Professional Documents
Culture Documents
Vice President Managed Care in Sacramento CA Resume Jeffrey Baumeister
Uploaded by
JeffreyBaumeisterCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vice President Managed Care in Sacramento CA Resume Jeffrey Baumeister
Uploaded by
JeffreyBaumeisterCopyright:
Available Formats
Executive Resume
Jeffrey A. Baumeister, CHC
Folsom, CA 95630 Telephone: (916) 351-9181 Email: jeff.baumeister@gmail.com
Leadership Profile
Outstanding track record of improving profitability by developing and implementing innovative programs to address complex operating problems. Seeking leadership opportunity with a leading health plan, managed care organization, benefits purchaser, medical group or integrated delivery system. Significant experience with startup, build and implementation of new programs including Medi-Cal Two Plan Model, Medi-Cal Rural Expansion, Medicare Advantage Plans, Health Insurance Exchanges and startup provider sponsored commercial health plans. Business Development: Key member of six person BD team that won $26.5M contract to file Knox-Keene license application and built startup health plan for Sutter Health. P&L and Operations: Served as GM with responsibility for $500M Medicaid P&L for major CA Health Plan increasing revenues by $52M. Medicare: Led multi-disciplinary project team that developed and implemented Group Medicare Advantage Prescription Drug Plan for CalPERS retirees on a six month build timeline. Knox Keene: Led team that developed and filed successful full service Knox Keene Application and subsequently built sales operations for startup Sutter Health Plan. Cost of Healthcare: Developed and implemented Cost of Healthcare program for 500k member CalPERS account that bent the trend saving $16M/year. RFP Wins/Account Management: Successful experience with new business development and large scale RFPs as well as managing and expanding large group employer and government contracts including CalPERS, State of Ohio, Department of Defense, GM, Ford and Chrysler. Health Plan Transformation: Appointed by CEO to lead enterprise wide transformation of Blues Plan implementing risk based provider contracts, new benefit plans and enhanced UM/DM programs resulting in $12M+ annual savings. Thirty years of broad based payer and provider experience including marketing, business development, provider network development, regulatory compliance, service area expansions, licensures, claims audits, call centers and health plan operations with industry leaders including several Blues, United Healthcare, Aetna, Foundation Health and Health Net. Proven ability to bring order out of chaos and develop and implement new internal progra ms, restore regulatory compliance, design and operationalize new products, open new markets, improve operating efficiencies, reduce administrative expenses, create narrow provider networks, expand service areas and better control healthcare costs.
Professional Experience
California Health & Wellness Plan Director Provider Relations Sacramento, California 2013
Plan, develop and implement all provider relations and education activities for startup health plan serving 93,000 Medi-Cal beneficiaries in 18 county Rural Expansion of Medi-Cal managed care. Optum Consulting/ United Health Group Director, West Region Payer Consulting Sacramento, California 2011 to 2013
Responsible for new business development for health plan/payer accounts of $2.5M+. Key member of senior executive business development team that sold and delivered on $26.5M engagement with Sutter Health to build startup commercial health plan.
