography.
Additional file 5: Table S5. Modified Quality Assessment of Diagnostic
Accuracy Studies (QUADAS) grading of studies referring to the clinical
question: Which adult patients with minimal, mild and moderate head
injury need in-hospital observation and/or a repeat head CT?. CT =
computed tomography.
Additional file 6: Figure S1. Discharge advice for adults following
minimal, mild and moderate head injury.
Additional file 7: Figure S2. Final management guidelines for adults
following minimal, mild and moderate head injury (including help sheet).
Authors contributions
This work was initiated and designed by JU with input from the SNC
committee. JU, TI and BR all participated in the review process and
recommendation/guideline draft, see text for details. For the Delphi process,
the entire SNC working group (see below), including JU, TI and BR, was
involved. Clinical stakeholders were involved in later processes of guideline
approval, see main text. All main authors approved the final manuscript.
Competing interests
JU and BR are organizers of the international BMBD conference (http://www.
bmbd.org) concerning neurological biomarkers in brain injury. Some SNC
meetings have been sponsored by Roche Diagnostics Scandinavia AB. These
sponsors have had no involvement or influence on any aspects of the SNC
work. JU and BR have been invited to speak at educational meetings
arranged by Roche Diagnostics Scandinavia AB but Roche have always
remained strictly independent from the scientific program and content and
these took place before the present work was initiated. JU, TI and BR have
in previous research received compensation for travel expenses and lab
analysis from Roche AB, Diasorin AB and Sangtec Medical AB. None of these
had any involvement or influence on any scientific aspects.
Acknowledgements
SNC working group: Carsten Kock-Jensen (SNC president), Hammel,
Denmark; Johan Undn, Malmo, Sweden; Bertil Romner, Copenhagen,
Denmark; Tor Ingebrigtsen, Tromso, Norway; Terje Sundstrom, Bergen,
Norway; Jacob Springborg, Copenhagen, Denmark; Knut Wester, Bergen,
Norway; Per Olof Grnde, Lund, Sweden; Vagn Eskesen, Copenhagen,
Denmark; Snorre Sollid, Tromso, Norway; Niels Juul, Aarhus, Denmark; Bo-
Michael Bellander, Stockholm, Sweden; Bent Dahl, Aarhus, Denmark; Christina
Rosenlund, Aarhus, Denmark; Peter Reinstrup, Lund, Sweden.
Additional clinical stakeholders: Per Wihlborg, Malmo, Sweden; Louis Riddez,
Stockholm, Sweden; Steen Mejdahl, Copenhagen, Denmark; Jesper Erdal,
Copenhagen, Denmark; Ole Molgaard, Aarhus, Denmark; Knut Melhuus, Oslo,
Norway; Martine Enger, Oslo, Norway; Kenneth Thors, Stavanger, Norway.
This work was funded by the non-commercial Swedish state sources of:
Region Skne, Sdra Sjukvrdsregionen and Vetenskapsrdet Hallands
Sjukhus, all in Sweden. None of the funding bodies had any involvement or
influence on any aspects of the work.
Author details
1
Department of Intensive Care and Perioperative Medicine, Institute for
Clinical Sciences, Sdra Frstadsgatan 101, 20502 Malm, Sweden.
2
Department of Neurosurgery, Institute for Clinical Medicine, Sykehusveien
38, 9038 Troms, Norway.
3
Department of Neurosurgery, Institute for Clinical
Medicine, Blegdamsvej 9, 2100 Copenhagen, Denmark.
Received: 18 October 2012 Accepted: 25 February 2013
Published: 25 February 2013
References
1. Cassidy JD, Carroll LJ, Peloso PM, Borg J, von Holst H, Holm L, Kraus J,
Coronado VG: Incidence, risk factors and prevention of mild traumatic
brain injury: results of the WHO Collaborating Centre Task Force on Mild
Traumatic Brain Injury. J Rehabil Med 2004, 43(Suppl):28-60.
2. Saab M, Gray A, Hodgkinson D, Irfan M: Warfarin and the apparent minor
head injury. J Accid Emerg Med 1996, 13:208-209.
3. Rutland-Brown W, Langlois JA, Thomas KE, Xi YL: Incidence of traumatic
brain injury in the United States, 2003. J Head Trauma Rehabil 2006,
21:544-548.
