Professional Documents
Culture Documents
Pediatrics Course Notes
Uploaded by
cubixmuresOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatrics Course Notes
Uploaded by
cubixmuresCopyright:
Available Formats
1
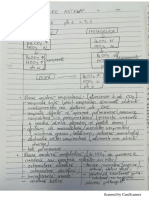
PEDIATRICS
COURSE NOTES
Editor:
Conf. Univ. Dr. Mrginean Cristina Oana
List of authors:
Prof. Univ. Dr. Tognel Rodica
Conf. Univ. Dr. Cucerea Manuela
Conf. Univ. Dr. Mrginean Cristina Oana
ef. Lucr. Dr. Borka Balazs Reka
ef Lucr. Dr. Duicu Carmen
Asist. Univ. Dr. Chincean Mihaela Ioana
Asist. Univ. Dr. Grama Alina Corina
Asist Univ. Dr. Pitea Ana Maria
2013
2
CONTENTS
Foreword .................................................................................................................. pag 4
Chapter I. Neonatal Pathology ................................................................................ pag 5
Perinatal asphyxia. New-born resuscitation ................................................................. pag 5
Respiratory distress in new-borns.............................................................................. pag 28
Neonatal infections ................................................................................................... pag 39
Neonatal pathological jaundice ................................................................................. pag 56
HIV-AIDS infections in neonates and children.......................................................... pag 62
Chapter II. Pathology of the Respiratory System.................................................. pag 69
Acute rhynopharyngitis ............................................................................................. pag 69
Acute angina ............................................................................................................ pag 71
Otitis and ostomastoiditis .......................................................................................... pag 74
Acute laryngitis......................................................................................................... pag 83
Epiglotitis ................................................................................................................. pag 80
Acute bronchyolitis ................................................................................................... pag 85
Pneumonias in children............................................................................................. pag 88
Childhood asthma ................................................................................................... pag 105
Chapter III. Pathology of the Cardiovascular System......................................... pag 114
Congenital heart diseases ....................................................................................... pag 114
Infective endocarditis ............................................................................................. pag 124
Myocarditis............................................................................................................. pag 128
Pericarditis.............................................................................................................. pag 129
Congestive heart failure .......................................................................................... pag 131
Shocks .................................................................................................................... pag 134
Chapter IV. Colagenoses (Colagenoses, Mesenchymal Diseases, Diseases of Vascular
Collagen, Autoimmune Diseases) ......................................................................... pag 143
Colagenoses General aspects ............................................................................... pag 143
Acute articular rheumatism .................................................................................... pag 144
Juvenile rheumatoid arthritis .................................................................................. pag 149
Henoch-Schonlein Purpura..................................................................................... pag 154
Kawasaki Disease ................................................................................................... pag 157
Chapter V. Diseases of the Digestive System........................................................ pag 158
Gastro-esophagian reflux ........................................................................................ pag 158
3
Gastritis in children................................................................................................. pag 161
Ulcer disease........................................................................................................... pag 165
Malabsorption syndrome (Cystic fibrosis, Celiac Disease) ...................................... pag 167
Food intolerance ..................................................................................................... pag 182
Acute diarrheal disease in infants and children........................................................ pag 189
Syndrome of acute dehydration............................................................................... pag 198
Recurrent abdominal pain ....................................................................................... pag 207
Parasites.................................................................................................................. pag 215
Chapter VI. Nutrition and Deficiency Diseases ................................................... pag 221
Malnutrition........................................................................................................... pag 221
Iron deficiency anemia ........................................................................................... pag 229
Rickets................................................................................................................... pag 233
Tetanus ................................................................................................................... pag 245
Diabetes mellitus.................................................................................................... pag 250
Chpater VII. Renal System................................................................................... pag 266
Urinary infections in children ................................................................................ pag 266
Vesicoureteral reflux............................................................................................... pag 277
Postinfectious glomerulonephritis .......................................................................... pag 279
Nephrotic syndrome................................................................................................ pag 292
Acute kidney injury................................................................................................ pag 302
Chronic kidney disease............................................................................................ pag 304
Chapter VIII. Pathology of the Central Nervous System.................................... pag 308
Acute meningitis .................................................................................................... pag 308
Acute encephalitis................................................................................................... pag 320
Seizures and epilepsy in children............................................................................. pag 323
CHAPTER IX. Hematology................................................................................. pag 336
Anemia in children principles of diagnosis ........................................................... pag 336
PTI.......................................................................................................................... pag 338
Hemophilia A.......................................................................................................... pag 342
Chapter X. Pediatric Oncology............................................................................. pag 347
Leukemias............................................................................................................... pag 347
Malignant lymphomas............................................................................................. pag 353
Solid tumors (Neuroblastoma, Nephroblastoma) ..................................................... pag 358
4
FOREWORD
The current book is a manual containing basic notions of pediatrics, of importance to
pediatric practice, addressing both medical students and residents and practitioners,
pediatricians, and other physicians eager of clarification of issues encountered in pediatric
medical practice. This third edition of the book has been enriched and up-dated with the latest
news in the field, according to the latest guidelines in pediatric pathology.
The book is divided into ten chapters and includes notions of neonatal pathology,
respiratory, gastrointestinal, cardiac, hematologic and oncologic pathology, pediatric
nephrology, collagenoses in pediatric pathology, neurological diseases, diabetes and
metabolic aspects of the child diseases.
The clear, concise style, employing the absolutely necessary "technical" language,
makes this book attractive and easy to read, the approach and editing of the book,
representing clear evidence of this fact. Mention should be made that this book was designed
by a remarkable collection of primary-care physicians and pediatric specialists, academics at
the University of Medicine and Pharmacy of Tirgu Mures.
By reading it, you gradually come to realize its wealth of information, clarification of
concepts, as well as its accessible style.
Assoc. Prof. Oana Mrginean, PhD
5
CHAPTER I THE NEW BORN
Conf. Univ. Dr. Cucerea Manuela, Conf. Univ. Dr. Mrginean Oana
CHAPTER I THE NEW BORN
PERINATAL ASPHYXIA
Definition: Perinatal asphyxia is a clinical syndrome determined by insults that cause
reduction in fetal/neonatal oxygenation (hypoxemia), impaired gas exchange (hypoxemia,
hypercarbia) and inadequate tissue perfusion (ischemia). Asphyxia is defined as progressive
hypoxemia and hypercapnea accompanied by the progressive development of metabolic
acidosis that will lead to cellular damage and ultimately death of the newborn. This definition
has replaced the old definition of asphyxia at birth which referred to failure to install
adequate spontaneous respiration within 1-2 minutes after birth and correlated asphyxia with
the Apgar score. The criteria for defining asphyxia by the American Academy of Pediatrics
and American College of Obstetrics and Gynecology (1996) are:
- metabolic or mixed acidosis (pH <7.00, base deficit 12 mmol/l) in the cord blood or in
very early neonatal blood samples)
- Apgar scores of 0-3 beyond 5 minutes after birth
- early onset of neonatal neurological manifestations (seizures, hypotonia, coma, hypoxic-
ischemic encephalopathy)
- multiple organ failure (heart, kidney, liver, small intestine).
Thus, we have to distinguish between neonatal depression and birth asphyxia. Depression at
birth is characterized by low Apgar score, without changes in blood gases. Most often, the
time and the main cause of asphyxia remain unknown; it is actually a combination of
antenatal, intrapartum, and postnatal factors.
Pathophysiology of asphyxia. Transition and normal cardiorespiratory adaptation
Birth is a stressful and risky event for the newborn. Placenta-dependent gas exchange should
be replaced immediately after birth by autonomous pulmonary respiration. In the womb, fetal
circulation is characterized by relative hypoxemia (pO2 25-30 mmHg), but the fetus develops
normally since the placenta replaces many functions, thus fetal energy requirements are
reduced. Although there are intrauterine respiratory movements, the fetal lungs are not
functional and they are filled with lung fluid. Under the action of catecholamines sintetized
6
and released due to the stress of birth, the newborn adapts to extrauterine life. The factors that
initiate the first postnatal breath are:
1. chest compression that occurs when crossing maternal pelvigenital channel (exerts a
pressure of 60-90 cm H
2
O) causes removal of 1/3 of lung fluid volume. With the chest
decompression after expulsion, the chest volume increases due to the pleural vacuum
created and air enters the lungs.
Table 1. Etiology and risk factors for perinatal asphyxia
antenatal factors
intrapartum
factors
postpartum
factors
maternal
utero-
placental
fetal
hypertension
/toxemia
uterine
malformations
congenital
anomalies
breech
presentation
severe
respiratory
distress
hypotension twins
abnormal
presentations
(facial, transverse,
bregmatic)
apnea spells
heart/
lung diseases
placenta
praevia
Prematurity
/postmaturity
obstetrical
maneuvers/forceps
application
patent ductus
arteriosus
maternal hemorrhage/
anemia
polyhydramnios
placental
detachment
septicemia
diabetes (preexisting/
gestational)
uterine
rupture
intrauterine
growth restriction
umbilical cord
prolapsing
critical
congenital
heart
malformations
infections
placental
infarcts
fetal infections caesarean section
haemolitic
anemia/
isoimmunisation
meconium
amniotic fluid
2. interruption of fetal-placental circulation stops the oxygen supply (hypoxia), causes
accumulation of CO
2
(hypercapnia) and moderate acidosis, determining the stimulation of
chemoreceptors and respiratory center, with the onset of breathing.
3. sensory stimulations (cold air, differences of pressure between the intrauterine and
extrauterine medium, light, noise, newborn handling) excite the respiratory center through
the reflex pathways (nerve endings in the skin).
The lung distension during rhythmic lung ventilation causes the passing of the remaining
lung fluid and its subsequent resorption in pulmonary lymphatic circulation. The increase of
pO2 resulting from the initiation and assumption of gas exchanges by the lungs, will cause
7
reduction in the lung resistance by vasodilation in the pulmonary arterioles, that means
dramatic increasing of pulmonary blood flow and redirection of blood to the lungs. The delay
in installation of respiration leads to tissue hypoxia, that could compromise the newborn
survival and normal development of the central nervous system.
With clamping and cutting of the umbilical cord and placenta removal at birth, increasing
systemic pressure occurs, wich means increased pressure in the left ventricle (LV) and left
atrium (LA). Increased pressure in the left heart toghether with increasing of pulmonary
blood flow determine decrease in the right-left shunt through the ductus arteriosus (DA), and
increasing the venous return to the left, to the left atrium. When the LA pressure exceeds the
pressure in the RA, the foramen ovale closes. Decreased shunt through the ductus arteriosus,
and increased pO2 cause its constriction. Oxygen is the most important factor that controls
the DA constriction and closure, especially when its partial pressure is approximately 50
mmHg, through the inhibition of prostaglandin E
2
production.
Hypoxemia, hypoxia, asphyxia
Hypoxemia is a reduction of O
2
blood transport, leading to the the decrease of pO2.
Hypoxemia decreases O
2
content in tissues, resulting tissue hypoxia. Fetal response to
hypoxia involves an increase of the O
2
extraction in tissues, a decrease of central nervous
system activity, release of catecholamines, redistribution of blood to vital organs
(centralization of blood circulation), which maintain the energy balance for several hours.
The prolongation of hypoxia will cause the initiation of anaerobic metabolism that will
produce lactic acid and metabolic acidosis. The intrapartum hypoxia is the most important
cause of neonatal asphyxia by altering the placental gas exchange.
Breath is the first vital sign that is affected in O
2
deprivation. Decreased oxygenation in the
fetus or newborns leads to a period of rapid irregular breathing attempts, followed by
stopping (apnea), accompanied by decreased heart rate to 100 beats/ minute. Cyanosis is
present and blood pressure is normal or slightly increased. This clinical presentation
corresponds to the primary apnea and the stimulation by introduction of a suction catheter in
the mouth, or tactile stimulations can cause the resumption of breathing and increase the heart
rate. In the old nomenclature, this form of asphyxia was known as blue asphyxia. If nothing is
done and hypoxia continues after primary apnea, breaths become superficial, and after a few
gasps (unexpected sudden inspiration, apneustic type inspiration) the newborn enters in a
period of secondary apnea. (Fig. 1) This is characterized by a pronounced decrease in the
heart rate and blood pressure, marked hypotonia, lack of reactivity to stimuli. The infant will
not respond to stimulation and death will occur unless resuscitation begins immediately.
8
Initiation of assisted ventilation with bag and mask is needed to improve tissue perfusion.
Fetal hypoxia can determine both primary and secondary apnea. Both phases can be produced
in utero and they are clinically indistinguishable (in both cases the infant is not breathing and
the heart rate is low), so that any apnea at birth should be treated as secondary apnea, and
resuscitation maneuvers must be initiated in the first minute of life, prior to the assessment of
Apgar score. Heart rate and respiratory response to stimulation can help to estimate the
duration of fetal distress. If the infant does not start to breathe immediately after tactile
stimulation, most likely he/she is in secondary apnea and further tactile stimulation will not
have the desired effect. As a general rule, the higher the fetal distress was prolonged, the
longer the time it will take to normalize vital signs. Delayed resuscitation maneuvers
significantly increase the risk of irreversible brain damage.
Figure 1. Primary and secondary apnea (American Academy of Pediatrics)
The degree of brain damage depends on the severity and duration of hypoxia, which
determines metabolic changes with alteration of cerebral blood flow.
Apgar Score is an objective and a rapid method assessing the clinical status of the newborn
infant at birth, being also a useful index of the response to resuscitation. The score is
estabilished at 1 and 5 minutes of life, and in the case of resuscitation at up to 20-30 minutes
(from 5 to 5 minutes). If neonatal resuscitation is needed, it should be initiated immediately
after birth, before setting the score at 1 minute. Therefore, the Apgar score is not used to
determine the need for resuscitation. The score comprises 5 components: heart rate,
respiratory effort, muscle tone, reflex irritability, and color of the skin, each of which is given
a score of 0, 1, or 2. The score is obtained by summing the score for each of the 5 aspects
evaluated. Apgar score is determined for all infants regardless of their gestational age (GA)
and weight. (Table 2)
Table 2. Apgar Score
9
2 1 0
Skin color pink acrocyanosis pale/cyanosis
Heart rate >100 beats/minute <100 beats/minute absent
Respiratory effort effective gasps absent
Muscle tone good weak flaccid
Reflex irritability good weak, grimaces absent
Apgar score values of 10, 9, 8 indicate a clinically good status of the newborn and score
values below 8 indicate disturbances in the newborn adaptation to extrauterine life. A score
below 7 may be the result of immaturity, maternal medications, presence of congenital
malformations. The Apgar score has been used inappropriately to predict specific neurologic
outcome. 1 minute Apgar score does not correlate with subsequent neurological development,
and a 5-minute Apgar score poorly correlates with neurological sequelae. For example, a
score of 0-3 at 5 minutes was associated with a slightly increased risk of cerebral palsy, but
75% of children with cerebral palsy had normal scores at 5 minutes. The risk of neurological
sequelae increases when the Apgar score is below 3 to 10, 15 and 20 minutes.
The incidence of perinatal asphyxia is about 1-1.5% of live births in countries with
advanced perinatal care. The incidence is inversely proportional to gestational age. Perinatal
asphyxia is responsible of 20% of perinatal deaths.
Diagnosis of asphyxia
a. Prenatally diagnosis is achieved by:
1. Cardiotocography: fetal heart rate monitoring (normally between 120-160 beats/minute).
The following can be detected: tachycardia, bradycardia, or early or late decelerations.
2. Non-stress test (NST): recording the fetal heart rate for 30 minutes to of the pregnant
woman in lateral decubitus. Normally, the fetal heart rate changes in response to fetal
movements. The test is considered normal if two or more fetal heart rate accelerations is
are detected for a period of 15 seconds.
3. Stress test (ST) on contractions: the administration of oxytocin or stimulation of the
periumbilical skin stimulates uterine contractions, which in a fetus with hypoxia causes
late heart rate decelerations.
4. Fetal biophysical profile (FBP): is a test that measures five variable parameters: fetal
heart rate (NST), breaths, movements, tone, and amniotic fluid volume. The total score
that can be achieved is 10. FBP is performed after a non-reactive NST test, or after a
suspect ST. Echography is used to measure fetal breathing by detecting fetal chest
10
movements. Fetal movements are estimated by detecting movements of separate limbs or
of whole body.
5. Fetal ultrasound: assessment of gestational age, weight, detection of oligoamnios
(associated with fetal distress, pulmonary hypoplasia, urinary tract obstruction) or
polyhydramnios (associated with intestinal atresia), detection of malformations
(hydrocephalus, cardiac, renal)
6. Doppler ultrasound: measurement of blood flow in the umbilical artery and cerebral
arteries
7. Amniocentesis: determiation of fetal karyotype, IgM, hemoglobin, hematocrit,
biochemistry determinations.
b. Postnatal diagnosis
1. Clinical and neurological exam of the newborn: the presence of apnea at birth, low
Apgar score, changing consciousness (hyperexcitability, obtundation, coma), changes in
the other organs and systems (oligo-anuria, dysrhythmia, heart failure).
Clinical presentation: clinical manifestations after hypoxic injury have a very broad
spectrum, from mild to severe. Thus, they can be grouped in postasfixic syndrome, with
multi-organ involvement in severe forms.
- the post-hypoxic cardiac damage may clinically translate by in: cardiogenic shock, heart
failure, arrhythmia, hypotension, myocardial ischemia, transient hypertrophic
cardiomyopathy
- the post-hypoxic respiratory distress can manifest itself by pulmonary edema, pulmonary
hypertension and pulmonary hemorrhage, meconium aspiration syndrome, respiratory
distress caused by surfactant deficiency
- the post-hypoxic kidney damage becomes apparent through transient oligo-anuria, renal
failure, renal vein thrombosis.
- the post-hypoxic liver damage causes hepatic necrosis, increased liver enzymes,
cholestatic jaundice, vitamin-K dependent coagulation factor deficiency
- the post-hypoxic gastrointestinal damage manifests as ulcerative necrotizing enterocolitis,
especially in prematures
- the post-hypoxic haematological dissorders are manifested by the tendency to bleed
through thrombocythemia, disseminated intravascular coagulation. Poliglobuly may be
also present
- thermoregulation disorders manifest as hyper/hypothermia
11
Post-hypoxic brain impairment is the most serious consequence of perinatal asphyxia.
Cerebral hypoxia is a trigger for hypoxic ischemic encephalopathy (HIE). Initially,
hypercapnia and hypoxia cause redistribution of cardiac output, increasing systemic blood
pressure, playing a role in maintainin the cerebral blood flow. Prolongation of asphyxia
causes loss of cerebrovascular autoregulation, so that the cerebral bllow flow varies
proportionally with the systemic blood pressure; the cerebral circulation becomes passive,
vulnerable to changes pression: risk of ischemia in case of systemic hypotension and risk of
bleeding in case of correction of hypotension. After primary injury, a reperfusion phase
appears and this is followed by a secondary injury phase determined by the action of
resulting macroergic compounds. During reperfusion, hypoxic-ischemic injury triggers a
complex cascade of neurochemical reactions causing neuronal death. The mechanism of
neuronal damage involves circulatory, metabolic, cellular and biochemical factors. Massive
neuronal destructions occur. The clinical picture is that of hypoxic-ischemic encephalopathy
(HIE), the worst consequence being cerebral palsy. Sarnat described three clinical stages of
severity of HIE.
Figure 2. Loss of cerebral autoregulation
Stage I, mild form: it is characterized by irritability, tremor, myoclonus, normal muscle tone,
poor sucking reflex, increased Moro reflex, mydriasis, tachycardia, normal EEG. The
outcome is favorable
Stage II, moderate form: is characterized by lethargy, moderate hypotonia, myoclonus, weak
or absent sucking reflex, incomplete Moro reflex, miosis, bradycardia, abundant secretions,
low voltage EEG. Seizures are present. 20% of children are at risk for subsequent sequelae,
especially when seizures last more than 5 days.
12
Stage III, severe form: is characterized by the lack of response to physical stimuli (stupor,
coma), generalized hypotonia, areflexia. Oculomotor disturbances may be present
(nystagmus, ocular immobility), fixed mydriatic pupils or poorly reactive to light. Seizures
appear less frequently than in stage II, they can be generalized and usually resistant to
conventional treatments. The presence of cerebral edema is characterized by bulging
fontanels. Severe respiratory depression may occur with irregular/superficial breaths, severe
pulmonary hypertension, pulmonary hemorrhage or edema, imposing the need for ventilatory
support. Cardiac posthypoxic impairment is evidenced by cardiac arrhythmias, reduced
myocardial contractility, hypotension, severe cardiomegaly, tricuspid regurgitation. Intestinal
lesions initially invisible, is sometimes manifested by peristaltic diminished and delayed
gastric emptying. (Table 3)
Table 3. Clinical staging according to Sarnat & Sarnat 1976
STAGE 1 STAGE 2 STAGE 3
State of consciousness hyperexcitability Lethargy/obnubilation Stupor/coma
Muscular tonus normal hypotonia + hypotonia +++
Myoclonus + + -
Sucking reflex weak weak/absent Absent
Moro reflex strong incomplete Absent
Tonic neck reflex weak exacerbated Absent
Activity of autonomous
system
Generalized
sympathetic
Generalized
parasympathetic
Sympathetic and
parasympathetic
depression
Pupils mydriasis miosis variable, unequal
Heart rate tachycardia bradycardia Variabile
Bronchial secretions reduced abundant Variable
Gastro-intestinal motility normal/reduced increased/diarrhea Variable
Convulsions absent frequent Rare
Duration <24 hours 2-14 days days/weeks
EEG
Normal aspect
(awake)
Initial: microvoltage,
Late: foci
Initial: periodic
suppression
Late: generalized
suppression
13
Four phases of symptoms are described in moderate and severe stages. In the first 12 hours
after birth (the initial depression of muscle tone and consciousness), the following prevail:
hypotonia, decreased spontaneous movements, stupor, coma, periodic breathing but
pupillary response to light is intact, seizures in 50% of cases. The period 12-24 hours after
birth is of apparent improvement when a clear improvement in the level of consciousness
occurs, the newborn presenting a hyperalert aspect, being irritable with marked tremor of
stimuli.
Seizures may occur in 15-20% of cases and apnea attacks in 50%. Marked hypotonia in the
legs is predominant in the premature newborn as well as in the pectoral arch of the mature
newborn. The worsening period is described between 24-72 hours after birth, when a
reduction in the level of consciousness occurs, accompanied by severe respiratory distress or
respiratory arrest, oculomotor disturbances, lack of pupillary response to light. Death often
occurs at this stage because of severe intraventricular hemorrhage (premature newborn) or
extensive cortical necrosis (mature newborn).
After 72 hours from birth (period of consciousness disturbance improvement) infants who
survive, present gradual improvement but persistent neurological abnormalities are
characteristic in severely affected patients. Generalized hypotonia and disorders involving
difficulty in sucking and swallowing and therefore feeding, are characteristic.
2. Paraclinic Modifications
Table 4. Paraclinic modifications in HIE
Paraclinic examinations Modifications
Acid-base balance pH<7, PaO
2
, PaCO
2
Pulsoximetry SaO
2
<90%
Blood pressure BP - (Average BP
normal value 30 mmHg)
Hypo/hypertension
Glycemia hypoglycemia < 40 mg%,
Calcium hypocalcemia< 7 mg%
Potassemia hyperpotassemia>6 mEq/l
Urea >20 mg%
Creatinine >1 mg%
14
Transaminases
AST >140 UI/L
ALT >50 UI/L
Hemoglobin, hematocrit
Thoracic X-ray
Hyaline membrane disease, meconium
aspiration, congenital pneumonia,
cardiomegaly
Tranfontanelar echography, MRI, CT
Cerebral edema, intraventricular
hemorrhage, leukomalacia
Positive Diagnosis of perinatal asphyxia is based on corroborating:
- historical data (risk factors)
- prenatal diagnosis
- clinical features caused by primary / secondary apnea, Apgar score <3 up
to > 5 minutes of life (neurological, cardiac, renal changes)
- paraclinical modifications
Treatment of perinatal asphyxia
a. Prophylactic treatment
- proper monitoring of pregnancy, early detection of risk pregnancies
- early diagnosis of fetal distress, cesarean section indication
- avoidance of trauma at birth
- proper resuscitation of the newborn in the delivery room
b. Curative treatment
- in the delivery room: correct resuscitation of the newborn
- in ICU
- treatment of complications.
NEONATAL RESUSCITATION
90% of newborns have a normal adaptation to extrauterine life with regular breathing, heart
rate 100 beats / minute, are pink-colored. Children are vigorous and healthy looking. 10% of
the newborns require intervention and/or supportive care at birth, 0.2-0.5% have apnea,
bradycardia, pallor, hypotonia, and below 0.1% are dead but resuscitable (the heart had been
detected 10 minutes before birth). Neonatal resuscitation (NR) is includes all the procedures,
15
maneuvers and medical therapy used to help a newborn's transition from the intra- to the
extrauterine life or if the cardiorespiratory failure occurs during the neonatal period.
Newborn resuscitation is an emergency intervention, so it should be performed quickly,
every minute of delay entailing subsequent increased incidence of neurologic sequelae and
neonatal mortality. The neonatal resuscitation guide is designed at national level and
establishes the standards, principles and the fundamental aspects of neonatal resuscitation to
be respected by practicians regardless of the health unit in which they work. The conditions
for adequate resuscitation must avoid heat loss, the trauma and infection of the newborn.
These conditions must be ensured through the existence of a reanimation area (room),
located preferably in the delivery room or in its immediate vicinity. The resuscitation table
will have a radiant heater while aseptic and antiseptic conditions will be rigorous. The
resuscitation area must be equipped with:
- equipment for thermal comfort: radiant heater, sterile linen for wiping the amniotic
fluid
- secretion aspirator and Nelaton sterile probes (disposable) No 5, 6, 8,10 for suction of
mouth and nose secretions
- 0 and 1 blade laryngoscope and endotracheal intubation probes of different sizes
- Ambu resuscitation Balloon (for newborns) with oxygen tank and masks of different
sizes
- drugs: Adrenaline 1/10000, 4.2% Na bicarbonate, volume expanders
- needles, syringes, catheters, gloves, sterile gowns
Neonatal resuscitation implies the existence of a trained staff who know the physiology of
transition to extrauterine life and the resuscitation algorithm. Resuscitation maneuvers must
be gentle and quick. The cycle: assessment-decision-action is continuously followed. The
newborn is assessed, a decision is made and then we operate (for 30 seconds), every action
being followed by a new evaluation in order to assess its effects. Three criteria are used for
rapid assessment of the newborn:
16
Figure.3. Neonatal resuscitation equipment
- Heart rate (HR) is determined stetacustically, through palpation of he femoral artery
pulse or by counting umbilical cord pulsations for 6 seconds and the result is multiplied
by 10 (to obtain the rate / minute).
- Respiratory rate (RR) is assessed by the presence / absence of breath and the breaths
count, and stetacustically by the presence / absence of the vesicular murmur;
- Skin color is assessed by inspection: acrocyanosis, cyanosis, pale, white teguments.
Resuscitation maneuvers represent the Resuscitation ABC
A - Airways - airway patency
B - breath - ensuring breath
C - Circulation - ensuring circulation
Immediately after birth the following questions about the newborn must be answered : Does
the baby scream or breathe? Does he have a good muscle tone? Is the newborn
delivered at term? If you answer YES to these questions (baby at term who breathes, has
good tone) the newborn does not require resuscitation, only supportive routine care. If the
answer is NO to the above questions, the infant needs resuscitation
17
1. the newborn
screams/breathes
2. good muscular tone
3. term newborn
Supportive care
1. the newborn does not breathe
2. decreased muscular tone
3. premature newborn
Initiation of resuscitation
steps
Until recently, the resuscitation evaluation was also based on the tegument coloration
criteria. This criterion was abandoned because newborns are often slightly cyanotic during
the first minutes after birth, normal transition lasting several minutes. Term-infants will
require> 10 minutes for the saturation to be > 90%. At birth, it is recommended to attach a
pulse oximeter sensor on the right hand for determining preductal saturation. (Table 5)
Table 5. Normal SaO
2
at birth
Minutes after birth SaO
2
1 60-65%
2 65-70%
3 70-75%
4 75-80%
5 80-85%
10 85-90%
Resuscitation first steps consist in a series of quick maneuvers to be carried out in all infants,
regardless of birth condition.
1. Ensure airways permeability (A - airways)
It is performed through aspiration of oropharyngeal and nasal secretions (mouth first,
followed by nose). If secretions are in a small amount, aspiration is not necessary. Basically,
aspiration of secretions is made with a sterile, disposable probe. The newborn is placed in
18
supine or lateral position, head in slight extension ("sniffing" position) to align the pharynx,
larynx and trachea. The aspiration pressure will be within the 80-100 mmHg range, avoiding
posterior pharyngeal stimulation (vagal response risk with apnea and bradycardia).
Figures.4, 5, 6. Positioning, aspiration
2. Wipe, stimulate, reposition.
Newborn hypothermia increases metabolic rate and hence the need for O2 and energy
substrate. Cold stress increases the risk of hypoglycemia and metabolic acidosis. The child
will be placed immediately under radiant heating, on warm diapers, the skin will be wiped in
sterile diapers, wet sheets being removed and replaced with dry ones. Light tactile
stimulation to the feet and back is performed. Do NOT use water spraying, alternative hot-
cold baths, upside down feet hanging and buttocks kicking. These maneuvers commonly
used once, are now outlawed.
Figure 7, 8. Tactile stimulation (ac.Neonatal Resuscitation, 2013)
These steps should last about 10 seconds (the first 10 seconds of postnatal life), followed by
rapid assessment: coloring, HR, RR, evaluation which decides whether to perform the
resuscitation itself. If the newborn is in apnea, we proceed immediately to the next step:
19
3. Breathing initiation (B)- positive pressure ventilation (PPV).
If the newborn is not breathing or gasps, balloon and mask ventilation is initiated. An
Ambu for newborns is used for ventilation (Figure 3), equipped with O2 tank, pressure relief
valves and masks of different shapes and sizes depending on the child's weight. Mask
application must be tight, covering the childs mouth and nose and avoiding the eyes (may
be harmed). Ventilation is achieved by compressing the balloon with your fingers (Figure 4).
The first blowing pressure should be 30-40 cm H
2
O, followed by 20-cm H
2
O so as to avoid
barotrauma. The pace of ventilation must be 40 breaths / min (counting: breathing in-2-3). If
the ventilation is effective, rhythmic rise and fall of the chest is observed, bilateral breath
sounds are audible
Figure 9. Ambu Baloon Figure 10. Ventilation with baloon and mask
Some centers are equipped with modern resucitation devices which can play both the role of
resuscitation balloon and manual ventilator and CPAP machine (ensuring continuous positive
pressure ventilation), i.e. Neopuff T-piece resuscitator (Figure 8, 9). Free flow of 21-100%
O
2
concentration can be administered with it.
The most important indicator of PPV success is the heart rate increase, followed by the
appearance of spontaneous breathing and improved coloration. When effective spontaneous
breathing is installed, i.e. HR is> 100 beats / minute, ventilation is interrupted, skin coloration
is monitored and O2 in free flow may be administered until teguments become pink.
20
Figures 11, 12. Neopuff T-piece resuscitator
Figures 13, 14, 15. Administration of O
2
in free flow
The old resuscitation protocol included administration of 100% O
2
. Clinical studies have
shown, however, that there is no difference in terms of neonatal mortality and the risk of
hypoxic-ischemic encephalopathy when using air (21% O
2
) or 100% O
2
in neonatal
resuscitation.
[15]
According to modern protocols, resuscitation starts with 21% oxygen.
Additional O
2
is administered in order to achieve the SpO
2
in Table 5. If PPV exceedes 2
minutes, a nasogastric probe must be inserted to avoid stomach distension (which can prevent
lung distension) and the risk of aspiration. The tip of the probe is left open.
21
Figure 16, 17. Measuring the nasogastric probe (nose-year-xiphoid appendix pyramid)
If the HR is <60 beats / minute after 30 seconds of PPV, ventilation is continued and
external cardiac massage is performed. Likewise, oro-tracheal intubation may be
considered.
4. External cardiac massage (ECM)
External cardiac massage ensures circulation, i.e. compresses the heart between the
sternum and spine and pushes blood to the systemic circulation. It can be performed in two
ways: with the two thumbs over one another (the thumb technique) or the index and medius
of the same hand (technique of 2 fingers). The pressure is applied perpendicular to the third
lower sternum (below the internipple line) to avoid the xiphoid appendix, while the rib
frames shall not exceed 1-1.5 cm (1/3 of the anterio-posterior diameter of the chest) in order
to prevent rib fractures and liver damage.
Figurr 18, 19. Techniques of external cardiac massage
ECM is coordinated with ventilation: three simultaneous chest compressions followed by one
balloon insufflation (counting: 1 . 2 . 3 insufflation, 1 . 2 . 3 insufflation). Thus, in one
22
minute 30 ventilations will be carried out and 90 chest compressions (if performed at the
same time, the ventilation is ineffective). The cardiac massage will always be accompanied
by ventilation!
After 30-45 seconds of PPV coordinated with ECM, the child is re-assessed. If HR is > 60
beats/min, ECM is stopped and PPV is continued until HR is > 100 beats/ minute.
Subsequently, if there is effective breathing, routine care is continued, possibly free flow O
2
.
If HR is <60 beats/ minute, PPV and ECM are continued, resorting to endotracheal
intubation and medication.
5. Endotracheal Intubation
Endotracheal intubation may be considered at any stage of the resuscitation, depending on the
resuscitators experience. Indications are:
- meconium amniotic fluid, the infant is not vigorous
- a prolonged PPV is anticipated
- PPv with mask and balloon is inefficient
- ECM and adrenalin administration are necessary
- special indications: prematurity, diaphragmatic hernia
The laryngoscope is used for intubation, preferably with cold-light (optic fiber ) and straight
blade no. 0 for premature and no. 1 for the full-term neonate. The intubation probes have
different sizes depending on the newborns weight (Table 6)
Table 6. Sizes of endotracheal probes
Weight (w) Gestation age (weeks) Probe size (diameter) mm
<1000 <28 2,5
1000-2000 28-34 3
2000-3000 34-38 3,5
>3000 >38 3,5-4
Intubation probes should have a uniform diameter and should be sterile and disposable. The
tip of the probe shall not exceed the vocal cords by 1-1.5 cm (the probe must be in the
middle, into the trachea, to avoid hyperventilation of one lung and hypoventilation of the
other).
The laryngoscope is inserted on the right side of the tongue and the blade is advancing until
the tip is just below the base of the tongue, emphasizing the glottis and vocal cords, which
23
appear as two vertical strips on both sides of the glottis (the letter V inverted, figure 19,20).
Intubation will be performed within 20 seconds. If we fail within this time span, the baby wil
be ventilated between trials with the balloon and mask. The probe insertion depth is
calculated as follows: 6cm + child weight in kg (eg for a child of 2 kg, the probe will be
inserted 6 +2 = 8 cm).
Endotracheal tube position control will be stetacustic in three places: armpits bilaterally, and
the epigastric region (breath sounds should be equal, symmetrical, bilateral, and there is
absence of air entry into the stomach). Signs of correct position of the probe are:
- chest rises with each breath
- respiratory sounds are perceived on both lung fields
- vapor condensation occurs inside the probe in expiration.
A naso-gastric probe is also placed with intubation. In case of secretions in the
tracheobronchial tree, these can be aspirated with an aspiration probe through the
endotracheal tube.
Figure 20, 21. Orotracheal intubation, vocal cords in inverted letter V aspect shape
6. Medication
The umbilical vein is used for the administration of medication by direct injection or by
catheterization. For some drugs, the endotracheal tube.can be used.
a. Adrenaline is the first drug used in resuscitation
Adrenaline produces peripheral vasoconstriction, increases myocardial contractility and
increases the heart rate. It is sold in vials of 1 ml with a concentration of 1/1000. For neonatal
resuscitation it is used in dilution 1/10000, (1 ml of the diluted 1/1000 is diluted with 9 ml
physiological serum). Adrenaline is not indicated before establishing the ventilation!
24
Dose: 0.1-0.3 ml / kg rapidly of the 1/10000 dilution, intraumbilically, repeated after 3-5
minutes. Adrenaline can be administered endotracheally until the establishment of
intravenous access, the dose being 0.5-1mL/kg of the 1/10000 dilution . After administration,
PPV and ECM are continued. High doses can cause high blood pressure post-resucitation and
cerebral haemorrhage. If HR remains <60 beats/ minute, PPV, ECM, and intubation
effectiveness are verified, and existence of hypovolemia and severe metabolic acidosis are
considered.
b. Volume expander
Volume expander is used if there are signs of hypovolemia (pale skin under ventilation, weak
pulse, capillary recoloring time > 3 seconds) or if hemorrhage occurred during labor or birth.
Administration is through the umbilical vein, at slow pace in 5-10 minutes. The following are
used:
- physiologic serum 10 ml / kg
- Ringer's lactate 10 ml / kg
- 0I Rh negative blood: 10 ml / kg
Signs of volemic re-expansion: pallor mitigation, good pulse, increased blood pressure. If
hypovolemia persists, the volume expander dose is repeated.
c. Sodium bicarbonate
Consequences of prolonged resuscitation are lactic acidosis, decreased cardiac contractility
and pulmonary circulation. However, routine administration of bicarbonate (without
demonstration of acidosis through determination of blood gases) is controversial. Without
adequate ventilation and oxygenation, administration of sodium bicarbonate will not increase
the pH.
Recommended dose: 1-2 mEq / kg slowly iv at a maximum rate of 1 mEq / kg / minute.
Sodium bicarbonate is sold in solutions of 8.4% concentration (molar solution 1 ml = 1
mEq). In neonatal resuscitation a 4.2% solution is used (semimolar: 1 ml = 0.5 mEq) by
diluting the molar solution with physiologic serum.
d. Naloxone is administered to children with respiratory depression from mothers on
narcotics, 4 hours before delivery. Dose: 0.1 mg / kg iv or endotracheally.
e. Atropine and calcium are no longer used in neonatal resuscitation
Resuscitation lasts until effective breathing, pink skin and heart rate over 100 beats / minute.
If the heart rate is absent after 10 minutes of resuscitation, stopping the resuscitation can be
considered. The lack of response to resuscitation may be due to several factors: extreme
prematurity, pneumothorax, congenital pneumonia, diaphragmatic hernia, pulmonary
25
hypoplasia.
After resuscitation, infants are kept under close supervision, usually in a neonatal intensive
care department, to notice and correct various pathological aspects in due time. Several
problems can be detected after resuscitation: pulmonary hypertension, aspiration, pneumonia,
infections, seizures, apnea, hypotension, hypoglycemia, etc.
Resuscitation in meconium aspiration
Meconium amniotic fluid is a sign of fetal distress. Intrauterine hypoxia causes the
elimination of meconium in the amniotic fluid with the possibility of aspiration into the
airways, therefore, obstruction (especially in mature newborns and post-matures) and
installation of a very serious characteristic syndrome. Prophylaxis: meconium amniotic fluid
aspiration from the mouth and nose with the head expulsion to the perineum, before the
shoulders are borne. The newborn is not stimulated. After birth, the trachea is aspirated under
laryngoscopy view, by intubation.
Resuscitation is NOT initiated in the following circumstances:
- GA under 24 weeks, W < 400g
- anencephaly
- confirmed trisomy 13 or 18
2. TREATMENT OF PERINATAL ASPHYXIA IN INTENSIVE CARE
General Measures
- thermal comfort by placing in a servo control incubator
- complex monitoring: HR, RR, blood pressure, O2 saturation by pulse oximetry, urine
output, blood gases, blood glucose
- minimal maneuvers and stimulation
- noninvasive oxygen therapy (CPAP-continuous positive pressure ventilation) or invasive
(IPPV intermittent positive-pressure ventilation)
- total or partial parenteral nutrition 3-5 days
- correction of imbalances:
Hypoglycemia: administration of glucose intravenously at a rate of 4-6 mg / kg /
min
Hypocalcemia: administration of Ca gluconate 10% 400mg/kg/day infusion
Metabolic acidosis: is corrected if EB is above -11. Bicarbonate 4.2% is
administered by slow infusion according to the formula:
NaHCO3 to be admin. = EB x G x0, 3 (mEq)
26
- antibiotics protection: Ampicillin + Gentamicin iv, which is discontinued if cultures are
sterile.
B. Specific measures
Specific measures refer to the treatment of complications of perinatal asphyxia, i.e. the
postasfixic syndrome.
Cerebral Complications: the treatment includes control of cerebral edema through fluid
restriction of 40-60 ml / kg / day, induced mild alkalosis by mild hyperventilation and the
administration of sodium bicarbonate, administration of antioxidants: vitamin C, 100mg/kg,
administration of magnesium sulphate, induction of cephalic end hypothermia; cropping of
seizures with phenobarbital (20mg/kg loading dose, then 4-5 mg / kg / day maintenance dose)
or Phenytoin (20 mg / kg loading dose, 10 mg / kg / day maintenance dose).
Cardiovascular complications: the treatment includes restriction of fluids, dopamine and /
or Dobutamine iv (5-10 mcg / kg / min), Sildenafil (Viagra) for pulmonary hypertension (1-2
mg / kg / dose every 4 hours).
Pulmonary complications: the treatment consists of oxygen therapy, mechanical
ventilation, antibiotics.
Renal complications: the treatment includes restriction of fluid, electrolyte imbalance
compensation, administration of furosemide (1 mg/ kg/ day).
Liver complications: the treatment includes plasma, blood transfusions, vitamin K.
Gastrointestinal complications: the treatment consists of digestive rest, total parenteral
nutrition, antibiotics.
Hematologic complications: the treatment includes plasma, blood transfusions,
exsanguinotransfusion.
Evolution and prognosis
Perinatal asphyxia may increase neonatal morbidity and mortality. HIE stage I mortality rate
is below 1%, 98-100% of infants having a normal neurological development. 20-37% of
children with stage II die or present neurological sequelae. In stage III, mortality is high
(50%) and neurologic disabilities are: severe cerebral palsy, mental retardation, epilepsy,
visual impairment. Accurate estimate of severity of long-term complications is difficult.
Increased risk of cerebral palsy and death is given by:
- lack of spontaneous breathing after 20 to 30 minutes from birth
- seizure (onset within the first 12 hours of life), persistent neurological abnormalities over
7-10 days of life (hypotonia, rigidity), persistence of difficulties in eating
27
Bibliography
1. Morales P, Bustamante D, Espina-Marchant P, Neira-Pea T, Gutirrez-Hernndez MA, Allende-Castro C, Rojas-
Mancilla E. Pathophysiology of perinatal asphyxia: can we predict and improve individual outcomes? EPMA J. 2011
Jun;2(2):211-230.
2. McGuire W. Perinatal asphyxia. Clinical Evidence 2007;11:320, 1-21.
3. American College of Obstetricians and Gynecoclogists. Inappropriate use of the terms fetal distress and birth asphyxia.
ACOG Committee Opinion No 3216. Obstet Gynecol 2005; 106:1469-1470.
4. Sunshine P. Perinatal asphyxia: an overview. In: David K. Stevenson, William E. Benitz eds. Fetal and Neonatal Brain
Injury: Mechanisms, Management and the Risks of Practice, 3
rd
Edition, 2003, I:1-30.
5. Sharma A, Ford S, Calvert J. Adaptation for life: a review of neonatal physiology. Anaesthesia And Intensive Care
Medicine 2010, Elsevier Ltd. 12:3, 85-90.
6. American Academy of Pediatrics, American Heart Association. Manual de reanimare neonatal - traducere n limba
romn, Ed. 6-a, 2013.
7. American Academy of Pediatrics, Committee on Fetus and Newborn, American College of Obstetricians and
Gynecologists and Committee on Obstetric Practice. The Apgar Score. Pediatrics 2006;117;1444-1447.
8. Nelson KB, Ellenberg JH. Apgar scores as predictors of chronic neurologic disability. Pediatrics.1981;68 :36 44
9. Papile LA. The Apgar score in the 21st century. N Engl J Med. 2001;344:519520
10. Hansen AR Soul JS. Perinatal Asphyxia and HypoxicIschemic Encephalopathy. In: Cloherty J.P, Eichenwald E.C,
Stark A R, Hansen AR, Eds: Manual of Neonatal Care 7
th
ed, Lippincott Williams&Wilkins Philadelphia, 2012, 55:711-
729.
11. Manning FA. Antepartum fetal testing: a critical appraisal. Curr Opin Obstet Gynecol. 2009 Aug;21(4):348-52.
12. Manning FA. Fetal Biophysical Profile Score: Theoretical Considerations And Practical Application. In Arthur
Fleischer Ed, Sonography in Obstetrics & Gynecology: Principles and Practice, Seventh Edition, 2011, 23:705-713.
13. Hansen AR Soul JS. Perinatal Asphyxia and HypoxicIschemic Encephalopathy. In: Cloherty J.P, Eichenwald E.C,
Stark A R, Hansen AR, Eds: Manual of Neonatal Care 7
th
ed, Lippincott Williams&Wilkins Philadelphia, 2012, 55:711-
729.
14. Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress: a clinical and encephalographics study. Arch
Neurol 1976;33(10): 696-705.
15. Saugstad O.D, Siddarth R, Soll R, Vento M: Resuscitation of Newborn Infants with 21% or 100% Oxygen: An Updated
Systematic Review and Meta-Analysis, Neonatology 2008; 94:176-182.
16. Asociaia de Neonatologie din Romnia, Colegiul Medicilor din Romnia, Comisia de Obstetric i Ginecologie,
Ministerul Sntii, Comisia Consultativ de Pediatrie i Neonatologie. Reanimarea neonatal, ghid naional, 2011,
ISBN 978-973-632-712-4
17. Perlman JM, Wyllie J, Kattwinkel J et al. Neonatal Resuscitation 2010 International Consensus on Cardiopulmonary
Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation.
2010;122:S516-S538
18. American Academy of Pediatrics and American Heart Association. Textbook of Neonatal Resuscitation. Elk Grove
Village, IL: American Academy of Pediatrics and American Heart Association; 2005
28
RESPIRATORY DISTRESS IN NEONATES
Neonatal respiratory distress is any breathing difficulty in the first 28 postnatal days. The
etiology is varied, involving respiratory, cardiac, neurological, surgical, metabolic, causes.
Respiratory causes: choanal atresia, hyaline membrane disease, transient tachypnea,
aspiration of amniotic fluid, congenital and postnatal pneumonia, pulmonary
malformations, pneumothorax, pulmonary hemorrhage, persistent pulmonary
hypertension.
Cardiac causes: Cyanotic congenital heart malformations
Neurological causes: cerebral edema, intracranial hemorrhage, hypoxic-ischemic
encephalopathy, muscular disorders, phrenic nerve lesions
Surgical causes: diaphragmatic hernia, esophageal atresia
Metabolic causes: acidosis, hypoglycemia, hypocalcemia, hypomagnesemia,
hyponatremia.
Hematologic causes: anemia, poliglobuly, shock.
The clinical picture is dominated by:
1. Tachypnea: respiratory rate is greater than 60 breaths/ minute - up to 120 breaths/ minute
(normal 40-60 breaths/ minute)
2. "Combat breathing" Syndrome
- expiratory grunting: breathing with the partially closed glottis to keep the air in the alveoli
- inter and subcostal retraction, xiphoid retraction: as a result of respiratory effort, due to
accessory respiratory muscle contraction
- flaring of the nares: mechanism of respiratory compensation of the increased upper
airway resistance, nostrils widening to increase the breathed in airflow
- thoracic bulging - increased pulmonary volume
- thoraco-abdominal balance - secondary to diaphragm contraction abdominal expansion
and thoracic retraction in inhalation, the opposite in exhalation
- apnea is the respiratory pause of over 20 seconds or less but accompanied by cyanosis
and/ or bradycardia.