MedeAnalytics Client Success Executive/Senior Director
Emeryville, California 2011
Cultivated relationships with largest health plan clients for this privately held data analytics firm. Developed and executed account management plans, annual training roadmaps, all medical director in-service trainings, identified product enhancements, and managed service request and new release schedule. Blue Shield of California (BSC) Director, Healthcare Value Sacramento, California 2007 to 2010
Developed new initiatives/health benefit products reducing cost of healthcare for CalPERS with projected cost savings of $16 million in 2010. Within a 120 day window, developed and implemented fourth largest group Medicare advantage prescription drug plan (GMAPD) in California as the retiree health care solution for California Public Employees Retirement System (CalPERS) account. Insight Health Corporation Lake Forest, California VP Managed Care, Director Business Development/Managed Care Contracting 2005 to 2007 Significantly revised managed care payer contract language and reimbursements to drive new revenues, improve operating efficiencies and obtain regulatory compliance. CHC Managed Healthcare Consulting Vice President Business Development and Client Services Sacramento, California 1998 to 2005
Designed, marketed, and implemented comprehensive healthcare contract services for managed-care payers and providers. Developed marketing materials, sales forecasts, industry research, identified target markets, product line enhancements and formed strategic alliances. Served clients Health Net, Foundation Health, PacifiCare and Blue Shield of California. Health Net Vice President/General Manager, California Health Programs Rancho Cordova, California 1998
P & L leadership for $500 million annual revenue Medi-Cal programs throughout California. Managed 130 employees and directed a $6 million annual budget. Directed all sales and marketing, enrollment, member services, health education, medical management, government relations, claims, finance, provider development, compliance and administrative operations. Increased revenues by 10 percent$52,000,000to a total of $480 million per year. Coopers & Lybrand, LLC Director, HMO Compliance Sacramento, California 1997
Direct responsibility for developing a comprehensive new product line of compliance consulting services for marketing to managed care organizations for the C & L Health Care Regulatory Group Practice. Developed marketing materials, designed and implemented audit procedures, best practices, pricing policies and performance standards. Foundation Health, a California Health Plan Vice President, Provider Compliance and Education Sacramento, California 1995 to 1997
Total P & L responsibility for all functions within provider compliance and education dedicated to capitated/delegated IPAs and medical groups. Managed annual internal annual budget of $3 million. Created and enforced corrective actions for non-compliant providers. Created and served as Chair of FH Corporate Provider Compliance Committee Vice President, Provider Services Director, Provider Relations Managed contractual relationships with provider networks and directed all activities in provider relations, provider inquiries, and provider education functions for commercial HMO, PPO and TriCare lines of business. Directed annual internal operating budget of $4 million and staff of 80 FTEs. 1992 to 1995
Blue Cross & Blue Shield of Ohio Corporate Director of Provider Relations/Manager of Program Development
Toledo, Ohio 1979 to 1992
Implemented "best practices" procedures for the resolution of provider inquiries regarding benefit programs, contract terms, and/or claims payments. Served as project manager and led task force to implement new hospital payment mechanisms and employer group benefit programs. Designed and implemented utilization management programs including pre-certification, concurrent review, retrospective review and second surgical opinions.