4. Soreide K, Kruger AJ, Vardal AL, Ellingsen CL, Soreide E, Lossius HM:
Epidemiology and contemporary patterns of trauma deaths: changing
place, similar pace, older face. World J Surg 2007, 31:2092-2103.
5. Ingebrigtsen T, Romner B, Kock-Jensen C: Scandinavian guidelines for
initial management of minimal, mild, and moderate head injuries. The
Scandinavian Neurotrauma Committee. J Trauma 2000, 48:760-766.
6. Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM:
Indications for computed tomography in patients with minor head
injury. N Engl J Med 2000, 343:100-105.
7. af Geijerstam JL, Britton M: Mild head injury-mortality and complication
rate: meta-analysis of findings in a systematic literature review. Acta
Neurochir (Wien) 2003, 145:843-850.
8. Morton MJ, Korley FK: Head computed tomography use in the
emergency department for mild traumatic brain injury: integrating
evidence into practice for the resident physician. Ann Emerg Med 2012,
60:361-367.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 12 of 13
9. Mower WR, Hoffman JR, Herbert M, Wolfson AB, Pollack CV Jr, Zucker MI:
Developing a decision instrument to guide computed tomographic
imaging of blunt head injury patients. J Trauma 2005, 59:954-959.
10. Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A,
McKnight RD, Verbeek R, Brison R, Cass D, Eisenhauer ME, Greenberg G,
Worthington J: The Canadian CT Head Rule for patients with minor head
injury. Lancet 2001, 357:1391-1396.
11. Smits M, Dippel DW, Steyerberg EW, de Haan GG, Dekker HM, Vos PE,
Kool DR, Nederkoorn PJ, Hofman PA, Twijnstra A, Tanghe HL, Hunink MG:
Predicting intracranial traumatic findings on computed tomography in
patients with minor head injury: the CHIP prediction rule. Ann Intern Med
2007, 146:397-405.
12. Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R,
Berrington de Gonzalez A, Miglioretti DL: Radiation dose associated with
common computed tomography examinations and the associated
lifetime attributable risk of cancer. Arch Intern Med 2009, 169:2078-2086.
13. Jagoda AS, Bazarian JJ, Bruns JJ Jr, Cantrill SV, Gean AD, Howard PK,
Ghajar J, Riggio S, Wright DW, Wears RL, Bakshy A, Burgess P, Wald MM,
Whitson RR, American College of Emergency Physicians; Centers for Disease
Control and Prevention: Clinical policy: neuroimaging and
decisionmaking in adult mild traumatic brain injury in the acute setting.
Ann Emerg Med 2008, 52:714-748.
14. af Geijerstam JL, Britton M: Mild head injury: reliability of early computed
tomographic findings in triage for admission. Emerg Med J 2005,
22:103-107.
15. Tauber M, Koller H, Moroder P, Hitzl W, Resch H: Secondary intracranial
hemorrhage after mild head injury in patients with low-dose
acetylsalicylate acid prophylaxis. J Trauma 2009, 67:521-525.
16. Livingston DH, Lavery RF, Passannante MR, Skurnick JH, Baker S, Fabian TC,
Fry DE, Malangoni MA: Emergency department discharge of patients with
a negative cranial computed tomography scan after minimal head
injury. Ann Surg 2000, 232:126-132.
17. Stein SC, Fabbri A, Servadei F, Glick HA: A critical comparison of clinical
decision instruments for computed tomographic scanning in mild
closed traumatic brain injury in adolescents and adults. Ann Emerg Med
2009, 53:180-188.
18. Smits M, Dippel DW, de Haan GG, Dekker HM, Vos PE, Kool DR,
Nederkoorn PJ, Hofman PA, Twijnstra A, Tanghe HL, Hunink MG: Minor
head injury: guidelines for the use of CTa multicenter validation study.
Radiology 2007, 245:831-838.
19. Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G,
Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J,
Zitzelsberger L, AGREE Next Steps Consortium: AGREE II: advancing
guideline development, reporting and evaluation in health care. J Clin
Epidemiol 2010, 63:1308-1311.
20. Schnemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE,
Williams JW Jr, Kunz R, Craig J, Montori VM, Bossuyt P, Guyatt GH, GRADE
Working Group: Grading quality of evidence and strength of
recommendations for diagnostic tests and strategies. BMJ 2008,
336:1106-1110.