Distress severity is assessed by the Silverman score:
29
Table 7. Silverman Score
Silverman
Score
Respiratory
movements
Xiphoid
Retraction
Intercostals
retraction
Grunting on
exhalation
Flaring of the
nares with
inhalation
Score 0 present Absent Absent absent absent
Score 1
Apnea
period
Minimum Minimum
Audible on
stethoscope
minimum
Score 2
Thoraco-
abdominal
balance
Marked Marked
Clearly
audible
marked
Interpretation
Total = 0 absent SDR
moderate SDR
severe SDR
Total = 4-6
Total = 7-10
The score is obtained by summing up the score for each of the 5 evaluated items. A score of 0
indicates no respiratory distress and a score above 2 means respiratory distress of different
degrees (max 10).
Development of respiratory system
The airway system is a process consisting of 5 phases:
1. embryonic stage: until the 5th week, proximal airway development occurs. Abnormalities
occurring in this period: tracheal agenesis, tracheo-oesophageal fistula.
2. pseudoglandular phase: Week 5 -16. It consists in the development of lower respiratory
ways, which are surrounded by lymphatic vessels and capillaries. First respiratory
movements appear (after weeks 13-15). Diaphragmatic hernia occurs in this period.
3. canalicular phase: weeks 17-24. Development of bronchioles occurs, decrease of the
connective tissue, development of the capillary system. Pulmonary pathways are filled with
lung fluid secreted by type I pneumocytes. Type II alveolar cells involved in surfactant
synthesis appear between weeks 20 to 24.
4. terminal sac stage: weeks 24-37. Pulmonary acinuses develop (subsac and alveoli),
decreased interstitial tissue, expansion of capillary invasion, exponential increase of the
alveolar-capillary barrier.
5. alveolar phase: week 37-3 years. Proliferation and further development of alveoli take
place.
Type I pneumocytes facilitate gas exchange, and the type II secrete and store the surfactant.
This is a phospholipid compound (mix of sphingomyelin and lecithin) that reduces surface
tension in the alveoli, thus ensuring alveoli stability. Surfactant biosynthesis begins after 23-
30
24 weeks of pregnancy, its production increasing after 32-34 weeks and it is in sufficient
amount in term pregnancies.
That is why children born under 24 weeks do not have the necessary equipment to adapt to
extrauterine life, morbidity and mortality of these children being inversely proportional to
gestational age. Lung fluid removal is achieved by chest compression during delivery (30-50
ml) and resorption into the bloodstreamand pulmonary lymphatic circuit.
RESPIRATORY DISTRESS THROUGH SURFACTANT DEFICIENCY
Hyaline membrane disease (HMD)
Definition: Infant respiratory distress syndrome (IRDS) through surfactant deficiency
(SDRDS) is a pulmonary impairment that begins at or soon after birth, being characterized
clinically by tachypnea (respiratory rate > 60 breaths / minute), dipneea (inter-, subcostal and
sternal retractions), grunting on exhalation and central cyanosis occurring within 4-6 hours of
life, to achieve maximum severity up to 48 hours after birth and resolution in survivors at 48-
96 hours of life.
IRDS is pathophysiologically defined by low pulmonary compliance and significant
atelectasis at the end of exhalation due to abnormal synthesis (qualitative and / or
quantitative) of surfactant. It is the disease of immature lungs and surfactant deficiency, being
associated with prematurity. Synonyms: idiopathic respiratory distress, respiratory distress
with surfactant deficiency.
The Surfactant: It consists of phospholipids, neutral fat, cholesterol and proteins:
monounsaturated phosphatidylcholine (25%) disaturated phosphatidylcholine (40%),
phosphatidylglycerol (8%), cholesterol (4%), proteins (10%), neutral lipids (5%). Surfactant
synthesis is activated by active fetal cortisol and the exogenous cortisol administered
prenatally.
Functionally, the surfactant lowers the superficial tension at the air-alveoli interface which
allows alveoli expansion in inhalation and stops their colabation at the end of exhalation,
increasing lung compliance. Asphyxia, hypoxemia, hypothermia can inhibit the surfactant
synthesis, therefore the hyaline membrane disease can also occur in the newborn at term.
Chronic intrauterine hypoxia caused by uteroplacental insufficiency has a protective effect,
stimulating the surfactant synthesis (table 8).
31
Table 8. Risk factors for respiratory distress through surfactant deficiency
Factors increasing the risk of HMD Factors decreasing the risk of HMD
Prematurity Delay in intrauterine development
Male gender Female gender
Acute asphyxia Chronic maternal hypertension
Neonatal shock Pregnancy-induced hypertension
Rh Isoimmunisation Intrauterine chronic hypoxia
Neonate of diabetic mother Advanced maternal diabetes
The 2
nd
twin Mothers abuse of narcotics
Placental detachment Subacute placental detachment
White (race) Black (race)
Family history of HMD Antenatal administration of steroids
Cesarean delivery Premature rupture of membranes
Pathophysiology: Primary deficiency of surfactant (premature) or secondary (hypoxia,
acidosis) causes atelectasis by increasing the surface tension in the lung alveoli. Atelectasis
causes hypoventilation and change of ventilation perfusion ratio. Alveolar O2 decrease leads
to vasoconstriction, which increases hypoxemia through intrapulmonary shunt (due to
vasoconstriction in poorly ventilated alveoli) and extrapulmonary shunt (ductus arteriosus
and foramen ovale).
Vasoconstriction produces local disorders: alveolar-capillary hyperpermeability, fluid and
plasma proteins extravasation in the alveoli with hyaline membrane formation and interstitial
edema, which increase airway resistance, reduce pulmonary compliance and pulmonary
perfusion and increase the physiological dead space.
Pathologic anatomy: the lung is colabated, has liver consistency, the alveoli are colabated.
The hyaline membrane is composed of fibrin and blood and alveolar cells destroyed in the
alveoli; interstitial edema is present and the muscle tunic of the arteriolar wall is thickened.
Electro-microscopically: alveolar epithelial necrosis and absence of lamellar grain from type
II pneumocytes.
32
Clinical presentation
Onset within the first 10 hours after birth with respiratory distress syndrome of varying
degrees, which is increasing in the next 72 hours. Symptoms:
- Tachypnea: over 60 breaths / minute to compensate for current volume decrease and
increase of residual volume
- inter and subcostal retraction: due to the lung-inflation effort
- exhalation grunting: due to the semi-closed glottis exhalation to maintain end-exhalation
pressure within physiological limits (3-5 cm H
2
O)
- Nares flaring: due to increased respiratory effort
- Paradoxical breathing: abdomen bulging in inhalation, the diaphragm lowers.
- central cyanosis present in ambient air: bluish coloration of teguments and mucous due
to deficient oxygenation (more than 3-5 g / dl hemoglobin is desaturated)
- Other signs: hypothermia, arterial hypotension, progressive edema, generalized
hypotonia.
Clinical examination: stetacustically: diminished vesicular murmurs; disseminated crepitant
rales are detected in both inspiration and expiration. A heart murmur can be detected due to
patent ductus arteriosus.
Radiological picture: characteristic image from birth, bilateral aspect, air bronchogram with
bronchial image present up to the bronchioles, fine reticulogranular pattern with nodular
opacity given by the collabated alveoli and transparencies given by alveolar ducts. In mild
forms diffuse blurring appears, whereas in severe forms the aspect of matte glass with opacity
and disappearance of cardiac silhouette (fig. nr. 22).
Fig. 22. HMD radiologic aspect before and after surfactant administration
The natural evolution of the disease includes worsening of respiratory damage within 72
33
hours after birth. In some newborns improvement occurs after 72 hours when there is a
regeneration of type II pneumocytes and surfactant synthesis, but in severely affected infants
a rapid deterioration of respiratory function appears, long periods of apnea, vascular collapse,
critical evolution.
Paraclinical examination: blood gases: pO2 <50 mmHg, pCO2> 50 mmHg, pH <7.2, pulse
oximetry: SaO2 <90%.
Required tests: blood count, blood group, Rh, electrolytes, glycemia, urea, creatinine
(necessary to detect metabolic complications) bacteriological examinations: hemocultures,
peripheral cultures (to assess the risk of infection), echocardiography (the differential
diagnosis), transfontanellar ultrasound in dynamics (to evaluate relatively common
neurological complications).
Antenatal diagnosis is achieved by determining the ratio of amniotic fluid lecithin/
sphingomyelin. The normal value is > 2, which is 0 risk of HMD. Values below 1.5 = high
risk of HMD.
Positive diagnosis is made by correlation of history, clinical, radiological and laboratory
data:
- History (risk factors)
- Clinical examination: respiratory distress syndrome occurring within hours after birth
- Radiography: bronchograms appearance of matte glass with air bronchogram
- Blood gas analysis - to assess the IRDS severity.
Differential diagnosis
It is sometimes difficult to perform. It is done with respiratory distresses of other causes:
1. Bacterial pneumonia (streptococcus) - clinical and radiological features may be identical
but gram-positive cocci are detected in the insemination of the maternal cervical canal and
newborns gastric aspirate.
2. Transient tachypnea - a visible improvement after birth is described.
3. Aspiration of amniotic fluid - rare in pre-term babies, different radiological appearance
4. Persistent pulmonary hypertension - extremely difficult to differentiate
5. Respiratory distress of cardiac malformations: distress is not severe but hypoxemia is
marked (cyanosis does not improve with O
2
administration)
6. Intraventricular hemorrhage: sometimes indistinguishable. The following are obligatory:
examination of CSF obtained by lumbar puncture, transfontanellar ultrasound.
7. Distress from poliglobuly: Htc >60%, intense erythematous and purple teguments
8. Distress from anemia: Hgb less than 13 g%
34
9. Distress from metabolic imbalances: hypoglycemia, hypocalcemia, acidosis.
HMD Treatment
a. Prevention
prevention of premature birth by administration of tocolytics to pregnant women
maternal corticosteroids: Betamethasone 12 mg im every 24 hours, 48 hours before
delivery, or 4 doses of 6 mg Dexamethasone every 12 hours. Corticosteroids decrease
HMD severity and reduce the incidence of prematurity complication.
the neonatologist/pediatrician as part of the perinatal team should collaborate with the
obstetrician to transfer pregnant women with premature delivery imminence to a level III
maternity, according to legislation on maternal-infant care regionalization. Level III
maternity has the specific equipment, medications and the team of specialists needed to
ensure stability and optimal postnatal treatment of the preterm baby.
b. Stabilization in the delivery room
after the expulsion/ extraction, if possible, it is recommended to delay the umbilical
stump clamping for 30-45 seconds holding the newborn below the mothers level in order
to allow placento-fetal transfusion
supplemental oxygen should be administered to all preterm babies with central cyanosis
and / or low peripheral oxygen saturation (SpO2) according to GA and postnatal age.
Oxygen should be administered in the lowest concentration that can maintain a heart rate
of over 100 beats/ minute
stabilization of the preterm babies with IRDS and spontaneous breathing is done through
administration of continuous positive airway pressure (CPAP) with values of 5-6 cm
H2O using the T-piece resuscitator for alveolar recruitment. This reduces the need for
further MV and surfactant administration.
in case of preterm babies with IRDS and inefficient spontaneous breathing, administration
of a single balloon inflation is recommended before CPAP initiation.
c. Therapeutic conduct
General measures
- ensure thermal comfort (incubator to monitor skin temperature)
- complex monitoring: respiratory rate, heart rate, blood pressure, temperature, hemoglobin
O2 saturation (Sa O2), diuresis, glycemia, electrolytes, hemoglobin)
- oxygen therapy: heated and humidified O2 should be administered. It can be administered
by the mask, tent, CPAP (continuous positive pressure ventilation by nasal fork) IPPV
assisted ventilation (intermittent positive pressure ventilation) or high frequency (HFV).
35
Oxygen therapy must be conducted so as to maintain PaO
2
between 50-70 mmHg in
arterial blood and SaO
2
by pulse oximetry is 88%. O
2
therapy is carried out with strict
monitoring of blood gases, with rapid decrease in the concentration of the administered
O
2
, to avoid complications.
- parenteral nutrition, electrolyte and acid-base balancing, fluid restriction in the first days.
It is administered by umbilical or central venous catheter.
- erythrocyte mass transfusions to maintain the hematocrit above 40%
- protection antibiotics: Ampicillin + Gentamicin until we obtain the antibiogram from the
harvested cultures (peripheral or central).
Etiologic treatment
It consists in the administration of exogenous surfactant. Prophylactic surfactant
administration and / or curative in these premature infants decreases morbidity and mortality
risk of IRDS and its complications
a. Prophylactic: administered in the delivery room (within the first 15 minutes of life
after balancing) to all preterm babies with VG < 26 weeks - according to national IRDS
guidelines. Immediate or early extubation is recommended whenever possible (depending on
the clinical condition) as well as CPAP to preterm babies with high risk of IRDS with GA <
30 weeks after prophylactic administration of surfactant (INSURE technique intubation-
surfactant-extubation in CPAP). A modern technique is LISA (less invasive surfactant
administration - administration of surfactant through an endotracheal catheter without
intubation) and MIST (minimally invasive surfactant therapy)
b. diagnosis of HMD. The surfactant can be administered: early curative in the first
two hours of life, in the presence of IRDS signs, if chest radiography excludes other
pathology and increases the FiO2 needed by the premature or: late curative, after 2 hours of
life.
Preparations:
- Curosurf (natural extract of porcine lung). The dose is 100-200 mg / kg
- Survanta (natural extract of bovine lung). The dose of 4 ml / kg. It is administered
endotracheally in divided doses, followed by balloon ventilation through the endotracheal
tube for 30 seconds, between doses. After administration, mechanical ventilation is
established.
- Exosurf (synthetic surfactant). The dose is 5 ml/ kg.
During the administration, SaO2 is monitored by pulse oximetry, chest excursions, tegument
color. The immediate effects of surfactant are: improved oxygenation, increased lung
36
compliance (rapid decrease of the ventilator pressures is necessary to prevent barotrauma)
and improved respiratory distress. Endotracheal tube suctioning is prohibited for 2 hours after
administration. Complications of surfactant administration are: hypoxia, hypotension,
pulmonary hemorrhage, clogging of the intubation probe.
HMD COMPLICATIONS
A. Early:
- Infection: positive cultures
- intraventricular hemorrhage: abnormal tone, seizures
- patent ductus arteriosus: apnea, systolic murmur, cardiomegaly
- pneumothorax, pulmonary emphysema: respiratory status deterioration
- complications of intubation: cardiac arrest, subglottis stenosis
- umbilical artery catheterization complications: embolism, thrombosis, renovascular
hypertension, foot gangrene
- Complications of umbilical vein catheterization: embolism, perforation.
B. Late:
- pulmonary bronchodysplasia: result of mechanical ventilation and oxygen therapy for
long periods of time. Areas of atelectasis and emphysema are evident on x-ray. The
treatment includes administration of diuretics (furosemide 1 mg / kg, spironolactone 2
mg/kg/day) and dexamethasone (0.5 mg / kg / day, and then 0.25 mg / kg / day 1-2
weeks).
- premature retinopathy (retrolental fibroplasia): requires laser correction
- neurological sequelae of varying degrees.
The prognosis depends on: gestational age, present complications, competence of the
neonatal intensive care units.
In recent years, there has been a decrease in HMD mortality through proper monitoring of
premature births, improved quality of care at birth, administration of exogenous surfactant,
assistance of these children in specialized centers. Mortality is correlated with gestational age
and disease complications.
TRANSIENT NEONATALTACHYPNEA (TNT)
Synonyms: delayed lung fluid resorption, type II respiratory distress. Incidence: 1-25%.
Pathogenesis: the lung is filled with pulmonary fluid in intrauterine life. During delivery,
while the fetus passes through the pelvi-genital passage, the thorax is compressed, facilitating
37
the elimination of one third of the lung fluid. The remaining lung fluid is absorbed in the
lymphatic circulation in the first 24 hours after delivery.
The syndrome is secondary to delayed lung fluid resorption, resulting in decreased lung
compliance and current volume (tidal), and increased dead space.
Risk factors: cesarean section, male gender, maternal diabetes.
Clinical presentation: onset within 24 hours with respiratory distress: tachypnea (over 100
breaths / minute), pulling in of the chest/intercostal retraction, grunting sounds on exhalation,
sometimes cyanosis (reversible with O2 administration).
Radiological picture: normal appearance or layout of "wet" lung with perihilar or alveolar
opacities, with occasional pleural fluid blade.
Paraclinic picture: usually normal, without hypoxia, hypercarbia and acidosis
The evolution is favorable in 24 hours.
Differential diagnosis: is difficult to perform with HMD in early stages. Rapid favorable
evolution and no reticulonodular radiological image indicate TNT
The treatment includes thermal comfort and oxygen therapy.
MECONIUM ASPIRATION SYNDROME
Incidence: 5-15% of term or postmature newborns
Predisposing factors postmaturity, fetal distress, SGA (smal for gestational age) neonate
Pathogenesis: intrauterine hypoxia causes the elimination of meconium in the amniotic fluid.
By intrauterine gasping, meconium may be aspirated into the airways antepartum or at the
onset of the first postpartum breaths. Usually, newbornss are dirty or meconium-impregnated.
Aspiration of meconium amniotic fluid produces airway obstruction and chemical
pneumonia.
Obstruction may be total, producingl atelectasis, or partial (with valve effect) resulting in
obstructive emphysema and pneumothorax. These determine the decrease of lung compliance,
disturbance of the ventilation-perfusion ratio triggering: hypoxia, hypercapnia, and metabolic
acidosis.
Clinical picture: is characterized by respiratory distress with tachypnea, expiratory grunting,
intercostal retraction, the barrel chest, cyanosis, crepitant or bronchial disseminated rales in a
newborn with meconium amniotic fluid, requiring resuscitation at birth.
Radiological picture:
Opaque areas with areas of condensation on both pulmonary areas are present, separated by
38
areas of emphysema, increased anterior-posterior diameter, pneumothorax,
pneumomediastinum.
Fig. 3. Meconium aspiration
Treatment
A. prophylactic
- early detection of fetal distress and postmature pregnancies, delivery initiation.
- aspiration of meconium amniotic liquid from the pharynx immediately after the expulsion
of the head to the perineum
B. curative: neonates without asphyxia, with meconium amniotic fluid of low consistency do
not usually require treatment.
When the meconium has high consistency (pureed peas), tracheal suctioning through
endotracheal intubation is required and avoidance of the newborn stimulation. Massive
aspiration of meconium requires conventional assisted ventilation, sometimes with high
frequency or nitric oxide to fight hipercarbia, hypoxemia and acidosis. For the treatment
of pulmonary hypertension, sildenafil (Viagra, Revatio) is used at a dose of 1-2 mg / kg /
dose, 2-3 days
antibiotics: for prophylaxis or treatment of superinfection: Ampicillin + Gentamicin is
used initially or a third-generation cephalosporin associated with Amikacin
Complications:
- bacterial infection
- pneumothorax, pneumomediastinum
- persistent pulmonary hypertension.
Evolution: rapid death in massive aspirations; positive evolution for early treatment
Prognosis depends on the degree of neurological damage and pulmonary complications.
References
39
1. Asociaia de Neonatologie din Romnia, Colegiul Medicilor din Romnia, Comisia de Obstetric i Ginecologie,
Ministerul Sntii, Comisia Consultativ de Pediatrie i Neonatologie. Managementul sindromului de detres
respiratorie prin deficit de surfactant. Ghid naional 2011, ISBN 978-973-632-714-8
2. Bhakta KY: Respiratory distress syndrome. In Cloherty JP, Einchenwald EC, Stark AR: Manual of Neonatal Care. 6
th
Ed Philadelphia Lippincott Williams and Wilkins 2007; 323-330
3. Cloherty J.P, Eichenwald E.C, Stark A R: Assesment of the Newborn Hystory and Physical Examination of the
Newborn. In: Manual of Neonatal Care, sixth ed, Lippincott Williams&Wilkins Philadelphia, 2008, 59-72, 228- 237,
309-315, 317-323, 518-528.
4. Escobedo M: Moving from experience to evidence: changes in US Neonatal Resuscitation Program based on
International Liaison Committee on Resuscitation Review. J of Perinatol 2008; 28: S35-S40
5. Gomella TL: Hyaline Membrane Disease (Respiratory Distress Syndrome). In Gomella TL: Neonatology:
Management, Procedures, On-call Problems, Disease, and Drugs. 6
th
Ed Lange Clinical Science 2009; 477-481
6. Gomella TL: Respiratory Management in Gomella TL Neonatology: Management, Procedures, On-call Problems,
Disease, and Drugs. 6
th
Ed Lange Clinical Science 2009; 48-67
7. Morley CJ: Respiratory distress syndrome. In Polin RA, Yoder MC: Workbook in Practical Neonatology. 4
th
Ed WB
Saunders Co Philadelphia 2007; 129-150
8. Moss M, Thompson RT: Definitions and clinical risk factors. In Choi AMK: Acute Respiratory Distress Syndrome. 2
nd
Ed Informa Healthcare NewYork 2009; 9-201
9. Stoicescu S: Sindromul de detres respiratorie. In Stoicescu S. Boli pulmonare neonatale. Ed Universitar Carol Davila
Bucureti 2009; 85-100
NEONATAL INFECTIONS
Poor resistance to infections (due to their morpho-functional features), gives the following
features to the new borns infections :
- increased frequency (> 1%) - tendency of generalization
- poor, atypical symptoms - severe evolution (mortality 20-30%)
Classification is made according to the moment of infection. Thus we have:
- prenatal infections (antepartum)
- intranatal infections (intrapartum)
- postnatal infections (postpartum)
I. MATERNAL-FETAL INFECTIONS
These are infections that occur in newborns under 48 hours old. These are:
- chronic intrauterine infections grouped under the TORCH syndrome
- infections caused by Treponema pallidum, Listeria monocitogenes, varicella-zoster virus
- infections transmitted during labor and delivery - perinatal infections and intrapartum
40
infection (Streptococcus spp., E. coli, Gramm negative germs)
Transmission of infection is by hematogenous way, transplacental (TORCH), by ascending
way (by infected amniotic fluid) or intrapartum, by faeces, secretions, blood (direct contact
or aspiration).
II. NOSOCOMIAL INFECTIONS - HOSPITAL INFECTIONS
Nosocomial infections are infections that occur in the newborn over 3 days old. These
infections can occur from mother, from flora and hospital equipment, and nursing staff.
TORCH Syndrome: T = toxoplasmoza, O = other: HIV, hepatitis, etc, R = rubella, C =
cytomegalovirus, H = herpes simplex.
The incidence of the syndrome is 2.5 of live newborns. Intrauterine infections can cause
repeated miscarriages, mortinatality, prematurity, congenital malformations affecting long-
term prognosis.
Pathogenesis: the effect on the concept product depends on gestational age at which the
infection occurs, the virulence of germs and if the infection in mother is primary or recurrent.
Pathogens affect embryogenesis (embryopathy) or cause destruction of tissues already
formed (fetopathy).
Clinical manifestations: most affected infants are asymptomatic in the neonatal period or
present subtle signs, nonspecific, making diagnosis difficult. Other signs: deafness, visual
disorders, motor dysfunction are detectable later, so that these children must have a long term
follow up. Suggestive signs of congenital infections are:
- intrauterine growth retardation - jaundice
- hepatosplenomegaly - microcephaly/ hydrocephalus
- skin lesions - eye injuries
Congenital toxoplasmosis (toxoplasmosis fetopathy)
It is caused by Toxoplasma gondii, an intracellular parasite whose definitive host is the cat.
Transmission to humans is by gastrointestinal way (through food contaminated with cysts, or
through contaminated hands) or transplacental (from mother with acute infection). The
parasite is known to infect the CNS and eyes. Transplacental transmission is reduced when
maternal infection occurs during the first term of pregnancy (14%), but the severity of
infection is higher, often causing abortion; the risk of subsequent sequelae is 40%. In the 3rd
quarter, the transmission rate is 60%, the infection is benign, without increased risk of
sequelae.
The infection causes diffuse or focal meningoencephalitis with cerebral calcifications and
41
loss of cerebral substance, resulting in microcephaly, obstruction of Sylvius aqueduct and
foramen Monro (by calcification), causing hydrocephaly. Eye injuries are chorioretinitis,
iridocyclitis, cataract and microphthalmia. Other alterations are found in the lungs, heart,
kidneys, digestive tract.
Clinical presentation
a. The septicemical form is severe, with multi-organ involvement, fever, hemorrhagic
syndrome, jaundice, hepato-splenomegaly, lymphadenopathy, encephalopathy,
convulsions and rapid death or non-progressive sequelae (hydro-/ microcephaly,
intracranial calcifications fig 23, 24). It occurs in 10% of cases.
Fig 23. Microphthalmia
Fig 24. CT: periventricular
calcifications
b. Attenuated form: with mild symptoms, prolonged jaundice, microcephaly/ hydrocephaly,
chorioretinitis, hypotonia, drowsiness, which may be expressed later by psychomotor
retardation (progressive), seizures, hydrocephaly.
c. Latent form: without clinical manifestations.
Positive diagnosis:
Isolation of the parasite: from body fluids reflects the acute stage of the disease, while
isolation of cysts from tissues obtained by biopsy, is evidence of an old infection.
Prenatal diagnosis: amniocentesis, amniotic fluid and cultures from fetal blood
Postnatal diagnosis:
1. Serology:
Sabin-Feldman color test determines particularly the IgG, is sensitive and specific
Indirect fluorescent reaction measures IgG and is widely used in practice. The
antibodies detectable by these reactions appear in 1-2 weeks after infection, reaching high
titers at 6-8 weeks and gradually decrease after a few months. Low titers may persist
throughout life. IgG titer does not correlate with disease severity. A negative result for
42
IgG antibodies excludes previous exposure to T. gondii, except immunocompromised
mothers.
RIF test (Remington) detects IgM antibodies, being used for the diagnosis of acute
infection. IgM occur within the first 5 days after infection and disappear early. A negative
result virtually excludes recent infection (within the past 6 months). False positives tests
are described (at 60% of pregnant women with positive IgM result, recent infection is not
confirmed).
ELISA method determines IgM and IgG antibodies. IgM titer is increased over 1000 U/l.
A color or RIF test with titre over 1/1000, a RIF-IgM titres over 1/80 or IgM ELISA over
1/256 signifies a recently acquired infection.
Polymerase chain reaction (PCR) - quick diagnosis from blood and CSF.
Diagnosis of infection in pregnant women
Pregnant women with positive IgM and negative IgG antibody should be retested every 2
weeks until the occurrence of seroconversion or exclusion of a non-specific IgM response.
RIF-IgM or IgM ELISA are performed, which, if positive, indicate an acute infection. In their
absence, IgG RIF will be done and if the result is over 1/1000, it will be repeated every 3
weeks; if the same values are obtained, it means that infection occurred more than 8 weeks
before and risk for the newborn is reduced. Toxoplasma antigen detection in amniotic fluid
can be made.
Diagnosis of infection in the newborn
Serological tests from cord blood are performed in parallel with those from maternal blood;
detection of significantly increased titer of IgG antibody compared to the maternal, the
presence of IgM and/ or IgA antibody is diagnosis for congenital infection (IgM are present
in only 50-60% of children with congenital toxoplasmosis in the first month of life, and rarely
detected in children born from treated mothers). Serological monitoring should be performed
during the first year of life and the disappearance of IgG during this period practically
excludes congenital infection, mentioning that specific treatment can lead to the reduction or
disappearance of antibodies, but with "serological rebound" at treatment discontinuation.
2. Isolation of the parasite: from placenta, umbilical cord, brain, muscle.
3. Transfontanellar ultrasound, CT: periventricular calcifications are seen, hydrocephaly.
Treatment
Prevention: avoid the cat, insufficiently cooked pork, screening for toxoplasmosis in pregnant
women, treatment.
Treatment: newborn treatment - the most used combination:
43
Pyrimethamine 2 mg/kg/day the first 2 days, and then 1 mg/kg/day for 6 months, and
then the same dose up to 1 year, 3 days/week.
Sulfadiazine: 50 mg/ kg / day a year.
Folic acid 10 mg twice/ week during treatment with pyrimethamine (avoiding bone
marrow depression).
Corticotherapy Prednisone 1 mg/ kg/ day when there are inflammatory ocular lesions
and increased proteinorachia.
It is recommended to treat hydrocephaly: subcutaneous reservoir, ventriculo-peritoneal shunt.
Congenital rubella (rubella embryopathy)
Incidence: 0.7-7 per 1000 births.
Etiology: rubella virus transmitted transplacental.
Rubella virus can infect the fetus at any time during the course of pregnancy, the infection
being almost certain if the maternal disease occurs in the first term of pregnancy, outlining
the panel of congenital rubella syndrome. Virus excretion by the infected children continues
postnatally; they are contagious up to one year or more after birth. Congenital rubella
serologic diagnosis is made by determining specific IgM and cultures from nasal secretion,
urine and cerebrospinal fluid. Fetal pathology appears when the infection occurred in the first
16 weeks of pregnancy (the first 11: cardiac malformations and deafness, in 11-16 weeks
deafness). The risk for children is 85% in first 2 months of pregnancy, when termination of
pregnancy is recommended, 30% at the third month of pregnancy and 16% in 4-5 months of
pregnancy.
Clinical presentation is variable, depending on the gestational age at the time of exposure to
the infectious agent. Congenital rubella has a wide spectrum of clinical manifestations; in the
classical form, there is a triad: impaired eye (microphthalmia, cataract, glaucoma,
chorioretinitis); hearing impairment (deafness of perception), cardiac malformations. The
generalized form is characterized by the classical triad plus hepatosplenomegaly, cholestatic
jaundice, interstitial pneumonia, meningoencephalitis, lymphadenopathy, thrombocytopenia,
purpura, and evolving microcephaly, mental retardation, behavioral disorders. There An
asymptomatic form is also described (at birth), with late-onset, in the first 5 years, as
encephalopathy.
Positive diagnosis is suspected in newborns from mothers with proven or suspected rubella
during pregnancy, or those with mentioned clinical signs. Serologic diagnosis: specific IgM
antibodies in the newborn, the persistence of specific IgG at 6-12 months of life.
44
Prophylaxis: rubella vaccination in girls 1-18 years (Trimavax, Priorix). Immunoglobulins
do not prevent the disease. The treatment is symptomatic.
Infection with cytomegalovirus (CMV)
Incidence: 1/3000 births.
First cytomegalovirus infection is asymptomatic in 90% of cases. The increased risk of
transplacental transmission is in the first 22 weeks of gestation. Only 10% of the newborns
present clinical infection. There are three clinical forms:
1. Generalized form: hepatosplenomegaly, petechiae, jaundice with increased direct
bilirubin, thrombocytopenia. The following may also be present: microcephaly, intracranial
calcifications, optic atrophy, chorioretinitis; 25% of the symptomatic children die in the first
year of life by hepatic dysfunction, bleeding, DIC phenomena, superimposed bacterial
infection, severe neurologic impairment.
2. Localized form: neonatal hepatitis, thrombocytopenic purpura, neurological impairment.
3. Latent form: asymptomatic but with serological changes.
Pregnant women diagnosis: detection of CMV infection or IgMantibodies.
Diagnosis in children: clinical examination and identification of anti-CMV IgM. Other
nonspecific tests: lymphocytosis, hyperbilirubinemia, elevated transaminases.
The most common long-term complication is hearing deficit that occurs in 60% of
symptomatic children and in 5-10% of asymptomatic children. Long term prognosis for
asymptomatic children is good.
Prophylaxis: hygiene in pregnant women, screening.
Treatment is supportive. Certain antiviral agents: Ganciclovir 10-15 mg / kg / day 2 doses,
3-6 wk., Idoxuridine are under study.
Infection with Herpes Simplex Virus
The incidence is 1/2000-1/5000 births per year, involving especially type II virus.
The intrauterine transmission is rare. The newborn may present skin lesions, chorioretinitis,
micro-/ hydrocephaly, neurological sequelae. Most commonly, transmission occurs during
delivery. It can involve the skin, eyes or mouth, CNS or a disseminated form may be present:
thermal instability, apnea, jaundice, hepatomegaly, seizures, DIC. The mortality is high.
Diagnosis: viral cultures, serology.
Prophylactic treatment: indication of caesarean section when there are maternal genital
lesions, newborn isolation; if the mother presents active lesions, we will administer 0.6 ml/kg
45
Ig. standard in the new born; if the mother has primary infection (positive cultures) a
treatment with Ara-A 30 mg/kg/day will be initiated for 10-14 days from the 38th week of
gestation.
Treatment: is represented by supportive therapy, administration of Acyclovir 10
mg/kg/dose, slow infusion every 8 hours for 14 days.
Infection with Varicella-Zoster Virus
Incidence in pregnancy: 1-7/10.000
Clinical manifestations:
when the infection occurs in the first term, congenital varicella syndrome is found:
intrauterine hypotrophy, skin scarring, limb paralysis and atrophy by necrotizing myelitis,
eye damages (chorioretinitis, microphthalmia, optic atrophy);
when the infection occurs between the first quarter and last weeks of pregnancy, it has
only serological expression;
if the onset of maternal chickenpox occurs between 21-5 days before the birth, the
newborn will present benign neonatal varicella (vesicular rash), due to the transfer of
antibodies from mother to fetus; the prognosis is good;
if the onset of maternal varicella is <4 days before birth and 2 days after birth, the
newborn may present severe neonatal varicella: generalized rash, sometimes polivisceral
lesions (pneumonia, meningitis)
Diagnosis: based on the infectious contact, the clinical and laboratory examinations
(highlighting virus vesicles, positive serology).
Prophylactic treatment: isolation of pregnant women with chickenpox during labor,
isolation of newborns with varicella from other children, but not from mother, specific Ig
administration. Curative treatment: specific antibodies (0.3 ml/kg), supportive care, hygiene
of skin lesions.
Hepatitis infection
The main types of viruses are A, B, C, D and E virus.
Viral hepatitis type A: fecal-oral transmission, rare in newborns. Neonates may be
asymptomatic or may present acute hepatitis.
Diagnosis: detection of antibody.
Treatment: specific anti-A immunoglobulin 0.5 ml im, in the newborn from mother with
hepatitis A in the last two weeks of pregnancy.
46
Viral hepatitis type B is the most serious form of neonatal hepatitis.
Hepatitis B virus causes: specific antigen HBs (surface antigen, indicating acute infection);
HBc antigen (found in infected hepatocytes nucleum); HBe antigen (indicates active
hepatitis). HBs antibodies indicate healing and immunity after hepatitis; HBc antibodies
indicate acute/ chronic infection, HBe-antibodies indicate the resolution of the disease.
Transmission to the newborn:
- vertical: at birth
- transplacentar: rare
- parenteral: blood and blood products, infectious maneuvres
Risk factors:
- maternal infection in the third quarter of pregnancy or one month postpartum (80-90%
risk)
- chronic carrier mother of HBsAg and HBeAg: 80% risk
- mother with HBeAg and HBeAb: low risk: 10-20%
- mother with HBsAg: no risk of transmission to the newborn
Clinical presentation:
- asymptomatic infection: moderately increased transaminases, mild hepatomegaly,
HBsAg positive
- clinical hepatitis: jaundice, hepatomegaly, malaise, elevated transaminases; newborns
become chronic carriers of HBsAg and 1/3 of them progress to chronic hepatitis and
cirrhosis
Prophylactic treatment: compliance with universal precautions for personal, premarital
screening, early washing of babies from HbsAg positive mothers, gentle suction of secretions
to prevent injuries.
If the pregnant woman gets viral hepatitis A close to (or before term), the new born will be
administered Ig standard 0.5 ml/kg, and if mother had hepatitis A 2 weeks before birth, the
new born will be administered 0.15 ml/kg Ig standard.
Standard hepatitis B vaccination (in new borns from mothers AgHBs negative) (EngerixB,
Euvax B, Recombivax HG), first dose at birth: 10g (0.5 ml) or Recombivax HB 5g (0.5ml)
at 0-1-6 months or 0-2-6 months, with specific hepatitis B immunoglobulin (Hepatect).
Infants from mothers AgHBs positive are classically immunized, and they will get a dose of
specific Ig for hepatitis B (HBIg) as quickly as possible (the first 12h after birth). Their
immunological status will be supervised at 9 months. If the titer of antiHBs Atb is
>10mIU/ml and AgHBs negative, the infant will get one more vaccination at 0-1-6 months.
47
Fecal-oral or breastfeeding transmission of HBsAg after birth is minimal; breastfeeding is the
mothers free choice.
Streptococcal infections
Etiology: Streptococcus group B
Transmission: 5-40% of women are carriers of streptococci (vagina, rectum), 50% of the
children are colonized from their mothers; only 1-2% of the children get an obvious infection.
Clinical presentation: The infection has acute onset (in the first week), of the new borns
have signs of infection since birth. It manifests itself as a neonatal sepsis with respiratory
distress, lethargy, low blood pressure, they all have bacterimia;
1
/
3
- have distress and/or
pneumonia and
1
/
3
meningitis; 50% die.
The infection with tardive onset appears between 1 week and 3 months of life (the average 3-
4 weeks), meningitis is more frequent, although clinical forms are mild, some of them lead to
coma, status epilepticus, and the element of gravity is neutropenia.
Evolution: More than 50% of the survivors are neurologically affected: late speaking, loss of
hearing, loss of sight, mental retardation, uncontrolled seizures; some late infections such as
osteomyelitis, arthritis, adenitis, might appear.
Treatment: in bacterial sepsis is started with Ampicillin + Gentamicin until the cultures are
known. As a rule, the treatment is continued with Penicillin 450,000 IU/kg IV/day for 10-14
days and in meningitis for 3 weeks.
Prophylaxis: In pregnant women colonized with group B streptococci and which represent
one or more risk factors: premature birth, membrane ruptured for more than 24 hours,
prolonged labor, corioamniotitis, Ampicilin will be administered during delivery. Researchers
try to obtain a specific vaccine.
Congenital Syphilis
Etiology: Treponema Pallidum
The rate of transmission from mother to child is 70% at mothers with primary syphilis, 90%
at mothers with secondary syphilis and 30% at mothers with latent syphilis. In the absence of
the mothers treatment to the mother, the fetal risk is: 25% risk of fetal death, 25% of
perinatal death and 50% of congenital syphilis in the newborn.
Clinical manifestations:
- confirmed congenital syphilis
48
- presumptive congenital syphilis: any newborn of a mother with untreated or
improperly treated syphilis in pregnancy, any newborn with positive serologic tests
for syphilis, or clinical and radiological signs for syphilis, positive VDRL test from
CSF, FTA-ABS 19S-IgM positive test
Most infants with congenital syphilis are asymptomatic at birth. Precocious congenital
syphilis occurs in the first 2 years of life, symptoms debuting after the third week of life with
general signs: fever, lymphadenopathy (isolated), irritability and triad: rhinitis, palmar-
plantar pemphigus and splenomegaly.
Pemphigus is characteristic (palms and plants); the liquid is very infectious. After breaking of
the vesicles, scabs form. Other skin lesions include: rash, annular or in clusters lesions,
disseminated petechial lesions on buttocks, back, accompanied by cracked or bleeding lesions
of the mucous membranes (nostrils, palate, tongue, anus) . Rhinitis is highly contagious and
is purulent or hemorrhagic. Untreated, the septal cartilage may lead to necrosis resulting in
perforation.
Neurologic involvement: syphilitic meningitis, proteinorahia, polymorphonuclear
pleocytosis, hydrocephaly, optic atrophy, hemiplegia. Eye damage: chorioretinitis, uveitis,
glaucoma, eyelid canker. Lung injury: interstitial pneumonia. Renal impairment: nephrotic
syndrome, glomerulonephritis. Other: myocarditis, pancreatitis, malabsorption.
Radiological abnormalities: osteochondritis, periostitis, osteitis (yatagan tibia).
Haematological abnormalities: anemia, leukopenia/ leukocytosis, thrombocytopenia.
Laboratory diagnostic: nonspecific tests: positive VDRL.
Specific tests: FTA-Abs (absorption fluorescent treponemal antibody test) MHA-TP (micro-
hemagglutination test for Treponema). CSF exam: pleocytosis mononuclear proteinorahia,
positive VDRL from CSF.
Treatment:
Neonatal criteria: clinical signs of congenital syphilis, VDRL 4 times higher than of the
mother. Penicillin G is administered 50,000 IU/kg/dose every 12 hours during the first 7 days
of life, then every 8 hours. The duration is 10-14 days.
Monitoring: newborns from positive mothers at birth are followed up clinically and
serologically until the normalization of the tests. Neonates with antibodies transferred from
the mother and those properly treated will have decreasing antibody at 3 months and will be
negative by 6 months. Abnormal CSF examination involves CSF checking until
normalization.
49
INTRANATAL INFECTIONS (Bacterial infections transmitted during labor and birth)
Risk factors: chorioamnionitis, ruptured membranes for over 18 hours, maternal fever over
38 C, urogenital infections, streptococcal or Gramm negative vaginal colonization,
prematurity.
Germs involved: Streptococcus group B, E. coli, Hemophilus influenzae, Klebsiella,
Enterobacter, Pseudomonas, Staphylococcus aureus, Listeria.
Listeria monocytogenes: neonate contamination takes place during birth, but also prenatally
(!).
Clinical manifestations: Early forms, septicemia, late form in 3-5 weeks after birth, located
at meningean level. Features: small white pharynx granulomas and no. of mononuclears in
the CFS.
Treatment: Ampicillin 200 mg / kg / day in 4 divided doses im Gentamicin 14 days, 21 days
in meningitis.
Chlamydia trachomatis (1970) most freq. cause of sexually transmitted infections
Clinical manifestations: Chlamydia conjunctivitis (inclusions) - 5-14 days incubation;
purulent secretion. (Epithelial inclusions are observed through Giemsa staining of secretions).
Mother-child transmission in 10% of cases also causes pneumonia
Diagnosis - expensive (cell culture, direct immunofluorescence, ELISA, PCR)
Treatment - macrolides (erythromycin, clarithromycin, azithromycin) and tetracycline.
Neisseria gonorrhoeae
Clinical manifestations: gonococcal conjunctivitis. Treatment: 10 days with penicillin G, i.m.
plus ocular instillation (2,500 IU / 1 ml), others recommend 1 % chloramphenicol, sol.,
neomycin, 0.5%, 0.3% gentamycin.
Nongonococcal conjunctivitis. Appears at 24 hours after birth,! NOT to be mistaken for
chemical irritation produced by conjunctival instillation with AgNO3.
Usually, the local treatment is sufficient (instillation into the conjunctival sac).
Some cases require antibiotics - depending on the causing agent, after results of insemination
of conjunctival secretion in various culture media.
ACUTE INFECTIONS IN NEONATES
The most frequent infections are: nn septicemia, nn meningitis, nn pneumonia, nn umbilical
infection and cutaneous. The most severe and feared is septicemia.
50
NEONATAL SEPTICEMIA
Neonatal septicemia (and meningitis) represents a serious clinical context, with
unpredictable evolution. These are determined by various germs, developing a primary
outbreak and the appearance of septic metastases by pathogen migration in general
circulation. Bacteremia is transient downloading of germs in the bloodstream, proven by
positive blood cultures. Incidence: 1-8% from live new borns, one third of them also develop
meningitis.
Predisposing factors:
immunological immaturity of newborns, the smaller the gestational age is, neonatal
asphyxia, intracranial hemorrhage
maternal infection: sepsis, bacteremia, urinary tract/ vaginal infections, premature
rupture of membranes for more than 24 hours, difficult birth, maternal toxemia
nosocomial infections: overcrowding, broken medical circuits, bubbled water and water
from incubators, invasive maneuveres (puncture, catheterization, central venous access),
mechanical ventilation, poor hygiene of staff, misuse of antibiotics.
The admission gate: respiratory, skin, gastrointestinal, umbilical.
Etiology: Group B streptococcus (15-20% of women are colonized), E. coli (the first case in
Romania), Klebsiella, Pseudomonas aeruginosa, Proteus, Salmonella, Candida albicans.
Clinical: no typical symptoms, even fever may be absent.
a. alarm signals (arise from several hours to several days after birth): the newborn who
"doesn`t looks good", pronounced weight loss, vomiting, refusal of food, hypothermia,
spontaneous groan or at handling, earth-colored tint of the skin
b. during the state period, there is a syndrome characterized by severe infection: malaise,
impaired thermoregulation, hypotension, changes in the skin (purpura, necrotic lesions,
early, intense jaundice, omphalitis, edema), respiratory disorders (apnea, tachypnea,
respiratory distress), cardio-circulatory collapse (tachycardia/ bradycardia, pale mottled
skin, hypotension, capillary recoloring for more than 3 seconds), digestive signs
(abdominal distension, hepatosplenomegaly, vomiting), signs of meningitis (irritability,
abnormal tone, seizures)
Laboratory examinations
When there is suspicion of sepsis:
51
bacteriological samples from gastric aspirate, blood, urine, CSF, throat, umbilicus, stool,
external auditory canal
CBC should be taken: leukopenia <5000/mm
3
, leukocytosis> 33000/mm
3
, neutrophil
count <1000/mm
3
, immature neutrophils report/ total neutrophils >0.2, thrombocytopenia;
other tests: ESR >15 mm/h in the first hour of life, positive CRP, impaired coagulation,
metabolic acidosis, hyperbilirubinemia, thoraco-abdominal radiological examinations.
Signs of certainty: positive blood culture, positive CSF culture (with low glicorahia and high
proteinorahia or low CSF glucose, increased CSF proteins).
Prophylactic treatment: screening in all pregnant women, at 35-37 weeks (cultures of
vaginal secretions, urine culture), antibiotic prophylaxis in those with positive cultures.
Treatment: antibiotics are initiated at the time of suspicion, after bacteriological sampling.
Broad-spectrum antibiotics are preferred: Ampicillin 150 mg/kg/ day IV to 12 hours,
Gentamicin 2.5 mg/kg/dose i.v. 12, 18 and 24 hours, depending on gestational age, or a 3
rd
generation cephalosporin. In nosocomial infections consider the 4
th
generation cephalosporin
(Maxepin), Vancomycin, Tienam, Meropenem. Antibiotic treatment is corrected according to
pathogen susceptibility results, treatment duration being 10-14-21 days, especially in cases of
meningeal involvement and 4-6 weeks in osteoarticular impairment
Association of first intention antibiotics according to etiology: Anaerobic - Penicillin, except
Bact. fragillis - chloramphenicol, carbenicillin, cefalosporne, Metronidazole, listeria -
Ampicillin + Gentamicin 14 days Gram neg. enterococci: Ampicillin + aminoglycoside
(Gentamicin, Kanamycin), Pseudomonas, Proteus indole + - carbenicillin, 10-14 days.
Supportive treatment: maintaining thermal comfort (incubator), complex monitoring
(respiratory rate, heart rate, blood pressure, diuresis, oxygen saturation, blood gases, urea,
creatinine), fluid resuscitation (umbilical catheterization).
Treatment of septic shock: plasma, human albumin 5% 10-20 ml/kg, Dopamine/ Dobutamine
5-20 mcg/kg/minute
Immunologic and hematologic treatment: human immunoglobulin 500-1000 mg/kg/dose
every 2 weeks, transfusion of fresh blood, plasma, red blood cell, platelet, exanguino-
transfusion.
Evolution: depends on the gestational age of the newborn, germ involved and the presence of
complications. Mortality is high; septicemia is the 3rd leading cause of death in ICU after
hyaline membrane disease and congenital malformations.
Neonatal Meningitis
52
Purulent meningitis is given by a different spectrum than bacterial meningitis of infants over
2 months.
