Professional Documents
Culture Documents
5292
Uploaded by
Andi Farras WatyOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
5292
Uploaded by
Andi Farras WatyCopyright:
Available Formats
WOMEN AND NEWBORN HEALTH SERVICE
King Edward Memorial Hospital CLINICAL GUIDELINES SECTION B: OBSTETRICS AND MIDWIFERY GUIDELINES
9 COMPLICATIONS OF THE POSTNATAL PERIOD 9.1 POSTPARTUM HAEMORRHAGE
Date Issued: Date Revised: Review Date: Authorised by: Review Team:
April 2002 November 2010 November 2013 OGCCU OGCCU
9.1.2 Uterine inversion Section B Clinical Guidelines King Edward Memorial Hospital Perth Western Australia
9.1.2 UTERINE INVERSION
BACKGROUND INFORMATION
2
The incidence of uterine inversion varies according to geographical location and ranges from 1:25001, to 1:200002, 3. CLASSIFICATION ACCORDING TO SEVERITY OF UTERINE INVERSION3 First degree Second degree Third degree The fundus reaches the internal os The body or corpus of the uterus is inverted to the internal os The uterus, cervix and vagina are inverted and are visible
CLASSIFICATION ACCORDING TO TIMING OF THE EVENT2, 3 Acute Subacute Chronic KEY POINTS 1. 2. 3. Concurrent maternal resuscitation with manual uterine replacement is the first line of management. If the placenta is still adherent following uterine inversion LEAVE IN PLACE to reduce blood loss.4 Uterine rupture should be excluded prior to performing hydrostatic reduction of the uterus. Occurs within 24 hours of birth Occurs after 24 hours, within 4 weeks Occurs after 4 weeks, rare.
CAUSES AND RISK FACTORS These include: mismanagement of the third stage e.g. premature or excessive cord traction during active management of the third stage2, 3, 5, a combination of fundal pressure and cord traction to deliver the placenta, or use of fundal pressure when the uterus is atonic during placental delivery3 abnormally adherent placenta2, 3, 5 spontaneous inversion of unknown etiology3 short umbilical cord3, 5 sudden emptying of a distended uterus3 nulliparity2, 5
DPMS Ref: 5292
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual
Page 1 of 4
fundal placement of the placenta2, 3 antepartum use of magnesium sulphate4
SIGNS OF A UTERINE INVERSION Symptoms of uterine inversion may include: postpartum haemorrhage2, 4 shock1, 4 thought to be due to the parasympathetic effect caused by traction of the ligaments supporting the uterus, and hypotension with inadequate tissue perfusion4 severe abdominal pain3 physical examination can reveal first or second degree uterine inversion3
MANAGEMENT Note: Maternal resuscitation while attempting uterine replacement should be initiated simultaneously. If the placenta is still in situ, leave in place until uterine replacement is complete. 1. 2. 3. Attempt manual replacement of the uterus by re-inverting it and keeping the hand in the uterus until firm contraction of the uterus is felt3 If uterine replacement is unsuccessful or no medical attention is immediately available : DIAL 55, CODE BLUE MEDICAL Insert two 16 gauge intravenous cannulae. Group and cross-match 4 units of blood and order a full blood picture.6 Consider performing coagulation studies.6, 7 Commence intravenous fluids: - See Clinical Guidelines Section B 9.1.1 Primary Postpartum Haemorrhage. - If the woman has blood loss more than 1000mls, continues to bleed, or show signs of clinical shock7, in consultation with the anaesthetist the volume and rate of fluids is adjusted according to the clinical situation. Warming of the solution may be required. If not already administered, withhold the oxytocic until uterine replacement is complete.2 Assess vital signs - blood pressure, pulse, respirations, and oxygen saturation levels 15 minutely (more frequently if maternal conditions necessitates). Monitor vital signs continuously as soon as practical with access to continuous monitoring equipment. Administer oxygen via a face mask. Insert an indwelling catheter. Monitor urine output. If the uterus is successfully replaced commence an oxytocic infusion (30iu Syntocinon in 500mL Hartmanns solution commencing at 240mL / hour) as per PPH therapeutic infusion regimen. See Clinical Guidelines Section B 9.1.3 Prophylactic and therapeutic oxytocin administration and infusion regimens. If the replacement of the uterus is not possible, resuscitate the woman and transfer her to theatre immediately. IN THEATRE 11.1 Stabilise the woman and obtain effective anaesthesia. 11.2 Relax the uterus with either: OR Glycereryl trinitrate 600micrograms sublingual
4. 5.