21. Stein SC, Spettell C: The Head Injury Severity Scale (HISS): a practical
classification of closed-head injury. Brain Inj 1995, 9:437-444.
22. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP,
Clarke M, Devereaux PJ, Kleijnen J, Moher D: The PRISMA statement for
reporting systematic reviews and meta-analyses of studies that evaluate
health care interventions: explanation and elaboration. Ann Intern Med
2009, 151:W65-94.
23. Heneghan C: EBM resources on the new CEBM website. Evid Based Med
2009, 14:67.
24. Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J: The development
of QUADAS: a tool for the quality assessment of studies of diagnostic
accuracy included in systematic reviews. BMC Med Res Methodol 2003, 3:25.
25. Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A,
Schunemann HJ: Going from evidence to recommendations. BMJ 2008,
336:1049-1051.
26. Jones J, Hunter D: Consensus methods for medical and health services
research. BMJ 1995, 311:376-380.
27. Heskestad B, Waterloo K, Ingebrigtsen T, Romner B, Harr ME, Helseth E: An
observational study of compliance with the Scandinavian guidelines for
management of minimal, mild and moderate head injury. Scand J
Trauma Resusc Emerg Med 2012, 20:32.
28. Heskestad B, Baardsen R, Helseth E, Ingebrigtsen T: Guideline compliance
in management of minimal, mild, and moderate head injury: high
frequency of noncompliance among individual physicians despite
strong guideline support from clinical leaders. J Trauma 2008,
65:1309-1313.
29. Yates D, Aktar R, Hill J: Assessment, investigation, and early management
of head injury: summary of NICE guidance. BMJ 2007, 335:719-720.
30. Fung M, Willer B, Moreland D, Leddy JJ: A proposal for an evidenced-
based emergency department discharge form for mild traumatic brain
injury. Brain Inj 2006, 20:889-894.
31. Bellner J, Ingebrigtsen T, Romner B: Survey of the management of
patients with minor head injuries in hospitals in Sweden. Acta Neurol
Scand 1999, 100:355-359.
32. Schriger DL, Newman DH: Medical decisionmaking: lets not forget the
physician. Ann Emerg Med 2012, 59:219-220.
33. Vos PE, Alekseenko Y, Battistin L, Ehler E, Gerstenbrand F, Muresanu DF,
Potapov A, Stepan CA, Traubner P, Vecsei L, von Wild K, European
Federation of Neurological Societies: Mild traumatic brain injury. Eur J
Neurol 2012, 19:191-198.
34. Lutz W, Sanderson W, Scherbov S: The coming acceleration of global
population ageing. Nature 2008, 451:716-719.
35. Ibanez J, Arikan F, Pedraza S, Sanchez E, Poca MA, Rodriguez D, Rubio E:
Reliability of clinical guidelines in the detection of patients at risk
following mild head injury: results of a prospective study. J Neurosurg
2004, 100:825-834.
36. Zongo D, Ribreau-Gayon R, Masson F, Laborey M, Contrand B, Salmi LR,
Montaudon D, Beaudeux JL, Meurin A, Dousset V, Loiseau H, Lagarde E:
S100-B protein as a screening tool for the early assessment of minor
head injury. Ann Emerg Med 2012, 59:209-218.
37. Ono K, Wada K, Takahara T, Shirotani T: Indications for computed
tomography in patients with mild head injury. Neurol Med Chir (Tokyo)
2007, 47:291-297.
38. Moore MM, Pasquale MD, Badellino M: Impact of age and anticoagulation:
need for neurosurgical intervention in trauma patients with mild
traumatic brain injury. J Trauma Acute Care Surg 2012, 73:126-130.
39. Fabbri A, Servadei F, Marchesini G, Stein SC, Vandelli A: Early predictors of
unfavourable outcome in subjects with moderate head injury in the
emergency department. J Neurol Neurosurg Psychiatry 2008, 79:567-573.
40. Fabbri A, Servadei F, Marchesini G, Stein SC, Vandelli A: Predicting
intracranial lesions by antiplatelet agents in subjects with mild head
injury. J Neurol Neurosurg Psychiatry 2010, 81:1275-1279.