Education and Professional Affiliations
Bachelor of Science in Education, Bowling Green State University, Bowling Green, Ohio, 1975. Graduated with Honors (Cum Laude). Member Phi Alpha Theta Honorary Society Earned Certified Health Consultant designation from Krannert Graduate School of Business, Purdue University/Blue Cross and Blue Shield Association with examination scores in top ten nationally. Member HCFA/CMS Region IX Claims Audit Task Force Appointed to Ohio Governors Task Force on Diabetes Education Licensed California Health and Life Insurance Broker, license number OC36581 Currently pursuing Certified Employee Benefit Specialist (CEBS) designation
You might also like
- Medicare Healthcare Sales Executive in CA Resume Bren WhitakerDocument2 pagesMedicare Healthcare Sales Executive in CA Resume Bren Whitakerbefoundjobs613No ratings yet
- Bend the Healthcare Trend: How Consumer-Driven Health & Wellness Plans Lower Insurance CostsFrom EverandBend the Healthcare Trend: How Consumer-Driven Health & Wellness Plans Lower Insurance CostsNo ratings yet
- CEO COO Healthcare VP in Southeastern USA Resume Rea OliverDocument5 pagesCEO COO Healthcare VP in Southeastern USA Resume Rea OliverReaOliverNo ratings yet
- Senior Vice President or Executive Vice President or Chief OperaDocument3 pagesSenior Vice President or Executive Vice President or Chief Operaapi-121373483No ratings yet
- Mark E. Locklear ResumeDocument5 pagesMark E. Locklear ResumeMark LocklearNo ratings yet
- Vice President in ST Louis MO Resume Karen Hercules-DoerrDocument2 pagesVice President in ST Louis MO Resume Karen Hercules-DoerrKarenHerculesDoerrNo ratings yet
- Employee Benefits Manager Healthcare in Chicago IL Resume Keri BemorasDocument2 pagesEmployee Benefits Manager Healthcare in Chicago IL Resume Keri BemorasKeriBemorasNo ratings yet
- Training Talent Change Management in USA Resume Lorita DeVriesDocument3 pagesTraining Talent Change Management in USA Resume Lorita DeVriesLoritaDeVriesNo ratings yet
- VP Client Services Healthcare in Greater Chicago IL Resume Marybeth ReganDocument5 pagesVP Client Services Healthcare in Greater Chicago IL Resume Marybeth ReganMarybeth ReganNo ratings yet
- Healthcare VP CFO Controller in South FL Resume Mark DelvauxDocument2 pagesHealthcare VP CFO Controller in South FL Resume Mark DelvauxMarkDelvauxNo ratings yet
- VP Marketing Bus Dev Strategic Planning International 3 19 PDFDocument9 pagesVP Marketing Bus Dev Strategic Planning International 3 19 PDFcarla singletonNo ratings yet
- VP Director Human Resources in Orange County CA Resume Robert BudaDocument2 pagesVP Director Human Resources in Orange County CA Resume Robert BudaRobert BudaNo ratings yet
- Senior Human Resources Director Attorney in Milwaukee WI Resume Christiane StandleeDocument3 pagesSenior Human Resources Director Attorney in Milwaukee WI Resume Christiane StandleeChristianeStandlee2No ratings yet
- Senior HR Director Attorney in Milwaukee WI Resume Christiane StandleeDocument3 pagesSenior HR Director Attorney in Milwaukee WI Resume Christiane StandleeChristianeStandleeNo ratings yet
- VP Health Insurance Operations in Boston MA Resume Thomas EverettDocument2 pagesVP Health Insurance Operations in Boston MA Resume Thomas EverettThomas EverettNo ratings yet
- Account Field Reimbursement Manager in CA Resume Roger WortsmanDocument2 pagesAccount Field Reimbursement Manager in CA Resume Roger WortsmanRogerWortsmanNo ratings yet
- Business Development Account Manager in ST Louis MO Resume Erin CheringtonDocument3 pagesBusiness Development Account Manager in ST Louis MO Resume Erin CheringtonErinCheringtonNo ratings yet
- General Counsel Regulatory Compliance in Washington DC Metro Resume Mary Elizabeth LynchDocument4 pagesGeneral Counsel Regulatory Compliance in Washington DC Metro Resume Mary Elizabeth LynchMary Elizabeth LynchNo ratings yet