6. 7. 8.
9. 10.
Terbutaline 250micrograms subcutaneous 11.3 Replace the uterus
Date Issued: April 2002 Date Revised: November 2010 Review Date: November 2013 Written by:/Authorised by: OGCCU Review Team: OGCCU DPMS Ref: 5292 9.1.2 Uterine inversion Section B Clinical Guidelines King Edward Memorial Hospital Perth Western Australia Page 2 of 4
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual
11.4 Administer prophylactic antibiotics: Cefazolin 2 gm intravenous one dose only AND Metronidazole 500 milligrams intravenous one dose only 12. Commence oxytocin therapy following uterine replacement. See Clinical Guideline Section B 9.1.3 Prophylactic and therapeutic oxytocin administration and infusion regimens. MANUAL REPLACEMENT (JOHNSON MANOEUVRE). The uterus may require relaxation prior to manual replacement. 1. Using the palm of the hand push the fundus of the uterus along the direction of the vagina towards the posterior fornix.3 2. Then lift the uterus towards the umbilicus and return to its normal position.3 3. Maintain the hand in situ until a firm contraction is palpated. Oxytocin therapy should be administered to initiate and maintain contraction of the uterus. HYDROSTATIC REDUCTION (OSULLIVANS TECHNIQUE)6 Hydrostatic reduction is a method of reinverting the uterus by infusing warm saline into the vagina. Note: uterine rupture should be exclude prior to this performing the procedure.6 The women may be placed in the reverse Tredelenburg position8 to assist gravity and reduce traction on the infundibulo-pelvic ligaments, round ligaments and the ovaries.9 Method one 1. Attach a 2 x 1 litre bags of warmed saline to a Y-Cystoscopy giving set. Additional fluids may be required. 2. Insert the hand into the vagina with the open end of the tubing near the posterior fornix. Obtain a seal at the vaginal entrance by enclosing the labia around the wrist/hand to prevent fluid leakage.9 3. Infuse warmed fluid under gravity. Several litres of fluid may be required. Method two 1. Attach a 2 x 1 litre bags of warmed saline to a Y-Cystosopy giving set. 2. Gently push the inverted uterus into the vagina.8 3. Insert a 6cm (or appropriate sized) silastic ventouse cup into the lower vagina. Avoid pushing the cup deep into the vagina. Attach tubing to a container with warmed saline tubing or the giving set, and then place it 1 metre above the patient.8, 9, 10 4. If leaking occurs at the introitus gently withdraw the cup until it fits against the inner aspect of the introitus. Following the procedure the uterus should be digitally explored. The hand should be kept in the uterus until the oxytocic therapy produces a contracted uterus.6, 8, 10 SURGICAL MANAGEMENT Laparotomy with open reduction of the uterine inversion may be necessary if the previous methods are unsuccessful.
Date Issued: April 2002 Date Revised: November 2010 Review Date: November 2013 Written by:/Authorised by: OGCCU Review Team: OGCCU DPMS Ref: 5292
9.1.2 Uterine inversion Section B Clinical Guidelines King Edward Memorial Hospital Perth Western Australia Page 3 of 4
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual
REFERENCES 1. You WB, Zahn CM. Postpartum Hemorrhage: Abnormally Adherent Placenta, Uterine Inversion, and Puerperal Hematomas. Clinical Obstetrics and Gynecology. 2006;49(1):18497. Mirza FG, Gaddipati S. Obstetric Emergencies. Seminars in Perinatology. 2009;33:97-103. Coates T. Midwifery and obstetric emergencies. In: Fraser DM, MA C, editors. Myles Textbook for Midwives. 15th ed. London: Churchill Livingstone; 2009. p. 625-47. Beringer RM, Patteril M. Puerperal uterine inversion and shock. British Journal of Anaesthesia. 2004;92(3):439-41. Majd HS, Pilsniak A, Reginald PW. Recurrent uterine inversion: a novel treatment approach using SOS Baki balloon. BJOG. 2009;116:999-1001. Grady K, Howell C, Cox C, editors. The Moet Course Manual. Managing Obstetric Emergencies and Trauma. 2nd ed. London: RCOG Press; 2007. Royal College of Obstetricians and Gynaecologists. Prevention and Management of Postpartum Haemorrhage. Green-Top Guideline. 2009(52). Tan KH, Luddin NSY. Hydrostatic reduction of acute uterine inversion. International Journal of Gynecology and Obstetrics. 2005;91:63-4. Baskett TF. Essential Management of Obstetric Emergencies 170. 4th ed. Bristol: Clinical Press Limited; 2004. Ogueh O, Ayida G. Acute uterine inversion: a new technique of hydrostatic replacement. British Journal of Obstetrics and Gynaecology. 1997;104:951-2.