41. Biberthaler P, Linsenmeier U, Pfeifer KJ, Kroetz M, Mussack T, Kanz KG,
Hoecherl EF, Jonas F, Marzi I, Leucht P, Jochum M, Mutschler W: Serum S-
100B concentration provides additional information fot the indication of
computed tomography in patients after minor head injury: a
prospective multicenter study. Shock 2006, 25:446-453.
42. Unden J, Romner B: Can low serum levels of S100B predict normal CT
findings after minor head injury in adults?: an evidence-based review
and meta-analysis. J Head Trauma Rehabil 2010, 25:228-240.
43. Unden J, Bellner J, Eneroth M, Alling C, Ingebrigtsen T, Romner B: Raised
serum S100B levels after acute bone fractures without cerebral injury.
J Trauma 2005, 58:59-61.
44. Pelinka LE, Bahrami S, Szalay L, Umar F, Redl H: Hemorrhagic shock
induces an S 100 B increase associated with shock severity. Shock 2003,
19:422-426.
45. Jonsson H, Johnsson P, Hoglund P, Alling C, Blomquist S: Elimination of
S100B and renal function after cardiac surgery. J Cardiothorac Vasc Anesth
2000, 14:698-701.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1741-7015/11/50/prepub
doi:10.1186/1741-7015-11-50
Cite this article as: Undn et al.: Scandinavian guidelines for initial
management of minimal, mild and moderate head injuries in adults: an
evidence and consensus-based update. BMC Medicine 2013 11:50.
Undn et al. BMC Medicine 2013, 11:50
http://www.biomedcentral.com/1741-7015/11/50
Page 13 of 13
You might also like
- The Code Stroke Handbook: Approach to the Acute Stroke PatientFrom EverandThe Code Stroke Handbook: Approach to the Acute Stroke PatientNo ratings yet
- Biomarkers For PDFDocument247 pagesBiomarkers For PDFBuga RazvanNo ratings yet
- Assessment Practices Cogn-Comm TBIDocument11 pagesAssessment Practices Cogn-Comm TBIRoisin McdonnellNo ratings yet
- RBANSDocument10 pagesRBANSFanel PutraNo ratings yet
- Management of Cerebral Edema, Brain Compression, and Intracranial PressureDocument29 pagesManagement of Cerebral Edema, Brain Compression, and Intracranial PressureNicolle Carrillo ForeroNo ratings yet
- ATLS 8th EditionDocument50 pagesATLS 8th EditionPaolo VegaNo ratings yet
- Scandinavian Guidelines For Initial Management of Minor and Moderate Head Trauma in ChildrenDocument20 pagesScandinavian Guidelines For Initial Management of Minor and Moderate Head Trauma in ChildrenRafael Mujica OreNo ratings yet
- Research: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryDocument8 pagesResearch: CATCH: A Clinical Decision Rule For The Use of Computed Tomography in Children With Minor Head InjuryCarlos Martin Yafac RiscoNo ratings yet
- Research Manuscript FinalDocument12 pagesResearch Manuscript FinalTHESSNAVARRONo ratings yet
- Subdural Hematoma in Adults - Prognosis and Management - UpToDate PDFDocument17 pagesSubdural Hematoma in Adults - Prognosis and Management - UpToDate PDFLinda RoldánNo ratings yet
- Assis 2017Document19 pagesAssis 2017widyadariNo ratings yet
- ISN KDIGO Early Screening Booklet PRINT UpdatedDocument14 pagesISN KDIGO Early Screening Booklet PRINT Updatedheba.barkasiehNo ratings yet
- CT Brain GuidelinesDocument6 pagesCT Brain GuidelinesMurali G RaoNo ratings yet
- ESCP CraniopharyngiomaDocument21 pagesESCP CraniopharyngiomaHermawan Pramudya IINo ratings yet
- 2020 Article 3403Document11 pages2020 Article 3403Gaetano De BiaseNo ratings yet
- NEJM JW TopGuidelineWatches 2013Document30 pagesNEJM JW TopGuidelineWatches 2013Hoàng TháiNo ratings yet