Etiology: Gram neg. Enterobacteriaceae: coli, streptococci gr.B, staphylococci, Listeria,
anaerobic, rarely H. influenzae, meningococcus, pneumococcus
Positive diagnosis: vague symptoms - irritability / lethargy, fever, bulging fontanelle (late),
rarely convulsions, vomiting, without signs of meningeal irritation
Fulminant onset with shock and rapid evolution - some signs in the teminal status.
Practical Rules: lumbar puncture is performed in the infant with suspicion of meningitis.
Agiation, irritability, fever - meningitis until confirmation of other diagnosis. Seizures
associated with fever - an indication of LP
Supporting positive diagnosis: LP shows cloudy CSF, l> 10/mm3, germs / smear, cultures +
glicorahia / glycemia <0.5 advocate for diagnosis support. Other foci are looked for (hemo-,
urine cultures)
Tratatamentul antibiotic se adminstreaza 21 zile, I.V.
Treatment: as in the case of sepsis, maximum doses of antibiotics according to antibiogram.
Group B streptococci - penicillin + gentamicin 14 days, then another 7 days Penicillin. Gram
neg. - Difficult (resistant to penicillin, some resistant to Ampicillin, gentamicin penetrates
CSF with difficulty). Moxalactam, other gen.III cephalosporins for. Gram.neg. resistant to
aminoglycosides and Bacteroides (50-100 mg / kg / day, 2 doses), for gen III E.coli -
Cefotaxime 50mg/kg/dose at 12 or 8 h; Ceftazidime, etc.
Antibiotics treatment is administered at 21 days i.v.
General treatment - supportive and symptomatic, seizure control, liquid restriction
(inappropriate ADH secretion) in newborns under 5 days max. liquids: 40ml/kg/day, after 5
days restriction may reach 20ml/kg/day
Discharge criteria: careful neurological assessment upon discharge, but not before 5 fever-
free days, as relapses occur in the third day from antibiotic cessation.
Ulcerative necrotizing enterocolitis
Etiology. It is considered that initially there are ischemic lesions of intestinal mucosa (due to
hypoxia and acidosis). Post-ischemic intestinal stasis and energy substrate provided by
enteral nutrition promotes proliferation of saprophytic or pathogenic gut flora (Enterobacter,
E. coli, Pseudomonas, Salmonella, Staphylococcus epidermidis, Klebsiella, Campylobacter,
enteroviruses), the emergence of intestinal pneumatosis (gas in the intestinal wall) and
perforation and peritonitis with septic disseminations.
53
Risk factors: prematurity, asphyxia, acute cardiopulmonary disease, enteral nutrition
(formula milk and hyperosmolar drugs), polycythemia and blood hyperviscosity syndrome,
exanguino-transfusion, umbilical catheterization.
Ulcerative necrotizing enterocolitis is a disease that occurs more frequently in neonatal
intensive care units taking care of children with low gestational age and where invasive
techniques are used for diagnosis and treatment.
Symptoms and diagnosis: ulcerative necrotizing enterocolitis occurs 3-7 days after initiation
of enteral feeding, the most common and early clinical signs (70%) being abdominal
distension (bloating). Also, there is ileus, with absence of intestinal noise, gastric residue that
becomes bloody or bilious (2/3 of cases), bloody stools, ascites, abdominal wall infiltration,
thermal instability, seizures, apnea, bradycardia, and finally signs of shock and DIC. Three
developmental stages are described: stage I (non-specific systemic signs, abdominal
distension, gastric residue, occult stool bleeding), stage II (bloody stools, abdominal wall
edema are added) and stage III (signs of shock).
Laboratory tests: abdominal radiography from AP and lateral incidence points, depending
on the stage of the disease: dilated bowel loops, pneumatosis and air leakage in the portal
system and pneumoperitoneum. CBC: anemia, leukopenia or leukocytosis with left deviation,
thrombocytopenia <50,000. Blood and stool culture analysis are usually positive, and blood
gases show metabolic acidosis. Biochemical determinations (urea, creatinine) are altered.
Hyperkalemia due to enhanced hemolysis is present.
Treatment
- cessation of enteral feeding in order to put the digestive tract to rest (10-14 days)
- continuous naso-gastric suction catheters for intestinal decompression
- strict cardio-respiratory monitoring, pulse oximetry, BP, urine output, fluid intake, stools,
waist circumference measurement
- repeated radiological control, surgical consult
- removal of umbilical catheters, removing potassium infusion
- antibiotics: Ampicillin + Gentamicin IV or Cefotaxime IV (10-14 days), and then
corrected after antibiogram; metronidazole may be considered
- total parenteral nutrition, correction of electrolyte and acid-base imbalances
- supportive care: oxygen therapy, mechanical ventilation, red blood cell transfusions,
plasma, Dopamine infusion
- surgical treatment in case of intestinal perforation
54
Prognosis: mortality is 20-40%; complications can occur: short bowel syndrome, subacute
intestinal occlusion caused by strictures and stenoses.
Skin and mucous infections
MONILIASIS - muguet
Etiology-Candida albicans at the passage through the pelvi-genital channel or postnatal
contamination from healthy carrier
Clinical manifestations: oral lesions (jugal, tongue, gums, palate) - small white deposits,
confluent, not detached; rare perianally or disseminated
Certainty diagnosis: - Methylene blue smear. micelles, spores
Local treatment: Na bicarbonate Sol. 4.2%, 0.5% dequalinum chloride, gentian violet 0.5%
of 3-4x/day, 3-4 days, 4-6 slow oral instillations with Stamicin suspension (100,000 U / ml);
Generally indicated in unfavorable evolution (! Food hygiene, boling the teats) - Treatment
with Stamicin 100,000 U / kg / day 4 times, 7-10 days + gel / suspension Miconazole or
Netamicin - instillation or local applications
BULLOS IMPETIGO (pemfigus)
Staphylococcal etiology
Clinical manifestations: bullous lesions with clear content, in 2-3 days - turbid and then
purulent, successive bursts up to 4 weeks, in good general condition.
Diagnosis by highlighting the content germ
Treatment: isolation, baths with KMnO4 solution 1:10.000, toilet with Rivanol 1%, powder
with sulphonamide antibiotics, ointment in case of crusts; in case of superinfection antibiotics
are administered parenterally
RITTER EXFOLIATIVE DERMATITIS
Etiology: staphylococcal endotoxin
Clinical manifestations: "Scalded skin" syndrome, - B. Ritter and Lyell syndrome,
staphylococcal scarlet fever; similar etiology with toxic shock syndrome. Sudden onset
generalized erythema, epidermal detachment (Nikolsky sign +), large breaking bubbles, toxic
condition
Treatment: local - as impetigo + symptomatics; General penicillinase-resistant penicillin -
Oxacillin 100-200mg/kg/day 4h 7-10 days. Supportive treatment, hydration, maintaining
body temperature.
55
Umbilical infections
After sectioning, through devitalization the umbilicus becomes a wonderful culture
environment for germs, being colonized in short time after sectioning through local flora
represented by streptococci and staphylococci.; Represents a gate for tetanos, diphtheria and
erysipelas.
Omphalitis: Inflammation of umbilical ring, it is an inflammatory process characterized
through hyperemia and edema of periumbilical regions, sometimes with a bad smell of the
umbilical blunt.
Etiology: staphilococci, streptococci
Symptomatology:
symptoms of inflammation (fever might be missing) +
manifestations depend - if the umbilical blunt fell or not
Blennorrhea = flowing of the navel cord after the fall.
Umbilicus ulceration =lack of substance covered by pus and tumefied sides.
Granuloma = red bud, juicing
Umbilical phlegmon appears when infection have propagated and also in subcutaneous
cellular tissue
Diagnosis - similar to septicemia
Treatment:
Remove any catheter
Aseptic care of umbilicus and desinfectants (rivanol 1%, hydrogen peroxide, KMnO
4
)
antibioticotherapy: Penicillin G 100000-200000 UI/kg/day + Oxacillin 100 - 200
mg/kg/day in 4 doses IM 10 - 14 days
outlining with nitrate de Ag in granuloma
Surgical treatment in phlegmon
Local treatment in blennorrhea and ulcerations
PROPHILAXY OF INFECTIONS IN THE NEW BORN
Rules for the prevention of infections in newborns
- depict and treat any infections in pregnant women
- correct birth assistance (maternity, qualified staff, hygiene)
- prophilaxy of pulmonary infection: correct oropharyngean vacuuming immediately after
birth
56
- ocular and umbilical prophilaxy
- serious measurements of asepsy and hygiene (in the delviery room, ward, home)
- hand hygiene: frequent washing with water and soap, short nails, avoid rings; most
infections are spread through hands!
- wear lint mask, frequently changed
- detection of germs carrier in medical staff, family
- precoceous isolation and fast treatment of the new borns infections, starting with
suspicion
- it is forbidden to visit the new born; ill mothers and medical staff are forbidden to have
contact with the new born if they present fever or have respiratory, skin infections or
enterocolitis
PATHOLOGICAL JAUNDICE IN NEW BORNS
Definition: Jaundice is the yellow coloration of teguments and mucosa through increase of
serical blirubin values. Jaudince is evident in new borns at values of 5-7 mg%.
There are three types of jaudince: physiological, pathological and nuclear.
I. Physiological jaundice
Physiological jaundice is a hyperunconjugated (indirect) bilirubinemia in which total
bilirubin is under 12 mg/100ml serum (N < 1.15 mml/l) and conjugated (direct) bilirubin is
under 15% from total bilirubin.
Incidence: it appears in 50-80% in new borns at term and 90% in premature.
Etiology: The causes of physiological jaundice are:
- increased blood volume - short period of life of fetal erythrocytes
- inefficient erythropoiesis - poor hepatic conjugation
- intensification of entero-hepatic circulation
Clinical: Physiological jaundice appears from the 3
rd
day (after 48h of life) and lasts for 7-10
days in the new born at term and more than 30 days in prematures. Physiological jaundice is
without hepatosplenomegaly.
Treatment:
Prophylactic treatment : precocious breastfeeding (colostrum has purgative effect).
Curative treatment phototherapy.
57
II. Pathological jaundice
Etiology: The pathological jaundice appears in:
- disorders of production
- disorders of metabolism
- disorders of bilirubin excretion
The pathological jaundice appears in the first 24-36 h (precocious jaundice), with a total
bilirubin over 12mg% in new borns at term and more than 15mg/100ml serum in prematures,
or a direct bilirubin over 1.5-2mg%. A jaudince for more than 10 days in new borns at term
and over 2 weeks in prematures defines the prolonged jaundice (table 9, 10, 11).
Table no. 9. Etiology of pathological jaudince
Precocious jaundice Prolonged jaundice
Hemolytic disease through Rh and ABO
incompatibility
Continues the physiological jaundice.
Hereditary spherocytosis
Minkowski -Chauffard disease
(anemia with sperocytes + fever)
Appears in intra/ extrahepatic atresy
Citomegaly
in prematures
a febrile jaundice
urine sediment with owl eye" cells
Table no. 10 Causes of indirect hyperbilirubinemia (Bi
I
>85% from Bi
T
)
Excess of production Decrease of Bi-clearance
Feto-maternal Rh/
AOB incompatibility
Errors of metabolism:
Crigler Najar jaudince
Dubin Johnson syndrome
Rotor-Schiff
Gilbert syndrome
Tyrosinosis
Galactosemia
Hereditary sperocytosis Prematurity
Hemolytic anemia
Hypothyroidism
Pituitary insufficiency
Breastfeeding at mothers with DM
Polycythemia Hepatic hypoperfusion
Extravasion/
swallowing of blood
Prematurity
Acceleration of entero-hepatic
circulation
Genetical factors
Inhibitors from breast milk (stopping
breastfeeding for 48 hours)
58
Table no. 11. Causes of direct hyperbilirubinemia (direct bilirubin over 15% from total
bilirubin)
Septicemia Intra-uterine infections- neonatal hepatitis
Coledocian cyst Obstructions of biliary ductus (tumors,
annular pancreas)
Trisomy 18 Galactosemia, thyrosynemia, methyoninemia
Cystic fibrosis Rotor-Schiff syndrome, Dubin Johnson
Sydrome of thickened bile Prolonged total parenteral nutrition
- Atresy of intra/ extrahepatic biliary
ways
Neonatal hemolytic disease is a feto-maternal Rh incompatibility (eritroblastosis) or ABO
incompatibility. The disease appears in the following situations:
- mother is Rh negative and child is Rh positive
- mother has O (I) blood group and child has A (II) or B (III) blood group
The fetus red cells produce antibodies in the mothers blood, which pass into the fetal
circulation and produce hemolysis.
Rh antigenes sensitize during the first pregnancy and in the second pregnancy the hemolysis
and the jaundice appear. More and more severe forms will appear. Sensitization can be
produced even by transfusions or abortions.
A and B antigens are widely spread in nature, that is why, isoimmunization is produced at the
first pregnancy, but it can appear also by heteroimmunization through infections, vaccines
The hemolytic disease in ABO system appears from the first pregnancy. It is more frequent,
but milder than the hemolytic disease in Rh system; it does not affect the intrauterine fetus; it
does not produce severe forms of jaundice at the moment of birth and prenatal diagnosis or
postnatal treatment are not necessary. In this form, mother has O (I) blood group and child
has A (II) or B (III) blood group. Natural agglutinins of those with group A (II) or B (III) are
IgM type, with heavy molecular weight, which do not pass the placenta. Agglutinins of those
with group O (I) - IgM type and IgG with small molecular weight, cross the placenta.
The physiopathological chain is: hemolysis - hyperbilirubinemia erythroblastosis (by
compensatory mechanism).
59
Clinical signs and symptoms: anemia, jaundice, hepatosplenomegaly, hemorrhagic
manifestations, neurological signs.
Clinical forms:
- Feto-placentary anasarca (fetal hydrops). The new born has: generalized edema, ascitis,
hepatosplenomegaly, paleness, cardiac failure, frequently: dead fetus.
- Hemolytic jaundice: jaundice present at birth: the newborn is apparently normal at birth,
with anemia, but Hgb exceeds 12 mg%, accentuated jaundice, hepatosplenomegaly,
localized edema, bilirubin values over 3-4 mg%.
- Hemolytic anemia: severe anemia at birth, newborn present low Apgar score, Hgb is less
than 12 mg%, bilirubin 3-4 mg%, hepatosplenomegaly.
Laboratory diagnosis
- blood group and Rh in parents and child
- titer of antibodies in pregnant women
- positive Coombs test: presence of antibodies in mothers serum
- blood test in the new born shows anemia, trombocytopenia
- leukocyte formula: erythroblasts > 25%, reticulocytes > 6%
- indirect bilirubin from umbilical cord > 4 mg%.
Prophylactic treatment
immunoprophilaxy anti-D (Ig specific)
- in Rh negative women: 300 g Ig anti-D in the first 72 h after abortion/ birth if the
new born is Rh positive;
- in female gender negative Rh new born from positive Rh mothers.
Curative treatment
In mild and medium forms: phototherapy and Phenobarbital 5-8 mg/day, 3-4 days
In severe forms:
- exanguinotransfusion with double volume (160 ml blood/kg, 85% of the blood
volume is changed)
- integral blood is used with Htc 40-45%, less than 48 h, group O (I) negative Rh or
isogroup with new born blood, but negative Rh
- immediately after phototherapy it is necessary to monitor bilirubin at 6h
- exanguinotransfusion is repeated if bilirubin increases above 1mg/h
- in hydrops or small weight - isovolumetric
- the blood is collected through umbilical artery and transfused through umbilical vein.
Types of jaundice- according to mechanism of production
60
- Hemolytic jaundice (prehepatic)
- Hepatic cellular jaundice
- Mechanical jaundice (posthepatic)
A. Hemolytic jaundice (prehepatic)
Signs and symptoms: yellow teguments and mucosa (flavinic jaundice), dark urine,
splenomegaly hepatomegaly, hemolysis
Laboratory: increased bilirubin
Treatment: phototherapy, exanguinotransfusion, Phenobarbital
B. Hepatocelular jaundice
Causes:
- septicemia - viral hepatitis
- herpetic disease - listeriosis
- congenital toxoplasmosis - intoxications (tetra, steroids)
- congenital enzymatic deficiencies (Crigler Naijar, Dubin Johnson, Rottor Schiff)
Features:
- yellow-orange teguments and mucosa - hepatomegaly without splenomegaly
- intensely colored urine - acholic feces
Laboratory:
- increased direct and indirect bilirubin
- increased transaminasis and sometimes aldolase, late.
Treatment: specific diets, antibiotics, corticosteroids (in neonatal hepatitis) unspecified
etiology.
C. Mechanic jaundice (posthepatic)
Causes:
- malformations of intra and extra hepatic biliary ways (atresia, agenezis)
- compression of intra and extra hepatic biliary ways (bracket, lymph nodes, tumors)
Features:
- onset: the 2
nd
week of life - verdinic progressive jaundice
- incresed direct bilirubin - hypercrome urine
- acholic feces - hepatomegaly
- positive hepatic samples
Treatment is surgical - in the first 4-8 weeks
- not faster, due to risk of colestasis syndrome
- not later, because biliary cirrhosis can appear
61
III. Nuclear jaundice (hyperbilirubinemic encephalopathy)
- bilirubin over 25 mg% in mature new born, 10 mg% in premature
- the consequence of toxic effect of indirect hyperbilirubinemia (unconjugated,
unbounded to albumin) on CNS
Clinical: jaundice + neurological symptoms (hypotonia, adinamia, difficult sucking,
hypertonia, opistotonus, seizures, apnea crisis)
- indirect bilirubin (unbounded) penetrates the hemato-encephalic barrier in the first 2-4
days of life and it fixes to the basal grey nuclei
- lethal or sublethal evolution (deficiency in CNS development)
Risk factors:
- hemolytical disease - prematurity
- acidosis - asphyxia
- hypoproteinemia - hypoglycemia
Evolution: severe, often death occurs
It can produce chronic encephalopaty:
- ataxia - athetosis
- deafness - mental deficieny
Treatment:
Phototherapy in risk of increasing bilirubin over bounding capacity of albumin; increased
bilirubin at dangerous levels: premature, extended bruisings, hemolytical disease
Blood transfusion indications:
- correct the severe anemia - prevent the nuclear jaundice
- septicemia - DIC
- severe metabolic imbalance
Exanguinotransfusion (ET): if mother has negative Rh, the following are determined in
the new born: blood test, blood group, Rh, bilirubin, Coombs test.
- ET is recommanded in the first hours after birth if:
the new born with jaundice, paleness, edema, hepatomegaly, bad general state
good general state, but Coombs test diectly positive, Hb < 11g% in mature new
borns, < 14g% in premature
bilirubin from umbilical cord > 4mg% and increasing with 0.5 g/h
bilirubin 25 mg% in new born at term without asphyxia or 20 mg% in new born at
term with asphyxia
62
bilirubin 18-20 mg% in premature new born without asphyxia or 15 mg% in
premature new born with asphyxia.
ET is repeated when bilirubin increases to values of neurological risk.
Blood transfusion will be done with:
- fresh blood (24h after collection) in suffering new borns
- irradiated blood if it got an intrauterine transfusion
- heparin blood
- gluco-citrate blood
HIV-AIDS INFECTION IN NEW-BORNS, NEONATES, AND CHILDREN
Acquired Immunodeficiency Syndrome (AIDS) is an infectious syndrome caused by the
human immunodeficiency virus (HIV) that attacks the body's immune system.
Immune depression caused by the virus favors the development of opportunistic infections.
Etiopathogeny
HIV belongs to the retroviruses class (RNA virus) which has an enzyme (reverse
transcriptase) that converts viral RNA into proviral DNA to be integrated into the host cell
genome.
Unlike other pathogenic viruses (influenza, polio, etc.) that damage cells, retroviruses only
transform them. When these cells will multiply, cellular genome-integrated provirus will
multiply simultaneously.
HIV infection is characterized by a continuous and active retroviral replication associated
with an intense renewal of infected cells (which invalidates the previous model regarding the
existence of a period of latency that would clinically correspond to the asymptomatic phase ).
HIV structure
(iantigenity)
p24
p18 gp
41
p17 gp
120
virus identification
ARN chain gp
160
(core)
Fig. no. 25. The HIV structure
63
The complex genetic structure provides HIV a tremendous genetic diversity. Analysis of
nucleotide sequences of HIV strains reveals extreme genetic variability, virtually there are
NO two similar strains, which is why a vaccine cannot be obtained.
The main targets of HIV are macrophages and T lymphocytes. HIV attaches to CD4 by
gp120 and enters the cell. The most important reservoir of these target cells are lymphoid
tissues, lymph nodes (which are the most important center of viral replication).
After primary infection, viral replication is very intense (p24 ATG): In the first month from 1
million-1 billion copies / ml and an increased number of infected lymphocytes. With the
second month the viral load decreases (up to about 9 months) by 100-1000 times (CD8
cytotoxic), decrease occurring before seroconversion and presence of neutralizing atb.
Without reduction in the viral load, as it happens in the case of malnutrition, tuberculosis and
in infants, development to AIDS is much faster.
In the next period (clinical latency / asymptomatic) viral load remains relatively constant
(infected CD4 lymphocites are replaced until the exhaustion of the regenerative capacity of
the immune system).
In the final stage of HIV infection (AIDS) there is again an increase in the viral load but with
a target cell depletion - 10-20% infected CD4 lymphocites.
It follows that in the early stages of HIV infection, the main factor that limits infection is the
immune system, and finally there is a depletion of target cells.
Natural evolution of HIV infection
Infection
Invading DISSEMINATION Invading of AIDS
regional lymphoid Destruction of
lymph nodes tissues lymph nodes
structure
5 years Invasion of
other organs
9-10 years
asymptomatic period (in 5% cases in
15 years)
Fig. Nr. 26. The evolution of HIV infection
64
Epidemiology
In Romania at the end of 2001 (WHO statistics) the number of HIV-positive was 6500 (2500
adults, 4000 children); in November 2002 -9000 cases. At the end of July 2007 - 15 000 HIV
positive people in Romania. The number of people receiving antiviral therapy - 6500 (70
pregnant women)
The source of infection. The source of infection is represented by infected humans, AIDS
being an infectious disease, not a contagious one. The virus does not resist at temperatures
above 60-64 degrees C or at ordinary disinfectants.
Transmission
- Inoculation of infected blood and blood products
- Sexually (sperm and the vaginal secretion)
Parent-child transmission can be:
- vertical transmission: HIV-positive mothers have HIV antibodies. These antibodies
cross the placenta, so the babies will be HIV positive. Antibodies persist 9-18 months.
Only 15-30% of viral antigens cross the placenta. Thus, in the absence of any intervention
70-85% of babies are protected, not being infected.
- transmission during birth / cesarean section: by inoculation of blood or vaginal
secretion
- transmission through breast milk is possible, therefore breastfeeding should be
prohibited in HIV mothers. The risk increases to 20-40% for naturally-fed children
(WHO recommends breastfeeding in developing countries where malnutrition is more
dangerous).
Responsiveness to infection. Although some cases meet the conditions for infection,
infection does not occur. It seems that individual genetic factors do not have a leading role,
rather the amount of viral load.
Symptoms, clinical diagnosis
If it is an intrauterine infection, the newborn presents growth retardation, brain anomalies
(most commonly microcephaly), and facial dysmorphism. The infected infant presents the
first symptoms within 3-6 months after birth: major signs or opportunistic or severe recurrent
infections. Major criteria (M) by WHO are: prolonged fever> 1 month, chronic diarrhea> 1
month, weight loss> 10%. Minor criteria are generalized lymphadenopathy (at least 2
regions), oropharyngeal candidiasis, persistent cough> 1 month, generalized dermatitis,
65
serologically confirmed maternal HIV infection. AIDS suspicion= 2M +2 m, in the absence
of other causes of immunosuppression: malnutrition, tuberculosis, tumors.
Laboratory diagnosis
ELISA Test detects Anti-HIV antibodies. It becomes positive at 6-8 weeks after infection.
To avoid false-positive reactions, testing is performed by two different ELISA techniques.
The test is not 100% specific
Western Blot test identifies viral antiproitein antibodies (antibodies directed against viral
envelope, gp120, gp160 and antibodies directed against p18, p24 cores)
Determination of viral antigens - antigens p24
Polymerase chain reaction-identification of the viral genome of blood lymphocytes
Immunity investigation: B lymphocites increase, decrease of T cells (<400/l shows a
severe defect of immunity), increased immunoglobulin.
Diagnosis of HIV infection in children perinatally exposed is through viral methods; HIV
serology can not be used as a diagnostic test due to the presence of maternal antibodies. In
our country it is recommended that HIV RNA testing should be done in children during the
first 2 days of life, on the 14th day, if the first test was negative; between month 1 and 2 of
life, to the 3rd and 6th month of life.
Etiologic treatment-(antiretroviral therapy)
Zidovudine (AZT, Retrovir) belongs to group A.
It is a nucleoside reverse transcriptase inhibitor, metabolised in the liver. The dose is
according to metabolization (extended in prematures). It produces anemia through medular
inhibition - hemoglobin is checked at birth and at 6 weeks.
Term newborn: 2 mg / kg every 6 hours
Prematures: 2 mg / kg every 12 hours, 2 mg / kg every 8 hours at 2 weeks of life and GA> 30
weeks, 2 mg / kg every 8 hours at 4 weeks and GA <30 weeks.
Lamivudine (3TC) belongs to group B
It has renal metabolization, the dose being proportional to glomerular filtration capacity
maturation in the newborn. It leads to lactic acidosis. Recommended dose: 2 mg / kg every 12
hours. There is recommendation to increase the dose at the age of 4 weeks to 4 mg / kg every
12 hours.
Nevirapine
It is non-nucleoside reverse transcriptase inhibitor with prolonged elimination time in the
newborn. The dose is 2 mg / kg in a single dose after birth, maintaining the plasma levels
increased up to day 7.
66
Schemes of neonatal ARV prophylaxis
Effective prophylaxis reduces the rate of maternal-fetal transmission of HIV to 1-2%. This
requires ARV prophylaxis in both mother and child, obstetrical interventions (scheduled
caesarean) artificial feeding of the child. Depending on the situation, management protocols
for the pregnant woman and the newborn have been employed.
In Romania, according to the Anti-AIDS Commission's recommendations, the interventions
designed to reduce the rate of maternal-fetal transmission of HIV are: artificial infant
feeding; initiation of antiretroviral therapy after the first 6 hours of life with AZT and 3TC
and its continuation for 6 weeks.
Zidovudine (AZT) administered during pregnancy, during labor and post-partum in mother-
child decreased vertical transmission from 25.5% to 8.3% in populations who are not
breastfeeding. At the parent-child pairs receiving combination therapy that included a
protease inhibitor (PI), the transmission rate fell to 0.1 - 1.3%. The protective role of cesarean
section was also demonstrated (intervention performed at 38 weeks of pregnancy).
1. Pregnant woman diagnosed with HIV infection during pregnancy with indication of
ARV therapy: newborns will not be breastfed; initiation of ARV therapy in the first 6
hours of life with AZT and 3TC and continued for 6 weeks.
2. Pregnant woman under antiretroviral therapy when pregnancy occurs: the newborn
will not be breastfed; ARV therapy is initiated in the first 6 hours of life with AZT
and 3TC and continued for six weeks; if the mother's ARV scheme was changed
because of virologic failure, the newborn will receive AZT, 3TC and NVP. If the
pregnant woman is under NVP treatment, the infant will receive the first dose of NVP
at 48-72 hours after birth, and then a daily dose of 2 mg / kg for 7 days followed by a
dose of 4 mg / kg up to 6 weeks; if the pregnant woman received NVP late during
delivery or 1-2 hours before delivery, the newborn will get a dose of 2 mg / kg
immediately after birth, and the next dose should be given after 24-72 hours.
3. Pregnant woman diagnosed with HIV infection in the eighth month of pregnancy: the
newborn baby will not be breastfed; ART therapy is initiated after the first 6 hours of
life with AZT, 3TC, NVP, the infant is considered at high risk of being HIV infected.
The duration of treatment is six weeks
Overall HIV Prevention aims to avoid blood, sperm and vaginal secretions and infected
maternal milk. Junkies, prostitutes (> 90% are infected) and newborns of infected mothers are
considered high-risk..
67
Family planning. HIV-positive mothers will be made aware that they can transmit the
infection to the newborn at a 15-30% rate (doctors will not make any "suggestion" only
mother decides to maintain the pregnancy).
Health education. It should be large, well coordinated at the governmental level. It will
include: recommendation to restrict partners, use of condoms (75% of HIV infections occur
through unprotected sexual intercourse); sterilization of needles and instruments for 30 min.
through boiling at 100 degrees C; burning of disposable syringes and needles in
crematoriums.
Mandatory preventive measures have been legislated in our country by testing: in partners,
prenuptially, in women in the first term of pregnancy (may decide to abort or be treated in the
last term of pregnancy), truck drivers and sailors , in persons working abroad for a period of
over 6 months.
Special measures in newborns
Protective measures at birth: disposable gown, gloves, mask, cap. Ball resuscitation and
suction system should be sterilized after each use, preferably they should be dedicated to
infants from HIV positive mother. Good resuscitation at birth lowers the risk of subsequent
need for laborious procedures of treatment, such infants should be treated as non-invasive as
possible. They can present any postnatal complications: hypoxia at birth, respiratory distress
syndrome, pulmonary hypertension, hypoglycemia.
Measures in the newborns section - isolation room (ideal rooming-in), use gloves to any
contact: changing diapers, suction of secretions; food. Vein puncture should be avoided as
much as possible given the risk of infection and the risk for the staff. Artificial nutrition
formula is recommended for mature infants; for prematures, special formulas (hypercaloric),
administered by continous or intermittent gavage, avoiding parenteral nutrition as much as
possible.
Communication with infectious diseases hospital
It is recommended that laboratory tests regarding existence of HIV infection should take
place in the infectious diseases clinics. The clinic should be informed about the existence of
HIV positive newborn form HIV positive mother; it should establish the ARV prophylaxis
and follow up the child after discharge.
Evolution, prognosis
Severe development invariably developing into AIDS and death.
The prognosis of life expectancy, as well as assessing the treatment effectiveness depends
mainly on the degree of the viral load.
68
References
1. Bopanna SB, Rivera LB, Fowler KB, et al. Intrauterine transmission of cytomegalovirus to infants of women with
preconceptual immunity. N Engl J Med 2001;344(18):1366-1371.
2. Cooper ER, Charurat M, Mofenson L, et al. Combination antiretroviral strategies for the treatment of pregnant HIV-1-
infected women and prevention of perinatal HIV-1 transmission. J Acquir Immune Defic Syndr 2002;29(5):484-494.
3. Benjamin DK, Stoll BJ, Fanaroff AA, et al. Neonatal candidiasis among extremely low birth weight infants: Risk
factors, mortality rates, and neurodevelopmental outcomes at 18 to 22 months. Pediatrics 2006;117(1):84-92.
4. Hyde TB, Hilger TM, Reingold A, et al. Trends in incidence and antimicrobial resistance of early-onset sepsis:
Population-based surveillance in San Francisco and Atlanta. Pediatrics 2002;110(4):690-695.
5. Kliegman RM., Stanton B, St. Geme J, Schor N, Behrman RE. Nelson Textbook of Pediatrics, 19th Edition, 2011
6. John P. Cloherty (Editor), Ann R., Md. Stark (Editor), Ann R. Stark (Editor). Manual of Neonatal Care. 6th Edition,
2008 Lippincott Williams & Wilkins
7. Boucher CA, Coll O, Hernandez M, et al. Vertical HIV-1 transmission correlates with a high maternal viral load at
delivery. J Acquir Immune Defic Syndr Human Retrovirol 1997;14:26-30.
8. Daffos F., Forestier F., Capella Pavloski M., et al. Prenatal management of 746 pregnancies at risk for congenital
toxoplasmosis. N Engl J Med 1988; 318: 271-275.
9. Newell ML. Mechanisms and timing of mother-to-child transmission of HIV-1. AIDS 1998;12:831-837
10. Newell ML, Gray G, Bryson YJ. Prevention of mother-to-child transmission of HIV-1 infection. AIDS 1997;11 (suppl
A): S165-172
11. Njenga S, Ombree JE, Ndinya-Achola, et al. Risk factors for postnatal mother-to-child transmission of HIV in Nairobi.
Conference on Global Strategies for Prevention of HIV Transmission from Mothers to Infants, September 1997,
Washington DC
69
CHAPTER II - RESPIRATORY PATHOLOGY
Conf. Dr. Oana Mrginean, ef lucr. Dr. Borka Balas Reka
UPPER AIRWAY INFECTIONS IN CHILDREN
ACUTE RHINOPHARYNGITIS
Definition: acute rhinopharyngitis (Rf) is an acute inflammation of the nasal and pharyngeal
mucosa, specific for infants and young children. (Up to the age of 2 years, upper airway
mucosa is immature and an inflammatory process at this level includes not only the throat
and nasal mucosa, but also the paranasal sinuses and the middle ear).
Etiology: can be viral or caused by mycoplasma. More common are mixoviruses (RSV -
respiratory syncytial virus - influenza, parainfluenza), adenoviruses, rhinoviruses and
enteroviruses (Coxsakie A and B).
Predisposing factors:
- Cold and damp, dry air, pollution
- Young age - under 2 years
- Rickets, anemia, malnutrition
Symptoms and diagnosis:
After a short incubation of 48-72 hours the onset is sudden, often with fever over 38 C,
malaise, capricious appetite and sleep disturbances.
During the acute phase the primary symptoms are nasal obstruction and rhinorrhea, leading
to difficulty in breathing and feeding. After a day of fever and nasal obstruction rhinorrhea
occurs, initially watery, than in 2-3 days becomes opalescent, viscous and sticky. (If the
secretion is purulent or with bloody streaks probably bacterial superinfection occurred).
Secretions can erode the skin or cause coughing and vomiting.
Physical examination: hyperemia of pillars, tonsils and oropharynx, sometimes, with
secretions on the posterior wall of the pharynx.
Laboratory diagnosis is not helpful for the diagnosis (in common practice viral cultures are
not performed).
Differential diagnosis:
- At the onset: with meningitis, especially when seizures occur in addition to fever, or
meningism is present.
70
- During acute phase: with rhinorrhea "a frigore", "secondary" rhinopharyngitis at the
onset of infectious diseases (measles, whooping cough, mumps, mononucleosis, etc.),
sinusitis, nasal foreign body and allergic rhinitis.
Complications:
- Adenoiditis, ethmoiditis, otomastoiditis
- Laringotraheobronchitis, bronchiolitis, pneumonia
- Albuminuria, hematuria
- Diarrhea, dehydration syndrome (due to fever, lack of intake and vomiting)
- Febrile seizures, meningoencephalitis
Healing occurs in 3-4 days (unless bacterial superinfection occurs).
Treatment:
Prophylactic treatment consists of:
- Judicious use of all factors of hardening the body
- Avoiding crowded places and contact with sick people
- Correct triage of children (and attendent) in the communities (nursery, kindergarten).
Curative treatment:
General measures:
- Well ventilated room with constant temperature (l8 -20 C), humidity (60%)
- Avoiding overheating but without giving up the air cure and daily bath
- In general normal feeding, with more liquids (water, soup, etc.). If feeding difficulty
occurs, fragmented or less frequent meals can be given (gavage is rarely necessary).
Symptomatic treatment:
Fever is treated with antipyretic agents, Paracetamol (Acetaminophen) 50 mg/kg/day PO
from 4 to 4 hours or 125 mg or 250 mg supp. as follows: less than 6 months - 3 x sup. 125
mg/day; 1-3 years - 3 x 1 sup. 125 mg/day; 3-7 years - 2-3 x 1 sup. 250 mg/day.
Nasal obstruction is treated with nasal decongestants and vasoconstrictors. For drainage of
watery secretions the child can be placed in ventral position for 15-20 minutes, especially
before meals. Saline intranasal solution are is used for decongestion followed by aspiration of
the secretion with a vacuum pump.
Topic vasocontrictor solutions: 0.5 % ephedrine or epinephrine 1:20000 (1f 1% epinephrine +
2 f saline solution) for 6 x 2-3 drops/day in each nostril (usually before meals and at
bedtime). Nasal decongestants such xylometazoline, oxymetazoline, phenylephrine are not
approved/suitable for children under the age of 2 years old.
71
Nafazolin (Rinofug) or oil and menthol containing products are not prescribed in infants and
small children. Silver containing disinfectants (0.5 % colargol or 0.5% argirol) can be used 2-
3 x 2-3 drops/day in serous rhinorrhea, but not more than 5 days (they can cause chemical
rhinitis). Skin erosions require protection with creams and ointments (Cutaden, Tetracycline
etc.).
Antibiotic treatment is necessary only if recovery did not occurred occur in 3-4 days (fever,
malaise amended). In preterm, malnourished and disabled (eg. cheilognatopalatoscizis)
infants antibiotic therapy will be introduced from the beginning of the treatment because
superinfection is a rule in these patients. The used antibiotics could be: Amoxicillin susp. 40
mg/kg/day p.o. in 4 doses or Ampicillin susp. 100-200 mg/kg/day PO. or IV. in 4 doses over
a period of 3-5 days. If the clinical evolution after 3-5 days of proper therapy is not favorable,
it is mandatory to carry out an otological examination, a chest x-ray and urinalysis.
ACUTE PHARYNGITIS (acute tonsillitis, acute angina)
Definition: Acute angina/Acute pharyngitis is an inflammatory process in the mucosa of the
pharynx and/or tonsils.
Etiology:
- the most frequent: viruses (adenoviruses, coronaviruses, enteroviruses, rhinoviruses, RSV
respiratory syncytial virus, Epstein-Barr virus - EBV, herpes viruses)
- Group A beta-hemolytic streptococcus (GABHS)
- other agents such as: Streptococcus Group C, Mycoplasma pneumoniae, fusobacterium
ACUTE STREPTOCOCCAL PHARYNGITIS
Epidemiology: Streptococcal pharyngitis produces 37 % of cases of acute pharyngitis in
children older than 5 years. It is uncommon before 2-3 years of age; it has a peak incidence in
the early school years, then it declines in teenagers. It is most common in winter and spring.
The spread of infection is during the acute phase. Symptoms disappear in 24 hours after
starting the antibiotic therapy.
Etiology: Group A beta -hemolytic streptococcus (GABHS)
Clinical manifestations (signs and symptoms)
The onset of streptococcal pharyngitis is rapid with "sore throat" (dysphagia ) and fever in
absence of cough. The incubation period is 2-5 days.
72
During acute phase, children present:
- intense erythema of the pharynx (soft palate, palatine tonsils, posterior pharyngx), the
tonsils are enlarged, covered with pus, false membranes, blood-tinged exudates, petechiae
of the soft palate, the uvula may be swollen and red.
- some patients may have headache, myalgia, malaise, depending on etiology
- some children may have scarlatiniform fever, with circumoral pallor, strawberry tongue,
fine maculopapular rash.
- often the anterior cervical lymphnodes are enlarged and painful.
Laboratory testing:
- throat culture, rapid diagnostic test (Rapid diagnostic test - RADT) for GABHS
(carbohydrate antigen test)
-
complete blood cell count, acute phase reactants
-
ASLO titer is not indicated because it will increase after healing.
Diagnosis
- The throat culture is an imperfect gold standard for diagnosis because false-positive
cultures can occur in children who are GABHS carriers of
- RADT test has a high specificity for GABHS, so if the rapid test is positive, throat culture
is not performed and antibiotic therapy is indicated. If the test is negative, the throat
culture should be done to confirm infection (false negative reactions may exist).
- C- reactive protein is positive if the infection is authentic.
The differential diagnosis includes other acute pharyngitis (with other streptococci,
diphtheria, anaerobs).
Complications of GABHS infection are suppurative and nonsuppurative.
-
suppurative complications (infection spread to underlying tissues): cervical
lymphadenitis, peritonsillar abscessus, retrofaringeal abscessus, otitis media, mastoiditis,
sinusitis.
-
nonsuppurative complications: acute rheumatic fever, Sydenham's chorea, reactive
arthritis, acute diffuse posstreptococcal glomerulonephritis
Treatment:
1. Antibiotic therapy: Although most streptococcal pharyngitis are resolved without
treatment, antibiotic therapy leads to the disappearance of symptoms in 12 to 24 hours after
initiation and prevents acute rheumatic fever.
Antibiotic treatment is recommended to be initiated immediately in:
- children with symptomatic streptococcal pharyngitis and positive RADT
73
- scarlet fever
- household contact with documented GABHS pharyngitis
- positive past personal history of rheumatic fever or recent history of rheumatic fever
of a family member.
Although multiple antimicrobial agents are effective in GABHS infection, most authors and
guidelines recommend initial treatment with penicillin. The most used antibiotics are:
-
Penicillin V (Phenoxymethylpenicilina): 250 mg/dose in children < 27 kg and 500
mg/dose for children > 27 kg in 2 or 3 divided doses for 10 days
-
Amoxicillin 50 mg/kg/day in 2 doses, max. 1 g/day 10 days
-
Benzathine penicillin (Moldamin): single dose of 600.000 IU i.m. in children < 27 kg
or under 12 years and 1.2 million IU in older children, provides adequate blood
concentration for 10 days
-
In case of penicillin allergy:
Erythromycin 20-40 mg/kg/day in 2-3-4 dose/day
Azytromicin 12 mg/kg/day 5 days (max 500 mg/day)
Clarithromycin 15 mg/kg/day in 2 doses/day, 10 days
Clindamycin 20 mg/kg/day in three doses/day, 10 days
Cefalorphorins as Cephalexin, Cephadroxil are indicated in case of resistance to
treatment with penicillin.
Follow up throat cultures are not recommended unless symptoms reappear.
Healthy carriers of GABHS involve little risk to their contacts. If necessary, streptococcal
carriers will be treated with clindamycin 20 mg/kg/day in 3 doses 10 days or Cefadroxil 30
mg/kg/day 10 days.
5
2. Symptomatic treatment
- antipyretic and analgesic treatment with Acetaminophen or Ibuprofen
- gargle with salty water, local anesthetic spray
- tablets containing benzocaine, menthol and phenol can relieve local pain.
3. Prophylactic treatment: multivalent streptococcal vaccine. Prophylactic antibiotic
treatment is recommended only to prevent recurrences of rheumatic fever.
Recurrent GABHS pharyngitis
Recurrent streptococcal pharyngitis appears in reinfection with GABHS from a family
member, or can be a sore throat due to another cause in a GABHS carrier. Diagnosis is
established by repeated throat cultures.
74
Treatment is performed with Clindamycin 20-30 mg/kg/day 10 days or
Amoxicillin/clavulanate 40-50 mg/kg/day 10 days or Cefuroxime 20 mg/kg/day PO for 10
days
Tonsillectomy is indicated in order to reduce the incidence of recurrent pharyngitis if the
child had more then seven episodes in the previous year or five in each of the preceding 2
years, in case of peritonsillar abscessus, hypertrophy of the tonsils with significant respiratory
distress, obstructive sleep apnea.
REFERENCES
1. Regoli M, Chiappini E, Bonsignori F, Galli L, de Martino M. Update on the management of acute pharyngitis in
children. Italian Journal of Pediatrics 2011,37:10. http://www.ijponline.net/content/37/1/10
2. http://www.refbooks.msf.org/MSF_Docs/En/Clinical_Guide/CG_en.pdf
3. Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, Martin JM, Van Beneden C. Clinical
Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis: 2012 Update by the
Infectious Diseases Society of America. Clinical Infectious Diseases Advance Access published September 9, 2012
4. Hayden GF, Turner RB. Cap. 373 Acute pharingitis In: Behrman R, Kliegman R, Nelson Waldo, et all eds. Nelson
Textbook of Pediatrics, XIXth ed., Philadelphia, W.B. Sauders Co., 2011
5. Man SC, Nanulescu MV. Pediatrie practic. Cluj Napoca, Risoprint 2006:70-82
ACUTE OTITIS AND OTOMASTOIDITIS
Definition - an inflammatory process of the lining of the middle ear, with a viral or bacterial
cause, which appears consequently, most of the time, after an upper respiratory tract
infection.
Terminology
Acute otitis media (AOM) or suppurative - refers to acute bacterial infection of the middle
ear
Otitis media with effusion (OME) or serous, secretory, or nonsuppurative refers to the fluid
in the uninfected middle ear. OME often precedes the development of AOM or appears
during the healing phase.
I. Epidemiology
Otitis media is the most common bacterial disease in children, with maximum incidence
between 1 and 2 years old children.
II. Etiology
a. Bacterial ( 2/3 of the cases)
- Streptococcus pneumonie (40% of all cases of bacterial otitis)
75
- Nontypeable Haemophilus influenzae (25-30% of cases of acute otitis media)
- Moraxella catarrhalis (in 10-15% of cases)
- Other germs: Streptococcus pyogenes group A, Staphylococcus aureus, Pseudomonas
aeruginosa, Enterobacter cloacae, Mycoplasma pneumonia, etc..
b. Viral: 5-15% of cases; respiratory syncytial virus, parainfluenzae viruses,
adenoviruses and Coxackie viruses
Risk factors with a role in the occurrence of AOM are:
- prematurity, low birth weight - low age
- early onset - positive family history
- abnormalities of the immune system - craniofacial malformations
- Race - Americans, Indigenous Australians Eskimos - allergies
- neuromuscular diseases - nurseries, agglomerations
IV. Clinical manifestations and diagnosis of various clinical forms
The disease usually occurs during the development of upper airway infection that lasts a few
days.
Thus, in the newborn, infant, symptoms are nonspecific, ear pain is manifested by irritability,
agitation, crying, food refusal, change of appetite and sleep; occasionally the child places his
hand on the ear or rubbs his head on the pillow. Sometimes general symptoms are associated:
vomiting, diarrhea or toxic condition, meningeal signs, seizures. The Vacher maneuver
(compression of the tragus) is painful, but the sign is only indicative.
In older children: fever, ear pain and hearing loss.
Ear pain without fever and hearing loss occurs in older children with otitis externa, or those
with dental abscess, temporomandibular joint disorders.
Any infant or young child with fever, without an obvious infectious outbreak, must be
examined for middle ear infection.
Clinical forms
1. Catarrhal otitis media (serous, congestive otitis) is the result of a physical process
secondary to the Eustachian tube obstruction and the negative pressure of the middle ear
which is objectified by the existence of a serous and sterile transudate in the middle ear.
Usually, obstructive catarrh is the result of the inflammation of the rhinopharynx.
The catarrh produces a sensation of pressure in the ear, hearing loss and noise (crackling) in
the ear during swallowing (deglutition) or jaw movements. The baby is agitated because of
the earache. He has a sensation of fullness, pressure in the ear. The existence of the third
relapse within a period of 6 months defines recurrent otitis.
76
2. Suppurative otitis media. The main symptom is otalgia: it is violent, throbbing and
exacerbated by swallowing. The child puts his hand to his ear and screams, places the
affected ear on the pillow, because the heat of the pillow soothes the pain. Deafness, ear noise
and general symptoms may appear, such as: high fever, malaise, vomiting, diarrhea and
sometimes meningism, seizures.
Together with eardrum perforation, the pain diminishes and the fever drops, otorrhea
occuring as the main symptom (which initially is bloody, and then becomes purulent). Often,
it is confused with the resulting liquid after washing the ear. Otoscopic examination reveals
the changes of the eardrum (edematous) or highlights perforation, and tympanometry shows
the immobility of the eardrum. Tympanocentesis performed in newborns in severe forms,
those that do not respond to antibiotic treatment, confirms the diagnosis even in complicated
forms. Typically, there is a hyperleukocytosis
3. Otomastoiditis in infants. Different anatomical conformation and special reactivity of the
infants ear cause, at this particular age, the affection of the entire otomastoidian apparatus
simultaneously, and repercussions on the body are more severe.
Otomastoiditis in infants has two forms:
The manifest form occurs in eutrophic infants who have not previously been treated with
antibiotics.