2. 3. 4. 5. 6. 7. 8. 9. 10.
Date Issued: April 2002 Date Revised: November 2010 Review Date: November 2013 Written by:/Authorised by: OGCCU Review Team: OGCCU DPMS Ref: 5292
9.1.2 Uterine inversion Section B Clinical Guidelines King Edward Memorial Hospital Perth Western Australia Page 4 of 4
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual
You might also like
- Toag.11.1.13.27463Document6 pagesToag.11.1.13.27463Andi Farras WatyNo ratings yet
- Uterine InversionDocument6 pagesUterine InversionAndi Farras WatyNo ratings yet
- Final OB Publications - The Female PatientDocument9 pagesFinal OB Publications - The Female PatientAndi Farras WatyNo ratings yet
- Assesment and Management of Cardiac Disease in PregnancyDocument6 pagesAssesment and Management of Cardiac Disease in PregnancyAndi Farras WatyNo ratings yet
- 9 First National Hepatitis B Strategy 2010-2013Document21 pages9 First National Hepatitis B Strategy 2010-2013Andi Farras WatyNo ratings yet
- Uterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DODocument4 pagesUterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DOAndi Farras WatyNo ratings yet
- NACE - National Competence Examination For Indonesian Health ProfessionalDocument1 pageNACE - National Competence Examination For Indonesian Health ProfessionalAndi Farras WatyNo ratings yet
- 18 Joseph Ahn HepBEvalDocument9 pages18 Joseph Ahn HepBEvalAndi Farras WatyNo ratings yet
- Chronic Hepatitis Band Chronic Hepatitis C inDocument18 pagesChronic Hepatitis Band Chronic Hepatitis C inAndi Farras WatyNo ratings yet
- 9 First National Hepatitis B Strategy 2010-2013Document21 pages9 First National Hepatitis B Strategy 2010-2013Andi Farras WatyNo ratings yet
- Expected and Unexpected Cardiac Problems During Pregnancy: P.G. PieperDocument3 pagesExpected and Unexpected Cardiac Problems During Pregnancy: P.G. PieperAndi Farras WatyNo ratings yet
- Cleveland Clinic Journal of Medicine 2009 RAMARAJ 289 96Document8 pagesCleveland Clinic Journal of Medicine 2009 RAMARAJ 289 96Andi Farras WatyNo ratings yet
- Occupational Contact Dermatitis in Cleaning Workers Our First ApproachDocument1 pageOccupational Contact Dermatitis in Cleaning Workers Our First ApproachAndi Farras WatyNo ratings yet
- Ah 063 yDocument6 pagesAh 063 yAndi Farras WatyNo ratings yet
- Dermatitis Guide 2011Document8 pagesDermatitis Guide 2011Andi Farras WatyNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Pelvic Floor Distress Inventory Questionnaire - Short Form 20Document2 pagesPelvic Floor Distress Inventory Questionnaire - Short Form 20Dana Ysabelle Ibarra100% (1)
- Tips For The NDECCDocument2 pagesTips For The NDECCMagda Jakubowska-EwiczNo ratings yet
- Nursing Care Plan (Angina Pectoris)Document2 pagesNursing Care Plan (Angina Pectoris)Jose Emmanuel Ribaya RuivivarNo ratings yet
- Evidence-Based Medicine: David L. SackettDocument3 pagesEvidence-Based Medicine: David L. SackettNicolas MarinNo ratings yet
- Fibromyalgia Journal TemplateDocument3 pagesFibromyalgia Journal Templatelauramariegonzalez100% (1)
- BCCDC TB ManualRevisedFebruary 2012Document141 pagesBCCDC TB ManualRevisedFebruary 2012zenagit123456No ratings yet
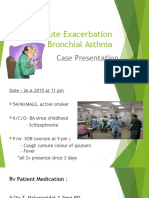