- Regional VP National Account Director in Los Angeles CA Resume Ken MadanDocument4 pagesRegional VP National Account Director in Los Angeles CA Resume Ken MadanKenMadanNo ratings yet
- CEO Chief Executive Officer in TN Southern USA Resume David HohlDocument4 pagesCEO Chief Executive Officer in TN Southern USA Resume David HohlDavidHohlNo ratings yet
- Workers Compensation Risk Manager in Pittsburgh PA Resume Seon PierceDocument3 pagesWorkers Compensation Risk Manager in Pittsburgh PA Resume Seon PierceSeon PierceNo ratings yet
- Training Development Director in Minneapolis ST Paul MN Resume Diane McClineDocument2 pagesTraining Development Director in Minneapolis ST Paul MN Resume Diane McClineDianeMcClineNo ratings yet
- Director Health Economics Reimbursement in Memphis TN Resume Michael McCormackDocument2 pagesDirector Health Economics Reimbursement in Memphis TN Resume Michael McCormackMichaelMcCormackNo ratings yet
- Vice President Sales in New York City Resume Brian HenryDocument2 pagesVice President Sales in New York City Resume Brian HenryBrianHenry1No ratings yet
- CEO CFO Healthcare SEC in Tampa FL Resume Jay JarrellDocument3 pagesCEO CFO Healthcare SEC in Tampa FL Resume Jay JarrellJayJarrellNo ratings yet
- Health System Director Administrator in Columbus OH Resume Cheryl GuymanDocument2 pagesHealth System Director Administrator in Columbus OH Resume Cheryl GuymanCherylGuymanNo ratings yet
- CFO Finance VP in Orange County CA Resume Peter HernandezDocument2 pagesCFO Finance VP in Orange County CA Resume Peter HernandezPeterHernandezNo ratings yet
- Management Consultant Interim CEO COO Healthcare in Detroit MI Resume Sarah BannonDocument4 pagesManagement Consultant Interim CEO COO Healthcare in Detroit MI Resume Sarah BannonSarahBannonNo ratings yet
- Executive Director Operations Healthcare in Charlotte NC Resume Gregory MillerDocument2 pagesExecutive Director Operations Healthcare in Charlotte NC Resume Gregory MillerGregory Miller1No ratings yet
- Director Healthcare Technology Marketing in Philadelphia PA Resume Robin SametDocument3 pagesDirector Healthcare Technology Marketing in Philadelphia PA Resume Robin SametRobinSametNo ratings yet
- Manager or Director or Executive or Team FacilitatorDocument2 pagesManager or Director or Executive or Team Facilitatorapi-77666759No ratings yet
- VP Healthcare Revenue Cycle Strategy in Cincinnati OH Resume Daniel PlavsicDocument2 pagesVP Healthcare Revenue Cycle Strategy in Cincinnati OH Resume Daniel PlavsicDanielPlavsicNo ratings yet
- Vice President or Executive Director or DirectorDocument4 pagesVice President or Executive Director or Directorapi-77396522No ratings yet
- VP Healthcare Sales Marketing in South Florida Resume Charles SchneiderDocument3 pagesVP Healthcare Sales Marketing in South Florida Resume Charles SchneiderCharles SchneiderNo ratings yet
- Healthcare Quality Management Regulatory Compliance Coordinator in Denver CO Resume Mary FrisciaDocument4 pagesHealthcare Quality Management Regulatory Compliance Coordinator in Denver CO Resume Mary FrisciaMaryFrisciaNo ratings yet
- Vice President Director Human Resources in Louisville KY Resume David JamesDocument2 pagesVice President Director Human Resources in Louisville KY Resume David JamesDavidJames2No ratings yet
- Michael A. DavisDocument2 pagesMichael A. DavisRandy DavisNo ratings yet
- Employee Benefits Director Manager in New York City Resume Michael HarrisDocument2 pagesEmployee Benefits Director Manager in New York City Resume Michael HarrisMichael HarrisNo ratings yet
- Healthcare Operations Management Consultant in Chicago IL Resume Brenda BehrensDocument2 pagesHealthcare Operations Management Consultant in Chicago IL Resume Brenda BehrensBrendaBehrens2No ratings yet
- CEO COO President Healthcare in Seattle WA Resume Matt CrockettDocument3 pagesCEO COO President Healthcare in Seattle WA Resume Matt CrockettMattCrockettNo ratings yet