Onset is sudden with high fever, ear symptoms and general intense symptoms (agitation,
sometimes seizures), meningism, diarrhea, vomiting. After eardrum perforation, symptoms
fail and often healing may be spontaneous. Sometimes symptoms do not yield, which
indicates the existence of an antritis which continues to evolve.
Latent otomastoiditis (latent otitis, latent antritis) mostly occurs in malnourished, premature
children with immune deficiencies and other disabilities, or in eutrophics undergoing
inappropriate antibiotic treatment which could not heal them, only masked the symptoms.
The onset is insidious, about 2-3 weeks after a nasopharyngeal infection; presenting with the
symptoms of a general illness: fever (some without fever), toxic facies, pallor, malaise,
agitation or sleepiness, torpor, diarrhea, vomiting and signs of dehydration. This neuro-toxic
syndrome with nervous, digestive and dehydration symptoms contrasts with the few objective
symptoms of otitis (they must be "sought" carefully and repeatedly).
4. Subacute and chronic otitis media. The persistence of negative pressure and sterile
transudation after acute otitis media for a period of 4-8 weeks defines subacute otitis. The
persistence of these conditions over 8 week define chronic otitis.
77
Diagnosis is made by ENT (ORL) examination which at the otoscopic examination shows
thickened, immobile tympanic membrane and indicates the presence of fluid in the middle the
ear. Tympanometry always shows the involvement of the eardrum mobility. In children over
3 years old audiometry can be tried, which highlights hearing loss. Extension of Eustachian
tube dysfunction can lead to the formation of a cholesteatoma.
V. Accurate diagnosis is determined by ENT examination
Investigations
1. Otoscopy: the eardrum intensely congested, eardrum which bulges, sometimes opaque or
perforated, with pus; luminous reflection of the eardrum- diminished or absent
2. Tympanometry: to confirm the diagnosis in some cases
- to follow the development of acute otitis media (facilitates the differentiation between the
quickly and completely healed OMA from OM in which the exudate persists, even
asymptomatically, situation in which the patient must be re-examined)
VI. The differential diagnosis of otitis is done with:
- acute nasopharyngitis, acute adenoiditis, meningo-encephalitis;
- dental pain, temporomandibular joint disorder, ear trauma
Complications: can be classified as:
Intratemporal: tympanic membrane perforation, facial nerve paralysis, acute labyrinthitis,
mastoiditis, chronic otitis media, cholesteatoma, otomastoiditis, chronic suppurative otitis
media, etc.
Intracranial: Meningitis, encephalitis, brain abscess, subdural or supradural abscess,
thrombosis or thrombophlebitis of lateral and sigmoid sinus, hydrocephalus
Systemic: Bacteremia/ septicemia, septic arthritis, parenteral diarrhea
Treatment of otitis
a. In catarrhal otitis media pain painkillers may be recommended (Paracetamol; Ibuprofem),
but not chemotherapy or antibiotics (do not have any proven effect).
b. In suppurative otitis media Amoxicillin is the first choice if the patient received no
Amoxicillin in the last 30 days, if he does not simultaneously associate purulent
conjunctivitis and he is not allergic to penicillin.
In children who received Amoxicillin treatment in the last 30 days, or in which H influenzae
and M catarrahalis B lactamazo + has to be treated, a treatment with Amoxicillin/ clavulanate
will be initiated.
As an alternative: Cefuroxime, Ceftriaxone can be used as well (table 10).
78
Table 10. Antibiotic treatment of AOM with antibiotics in patients with initial treatment
with antibiotics or who evolved unfavorably with symptomatic treatment only during the
first 48-72 hours
Fever > 39C and / or severe ear pain
NO YES
At diagnosis for patients
initially treated with ATB
Amoxicillin 80-90 mg/ kg/
day
Amoxicillin-clavulanate: 90
mg/ kg/ day (amoxicillin)
with 6.4 mg/ kg/ day of
clavulanate
Penicillin allergy: Cefdinir,
cefuroxime, cefpodoxime,
azithromycin, clarithromycin
Penicillin allergy:
Ceftriaxone for 3 days
Unfavorable outcome of
patients only after 48-72
hours of observation
Amoxicillin Amoxicillin-clavulanate
Penicillin allergy: Cefdinir,
cefuroxime, cefpodoxime,
azithromycin, clarithromycin
Penicillin allergy:
Ceftriaxone 1 or 3 days
Unfavorable outcome after
48-72 hours in patients with
initial antibiotic treatment
Amoxicillin Amoxicillin-clavulanat
Penicillin allergy:
Ceftriaxone Ceftriaxone for 3
days; Clindamycin
cephalosporin type 3
Penicillin allergy:
In case of failure at the
second antibiotic:
Clindamycin + cephalosporin
type 3
tympanocentesis
ENT re -evaluation
New data show that approximately 83-87% of S. pneumonia isolates are susceptible to 80-90
mg/kg/zi doses of Amoxicillin.
In case of poor outcome under treatment with Amoxicillin tympanocentesis, ENT re-
examination and initiation of treatment with Clindamycin will be indicated in order to have
an effect on nontypeable h influenzae and M catarrhalis, such as: Cefdinir, cefixime or
cefuroxime. In proven cases of multidrug-resistant S pneumonia (serotype 19A) including
Clindaicina levofloxacin or linezolid may be used.
Duration of treatment
79
- In children <2 years old and those with severe symptoms: 10 days
- Children 2-5 years old with mild / moderate symptoms of AOM: 7 days
- Children > 6 years old with mild / moderate symptoms of AOM: 5-7 days
3. In otomastoiditis in infants the germs which are frequently incriminated are: S pneumonia
and nontypeable H influenzae; while Pseudomonas aeruginosa occurs more frequently in
cases of chronic suppurative otitis media. Broad spectrum iv antibiotic treatment will be
initiated and mastoidectomy will be performed. Depending on the outcome of cultures
antibiotic treatment is continued (preferably "aimed") for 10 days.
4. In subacute and chronic otitis media middle ear ventilation is tried to be improved by
teaching the child to practice the Valsalva's maneuver or a balloon inflation (decongestants,
antihistamines and adenoidectomy have not proved to be effective).
The presence of secretions in the middle ear for more than 12 weeks shows timpanotomia,
with the insertion of a ventilation tube (especially if hearing is affected).
Prophylaxis: The prevention of otitis is complex, characterized by teaching the child to blow
his nose (only one nostril at a time), treating rhino pharyngeal infections correctly and
fighting against multiple factors favoring otitis, vaccination against Streptococcus
pneumoniae and H. influenzae, two of the most common germs involved in the occurrence of
otitis
Bibliography:
1. Muntean I., Mrginean O. Infecii ale cilor respiratorii superioare n Pediatria Tratat, sub redacia Eugen Ciofu i
Carmen Ciofu, ediia 1, Ed Medical, 2001 , 206-220 (Upper respiratory tract infections in Tediatrics Treaty,
edited by Eugen Ciofu i Carmen Ciofu, 1 edition, Medical Publishing, 2001 , 206-220)
2. Ciofu E, Ciofu C. Penumologie n Esenialul n pediatrie, ediia a 2-a, Ed Medical Amaltea 2002, 166-256
(Pneumology in The Essential in Pediatrics)
3. Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, et al. The diagnosis and
management of acute otitis media. Pediatrics. 2013 Mar;131(3):e964-99. doi: 10.1542/peds.2012-3488. Epub 2013 Feb
25
4. Kerschner JE. Otitis media in Nelson Textbook of Pediatrics, 19
th
Edition, Ed Sunders Elsevier, 2007, chapter 632,
2199-2213
5. Falup-Pecurariu O, Bleotu L, Zavarache C, Peled N, Anton O, Robu M, et al. Streptococcus pneumoniae
nasopharyngeal colonization in children in Brasov, Central Romania: high antibiotic resistance and coverage by
conjugate vaccines. Pediatr Infect Dis J. 2011 Jan;30(1):76-8. doi: 10.1097/INF.0b013e3181f42bb6.
6. Falup-Pecurariu O, Leibovitz E, Mercas A, Bleotu L, Zavarache C, Porat N, et al. Pneumococcal acute otitis
media in infants and children in central Romania, 2009-2011: microbiological characteristics and potential coverage by
pneumococcal conjugate vaccines. Int J Infect Dis. 2013 Mar 19. pii: S1201-9712(13)00082-9. doi:
10.1016/j.ijid.2013.02.002.
80
7. Leibovitz E, Piglansky L, Raiz S, Press J, Leiberman A, Dagan R. Bacteriologic and clinical efficacy of one day vs.
three day intramuscular ceftriaxone for treatment of nonresponsive acute otitis media in children. Pediatr Infect Dis J.
2000 Nov;19(11):1040-5.
ACUTE LARYNGITIS
Definition: Acute laryngitis is a viral or bacterial infection of the laryngeal mucosa which
can cause distress and / or respiratory failure by laryngeal obstruction.
Classification:
- without respiratory distress - simple acute laryngitis
- with respiratory distress (obstructive laryngitis):
acute spasmodic laryngitis (stridulous),
edematous acute laryngitis: subglottis (acute laryngotreheobronchitis),
supraglottic (epiglottitis)
Epidemiology: age of occurrence of acute laryngitis, especially children between 3 months
to 5 years, with a peak at the age of 2.
Etiology
The etiology of most viral laryngitis is of viral origin: influenza viruses, parainfluenza,
adenovirus, respiratory syncytial virus (RSV), measles virus.
Bacterial etiology is rare and is represented by Haemophilus influenzae (common in the past
in epiglottis, rarely now after HiB vaccine introduction), Streptococcus pyogenes,
Streptococcus pneumoniae, Staphylococus aureus.
2,5,10
Clinical forms
I. Simple acute laryngitis (mild clinical form)
Etiology: viral.
Clinical manifestations:
Onset is by acute upper respiratory tract infection (AURTI) with dysphagia, hoarseness,
cough; dyspnea and stridor are missing or are very discrete.
On examination there was only a pharyngeal inflammation, and laryngoscopy may reveal
swelling of the vocal cords and subglottis tissue.
The evolution is benign.
II. Obstructive laryngitis
They are clinically characterized by:
- acute inspiratory stridor - barking cough or with a metallic sound;
81
- dysphonia (hoarseness) - inspiratory dyspnoea;
- suprasternal and supraclavicular drafts
II.1. Stridulous laryngitis or spasmodic croup (pseudocroup)
Etiology: virus in some cases, but allergic and psychological factors play an important role,
the pathogenesis is uncertain.
Occurance: age 1-3 years, children with paratrophy or adenoids.
The viral prodrome may be present (acute nasopharyngitis, acute tracheobronchitis).
Clinical manifestations:
The onset is acute, it usually occurs at night, and is preceded by a crisis and hoarseness.
Children will suddenly wake up from sleep and present hoarseness, cough, breathlessness,
respiratory distress, anxiety. The severity of the symptoms is reduced in a few hours. The
child may present some attacks, which will become lighter in the next 1-2 days.
Spasmodic croup treatment is done at home.
Although in the past it was thought that placing the child in the cold night air would improve
spasmodic croup, a Cochrane review has not shown its benefits, on the contrary, the croup
and wheezing worsen in the cold night air.
If the child is in hospital, a nebuliser will be made with racemic epinephrine.
10
II.2. The croup (Edematous subglottis acute laryngitis, acute laryngotracheobronchitis)
Acute laryngotracheobronchitis is an acute inflammatory process where the edema includes
subglottis regions.
Etiology: viral.
Occurance: children aged between 6 months - 3 years.
Clinical manifestations:
The Prodrome is by AURTI with running nose, sore throat, cough, not very high fever by 1-3
days before the onset of obstructive symptoms.
Symptoms of laryngitis are installed progressively, respiratory distress manifesting in 2-3
days. The child has: barking cough, hoarseness, inspiratory stridor, suprasternal and
supraclavicular draft, fever (39-40 C). Symptoms worsen at night, fade in a few days and the
82
child cures in a week. Children prefer to stay in bed or slightly raised, they are nervous. Their
general condition is quite good.
Physical examination shows hoarse voice, coryza, inflammation of the throat, mild
tachypnea, rarely nasal wings beat, suprasternal, infrasternal drafts and rib retractions,
continuous stridor hypoxia, cyanosis, pallor. Sometimes severe laryngotracheobronchitis
hardly differs from epiglottis, the latter having an acute onset and a more rapid development.
Paraclinical investigations:
Latero-cervical radiography - indicates narrowing subglottis, labeled "Gothic tower" (the
previous posterior view).
The differential diagnosis of laryngotracheobronchitis is done with: diphtheria, foreign body,
retropharyngeal abscess, angioedema, asthma attack, laryngospasm of tetany, trauma, tumors
or malformations of the larynx, measles and whooping cough.
Complications: otitis media, bronchiolitis, pneumonia, and even more rarely pneumothorax
and mediastinal or subcutaneous emphysema, bacterial tracheitis and toxic shock.
Treatment
a). Most forms of croup are mild so they can be treated at home where a humid atmosphere in
a clean, well-ventilated room is assured
b). In other forms the childs admission to hospital is ensured and a treatment is given, which
includes:
- ensuring a humid atmosphere and hydration of the child, and, if necessary, even the
administration of O
2
;
2
- aerosol with classic racemic epinephrine dose: 0,25-0,5 ml racemic epinephrine solution
2,25% - 0,5 ml in 3 ml of normal saline solution, may be repeated every 20 minutes. The
effect of racemic epinephrine is less than 2 hours. Administration of corticosteroids reduces
laryngeal mucosal edema, having an anti-inflammatory effect. Dexamethasone may be
administered IM dose 0.3-0.6 mg/kg/24 hours. Prednisone 2-4 mg/ kg/ hour can be
administered as well;
- intubation, for 2-3 days, may be needed in severe forms of respiratory failure; after
extubation, the child will be observed 1-2 days;
- no antibiotics are administered;
- admission to hospital is recommended in case of progressive stridor, stridor at rest,
espiratory distress, hypoxia, cyanosis, impaired consciousness;
83
- racemic adrenaline and Dexamethasone 0.5 mg / kg / dose every 6 hours are useful in the
treatment of croup associated with extubation.
-
II.3. EPIGLOTTITIS (supraglottitis)
Epiglottitis referred to as supraglottitis, is an inflammatory, acute edema of the epiglottis and
hypo-pharynx. Basically, it is a rapidly progressive bacterial cell, that comprises the region
above the vocal cords, leading to the total obstruction of the airways (this is why it is
considered a medical emergency!).
Etiology. Haemophilus influenzae type B. It is rare, it occurs at any age and it is more
common between the ages of 1-6.
Clinical manifestations:
Onset is sudden, with fever, wheezing, sore throat (dysphagia), shortness of breath, with the
rapid occurance of respiratory obstruction.
The symptomatic progression is so fast, that in a few hours the patient becomes toxic, and
shows difficulties in swallowing and breathing.
During the onset period the child has high fever, malaise (lethargy) and a toxic appearance.
The baby's head is in hyperextension (without any signs of meningeal irritation), and the
child is leaning on his hands with the neck extended and his mouth open while his tongue is
out (the tripod position). He may present inspiratory stridor (spiratory dyspnea with rough,
noisy breathing), associated with more pronounced forms of obstruction, with over- and
substernal draft, supra clavicular and intercostal), cough or hoarseness (hoarseness, muffled
voice; it seems that "it comes from far away), dysphagia and agitation. Due to the
obstruction, on auscultation, the vesicular murmur is diminished.
Diagnosis: Local examination of the pharynx with the laryngoscope shows a red edematous
epiglottis on the base of the tongue, impaired vocal cord. Examination with a spatula,
laryngoscopy will be performed in a specialized service, because at the hypoxic child,
manipulation in the pharynx, including the use of a tongue depressor can produce a vagal
reflex with possible cardiac arrest.
Paraclinical investigations:
Throat radiography, in lateral incidence, well delimits the epiglottis and the aretino
epiglottis areas (thumb sign). The examination will be performed in appropriate conditions,
84
with the necessary equipment to perform the required intubation or tracheostomy. Intubation
is maintained for 2-3 days until the disease responds to the antibiotic treatment.
Laboratory investigation shows a leukocytosis of 15-25000/mm
3
, with a marked neutrophilia.
Bacteremia is present in over 90% of cases.
Complications: pneumonia, cervical lymphadenitis, otitis media, meningitis, septic arthritis,
mediastinal emphysema and pneumothorax (after tracheotomy)
Differential diagnosis:
1. Bacterial tracheitis determined by Staphylococcus aureus, Moraxella catarrhalis,
Corinebacterium diphtheriae, H. influenzae or anaerobic is the most important condition with
which the differential diagnosis is made as it has an increased risk of acute airway
obstruction. It requires tracheostomy, intubation and antibiotic treatment (Vancomycin,
Naficilin, Oxacillin, etc.), plus oxygentherapy.
2. Foreign body aspiration that occurs in young children and is manifested by attacks of
choking, coughing, diaphragm balance.
3. Retrofaringean or peritonsillar abscess can mimic respiratory obstruction.
4. Extrinsic compressions on the airways given by a vascular ring or intrinsic (faryngeal
papilloma, subglottic hemangioma).
5. Angioedema after anaphylactic reactions, edema after oro-tracheal intubation, tetany,
infectious mononucleosis.
Treatment of epiglottitis
Epiglottitis is a medical emergency and the child should be admitted to the intensive care
unit.
1). It is advisable that in severe cases the initial treatment include nasal tracheal
intubation to prevent sudden death. Extubation is done after a few days. Intubation in
epiglottitis has greatly reduced mortality, to nearly zero. Intubation is done in an intensive
care unit.
2). Racemic adrenaline and corticosteroids are ineffective.
3). The antibiotic therapy is aimed for H. influenzae and consists of the administration of
Ceftriaxone 100 mg / kg / day in 2 IM / IV doses, Cefotaxime or Meropenem according to the
antibiogram results from cultures as 10-40% of H. influenzae strains are resistant to
Ampicillin. Antibiotic treatment should be continued for 7-10 days after extubation of the
patient.
85
You can also use Ampicillin 200 mg/ kg/ day iv administered in 3-4 doses, or Amoxicillin
100 mg/ kg/ day in 2-3 doses, orally, for 5 days.
4). Prophylaxis with H. influenzae is made to all family members if the sick child is under 4
years old and he is immunized incompletely or he is under 1 year old and did not receive the
primary vaccination or immunocompromised. Prophylaxis is done with Rifampicin 20 mg/ kg
orally in a single dose for 4 days.
Bibliography
6. Regoli M, Chiappini E, Bonsignori F, Galli L, de Martino M. Update on the management of acute pharyngitis in
children. Italian Journal of Pediatrics 2011,37:10. http://www.ijponline.net/content/37/1/10
7. http://www.refbooks.msf.org/MSF_Docs/En/Clinical_Guide/CG_en.pdf
8. Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, Martin JM, Van Beneden C. Clinical
Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis: 2012 Update by the
Infectious Diseases Society of America. Clinical Infectious Diseases Advance Access published September 9, 2012
9. Hayden GF, Turner RB. Cap. 373 Acute pharingitis In: Behrman R, Kliegman R, Nelson Waldo, et all eds. Nelson
Textbook of Pediatrics, XIXth ed., Philadelphia, W.B. Sauders Co., 2011
10. Man SC, Nanulescu MV. Pediatrie practic. Cluj Napoca, Risoprint 2006:70-82
11. Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the
emergency room. Med Decis Making. 1981;1(3):239-46.
12. McIsaac WJ, White D, Tannenbaum D, Low DE: A clinical score to reduce unnecessary antibiotic use in patients
with sore throat. CMAJ 1998,158(1):75-83.
13. Muntean I., Mrginean O. Infecii ale cilor respiratorii superioare n Pediatria Tratat, sub redacia Eugen Ciofu i
Carmen Ciofu, ediia 1, Ed Medical, 2001 , 206-220
14. Sun J, Keh-Gong W, Hwang B. Evaluation of the etiologic agents for acute suppurative tonsillitis in children.
Zhonghua Yi Xue Za Zhi (Taipei). 2002;65(5):212-7.
15. Roosevelt GE. Infections Upper Airway. In: Behrman R, Kliegman R, Nelson Waldo, et all eds. Nelson Textbook of
Pediatrics, XIXth ed., Philadelphia, W.B. Sauders Co., 2011
16. Sittel Ch, Koitschev A. Erkrankungen des HNO-Bereichs. In Gortner L, Meyer S, Sitzmann FC. Padiatrie, 4 Auflage,
Dual Reihe 2012:816-18
17. Moore M, Little P. Withdrawn: Humidified air inhalation for treating croup. Cochrane Database Syst Rev. 2011 Jun
15;(6):CD002870. doi: 10.1002/14651858.CD002870.pub3.
ACUTE BRONCHIOLITIS (AB)
Definition: Acute bronchiolitis is a severe inflammation of bronchioles usually due to a viral
infection leading to bronchiolar obstruction.
86
Etiology: is viral. The most frequently incriminated is the respiratory syncytial virus (RSV -
up to 80 % of the cases), followed by parainfluenza virus (type 1,3), metapneumovirus, adeno
- and rhinovirus.
Epidemiology: AB occurs most frequently in infants and small children under 2 years of age,
in the cold season (October - March), in small epidemics, more often in boys and in infants of
those young mothers who smoked during pregnancy.
Clinical manifestations:
Symptoms: After a prodrome of 1-2 days with clear rhinorrhea and sneezing, wheezing occurs
with a paroxysmal dry cough, dyspnea, perioral cyanosis and of extremities, tachypnea,
agitation or drowsiness and anorexia. Fever may range from feverish to high fever (38-40C).
Physical examination is dominated by wheezing, nasal flaring, retraction at the suprasternal
notch, supraclavicular and intercostal spaces, hyperresonant percussion, prolongation of the
expiratory phase of the breathing, fine crackles. Decreased intensity breath sounds suggest an
imminent acute respiratory failure due to nearly complete bronchiolar obstruction.
Patients may have feeding difficulties and some of them could have neurotoxic syndrome
(diarrhea, vomiting, flatulence, lethargy).
Chest X-ray shows pulmonary hyperinflation manifested by:
- increased anteroposterior diameter of the chest
- descent of the diaphragm
- hyperexpansion of lungs
In some cases atelectatic areas can be identified.
Diagnosis of AB: is clinical. In an apparently healthy infant a first episode of wheezing
appears in the context of viral infection.
Laboratory findings:
- Pulseoximetry - to determine the severity degree
- ASTRUP - in case of acute respiratory failure to determine an uncompensated
respiratory acidosis
- Complete blood count: initially may show slight leukopenia or normal leucocyte
value. In case of bacterial superinfection leukocytosis with high neutrophil count will
occur.
- For etiologic diagnosis viral culture may be done from the nasal secretion.
Differential Diagnosis:
- Pneumonia (viral and bacterial)
- Gastro-esophageal Reflux Disease
87
- Asthma bronchiale
- Foreign body aspiration
- Cystic fibrosis
- Whooping Cough
Complications: Acute dehydration, acute respiratory failure, otitis media, pneumonia,
recurrent wheezing episodes (occurs in of patients admitted in the first 2 years of life).
Evolution: In eutrophic children is good. It is reserved in preterm and those with cardiac
malformation, which typically presents complications. Usually AB improves obviously in the
first 3-4 days and heals in 7-10 days. The cough may last up to 3 weeks.
Treatment:
- Adequate hydration (in those with acute respiratory failure oral liquids are
countraindicated)
- Oxygen (in the hospital, if necessary)
- Bronchodilators (unproven effect) - salbutamol 15 mg/kg/dose every 20 minutes, 3 to
4 doses
- Adrenaline: nebulization through mask, 0.3-0.5 ml/kg/dose (1mg/ml adrenaline sol.
with 2-3 ml of saline solution) 2-3 doses, every 20 minutes
- Corticosteroids (controversial efficacy): used in case of neuro-toxic syndrome
- Antibiotics - should not be used routinely, are given in case of bacterial infection
(fever > 38.5C for 3 days). Amoxicillin/clavulanate or a cephalosporin is preferred.
- Ribavirin is active on RSV. (Aerosols are recommended for children at high risk, such
as premature infants, and with malformations).
Admission is required if:
- Infant under 6 weeks of age
- Presence of risk factors (prematurity, congenital heart defects, immunosuppression)
- Tachypnea > 60/min
- Progressive worsening with apnea attacks
- O2 saturation < 92 %
Prophylaxis: RSV is contagious. Specific anti - RSV immunoglobulins are administered I.V.
in infants under 6 months of age, premature or with multiple diseases. Hospitalized patients
will be isolated because they spread RSV (even for 1-3 weeks after cure).
88
PNEUMONIA
Definition: pneumonia is an acute inflammation of the parenchyma of the lungs (at alvelolar,
interstitial and sometimes simultaneous bronchial level) caused by bacterial, viral, fungal or
parasitic infections, chemical or physical causes (radiation, barotrauma).
Classification of pneumonia:
- Community-acquired pneumonia
- Pneumonia in immunocompromised patients
- Pneumonia - nosocomial infection
Etiology is depend on age (table 11):
Table 11. Ethiology of Pneumonia
AGE PATHOGENS COMMONLY INVOLVED
Neonates Group B Streptococci, Gram negativ bacilli
2 months - 5 years Viruses, Haemophilus influenzae, Streptococcus pneumoniae
2 months - 5 years Staphylococcus aureus/epidermidis, Enterobacteriaceae
5 - 10 years Viruses, Streptococcus pneumoniae
Over 10 years
Viruses, Mycoplasma pneumoniae, Chlamydia pneumoniae;
Streptococcus pneumoniae, Haemophilus influenzae
PNEUMOCOCCAL PNEUMONIA
Streptococcus pneumoniae (Pneumococcus) can be involved in 13-28 % of pneumonia in
children.
Pneumococcal pneumonia recognizes three main clinical and radiological forms according
classic semiology: lobar pneumonia, segmental pneumonia and lobular pneumonia
(bronchopneumonia), the latter tends to be abandoned in the current terminology of lower
respiratory airway infections.
89
A. LOBULAR PNEUMONIA (BRONCHOPNEUMONIA) is the most frequent in infants
and toddlers under 2 years. It is characterized by a bronchoalveolitis of the lung lobe
associated with bronchitis (purulent exudate in the bronchi).
Etiology:
- Determining factor is the pneumococcus (Streptococcus pneumoniae).
- Contributing factors are represented by age and deficit of anti-infective defense
mechanisms of the body (prematurity, dystrophy, rickets, anemia, cleft palate, cystic
fibrosis), immunological dysfunction, infectious diseases (measles, whooping cough,
influenza), unbalanced diet and chronic diseases (heart failure, chronic obstructive
pulmonary disease, diabetes mellitus, etc.).
Clinical manifestations and diagnosis:
Onset: More often is slow, insidious, preceded by several days of symptoms of an upper
respiratory tract infection with rhinorrhea, fever, fatigue or cyanosis during feeding,
tachypnea, cough, possibly vomiting, agitation or drowsiness. Rarely, the onset may be
sudden, with fever of 39-40 C, respiratory distress, sometimes febrile seizures or
meningism.
Later on the course of the illness occur following syndromes:
- Respiratory distress syndrome
- Cardiovascular syndrome
- Toxico-septic syndrome
a. Respiratory distress syndrome includes:
- Tachypnea - is the most consistent clinical sign, expiratory dyspnea, moan
- Inter - and subcostal retractions, nasal flaring
- Cough - initially dry afterwards wet
- Cyanosis - initially perioral later generalized
Physical findings: dullness on percussion and fine crackles exacerbated by coughing and
crying on auscultation. There may have bronchophony and/or tubal respiration.
b. Cardiovascular syndrome occurs in extensive forms due to:
- Direct action of microorganisms or toxins on the myocardium and vessels
- As a consequence of anoxia, hypercapnia and acidosis
It is characterized by: tachypnea, tachycardia, hepatomegaly, edema, cyanosis and
collapse.
90
c. Toxico-septic syndrome is characterized by fever (most common septic type), pallor,
drowsiness, dizziness or agitation, seizures, flatulence, vomiting and diarrhea, sometimes
kidney irrigation impairment (oliguria, albuminuria, hematuria).
Clinical forms:
Majority of clinical forms occurs only with respiratory signs; there are also "silent" forms
which are accidentally discovered on radiologic exam; and also superacute forms. There are
two particular clinical types:
- One, that mimics acute surgical abdomen due to paralytic ileus with abdominal pain,
vomiting, anorexia and flatulence
- One, pseudomeningeal form with headache, vomiting and signs of meningeal
irritation (which usually requires lumbar puncture).
Diagnosis is based on clinical symptoms (fever, chills, tachypnea, wet cough), radiological
examination (pulmonary consolidation) and laboratory findings (leukocytosis with
predominance of neutrophils, elevated CRP, accelerated ESR).
a. Chest radiography indicates the following forms:
- Paravertebral form (paravertebral opacities) more common in premature, newborn and
dystrophic infants
- Disseminated macronodular
- Disseminated micronodular
- Hilio - basal form
- Pseudo - lobar or segmental form, which can simulate lobar pneumonia
b. Laboratory findings:
- Leukocytosis with elevated neutrophil count
- Positive acute phase reactants: accelerated ESR, positive CRP (> 60 mg/l), high
fibrinogen level, increased alpha2 - globulin
- Positive cultures from sputum, pleural fluid, blood (positive in 30% of cases)
- ASTRUP: assess severity of respiratory failure
Differential diagnosis: acute bronchiolitis, acute laryngitis, pulmonary tuberculosis,
interstitial pneumonia, pleuro - pulmonary staphylococcal infection, pulmonary atelectasis
other etiology lobular pneumonia, foreign body aspiration.
Complications:
- Local: pleurisy, pneumothorax, pyopneumothorax, pulmonary suppuration
- General: diarrhea, dehydration, otomastoiditis, febrile seizures, sepsis
91
B. LOBAR PNEUMONIA occurs in children older than 2-3 year of age.
Clinical manifestations and diagnosis:
Onset is sudden with: shaking chill, high fever (39-40 C), stabbing, headache, vomiting,
herpes labialis. Rarely the onset is pseudoapendicular/pseudomeningeal.
Later on the course of the illness occurs frequent cough, initially dry than wet, tachypnea,
polypnea, tachycardia, mild oliguria with albuminuria, fatigue, impaired general condition.
Auscultation of the chest reveal - the pulmonary consolidation syndrome: dullness,
diminished breath sounds, bronhophony, fine crackles.
After approx. 7-10 days fever drops suddenly, the evolution is good in approx. 3-4 weeks.
Chest radiography:
Pulmonary consolidation - homogeneous opacity, triangular, with base to the periphery and
top to the hilum of the lung, sharply demarcated, with subcostal intensity, localized to an
entire lobe or segment of the lung. Rarely is associated with pleural effusion (fig 27).
Fig . 27 - Right lobar pneumonia
Laboratory findings:
- Leukocytosis with elevated neutrophil count
- Positive acute phase reactants: accelerated ESR, positive CRP (> 60 mg/l), increased
fibrinogen level
92
PNEUMONIA with PULMONARY ABSCESS
Etiology:
- Staphylococcus aureus
- Gram negative microorganisms
- Pneumococcus Type 3 (with thick polysaccharide capsule)
A. STAPHYLOCOCCAL PNEUMONIA (Pleuro-pulmonary staphylococcal infection)
Definition: severe, rapid evolution pneumonia caused by Staphylococcus aureus, transmitted
by inhalation or hematological spread.
Clinical manifestations and diagnosis:
Usually starts suddenly with a toxico - septic syndrome with high fever, pallor, agitation or
drowsiness and digestive signs: marked anorexia, vomiting, diarrhea, flatulence. Respiratory
distress syndrome and heart failure can be installed quickly.
Later on the course of the illness (which can be installed in a few hours or days) four clinico-
radiological stages can be distinguished: interstitial, abcedant, pleuretic and bullous.
a. In the interstitial stage toxico - septic syndrome is prevailing with high fever, mottled
skin, circles round the eyes, perioronasal cyanosis, cold extremities and digestive
symptoms, which are more severe, especially persistent flatulence (sometimes up to
ileus). The child has the appearance of "intoxicated " (key clinical features), lethargic
or agitated. Functional respiratory syndrome is manifested by: tachypnea, expiratory
moan, nasal flaring, dyspnea. Sometimes, cardiovascular syndrome is present with
hypotension and tachycardia. Radiological characteristics: pulmonary interstitial
thickening occurs.
b. Abcedant stage: toxico - septic and respiratory syndrome are more intense.
Radiological characteristics: micro- or macronodular opacities, incompletely
delimitated and confluent corresponding to pulmonary microabcesses. These tend to
confluate and empty as vomica. Physical examination reveals: dullness, bronhophony
and crackles. Radiological characteristics: initially aspect of bronchopneumonia with
confluent micro- and macronodular opacities then air-fluid levels.
c. Pleuretic stage: pleuretic syndrome characterized by: dullness, diminuation of tactil
fremitus, decreased breath sounds, decreased respiratory excursions on the affected
93
side. Radiological characteristics: simple pleural thickening or massive pleural
effusion with or without associated pneumothorax.
d. Bullous stage: There is not a proper stage, as bullae may be missing in 20% of cases
or can be added in any other stage. Radiological characteristics: pneumonocele which
can persist for months (fig. 28).
Fig 28 . Right staphylococcal pneumonia
Diagnosis is based on:
- Clinical signs (especially the appearance of "intoxicated" child and abdominal
bloating rebellious to treatment)
- Radiological findings (4 stages)
- Laboratory findings:
o Leukocytosis with elevated neutrophil count, accelerated ESR, positive CRP
(especially important for assessing the clinical progress), intrainfectious
anemia
o Staphylococcus aureus cultures from blood and pleural fluid
o Thoracocentesis: pleural fluid - exudate with polymorphonuclear leucocytes
Evolution: in the early days due to severe toxico-septic syndrome, deaths may occur. The
acute evolution is approx. 2-3 weeks followed by a slow regression period of weeks or
months.
Complications:
- Suppurative: septic arthritis, meningitis, brain abscess, sepsis
94
- Nonsuppurative: pneumothorax, pneumomediastinum
B. PNEUMONIA WITH GRAM-NEGATIVE MICROORGANISMS
Etiology: Klebsiella pneumoniae, Haemophilus influenzae, Psuedomonas aeruginosa,
Proteus, Serattia, rare E. coli, Aerobacter. Frequently are "hospital" germs, nosocomial
infections with resistant bacteria.
Predisposing factors: they occur more frequently in:
- Neonates, premature, malnourished infants and young children, immundepressed
patients with anemia, rickets, hospitalized.
- Malabsorption (cystic fibrosis, celiac disease).
- Immunocompromised patients (leukemia treated with immunosuppressants).
Usually starts slowly, insidiously, through a toxico - septic syndrome with marked digestive
disorders comperative to respiratory syndrome, radiologically with pleural involvement and
typical biological characteristics of bacterial infections.
ATYPICAL PNEUMONIA
It is characterized by:
- Lack of evidence of bacterial etiology
- Without leukocytosis
- Discrepancy between obvious radiological signs and poor pulmonary clinical findings
- Chest radiography: predominantly affecting the basal interstitial lung
- Clinical forms ("common cold", headache, muscle aches, mild fever and cough)
Etiology: frequently viral but other microorganisms may be involved to:
- Viruses with pulmonary tropisms: respiratory syncytial virus, influenza virus,
parainfluenza virus, adenoviruses, rhinoviruses
- Viruses with pulmonary and other tropisms: enteroviruses, hepatitis viruses,
cytomegalovirus, measles, rubella, etc.
- Other mircoorganisms: Mycoplasma pneumoniae, Chlamydia pneumoniae, rickettsia,
pararickettsia, Pneumocystis jiroveci (carinii).
95
A. VIRAL PNEUMONIA
Etiology: respiratory syncytial virus (most frequently involved viral agent in infants and
small children).
Clinical manifestations:
The onset is usually sudden, after a short period or concurrently with an acute upper
respiratory tract infection with anorexia, agitation, fever and wheezing.
Later on the course of the illness:
- High fever, respiratory functional syndrome with marked expiratory dyspnea,
irritating cough, inter- and subcotal retraction, nasal flarring, perioral cyanosis.
- Physical findings are poor, often negative, rarely wheezing or crackels can be find.
Diagnosis is based on epidemiological, clinical, radiological and biological findings.
Radiological characteristics: interstitial thickening especially from hilum to the base of the
lung, like "monk locks", sometimes microopacities (difficult to distinguish from lobular
pneumonia) (fig. 29).
Fig . 29 - Interstitial pneumonia
Laboratory findings:
- Possible leukopenia, low ESR (not rule)
- Procalcitonine: to differentiate between viral and bacterial infections ( if is justified
to use antibiotics)
- Etiological diagnosis - serology: complement binding, hemagglutination, cold
agglutination tests - antibody titer , viral culture (rare)
Differential diagnosis:
96
- Pneumonia with Mycoplasma pneumoniae or Chlamydia
- Pneumocystis jiroveci (carinii) pneumonia
- Bacterial pneumonia
- Acute bronchiolitis
Complications: bacterial superinfections
Evolution: healing in approx. 8-10 days
B. PNEUMONIA with MYCOPLASMA PNEUMONIAE
Occurs more frequently in children older than 5 years and adolescents, in small epidemics,
accounting for 7-40 % of community-acquired pneumonia in children. Incubation lasts 1-3
weeks.
Clinical manifestations:
Onset is pseudoinfluenza like with fever, headache, myalgia, dysphagia.
Later on the course of the illness appears paroxysmal, irritating, initially dry than wet cough,
productive with white or rose-coloured sputum, sometimes dyspnea.
Physical examination of the lung is poor - fine crackles, sometimes wheezing (differential
diagnosis with bacterial pneumonia where wheezing is missing) or bronchial rales can be
identified.
Chest radiography: is nonspecific, changes occur especially unilateral, in the lower lobe of
the lung in 75 % of cases. In the early stage of pneumonia interstitial thickening, reticular
aspect can be seen, later macronodular or segmental opacities occur.
Laboratory findings:
- Serology: antimycoplasma pneumoniae antibodies (IgM remains positive up to 6-12
months after the infection), the presence of cold agglutinins, complement binding
reaction
- Frequently accelerated ESR
- Cultures of sputum or throat culture
Complications are rare: Stevens Johnson syndrome, neurological complications (aseptic
meningitis, meningoencephalitis), hematological complications (thrombocytopenia,
hemolysis), rarely pancreatitis, myocarditis or pericarditis.
97
C. PNEUMONIA with PNEUMOCYSTIS JIROVECI (CARINII)
Definition: it is an interstitial plasma cell pneumonitis caused by a parasite, Pneumocystis
jiroveci (formerly Pneumocystis carinii), which occurs in immunocompromised patients: HIV
infected patients, congenital immunodeficiency, malnourished, premature, malignancies,
patients with organ transplants, etc. The incubation period is 3-8 weeks.
Clinical manifestations:
The onset is slow, insidious with marked tachypnea without fever, later gradually associated
dry cough, inter- and subcostal retraction, nasal flaring, cyanosis.
Later on the course of the illness a sever functional respiratory syndrome appears, but the
physical examination is poor or increased breath sounds may occur. Cardiovascular syndrome
may be present with tachycardia, hepatomegaly, edema, restlessness.
Radiological findings: micro- and macronodular diffuse infiltrates occurring, bilateral,
confluent ("sett" aspect) and later both lungs looks as "matt glass".
Accurate diagnosis is established by demonstrating the presens of Pneumocystis jiroveci with
bronchoalveolar fluid lavage.
TREATMENT OF PNEUMONIA
Therapeutic goals of treatment of pneumonia are:
1. Providing vital functions
2. Etiological treatment
3. Hygienic-dietary treatment
Hygienic-dietary reccomandations
- Isolation, room temperature 18 to 21 C, humidity 40 %
- Position in bed: with lift shoulders, position changed every 1-2 hours to avoid stasis, bath
made with 1 hour before meals
- Feeding: will be unchanged if the child is not anorexic or with dyspnoea; may be reduced
or given in divided doses or by gavage. Provide the required amount of liquid, lossed by
sweating and polipnee.
98
Treatment of acute respiratory failure
Desobstruction of upper airways: aspiration of secretions. Respiratory physiotherapy is NOT
useful in patients with severe associated dyspnoea without other pathology. Using of
nasogastric probe will be avoided because of further hampering respiration.
b. Oxygen therapy: improves blood oxygenation, decreases anxiety, labor and respiratory
effort and pulmonary vascular resistance.
Indications of oxigen therapy:
- SaO
2
< 92 % if the patient is breathing spontaneously, effitiently
- cyanosis and a "combat for air syndrome " (polipnea, " air hunger ", sweating,
agitation)
- O
2
concentration will be 30-100 % to bring pO
2
to 60-100 %
- In the tent, face mask: a flow rate of 4 liters/minute, can lead to a saturation of
100% O
2
- The optimum level of O
2
(if the pressure O
2
can not be monitorized) is the flow of
O
2
at which cyanosis disappeared plus of this flow
- Optimal flow of O
2
given by nasopharyngeal probe for infant and young child is:
2-4 liters/minute, administered discontinue - before meals and treatments.
- O
2
is cold and dry, must be warmed and humidified by bubbling in oxygenator
- Do not use O
2
concentration > 40% in preterm infants and newborns because
retrolental fibroplasia can occurring followed by blindness
- Side effects in case of administration of high concentrations O
2
: tracheobronchial
hypersecretion, fatigue, vomiting, dizziness, epileptic spasms, atelectasis,
pulmonary edema
c. Improve of ventilation:
- Aerosol therapy: provides moisture, allows nebulization of bronchodilators
- Endotracheal intubation and assisted mechanical ventilation are indicated if: pO
2
< 50 mmHg, pCO
2
> 75 mmHg
d. Correction of acidosis: based on ASTRUP parameters.
e. Reduction of O
2
consumption at the periphery:
- bed rest, administration of Phenobarbital 3-5 mg/kg/day PO/IM (the goal is to
maintain an O
2
saturation > 92% monitored by pulse oximeter)
99
- improving transport O
2
if Hb <7 g% with: red blood cell concentrate: 5 ml/kg or
whole blood 10 ml/kg transfusions
Special therapeutic measures:
+ In pneumonia with hypersecretion: thinning and removal of secretions by:
- Keeping the cough reflex (in case of dry and irritating cough: Codeine 0.3
mg/kg/day, or Calmotusin 3x 4-5 drops/day)
- Postural drainage
- Ensuring the necessary liquids
- Expectorants mucolytics: Bromhexin 3x10 drops under 2 years, 3x15 drops between
2-6 years of age
- Corticosteroids: HHS 10 mg/kg/day, 4-6 x/day, iv; or prednisone 1-2 mg/kg/day, po,
in short courses of 4-7 days (after which period may be cut short without withdrawal).
Corticosteroids have the following effects:
- Suppress tissue response to injury, inhibiting the formation of fibroblasts
- Reduce bronchospasm produced by histamine
- Reduce the inflammatory edema
+ In pneumonia with bronchospasm: bronchodilators:
Short-acting beta 2 agonists in aerosol:
- Salbutamol (Ventolin) sol. aerosols (5 mg/ml) 0.15 mg/kg/d (up to 5 mg)
- Terbutaline (Bricanyl) sol. aerosols (2.5 mg/ml) 0.15 mg/kg/d
Anticholinergic agents in aerosols:
- Ipratropium bromide (Atrovent) sol. aerosols (0.025 mg/ml)Treatment of
cardiovascular syndrome
- Change the patient's position: trunk elevated
- Reduce the amount of fluid intake
- Place low sodium diet
- Administer cardiac glycosides, diuretics
- In collapse: filling the vascular bed
Treatment of toxico - septic syndrome
I. Antiinfectious treatment
II . Treatment of neuro - toxic symptoms
I. Antiinfectious treatment etiological treatment: antibiotics (AB), chemotherapy,
antiviral- and antifungal therapy
100
General considerations:
1. Most community aquired pneumonia in children are viral: AB therapy IS NOT
required, only symptomatic treatment will be administered (in case of fever
antipyretics), although in current practice due to the difficult differentiation of the
bacterial and viral pneumonia, and the risk of superinfection of viral pneumonia,
antibiotic therapy is initiated (this usually becomes the roule in newborn and infants
under 6 months of age).
2. Antibiotic treatment is usually empirical because of the difficulty of identification of
the etiological agent.
3. The type antibiotic and method of administration depend on: patient's age, severity of
disease, the involved etiologic agent, the patient's immunological status, regional
sensitivity to antibiotics of bacteria.
Antibiotic treatment:
a. Depending on the severity of the disease:
- Mild and moderate forms of the disease (with good digestive tolerance) are treated as an
outpatient with oral antibiotics (PO)
Aminopenicillin (broad-spectrum penicillins)
- Amoxicillin (Ospamox, Standacilin): 20-40 mg/kg/day, 3x/day, suspension or capsule
(is the drug of choice in the age group 2-5 years)
- Amoxicillin - acid clavulanique (Augmentin, Amoxiclav, Bioclavid): 20-40
mg/kg/day calculated for amoxicillin 2x/day suspension, capsules
Cephalosporins - 2nd, 3rd generation
- Cefuroxime (Zinnat): 30 mg/kg/day, 2x/day
- Ceftibuten (Cedax): 9 mg/kg/day, 1x/day
Macrolides:
- Erythromycin (rarely, because of digestive intolerance)
- Azithromycin (Sumamed): 10 mg/kg/day, for 3-5 days 1x/day
- Clarithromycin (Klacid, Fromilid): 15 mg/kg/day, 2x/day
- Severe forms - requiring hospitalization; antibiotic will be administered parenterally
(IV,IM )
Criteria for hospitalization:
- Infants under 6 months of age
- If outpatient treatment was inefficient after 48-72 hours
101
- Child has dehydration, hypoxia or significant respiratory failure
- Leukopenia (<5000/mm
3
)
- Unfavorable family or social environment
Aminopenicillin (broad-spectrum penicillins
- Ampicillin 100-200 mg/kg/day, 3-4x/day
Cephalosporins - 2nd, 3rd generation
- Cefuroxime (Kefurox, Cefuroxime, Axycef ): 100-150 mg/kg/day, 2-3x/day
- Ceftriaxone (Rocephin, Ceftriaxone): 50-80 mg/kg/day, 1-2x/day
A. Depending on the most likely etiology at a certain age:
In the newborn:
Streptococcus gr. B: Penicillin G
Gram negative microorganisms: Ampicillin + aminoglycosides (Amikacin, Tobramycin) or
3
rd
generation cephalosporins (Cetotaxim)
2 months - 5 years: Haemophilus influenzae, Streptococcus pneumoniae (Pneumococcus),
rarely Staphylococcus aureus, and gram-negative bacteria (Klebsiella, Psuedomonas)
Haemophilus influenzae pneumonia: Amoxicillin first choice. In severe forms
Chloramphenicol + parenteral Ampicillin or cephalosporins - Ceftriaxone, Cefotaxime
- About 35 % of Haemophilus influenzae strains produce beta - lactamase, theirfore
beta- lactamase resistant antibiotics are required, such as cephalosporins, macrolides
(clarithromycin, azithromycin), amoxicillin/clavulanate
- Streptococcus pneumoniae pneumonia (Pneumococcus)
Drugs of first choice: Amoxicillin, Amoxicillin/Clavulanate, Penicillin G (Penicillin - very
seldom used because 25-50 % of pneumococcal strains are resistant)
- In cases with resistance can be given: Cephalosporins, Vancomycin
- Staphylococcus pneumonia
- Methicillin-susceptible staphylococci: Oxacillin 200mg/kg/day, Cephalosporins -
2nd, 3rd generation. In case of - lactam antibiotic allergy - Clindamycin 10-30
mg/kg/day po, in 3 diveded doses.