- Acute Exacerbation Bronchial AsthmaDocument21 pagesAcute Exacerbation Bronchial AsthmaChekNatrahNo ratings yet
- Palatine IL Ex-Mayor Rita Mullins Claims Save-A-Life Foundation Trained Chicago Police (2001)Document2 pagesPalatine IL Ex-Mayor Rita Mullins Claims Save-A-Life Foundation Trained Chicago Police (2001)Gordon T. PrattNo ratings yet
- Saint Peter's Physician Associates - Our Doctors in Your NeighborhoodDocument2 pagesSaint Peter's Physician Associates - Our Doctors in Your NeighborhoodSaint Peter's Healthcare SystemNo ratings yet
- Icmr PPT (1) VidhiDocument32 pagesIcmr PPT (1) VidhiVidhi GuptaNo ratings yet
- Dosages and SolutionDocument68 pagesDosages and SolutionRuan MarchessaNo ratings yet
- הוראות הפעלה Resmart Gii Auto Cpap System e 20a h oDocument37 pagesהוראות הפעלה Resmart Gii Auto Cpap System e 20a h oAntonio AcostaNo ratings yet
- Liver AnatomyDocument34 pagesLiver AnatomyAmit Kumar RanoNo ratings yet
- Discharge PlanningDocument1 pageDischarge PlanningChyNo ratings yet
- Causality assessment of single case reportsDocument11 pagesCausality assessment of single case reportsM LyaNo ratings yet
- Molekular Docking Dengan Metode Molegro Virtual Docker Turunan Kalkon Sebagai AntimikrobaDocument9 pagesMolekular Docking Dengan Metode Molegro Virtual Docker Turunan Kalkon Sebagai AntimikrobaWilliam SmithNo ratings yet
- Nclex Exam Maternal and Child Health Nursing 2 30 Items PDF FreeDocument8 pagesNclex Exam Maternal and Child Health Nursing 2 30 Items PDF FreeLianne BuensucesoNo ratings yet
- 14 - 2007 Urinalysis Checklist CAP Accreditation ProgramDocument45 pages14 - 2007 Urinalysis Checklist CAP Accreditation Program28850No ratings yet
- SPPDDocument1 pageSPPDBahul MunirNo ratings yet
- Buku Publikasi FKep UH TW II 2021 CompressedDocument118 pagesBuku Publikasi FKep UH TW II 2021 CompressedmakhenNo ratings yet
- Implant Surgery Complications - Etiology and TreatmentDocument10 pagesImplant Surgery Complications - Etiology and TreatmentStephanie JaramilloNo ratings yet
- InfoDocument9 pagesInfoDrNeetha ShenoyNo ratings yet
- Warfarin INR Antibx InteractionDocument3 pagesWarfarin INR Antibx InteractionSheila UlinaNo ratings yet
- Novus Knowledge Webinar - Feed Milling For Sustainable Food Production - Feed Mill Biosecurity - Dr. Charles Stark PDFDocument43 pagesNovus Knowledge Webinar - Feed Milling For Sustainable Food Production - Feed Mill Biosecurity - Dr. Charles Stark PDFaradhya bhatiya0% (1)
- OBDocument9 pagesOBDennis ArevaloNo ratings yet
- TLE Beauty Care Pretest Grade910Document4 pagesTLE Beauty Care Pretest Grade910KENT REEVE ROSALNo ratings yet
- Sports Massage Therapist - Sports Injury ChiropractorDocument3 pagesSports Massage Therapist - Sports Injury ChiropractorDr. Dale MacdonaldNo ratings yet
- Gram Positive Cocci (GPC) Gram Neg (Rods GNR) Anaerobes Atypicals Classification AntibioticDocument2 pagesGram Positive Cocci (GPC) Gram Neg (Rods GNR) Anaerobes Atypicals Classification AntibioticRami RaedNo ratings yet
- Immunology and Serology Lecture HistoryDocument3 pagesImmunology and Serology Lecture HistoryLyka ReyesNo ratings yet
- SBRT Pulmon Presentacion - TIPs and TricksDocument197 pagesSBRT Pulmon Presentacion - TIPs and TricksDavid GarciaNo ratings yet