- National Strategic Account Director in Louisville KY Resume Tom MiddletonDocument2 pagesNational Strategic Account Director in Louisville KY Resume Tom MiddletonTomMiddleton1No ratings yet
- Business Development Director Healthcare in Ontario Canada Resume Harley RodinDocument4 pagesBusiness Development Director Healthcare in Ontario Canada Resume Harley RodinHarley RodinNo ratings yet
- Healthcare CFO CPA MBA in Miami/Fort Lauderdale FL Resume Henry BrownDocument3 pagesHealthcare CFO CPA MBA in Miami/Fort Lauderdale FL Resume Henry BrownHenry BrownNo ratings yet
- Houston ISD School Board Agenda Item Regarding Consultant Kenneth Wells and AlkenDocument2 pagesHouston ISD School Board Agenda Item Regarding Consultant Kenneth Wells and AlkenTexas WatchdogNo ratings yet
- Robert Palussek ResumeDocument4 pagesRobert Palussek ResumeNews-PressNo ratings yet
- Vice President Sales Marketing Medical in San Francisco CA Resume Dale RichardsonDocument2 pagesVice President Sales Marketing Medical in San Francisco CA Resume Dale RichardsonDaleRichardsonNo ratings yet
- Pharmaceutical Reimbursement Access Manager in Austin TX Resume Brian BucklesDocument2 pagesPharmaceutical Reimbursement Access Manager in Austin TX Resume Brian BucklesBrian Buckles100% (1)
- Regional Director Healthcare Operations in Atlanta GA Resume Cheryl Cust-HarrisDocument2 pagesRegional Director Healthcare Operations in Atlanta GA Resume Cheryl Cust-HarrisCherylCustHarrisNo ratings yet
- Interim Chief Executive Officer in United States Resume John WinengerDocument2 pagesInterim Chief Executive Officer in United States Resume John WinengerJohnWinengerNo ratings yet
- Quality Management Healthcare AdministrationDocument3 pagesQuality Management Healthcare Administrationapi-122235893No ratings yet
- CFO Vice President Finance in United States Resume Salmon KaplanDocument3 pagesCFO Vice President Finance in United States Resume Salmon KaplanSalmon Kaplan1No ratings yet
- HR Business Partner Generalist Director in South FL Resume Tina CulverDocument2 pagesHR Business Partner Generalist Director in South FL Resume Tina CulverTinaCulverNo ratings yet
- VP Sales Marketing Health in Raleigh Durham NC Resume Donald SwankieDocument4 pagesVP Sales Marketing Health in Raleigh Durham NC Resume Donald SwankieDonaldSwankieNo ratings yet
- Chief Executive Officer in Brentwood TN Resume Gary FergusonDocument3 pagesChief Executive Officer in Brentwood TN Resume Gary FergusonGaryFerguson1No ratings yet
- Sales Executive Business Development in Pittsburgh PA Resume Gary RetoneDocument3 pagesSales Executive Business Development in Pittsburgh PA Resume Gary RetoneGaryRetone3No ratings yet
- Corporate Financial Planning Analysis in Raleigh Durham NC Resume Frank DeLuciaDocument1 pageCorporate Financial Planning Analysis in Raleigh Durham NC Resume Frank DeLuciaFrankDeLuciaNo ratings yet
- CFO SVP Vice President Finance in ST Louis MO Resume Matt StrateDocument1 pageCFO SVP Vice President Finance in ST Louis MO Resume Matt StrateMattStrateNo ratings yet
- Key Account Manager Healthcare in Cleveland OH Resume James GrayDocument2 pagesKey Account Manager Healthcare in Cleveland OH Resume James GrayJamesGray1No ratings yet
- VP Pharmaceutical Sales Marketing Management in Greater New York City Resume Greg PaladinoDocument2 pagesVP Pharmaceutical Sales Marketing Management in Greater New York City Resume Greg PaladinoGreg PaladinoNo ratings yet
- Dell Inspiron 5547 15Document7 pagesDell Inspiron 5547 15Kiti HowaitoNo ratings yet
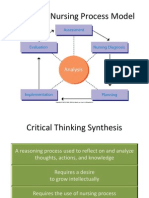
- NUR 104 Nursing Process MY NOTESDocument77 pagesNUR 104 Nursing Process MY NOTESmeanne073100% (1)
- Motor BookDocument252 pagesMotor BookKyaw KhNo ratings yet
- DesignDocument402 pagesDesignEduard BoleaNo ratings yet
- Charging Station For E-Vehicle Using Solar With IOTDocument6 pagesCharging Station For E-Vehicle Using Solar With IOTjakeNo ratings yet
- Application Tracking System: Mentor - Yamini Ma'AmDocument10 pagesApplication Tracking System: Mentor - Yamini Ma'AmBHuwanNo ratings yet