- Methicillin - resistant staphylococci: Vancomycin 40-60 mg/ kg/day in 3-4 divided
doses
- Klebsiella pneumonia
- Aminoglycosides: Amikacin (Pyerami) 15 mg/kg/day 2 diveded doses,
Netilmicin, Tobramycin)
102
- Cephalosporins - 2nd, 3rd generation
- Combination of aminoglycosides with cephalosporins
- Pneumonia with Pseudomonas aeruginosa (Pseudomonas)
- See Klebsiella, but use cephalosporins effective on Pseudomonas (ceftazidime,
cefoperazone)
- Carbenicillin, Imipenem
- Aspiration pneumonia: etiologic agents incriminated are usually anaerobic germs or
Staphylococcus aureus, Pyogenic streptococci. For anaerobes should be used:
Metronidazole. Clindamycin, Penicillins, Cephalosporins third generation.
- Mycoplasma pneumoniae pneumonia:
- Macrolides: Erythromycin, Clarithromycin, Azithromycin
- Alternative: Tetracyclines (after age 8 years), new generation quinolones
- Chlamydia pneumoniae pneumonia:
- Macrolides: Erythromycin, Clarithromycin, Azithromycin
- Alternative: Doxycycline
- Pneumocystis jiroveci (carinii)
- Trimethoprim/sulfametoxazole (Co-trimoxazole, Biseptol): 20 mg/kg/day
calculated for Trimethoprim, 3x/day, PO for 10-14 (21) days
- Alternative: pentamidine inj. 4 mg/kg/day, 2 weeks.
c.Duration of antibiotic therapy:
- Generally 7-10 (14) days in uncomplicated pneumonia
- Pneumonia complicated with pleural effusion, abscess: requires 14-21 days of
treatment
- Pleuro-pulmonary staphylococcal infection: considered a surgical disease that requires
parenteral treatment three weeks, followed by at least 1-3 weeks oral antibiotics. In
the 3
rd
- 4
th
weeks of evolution fibrous connective tissue reaction occurs around the
lesions, which interfering the antibiotic entering in the affected area and
complications may occur: pleural thickening, persistent pleural fluid, pneumothorax,
which requiring surgical treatment (thoracentesis, drainage of abscess, minimum
pleurotomy).
d. Rules of antibiotic therapy:
- In severe forms is recommended, at least initially, antibiotics in iv infusion, and at
shorter intervals of administration
103
- If after 48-72 hours of administration, an antibiotic not prove effective, it will be
changed or will be associated with another antibiotic
- Penicillin G 100.000 IU will be dissolved in 1 ml of normal saline to avoid fibrosis of
quadriceps, when administered IM
- In the event of using two antibiotics, their administration will not be stopped suddenly
at the same time. An antibiotic (usually the most " toxic") will cease sooner.
- Whenever possible, treatment should be conducted on the streight of antibiogramma.
Antiviral treatment (restricted to pneumonia where the causative viral agent is revealed):
Ribavirin (RSV), amantadine (flu), etc.
Antifungal treatment: Pneumonia with Candida albicans (in immunocompromised patients):
Amphotericin B, Flucytosin, Fluconazole (Diflucan)
Prophylaxis:
- Haemophylus influenzae type B vaccine
- Pneumococcal vaccine: immunocompromised children, splenectomised patients,
patients with malformations
- Flu vaccine A, B , C: annual in high-risk children: broncho-pulmonary dysplasia,
lung malformations, congenital heart defects, immunosuppression
Treatment of neuro-toxic symptoms:
- Intravenous corticosteroids: HHS/Methylprednisolone IV
- Administration of 10 g glucose/kg/day
Symptomatic treatment
Antipyretic treatment: over 38.5 C rectal
- increased fluid intake
- bath with light warm water, prisnitz
- Antipyretics: Paracetamol 10-15 mg/kg 3-4 x/day (oral, supp.), Ibuprofen: 20-40
mg/kg/day, Aspirin 10-15 mg/kg/day (CONTRAINDICATED in varicella, influenza,
INFANTS AND TODDLERS can cause Reye syndrome)
Fighting flatulence:
- Local warmth on the abdomen
- Rectal probe
104
- Miostin (neostigmine): 0.2-0.3 ml I.M. or S.C
In hypokalemia: administration of potassium
Adjuvant therapy:
- Volume and hydro-electrolytic rebalancing
- Acido-basic rebalancing
- Combat cerebral edema
- Treatment of febrile seizures
- Treatment of digestive disorders: diarrhea, vomiting (Plegomazin: 0.5-1 mg/kg/day)
Maneuvers or surgical procedures: pleural puncture, pleural drainage, exsufflation
pneumothorax, pleurotomy.
References
1. The Management of Community - Acquired Pneumonia in Infants and Children Older Than 3 Months
of Age : Clinical Practice Guidelines by the Pediatric Infectious Diseases Society and the Infectious
Diseases Society of America , IDSA Guidelines , 2011
2. Samir S. Shah - Current Diagnosis & Treatment of Community - Acquired Pneumonia in Children,
Highlights of the PIDS / IDSA National Guidelines , American Academy of Pediatrics, 2012
3. Jeremy Hull - Community Acquired Pneumonia in Children, Oxford Children's Hospital, UK,
European Respiratory Society, 2012
4. Assessment and Management of Pediatric Community Acquired Pneumonia, Intermountain Healthcare,
2013
5. Guidelines for the Management of Community Acquired Pneumonia in children: update 2011 British
Thoracic Society Community Acquired Pneumonia in Children Guideline Group. - Thorax 2011
6. Shields, M.D. , Bush A , Everard M. L. et al : British Thoracic Society guidelines. Recommendations
for the assessment and management of cough in children. Thorax, 2008, 63
7. Everard ML . - Recurrent Lower Respiratory Tract Infections " - going around in circles, respiratory
medicine style. Paediatric Rev Respir. 2012 Sep, 13 (3):139-43.
8. A. Georgescu, Anca Ioana - Compendiu de pediatrie, ediia III, Editura ALL, 230-237, 251-255
9. Brand PL , Hoving MF de Groot EP. - Evaluating the child with recurrent lower respiratory tract
Infections . Paediatric Rev Respir . 2012 Sep , 13 (3) :135-8
10. Kliegman, Stanton St . Gems et al. - Nelson Textbook of Pediatrics, 19th Edition, Elsevier Saunders ,
1475-1479
105
CHILDHOOD ASTHMA
Definition: asthma (i.e Bronchial asthma - AB) is a chronic inflammatory condition of the
lung airways characterized by variable airway obstruction (reversible either spontaneously or
with treatment) associated with bronchial hyperresponsiveness to a variety of provocative
exposures.
Etiology: is multifactorial.
- Hereditary predisposition for bronchial hyperreactivity to certain conditions.
- Presence of atopy (respiratory allergy) or the ability to develop serum reagin levels
(Antibodies) IgE, IgG against pneumoallergens (rarely to food allergens).
- AB exacerbation precipitating factors can be: environmental factors - exposure to
allergens:
o dust mites
o pollen, mold, animal dander
o viral infection, chemicals, tobacco smoke
o exercise, emotions, meteorological factors
o aspirin, food additives, endocrine factors, etc.
Avoidance of food and aeroallergens in infants decreases the incidence of atopic dermatitis
in infancy and asthma in high risk children.
4
Types of childhood asthma (pathogenic mechanism)
1. Extrinsic or allergic asthma appears in atopic conditions due to various allergens by
immunoallergic mechanism.
2. Intrinsic asthma (non-allergic, idiopathic) is secondary to disturbances of bronchial
reactivity by changes of chemical mediators, without atopy (IgE values are normal,
absent or moderate eosinophilia - below 10%).
3. Infectious asthma - wheezing episodes are triggered mainly by viral infections.
Subsequently, it can be complicated by other types of asthma.
4. Chronic cough (recurrent, spasmodic). Is a latent form of asthma, a bronchial
hyperreactivity.
5. Effort induced asthma - bronchoconstriction occurs after a prolonged effort over 6
minutes.
6. Aspirin - induced asthma - is an intrinsic asthma associated with nasal polyps and
sinusitis.
106
7. Mixed asthma - the predominance of one of the triggers of the exacerbation.
Diagnosis:
AB clinical suspicion arises when a child presents:
- Frequent episodes of nocturnal cough
- Dyspnea
- Wheezing
especially if it develops or worsens during exercise or the at night, or are is triggered by
exposure to dust, pollen, tobacco smoke, pets, emotions etc.
AB diagnosis is based on:
Medical history: recurrent paroxysmal expiratory dyspnea, nocturnal symptoms, seasonal
exacerbations to allergen exposure, the existence of AB or other atopic manifestations in the
family (allergic rhinitis, atopic dermatitis), etc.
Clinical manifestations:
Key clinical signs suggestive for atopic phenotype include:
- Eczema or atopic dermatitis
- Dry skin
- Ringed eyes
- Conjunctival irritation
- Persistent swelling of the nasal mucosa, rhinorrhea, itchy nose/frequent rubbing of the
nose with the hand and allergic fold on the root of the nose.
Clinical manifestations of asthma:
A. Exacerbation: paroxysmal expiratory dyspnoea reversible either spontaneously or to
bronchodilators. It can be manifested only by spasmodic cough lasting 20-30 minutes during
the night or severe crisis with:
- Expiratory dyspnoea - polipnoea in infants and toddlers, bradipnoea in older children
- Intercostal retraction
- Nasal flaring
- Prolonged expiration, wheezing
- Dry then wet cough
- + / - Cyanosis
Physical examination: anxious child with orthopnoea position (in older children)
- Distended thorax, fixed "in inspiration", hypersonority
- Bronchial rales (ronchi at the beginning of the crisis then crackels)
- Lowering of liver and spleen
107
- Evolution: hours for children, days for infants
B. Status asthmaticus: paroxysm of expiratory dyspnoea lasting over 24 hours, with signs of
severe acute respiratory failure, unresponsive to bronchodilators and associated with hypoxic
encephalopathy (table 12).
Table no. 12 .The symptoms of status asthmaticus
Combat phase - respiratory manifestations
- Marked suprasternal and
intercostal retraction
- Nasal flaring
- Intense expiratory dyspnoea, short
inhalation period
- Cyanosis
- Regular breathing with tachypnea,
then progressively irregular with
short apnea periods short
- Hyperinflation
- Pulmonary hypersonority
- Decreased breath sounds
Phase of bronchoplegia
Respiratory symptoms
- Bronchoconstriction replaced by
bronchodilation
- Shallow, rare breathing
Cardiovascular symptoms
- Tachycardia
- Heart failure
- Initially hypertension, then
hypotension and collapse
Neuropsychiatric manifestations
- Agitation, anxiety
- Drowsiness
- Progressive hyporeactivity
- Coma, seizures
- Cardiopulmonary arrest
C. Intercritical period: the period between exacerbations in which the child may be
completely asymptomatic or presents minimal symptoms (night and/or in the morning
cough). Persistence of clinical manifestations in this period in children with AB represents
elements of sever prognosis. Severe forms of asthma are characterized by intercritical
residual obstruction progressing to chronic respiratory failure which will associate: chest
deformity, cyanosis, clubbing, stature-weight weakness, delayed puberty.
3. Laboratory investigations:
- Blood gas analysis (PaO
2
, PaCO
2
- to assess the severity of exacerbation)
- Chest X-ray: shows hyperinflation, emphysema or atelectatic areas.
108
- Allergy tests: blood eosinophilia, total serum IgE and specific IgE determination, skin
allergy tests
- Pulmonary function testing spirometry - to confirm bronchial obstruction and its
severity by measuring lung volumes and flows (vital capacity VC, forced expiratory
volume in one second FEV
1
, peak expiratory flow - PEF) allowing monitoring of
spontaneous evolution under treatment. If FEV
1
increases with by 12% after
administration of inhaled beta2-agonist, reversibility of bronchial obstruction is
confirmed.
Table no. 13. Classification of asthma severity
Asthma severity Daytime
symptoms
Nightime
symptoms
FEV
1
/PEF
variability
Intermittent < 1/week 2/month Normal
80%
Variability < 20%
Persistent mild > 1/week (< 1day) > 2/month 80%
Variability: 20% -
30%
Persistent
moderate
Daily
Using of | agonist
daily
> 1/week 80-60%
Variability: 30%
Persistent severe True out the day,
frequent
exacerbations
Frequent < 60%
Variability > 30%
Fig. no. 30. Evaluation of severity of asthma exacerbation
109
TREATMENT OF ASTHMA
Immediate objectives:
- Bronchodilation
- Repermeabilization of airways
Long-term goals:
- Suppressing the chronic inflammatory process
- Avoiding contact with triggers
Home management of asthma:
- Short-acting beta2-agonists (Salbutamol, Bricanyl, Berotec - spray, spacer): 2 puffs
three times at intervals of 20 minutes, then 1 hour and 4-6 hour respectively. The
following can be administered po: Salbutamol (Ventolin) 0.2-0.3 mg/kg/day divided
into 3 doses.
110
- Corticosteroids: When evolution is unfavorable, if needed, inhalations at intervals of
less than 3-4 hours (PEF as 65-50% of baseline values) are given. Prednisone 1-2
mg/kg/day po in 2 doses or Methylprednisolone (Medrol) 0.5 mg/kg/day in 2 doses.
- Theophylline - 10-15 mg/kg/day po in 2 doses at 12 hours.
Treatment of exacerbations of asthma in emergency room, hospital, intensive care unit: is
a more complex treatment based on careful monitoring of the patient (oxygen, nebulization of
beta2 - agonists, I.V. corticosteroids, anticholinergics - ipatropium bromide (Atrovent)
nebulization, restoration of acid-basic balance, heart failure treatment and mechanical
ventilation (fig. no. 31).
Fig. no. 31. Treatment of exacerbations of asthma in emergency room, hospital, intensive
care unit
111
In case of exacerbation the following should be avoided: sedation, expectorant, high-
volume hydration, chest physiotherapy.
Long-term controller therapy: for management of the chronic inflammatory process and
avoidance of allergens/triggers (table no. 14).
Table no. 14. Long-term control medication according to asthma severity
Asthma severity Controller therapy Symptomatic
treatment (Rescue
medication if needed)
Intermittent - Short-acting
beta2-agonists
Persistent mild Cromone
Low dose inhaled cortico-steroids:
200-500 mcg/day
Or
Oral leukotriene receptor
antagonists (Singulair -Montelukast)
Short-acting
beta2-agonists (max 4 x
day)
Persistent moderate Cromolyn
Low/medium dose inhaled
corticosteroids: 500-800 mcg/day
Or
Low dose inhaled corticosteroids +
oral leukotriene receptor antagonists
Or
Inhaled corticosteroids + Long acting
beta2 agonists
Short-acting
beta2-agonists
Ipatropium bromid
Persistent- severe High-dose inhaled corticosteroids:
800-1200 mcg/day
Or
Low dose inhaled corticosteroid +
Long acting beta2 - agonists
+ Oral corticosteroids
+ IgE antagonists (Omalizumab)
Theophylline retard
Short-acting
beta2-agonists
Ipatropium bromide
112
Long term controller therapy of asthma - "STEP-UP STEP-DOWN" approach, according to
symptom control. Once good asthma control is achieved for at least three months, the
guidelines (GINA 2011) suggest decreasing the dose or number of controller therapy and
moving one step lower to the minimum treatment that maintains control, parallel with close
monitoring of evolution. In case of uncontrolled asthma, the treatment goes up one step to a
higher level, or even in severe cases, will jump two treatment steps (table no 15).
Table no. 15. The controller medication in asthma by steps
Controller medication
STEP 5 STEP 4 + oral corticosteroids
Anti IgE (Omalizumab for children older than 12
years with allergies)
STEP 4 Medium or high dose ICS + Long acting beta2
agonists
Or
Medium or high dose ICS + Leukotriene
receptor antagonists
Or
Medium dose ICS + teophyilline retard
STEP 3 Medium or high dose ICS
Or
Low dose ICS + PO Leukotriene receptor
antagonists
Or
Low dose ICS + Long acting beta2 - agonists
Or
Low dose ICS + teophyilline retard
STEP 2 Low dose ICS
Or
Leukotriene receptor antagonists
STEP 1 -
ICS inhaled corticosteroids
*Global strategy for asthma management and prevention in children 5 years and younger modified, adapted
113
Elimination, reduction and control of trigger factors: reduces exposure to allergens; it is
composed of avoiding of moisture and dampness, dust, smoke, fresh paint, carpets, curtains,
materials of wool and feathers, aspirin, but also ventilation, dust extraction, air conditioning,
constant temperature (18-20C) and avoiding pets. Food restrictions are only necessary in
well proven cases. Breastfeeding has an important prophylactic role.
Efficacy and success of anti-asthmatic therapy depends also on the education of the child and
family. They need detailed description of the signs and symptoms that indicate an impending
exacerbation, accurate information about allergens and triggers, explaining and checking the
inhalation technique and verifying of the correct monitoring of respiratory parameters.
REFERENCES
1. S.Holgate, H.Bisgaard, L.Bjermer et al. - The Brussels Declaration: the need for change
in asthma management Eur Respir J, 2008; 32/6
2. Pearce N, Ait-Khaled N, Beasley R. - Worldwide trends in the prevalence of asthma
symptoms: phase III of the International Study of Asthma and Allergies in Childhood
(ISAAC), Thorax 2007; 62,758 - 766
3. J. Bizzintino, N. M. Lee, F. Vang - Association between human rhinovirus C and severity
of acute asthma in children Eur Respir J., 2011; 37: 1037-42
4. Arshad SH, Bateman B, Matthews SM - Primary prevention of asthma and atopy during
childhood by allergen avoidance in infancy: a randomised controlled study, Thorax.,
2003; 58: 489-93.
5. http://www.sign.ac.uk/pdf/sign101.pdf - British Guideline on the Management of
Asthma 2012
6. http://ginasthma.org/local/uploads/files/GINA_Under5_2009_CorxAug11_1.pdf - Global
strategy for asthma management and prevention in children 5 years and younger
7. http://ginasthma.org/local/uploads/files/GINA_Report_March13.pdf - Global strategy for
asthma management and prevention
114
CHAPTER III - CARDIOVASCULAR PATHOLOGY
Prof. Univ. Dr. Tognel Rodica
CONGENITAL HEART DEFECTS (CHD)
Definition Failure of normal cardiac development or of the fetal circulation after birth.
Incidence 7-9/1000 live births.
Causes are unknown in the majority of cases, commonly associated with chromosomal
defects, gene defects, congenital infection (e.g. rubella), teratogenic drugs (e.g. phenytoin,
warfarin, alcohol).
Diagnostic methods The history and physical examination are the keystones for diagnosis
of cardiac problems . A variety of other diagnostic techniques can be employed beyond
besides history and physical examination.
A history of the following may indicate the possibility of CHD: poor weight gain, with a
history of a feeding problem, difficulty in swallowing, fainting attack, respiratory difficulties,
exercise intolerance, with the child assuming a squatting position, intermitent or continuous
cyanosis, history of maternal illness during the first trimester of pregnancy, including rubella,
bleeding, severe anemia, drug ingestion, or other teratogen. The physician should obtain a
complete family history to disclose the presence of CHD, syndromes, or other disorders.
The suspicion of cardiovascular abnormality may be raised initially by specific symptoms,
but more commonly is the discovery of a cardiac murmur. Distinguishing an innocent from a
pathological heart murmur may be difficult. Innocent heart murmurs is are the most common
causes of a heart murmur in children. It arises due to the rapid flow and turbulence of blood
through the great vessels and across normal heart valves. It does not signify the presence of
any underlying cardiac abnormality or any other pathology.
The characteristics of innocent heart murmurs are: systolic in timing, short duration, low
intensity sound, it intensifies with increased cardiac output (e.g. exercise, fever), may change
in intensity with change in posture; no associated cardiac thrill, no radiation, asymptomatic
patient.
Clasification Congenital cardiac malformation may be classified in various ways; a clinical
useful clasification is based on two clinical features: the presence or absence of cyanosis and
the type of pulmonary vascularity as determined by chest X-ray (increased, normal,or
115
diminished). CHD can be classified into acyanotic or cyanotic types depending on whether
the predominant presentation is with or without central cyanosis caused by deoxygenated
blood gaining abnormal access to the systemic side of the circulation via the left side of the
heart or the aorta.
Acyanotic CHD: e.g. ventricular septal defect, atrial septal defect, patent ductus arteriousus,
coarctation of the aorta, aortic stenosis.
Cyanotic CHD: e.g.tetralogy of Fallot, transposition of the great arteries, tricuspid atresia,
total anomalous pulmonary drainage.
ATRIAL SEPTAL DEFECT (ASD)
Definition Any opening in the atrial septum is described as an ASD. This definition includes the
secundum atrial defect, septum primum defects and sinus venosus defects.
Prevalence: 5% to 10% of all congenital heart diseases (CHDs). Female preponderance (male-
to-female ratio of 1:2).
Pathology and pathophysiology Three types af atrial septal defects (ASDs) occur in the atrial
septum. Secundum ASD is in the central position of the septum and it is the most common type.
Primum ASD (or partial endocardial cushion defect) is low in the septum and often with deformity
of the mitral or/and tricuspid valve and with persistent atrioventricular canal.(30% of ASDs). Sinus
venosus defect is near the entrance of the superior vena cava (SVC) or inferior vena cava (IVC) to
the right atrium (RA). Partial anomalous pulmonary venous return is common with a sinus venous
defect.
A left-to-right shunt (L-R shunt) is present through the defect, with a volume overload to the RA
and right ventricle (RV) and an increase in pulmonary blood flow.
Clinica manifestations The patients are usually asymptomatic.
A widely split and fixed S2 and a grade 2 to 3/6 systolic ejection murmur at the upper left sternal
border (ULSB) are characteristic of moderate-size ASD. With a large L-R shunt a middiastolic ruble
(resulting from relative tricuspid stenosis [TS]) may be audible at the lower left sternal border
(LLSB). The typical auscultatory findings are usually absent in infant and toddlers, even those with
large defect, because the RV is poorly compliant.
The ECG shows right axis deviation (RAD) (+ 90 to +180 degrees) and mild right ventricular
hypertrophy (RVH) or right bundle branch block (RBBB) with an rsR pattern in V1.
Chest x-ray (CXR) films show cardiomegaly (with right atrial enlargement [RAE), increased
pulmonary vascular markings (PVMs), and a prominent main pulmonary artery (MPA) segment.
116
Two-dimensional echo shows the position and the size of the defect. Cardiac chateterization is
usually not necessary.
Spontaneous closure of the defect occurs in patients with defects 3 to 8 mm (diagnosed by echo)
before 1 !/2 years of age. An ASD with diameter greater than 8 mm rarely closes spontaneously. The
defect may reduce in size in some patients. If the defect is large and left untreated, pulmonary
hypertension develops in the third and fourth decades of life. Cerebrovascular accident due to
paradoxical embolization through an ASD is possible.
Management Exercise restriction is not required.
Nonsurgical closure of the defect using a catheter-delivered closure device has become a preferred
method, provided the indications are met.
Surgical For patients with primum ASD and sinus venosus defect, and some patients with secundum
ASD for which the device closure is considered inappropriate, surgical closure is indicated when
there is a significant L-R shunt with Qp/Qs of 1,5:1 or greater. Surgery is usually delayed until 2 to 4
years of age, unless congestive heart failure (CHF) develops. Open repair with a mid-sternal incision.
High pulmonary vascular resistance (PVR) (10 units/m
2
) is a contraindication to surgery.
VENTRICULAR SEPTAL DEFECT
Definition The term ventricular septal defect (VSD) describes an opening in the ventricular
septum. They may occur in isolation or as part of complex malformations. The clinical
features depend on size and location of the defect.
Prevalence. Ventricular septal defect (VSD) is the most common form of CHD, accounting
for 25% of all CHDs. .
Pathology and pathophysiology As a result of the defect, shunting of blood occurs between
the ventricules. When the size of the defect approaches the size of the aortic annulus, flow is
governed by the relative pulmonary and systemic vascular resistances. When the defect is
smaller, blood flows from the left to the right ventricle because of the higher systolic pressure
in the left ventricle.
The ventricular septum consists of all small membranous septum and a large muscular
septum. The muscular septum has three components: the inlet, infundibular, and trabecular
(or simply muscular ) sept. A membranous VSD often involves a varying amount of muscular
117
septum adjacent to it (i.e., perimembranous VSD). The perimembranous defect is more
common (70%) than the trabecular, infundibular, or inlet defects.
In VSDs with small to moderate L-R shunt, volume overload is placed on the left atrium
(LA) and the left ventricle (LV) (but not on RV). With large defects the RV is also under
volume and pressure overload, in addition to a greater volume overload on the LA and LV.
Pulmonary blood flow (PBF) is increased to a varying degree depending on the size of the
defect and the pulmonary vascular resistance. With a large VSD, pulmonary hypertension
result. With a long-standing large VSD, pulmonary vascular obstructive disease (PVOD)
develops, with sever pulmonary hypertension and cyanosis resulting from a right-to-left shunt
(R-L shunt). At this stage, surgical correction is nearly impossible
Clinical manifestations. Patients with small VSDs are asymptomatic, with normal growth
and development. With large VSDs, delayed growth and development, repeated pulmonary
infections, CHF, and decreased exercise tolerance are relatively common. With PVOD,
cyanosis and decreased level of activity may result.
With a small VSD, a grade 2 to 5/6 holosystolic murmur maximally audible at the lower left
sternal edge and a systolic thrill may be present. With a large defect, an apical diastolic
rumble is audible, which represents a relative stenosis of the mitral valve due to large
pulmonary venous return to the LA. The S2 may split narrowly, and the intensity of the P2
increases if pulmonary hypertension is present.
ECG findings: Small VSD, normal; moderate VSD, left ventricular hypertrophy (LVH) and
left atrial hypertrophy (LAH) (); large VSD, biventricular hypertrophy (BVH) and LAH ();
PVOD, pure RVH.
CXR film reveal cardiomegaly of varying degrees with enlargement of the LA, LV, and
possibly the RV. PVMs are increased. The degree of cardiomegaly and the increase in PVMs
are directly related to the magnitude of the L-R shunt. In PVOD the heart size is no longer
enlarged and the MPA and the hilar pulmonary arteries are notably enlarged, but the
peripheral lungs fields are ischemic.
Two-dimensional echo studies provide accurate diagnosis of the position and size of the
VSD. LA and LV dimensions provide indirect assessment of the magnitude of the shunt.
The Doppler studies of the pulmonary artery (PA), tricuspid regurtation (TR), and the VSD
itself are useful in indirect assessment of RV and PA pressures.
Spontaneous closure occurs in 30% to 40% of all VSD, most often in small trabecular
VSDs. CHF develops in infants with a large VSD but usually not until 6 or 8 weeks of age,
118
when the PVR drops below a critical level. PVOD may begin to develop as early as 6 to 12
months of age in patients with large VSD.
Management Medical. Treatment of CHF. No exercise restriction is required in the absence
of pulmonary hypertension, antibiotic prophylaxis.
Surgical. PA banding is rarely performed unless additional lesions make the complete repair
difficult.
Direct closure of the defect is performed under cardiopulmonary bypass and/or deep
hypotermia.
PATENT DUCTUS ARTERIOSUS
Definition Patent ductus arteriosus (PDA) defined the failure of ductus arteriosus to close.
The ductus is functionally closed in about 90% of full term infants by 48 hours of age.
Prevalence 5% to 10% of all CHDs, excluding those in premature infants.
Pathology and pathophysiology There is a persistent postnatal patency of a normal fetal
structure between the PA and the descending aorta. The magnitude of the L-R shunt is
determined by the diameter and the length of the ductus and the level of PVR. With a long-
standing large ductus, pulmonary hypertension and PVOD may develop with an eventual R-L
shunt and cyanosis.
Clinical manifestations Asymptomatic when the ductus is small. When the defect is large
signs of CHF may develop.
A grade 1 to 4/6 continuous (machinery) murmur best audible at the upper left sternal edge.
An apical diastolic rumble is audible with a large shunt PDA. Bounding peripheral pulses
with wide pulse pressure are present with a large shunt PDA.
ECG findings are similar to those to VSD: Normal or LVH in a small to moderate PDA;
BVH in a large PDA; RVH if PVOD develops.
CXR findings are also similar to those of VSD: normal with small shunt PDA. With a large-
shunt PDA, cardiomegaly (with LA and LV enlargement) and increased PVM are present.
With PVOD the heart size is normal, with a marked prominence of the MPA and hilar
vessels.
The PDA can be directly imaged and its hemodynamic significance determined by 2D echo
and color flow Doppler examination. Cardiac catheterization is usually not indicated in
isolated PDA.
119
CHF or recurrent pneumonia or both develop if the shunt is large. Spontaneous closure of
PDA usually does not occur in term infants.
Management Medical No exercise restriction is required in the absence of pulmonary
hypertension.
Consider pharmacological closure (e.g. indometacin or ibuprofen).
Catheter closure of the ductus may be employed.
Surgical closure is reserved for those patients in whom nonsurgical technique is not
considered applicable. Ligation and division through left posterolateral thoracotomy. PVOD
is a contraindication to surgery.
COARCTATION OF THE AORTA
Definition Coarctation of the aorta (CoA) is a narrowing of the descending aorta.
Prevalence 8% to 10 % of CHDs, with a male preponderance (2:1). Among patients with
Turner syndrome, 30% have COA.
Pathology and pathophysiology CoA may occur at any point in the descending aorta. In the
majority of cases, it is distal to the origin of the left subclavian artery at the level of ductus
arteriosus.
In CoA a narrowing of the upper thoracic aorta is present. There are two groups of patients
with CoA: one group of patients presenting symptoms early in life and the other group
remaining asymptomatic.
In symptomatic infants with CoA, other cardiac defects (such as aortic hypoplasia, VSD,
PDA and mitral valve anomalies) are often present. These abnomalities may have reduced
antegrade flow through the aorta during fetal life.
In asymptomatic children with CoA, associated anomalies are uncommon. The anterograde
flow through the aorta has resulted in a pressure gradient and stimulated the development of
the collateral circulation during the fetal life.
As many as 85% of patients with CoA have a bicuspid aortic valve.
Clinical features Symptomatic Infants
Signs of CHF (poor feeding, dyspnea) and renal failure (oliguria, anuria) with general
circulatory shock may develop in the first 2 to 6 weeks of life.
A loud gallop is usually present, but heart murmur may be absent with weak and thready
pulses in sick infants.
120
The ECG usually shows RVH.
CXR films show a marked cardiomegaly and signs of pulmonary edema or pulmonary
venous congestion.
Two-dimensional echocardiography shows the site and extent of the CoA and other
associated cardiac defects. The Doppler examination reveals a disturbed flow distal to the
CoA, and signs of delayed emptying in the proximal aorta. In symptomatic infants with CoA,
early death from CHF and renal failure is possible.
Management
Medical: Intensive anticongestive measures should be given with fast-acting inotropic agents,
diuretics, and oxygen to stabilize the patient. PGE1 infusion is indicated to reopen the ductus
before any intervention takes place to maintain the systemic circulation.
Balloon angioplasty is controversial, but it can be useful procedure for sick infants;
Surgical repair- Resection and end-to-end anastomosis
Clinical manifestation Asymptomatic Children
These patients are usually asymptomatic except for rare complaints of leg pain.
The pulse in the leg is absent or weak and delayed. Hypertension in the arm or higher blood
pressure (BP) reading in the arm that the thigh may be present. An ejection click resulting
from the bicuspid aortic valve is frequently audible at the apex and/or base. A systolic
ejection murmur grade 2 to 3/6, is audible at the URSB and MSLB and in the left
interscapular area in the back.
The ECG usually shows LVHl.
CXR films show a normal or slightly enlarge heart. Rib notching by collateral vessels may
be seen in the children after about 5 years of age.
Two-dimensional echo shows a discrete, shelflike membrane in the posterolateral aspect of
the descending aorta. The Doppler examination reveals disturbed flow and increased flow
velocity distal to the coarctation. The bicuspid aortic valve is frequently imaged.
Bicuspid aortic valve may cause stenosis and/or regurgitation later in life. If a CoA is left
untreated, LV failure, intracranial hemorrhage, or hypertension encephalopaty may develop
in childhood or adult life.
Management
Medical
Hypertension or hypertensive crisis should be detected and treated
Balloon angioplasty for native CoA is controversial.
A balloon-expandable, stainless-steel stent implanted concurrently with balloon angioplasty.
121
Surgical Resection of the coarctation segment and end-to-end anastomosis.
If CoA recurs following either surgery or angioplasty, balloon angioplasty is the procedure of
choice.
TETRALOY OF FALLOT
Definition Tetralogy of Fallot is a cyanotic congenital heart malformation comprising
infundibular pulmonary stenosis, a ventricular septal defect, dextroposition of the aorta such
that the aortic root overrides the crest of ventricular septal defect , and right ventricular
hypertrophy.
Prevalence. 10% of all CHD. It is the most common cyanotic CHD beyond infancy.
Pathology and pathophysiology
The original description of TOF included four abnormalities: a large DSV, RVOT
obstruction, RVH, and an overriding aorta. Systemic venous retour to the right side of the
heart is normal In the presence of pulmonary stenosis, however, the blood is shunted across
the VSD into th aorta and persistent arterial desaturation and cyanosis result. The severity of
cyanosis is dependent on the degree of RV outflow obstruction .
Clinical manifestations
Most patients are symptomatic, with cyanosis, clubbing, dyspnea on exertion, failure to
thrive, squatting, or hypoxic spells.
A right ventricular tap and a systolic thrill at the lower and middle LSB are usually found. A
loud and single S2, and a loud (grade 3 to 5/6) systolic ejection murmur at the middle and
upper LSB are present.
The ECG shows RAD and RVH
CXR films show normal heart size, decreases PVMs, and boot-sharped heart with a concave
MPA segment. Right aortic arch is present in 25% of the cases.
2D echo shows a large subaortic VSD and an overriding of the aorta. The anatomy of the
RVOT, pulmonary valve, and pulmonary arteries can be imaged
Polycythemia is common, but relative iron deficiency state (hypochromic) with normal
hematocrit may be present. Coagulopathies are late complications of a long-standing severe
cyanosis.
Hypoxic spell
Hypoxic of TOF requires recongnition and treatment, as it can lead to serious CNS
complications. It occurs in young infants, with peak incidence between 2 and 4 months of
122
age. It is characterized by a paroxysm of hyperpnea (rapid and deep respiration), irritability
and prolonged crying, increasing cyanosis, and decreased intensity of the heart murmur. A
severe spell may lead to limpness, convulsion, cerebrovascular accident, or even death.
Treatment of the hypoxic spell is aimed at breaking the vicious circle. One or more of the
following may be employed in decreasing order of preference:
1. Pick up the infant and hold in a knee-chest position
2. morphine sulfate, 0.1 to 0.2 mg/kg SC or IM, suppresses the respiratory center and
abolishes hyperpnea.
3. Treat acidosis with sodium bicarbonate, 1 mEq/kg IV. This reduces the respiratory
center stimulating effect of acidosis.
4. oxygen inhalation has only limited value, since the problem is a reduced PBF, not the
ability to oxygenate.
5. Propranolol 0.01 to 0.25 mg/kg (average 0.05 mg/kg) in a slow IV push, reduces the
heart rate and may reverse the spell.
Management Medical Hypoxic spells should be recognized and appropriately treated.
Oral propranolol, 2-4 mg/kg/day, may used to prevent hypoxic spells and delay surgery.
Detection and treatment of relative iron deficiency stare. Anemic children are particularly
prone to cerebral accident.
Surgical Palliative procedures are indicated to increase PBF in infants with severe cyanosis
or uncontrollable hypoxic spell on whom the corrective surgery cannot safely be performed,
and in children with hypoplastic PA on whom the corrective surgery is technically difficult.
Different types of S-P shunt have been performed.
The Blalock-Taussig shunt (anastomosis between the subclavian artery and the ipsilateral
PA) may by performed in older infants.
Gore-Tex interposition shunt between the subclavian artery and the ipsilateral PA (modified
Blalock-Taussig shunt) is the procedure of choice in small infants.
Conventional repair surgery: Symptomatic or cyanotic infants with favorable anatomy of the
RVOT and PAS may have primary repair at any time after 3 to 4 months of age.
Asymptomatic and minimally cyanotic children may have repair between age 3 and 24
months, depending on the degree of the annular and pulmonary hypoplasia.
Total repair of the defect is carries out under cardiopulmonary bypass. The procedure
includes patch closure of the VSD, widening of the RVOT resection of the infundibular
muscle tissue, and usually placement of the fabric patch to widen the RVOT.
123
COMPLET TRANSPOSITION OF THE GREAT ARTERIES
Definition Transposition of the great arteries (TGA) describes reversal of the anatomic
relation of the great arteries and ventriculoarterial relationship.
Prevalence: TGA constitutes 5% of all CHD. It is more common in boys (3:1).
Pathology and pathophysiology
The aorta arises anteriory from the RV, the pulmonary artery arises posteriory from the LV.
Blood from the right heart goes through the systemic vessels and returns to the right side.
Blood from the left heart goes through the lungs to return to the left side. The end result is
complete separation of the two circuits, with hypoxemic blood circulating in the body and
hyperoxemic blood ciculating in the pulmonary circuit. This anomaly is incompatible with
life unless ASD, PDA or VSD is also present, that permit mixing of the two circulations
The classic complet TGA is called D-transposition, in which the aorta is located anteriorly
and to the right of the PA; When the transposed aorta lies to the left of the PA, it is called L-
transposition.
In neonates with poor mixing of the two circulations, progressive hypoxia and acidosis result
in early death, requiring early intervention. CHF develops in the first week of life in many
patients with this condition.
Clinical manifestations
Cyanosis and signs of CHF (dyspnea, feeding difficulties) develop in the newborn period.
Auscultatory findings are nonspecific.
Sever arterial hypoxemia unresponsive to oxygen inhalation and acidosis are present in
infants with poor mixing. Hypoglicemia and hypocalcemia are occasionally present.
The ECG shows RAD and RVH.
CXR films show cardiomegaly with increased PVMs. An egg-shaped cardiac silhouette with
narrow superior mediastinum is characteristic.
2D echo study is diagnostic. It fails to show a circle-and-sausage pattern of the normal
great arteries in the parasternal short axis view. Instead, it shows two circular structure. Other
view reveal the PA arising from the LV and the aorta arising from the RV.
Management
Medical Metabolic acidosis, hypoglicemia, and hypocalcemia should be treated if present
PGE1 infusion is started to raise arterial oxygen saturation by reopening the ductus.
124
Administration of oxygen may help raise systemic oxygen saturation by lowering PVR and
increasing PBF, with resulting increase in mixing.
A therapeutic balloon atrial septostomy (Rashkind procedure) may be performed if
immediate surgery is no planned. Treatment of CHF with digitals and diuretics may be
indicated.
Surgical Arterial switch operation (ASO), is the procedure of choice in many cardiac centers.
INFECTIVE ENDOCARDITIS
(SUBACUTE BACTERIAL ENDOCARDITIS)
Definition Infective endocarditis (IE) is an infection of the endocardium and/or heart valves
that involves thrombus formation (vegetation), which may damage the endocardial tissue
and/or valves. Although uncommon in children, it is important to identify and treat IE
because of it significant morbidity and mortality.
Prevalence: IE affects 0.5:1000 to 1:1000 hospital patients, excluding those with
postoperative endocarditis.
Pathogenesis and pathology: IE is the result of a series of complex interactions among
blood-borne pathogens, damaged endothelium, fibrin, and platelets. Most children with IE
have an identifiable risk factor for the disease.
The endocardial surface is initialy injured by shear forces associated with turbulent blood
flow in children with CHD, or indwelling central venous catheters in children without CHD.
At the site of endothelial damage, fibrin, platelets, and occasionally red blood cells are
deposited and initially form a noninfected thrombus.
Transient bacteriemia or fungemia result in adherence of microbial pathogens to the injured
endocardium and thrombus. Subsequent fibrin and platelet deposition over the infected
vegetation result in a protective sheath that isolates the organisms from host defenses and
permits rapid proliferation of the infectious agent.
Two factors are important in the pathogenesis of infective endocarditis: (1) structural
abnormalities of the heart or great arteries with a significant pressure gradient or turbulence,
with resulting endothelial damage and platelet-fibrin thrombus formation, and (2)
bacteriemia, even if transient. Bacteremia frequently results from dental procedures and
chewing with diseased teeth.
125
All CHDs (except secundum ASD) and valvular heart disease predispose to endocarditis.
Those with prosthetic heart valve or prosthetic material in the heart are at particularly high
risk for IE. Surgical repair of CHD may reduce but does not eliminate the risk of
endocarditis, with the exception of a simple ASD or PDA. Drug addicts may develop
endocarditis in the absence of known cardiac anomalies.
Vegetation of endocarditis is found usually in the low-pressure side of defect, either around
the defect or on the opposite surface of the defect. For example, vegetations are found in the
PA in PDA or an S-P shunt and in the ventricular surface of the aortic calve and mitral
chordae in AR.
Incolvement of other organs is secondary to embolization or immune-mediated processes.
Microbiology In the past, Streptococcus viridans, enterococci and Staphylococcus aureus
were responsible for over 90% of case. In recent years, this frequency has decreased with a
concomitant increase in cases caused by fungus and HACEK Organisms (Haemophilus,
Actinobacillus, Cardiobacterium, Eikenella, and Kigella)
S.viridans is the most common cause of IE following dental procedures or dental pr
periodontal disease. Enterococcus is the organism most often found after genitourinary or
gastrointestinal surgery or instrumentation. The organism most commonly found is
postoperative endocarditis is the staphylococcus. Fungal endocarditis may occur in sick
neonates, in patients who are on long-term antibiotic or steroid therapy, or after open heart
surgery. HACEK organisms are particularly common in neonates and immunocomplomised
children. Pseudomonas aeruginosa or Serratia marcescens is seen more often is intravenous
drug users.
Clinical manifestations The clinical presentation of IE is variable. It is dependent upon the
extent of the local cardiac disease, degree of involvement of other organ and the causative
agent. Underlying heart defect is present in almost all patients. History of recent dental
procedures, tonsillectomy, or toothache is common. The onset of the illness is insidious, with
fever, fatigue, loss of appetitie, and pallor, myalgi, headache, night sweats.
Heart murmur and fever are almost always present. Splenomegaly is common (70% of
patients).
Skin manifestations (seen in 50% of patient), probably secondary to microemboli, may
include petechiae, Osler nodes (tender red nodes) at the ends of the fingers or toes, Janeway
lesions ( small, painless hemorrhagic areas on the palms or soles), and splinter hemorrhage
(linear hemorrhagic streaks beneath the nails).
126
Embolic phenomena to other organs (e.g, pulmonary emboli, seizures and hemiparesis,
hematuria) affect 50% of patients.
Positive blood culture are found in more than 90% of patients is the absence of a recent
antimicrobial therapy. Antimicrobial pretreatment reduces the yield of positive blood culture
to 50% to 60%. Other laboratory findings include anemia, leukocytosis, and increased
erythrocyte sedimentation rate (ESR).
2D echo may actually demonstrate the vegetation. A transesophageal echo study is usually
more productive in demonstrating the vegetation. It is unlikely that vegetation less than 2 mm
in maximum dimension will be image by 2D echo.
Diagnosis: A presumptive diagnosis on infective endocarditis is made when a patient with an
underlying heart lesion has a fever of unknown origin of several days duration and any of the
typical physical findings or laboratory changes is present. The diagnosis of IE is based upon
careful history and physical examination, blood culture and laboratory results, and
echocardiogram.
According to the revised Duke criteria, IE is diagnosed based upon the presence of one of
two pathologic criteria or, more commonly, with certain combination of clinical findings.
Pathologic criteria: one of the following two pathologic criteria are required for the diagnosis
of IE -
- direct evidence of endocarditis based upon histological findings
- positive Gram stain results or cultures of specimens obtained from surgery or autopsy.
Clinical criteria are divided into major and minor findings. The clinical diagnosis of
definitive IE require the presence of either two major criteria, one major and three minor
criteria, or five minor criteria.
Major criteria: blood culture positive for IE; Evidence of endocardial involvement
(echocardiogram positive for IE).
Minor criteria: predisposition, fever, vascular phenomena, immunologic phenomena,
microbiologic evidence.
Management. Three to five blood culture are drawn in succession over 24 or 48 hours,
unless the patients is very ill. In 90% of the cases, the causative agent is recoveres from the
first two culture.
Initial empiric therapy is started with following antibiotics wile awaiting the result of blood
culture
The usual initial regiment is an antistaphyloccal semisyntetic penicillin (nafcilin, oxacilin or
methicilin) and an aminoglycoside (gentamicin
127
If a methicilin-resistent S.aureus is suspected, vancomycin should be substitude for the
semisynthetic penicillin.
The final selection of antibiotics depends on the organism isolated and the result of an
antibiotic sensitivity test.
In general, a highly sensitive S.viridans can be successfully treated with IV penicillin for 4
weeks.
The drug of choice for staphylococcal endocarditis is one of the semisynthetic penicillinae-
resistant penicillin, given IV for 4 to 6 weeks. Vancomycin is used in patients allergic to
penicillins.
Enterococcus cause endocarditid usually requires a combination of IV penicillin or ampicillin
for 4 weeks and IV gentamicin for 2 weeks
HACEK organisms may have become resistant to ampicilin. A third-generation
cephalosporin, such as ceftriaxone, is generally recommended.
Amphotericin B is the most effective agent for most fungal infections.
Operative intervention may be necessary before the antibiotic therapy is complete if the
clinical situation warrants (e.g., progressive CHF, significant malfunction of prosthetic
valves, persistently positive blood cultures after 2 weeks therapy). Bacteriologic relapse after
an appropriate course of therapy also calls for operative intervention.
Prevention: Endocarditis prophylaxis is indicated only for certain cardiac conditions and
procedures: prosthetic cardiac valve, previous infective endocarditis, CHD, cardiac
transplantation
The antibiotic prophylaxis is given orally 1 hour before a procedure. It should not be started
several days before the procedure. Parenteral antibiotics are given within 30 minutes of
starting procedure.
for dental ( all dental procedures that involve manipulation of gingival tissue of the
periapical region of teeth or perforation of the oral mucosa), respiratory tract (for procedures
that involve incision or biopsy of respiratori mucosa, such as tonsillectomy and
adenoidectomy), or esophageal procedure are directed against Streptococcus viridans; for
genitourinary (GU) and gastrointestinal (GI) procedure (in patients with infected GI or GU
tract) are directed against Enterococcus faecalis (enterococci).
128
MYOCARDITIS
Myocarditis is an inflammation or degeneration of the heart muscle, usually secondary to
systemic infection
Etiology: myocarditis may be caused by an infectious agent, immune-mediate process,
collagen disease, or toxic agent. A cell-mediated immunology reaction, not merely
myocardial damage from viral replicatiom, appears important in viral myocarditis.
Infections: Viruses are probably the most common cause of myocarditis; adenovirus,
coxsackie viruses and echoviruses are the most common agents. Many other viruses (such as
poliomyelitis, mumps, measles, rubella, cytomegalovirus, HIV, arboviruses, adenovirus, and
influenza) can cause myocarditis. Rarely, bacteria, rickettsia, fungi, protozoa and parasites
are the causative agents.
Immune mediated disease: cut rheumatic fever, Kawasaki disease
Collagen vascular disease toxic myocarditis (drug ingestion, diphtheria exotoxin, and anoxic
agents)
Clinical manifestations
History of an upper respiratory infection may be present in older children. The onset of
illness may be sudden in neonates and small infants, causing anorexia, vomiting, lethargy and
occasionally circulatory shock.
The presentation depends on the patients age and the acute or chronic nature of the infection.
Typical cardiovascular examination includes: weak pulses, tachycardia, gallop rhythm distant
hear sound
The ECG may show any one or combination of the following: low QRS voltage, ST-T
changes ,prolongation of the QT interval, and arrhythmias, especially premature contractions.