- 2022 Non-Cardiac SurgeryDocument105 pages2022 Non-Cardiac Surgeryhosameldin ahmedNo ratings yet
- Acute Stroke Intervention: The Heart of The Matter: SciencedirectDocument2 pagesAcute Stroke Intervention: The Heart of The Matter: SciencedirectMarianaPlataNo ratings yet
- FINAL Ranking Top 30 v2Document6 pagesFINAL Ranking Top 30 v2rajayasminNo ratings yet
- Management of Mild and Moderate Head Injuries in Adults: Dana Turliuc, A. CucuDocument11 pagesManagement of Mild and Moderate Head Injuries in Adults: Dana Turliuc, A. CucuSarrah Kusuma DewiNo ratings yet
- Neurosurgery 4 Mental DisordersDocument82 pagesNeurosurgery 4 Mental DisordersTomChristianNo ratings yet
- Minor Ped Head TraumaDocument25 pagesMinor Ped Head Traumalaila.forestaNo ratings yet
- MonitoreoicpnoinvasivoDocument7 pagesMonitoreoicpnoinvasivoCristianMP96No ratings yet
- Tuberous SclerosisDocument17 pagesTuberous SclerosiswardahkhattakNo ratings yet
- Int Forum Allergy Rhinol - 2018 - Mattos - Establishing The Minimal Clinically Important Difference For The QuestionnaireDocument6 pagesInt Forum Allergy Rhinol - 2018 - Mattos - Establishing The Minimal Clinically Important Difference For The QuestionnaireSid TNo ratings yet
- Slide Jurnal NeuroDocument16 pagesSlide Jurnal NeuroWilla MutiaNo ratings yet
- Diagnosis of Idiopathic Normal Pressure Hydrocephalus Is Supported by MRI-based Scheme: A Prospective Cohort StudyDocument11 pagesDiagnosis of Idiopathic Normal Pressure Hydrocephalus Is Supported by MRI-based Scheme: A Prospective Cohort StudyDini NanamiNo ratings yet
- Journal Bedah SarafDocument4 pagesJournal Bedah SarafWisnuardhyHendrawardhanaNo ratings yet
- CPG Management of Percutaneous Coronory Intervention (PCI) 2009Document92 pagesCPG Management of Percutaneous Coronory Intervention (PCI) 2009umiraihana1No ratings yet
- The Management and Outcome For Patients With Chronic Subdural Hematoma: A Prospective, Multicenter, Observational Cohort Study in The United KingdomDocument8 pagesThe Management and Outcome For Patients With Chronic Subdural Hematoma: A Prospective, Multicenter, Observational Cohort Study in The United KingdomRosario RosarioNo ratings yet
- NON CARDIAC SURGERY. ESC POCKET GLS.2022. Larger FontDocument63 pagesNON CARDIAC SURGERY. ESC POCKET GLS.2022. Larger FontGeoNo ratings yet
- Brain Death Scintigraphy V2.0 Final Draft For ApprovalDocument6 pagesBrain Death Scintigraphy V2.0 Final Draft For ApprovalLeticia PortilloNo ratings yet
- ESUR Guidelines On Contrast MediaDocument10 pagesESUR Guidelines On Contrast MediatsimitselisNo ratings yet
- Euro J of Neurology - 2017 - Ferro - European Stroke Organization Guideline For The Diagnosis and Treatment of CerebralDocument11 pagesEuro J of Neurology - 2017 - Ferro - European Stroke Organization Guideline For The Diagnosis and Treatment of CerebralIvan MihailovicNo ratings yet
- Gala TrialDocument11 pagesGala TrialRichard ZhuNo ratings yet
- Testing The Impact of Protocolized Care Of.5Document9 pagesTesting The Impact of Protocolized Care Of.5Nelson Da VegaNo ratings yet
- CPG Unstable AnginaDocument58 pagesCPG Unstable AnginaAmir HassenNo ratings yet
- Cancer de Pulmon Up To DateDocument197 pagesCancer de Pulmon Up To DateFernando HuertasNo ratings yet
- Which CT Features Help Predict Outcome After Head Injury?: PaperDocument5 pagesWhich CT Features Help Predict Outcome After Head Injury?: PaperLady KweeNo ratings yet
- STITCH Protocol 2011Document9 pagesSTITCH Protocol 2011Crhistian GarcíaNo ratings yet