- IAU Logbook Core 6weeksDocument7 pagesIAU Logbook Core 6weeksbajariaaNo ratings yet
- Resume LittletonDocument1 pageResume Littletonapi-309466005No ratings yet
- Dr. N. Kumarappan IE (I) Council Candidate - Electrical DivisionDocument1 pageDr. N. Kumarappan IE (I) Council Candidate - Electrical Divisionshanmugasundaram32No ratings yet
- Science: BiologyDocument22 pagesScience: BiologyMike RollideNo ratings yet
- Finite Element Modeling Analysis of Nano Composite Airfoil StructureDocument11 pagesFinite Element Modeling Analysis of Nano Composite Airfoil StructureSuraj GautamNo ratings yet
- Being Agile. Staying Resilient.: ANNUAL REPORT 2021-22Document296 pagesBeing Agile. Staying Resilient.: ANNUAL REPORT 2021-22PrabhatNo ratings yet
- Service Marketing - Term End Examination 2021 School of Business Management Narsee Monjee Institute of Management Studies, HyderabadDocument2 pagesService Marketing - Term End Examination 2021 School of Business Management Narsee Monjee Institute of Management Studies, Hyderabadnatasha bennyNo ratings yet
- Recruitment Process Outsourcing PDFDocument4 pagesRecruitment Process Outsourcing PDFDevesh NamdeoNo ratings yet
- Ddec VDocument30 pagesDdec Vllama100% (1)
- Учебный предметDocument2 pagesУчебный предметorang shabdizNo ratings yet
- VectorCAST QA Factsheet ENDocument2 pagesVectorCAST QA Factsheet ENChaos XiaNo ratings yet
- Project in Precal: Mary Joyce MolinesDocument11 pagesProject in Precal: Mary Joyce MolinesJaja KeykNo ratings yet
- Sketch NotesDocument32 pagesSketch NotesFilipe Rovarotto100% (8)
- Croda Smarter Polymers Guide Sep 2019Document20 pagesCroda Smarter Polymers Guide Sep 2019Keith Tamura100% (1)
- 56257375851Document3 pages56257375851Anneliese FernandesNo ratings yet
- Thermal ComfortDocument50 pagesThermal ComfortSSNo ratings yet
- Week 1 Macro (DDR)Document49 pagesWeek 1 Macro (DDR)Stevie Sean100% (1)
- Challenges Affecting Devolution PDFDocument94 pagesChallenges Affecting Devolution PDFELIJAH M. OMBEONo ratings yet
- Research Paper OutlineDocument2 pagesResearch Paper Outlineapi-270769683No ratings yet
- Christine Remembered That Today Is The Birthday of Her BossDocument1 pageChristine Remembered That Today Is The Birthday of Her BossA.No ratings yet
- S P 01958 Version 2 EPD OVO ArmchairDocument16 pagesS P 01958 Version 2 EPD OVO ArmchairboiNo ratings yet
- Ericsson AXE 810: Switch (ROTD)Document4 pagesEricsson AXE 810: Switch (ROTD)Kao Sun HoNo ratings yet
- Dr. Alberto A. Jumao-As JRDocument46 pagesDr. Alberto A. Jumao-As JRClinton Mazo100% (1)
- THE PERFECT DAY Compressed 1 PDFDocument218 pagesTHE PERFECT DAY Compressed 1 PDFMariaNo ratings yet
- The Coaching Habit: Say Less, Ask More & Change the Way You Lead ForeverFrom EverandThe Coaching Habit: Say Less, Ask More & Change the Way You Lead ForeverRating: 4.5 out of 5 stars4.5/5 (186)
- How to Talk to Anyone at Work: 72 Little Tricks for Big Success Communicating on the JobFrom EverandHow to Talk to Anyone at Work: 72 Little Tricks for Big Success Communicating on the JobRating: 4.5 out of 5 stars4.5/5 (37)
- High Road Leadership: Bringing People Together in a World That DividesFrom EverandHigh Road Leadership: Bringing People Together in a World That DividesNo ratings yet
- Summary of Noah Kagan's Million Dollar WeekendFrom EverandSummary of Noah Kagan's Million Dollar WeekendRating: 5 out of 5 stars5/5 (2)
- The 7 Habits of Highly Effective PeopleFrom EverandThe 7 Habits of Highly Effective PeopleRating: 4 out of 5 stars4/5 (2567)
- Think Like Amazon: 50 1/2 Ideas to Become a Digital LeaderFrom EverandThink Like Amazon: 50 1/2 Ideas to Become a Digital LeaderRating: 4.5 out of 5 stars4.5/5 (61)
- The Introverted Leader: Building on Your Quiet StrengthFrom EverandThe Introverted Leader: Building on Your Quiet StrengthRating: 4.5 out of 5 stars4.5/5 (35)
- Transformed: Moving to the Product Operating ModelFrom EverandTransformed: Moving to the Product Operating ModelRating: 4.5 out of 5 stars4.5/5 (2)