Cardiomegaly on CXR films is the most important clinical signs in myocarditis
Echo studies reveal cardiac chamber enlargement and impaired LV function, often regional.
Occasionally, increased wall thickness and LV thrombi are found.
Cardiac troponin levels (-I and -T) and myocardial enzyme (creatine kinase [CK], MB
isoenzyme of CK[CK-MB]) may be elevated. Troponin levels may be more sensitive than the
cardiac enzyme. The normal value of cardiac troponin I in children is 2 ng/ml or less.
Radionuclide scanning (after administration of gallium 67 or technetium 99m pyrophosphate)
may identify inflammatory and necrotic changes characteristic of myocarditis. Myocarditis
can be confirmed by an endomyocardial biopsy.
Myocarditis may be a precursor to idiopathic dilated cardiomyopathy in certain patients.
129
Management
Treatment is directed at the underlying cause at controling symptoms of congestive heart
failure.
Bed rest and limitation of activities are recommended during the acute phase (because
exercise intensifies the damage from myocarditis in experimental animals).
Anticongestive measures include rapid-acting diuretics (e.g., furosemide or ethacrynic acid),
rapid acting inotropic agents (e.g., isoproterenol, dobutamin, dopamine), administration of
oxygen, and bed rest.
Digoxin may be given cautiously, using half of the usual digitalizing dose, as some patients
with myocarditis are exquisitely sensitive to it. An ACE inhibitor (e.g., captopril) may be
benefical in the acute obese.
Arrhythmias should be treated aggressively and may require the use of IV amiodarone.
Beneficial effects of high dose -globulin (2g/kg over 24 hours) have recently been reported
(with better survival an batter LV function by echo). A high dose of -globulin have been
reported to be effective in myocarditis secondary to Kawasaki disease.
The role of corticosteroids is unclear except for the treatment as sever rheumatic carditis.
PERICARDITIS
Inflammation of the pericardium may be primary, or a manifestation of more generalized
illness.
Etiology Viral infection is probably the most common cause, particularly in infancy.
Acut rheumatic fever is also a cause of pericarditis
Bacterial infection (purulent pericarditis). Commonly encountered are S.aureus,
Streptococcus pneumoniae, Haemophylus influenzae, Neisseria meningitis, and streptococci.
Tuberculosis (an occasional cause of constrictive pericarditis with insidious onset). Heart
surgery (postpericardiotomy syndrome). Collagen disease such as rheumatoid arthritis. A
complication of oncologic disease or its therapy including radiation. Uremia (uremic
pericarditis)
Pathophysiology Pathogenesis of symptoms and signs of pericardial effusion is determined
by two factors: speed of fluid accumulation and competence of the myocardium. A rapid
accumulation of a large amount of fluids or a slow accumulation of a small amount of fluids
130
in the presence of myocarditis can produce circulatory embarrassment. Slow accumulation of
a large amount of fluid may be well tolerated if the myocardium is intact.
With the development of pericardial tamponade, several compensatory mechanism are
called on: systemic and pulmonary venous constriction (to improve diastolic filing), an
increase in the SVR (to raise falling blood pressure), and tachycardia (to improve cardiac
output).
Clinical manifestations
The patients may have a history of upper respiratory tract infection. Precordial pain with
occasional radiation to the shoulder and neck may be presenting complaint. The pain may be
relieved by leaning forward and made worse by supine position or deep inspiration.
Pericardial friction rub is the cardinal physical sign. In children with purulent pericarditis,
septic fever (38
o
ti 41
o
C), tachycardia, chest pain, and dyspnea are almost always present.
Signs of cardiac tamponade may be present (distance heart sounds, tachycardia, pulsus
paradoxus, hepatomegaly, venous distension, and occasional hypotension with peripheral
vasoconstriction).
The ECG may show a low-voltage QRS complex, ST segment shift, and T wave inversion.
CXR films may show a varying degree of cardiomegaly. Water battle-shaped heart and
increased pulmonary venous markings are seen with large effusion.
Echo is the most useful tool in establishing the diagnosis of pericardial effusion and in
detecting cardiac tamponade.
Management
Pericardiocentesis or surgical drainage to identify the cause of the pericarditic is mandatory,
especially when purulent or tuberculosis disease is suspected.
Salicylates may be administrated for precordial pain in nonbacterial pericarditis and
rheumatic fever. Costicosteroid therapy may be indicated for children with severe rheumatic
carditis or postpericardiotomy syndrome.
For cardiac tamponade, urgent decompression by surgical drainage or pericardiocentesis is
indicated
Urgent surgical drainage is indicated when purulent pericarditis is suspected. Purulent
pericarditis is treated with an IV antibiotic therapy for 4 to 6 weeks.
Constrictive pericarditis
A fibrotic, thickened, and adherent pericardium restricts diastolic filling of the heart.
Although rare in children, it may be associated with earlier idiopathic or viral pericarditis,
131
tuberculosis, incomplete drainage of purulent pericarditis, hemopericardium, mediastinal
irradiation, neoplasic infiltration, or connective tissue disorders.
Diagnosis of constrictive pericarditis is suggested by the following clinical finding:
signs of elevate jugular venous pressure; hepatomegaly with ascites and systemic edema;
diastolic pericardial knock; calcification of the pericardium, enlargement of the SVC and the
A, and pleural effusion on CXR films; low QRS voltage, T wave inversion or flattening,
LAH, and atrial fibrillation on the ECG.
An M-mode echo may reveal two parallel lines representing the thickened visceral
and parietal pericardia or multiply dense echoes. Also, 2D echo show an immobile and dense
appearance of the pericardium
The treatment for constrictive pericarditis is complete resection of the pericardium;
symptomatic improvement occurs in 75% of the patients.
CONGESTIVE HEART FAILURE
Definition Hear failure is a clinical condition that results from impairment of the ventricle to
fill with or eject blood.
Pathophysiology and Etiology: Congestive heart failure (CHF) may result from congenital
or acquired heart diseases with volume and/or pressure overload or from myocardial
insufficiency.
CHD is the most common cause of CHF in children. The time of onset of CHF varies rather
predictably with the type of the defect.
The underlying pathophysiology mechanisms that lead to compromise of cardiac stroke
volume and heart failure include: increase afterload (pressure work), increased preload
(volume work), myocardial abnormalities, arrhythmias.
Ventricular pump dysfunction results in reduced ventricular contractility that lead to impaired
ejection of blood from the ventricle (cardiomyopathy, myocarditis, arrhythmias).
Volume overload with preserved ventricular contractility ( increased preload) resulting in
CHD is due to CHD with significant left-to-right shunt, or less commonly, valvular
insufficiency.
Pressure overload is due to CHD with severe ventricular outflow obstruction that impedes
ejection of blood from the hear resulting in inadequate cardiac output.
132
Clinical manifestations. The diagnosis of CHF relies on several sources of clinical findings,
including history, physical examination, and CXR film. Cardiomegaly is almost always
present on CXR film.
Poor feeding of recent onset, tachypnea, poor weight gain, and cool sweat on the forehead
suggest CHF in infants. In older children, shortness of breath, especially with activities, easy
fatigability, puffy eyelids, or swollen feet may be presenting complaints. Physical findings
can be divided by pathophysiologic subgroups.
1. Compensatory responses to impaired cardiac function: Tachycardia, gallop rhythm, weak
and thready pulse and cardiomegaly; CXR films are more reliable than physical examination
in demonstrating cardiomegaly. Signs of increased sympathetic discharges (growth failure,
perspiration, and cold wet skin.)
2. Signs of pulmonary venous congestion (left-side failure) include tachypnea, dyspnea or
exertion (poor feeding in small infants), orthopnea in older children, and wheezing and
pulmonary crackles.
3. Signs of systemic venous congestion (right side failure) include hepatomegaly and puffy
eyelids. Distended neck vein and ankle edema are nor seen in infants.
Cardiomegaly on CXR films is almost always present.
The electrocardiogram may be helpful in determine the cause. Sinus tachycardia is common.
Echocardiography can confirm the presence of chamber enlargement or impaired LV
function and determine the cause of CHF.
Management Elimination or correction of predisposing factors (e.g, fever, anemia, infection)
and treatment of underlying causes (hypertension, arrhythmias, or thyrotoxicosis), general
supportive measures and control of heart failure by inotropic agents, diuretics, afterload
reducing agents are the treatment goals.
Pharmacologic therapy: Improvement in symptoms can be achieved by inotropic agents,
diuretics, digoxin, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin II
receptor blockers (ARBs).
Prolongation of patient survival has been documented with beta-blockers, ACE inhibitors,
ARBs, and aldosterone antagonists. Improvement in LV function and reversal of LV
dilatation, LV remodeling with chronic use of ACE inhibitors, ARBs, and aldosterone
antagonists.
Rapidly acting inotropic agents (dopamine, dobutamine, milrinone) are used in critical ill
infants and children with CHF, in those with renal dysfunction; rapidly acting catecholamines
with a short duration of action are preferable to digoxin
133
Diuretics decrease preload by promoting natriuresis and provide relief of volume overload
symptoms. Patients with CHF often improve rapidly after a dose of fast-acting diuretic, such
as furosemide or acid ethacrynic. Side effects of diuretic therapy include hypokalemia, and
hypochloremic alkalosis; both may increase the likelihood of digitalis toxicity. Diuretic
almost always are used with inotropic agents.
Digoxin has a positive inotropic effect, a negative chronotropic effect that slow atrial
conduction, and vagotonic properties. Digoxin is used in all noncritical patients. The use of
digoxin is contraindicated in CHF caused by hypertrophic cardiomyopathy, complete heart
block, or cardiac tamponade. Therapeutic ranges of serum digoxin levels for treating CHF
are 0.8 to 2 ng/ml, levels obtained during the first 3 to 5 days after digitalization. A serum
digoxin level greater than 2 ng/ml is likely associated with toxicity if the clinical findings
suggest digital toxicity.
Afterload-reducing agents are popular because they can increase cardiac output without
increasing myocardial oxygen consumption. Reducing the afterload tends to augment the
stroke volume without change in the contractile state of the heart and therefore without
increasing myocardial oxygen consumption. These agents are usually used in conjunction
with digitalis glycosides and diuretics. In addition to myocardial dysfunction, patients with
CHF from large L-R shunts (such as VSD, AV canal, PDA) have been shown to benefit from
captopril. Angiotensin-converting enzyme inhibitors (captopril, enalapril) are accepted as an
important component of CHF therapy in children.
Beta-blockers counteract the maladaptive effects of chronic sympathic activation of the
myocardium. In adults with CHF they improve patient survival, reverse LV remodeling and
decrease myocardial fibrosis.
Nonpharmacologic interventions for advanced heart failure: positive pressure ventilation,
mechanical circulatory support in end-stage heart failure and heart transplantation.
Nonpharmacologic therapy for chronic heart failure. Nutrition- caloric intake and growth
should be carefully assessed. Some children may need a daily intake greater than 120kcal/hg
for optimal growth because of increased metabolic demands. In order to provide adequate
caloric intake, intermittent or continuous nasogastric or gastrostomy tube feeds may be
required. In addition, salt and fluid restriction is recommended in children with severe CHF
to reduce volume overload.
For patients with structural heart disease with preserved pump function, surgical or catheter-
based interventions are used to correct the underlying defects causinh CHF.
134
SHOCK
Definition. It is a plurietiologic, multipathogenetic clinical syndrome, characterized
haemodynamically by reduction in the tissue blood flow below a certain critical level
necessary for the normal metabolic processes. Therefore, the shock is determined mainly by
tissue perfusion deficit, independent of blood pressure value and can evolve with normal
blood pressure and a normal or increased cardiac activity.
Etiopathogenic classification of shock- table no. 16:
HYPOVOLEMIC SHOCK - decreased intravascular volume with decreased
venous return and preload
- Water and electrolyte loss: diarrhea, vomiting,
diabetes insipidus, renal losses, burns
- Hemorrhage: internal, posttrauma, post surgery
- Plasma loss: burns, nephrotic syndrome, peritonitis
DISTRIBUTION SHOCK - secondary to alteration of vascular tone through
vasoplegia marked decrease in the BP
- Anaphylaxis: antibiotics, vaccines, blood products,
local anesthetics, insect bites, food
- neurological injuries: head trauma, spinal cord injury
- early stage of septic shock: meningococcal
septicemia, staphylococcal, gram negative flora
- drugs: barbiturates, phenotiazidics, tranquilizers,
antihypertensives
CARDIOGENIC SHOCK - congenital or acquired heart disease
- MCC: hypoplastic left heart syndrome
- Primary cardiomyopathy: obstructive, degenerative
- acquired cardiomyopathy: infectious, toxic,
irradiation
- Congestive heart failure
- After cardiovascular surgery
- dysrhythmias
- obstruction: cardiac tamponade
SEPTIC SHOCK - occurs initially through vasogenic mechanism
subsequently associated with hypovolemic and
cardiogenic mechanism
- etiology: different depending on the age and
immune mechanism competence
- Newborn: beta-hemolytic streptococci gr. B,
Enterobacteriaceae, Listeria monocytogenes,
Staphylococcus aureus
- Infant: H. influenzae, Streptococcus pneumoniae,
Staphylococcus aureus
- Child: Streptococcus pneumoniae, Neisseria
meningitidis, S. aureus
- immunocompromised patients: S aureus,
135
Pseudomonadaceae, Enterobacteriaceae, Candida
albicans
DISSOCIATIVE SHOCK - severe anemia
- carbon monoxide poisoning
- methemoglobinemia
Pathophysiology
In all pathogenetic forms of shock, cardiac output is inadequate for the tissue needs due to
mismatches between the vascular bed and the blood volume.
hypovolemic shock: vascular bed is normal, but low volemia
cardiogenic shock: the circulating blood volume is low, while the vascular bed is
normal. Cardiac output is affected either due to ineffective diastolic filling (in the
context of dysrhythmias) or as a result of the serious compromise of myocardial
contractility (myocarditis or cardiomyopathy).
In cardiogenic shock, as a particular form of shock in pediatrics due to myocardial
insufficiency, venous stasis occurs with increased risk of acute pulmonary edema,
with systemic venous stasis, with increased central venous pressure (PVC).
Cardiogenic shock is a form of increased PVC shock congestive shock, and
therefore therapy will be conducted so that the patient will need only fluid and
electrolyte as maintenance, providing basic needs and treatment target remains the use
of vasoactive substances and inotropic medication.
vasogenic shock: total blood volume is normal, but the vascular bed capacity
is increased
These details are useful for therapeutic conduct.
Links involved in the pathophysiology of shock are:
reduced effective circulating volume
pump failure
hemodynamic disturbances in the microcirculation
decreased venous return
metabolic disorders
There are three stages in the shock evolution:
compensated stage: homeostatic mechanisms act to maintain perfusion of vital organs;
blood pressure, urine output and cardiac function are normal
- consequence of inadequate cardiac tissue needs leads to the onset of two
compensatory mechanisms needed to ensure proper circulation at myocardial
and cerebral levels:
136
a) centralization-by vasoconstriction in the kidney (oligoanuria
appears), mesenteric territory, liver, muscle, skin (vasoconstriction in the skin,
it is a cold shock) and is made through adrenaline, noradrenaline, renin and
angiotensin
b) penetration of interstitial fluid in the vascular bed - occurs due to
reduced hydrostatic pressure at capilary level.
decompensated stage: diminishes compensatory mechanisms
- If the shock-triggering cause persists, inadequate irrigation of tissues and inadequate
intake of oxygen in the cessl will cause vasoconstriction with vasodilatation replacement
(vasoplegia), increased capillary permeability (fluid moves to interstitium), activation of
disseminated coagulation with microthrombi formation in different organs and significant
reduction of the contraction ability of the heart. These changes announce decompensated
shock and are triggered by hypoxemia, acidosis, increased permeability of the digestive tube
to endotoxins, excessive formation of free radicals, activation of kinin pathways.
Final stage: compensatory mechanisms are compromised, evolution is progressive to exitus
Clinical presentation
General Signs: drowsiness, pale and cold teguments (except for septic shock), dry, often
cyanotic lips, sometimes nasal flare.
Neurological signs: dizziness to the stage of coma, general sensitivity diminished to coma,
diminished tendon reflexes
Cardiovascular signs:
- in the first phase of shock vasoconstriction predominates: tachycardia, blood pressure can
be normal due to increased peripheral vascular resistance;
- In final stages: deafness of heart sounds, tachycardia, abrupt fall in the blood pressure,
filiform pulse, colabation of shallow veins, cyanosis of extremities, mottled skin;
- when shock is associated with heart failure: jugular venous turgor
Respiratory signs:
- Initial phase: tachypnea, caused by stimulation of respiratory centers and by metabolic
acidosis. Hyperventilation causes increased CO2 elimination, stimulates vasoconstriction
(especially venous), improving venous return.
137
- In final stages: lung structural alterations with alveolar hypoventilation, hypoxemia and
hypercapnia: PaO2 <65mmHg, PaCO2:> 50mmHg
Digestive Signs: Although the shock causes digestive mucosal lesions, gastrointestinal
bleeding rarely presents digestive hemorrhages. Hepatocellular lesions: early alteration of
coagulation factors, cholestasis syndrome.
Renal Signs
- In the initial stages: signs of acute functional renal failure: oliguria, anuria, in relation to the
degree of renal ischemia
- In the late stages: acute renal organic failure: acute tubular necrosis
Diagnostic explorations table no. 17:
Blood Urine Other investigations
- CBC
- ionogram
- glycemia
- urea, creatinine
- Astrup
- lactic acid
- BT, BD
- procalcitonin
- amilazemia
- GOT, GPT, GGT
- hemostasis: PT and
aPTT
- hemoculture
- urine summary
- urine culture
- Thoracic X-ray
- thoracic, abdominal,
cerebral CT
- Marrow MRI
- coproculture
- toxicologic tests
- ECG
- ecocardiography
Invasive investigations:
- Invasive blood pressure monitoring
- Determination of PVC (catheter placement in an intrathoracic vein, normal values:
4-8 cm water). Determination of PVC provides information on right atrial venous return
(preload), and the cardiac contractility. A high PVC shows either a relative hypervolemia or
cardiac decompensation, or both. In such situations administration of fluids is not
recommended, rather cardiac tonics in order to increase the cardiac output.
138
Table no. 18. Medical monitoring
Clinical Admission 10
min
30min hourly o Paraclinical
FC HLC
FR ASTRUP
SaO2 Serum ionogram
BP Urea, creatine
Diuresis Glycemia
Caplillary reload
time
Neurologic status
Rectal, skin
temperature
Diagnosis :
Diagnosis of the state of shock and the evolutionary phase (compensated,
uncompensated, final) is defined by clinical criteria and listed diagnostic explorations and
etiopathogenetic form on the clinical context in which the shock installed.
Early diagnosis of shock requires a high degree of suspicion and knowledge of the
conditions that predispose children to shock. The childs age can provide the diagnosis key in
conditions such as congenital heart disease, cardiac surgery, immunodeficiency states,
ingestion of certain substances or recent traumatic history raise the suspicion of shock in
children.
Treatment
The treatment is applied according to the etiology of shock and its evolutionary stage
and consists of a complex of therapeutic measures aimed at:
- Removal of the shock-producing factor
- Pathogenetic chain termination by removal of main pathogenetic factors
- Correction of metabolic disorders
In the first hour from the onset of shock, emergency measures to be taken are:
- Ensuring higher permeability of superior air pathways
- O2 administration by mask or in some cases assisted ventilation (positive pressure
ventilation)
- Installation of catheter for PVC monitoring
139
- vascular access should be rapidly established, if intravenous approach fails, then
intraosseous approach is indicated. Vascular access makes it possible to correct volemia
through fluid volume expansion.
1. Treatment of hypovolemic shock:
a. volemia correction through fluid administration:
i crystalloid solution (9%0 NaCl or mixture of NaCl 9%0 and 5% glucose 0),
20ml/kgb in the shock with acute dehydration
ii. isogroup blood, izoRH, 10-20ml/kgb in acute dehydration
iii. fresh plasma: 10-20ml/kgb if any sign of CID
iv. colloidal solutions: dextran, albumin, 20ml/kgb
b correction of acidosis and hypocalcaemia:
i antiacid solution: Na bicarbonate, THAM if pH <7.2, the amount of 1-
2mEq/kgb or the formula: base deficit x W (kg) x 0.3, administering half the
amount resulting from the calculation , mixing equal parts with sol.of Dextrose
5% in a period of 2 hours
ii. hypocalcemia: CaCl2 10% 10-20mg/kgb slowly infused (Do not mix Na
bicarbonate)
The amount of liquids and the rhythm of administration are determined by
clinical criteria (BP, pulse, recoloring, appearance of rales, gallop rhythm,
hepatomegaly, increased respiratory effort), and more precisely, according to
the monitoring of PVC.
c. Other therapeutic measures:
i management of hypoxia by oxygen therapy
ii. maintaining the patient temperature around 36.5 to 37.2 degrees C
iii. management of neurological signs by improving cerebral perfusion
iv. prevention and treatment of CID by coagulation factors (fresh blood, fresh plasma),
heparin 25UI/kgb/h when coagulation factor intake does not affect CID
After volume expansion, fluid administration continues for the correction of losses produced
after initiation of rebalancing and physiological needs.
1. Treatment of distribution shock :
Treatment of anaphylactic shock :
140
i. applying tourniquets where allergen inoculation occurred at limb level
through sc, im injection, insect bites (applied above the inoculation site
)
ii. placing the patient in Trendelemburg position to prevent ischemia and
irreversible brain damage
iii. Adrenaline - of choice in anaphylactic shock , sc, im , iv
administration in doses of 0.1 mg / kgb (max 0.35 ml ) of solution 1:
1000 it can be repeated at 20min. If allergen inoculation was by
injection or insect bites, first administration is in place of inoculation to
restrain antigen resorption and release of chemical mediators . If after
repeated administration of Adrenaline, BP does not increase,
Noradrenaline can be administered.
iv . volume liquids: colloidal solutions , if after the initial adrenaline ,
followed by Noradrenaline, BP does not increase
v. Oxygen
vi . Miofilin ( 5-6mg/kgb ) - in cases with severe bronchoconstriction ,
where bronchospasm has not responded to the administration of
adrenaline and hydrocortisone hemisuccinate
vii . Antihistamines - with secondary importance in anaphylactic shock
( Claritin , Ketotifen , Romergan , Feniramin , Tavegyl )
viii .tracheostomy in case of asphyxia in patients with acute laryngeal
edema , followed or not by mechanical ventilation
2. Septic shock treatment :
i. antibiotice conform antibiogramei germenilor izolai prin hemoculturi,
uroculturi sau culturi din alte produse biologice
ii. antibiotics according to the antibiogram of germs isolated by blood
cultures, urine cultures and cultures of other biological products
iii. volume expansion according to PVC (whole blood, colloid and
crystalloid solutions)
iv. vasoactive-inotropics where fluid administration does not correct BP;
Dopamine, Norepinephrine, isoproterenol
v. Oxygen-therapy
vi. corticosteroids when adrenergic function is impaired when, as in the
Waterhouse-Friderichsen syndrome
141
vii. Naloxone, an antagonist of epinephrine effective in septic shock
viii. correction of acidosis: Na bicarbonate
ix. Surgery: removal of the source of infection (where surgical approach is
possible), but only after 24 hours of intensive treatment
3. Treatment of cardiogenic shock : addresses the essential pathogenetic links of
cardiogenic shock: pump failure, hypovolemia and changes in vascular resistance
a. fluid infusion: to control volume expansion (counterindicated in hypervolemic
form with PVC> 20cmH2O). NaCl9%0 5ml/kg bis indicated in 30min or
colloids. Fluid administration is mandatory in cases of cardiogenic shock with
acute pulmonary edema associated with PVC <5cmH2O, noting that volume
overload should be avoided
b. Vasoactive inotropics - indicated after volume expansion, if the deficit of tissue
perfusion is maintained or signs of heart failure are present, except for
dysrhythmia or tamponade.
Dopamine is the agent of first choice, natural precursor of adrenaline, with
Vasomotor effects that vary by dose: low doses 1-6 mcg / kg / min, have an effect on
beta and delta receptors, causing renal and mesenteric vasodilation and reduce
afterload . Middle doses of 6-12 mcg / kg / min, have an effect on beta receptors,
increasing the capacity of contraction of the heart, and high doses> 12 mcg / kg / min
have an effect on alpha-and beta receptors, maximum inotropic and peripheral
vasoconstrictor effect, in which case association of vasodilator medication is
recommended.
Other vasoactive inotropic agents: Dobutamine, Isoproterenol,
Epinephrine, Norepinephrine, Na nitroprusside, Nitroglycerin
c. -adrenergic blockers-indicated in cases evolving with intense vasoconstriction
and increased total peripheral resistance, or the administration of Dopamine is
not followed by signs of improvement in tissue perfusion. Phentolamine
(Regitine) at a dose of 0.5-1mg / kgb/24ore iv infusion. If the shock condition
persists or worsens under Phentolamine treatment, Epinephrine is added.
d. Digitalis-management involves risks to children electrolyte disturbances, heart
failure, acid-base disorders, compromised renal function. Along with medication
administration, acidosis, hypoxia, diselectrolitemia, anemia, are corrected.
4. Support treatment
142
a. coagulation abnormalities: may increase hypoperfusion regardless shock
etiology. Monitoring of prothrombin time, partial thromboplastin time, platelets
is necessary. Therapy is aimed at correcting specific coagulation factors. The use
of vitamin K, fresh plasma and platelet transfusion corrects most coagulation
imbalances.
b. gastrointestinal complications: hemorrhages and ileus. Ileus, resulting from
fluid and electrolyte disorders, produce abdominal distension with impaired
respiration. Gastrointestinal bleeding can be prevented by administration of
antacids and / or H2 receptor blockers (omeprazole).
c. Renal support: to prevent acute renal insufficiency, increased circulating
volume, diuretics (mannitol, furosemide). 3-5microg/kgb/min doses of
Dobutamine increase renal flow with beneficial effect in the prevention of acute
renal failure in shock.
d. respiratory support: increasing the amount of oxygen, tracheal intubation
opportunity to improve hypoventilation and hypoxia
Shock treatment is multifactorial. Therapy should be assessed for each stage and
for each type of shock
143
CHAPTER IV COLAGENOSES
Asist. Univ. dr. Grama Alina Corina, Conf. Univ. Dr. Mrginean Oana
INTRODUCTION
Definition: chronic diseases including a heterogeneous group of clinical and pathologic states
that share inflammatory structural changes of the connective tissue throughout the body,
mainly in the blood vessel walls.
There are multiple collagenous diseases: Systemic lupus erythematosus, scleroderma,
Periarterita nodosa, juvenile idiopathic arthritis, Acute articular rheumatism, Vasculitis:
Henoch Sconlein purpura, Wegener granulomatosis, Churg-Strauss Syndrome; Polyarteritis
nodosa, Kawasaki disease, Takayasu arteritis.
Etiology: unknown.
Pathogeny: probably due to body background in each of these conditions there is an
inadequate response to infection, stress and hormonal changes, conducting to the production
of autoantibodies and immune complex formation.
- trigger causes remain a mystery
- primary pathologic immune event initiating the inflammatory vascular disease cannot
be identified in most of the cases
- proinflammatory cytokines involved in the immunologic process include: gamma
interferon, IL 1,2,6,8, tumor necrosis factor (TNF), platelet-growth factor (PDGF),
and the involved cells are macrophages, neutrophils, endothelial cells, Ly T, B, NK,
fibroblasts, smooth muscle cells, platelets
- vascular endothelium has an important role in: hemostatic equilibrium, achieving
vascular tone, vascular inflammatory reactions.
Immuno-pathological mechanisms characterize each type of collagenosis differently:
- formation of pathogenic immune complexes: Henoch Sconlein purpura vasculitis
associated with collagen diseases,
- production of endothelial anticell antibodies: Kawasaki disease,
- production of anti-neutrophil citoplasmic antibodies (ANCA): Churg-Strauss
syndrome, Wegener's granulomatosis,
- pathogenic response of Ly T (CD4 +) and granuloma formation: Kawasaki disease,
Takayasu arteritis, Wegener's granulomatosis.
144
Positive diagnosis of colagenosis is difficult to establish because there are specific clinical
and laboratory criteria. Polymorphic profiles exist in colagenoses and any organ can actually
be affected in any type of colagenosis.
Clinical symptoms are uncharacteristic, realizing various profiles with fever, leukocytosis,
accelerated erythrocyte sedimentation rate, arthralgia, rash. The diagnosis should always be
done by excluding other conditions that could present the same symptoms.
Laboratory
1. Routine tests:
- blood count - ESR
- C-reactive protein - Creatinine, Urea
- liver and muscle enzymes (SGPT, SGOT, CPK, aldolase)
- Protein electrophoresis - Urine test
- Test for occult bleeding - Chest Rx, chest CT, MRI
2. Serologic tests:
- Immunoglobulins - rheumatoid factor
- LE Cells - AAN's
- immune complexes - Complement and complement fractions
- Cryoglobulins - Tests for hepatitis B, C, CMV, EBV
- "gold standard": ANCA-c (proteinase 3), ANCA-p (myeloperoxidase)
3. Analytical tests for determining proinflammatory factors endothelial products
- Il-1,2,6,8, TNFo
- VCAM-1 (vascular adhesion molecule)
- ICAM-1 (intercellular adhesion molecule)
- MCP-1 (monocyte chemotactic protein)
- E Selectin
4. Other tests: Angiography, Ultrasound, skin biopsy, scintigraphy with Th / Tc
ACUTE ARTICULAR RHEUMATISM
(AAR, rheumatic fever, Bouillaud rheumatism)
Definition : Systemic inflammatory disease of the connective tissue that occurs as a result of
an infection with group A beta-hemolytic streptococci, mainly affecting the heart, joints and
nervous system, with recurrent development in bursts and self-limited character.
145
Etiology: the causative agent is the beta-hemolytic Streptococcus group A :
Obligatory faringian location (premonitory angina followed by a period of asymptomatic
latency, lasting 1-5 weeks)
Not all serotypes can cause the disease
The most common serotypes isolated from AAR patients: Type M(1,3,5,6,14,18,19,24)
Streptococcal skin infection is NOT associated with AAR
The epidemic of streptococcal pharyngitis in communities (schools, boarding schools)
can cause AAR peaks.
Predisposing factors:
- background (there is a familial predisposition)
- season (most commonly occurs in winter and spring)
- climate (temperate zone)
- living conditions (overcrowding, socioeconomic standard: it is considered "a poverty-
specific disease")
Pathogeny
The link between Streptococcus group A beta-hemolytic infection in the upper respiratory
tract and cardiac and joint lesion production is still unclear.
- Cytotoxicity theory
- Enzymes (streptolysin O) can produce injuries on experimental models: animals
- Can not explain the latency between infection and organ damage
- Immunological theory is supported by :
- High antigenicity on streptococcus surface
- Reproduction of the experimental model by using antigens (protein M1, M5, M6,
M19)
Morphopathology: evolving inflammatory AAR process has four phases: Mucoid, fibrinoid
stage, granulomatous and scarring phase.
Clinical manifestations:
Onset
- Sudden - febrile arthritis or
- Insidious: asthenia, fever, pallor, malaise, weight loss
The state period is characterized by presence of isolated or various combinations of the
following five major symptoms:
1. Arthritis (polyarthritis)
146
- often febrile, migratory, asymmetric
- includes large joints: knee, ankle, elbow, radio-carpal, shoulder
- celsiene signs are present: redness, swelling
- pressure and movement pain, improving on local heating
- it is not accompanied by radiographic changes and leaves no sequelae.
2. Carditis
Essential for the diagnosis:
- occurrence of an organic murmur (apical systolic, diastolic basal, apical mezodiastolic)
- friction or pericardial effusion, radiologically-confirmed cardiomegaly, endocarditis,
myocarditis, pericarditis, generally pancarditis
- common symptoms
tachycardia deafness of heart sounds
cardiomegaly congestive heart failure: acute pulmonary edema
Consequences: Progressive valve disease.
3. Coreea (Coreea minor, Sydenham disease)
- more common in girls, at about 3 months after streptococcal infection
- remitted within weeks, sometimes years
- emotional lability, abnormal behavior, mental instability
- lack of movement coordination
- reduced school performance
- facial grimacing exarcebate by stress and disappear in sleep
- requires neurological examination
4. Leiner marginated erythema
- is a nonpruriginous erythema, with severe lesions with circular edges and clear central
area
- appears on the trunk and limbs, never on the face
- can occur in waves, over a period of weeks and exacerbates with heat.
5. Meynets subcutaneous nodules (rheumatic)
- hard, mobile, painless, nodules
- placed on the elbows, back of the hands and feet
- up to 2 cm in size
- are fugitive
Laboratory: evidence of streptococcal infection is required
147
- ASLO - positive a few weeks after streptococcal infection
- ESR, C-reactive protein, alpha-2-globulin - certify inflammation of conjunctive tissue
- Blood count - no diagnostic value
- chest Rx
- EKG, echocardiogram
Positive diagnosis : based on amended Jones criteria (table.no.16)
Table 19 Allen Jones criteria
Major criteria (M) Minor criteria (m)
Evidence of
streptococcal infection -
obligatory criterion (O)
Carditis
Poly (arthritis)
Coreea
Marginated erythema
Subcutanous nodules
Fever
Arthralgia
Presence of acute phase Reactants
(ESR, CRP)
Prolonged PR interval on the ECG
Scarlet fever history
Positive throat swab
Positive ASLO
Positive diagnosis is based on:
2M + O
1M + 2m + O
When neither of the above equations is the case but there are minor criteria and evidence of
streptococcal infections, we have minor post-streptococcal syndrome (MPSS).
Differential diagnosis:
a. When arthritis is present:
- rheumatoid Arthritis
- Reactive arthritis (Shigella, Salmonella, Yersinia)
- Serum disease (history data are important)
- Siklemia (rare in our country)
- Malignancies (osteosarcoma, acute lymphoblastic leukemia)
- SLE
- Lyme disease (borreliosis)
- Gonococcal infection (in older sexually-active children)
b. When differential carditis is made by:
- viral myocarditis - viral pericarditis
148
- infective endocarditis - Kawasaki disease
- MCC - mitral valve prolapse
c. Coreea imposes differential diagnosis with the following diseases:
- Coreea Huntigton - Wilson disease
- SLE - cerebral palsy, brain tumors
- tics - hyperreactivity
- encephalitis
Evolution: AAR is a self-limited disease, flare-ups heal spontaneously in 8-12 weeks,
actually within the treatment period.
Treatment:
1. Absolute rest in bed 2 to 3 weeks, followed by another 2-3 weeks of relative rest
- in case of articular forms, school activity will be resumed
- in cardiac forms, rest is extended to 8-12 weeks and school activity will begin after 16
weeks
2. Careful cardiologic monitorization
3. Antibiotherapy after the diagnosis is made and streptococcal infection is confirmed :
- Penicillin G 1.2-1.8 million U/ day injection at 6 hours, for 10 days
- Erythromycin, 40 mg/ kg/ day po at 6 hours, Clarithromycin 15 mg/ kg/ day, 2 doses
for 10 days (in case of an allergy to penicillin)
- a single dose of benzathine penicillin i.m.
4. Anti-inflammatories: salicylates and cortisone
- Aspirin 100 mg / kg / day divided into 4 doses for 7 days, and 75 mg / kg / day for 4
weeks
- Patients with carditis and/or cardiomegaly will be treated with cortisone
Prednisone 2 mg / kg / day divided into 4 doses for 2-3 weeks, then
a. Withdrawal: 5 mg/24h at 2-3 days
b. At this point will be associated with aspirin at a dose of 75 mg / kg / day divided
into 4 doses for 6 weeks
c. In congestive heart failure: fluid restriction, digoxin, diuretics, oxygen.
5. Coreea treatment symptomatic
- Fenobarbital 2-3 mg/kg/dose at 8 h po
- Haloperidol 1 mg/kg/24h, divided in 2-3 doses
- Diazepam 0,1-0,5 mg/kg/day in 3-4 doses
6. SPSM treatment
149
- Anti-infective treatment with penicillin is identical to AAR
- Treatment with aspirin is enough for 4 weeks
- Streptococcus prophylaxis lasts 1 year.
7. Prophylactic treatment
a. Prophylaxis of the first AAR attack:
- correct treatment of scarlet fever
- correct treatment of streptococcal angina
b. Prophylaxis of AAR relapses (American Academy of Pediatrics, Red Book, 2006) aimed
at preventing streptococcus and lasts at least 5 years after acute flare-up:
Benzatinpenicilin im 1x/month
- AAR with confirmed carditis, ecocardiography without heart valve lesions, 10 years
- AAR residual valvular lesions with heart ecocardiography confirmation, until the
patient is 40 years old.
JUVENILE RHEUMATOID ARTHRITIS (JRA)
Definition: chronic inflammatory disease of the connective tissue, of unknown etiology,
occurring frequently in childhood (<16 years), clinically characterized by painful and
swelling joints, functional impotence, extraarticular systemic manifestations, lasting 6
weeks and pathologically by chronic infiltrative-proliferative inflammation of the chronic
synovitis type. Option for the current JRA name is the result of consensus reached in 1997 at
the ILAR Congress (International League Against Rheumatism) from Duban (South African
Republic).
Disease etiology is unknown.
Pathogeny: we can speak of a specific immunological susceptibility and the existence of
trigger factors :
- External trigger: viruses - EBV, parvovirus B19, rubella, bacteria - Listeria
monocytogenes, some types of Mycoplasma
- Host hyper-reactivity to its own antigens
- LyT Hyper-reactivity to bacterial infections
- Genetic predisposition : HLA-DR4 (polyarthritis), HLA-DR5, HLA-DR8 (oligoarthritis)
Aspects of the inflammatory process are manifested through :
- congestion, edema on the internal surface of the synovium, necrosis and fibrosis of
the superficial synovial layer
150
- granulation tissue, multiplication and increase in volume of synovial cells
- subchondral osteolysis, resulting in: destruction of cartilage, ankylosis and joint
deformities.
Clinical manifestations:
The onset may be:
- Insidious (common): articular manifestations (especially small joints of the limbs,
numbness, swelling of soft parts, morning joint stiffness) and general : asthenia,
fatigue, low grade fever
- superacute (especially in infants and small children) : affected general condition,
fever
- atypical (rarely) : arthralgia with local inflammatory signs, often monoarticular
arthralgia
Juvenile rheumatoid arthritis diagnosis during the onset can sometimes be extremely difficult
because of the initial symptomatic polymorphism.
Clinical forms:
I. Systemic form (Still's disease) more frequent in males and young ages (1-3 years)
characteristic: discrepancy between general extra-articular manifestations and scarcity of
articular ones (occurring late)
General manifestations :
- prolonged fever, septic aspect responding to cortisone treatment
- erythematous rash - nonpruritic maculopapular elements in various locations, except
the face, fugitive nature
- Koebner phenomenon: new lesions appearing in minor superficial injuries or after
bath
- moderate adeno-hepato-splenomegaly
- pleuritis, pericarditis, myocarditis, encephalitis
- neurological symptoms (seizures, psychotic disorders)
Joint manifestations (polyarthritis) may occur 4-6 months after the onset of the general
ones, making it difficult to diagnose the disease in the early stages (joint-radiocarpal,
tibiotarsal, knee)
II. Pauciarticular form (oligoarticular)
- affects 1-4 large joints (knees, ankles, hands, hip), asymmetric, moderate severity
- general signs (fever, hepatoslenomegaly) if existing, they are not severe
151
- major evolutionary risk is represented by the chronic iridocyclitis
- monoarticular impairment raises issues of DD with bacterial arthritis
III. Polyarticular form :
- articular manifestations that occur early in any joint ( 5 joints affected) except
vertebral dorso-lumbar joints
- morning stiffness, important joint deformity
- presence of rheumatic nodules on the extensor of the elbow
- rare extra-articular manifestations
- FR positive and FR negative forms (forms are either HIV (+) or HIV (-) on the
onset and do not change in the course of the disease)
IV. Enthesitis-associated arthritis :
- occurs more frequently in boys over 8 years old, 50% of cases being HLA-B27 positive
- Arthritis affects large joints (hips, knees, shoulders), lumbar spine, sacroiliac joints
- associated with enthesitis
- eye impairment occurs in 10% of cases, being of acute type - Previous acute uveitis
V. Psoriatic form
- in 5% of cases, patients may develop: arthritis, psoriasis, dactylitis, nail abnormalities.
Laboratory and paraclinic examinations:
- CBC: hypochromic anemia, leukocytosis, thrombocytosis
- Acute phase reactants: ESR, CRP, fibrinogen, alpha 2 globulin - especially in systemic
forms
- Rheumatoid factor present in HIV-positive polyarticular forms
- Antinuclear antibodies (ANA)
- Seropositivity is associated with chronic uveitis.
- Other examinations :
bone radiography: osteoporosis, periostitis, periarticular soft tissue swelling
subsequently subchondral erosions, joint space narrowing (stages I-IV of articular
manifestations)
joint puncture + cytology, biochemistry and immunologic examination of the joint
fluid (rarely indicate and contribute to septic arthritis DD)
Positive diagnosis :
- based on clinical findings, laboratory data and exclusion of other diseases (required AAR
and Lupus erithematosus)
152
- the following criteria are used in the absence of specific tests:
- time!!!- Persistence of mono / polyarthritis > 6 weeks (3 months, according to other
specialists) if other diseases had been excluded;
- leukocytosis, anemia, elevated ESR, positive acute phase reactants (fibrinogen, CRP)
nonobligatory;
- presence of "rheumatoid factor" (anti--globulin autoantibodies emphasized through
Latex and Waler-Rose test), present especially in polyarticular forms, with prognostic
role (HIV forms - most severe);
- presence of antinuclear antibodies, especially in cases of chronic iridocyclitis
- synovial fluid extracted by puncture is yellow-green, turbid, of low viscosity with 10-
50.000/mm3 leukocytes (about 75% polymorphonuclear)
- initial X-ray examination shows edematous soft tissues, osteoporosis without erosive
joint changes
Differential diagnosis with other arthritis :
- Reactive arthritis : acute nonsuppurative inflammatory arthropathy, sterile, appears
after a distant infection in people with a certain genetic predisposition: digestive
infection with Salmonella, Shigella, Yersinia or genital infections Chlamydia
- Osteomyelitis
- Autoimmune hepatitis
- Lyme disease (borreliosis)
- Legg-Calve-Perthes Disease
- Inflammatory bowel disease
- Acute lymphoblastic leukemia, TBC
- Lupus erithematosus, Schonlein Henoch purpura
- Joint Injuries
Treatment: The proposed objective is to achieve medication-based remission with minimal
risk of adverse effects; multidisciplinary team!!!
1. Hygienic-dietary treatment:
- normocaloric, normoglucidic, normoprotidic diet
- in case of corticotherapy: further restriction of sodium and supplement of protein,
potassium, calcium and vitamin D3
- physical exercises as tolerated by the patient.
2. Etiologic treatment not known
153
3. Pathogenic treatment
NSAIDs 4-6 weeks: Aspirin, Ibuprofen, Diclofenac, Indomethacin, Piroxicam
(attention to adverse effects) intraarticular triamcinolone hexacetonid
steroidal anti-inflammatory only in systemic forms, chronic iridocyclitis and
NSAIDs-resistant forms
Methotrexate (MTX) - 10-15 mg/m
2
/week administered orally or parenterally, the
therapeutic benefit is evident after 3-4 weeks, maximum response is achieved only
after 3-6 months of treatment
Cyclosporin A is used in the systemic forms of JIA that are resistant to MTX
treatment
Etanercept (Enbrel)
- antagonist of tumor necrosis factor produced by recombinant DNA technology is
indicated in severe forms of systemic JIA / polyarticular refractory to MTX
treatment or in the presence of corticosteroid-related toxicity with prolonged
administration of high doses
- 0.4 mg / kg sc 2 times/ week, alone or in combination with MTX
- response is observed in 2 weeks - 80% of children with polyarticular onset have
favorable response
- demonstrate outstanding benefits
- the only approved biologic agent and covered by a national program of CNAS,
Etanercept does not guarantee remission in all cases
4. Balneophysiotherapy and kinesitherapy important as an adjunct to preserve joint
movement, maintain joint force
5. Surgical: in pauciarticular forms not responding to conservative therapy
6. Psychotherapy: as optimal as possible integration of the patient in his environment,
social security in order to ensure compliance to treatment.
Evolution is unpredictable, with exacerbations and remissions for many years :
- polyarticular forms have prolonged development, HIV forms are frequently
accompanied by disability, the sero-negative can have better evolution;
- oligoarticular forms in children under 6 years will develop chronic uveitis;
- systemic forms are difficult to control.
Complications: rare but severe - ankylosing joints, growth retardation, skeletal deformities,
cecity (due to chronic iridocyclitis), psychological complications
Prognosis factors of reserved prognosis :
154
- active systemic disease at 6 months after onset
- polyarticular onset or development
- female
- positive Rheumatoid factor, positive antinuclear antibodies
- tenosynovitis, subcutaneous nodules
- early impairment of small joints of the hands and feet
- rapid emergence of joint erosion.
Bibliography :
1. Arion C., Dinu B. Boli inflamatorii sistemice n Ciofu E., Ciofu Carmen Pediatria Tratat, Ed. Medical, Bucureti,
2001, p. 948-971
2. Man Sorin C., Nanulescu Mircea V. Pediatrie practic, Ed. Risoprint, Cluj-Napoca, 2006, p. 513-530
3. Militaru Andreea - Artrita juvenil idiopatic n Nanulescu M. - Protocoale de diagnostic i tratament n pediatrie,
Ed. Medical Amaltea, Bucureti, 2013, p. 321-326
4. Miller L. Michael, James T. Cassidy Rheumatic Diseases of Childhood n Kliegman R.M., Behrman R.E., Jenson
H.B. et al (eds) - Nelson Textbook of Pediatrics, 18
th
edition, Saunders Elsevier, Philadelphia, 2007, p. 995-1052
5. Miller L. Michael - Approach to the Child with Joint Pain, but Normal Physical Examination, 2006
6. Muntean I. - Vademecum de Pediatrie, Ed. Medical, Bucureti, 2007, p. 375-388
7. Popescu V. Algoritm diagnostic i terapeutic n pediatrie, vol I, Ed. Medical Amaltea, Bucureti, 1999, p. 715-
724
8. Popescu V. Algoritm diagnostic i terapeutic n pediatrie, vol II, Ed. Medical Amaltea, Bucureti, 1999, p. 690-
702
SCHNLEIN-HENOCH PURPURA
Definition: immune vasculitis, with peak incidence between 4-15 years, with skin, joint,
abdominal and renal determinations by affecting small arterioles and capillaries.
Etiology: Unknown; the disease may occur secondary to a bacterial infection (streptococcal),
viral (measles, hepatitis), after some foods (milk, eggs, chocolate), drugs (penicillin, aspirin),
stinging insects.
Pathogeny: generalized vasculitis of arterioles and capillaries with <2 mm diameter,
produced by immunological mechanisms similar to those of collagenoses (in lupus
erythematosus and periarterita nodosa only arterioles are affected).
Clinical manifestations: the onset may be slow or acute in 50%, by fever or low grade
fever, headache, malaise, abdominal pain. State period is marked by four different clinical
manifestations (skin, joints, abdominal, renal) that may either occur all or in various
combinations.