- Outcomes of Prophylactic Cranial Irradiation in Patients With Small Cell Lung Cancer in The Modern Era of Baseline Magnetic Resonance Imaging of TheDocument9 pagesOutcomes of Prophylactic Cranial Irradiation in Patients With Small Cell Lung Cancer in The Modern Era of Baseline Magnetic Resonance Imaging of Theband pulmounandNo ratings yet
- 17.PLDD Vs Surgery RCTDocument9 pages17.PLDD Vs Surgery RCTBeata SviantickaNo ratings yet
- Jurnal CT ScanDocument9 pagesJurnal CT ScanPungki Putra TamaraNo ratings yet
- Clinical Neurology and Neurosurgery: SciencedirectDocument3 pagesClinical Neurology and Neurosurgery: SciencedirectGd SuarantaNo ratings yet
- 2018 Article 1048Document18 pages2018 Article 1048hectorNo ratings yet
- Chronic SDHDocument8 pagesChronic SDHAnonymous A9R0aLsNo ratings yet
- ClinKidneyJ 2015 Marcelli CKJ - Sfu145Document7 pagesClinKidneyJ 2015 Marcelli CKJ - Sfu145Bung HerryNo ratings yet
- Jurnal Syifa 4Document9 pagesJurnal Syifa 4cornelia cindy SRDNo ratings yet
- Rajajee - 2019 PDFDocument91 pagesRajajee - 2019 PDFAlexNo ratings yet
- Treggiari Miriam M Guidelines For The NeurocriticalDocument28 pagesTreggiari Miriam M Guidelines For The NeurocriticalBelén Fabbrizi100% (1)
- Drug-Eluting Stents: A Systematic Review and Economic EvaluationDocument6 pagesDrug-Eluting Stents: A Systematic Review and Economic EvaluationAleksandar CokanovicNo ratings yet
- Department of Brain Repair & RehabilitationDocument23 pagesDepartment of Brain Repair & Rehabilitationkuruvagadda sagarNo ratings yet
- Cerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDocument11 pagesCerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDaniel EllerNo ratings yet
- Jer 206 BBBDocument31 pagesJer 206 BBBVina SalsabilaNo ratings yet
- Journal 4 - Management of Traumatic Brain Injury A Narrative Review of Current EvidenceDocument11 pagesJournal 4 - Management of Traumatic Brain Injury A Narrative Review of Current EvidenceNatalindah Jokiem Woecandra T. D.No ratings yet
- 2023 Guideline Aneurysmal Subarachnoid HemorrhageDocument165 pages2023 Guideline Aneurysmal Subarachnoid Hemorrhagewmy6rf7nypNo ratings yet
- JofIMAB 2019 25 2p2471 2475Document5 pagesJofIMAB 2019 25 2p2471 2475afriskha bulawanNo ratings yet
- 2023 Guideline For The Management of Patients With Aneurysmal Subarachnoid Hemorrhage - A Guideline From The American Heart Association - American Stroke Association - StrokeDocument145 pages2023 Guideline For The Management of Patients With Aneurysmal Subarachnoid Hemorrhage - A Guideline From The American Heart Association - American Stroke Association - StrokeDaniel AraujoNo ratings yet
- Prehospital Stroke Care: New Prospects For Treatment and Clinical ResearchDocument8 pagesPrehospital Stroke Care: New Prospects For Treatment and Clinical ResearchmiriamneuroNo ratings yet
- 2004 Echo Standards PDFDocument25 pages2004 Echo Standards PDFMiki MarzukiNo ratings yet
- Stroke Nursing DissertationDocument4 pagesStroke Nursing DissertationBestCollegePaperWritingServiceCanada100% (1)
- Aneurysmal SAHDocument19 pagesAneurysmal SAHlakshminivas PingaliNo ratings yet
- ARTG - 2022 - Long-Term Outcomes of Patients With Primary Brain Tumors After Acute RehabilitationDocument11 pagesARTG - 2022 - Long-Term Outcomes of Patients With Primary Brain Tumors After Acute RehabilitationSM199021No ratings yet
- Computed-Tomography a Powerful Tool for Diagnosis of Pediatric and Adult Congenital Heart Disease: Methodology and Interpretation GuideFrom EverandComputed-Tomography a Powerful Tool for Diagnosis of Pediatric and Adult Congenital Heart Disease: Methodology and Interpretation GuideNo ratings yet