- Leadership Skills that Inspire Incredible ResultsFrom EverandLeadership Skills that Inspire Incredible ResultsRating: 4.5 out of 5 stars4.5/5 (11)
- The First Minute: How to start conversations that get resultsFrom EverandThe First Minute: How to start conversations that get resultsRating: 4.5 out of 5 stars4.5/5 (57)
- Billion Dollar Lessons: What You Can Learn from the Most Inexcusable Business Failures of the Last Twenty-five YearsFrom EverandBillion Dollar Lessons: What You Can Learn from the Most Inexcusable Business Failures of the Last Twenty-five YearsRating: 4.5 out of 5 stars4.5/5 (52)
- Transformed: Moving to the Product Operating ModelFrom EverandTransformed: Moving to the Product Operating ModelRating: 4 out of 5 stars4/5 (1)
- Scaling Up: How a Few Companies Make It...and Why the Rest Don't, Rockefeller Habits 2.0From EverandScaling Up: How a Few Companies Make It...and Why the Rest Don't, Rockefeller Habits 2.0Rating: 5 out of 5 stars5/5 (2)
- The Friction Project: How Smart Leaders Make the Right Things Easier and the Wrong Things HarderFrom EverandThe Friction Project: How Smart Leaders Make the Right Things Easier and the Wrong Things HarderNo ratings yet
- Unlocking Potential: 7 Coaching Skills That Transform Individuals, Teams, & OrganizationsFrom EverandUnlocking Potential: 7 Coaching Skills That Transform Individuals, Teams, & OrganizationsRating: 4.5 out of 5 stars4.5/5 (28)
- How to Lead: Wisdom from the World's Greatest CEOs, Founders, and Game ChangersFrom EverandHow to Lead: Wisdom from the World's Greatest CEOs, Founders, and Game ChangersRating: 4.5 out of 5 stars4.5/5 (95)
- The Power of People Skills: How to Eliminate 90% of Your HR Problems and Dramatically Increase Team and Company Morale and PerformanceFrom EverandThe Power of People Skills: How to Eliminate 90% of Your HR Problems and Dramatically Increase Team and Company Morale and PerformanceRating: 5 out of 5 stars5/5 (22)
- Summary of Marshall Goldsmith & Mark Reiter's What Got You Here Won't Get You ThereFrom EverandSummary of Marshall Goldsmith & Mark Reiter's What Got You Here Won't Get You ThereRating: 3 out of 5 stars3/5 (2)
- Superminds: The Surprising Power of People and Computers Thinking TogetherFrom EverandSuperminds: The Surprising Power of People and Computers Thinking TogetherRating: 3.5 out of 5 stars3.5/5 (7)
- Good to Great by Jim Collins - Book Summary: Why Some Companies Make the Leap...And Others Don'tFrom EverandGood to Great by Jim Collins - Book Summary: Why Some Companies Make the Leap...And Others Don'tRating: 4.5 out of 5 stars4.5/5 (64)
- The Effective Executive: The Definitive Guide to Getting the Right Things DoneFrom EverandThe Effective Executive: The Definitive Guide to Getting the Right Things DoneRating: 4.5 out of 5 stars4.5/5 (469)
- 7 Principles of Transformational Leadership: Create a Mindset of Passion, Innovation, and GrowthFrom Everand7 Principles of Transformational Leadership: Create a Mindset of Passion, Innovation, and GrowthRating: 5 out of 5 stars5/5 (52)
- The 7 Habits of Highly Effective People: 30th Anniversary EditionFrom EverandThe 7 Habits of Highly Effective People: 30th Anniversary EditionRating: 5 out of 5 stars5/5 (338)
- The E-Myth Revisited: Why Most Small Businesses Don't Work andFrom EverandThe E-Myth Revisited: Why Most Small Businesses Don't Work andRating: 4.5 out of 5 stars4.5/5 (709)
- 300+ PMP Practice Questions Aligned with PMBOK 7, Agile Methods, and Key Process Groups - 2024: First EditionFrom Everand300+ PMP Practice Questions Aligned with PMBOK 7, Agile Methods, and Key Process Groups - 2024: First EditionRating: 5 out of 5 stars5/5 (1)
- Management Mess to Leadership Success: 30 Challenges to Become the Leader You Would FollowFrom EverandManagement Mess to Leadership Success: 30 Challenges to Become the Leader You Would FollowRating: 4.5 out of 5 stars4.5/5 (27)