1. Skin manifestations
155
- urticariform petechial maculopapular layout with hemorrhagic center not disappearing
under pressure (hemorrhagic purpura)
- hemorrhagic center can be the size of a pin to that of a pea and evolve gradually from red
to pale
- purpura is present in all cases, symmetrically on extremities, especially on ankles and
buttocks, around the knee joints and external faces of the limbs
- purpura is "palpable" as opposed to the ITP
2. Joint manifestations: appear in 2/3 of the patients and affect one or more joints
- ankle and knee joints are most commonly affected as polyarthralgias
- the joint may be swollen, warm and painful to movement (arthritis), sometimes with
synovial collection
- joint symptoms usually disappear within a few days
3. Abdominal manifestations (Henoch form)
- abdominal cramps
- vomiting
- occult bleeding or melena
- sometimes haematemesis; due to edema and bleeding in the gut wall, invagination or
bowel perforation may sometimes occur
4. Renal manifestations: occur in 20-50% of cases and are crucial for prognosis;
- may occur in the first week of illness or late
- micro or macroscopic hematuria cylindruria
- proteinuria
- rarely, oliguria, edema, nitrogen retention, hypertension and nephrotic syndrome
A. Laboratory
- leukocytosis, accelerated erythrocyte sedimentation rate, posthaemorrhagic
anemia
- changes in urinary disorders: hematuria, albuminuria, leucocyturia
- occult hemorrhages in stool
- hypoalbuminaemia in severe forms
- -hemolytic streptococcal (+) in throat swab, incresed ASLO
- tourniquet test (+) in 25% of cases
B. Positive diagnosis: is based on clinical manifestations in conjunction with normal
hemostasis tests.
C. Differential diagnosis
156
- purpura may be mistaken for that of ITP but in this case the platelet count is low
- joint manifestations will differ from those in the AAR, JRA
- abdominal pain requires differential diagnosis with other causes of acute abdomen
(cecal colic, invagination, intestinal perforation)
- renal manifestations will differ from those of AGN (acute glomerulonephritis),
especially the poststreptococic type
D. Treatment
Hygienic dietary measures
- Bed rest and regular, light food - 3-6 weeks while the disease heals; if renal
manifestations prevail, AGN diet is adopted.
- If the -hemolytic streptococcus is present in the pharyngeal exudate or ASLO titre is
increased, penicillin G 50-100000 U / kg / day is administered for 10 days.
Treatment
Most cases receive only symptomatic treatment:
- for edema, fever, rash
- Arthritis - Aspirin 100 mg / kg (alleviates joint phenomena)
- antihistamines
- capilarotrofic
- sedatives
Corticotherapy:
- In renal forms, especially when hematuria is persistent, low doses of heparin and
prednisone are administered for 3 weeks
- When abdominal colics are in the foreground, a short cure (about 7 days) of
prednisone (1-2 mg / kg / day) is administered; prednisone reduces swelling and the
intestinal hemorrhage and thus prevents intestinal invagination.
Immunosuppressive therapy: in case of persistent nephritis
Anticoagulants and immunosuppressives: in installed purpuric nephropathy
Evolution and prognosis: in most cases the evolution is favorable, the disease heals within
3-6 weeks. There are cases with 1-3 episodes of purpura; the disease can evolve with periods
of remissions and exacerbations.
In some cases the disease can take months and years.
Overall prognosis is excellent; one third of the cases have a recurrence within the first 6
weeks. Prognosis depends on renal involvement; sometimes cases may develop for months or
years leading to chronic glomerulonephritis.
157
KAWASAKI DISEASE (KD)
Synonyms: cutaneous-mucous lymphadenopathy syndrome, infantile polyarteritis nodosa
Definition: febrile vasculitis affecting the coronary vessels with propensity.
KD is found worldwide. Asian populations are at increased risk of developing the disease.
The peak incidence is between 9-12 months, and 50% of cases occur under the age of 2 years.
Epidemiology:
Japan: incidence: 100/100.000/year children under 5 years; bimodal seasonality: January and
June
Taiwan: Incidence: 66/100.000/year children under 5 years
USA: Incidence 17-18/100.000 children under 5 years
UK: Incidence: 5.5 / 100,000 children under 5 years
Diagnostic criteria
Fever lasting for at least five days (100%), plus four of the five criteria listed below:
1. Bilateral bulbar conjunctival congestion (85%)
2. Changes of buccopharyngeal mucosa, raspberry tongue (90%)
3. Skin changes of the extremities (palmar erythema / edema, desquamation of fingertips)
4. Rash on the trunk
5. Unilateral cervical lymphadenopathy non suppurating
Severe cardiac impairment is manifested by:
Myocarditis (50%)
Pericarditis - in the acute phase
Coronary aneurysms that occur in the 2nd and 3rd week with rupture risk on > 8 mm
KD should be considered as differential diagnosis when are existing:
Fever for several days + rash + serous conjunctivitis in a child under the age of 1 year
There is a possibility of error diagnosis in the following situations:
- a rash from antibiotics
- a sterile pyuria after partial treatment for UTI
- CSF with pleocytosis for a typical viral meningitis.
Treatment:
- association of steroids if fever persists after 2 doses of IVIG
- Infliximab (Remicade-monoclonal antibody against TNF)
- plasmapheresis
158
CHAPTER V - DISEASES OF THE DIGESTIVE SYSTEM
Conf. Univ. Dr. Mrginean Oana, Asist. Univ. Dr. Pitea Ana Maria
GASTROESOPHAGEAL REFLUX
Definition: repeated flow (passage) of the gastric contents into the esophagus
regurgitation
the flow of the stomach content into the pharynx/the oral cavity sometimes protrudes,
generally without any effort
vomiting
pharyngeal receptor stimulation triggered by gastric contents
rumination
remastication/redeglutition of the regurgitated gastric contents in the mouth
Etiopathogeny: GERD is common (1/500 live births) in the first months of life: 30 - 40% of
the infants present regurgitation (small amount) and more frequently the premature and
dismature ones.
Infant reflux becomes evident in a few months with a peak at 4 months, resolving to 12-24
months.
Genetic predisposition associated with oesophagitis, hiatus hernia syndrome Barrett
adenocarcinoma. It is an autosomal dominant transmission, localized on chromosome 13q14.
Pathogenic mechanisms
1. Lower esophageal sphincter incompetence (LES) which maintains a pressure of 15-40
mmHg (gastric pressure: 6-10mmHg); pressure changes causes reflux.
2. Extension of esophageal clearance: hiatal hernia, malposition of the cardia and
gastric tuberosity, causes a prolonged peristaltic and even aspiration of gastric contents.
3. Delayed gastric emptying, found in acid levels after meals which are rich in lipids.
GERD once installed maintains the lower esophageal sphincter incompetence,
determining motor failure mechanisms and a prolonged contact of the esophageal mucosa
with the gastric pepsin, bile salts, and the pancreatic proteolytic enzymes; while the
esophageal mucosa erodes, causing peptic esophagitis.
Clinical symptoms
Newborn and infants, 80-90% of cases, regurgitation and vomiting occur (the bloody ones
are a sign of esophagitis); commonly associated with respiratory symptoms: bouts of apnea,
159
recurrent cough, nocturnal wheezing, bronchospasm and can be wrongly labeled as asthmatic,
obstructive bronchitis. Infants are irritable, anorexics, have colic, do not gain weight, they
show distrophy, in small infants sudden death may occur.
Food refusal in infants appears to be associated with GERD.
In older children GERD is rarely manifested by epigastric pain, heartburn (dominant
symptoms), dysphagia, vomiting, chronic, recurrent pneumonia (vacuum), areas of gastric
metaplasia (Barrett epithelium) or peptic stricture asymptomatic post oesophagitis.
Occasionally both infants and preschool children present contortions of the neck or head and
opisthotonus posture, which can be mistakenly interpreted as seizures or neurological
distress. This is called Sandifers syndrome.
The following can be associated with reflux: otitis media, sinusitis, lymphoid hyperplasia,
nodules of the vocal cords, laryngeal edema.
Diagnosis
Laboratory investigations
1. Radiography (esogastric) with a contrast substance provides information about esogastric
junction: hiatal hernia, Hiss obtuse angle, stenoses, and compressions
2. Oesophageal manometry evaluates the pressure of LES.
3. Scintigraphy with technetium (Tc99) allows visualization of the bile reflux, flow in the
bronchial tree and esophageal clearance.
4. Esophageal pH monitoring is done using an electrode placed in the esophagus,
determining the esophageal pH for 16-24 hours (n = 5-7, the stomach has a pH = 2); in
GERD esophageal pH is less than 4. The number and duration of flows will be recorded. In
GERD there are 2 flows/hour with a pH below 4 the slumping being present in more than 5%
during the determination.
5. Esophageal endoscopy (with flexible fiberscopes) allows the visualization of the lesions of
the esophagus and collection of biopsy material for histological diagnosis (there are four
degrees of peptic oesophagitis), diagnosis of hiatal hernia, and diagnosis of the
complications: esophageal stenosis.
6. Intraluminal impedance is difficult to perform, helps in the diagnosis of nonacidic reflux.
7. Laringotraheobronhoscopia assesses signs associated with GERD, posterior inflammation
of the larynx and the vocal cords, highlighting silent aspiration.
8. Ultrasonography (> 3 slumpings/20min of examination) and oesophageal scintigraphy
Differential diagnosis is made with:
- recurrent wheezing - asthma
160
- apnea attacks - gastritis
- neurological suffering, seizures - acute laryngitis
- infections, allergies - cystic fibrosis
Complications: oesophagitis, Barrett's esophagus, esophageal stricture, haematemesis,
aspiration pneumonia, anemia.
Treatment
1. Hygienic-dietary in infants
A. Dietary treatment
- changing the preparation of milk powder (HA, hydrolysed)
- substantial increases of meals with milk
a. with nutritional value: rice flour; a dose 5-15 g/100ml milk
b. no nutritional value: carob seed flour, pectin- cellulose
B. Postural therapy
prone anti-Trendelenburg
supine anti-Trendelenburg
position change
2. Medicamentary
- motility disorder control - reducing the frequency of slumpings ( receptor agonist of
GABA) - Baclofen 0.6 mg/ kg, 3-4 doses/ day
Prokinetic (acetylcholine), increases oesophageal peristalsis and LES tonus, accelerates
gastric and duodenal emptying:
- Metoclopramide 0,1 mg/kg before meals, Cisapride: 0,2 mg/kg/day - 3 doses - 20-30`
before meals.
- Erythromycin 5-10 mg/ kg/ day Ranitidine 5-10 mg/ kg/ day - 3 intakes before
meals, 1 month.
- Domperidom (Motilium) has fewer adverse effects on the CNS, but has similar side
effects as Cisapride (intravenously administration of QT prolongation): children: 0.8-
1 mg/ kg/ day in 3-4 doses, 15-30 minutes before meals, adults: 10-20 mg/ dose, 30
minutes prior to meals and at bedtime
Inhibitors of H2 receptors in mild and medium forms of oesophagitis at least for three
weeks: Ranitidine 5 mg/ kg/ day - 2 doses, Famotidina 1 to 1.5 mg/ kg/ day - 2 doses.
Proton pump inhibitors in case of severe oesophagitis: Omeprazole (Losec, Ultop), Controloc
(Pantoprazole) 0.7 mg/ kg/ day - single dose - 4 weeks (8 weeks).
161
In older children and adolescents, with frequent recurrence, the medication should be
continued for another 6 months -a single small dose.
Sucralfate for mucosa healing.
Respond poorly to drug therapy: children under 18 months old if there is hiatus hernia or
neurological disabilities.
3. Surgery - indications: persistent oesophagitis at 6-8 weeks of medical treatment
oesophageal stricture, persistent vomiting, malnutrition, seizures, apnea, chronic lung disease
or lack of response to medical treatment for 2-3 months.
Evolution and prognosis
In mild to medium forms it occurs through dietary and medicinal healing. In complicated
cases (aspiration pneumonia, anemia) the evolution is extended.
The prognosis is good.
GASTRITIS IN CHILDREN
Definition: inflammatory processes in the gastric mucosa, with histopathological arguments,
commonly associated with peptic ulcer and duodenitis.
Etiopathogenical classification
infectious
- bacterial: H.pylori, H. heilmannii
- viral: CMV (b.Menetriere), v.herpetic
- fungi, parasites
non-infectious, immune
- eosinophilic gastritis
- gastritis in Henoch-Schonlein
- gastritis in celiac disease
idiopathic
- gastritis in Crohn's disease
- collagenous gastritis
reactive
- by bile reflux
- medicines, toxic
- mucosal prolapse, gavage probe
vascular
162
- from portal hypertension
metabolic diseases
- chronic granulomatous disease
Contributing factors: alcohol, smoking, fast chewing - poor teeth, too cold or too hot food,
food abuse.
Pathogenesis - imbalance between aggressive factors and mechanisms of defense. Among
aggressive factors we mention acid secretion, pepsin secretion, stress, aspirin, NSAIDs, H.
pylori and among defense mechanisms of the mucosa: mucus and bicarbonate secretion,
mucosal blood flow, prostaglandins (PG) (which stimulates other mechanisms).
Clinical symptoms
Onset can be fast, characterized by nausea and vomiting, or slow, non-ulcer dyspepsia (NUD)
without endoscopic signs, epigastric pain, rhythmed by food intake, as in UDS (ulcer
dyspepsia syndrome), rarely diffuse or periumbilical, frequent nausea, consequence of bile
salts, pancreatic ferments (by duodeno-gastric reflux), food, bilious, bloody vomiting
(hematemesis is relatively characteristic of H. pylori); anorexia, regurgitation and heartburn,
bloating, constipation or diarrhea completes the picture NUD - functional dyspepsia.
Positive diagnosis
Measuring acidity, gastric barium examinations are inconclusive. The positive diagnosis
system requires the criteria of the Sydney system (1994).
Endoscopic criteria: erythematous-exudative gastritis, erosive, atrophic, bleeding, reflux or
folds hypertrophy.
Histological criteria: acute gastritis, chronic, special (eosinophilic, lymphocytic,
granulomatous); in acute forms the infiltration is with neutrophils, when in chronic forms is
lymphoid.
Differential diagnosis
Clinical - other causes of recurrent abdominal pain.
HELICOBACTER PYLORI GASTRITIS
Nobel Prize for Medicine in 2005.
When the infection occurs an ulcerous or non-ulcerous dyspepsia syndrome appears and as it
becomes chronic the symptoms alleviate.
Most infections are asymptomatic. Slow infection of the gastric mucosa begins in childhood,
with an annual rate of infectivity of 1%, showing the origin of childhood infection
prevalence.
163
The phenomenon of "cohorts" is known: infection of 20 years is about 20%, at 50 is 50%.
Maximum prevalence is at the age of 3-4; 10-20% of children have IgG, IgA positive (H.
pylori colonization). H.p. is the most frequent cause of gastritis, ulcersIn 1994 WHO situates
the infection in group I carcinogen; gastric cancer is the second leading cause of cancer
death. The incidence of gastritis in children is 1% in developed countries, 10% in developing
countries.
Current assumptions
The etiology of gastroduodenal diseases include environmental factors, genetic
predisposition consisting of genetic susceptibility to infection and DNA repair mechanisms
related to carcinogenesis, respectively host polymorphism - CZP2C19 and MDR1 genes
that influence the pharmacokinetics and efficacy of treatment with proton pump inhibitors.
The source of infection is the human being (and possibly cats). The route of transmission is
the fluid one. The weight of infection in urban areas is 70%, the water in the system is
infected; bacteria live 16 hours in the water, mostly in cold water, a possible role have
carbonated juices.
Contamination may be oral-oral or fecal-oral, the infection is more common in countries with
lower socio-economic conditions (congestion, local children).
Diagnosis
1. Biopsy bioptic fragment analysis sampled with scopes.
Histologically the spiral H. pylori microorganism can be identified by Warthon - Starry
argentic staining (very sensitive and specific), modified Giemsa staining, acridine orange
staining and cresyl violet.
Rapid urease test identification of H. P. from the gastric mucosa specimens from different
urea; the colour change occurs in 30 minutes; with a turn in 24 hours if the number of
bacteria is low.
Tests for infection deceleration:
2. Urea breath test labeled with C13, C14. Principle: urease produced by H. P. catalyzes the
hydrolysis of urea into NH3 and CO2 (2 samples of 20 in 20 min.), rapidly normalized after
resolution of infection, evaluating the effectiveness of treatment, tests that detect the presence
of specific Ig remain positive up to 6 months.
3. Serological tests detect antibodies
Elisa - IgG, IgA serum. IgG serum has a specificity below 50% in children under the age of
7, similar with the specificity in adults after the age of 12.
164
4. Determination of specific IgG in saliva has a specificity of 82%, sensitivity 93%, varying
according to the used reagents.
5. Immunoassay determination of Atg from stool (HpSA) (H. pylori stool antigen test)
with polyclonal antibody, or recently - monoclonal ones, is a non-invasive method, with a
sensitivity of 91-98% and specificity of 83 - 100%.
6. Immunological tests PCR and DNA- enzymes: PCR with amplification - detected by gel
electrophoresis the use of colorimetric detection, a faster method, which may be automated.
Treatment
The best diet in acute forms is abstinence from any food for 12 to 24 hours, if hardly bear
hunger - tea, juices, soups are allowed, on the second day one can try toast, cottage cheese,
grated apple, rice, and then gradually introduce vegetables, meat and other, after tolerance.
Medications
The North American Society of Pediatric Gastroenterology and Nutrition (2000) recommends
combinations.
- Amoxicillin 50 mg/ kg/ day in 2 doses + Clarithromycin 15 mg/ kg/ day - 14 days + 2
doses of proton pump inhibitors (omeprazole, pantoprazole) 0.7 to 1 mg/ kg/ day - 2
doses - 1 month.
- Amoxicillin 50 mg/ kg/ day - 2 doses + Metronidazole 20 mg/ kg/ day - 2 doses - 14
days + proton pump inhibitors (Omeprazole, pantoprazole) 0.7 to 1 mg/ kg/ day - 2
doses - 1 month.
- Clarithromycin 15 mg/ kg/ day - 2 doses + Metronidazole 20 mg/ kg/ day - 14 days + 2
doses of proton pump inhibitors (Omeprazole, pantoprazole) 0.7 to 1 mg/ kg/ day - 2
doses - 1 month.
The scheme has good results in the eradication of the infection (80%). Some schemes use:
Clarithromycin, Erythromycin, Tetracycline.
Anti-infective therapy is associated with antisecretory for 3-8 weeks:
a). Proton pump inhibitors: Omeprazole 0.7 mgkg/ day - single dose after lunch
b). H2 receptor inhibitors: Ranitidine 5 mg/ kg/ day or Nizatidine -2 doses (Axid) 2-3 mg/ kg/
day - 2 doses, Cimetidine 5 mg/ kg/ day after meals; Famotidina 1-1.5 mg/ kg/ day - single
dose.
The treatment of other gastritis
Objective: to maintain the pH above 4 with antacids and antisecretory.
In gastroesophageal reflux prokinetics are administered.
165
Estimation of healing is done after two months, usually after treatment clinical and
histological recovery
Prognosis - favorable.
Prophylaxis: general rules of food hygiene, avoiding alcohol and smoking, and in future
vaccination of children for H. pylori.
ULCER DISEASE (peptic ulcer)
Definition: the gastric or duodenal location of a loss of substance (solution of continuity) at
the level of mucosa. Clinically we encounter the dyspeptic ulcer syndrome with food
rhythmicity and seasonal periodicity.
The etiology is multifactorial.
Hereditary factors: 1/3 of children have degree I, II relatives who have suffered or suffer from
ulcers.
Infectious factor ("rarely - ulcer without H. pylori "); eradication of the bacteria decrease
recidivism (60-70% to 1-2%); H. pylori is present in 70% of cases in gastric ulcer and over
90% in the duodenal one.
The stress factor: Cushing stress ulcer by CNS injury, Curlings ulcer in burns, emotional
ulcer
Ulcerogenic drugs: aspirin, NSAIDs, corticosteroids.
Contributing factors: food abuse, tobacco, coffee, alcohol excess.
Pathogenesis: (see gastritis).
Clinical symptoms
In newborn hematemesis, melena, perforation are the first signs; usually there is sepsis,
severe respiratory distress.
Between the ages of 1-6 the primary symptom is vomiting, pain - especially in the
periumbilical region, abdominal discomfort (irritable bowel syndrome or functional
dyspepsia), and gastrointestinal bleedings are relatively common.
Over the age of 6 the triad appears: abdominal pain, vomiting, gastrointestinal bleeding, most
commonly after 12 years.
The onset may be sudden or insidious (approximately in equal proportions).
Duration: in this stage the dyspeptic ulcer syndrome occurs (DUS) in 2/3 of cases, rhymed
nutrition pain, shortly after in gastric ulcer, approximately 3 hours after meals and at night in
duodenal ulcer. The intensity of the pain is variable (cramp, colic) and it is located in the
166
epigastric region with radiation to the hypochondrium, septic iliac (confusion with
appendicitis!); the painful episode is followed by calmness, repeatable in spring (very rarely
in children it may occur in autumn). Sometimes the pain is diffuse or periumbilical and it is
associated with a feeling of fullness, heartburn, malaise, neuro-vegetative disorders. In case
of sudden onset gastrointestinal bleedings and perforations are common. Patients diagnosed
with peptic ulcer rarely present abdominal pain given by the perforation itself or symptoms of
a secondary pancreatitis may be present to a posterior penetrating ulcer.
The pains are often dull, than become sharp and are associated with heartburn. The pain may
last from minutes to hours, and can evolve with exacerbations or remissions lasting weeks or
months. Nocturnal pain occurs mostly in older children. Positive history with aspirin was
detected in 33% of cases.
Positive diagnosis
Highlighting ulcer niche at the radiological examination- has lost importance.
Endoscopic examination with the fibroscope: of duodenal ulcers are situated on the
anterior wall of the duodenal bulb; in over one third of the cases in the sampled biopsy H.
pylori is found.
The ulcer crater often presents gray-whitish debris and it is brownish-if there is bleeding. The
bottom of the ulcer is round, with straight-edges - benign ulcer. Ulcers can be round, oval,
oblong or linear.
Differential diagnosis
It is made in other causes of acute or chronic abdomen pain
Complications: hematemesis, melena, perforation, pyloric stenosis (very rare in childhood).
Treatment
1. Dietetic in acute phases, initially milk, then vegetable soups, boiled egg, toast, later meat
and other foods; diet has lost its importance.
Prohibitions: alcohol, coffee, carbonated water, smoking.
2. Medicamentary
- Alkalines Ulcerotrat, Trisilicalm, Dicarbocalm, Gelusil, Maalox, Alumag. Pain
killers- an hour after eating (acid secretion is the highest, the effect takes about 3h, on
the "empty stomach" the effect is 30 min., together with the antisecretory maintains a
pH above 4.
- Anti-infective therapy - As with gastritis, for the eradication of H. pylori one of the
three schemes is used
167
- Antisecretory: Omeprazole 20 mg/ day 1 caps/ day (children 0.7 mg/ kg/ day) 4 weeks
in duodenal ulcer, 8 weeks in the gastric one; Ranitidine 5 mg/ kg/ day - 2 doses;
Nizatidine (Axid) 2-3 mg/ kg/ day - 2 doses; Famotidine 1-1.5 mg/ kg/ day as a single
dose during meals, 4-8 weeks (rarely 8-12 weeks); Cimetidine 5 mg/ kg/ day after
meals, with the disadvantage that inhibits the liver enzyme (cytochrome).
- Cytoprotective agents Sucralfate has good results in some forms.
- Other agents: parasympathetic (Scobutil), anticholinergics (Metoclopramide) sedative
agents used to treat specific basic diseases (burns, head trauma, sepsis)
3. Surgery is indicated in complications or failure of medical treatment.
Evolution and prognosis can record relapses, but the overall prognosis is good.
It is possible that a gastric cancer at the age of 40-50 be the continuation of a gastritis or a
gastric ulcer from childhood.
THE MALABSORPTION SYNDROME
Definition. The syndrome encompasses a wide range of digestive disorders (>100) that have
as a common feature, the inability to supply the body (partially or completely) with trofins,
vitamins, minerals and water.
(The classification in malabsorption and maldigestion sundromes is not a current one, their
confusion being proven).
The consequences of the syndrome are of deficiency, having various nutritional and
metabolic effects.
The syndrome comprises, roughly, the following mechanisms:
1. Intraluminal digestion (modification of motor and gastric secretory function;
pancreatic insufficiency; hepatobiliary disorders; short bowel; intestinal
dysbiosis).
2. Intestinal absorption.
3. Blood or lymphatic transport
4. Exudate and intestinal motility.
5. Synthesis and altered catabolism of food principles
6. Unknown mechanism.
168
CYSTIC FIBROSIS (Cystic fibrosis C/F; Mucoviscidosis; Cystic fibrosis of the
pancreas)
It is a chronic disease characterized by airway obstruction and chronic infections and
maldigestion; it is an autosomal recessive genetic disease characterized by the dysfunction of
the exocrine gland epithelium, with a high frequency: 1 case/ 2000 births. It is more common
in white people of northern Europe, North America, Australia and New Zeeland.
The etiopathogeny the C/F gene located on the long arm of chromosome 7 (the largest
gene), it is the gene that codifies the synthesis of membrane glycoproteins, called
Transmembrane conductance regulator of C/ F (CFTR), is placed at the apical poles of
secreting or resorptive cells, facilitates transmembrane transport of Cl
-
, 40 mutations, which
may affect the gene..
Abnormal CFTR determines an excess of Cl
-
i Na
+
at the level of the glands of various
organs, the secretory epithelium of the mucous glands becomes waterproof for Cl
-
ions (then
Na
+
, K
+
and water) resulting in viscous fluids.
A particular situation is represented at the level of the serous glands (sweat and salivary
glands), the resorptive ducts being affected; the epithelium is impermeable for Cl
-
ions, the
final sweat will contain high amounts of Cl- (secondary to Na
+
), the water content being
normal.
Types of C/F: without exocrine pancreatic insufficiency and with exocrine pancreatic
insufficiency (85%).
Pathophysiology: bronchial mucous gland hyperplasia, cystic pancreatic ducts surrounded
by fibrous tissues, aspect of biliary cirrhosis and other changes that cause pluriorganic
sufferings.
According to the alteration mechanism of the CFTR protein function there are:
- Class I mutations, that determine the synthesis of some defective, unstable CFTR
proteins, with little or no function
- Class II mutations, because of which the protein would be incompletely glycosylated
(immature), without the correct spatial conformation, undetected at the cell surface;
the most frequent mutation (70%) A F 508: deletion of three base pairs from exon 10
of the gene ausing loss of phenylalanine at position 508 of the primary sequence of
CFTR.
- Class III mutations, CFTR proteins having defective adjustments
169
- Class IV mutations, the conductivity of the formed CFTR proteins being affected in
the apical membrane.
- Class V mutations reduced production of CFTR.
- Class VI mutations stressed turnover on the cells surface
Class I-III mutations cause severe diseases with reduced survival, whereas Class IV-VI
mutations determine mean forms of diseases.
Many hypotheses have tried to explain how CFTR dysfunction acts in order to determine
clinical phenotypes. The most plausible are the assumptions that highlight the inability to
secrete salt and secondary to secrete water in the presence of excessive salt and water uptake.
In CF high intake of Na through altered CF cells is associated with increased conductance
amiloride sensitive - Na in the apical pole of the membrane and increasing the locus Na-K-
ATPase in the basal pole side of the membrane.AMPc mediates at the level of the apical pole
(luminal) of the Cl
-
secretion membrane associated with CFTR that does not work in the
epithelium of patients with CF, but an alternative way of Ca2 + - Cl- conductance is present
in normal cells with CF as well. CF cells have a limited ability to secrete Cl and absorb
excess Na limiting the water available to hydrate secretions.
The proposed mechanism is explained by insufficient water at the level of the airways in
order to hydrate secretions. Dehydrated secretions become more viscous and elastic and are
more difficult to clean by muco-ciliary activity and other mechanisms. In addition CFTR
dysfunction alters the microclimate with low concentrations of HCO
3
-
and a more acid pH,
which alters the rheology of the mucus and makes the low mucociliary clearance worse. The
result is the stagnation of the secretions in the airways, starting with the smallest ones
bronchiole, airway obstruction and then superinfections with Staphylococcus aureus,
Pseudomonas aeruginosa and Burkholderia cepacia. This causes bronchiolitis, then, over
time the accumulation of mucus in the higher airways leads to bronchitis. With time mucus
superinfects - bacterial invasion. Bronchioles obstruction, bronchiectasis, emphysematous
bubbles or subpleurale, pneumothorax, hemoptysis (by dilating the bronchial arteries) appear.
Paranasal sinuses are uneven filled with secretions leading to polypoid lesions (polyps
around maxillary and ethmoid sinuses).
Similar changes occur at the level of the pancreatic ducts usually small ones, occasionally
cystic. In 85-90% of the cases lesions progress to replace acini with fibrous tissue and fat,
calcifications, resulting in most cases in exocrine pancreatic insufficiency, sometimes an
endocrine one.
170
At the level of the intestinal tract the modifications are minimal, possibly destines glands
with mucus secretion. Changes at the level of the biliary tracts lead to the obstruction of the
intrahepatic bile ducts with the onset of focal biliary cirrhosis (30-70% of cases).
The obstruction of the uterine cervical glands can lead to endocervisitis, and at males the
obstruction of the ependymal ducts can occur of the vas deferens, seminal ones, with
secondary infertility.
Clinical symptoms
1. Respiratory symptoms: occur early in 90% of the cases/ in infancy. The onset is
characterized by monoliform, dry cough, leading to confusion with pertussis, then productive
sputum, often like bronchitis; while evolving to hyperinflation, peribronchitis, bronchiectasis,
atelectasis (right upper lobe), low hematosis ventilation reduction with chronic respiratory
failure and death may occur.
Complications: pneumothorax and hemoptysis, late bronchiectasis and chronic respiratory
insufficiency; infection is frequent (viscous mucus, aderent being adherent culture medium
especially for. Staphylococcus and Pseudomonas, B. cepacia encountered in over 90% of
cases), lung colonization and rapid deterioration of the respiratory functions; the infection
worsens the obstruction and favors the infection (a vicious circle is created). Non tubercular
cystic fibrosis is the most common chronic disease in children.
2. Digestive symptoms:
Meconium ileus (15 - 20%), not removing the meconium 24-48 hours after birth causes
symptoms of intestinal obstruction, with flatulence, air-liquid images; the normal meconium
is rich in carbohydrates, but in cystic fibrosis has a high content of protein and is viscous.
Drug treatment consists of the administration of gastrografin (a contrast agent with increased
osmotic pressure), or N-acetylcysteine for dissolving. Surgery is temporary ileostomy (with
poor results).
Malabsorption is another digestive symptom, given by the exocrine pancreatic insufficiency
at birth which occurs after 6 months by chronic diarrhea and malnutrition; the viscous mucus
obstructs the pancreatic ducts, and in the absence of the pancreatic juice, the digestion
disorder of lipids and proteins occur; malabsorption: steatorrhea, azotorrhea,
hypoproteinemia, hypocholesterolemia, malabsorption of fat soluble vitamins A, D, E, K,
with clinical consequences: edema, impaired night vision, rickets, haemorrhages. The
children are weak, malnourished, with a "voracious" appetite. The abdomen is distended, the
stools are steatorrheic (celiac differentiation!).
Rectal prolapse (2%) is a pathognomonic sign in children under 2 years old.
171
3. Hydroelectrolyte disorders may occur when patients sweat excessively (fever, high heat),
causing hypernatremic dehydration or hypochloremic alkalosis.
4. Other symptoms: pansinusitis, slowed growth, intussusception, subocclusions, sterility,
biliary cirrhosis.
Positive diagnosis
It shall be based on clinical symptoms and sweat test.
Suspicion arises in a child with chronic digestive distress, recurrent respiratory infections or a
child under 2 years old with rectal prolapse.
The sweat test allows Cl-and Na + dosing from the collected sweat after iontophoresis with
pilocarpine; values over 60 mEq/ L at two consecutive tests are suggestive, and under age 3 -
over 40 mEq/ L).
Diagnosis of pancreatic insufficiency requires a stool test, which detects undigested muscle
fibers, neutral fat and a duodenal tubing showing a reduced viscous pancreatic secretion, with
no pancreatic enzymes (trypsin, lipase, amylase, chymotrypsin) when the secretion is
analyzed. For endocrine pancreatic insufficiency the oral glucose tolerance test is
recommended in children over the age of 10.
Other modifications: hipolipemia with hypocholesterolemia, hypoproteinemia, malabsorption
of fat-soluble vitamins (A, D, E, K) and of vitamin B12, Zn, Se, Fe deficiency, hyponatremia
and hypochloremia in sweating.
Genetic screening allows diagnosis of pathological CFTR mutations on both chromosomes.
Tests for 30-96 mutations of CFTR are done.
Chest radiography highlights the hyperinflation, pulmonary infiltrations, cysts,
bronchiectasis, pneumothorax, etc.
The study of lung function by assessing residual volume, functional residual capacity is
recommended after the age of 4-6.
Evaluation of microbial superinfection (S. aureu, P. aeruginosa, B. cepacia or Mycoplasma)
is useful for making the correct treatment according to the antibiogram and to preserve the
correct lung function. If children do not expectorate bronchoscopy is recommended.
Detection before birth: trophoblast biopsy study (week 10), determining the activity of
intestinal enzymes in the amniotic fluid (week 18).
Neonatal diagnosis between the 5th day and the first two months of life: demonstration of an
increased level of immunoreactive trypsin in blood.
Differential diagnosis
a) Digestive symptoms will differ from intestinal obstruction and other malabsorptions
172
b). Pulmonary symptoms require differential diagnosis with pertussis, bronchitis, pneumonia,
asthma, bronchiectasis, tuberculosis, foreign body.
Treatment
The goals of the treatment are:
1. Monitoring
2. Pulmonary therapy
3. Digestive therapy
1. Monitoring and follow-up every 1-3 months. Sputum examination or throat swab is
recommended after each episode of cough and treatment according to the antibiogram. A
multidisciplinary assessment is required: pulmonologist, gastroenterologist, dietician, and
psychologist. Adequate hydration is recommended (oral or intravenous) in order to minimize
the complications associated with a viscous mucus. Scopul The goal of therapy is to ensure a
stable condition as long as possible.
2. Pulmonary therapy:
a. Inhaler treatment is used to deliver medication and adequate hydration of the lower
airways. Bronchodilators, corticosteroids and mucolytics are used:
- Mucolytics: N. ACC - Fluimukan, f 3 ml solution, with good effects (FEV> 50%), 1-3
ml/ session - 2-3 times/ day. N ACC is toxic to the ciliated epithelium and repeated
administrations will be avoided.
- Bronchodilators for patients who respond to the treatment: Albuterol 0,1-0,2
mg/kg/day (2-3x), Metropoterenol, Terbutalin, Teofilin, etc.
- Recombinant human deoxyribonuclease (2.5 mg) administered daily as a single dose
improves lung function, decreases the number of pulmonary exacerbations, promoting
well-being in patients with moderate disease (Pulmozyne). The treatment is
administered continuously 12 months.
- Nebulization with a hypertonic saline solution (7%), being hyperosmolar rehydrates
the mucus, and the pericilliary film, improving muco-ciliary clearance. DNA from
neutrophils destruction increases the viscosity of the sputum slowing down the
removal of the mucus, 2.5 ml/ day/ session, minimum 6 months.
- Antibiotics in aerosols (tobramycin) in case of airway colonization with P. aeruginosa
b. Therapy for airway clearance (chest physiotherapy) consists of percussion combined with
postural drainage, forced expiratory in young children who do not cooperate, chest percussion
and vibration application (1-4 hours/day)
173
c. Antibiotic treatment - aimed at controlling progression and lung infections. Treatment with
antibiotics may be given orally, in aerosol and IV.
Oral antibiotic therapy is administered to eradicate antibiotic agents isolated from respiratory
cultures as S. aureus, H. influenzae, P. aeruginosa, B. cepacia, gram-negative Mycoplasma.
Staphylococcus and H. influentzae can easily be eradicated per os, but Pseudomonas requires
prolonged treatment over 2 weeks, with the maximum dose. For S. aureus the following can
be used: Dicloxacillin 25-50 mg/ kg/ day in 4 doses, Linezolid 20 mg/ kg/ day in 2 doses,
Clindamycin 10-30 mg/ kg/ day in 3-4 doses, Amoxicillin/ Clavulanic 25-45 mg/ kg/ day in 2
doses; for H. influentzae Amoxicillin 50-100 mg/ kg/ day in 2-3 doses; for Pseudomonal -
Ciprofloxacin or other quinolones 20-30 mg/ kg/ day in 2-3 divided doses; for B. cepacia
Trimetroprin 8-10 mg/ kg/ day in 2-4 doses., empirical macrolide as Azithromycin 10 mg/ kg/
day, on day 1 and 5 mg/ kg/ on days 2-5 or Erythromycin, or Clarithromycin, macrolides that
reduce the virulence of P. aeruginosa.
Inhaled antibiotics are administered for P. aeruginosa and other gram-negative germs, which
are resistant to oral antibiotics.
In the aerosol, antibiotics such as Tobramycin (300 mg 2 times/ day), Colistin (75-150 mg in
aerosols, 2-4 times/ day) or Gentamicin can be used. With this inhaled therapy the P.
aeruginosa density decreases in sputum and hospitalizations are reduced. Intravenous
antibiotic therapy is given to patients with progressive pulmonary and persistent disease, for a
period of 7-14 days. Suitable for P. aeruginosa: Tobramycin 8-12 mg/ kg/ day 1-3 doses,
Amikacin 15-30 mg/ kg/ day in 2-3 doses, Ticarcillin 400 mg/ kg/ day in 4 doses, Piperacillin
300 -400 mg/ kg/ day in four doses, Meropenem 60-120 mg/ kg/ day in 3 doses, Imipenem
45-100 mg/ kg/ day in 3-4 doses, for Staphylococcus Vancomycin 40 mg/ kg/ day in 3 -4
doses, Nafcillin 100-200 mg/ kg/ day in 4-6 doses, and for B. cepacia Meropenem 60-120
mg/ kg/ day in 3 doses. For Pseudomonas a combination of two antibiotics eg tobramycin +
piperacillin) and for staphylococcus another antibiotic is usually used. (Initial doses are
higher, and if the patient's progress is good, the doses are adjusted.
d. Anti-inflammatory treatment: glucocorticoids in bronchopulmonary aspergillosis, 2 mg/
kg/ day, NSAIDs have the same effects as steroids, with fewer side effects: Ibuprofen,
Piroxicam; Pentoxifylline and fish oil preparations are useful.
e. Endoscopy and bronchial lavage especially in the case of atelectasis or obstructive mucus.
Antibiotics such as Tobramycin or Gentamicin can be instilled directly.
f. Potential Therapies: Gene mutation therapies (PTC 124 can suppress codon termination)
3. Fighting digestive disorders - correcting digestive disorders;
174
The diet will be rich in proteins, glucagons, poorer in lipids with 1 g ClNa supplement under
2 years and 2 g over 2 years, in summer and in case of fever, with vitamins (A, D, E , K), zinc
(risk of enteropathic acrodermatitis)
Pancreatic extracts are required at every meal, individualized, 4-12 tablets/ day in order to
obtain 1-2 stools/ day. Infants need 2000-4000 U lipases/ meal administered with apple juice.
Pancreatic enzymes will not exceed 200 units lipase/ kg/ meal.
Evolution and prognosis
The evolution is constantly overshadowed by infections.
The prognosis is reserved, depends on the lungs (95% of deaths occur in bronchopulmonary
damage). The average life expectancy has increased to 35 years.
Prevention: an early detection.
The test for the assessment of albumin content of meconium (N = 0-5 mg%); in cystic
fibrosis the value is of 20-80 mg%. The downside is the possibility of false-positive reactions
(in premature infants); the test is positive when the color is green instead of yellow.
The determination of circulating immunoreactive trypsin: in blood the quantity of trypsin is
little (inactive) and increases with increasing pressure in the pancreatic ducts A screening
may be made concurrently with the detection of phenylketonuria and hypothyroidism.
Determination of potential differences in the nasal mucosa.
Genetic tests for highlighting mutations.
GLUTEN-SENSITIVE ENTEROPATHY (CELIAC DISEASE, CELIACHIA)
Frequency of celiac disease (CD) is estimated at 1-2500 inhabitants, and in Northern Europe
1/500 inhabitants. It seems, however, that the incidence is higher. The iceberg theory was
entertained, according to which CD is 0.5-1% of the general population as the disease is not
properly diagnosed and therefore, in to one diagnosed case, correspond other 5-10
undiagnosed ones.
Definition: CD is a systemic disease, immune mediated, triggered by sensitization to gluten
in the flour and prolamin in the barley, oats and rye, with clinical manifestations - due to
gluten sensitization and CD specific-antibodies (Autoantibodies transglutaminasis TG
2
,
antiendomisium EMA, Antibodies against deaminated gliadin peptides DGP) Patients have
haplotypes HLA-DQ
2
or HLA-DQ
8
and enteropathy
Etiology is multifactorial, with high genetic predisposition
175
Children with celiac disease have hypersensitivity to gluten proteins of some
cereals (wheat, rye, barley, oat)
In patients with celiac disease, T lymphocytes have been determined in the
thin intestine, which recognize the gliadin peptides in HLA DQ2 or HLA
DQ8 context
The TG2 atb determination as major auto-antigens in celiac disease led to the
recognition of the autoimmune nature of the disease
The disease is very rare in rice consumers, the risk being much lower in those
naturally fed.
Predisposing factors: infections, stress, hunger.
Pathogenesis:
The celiac enteropathy is the result of the immune-mediated lesion on the mucosa of
the bowel
The physiopathological cascade of events begins with alteration of barrier function of
the bowel mucosa
zonulin override (an intestinal peptide), has a role in the increased intestinal
permeability to the gliadin peptides in patients with CD
tissue transglutaminasis is present in lamina propria , an enzyme that catalyzes the
cross linking of the proteins, deamidated peptides of the gliadin, increasing their
affinity for HLA molecules located on the membrane of the antigen-presenting cells
(APC) (macrophages)
HLA molecules form a ditch" where the peptide can be specifically connected the
intestinal T lymphocytes are activated
T lymphocytes release pro-inflammatory cytokins (interferon , TNF ) which
determine enterocytes damages, increased proliferation in the intestinal crypts and
severe lesion of the arhitecture of the intestinal mucosa (atrophy)
Cascade of events
intraluminal digestion of gliadin peptides and release of toxic epitopes;
intraluminal release of zonulin dependent gliadin (circle);
opening fine intercellular junction secondary to zonulin action followed by passage of
toxic gliadin fragments in the submucosa;
tissue transglutaminase(star) -mediated gliadin deamidation followed by engagement
to HLA DQ2/DQ8 located on the surface of antigen presenting cells (APC);
176
antigen presentation to T lymphocytes;
presentation to B lymphocytes;
generation AGA-producing plasma cells (antigliadin antibodies) and EDA / tTG atb
(anti endomisium / anti transglutaminase);
killer T cell activation and increased production of cytokines, which leads to damage
of the intestinal mucosa.
Symptoms
The onset in classic forms is at 6-18 months, in a few weeks/ months after the introduction of
pasta in the diet.Atypical forms can appear at any age.
Clinically, children are weak, pale, anemic, and irritable, with hypotonic muscles, distended
abdomen, hepato-splenomegaly, fused buttocks, stopped growth and weaknesses: rickets,
osteoporosis, and anemia.
Because the atypical form is more frequent than the classical form the working team
ESPGHAN has decided to use for symptomatology: gastrointestinal signs and symptoms and
extra intestinal signs and symptoms: anemia, neuropatia , decrease of bone density
increased risk of fractures and so on
Gastrointestinal manifestations (clasic symptomatology):
chronic diarrhea (50% of the cases) . Features at a young age are stools which
are: abundant, pasty, fatty, with a characteristic odor (steatorrhea) and during
acute diarrhea they become watery, frothy. Infections, stress and starvation
cause episodes of acute diarrhea, the so-called "celiac crisis", where quick
dehydration occurs which can lead to collapse.
recurrent abdominal pains
abdominal distension (here comes the name of the disease)
anorexia
chronic constipation
loss of weight
vomiting
flatulence
height and weight retardation
Extraintestinal manifestations (more often):
malnutrition
177
deficiency signs: iron deficiency anemia or other types of anemia,
osteoporosis (decreased bone density), rickets, delayed puberty, amenorrhea,
irritability, chronic tiredness
transaminases increase
herpetiformis dermatitis
dental dystrophy
aphthous stomatitis
chronic hepatitis
neuropathy
arthralgia
After the age of 5-6 years 50% of cases begin with extradigestive symptoms: dermatitis
herpetiformis, iron deficiency anemia, dental dystrophy, osteoporosis, chronic hepatitis and
others.
In adolescents, young adults the latent disease can be met with weight loss and diarrhea, only
with fatigue, abdominal pain, bloating, anemia or Duhring-Brock dermatitis herpetiformis.
Clinical forms:
classic form with characteristic symptoms
latent form (which seems to be more common than the classic form with atypical
symptoms - fatigue, adinamia, anemia, neuropathy, decreased bone density, increased
fracture risk, etc.)
The silent form with CD positive antibody , positive HLA, histopathological changes
compatible with CD, but without signs and symptoms which justify a celiac disease
suspicion
Latent form: positive HLA , but without enteropathy in a patients who had suffered
once of sensitive gluten enteropathy.
Potential form: has specific anti CD antibodies has positive HLA, but without
histopathological changes in the duodenal biopsy
CD Associated diseases are:
- associated conditions (after AHRQ Healthcare Research and Quality):
- High prevalence of the disease in the relatives of the patient with celiac
disease (10-20%)
- Children with DM type I (the prevalence is 3-12%)
- Autoimmune thyroiditis (up to 7%)
178
- Chromosomal aberrations (Down syndrome 3-12%, Turner syndrome,
Williams syndrome - up to 9%)
- IgA nephropathy
- selective IgA deficiency (10-20 times more increased prevalence)
- Autoimmune hepatitis (12-13%)
- Juvenile chronic arthritis
Therefore, patients with classic symptoms and those with extraintestinal manifestations
and related diseases will be tested for CD.
Laboratory:
Serological tests: anti TG2, EMA antibodies or anti DGP (antigliadin peptide). For
the interpretatation of the antibodies results, we must consider: if the total level of
IgA in serum is +(< 0,2 g/L), the diagnosis will be set according to antibodies type
IgG . Deficiena de IgA,este boal asociat cu o incidena crescut a celiakiei.
Atc anti TG2 and/ or EMA are associated with a high probability of celiac disease,
having a specificity of 98-100%. Anti TG2 antibodies with high values of > 10 times
are associated to vilositary atrophy. Therefore, when anti TG2 Atb are done of routine
and when they are 10 times the normal value, duodenal biopsy is no longer performed
but genetic testing is recommended. DGP antibodies (deamidated gliadin peptides)
have high specificity and sensitivity similar to IgA tTG IgA EmA and therefore are
used as screening. The best diagnostic test is anti-TG2 atb+ DGP atb (combined).
HLA tests - major antigens of histocompatibility HLA-DQ2 and HLA-DQ8 are useful
to exclude celiac diseases. These examinations are recommendedwhen specific Atb
for celiac disease are negative, but histopathological there are medium changes in the
bowel mucosa, when there is great suspicion of celiac disease, antibodies are
intensively positive,and the biopsy is negative, in patients belonging to the group at
risk
The genetical susceptibility for celiac disease is given by HLA class II, DQA and
DQB, genes situated on the short arm of the 6
th
chromosome. More than 95 %of the
patients with celiac disease are heterodymer HLA-DQ2 (cis [encoded by HLA-DR3-
DQA1-05:01-DQB1-02:01], or trans [encoded by HLA-DR11-DQA1-05:05 DQB1
03:01 /DR7-DQA1-02:01 DQB1 02:02]) and approximately 5% heterodymer HLA-
DQ8 (encoded by DQA1-0301-DQB1-0302). The expression of HLA DQ2 or
179
HLA-DQ8 molecules is necessary, but not enough (30-40% of the white population
have these haplotypes, but only 1%get the disease).