- State of the Art Techniques in Critical Care Echocardiography: 3D, Tissue, ContrastFrom EverandState of the Art Techniques in Critical Care Echocardiography: 3D, Tissue, ContrastKonstantin YastrebovNo ratings yet
- Daftar Kelulusan MCQSCBT Periode November 2018Document58 pagesDaftar Kelulusan MCQSCBT Periode November 2018larasNo ratings yet
- 3) Karakteristik Anak Yang Menderita Leukemia Akut Rawat Inap Di Rsup H. Adam Malik Medan Tahun 2011-2012 (Sulastriana)Document10 pages3) Karakteristik Anak Yang Menderita Leukemia Akut Rawat Inap Di Rsup H. Adam Malik Medan Tahun 2011-2012 (Sulastriana)Desy RusianaNo ratings yet
- TransDocument52 pagesTransDesy RusianaNo ratings yet
- 9) How I Treat Pediatric AML (Rubnitz JE)Document10 pages9) How I Treat Pediatric AML (Rubnitz JE)Desy RusianaNo ratings yet
- AML (Lymphoma Society)Document56 pagesAML (Lymphoma Society)Desy RusianaNo ratings yet
- Drugs PregnancyDocument9 pagesDrugs PregnancyPamelaS9No ratings yet
- End PointsDocument15 pagesEnd PointsDesy RusianaNo ratings yet
- Self-Induced Water Intoxication Treated With RisperidoneDocument3 pagesSelf-Induced Water Intoxication Treated With RisperidoneAlexi LaxiusNo ratings yet
- sglt2 InhibitorDocument6 pagessglt2 InhibitorDesy RusianaNo ratings yet
- Faril Elderly As Disaster Victims. Emergency Managment StrategiesDocument8 pagesFaril Elderly As Disaster Victims. Emergency Managment StrategiesJuliana SartoriNo ratings yet
- Diagnosis and Classification of Diabetes 2013Document8 pagesDiagnosis and Classification of Diabetes 2013Armando ATNo ratings yet
- sglt2 InhibitorDocument5 pagessglt2 InhibitorDesy RusianaNo ratings yet
- Effect of Heavy Metal On Malondialdehyde and Advanced Oxidation Protein Produtcs Concentration A Focus On Arsenic, Cadmium, and MercuryDocument6 pagesEffect of Heavy Metal On Malondialdehyde and Advanced Oxidation Protein Produtcs Concentration A Focus On Arsenic, Cadmium, and MercuryDesy RusianaNo ratings yet
- Effect of Heavy Metal On Malondialdehyde and Advanced Oxidation Protein Produtcs Concentration A Focus On Arsenic, Cadmium, and MercuryDocument6 pagesEffect of Heavy Metal On Malondialdehyde and Advanced Oxidation Protein Produtcs Concentration A Focus On Arsenic, Cadmium, and MercuryDesy RusianaNo ratings yet
- LyricsDocument29 pagesLyricsDesy RusianaNo ratings yet
- Long Term Sequelae From Childhood Pneumonia Systematic Review and Meta-AnalysisDocument9 pagesLong Term Sequelae From Childhood Pneumonia Systematic Review and Meta-AnalysisDesy RusianaNo ratings yet
- Ichard: Daftar PustakaDocument4 pagesIchard: Daftar PustakaDesy RusianaNo ratings yet
- AntithrombotikDocument18 pagesAntithrombotikDesy RusianaNo ratings yet
- Emerg Med J 2004 Wittenberg 429 32Document5 pagesEmerg Med J 2004 Wittenberg 429 32Desy RusianaNo ratings yet
- Ichard: Daftar PustakaDocument4 pagesIchard: Daftar PustakaDesy RusianaNo ratings yet
- Sims 3Document1 pageSims 3Desy RusianaNo ratings yet
- LyricsDocument29 pagesLyricsDesy RusianaNo ratings yet
- Ebook Development Infancy Through Adolescence 1St Edition Steinberg Test Bank Full Chapter PDFDocument61 pagesEbook Development Infancy Through Adolescence 1St Edition Steinberg Test Bank Full Chapter PDFbastmedalist8t2a100% (9)
- ATLS 10th Edition Update Summary - Banana Bag Blog - Emergency Medicine BlogDocument21 pagesATLS 10th Edition Update Summary - Banana Bag Blog - Emergency Medicine BlogapisaraearthNo ratings yet
- Color Trail TestDocument13 pagesColor Trail Testallexa726083100% (4)
- Classification of Trauma in Children - UpToDateDocument15 pagesClassification of Trauma in Children - UpToDateLeonardo Tavares de OliveiraNo ratings yet
- TCCC Handbook Fall 2013Document192 pagesTCCC Handbook Fall 2013AMG_IA100% (4)
- Airway and Ventilatory ManagementDocument19 pagesAirway and Ventilatory ManagementChynthea ParamithaNo ratings yet
- Prelims: - Intro To Calvarium and Head/brain Imaging Modalities - Craniofacial TraumaDocument97 pagesPrelims: - Intro To Calvarium and Head/brain Imaging Modalities - Craniofacial TraumaRica AriasNo ratings yet
- Epidemiology of Traumatic Brain Injury-Associated Epilepsy in WesternDocument7 pagesEpidemiology of Traumatic Brain Injury-Associated Epilepsy in Westernhermalina sabruNo ratings yet
- Polytrauma - Student's PresentationDocument24 pagesPolytrauma - Student's PresentationabdulazizNo ratings yet
- Trauma Care Manual-CRC Press Ian Greaves (Editor), Sir Keith Porter (Editor), Jeff Garner (Editor) - (2021)Document595 pagesTrauma Care Manual-CRC Press Ian Greaves (Editor), Sir Keith Porter (Editor), Jeff Garner (Editor) - (2021)Silvio danteNo ratings yet
- Occupational Therapy Assessment ToolsDocument19 pagesOccupational Therapy Assessment ToolsThirdy BullerNo ratings yet
- Raised ICP, SOL, HerniationDocument5 pagesRaised ICP, SOL, HerniationGrilled CroweNo ratings yet
- University of Cebu Lapu-Lapu and Mandaue: A.C. Cortes Ave., Looc, Mandaue, PhilippinesDocument12 pagesUniversity of Cebu Lapu-Lapu and Mandaue: A.C. Cortes Ave., Looc, Mandaue, PhilippinesZel ZozobradoNo ratings yet
- ConcussionsDocument3 pagesConcussionsKarlie CapozzoliNo ratings yet
- Subdural HematomaDocument5 pagesSubdural Hematomaluisse ann100% (1)
- Perfusion 1Document12 pagesPerfusion 1zixdiddyNo ratings yet
- Head Injury: Manali H. Solanki F.Y. M.Sc. Nursing J G College of NursingDocument31 pagesHead Injury: Manali H. Solanki F.Y. M.Sc. Nursing J G College of NursingWaqar AhmedNo ratings yet
- COT - June 2015 - Conference ProgrammeDocument42 pagesCOT - June 2015 - Conference ProgrammeBeccaNo ratings yet
- Early Outcomes of Assault Injuries Among Trauma Patients Presenting at Kampala International University Teaching Hospital and Jinja Regional Referral HospitalDocument11 pagesEarly Outcomes of Assault Injuries Among Trauma Patients Presenting at Kampala International University Teaching Hospital and Jinja Regional Referral HospitalKampala International UniversityNo ratings yet
- Gabbatore 2015Document15 pagesGabbatore 2015GsNo ratings yet
- Management of Acute Moderate and Severe Traumatic Brain InjuryDocument34 pagesManagement of Acute Moderate and Severe Traumatic Brain InjuryAndra MariaNo ratings yet
- Managing - Patients - With - Severe - Traumatic - Brain WITH HIGHLIGHTSDocument8 pagesManaging - Patients - With - Severe - Traumatic - Brain WITH HIGHLIGHTSTre OfficialNo ratings yet
- Perinatology Clinics 2008, Vol.35, Issues 4, Neuroprotection in The NewbornDocument210 pagesPerinatology Clinics 2008, Vol.35, Issues 4, Neuroprotection in The NewbornJhonny MarquezNo ratings yet
- WSES Consensus Conference Guidelines - TCEDocument9 pagesWSES Consensus Conference Guidelines - TCEDr. Victor Alonso Hernández HernándezNo ratings yet
- Prospectus: Auckland University of Technology, New ZealandDocument60 pagesProspectus: Auckland University of Technology, New ZealandPeram Amarnath 7147No ratings yet