The biopsy will be multiple and they are taken through superior digestive endoscopy
(from D III). Biopsies by suction capsule can be made. Histopathological changes
described by Marsh are:
Marsh I infiltrative lesion; normal structure of the intestinal mucosa; -
lymphocytic inflammatory infiltrated in the villi epithelium (> 30 lymphocytes
at 100 enterocytes)
Marsh II hyperplastic lesion; increased intraepithelial lymphocytic
inflammatory infiltrated; crypts widening , | crypts depth
Marsh III the destructive lesion is present
Marsh III a partial villi atrophy, villi shortening, inflammatory infiltrated
Marsh III b subtotal villi atrophy; clear villi atrophy, but villi can be
recognized; crypts widening and rich inflammatory infiltrated are associated
Marsh III c total villi atrophy; almost total absence of villi; hyperplasic and
inflammatory lesions
- Other investigations:
Anemia (serum iron under 50%in the context of malabsorption),
decreased coagulation factors,
hypoproteinemia, Ca + + and P +3 low serum (osteoporosis)
Zn + + low, which causes "blunt taste" and loss of appetite.
Microscopic examination of the stool will highlight the unabsorbed fatty acids
(not neutral fats such as in cystic fibrosis). Determination of the fecal fat (3 days)
shows a fecal excretion over 15% in infants and above 8%.in children.
Biopsy is not recommended ed if TG2 atb are over 10 times the normal value. In other cases
biopsy is mandatory. Biopsy should be repeated after the introduction of gluten. Assessment
of therapeutic efficacy is made by serological tests
Positive Diagnosis
Presumptive diagnosis is based on symptoms and serological tests, HLA testing, duodenal
biopsy.
Differential diagnosis
It is necessary with cystic fibrosis and celiachiform syndrome which occurs in the case of
giardiasis, and long antibiotherapy (5-10% of cases with transient intolerance to gluten).
180
ESPGHAN proposes the following diagnostic algorithms in CD children:
Fig.no. Algorithm of diagnosis In children and adolescents with signs and symptoms
suggestive of celiac disease
Fig. no. Algorithm of diagnosis in children and adolescents without signs and symptoms of
celiac disease
181
Treatment
The basis of the treatment is a gluten-free regime; the following will be excluded from the
diet: wheat flour, barley, oats, rye and derivatives. Rice, corn flour, potato and millet will be
used. There is also gluten-free flour. The regime will be easily hipercaloric (+25%), with an
intake of protein and vegetable oils.
Under diet: the symptoms disappear within 1-2 weeks, histologic lesions (variable after the
degree of villous atrophy) disappear within 2 months - 5 years or more.
Additional vitamin intake is required: vitamins A, B, C, D, E, folic acid, iron and calcium.
In celiac disease crises Prednison 1-2 mg/kg/day is administered, rapid rehydration is
initiated (to avoid anhidremic collapse).
Evolution and prognosis
The evolution is long, with crises. The prognosis is reserved. Untreated, in these patients, the
incidence of lymphomas and adenocarcinomas of the intestine are greatly increased.
The "detoxification" of the gluten is tried by changing a nucleotide from the DNA chain in
the grain of wheat and creating a vaccine and also genetic modulation.
182
FOOD INTOLERANCE
DISACCHARIDE INTOLERANCE
Defition: an autosomal recessive metabolic disease, resulting from the mutation of the
specific gene (from chromosome 2, resulting in the inability of the enterocytes to synthesize
lactase.
- Can be of an infantile type - congenital alactasia- of two types
true very rare, 32 cases published in the literature up to this date
false - "physiological" intolerance that occurs in infants
- The second type is the adult type by a posttranslational defect in the synthesis of the
enzyme.
Clinical picture: there are some common and some particular elements of the disease.
The common elements are diarrhea and deficiency syndrome (in chronic forms).
Diarrhea is the main symptom; the child has 4-10 watery, frothy, yellowish stools/ day, which
are eliminated in an explosive way, and associated with perianal skin irritation and intertrigo.
The onset of diarrhea depends on the etiopathogenical shape.
It has a chronic/ recurrent character correlated with milk nutrition; disappears when milk is
excluded from the daily diet and reappears when milk is reintroduced. It can also present:
abdominal cramps, gurgling, flatulence and vomiting.
Deficiency Syndrome occurs in children who, without specifying the diagnosis, are still on
milk diet; the diarrhea becomes chronic, children present somatic deficiency, weight curve is
downward, height gain slowed or stopped, anemia, multi vitamin deficiencies.
The diagnosis is suggested by: pediatric clinical symptoms disappear after a steady diet of
removing lactose over a period of at least 2 weeks, with recurrence of symptoms when
reintroducing the lactose.
Laboratory:
determination of pH in the stool: acid pH, below 5.5 (even up to 3.8).
microscopic examination of the stool highlights incompletely digested food scraps from
all food sectors
test for reducing substances in the stool is positive
oral lactose loading test is pathological: flat curve of the glucose appears and diarrhea,
cramps, gurgling may be associated
oral glucose loading test is normal
183
expiratory test of the hydrogen is positive. In order to perform the test a 2g/kg lactose is
used, the test has a better performance if is performed after a 6-hour post; false-negative
tests may occur, especially after antibiotic treatment (hydrogen is metabolized by bacteria
to methane).
radiological examination of the digestive tract involving lactose or barium sulfate is not
indicated in children. In adult, radiolgically the The Preger triad appears: shortened
intestinal transit time, distended jejunal loops, imprecisely defined outline due to enteral
hypersecretion
determination of lactase activity in jejunal mucosa biopsies: its absence is seen in a
genetic form with a neo-natal onset and low values in other forms.
histological examination of intestinal mucosa reveals a normal aspect in the genetic form
and it is altered specifically to the causing disease as acquired.
1. Primary genetic lactase deficiency - infantile type (Alactasia)
It is an exceptionally rare disease, has an early onset, AR transmission described in a few
cases (32), with homozygous mutations (Y1390X named Fin) in 84% of cases and
heterozygous mutations (S166 fsx1722, S 218 fsx 224, Q268H and G 1363 S) in the rest of
the cases.
Symptoms appear a few days after birth, after breast feeding or formula containing lactose.
The selective, persistent, severe character, with acid and liquid diarrhea, flatulence, leads to
severe malnutrition.
Children are hungry, rarely present vomiting; some may have hypercalcemia and
nephrocalcinosis by metabolic acidosis and/or increase of calcium absorption after
administration of lactose. At the appearance of suspicion a lactose-free diet is started, and in
case the effects are positive the diagnosis is supported.
In order to confirm the diagnosis it is necessary to emphasize the deficit lactase activity in the
jejunal mucosa biopsy with normal morphology of the jejunal mucosa and molecular genetic
tests- to strengthen the diagnosis
Treatment
The treatment consists of a strict lactose-free regime, with adequate preparations: lactose-free
Nan, Lactopriv, Pregomin, Isomil, older children will receive additional lactase with
preparations containing enzyme - Lact-Aid, Lactase; lifelong treatment.
2. Primary genetic lactase deficiency - adult type (Hypolactasia) (Late-onset)
184
It is very common in humans, with different prevalence: 10-90% by geographic area and
race (5-12% at white population, up to 70% in U.S. blacks). The disease is rare in northern
Europe, as in some tribes in Africa and India where10-20% occur.
It is a post-translational defect in the synthesis of the enzyme, which becomes apparent in all
mammals after weaning. Lactase deficiency in this form is installed progressively after
infancy, clinical onset may be after 3-5 years or in adolescence, and intolerance symptoms
may develop in adolescence or adulthood. Enzyme deficiency is only partial, sometimes
allows milk consumption in small quantities (1-1 glasses), the diarrhea installing only after
the consumption of large quantities of milk.
Symptoms occur after milk consumption: abdominal discomfort (colic), flatulence, low
consistency stools, diarrhea. It is believed that 30-40% of children with DAR may present
lactase deficiency.
Treatment
Corresponding decrease in milk intake of individual tolerance, delactosed milk consumption,
lactase replacement therapy: Lact-Aid solution, Administration of calcium (for bone
mineralization) is important in these patients, noting an increased incidence of osteoporosis
secondary to milk avoidance.
Daily intake of calcium-fortified fruits (oranges) is recommended, vegetables and milk
without lactose and consumption of yogurt containing Lacto-bacillus bulgaricus and
Streptococcus thermophilus cultures producing lactose digestion.
Lactobacillus acidophilus has lactase activity and is available in sweet acidified milk, with
similar taste to milk.
3. (Secondary) Acquired lactase deficiency
It is secondary to some acute illnesses, usually an acute enterocolitis, or secondary to chronic
disease development: EGS, CF, lambliasis, b. Brohn, bowel resections, severe malnutrition,
drug enteropathies.
Pathogenetic mechanisms:
- reducing the number of enterocytes in diseases that are accompanied with villous
atrophy (EGS) or patients with jejunal resection and
- the reduction of the enzymatic synthesis of the enterocytes, due to cellular metabolic
suffering (in inflammatory bowel diseases, FC).
Diagnosis
185
Includes common criteria and variable-onset (especially in infants, not after birth), it has a
transient, non-selective nature (associated with other disaccharide deficiencies), jejunal
morphology specific to the underlying disease.
Treatment
Dietary treatment with hypo-allergenic milk or a lactose free one and a substitution treatment
with lactase preparations (Lact-Aid, Lactrase, etc), are required for a variable period,
depending on the causing disease.
ALLERGIES AND FOOD INTOLERANCES
Definition
There are sensibilizations of the mucous membranes at one/ more food components, more
frequent sensibilizations associated with gastrointestinal manifestations are given by cow's
milk protein or soy products.
Intolerance (allergy) to cow-milk (CM) proteins (CMPI)
It is characterized by a group of acute "allergic" or chronic manifestations, malabsorption
syndrome produced by CM protein sensitization. Cow's milk contains 20 proteins, 5 of which
have proven antigenic properties: -lactoglobulin, -lactalbumin, casein, bovine
seroglobulina and bovine serumalbumina.
Clinical symptoms:
Digestive manifestations dominate the picture: brutal, explosive, bloody diarrhea or
abundant, soft, coarse stools with vomiting.
The acute symptoms appear after eating, often a shock emerges, hypotonia, disorders of
consciousness, gray pale, peribuccal cyanosis; ymptoms disappear within a few hours,
reappear after feeding.
The chronic form is insidious, diagnosed late, the rarer being the forms prone to paralytic
ileus, necrotising enterocolitis, exudative enteropathy, colic symptoms: inflammatory
proctocolitis in newborn, hemorrhagic colitis.
Extradigestive manifestations are varied with:
- anaphylactic shock,
- rare respiratory manifestations: asthmatic bronchitis, pulmonary infiltrates, allergic
rhinitis,
- dermatological symptoms: eczema, hives, Quinke swelling, dermatitis herpetiformis or
- controversial symptoms, such as sudden infant death, severe insomnia, myocardial
infarction, nephrotic syndrome.
186
Diagnosis
It is based on the disappearance of symptoms after exclusion of CM and recurrence in 48
hours after milk reintroduction, after eliminating other causes of digestive disorders.
It is useful for diagnosis:
- the presence of red blood, Charcot-Leyden crystals, leukocytes in the stool,
- loss of plasma proteins in exudative enteropathy,
- increase of the level of anti-milk serum antibodies
- lymphoblastic transformation test (involvement of cellular immunity)
- intestinal malabsorption research
Treatment
- is essentially dietetic, through CM exclusion, its derivatives and foods containing it
- the use of soy formulas (Humana SL, Nutry-Soy, Lactopriv),
- synthetic formulas and
- supplementing the diet with meat (beef, chicken), vegetable oil, glucose for caloric
intake
- good results are obtained by refilling with mother milk
- in severe forms parenteral supine then elemental diet or APT.
Primary prophylaxis is to promote natural feeding
Soy protein intolerance
May be isolated or associated to CMPI.
Clinically
The onset occurs in the moment of introduction of a soy food.
Symptoms: watery diarrhea, vomiting, anaphylactic shock.
Laboratory: hyposideremic hypochromic anemia, hypoproteinemia, acid pH of the stool and
unsteady blood in stool may occur
Treatment: exclusion of soy proteins from the diet.
Eosinophilic gastroenteritis
It is a rare disease; represented by sensitization to food.
Clinically children present abdominal pain, vomiting, diarrhea after ingestion of certain food.
Associated atopic symptoms as rhinitis, asthma, and eosinophilia can be observed, suggesting
the allergic base of the disease. Protein loss can be produced determining decreased albumin
and Ig.serum
The diagnosis is suggested by:
- recurrent symptoms,
187
- eosinophilia,
- endoscopy with biopsy (gastric and duodenal lesions, eosinophilic congestion of the
lamina propria, shortening of villi, bleeding, muscular involution determining
strictures)
- and changes of the serous until ascites
Evolution
It is often chronic sometimes with severe, exacerbations; elimination of the incriminated food
can help, but most patients require systemic corticosteroids.
Food allergy
Sensitization reactions after food ingestion are based on immune mechanisms, differ from
commonly occurring adverse reactions and are given by food toxins and non-immune factors,
through pharmacological and biochemical mechanisms.
Etiology
Involved allergens are different with age.
Atg sources at infants are LV, cereals, citrus, bananas, vegetables, meat poultry and beef.
Atg sources in older children: eggs, chocolate, strawberries, walnuts, peanuts, fish, pork and
shellfish.
Hypersensitivity phenomena can alleviate when advancing in age.
Clinical symptoms
Symptoms of allergic reactions to foods are: urticaria, angioedema, gastrointestinal disorders,
severe asthma attack, even anaphylactic shock.
The response to an allergen can be immediate, after a few minutes or delayed (2 hours).
In case of late manifestations, problems of differential diagnosis with non-allergic reactions
may occur.
Syndromes associated with hypersensitivity to food:
Angioedema often accompanied by urticaria, is manifested as a swelling of the lips and
periorbital mild arthralgia, malaise, in severe cases swelling of the tongue, pharynx, larynx,
with joint swelling and death by suffocation.
Anaphylaxis is an immediate reaction with dizziness, pallor, paraesthesia, generalized
pruritus, palpitation, tachycardia, syncope, signs of pulmonary edema, severe asthma attack,
and vascular collapse.
Gastrointestinal intolerance presents symptoms attributed to "allergy" but the basic
mechanisms are unclear: nausea, flatulence, bloating, abdominal discomfort, diarrhea; in
188
severe cases incoercible vomiting occurs, colic, bloody diarrhea, dehydration, these repeated
episodes causing dystrophy and growth retardation.
It is unclear whether the tension asthenia syndrome is associated with an allergic
mechanism; nervousness, insomnia, fatigue, pallor, ringed eyes, vague abdominal pain,
headache, atopic symptoms to abundantly ingested food, (eggs, LV, cereals, chocolate, pork)
may occur.Allergic rhinitis, asthma, atopic dermatitis and urticaria may be signs of allergic
reactions to food as well.
Laboratory
- eosinophilia is observed in the fecal mucus and blood
- skin tests present strongly positive reactions which may have an aetiological
significance but negative reactions DO NOT exclude an allergy
- serological tests have about the same value
- food challenge tests are rarely used, only in less severe forms.
The treatment consists of:
- removing foods that cause allegric reactions and ensuring an appropriate nutritional
intake.
- administration of breast milk up to the age of 1
- late introduction of solid foods
- using goat milk (!anemia), meals based on soybeans, avoiding the food that triggers
the allergy up to 8-10 years, later being reintroduced carefully, under supervision
- if allergic symptoms may occur upon reintroduction, these foods will be avoided
forever
Prophylactic treatment
Na cromoglycate (Nalcron), Ketotifen po in extended cures (variable results) can be used,
lowering the frequency and intensity of reactions.
Symptomatic and etiopathogenic treatment
It is based on the symptoms.
Prognosis
It is good if the foods can be identified and are no longer given.
189
ACUTE DIARRHEA OF INFANTS AND SMALL CHILDREN
Definition
Acute gastroenteritis (AGE) is defined by softening stools and/ or an increase in discharges
( 3 in 24 hours), with or without fever and vomiting. The diarrhea lasts less than 7 days, but
no more than 14 days. However, a change in stool consistency in relation to the consistency
of previus stools is more predictive for diarrhea than the number of stools, especially in the
first month of life (ESPGAN definition).
We have to mention that in the first 3 months of life infants have more stools depending on
the type of food they are given.
Persistent diarrhea is defined as diarrhea episodes that begin as acute ones and last 14 days.
These episodes represent 3-20% of the diarrheal episodes in children under 5 years and up to
50% of the total episodes of diarrhea.
Epidemiology
The incidence of diarrhea varies between 0.5 - 1.9 episodes/ child/ year in children aged
under 3 years in Europe.
Etiology
- viral - the most frequent agents rotavirus 10-35% (with the highest incidence in the
cold season (from october until May), norovirus, adenovirus
- bacterial the most frequent agents Campylobacter jejuni (4-12%) and Salmonella spp
(5-8%), more rarely E. Coli (EPEC, ETECT, EHEC, EAggEC), Yersinia, Shigella,
cholera. Bacterial diarrhea occur mostly in summer, with two peaks in May-June and
September-October.
- parasitic Giardia lamblia and Cryptosoridium in immunocompromised children,
Entamoeba hystolitica, Trichiuris trichiura, Strongyloides stercoralis (rarely).
If AGE occurs at a higher incidence than expected, we may speak about an epidemic
diarrhea.
Age-related etiology is presented in the following table:
Table ccc Acute diarrhea etiology
< 1 year 1-4 years > 5 years
Rotavirus Rotavirus Campylobacter
190
Norovirus
Adenovirus
Salmonella
Norovirus
Adenovirus
Salmonella
Campylobacter
Yersinia
Salmonella
Rotavirus
Table cccc Risk factors for severe and/or persistent diarrhea:
Severe diarrhea Persistent diarrhea
The severity of the diarrhea, linked to the
degree of dehydration and vomiting
Loss of appetite, fever, vomiting and
mucus in stools
SDA in infants less than 6 months old
associated with rotavirus infection (most
severe pathogen of infant diarrhea)
Under 6 months old Under 6 months old
Rotavirus, norovirus, astrovirus,
enteroagregative E. Coli in industrialized
countries
Poor socio-economic conditions
(developing countries)
Poor socio-economic conditions
(developing countries)
Collectivity (care centers)
Congenital or acquired immune
deficiencies (HIV) favor persistent
diarrheal episodes, (opportunistic agent -
Crystosporidium parvum)
1. Predisposing factors
2. ex constitutione: newborn, small, premature baby, diatheses (lymphocytic, exudative
allergic).
3. Ex curatione: personal hygiene, house, season, the use of hardening factors such as water,
sun, air, vaccination, etc.
Pathogenesis. The pathogenesis and severity of the bacterial diarrhea depends on the
production of bacterial toxins (Salonella, Bacillus cereus), which produce secretory diarrhea
191
(cholera, E. Coli, Salmonella, Shigella), cytotoxins (Shigella, S. Aureus, C. difficile, E. Coli,
C, jejuni), and are invasive germs or multiply in food.
Enteropathogens agents can lead, at the level of the intestinal mucosa, either to an
inflammatory response or to a non- inflammatory response.
The non-inflammatory response by enterotoxins (ie "exudative" noninvasive because
germs do not penetrate the mucosa and do not damage it) or superficial adhesion/ invasion
produces diarrhea by increasing the adenyl-cic from the intestinal mucosa and thus cAMP
increases, inhibits the absorption of NaCl, but have no effect on the glucose pump - Na,
leading to an increased secretion of water and electrolytes (Na
+
, K
+
, Cl
-
, bicarbonate). The
cytoskeleton rearrangement is affected by altering the flow of water and electrolytes. This
type is found in cholera, being produced by E. coli (ETEC, EPEC, LT, ST), Clostridium
perfringens, Bacilus cereus, S. Aureus, Rotavirus, Giardia lamblia as well.
a. The inflammatory response is caused by bacteria directly invading the bowel or
sometimes cytotoxins with penetration into the lumen of fluids, proteins, cells
(erythrocytes, leukocytes): E. Coli (EIEC, EHEC), Campylobacter, .a. An alteration of
the cell morphology is produced with the decrease of the glucose-Na pump function and
NaCl absorption. For example ETEC colonizes and adheres to intestinal enterocytes at the
level of the fimbriae and induce the hypersecretion of fluids and electrolytes by toxins 1
and 2.
b. Mechanism of penetration acts at the level of the distal small bowel, causes enteric
fever, the appearance of leukocytes in feces. The diarrhea caused by this mechanism is
given by Salmonella typhi, Yersinia, Campylobacter fetus. Salmonella behaves somewhat
differently in newborns and infants. Some types penetrate the epithelium until the lamina
propria where they produce inflammation (therefore oral antibiotics are ineffective) but
easily penetrate blood and lymphatic vessels, leading to septicemia.
Symptoms. The onset of the disease is made by a prodrome, in which the infant presents:
anorexia, stagnant growth rate, and behavioral changes (malaise, restlessness, sleep patterns
change), and in some change in stool appearance and nappy rash.
High fever, blood in the stool, abdominal pain, CNS symptoms suggest a bacterial etiology
(shigella, salmonella), and vomiting and respiratory withdrawal symptoms suggests the
etiology of a viral disease. However, in AGE with rotavirus more severe forms of the illness,
vomiting and dehydration can be met.
During the state period the triad usually occurs: anorexia, diarrhea and vomiting.
Vomiting, which is not mandatory, is more frequent, when it occurs
192
Stools, more frequent in numbers, 3-5/day are aqueous (las leaves large halo on the diaper)
of fermentation (light yellow, airy with a sour, acidic smell). Rarely may be muco-coarse,
semi consistent ones
Some children present abdominal colics as well, (rub their heels), flatulence. The growth
rate decreases. If nothing is done, the symptoms of acute dehydration may install.
Fever may be absent, or may be the consequence of dehydration. Infants with 6 to 10 stools/
day are not in danger of dehydration if intake is adequate. Those with more than 10 stools/
day are at risk of dehydration even in case of an adequate intake. Premature infants, severely
malnourished ones and other handicapped infants do not have usually fever.
Clinical forms
1. Etiologically unlabeled, nonspecific acute diarrhea: insidious or brutal onset, with
prodrome of anorexia, behavioural changes, weight stagnation, nappy rash., vomiting,
thirst fever
2. Acute enter-infectious diarrhea
- bacillary dysentery (shigelloza) - sudden onset with fever, chills, sensory disorders,
convulsions, colic, tenesmus, pathological stools.
- Salmonellosis: gastroenteritis form and enteric fever
- acute diarrhea with E. Coli - high fever, vomiting, dehydration, metabolic acidosis,
watery, smelling, acid green, explosive stools.
3. Acute viral diarrhea, gastroenteritis - occurs during winter, it is given by rotavirus The
onset is sudden, with fever, vomiting, watery diarrhea, myalgia, rush, respiratory catarrh.
4. Parenteral diarrhea - "dyspepsia" secondary ITU, otitis, pneumonia. It is resolved after
the treatment of the underlying disease.
Positive diagnosis
It is based on clinical signs and simple laboratory tests.
a) Stool test which highlights only constant pathogenic specific bacteria; has the
disadvantage that it is obtained late (~ 72 h). Remains the primary means of
determining the etiology for entero-bacteria (Vibrio cholerae, Salmonella, Shigella, E.
coli, Proteus, Pseudomonas). In 50-80% of BDA in infants, stool test remains negative
(viral etiol.).
b) The pH of the stool is normally 5-8, and a pH below 5 shows an intolerance to glucose
c) The virological examination of the stool is useful for diagnosis, although it is less
accessible; special kits are sold for rotaviruses.
d) Fecal examination may reveal the causative agent in parasitic diarrhea.
193
e) Fecal examination consists of highlighting leukocytes in stool using methylene blue
stain; normally there are no leukocytes in the stool; 0 leukocytes/ field in infants are
allowed. Leukocytes can appear in the stool in bacterial infections.
f) Immunoassay tests: ELISA, ROTALEX
g) The Gregersen reaction allows highlighting occult bleeding (product harvested after 72
h of food without meat)
h) Blood count, Ionogram, microASTRUP; Biochemistry: urea, creatinine
i) Bacteriological examination from products other than stools
If the diarrhea persists more than two weeks, and stool cultures are negative, radiographic
examinations and endoscopy should be carried out for harvesting biopsy material.
Differential diagnosis is carried out with:
- osmotic diarrhea (much sugar in the diet), is a "false diarrhea"
- food abuse (especially cold drinks, spicy or fatty food),
- food poisoning,
- acute exogenous poisoning,
- intussusception,
- perforated Meckel diverticulum,
- parenteral diarrhea,
- acute episodes of diarrhea in the case of:
malabsorption
malnutrition
allergy (in particular cow's milk protein intolerance)
prolonged therapy with antibiotics
Evolution and complications. Most infectious diarrhea are self-limiting; they heal in about
two weeks, the period for rebuilding intestinal mucosa, of the enterocytes. It is very important
to assess the degree of dehydration (mild, moderate or severe) associated to diarrhea in order
to provide appropriate treatment.
The child will consult a doctor if he/she has > 8 diarrheal episodes/ day, persistent vomiting,
severe underlying disease, age < 2 months.
The child will be admitted to hospital if he/she has: shock, severe dehydration (> 9% of body
weight), neurological changes, incoercible vomiting, failure to rehydrate with ORS, suspicion
of impaired operation.
Another possible evolution are recurrences. We are talking about a chronic evolution, usually
after 2-3 weeks of poor outcome in treatment.
194
Two complications are more common as children are smaller:
- acute severe dehydration syndrome ascending to collapse and
- septicemia, by generalized infection.
The prognosis is favorable.
Treatment of acute diarrhea
Basic measures are- adequate diet selection, oral rehydration, enteral nutrition,
supplementation with micronutrients (zinc) and additional therapies such as adjuvant therapy
and probiotics. Drug therapy and parenteral rehydration are reserved for severe cases.
1. Dietary treatment
Oral rehydration
The first line of treatment in AGE is oral rehydration with ORS solution. The one
recommended by WHO is that with 75 mmol/l Na, but the one recommended by ESPGHAN
is the hypoosmolar one with 60 mmol/l Na. It is the therapy of choice and it is sufficient in
diarrhea produced by Vibrio cholerae, but also in the non choleric one. Hypoosmolar solution
reduces the volume of stools, vomiting, and decreases the need for intravenous fluid
supplements. ORS solution with rice can be administered as well respectiv;it is recommended
to ORS solutions with probiotics.
Its indications: acute diarrhea, SDA gr. I and II without vomiting, in the presence of
peristalsis.
Way of administration
In the first 3-4 h 10 ml/ kg/ hour is given in the mild forms and 20 ml/kg/hour in medium
forms, or 50 ml/kg during the first 4 h in mild forms and 80-100 ml/kg during the first 6 h in
medium forms.
Rehydration with administration of 50 ml ORS will be continued for each modified stool
under the age of 2, and 100 ml ORS for each modified stool for children over 2, until
recovery, or 20-50 ml/ kg after 3-4 hours.
Oral Rehydration Solutions administration rules:
1. Chilled or frozenoral rehydration solution (ORS) is tolerated
2. Give ORS with a spoon rather than with a bottle
3. Consider adding flavor to ORS
4. Gelified ORS, if available, is more palatable
5. Adding honey to ORS may be of benefit
Nutritional interventions
Breast-fed infants will continue to receive breast milk.
195
The maintanance of natural feeding is recommended and rapid return to age-appropriate
nutrition in order to prevent villous atrophy and damage of the luminal enzyme production.
In children with mild or moderate dehydration normal diet is recommended after 4-6 hours
from the onset of rehydration. In these cases there is no need to dilute the formula. Most
children can continue eating the formula with a normal amount of lactose, the lactose-free
formula benefits compared to the standard ones are negligible. Soy-based formulas or
hydrolyzed protein ones are indicated only in the first 2 months of life.
The BRAT diet (bread, rice, apple, toast) is not recommended and sweetened juices should
not be used.
When the rehydration is complete, appropriate nutrition will be resumed continuing the
administration of rehydration solutions in order to compensate any loss due to vomiting or
stools and for maintenance.
Restrictive diets should be avoided during acute diarrheal episodes. Breastfeeding will
continue "on demand" even during oral rehydration. Infants too weak to be able to consume
will receive milk or formula through nasogastric tube. Usually lactose formulas are well
tolerated. If there is clinically significant lactose malabsorption, a lactose-free formula can be
used. Alternative strategies to reduce the lactose content in children with extended diarrhea
include the adding of different cereals in the milk or replacing milk with fermented products
(yogurt).
It was seen that there were no differences between early and late refeeding as regards
unscheduled intravenous fluid therapy, vomiting, persistent diarrhea, duration of
hospitalization, total stool output, percentage of weight gain at 24 hours or at resolution of
illness, and hyponatremia. In addition, early refeeding was associated with a shorter duration
of diarrhea.
In several European and non European countries, attempts have been made to find a food to
counteract diarrhea. In other words, is there something that can help resolve this problem
sooner in children with AGE? Various foods have been tested for their antidiarrheal effect.
These include yoghurt, staple foods, cereal-milk mixtures, solid foods, and more recently,
amylase digestive starch. Although some studies found evidence of a limited advantage for
selected nutrients, there is no agreement about whether a particular food can be useful in the
treatment of diarrhea. Consequently, this approach is not included in the treatment of
gastroenteritis.
Rehydration in a hospital setting
196
When oral rehydration is not feasible, rehydration by the nasogastric route or IV route should
be considered. The nasogastric route is as effective if not better than IV rehydration.
Nasogastric rehydration is associated with significantly fewer severe adverse events and a
shorter hospital stay compared with IV therapy and is successful in most cases. In particular,
its use is associated to prompt rehydration, reduced number of hospitalizations, better
replacement of bicarbonates, reduced number of episodes of diarrhea and vomiting, and
overall a better gain of weight at discharge.
Adjuvant and symptomatic therapy
a). Probiotics
Probiotics may be an effective adjunct to the management of diarrhea. Available data suggest
the use of probiotic strains with proven efficacy and in appropriate doses for the management
of children with AGE as a adjunct to rehydration therapy: Lactobacillus GG, Saccharomyces
boulardii.
Lactobacillus GG:
- reduces duration of diarrhea
- highly effective for rotavirus AGE
- reduces the risk of diarrhea at 48 and 168 h
- no studied effects on fecal output
Saccharomyces boulardii
- reduces duration of diarrhea
- reduces number of evacuations
- reduces the risk of diarrhea at 48, 144 and 168 h
- no studied effects on fecal output
b). Adsorbers
197
An extract of clay is given (Smecta) 1,5 g ( sachet) 1-3 x/day in foods for infants and 1-2
sachets/ in children over 1 year. You can also use Hidrasec 2 x sachet/ day <1 year and 2-3
x 1/day in children> 1 year.
Recadodril can be used in the management of AGE.
c). Zinc supplementation
There is evidence that zinc supplementation in children reduces the duration and severity of
the diarrhea. WHO and UNICEF recommended for children in areas of risk the administration
of oral zinc preparations for 10-14 days during and after diarrhea (10 mg/ day less than six
months and 20mg/day over 6 months).
d) Collapse is to be controlled by rehydration in severe cases.
e) Vomiting - Plegomazin 1-2 mg/ kg/ day or Phenobarbital 5-10 mg/ kg im. Ondansetron
may be used - non-toxic effective antiemetic - a sublingual dose or 1 effervescent tb. (8-15
kg: 2 mg, 15-30 kg: 4 mg over 30 kg: 8mg). Beware because Ondansetron may increase the
QT interval on ECG, risk of death
f) Fever is to be fought by physical methods and administration of the well- known
antithermics (Paracetamol).
g) Flatulence is fought by local heat, rectal probe or 0,2-0,3 ml Miostin S.C. or I.M. de 1-2 x.
In some situations K are given, bloating being a symptom of hypokalemia.
h) Motility inhibitors (loperamide) controversial, ESGHAN, not recommended
2. Drug treatment
Eutrophic infants, in mild/ medium forms of the disease, do not require medication, the oral
rehydration being sufficient. Most infectious diarrhea is self-limiting. In most cases of BDA,
antibiotic treatment is NOT necessary, as the etiology is a viral one (50-80%), even in the
presence of bacterial etiology, the antibiotic treatment may not be beneficial, producing side
effects. Antibiotic therapy is indicated in patients infected with a pathogen agent, agent that
acts through an invasive mechanism, if the patients presents fever, severe colicky abdominal
pain, stool with blood or pus, digestive occult bleeding (Gregersen positive reaction),
leukocytes in stool, in new born and in lambliasis. It is especially recommended in
shigellosis, salmonellosis, forms of dysentery with Champilobacter gastroenteritis
The following can be administered:
- Furazolidone 8-10 mg/ kg/ day in three doses for 3-5-7 days
- Biseptol 6-8 mg/ kg/ day in 2 doses, 3-5-7 days
The most commonly used oral antibiotics are:
- Ampicillin 100-200 mg/ kg/ day in 4 doses for 3-5 days
198
- Amoxicillin 50 mg/ kg/ day in four doses over 3-5 days
- Colimicina 125,000 u/ kg/ day in 4 doses for 3-5 days
- Negamicina (Neomicyna) 100 mg/ kg/ day in four doses over 3-5 days
- Ciprofloxacin 15 mg/ kg/ day in 2-3 doses/ day for 5-7 days (especially in infections
with salmonella and invasive shigelle)
In the traveler's diarrhea, for Clostridium difficile the following medication is recommended:
- Vancomicyn 40 mg/ kg/ day in 4 doses, 10 days
- Metronidazole 15 mg/ kg/ day in 3 doses, 10 days
and for Entamoeba histolytica
- Metronidazole 45 mg/ kg/ day in 3 doses, 10 days
At present, effective antibiotic agents for shigellosis include third-generation
cephalosporines, azithromycin, nalidixic acid, and fluoroquinolones. Trimethoprim-
sulfamethoxazole and ampicillin, which were the classical antibiotics for Shigella, should be
considered only if the strain isolated is susceptible to those specific antibiotics.
In BDA short-term administration of these drugs is recommended (in order to avoid
resistance), the antibiotic is chosen until DST arrival based on the experience of the
physician, in severe cases concomitant therapy is administered.
Prolonged antibiotic treatment will be associated with B vitamins, mycostatics (Stamicin
50,000 IU/ kg/ day) and vitamin K (1 mg/ kg/ week).
ACUTE DEHYDRATION SYNDROME (ADS)
The syndrome produced by the loss of water and electrolytes is called acute dehydration
syndrome. A body, the younger, the more water it contains. Water represents a large
percentage of body weight, so: in prematures 80%, in newborns 78%, in infants 65%, while
in adults 60%.
Water distribution throughout the fluid sectors is as follows:
in infants:
65% 25% Extracellular sector (E.C.S.) 5% compartment (plasma compartment
20% compartment
(interstitial comp.)
40% Intracellular sector (I.C.S.)
199
after the age of 1 year, fluid distribution by sector is similar to adults:
60% 20% E.C.S. 5% plasma compartment
15% interstitial compartment
40% I.C.S.
(There is also a transcellular compartment made up by L.C.R., synovial, pleural, pericardial,
intestinal fluid with a lower practical role and which is taken into consideration only in case
of ileus, massive pleural effusion , etc.) A rapid weight loss (24-36 hours) and 1% of body
weight means a loss of water. Water, however, does not circulate"freely" in the body, but as
an ionic solution (linked by electrolytes) and much less in the form of colloidal solutions
(linked by proteins).
Therefore, any loss of water means as well loss of electrolytes. Dehydration means not only
loss of water, but a hydro- electrolyte disorder as well (hydromineral).
Given the peculiarities of the hydromineral metabolism in infants and toddlers (low resistance
to thirst, more lively exchange of water, etc.) dehydration retention of water and electrolytes
(edema)( in the pathology of the adult) prevail.
Causes
1. Determining causes: insufficient intake (thirst, starvation); exaggerations in removing
water and electrolytes by physiological methods: a. intestinal (diarrhea, vomiting), b. skin
(abundant sweating), c. pulmonary (polipnee) and/ or reducing intake (anorexia, intolerance,
abolition in swallowing); other diseases: renal, endocrine, medications causing polyuria
(diuretics, lithium salts, hypokalemia, hypercalciuria).
2. Favoring causes: young age, constitutional diatheses, prematurity, rickets and dystrophy,
diabetes.
Diagnosis
The syndrome has two aspects, a clinical and a pathophysiological one.
From a clinical point of view, there are three degrees of ADS, stages of severity and also
developmental stages
ADS gr. I - mild dehydration
In infant (description model) represents a weight loss up to 5% of the total body weight, the
child is more anxious/ drowsy, more apathetic/ agitated, thirsty, his lips and the tongue - "are
200
somehow" drier, minor symptoms, usually go unnoticed, the only objective sign is the fact
that the tongue loses its shininess.
ADS gr. II - medium dehydration
Losing weight is between 5-10% of the total body weight, with the same symptoms as in
ADS gr. I, but more pronounced, agitation, drowsiness, fried lips, dry tongue; decreased
turgor occurs in addition (persistent), sunken (depressed) fontanelle (if still open).
ADS gr. III - severe dehydration
It is a weight loss of more than 10% of the total body weight, symptoms from ADS gr. II are
more pronounced, further (memotehnic one/ more Cs): C - disorders of consciousness
(restlessness, drowsiness, torpor, sleepiness) - up to coma, C collapse or C convulsions. It
is enough to have signs of dehydration and 1 C for a severe dehydration. Some authors call it
"syndrome" only ADS gr.III (emergency). Toxicosis is an ADS gr. III of a digestive origin.
Infants and toddlers, at losses of over 15% evolve rapidly to death (an adult can withstand the
loss of abou 27%). High risk categories are malnourished premature, small babies (under 3
months). Fat children are more hydrolyzed (fat is poor in water). Depending on the particular
hydro-mineral metabolism, rates of water loss are lower: mild dehydration - up to 3%,
medium dehydration 3-8%, severe dehydrationmore than 8%.
At adolescents and in adults, a 3, 6 up to 9% is allowed.
Table CCCC Clinical dehydration scale
Characteristics 0 1 2
General
appearance
normal
thirsty, restless, or lethargic but
irritable when touched
drowsy, limp, cold, or
sweaty, comatose or not
Eyes normal slightly sunken very sunken
Mucous
membranes
moist Sticky dry
Tears tears Decreased absent
Score of 1= no dehydration
Score of 1 to 4= mild/moderate dehydration
Score of 5 to 8= sever dehydration
(Bailey B, Acad Emerg Med 2010)
From the pathophysiological point of view three forms are recognized, based on water
movements that attract major changes in ions: Na + (the ion of the extracellular space), K
+
201
(the ion of the intracellular space). It disrupts the acid-base balance, Cl- concentration,
bicarbonate (the concentration varies inversely on the anion column), and of H
+
.
Table zzzz Changes in ions
Cations+ (B) Anions- (Ac) Total
Na+ 140 mEq/l Cl- 110mEq/l - acidosis
K+ 5 mEq/l HCO3- 25 mEq/l - alkalosis
and Ca
++
, Mg
++
... SO4
-
... 310 mEq/l
The sodium is the main electrolyte of the extracellular space, the basic element of the
pathophysiological classification of dehydration. There are 3 forms.
1. Hypernatremic Dehydration (hypertonic, intracellular)
The plasma sodium is above 150 mEq/L (N = 140 mEq/L), the body loses proportionately
more water than Na
+
, children are febrile, thirsty, the skin and mucous membranes are dry
(~hot), wrinkled tongue, H-irritability, agitation prevails, the pulse is more rapid, the TA is
relatively normal for a long time, signs of water loss are predominant intracellularly and for a
while the plasma compartment of E.C.S is relatively well preserved, shown by the pulse and
TA; usually hyperglycemia occurs (poor utilization of glucose by dehydrated cells), or
hypocalcemia (the cause is unclear). It is estimated that this form represents ~ 20% of total
dehydrations.
Causes: the use of inappropriate infusion concentrates to restore dehydration, a renal
concentrating defect with the loss of free water. The excess of glucose, urea or mannitol can
cause the same problems as the excess Na +.
2. Hyponatremic dehydration
The plasma sodium is below 130 mEq/L, is as hypotonic, extracellular form, the body loses
proportionately more water than Na +. Children are afebrile, refusing food and water, the skin
is wet, cold, decreased turgor, apathy, drowsiness prevail, to coma, the pulse is rapid (without
fever), low TA, frequently progresses to collapse. In this form we meet water loss symptoms,
predominantly extracellular ones; the plasma and interstitial compartment suffers faster and
more intense, frequently occurring seizures (hyponatremia) and cerebral edema. Represents
202
5% of total dehydration, is the most "noisy form, fastly connected to the plasma
compartment, therefore some admit small percentages in this form - 3, 6, 9%.
Causes: incorrectly replaced enteral losses, only with water, tea, fruit juice, i.v. correction of
the loss of "free water", the solution of glucose or solutions with a low Na
+
content.
3. Isotonic/isonatremic dehydration
The plasma sodium is relatively normal (130-150 mEq/L), the body loses evenly water and
Na +, the clinical signs of dehydration are as hypotonic ones, with dry skin and mucous, the
turgor is not so low. It represents about 75% of the dehydration, the majority begin with
isotones, almost all body fluids (exception saliva, tears) being isotonic with plasma (fluid
homeostasis).
Assessment of dehydration:
- capillary refill time (> 2 seconds)
- skin turgor
- respiratory rate
These are the three best individual examination signs for assessment of dehydration.
Treatment
Etiological treatment treatment of the condition which led to dehydration: acute diarrhea,
vomiting, pneumonia, etc..
Pathogenic treatament of the ADS. The pathogenic treatment should be initiated always in the
presence of ADS, being in front of a state of hypovolemic shock. The main purpose is to
preserve functional the plasma compartment, volemia (relatively stable compartment and
absolutely necessary to the homeostasis of the body).
In practice dehydration treatment is confused with rehydration, replacement of lost water and
electrolytes.
There are two methods for rehydration: oral (per os) and parenteral (i.v.)
Oral rehydration - see BDA
Indications: ADS gr. I and II without vomiting, with peristalsis
Parenteral rehydration
Indications: ADS gr. III, ADS gr. I+II with continuous vomiting and if the patient can not
receive oral treatment (stomatitis, burning, and so on).
Venous access is difficult in the newborn and infant, peripheral veins are collapsed.
Other avenues of approach are the superior longitudinal sinus (if the fontanelle is open), tibial
bone puncture, discovery of the cephalic vein in the arm; infusion line installed will be kept
for 24 hours.
203
Parenteral rehydration methods:
A. Standard rehydration
The method comprises administering electrolyte solutions (Ringer, Ringer's lactate, Starter,
and others), n order to correct electrolyte and acid-base disturbances during 24-48 hours.
B. Directed rehydration
Method of fineness; applied if standard rehydration fails.
Correction of electrolyte and acid-base disorders is based on data obtained by flamfotometry
(plasma and urinary ionograma), microASTRUP parameters.
A. The standard method
A.1. Calculation of current needs (maintenance ratio)
A.1.1. Water needs, resulting in energy metabolism:
- between 3-10 kg body weight ...100 kcal/kg
- between 10-20 body weight 1000 kcal + 50 kcal for each kg > 10
kg
- > 20 kg ..1500 kcal + 20 kcal for each kg > 20 kg.
Because for 100 metabolized kcal 100 ml water is needed, the above formula also applies
to determine current needs of water.
A simplified formula (Chicoine, Ayotte) according to age:
- under the age of 1: 90 ml/kg/day
- over the age of 1: (85 ml 3a)/kg/day, a = age in years
A.1.2. Current needs of electrolytes, resulting also from energy metabolism, respectively loss
of electrolyte to 100 metabolized kcal, thus:
Table xxxxxx Loss of electrolyte
Way Water Na (mmol) K (mmol)
Perspiration 15 0 0
Sweating 40 0,1 0,2
Feces 5 0,1 0,2
Urine 65 3,0 2,0
Total 125 ml 3,2 mmol 2,4 mmol
Considering that 15 ml of water comes from the intermediary metabolism, the following ratio
is toi be taken into consideration: 100 ml water + 3 mmol Na + 2 mmol K.
204
Reported per liter, the current needs of electrolytes are:
1000 ml + 30 mmol Na + 20 mmol K
Fanconi's solution (1/5 normal saline solution + 4/5 glucose 5%) covers the current
necessities of Na, making 30 mmol Na/L and 30 mmol Cl/L (plus an energy intake by those
40 g glucose/1 L).
A.2. Deficit calculationcitului (of losses)
A.2.1. Water loss. It results from the percentage of weight loss (by weighing). If someone lost
"on scale" 1 kg, it means he lost 1 liter of water. If he has not been previously weighed,
assessment is made by clinical appearance, respectively ADS gr. III over 10%, ADS gr. II: 5-
10%; ADS gr.I: 3-5%.
A.2.2. The loss of electrolytes. It is calculated using Darow-Viallates scheme so: at 100 ml
of water lost by various means, the following electrolytes are lost:
Way Na (mmol) Cl (mmol) K (mmol)
Vomiting 10 10 2
Diarrhea 6 6 6
Sweating (fever) 2 2 2
If losses occur in several ways, an average is made in the first place. (i.e. 100 ml is lost due to
vomiting and diarrhea, meaning 10 + 6 = 16/2 = 8 mmol Na).
Standard methods take into account some mandatory rules. In addition to current needs the
following must be known:
a). The duration of dehydration (affects, in time,the hydro sectors)
The duration of dehydration % ECS loss % ICS loss
< 2 days 75% 25%
> 7 days 50% 50%
2-7 days 60% 40%
b). The composition of hydro sectors (it is very different)
- ECS: Na = 140 mEq/L; K = 5 mEq/L
- ICS: Na = 10 mEq/L; K = 160 mEq/L
Principles of parenteral rehydration:
- Fast filling and completion of the circulating volume with an isotonic solution with
LEC (normal saline solution, Ringer, Ringer-lactate, Starter)
205
- Replacing deficit and current needs of water and electrolyte with a solution made
according to the severity and type of dehydration (hypo, hyper, isotonic) solution
which is administered 24-48 hours.
- Concomitant administration of both the deficit and the current needs of water and
electrolytes, as far as oral administration is not optimal.
The first stage is to combat hypovolemic shock (collapse), because dehydration decreases
the volume of ECS leading to the decrease of the tissue perfusion with impaired renal
function, compensatory tachycardia and lactic acidosis.
In the decrease of circulating volume, the child responds by tachycardia, keeping TA before
dehydration. Therefore, a significant decline or a TA crash is a sign of collapse.
20 ml/kg i.v. (PEV) crystalline solutions (normal saline solution, Ringer sol., etc) or plasma
substitutes (dextrans, products of gelatin, 5-10% of human albumin) are is urgently
administered in bolus and it is repeated, if needed, until restoring the blood volume
(maximum is 60 ml/ kg).
If circulation is not restored after the administration of 40 ml/kg isotonic solution, the
existence of a sepsis, cardiogenic shock or occult bleeding must be infered.
In anhidremic shock (as well as in the haemorrhagic one) the loss of the interstitial
extracellular fluid must be taken into account (LEC), the one that passes intravascularly
(where the colloid osmotic pressure is higher, especially due to glucose which increases after
bleeding).
In intensive care the relationship between the plasma/ interstitial compartment is taken into
consideration, respectively 1:3 and therefore, 3-4 times more fluid should be administered
than lost blood.
The next step is to restore the LEC administering in the first 8 hours: of water and
electrolytes lost, and the other in the next 16 hours. Simultaneously content
maintenance is administered as well.
B. Conducted rehydration
It requires the cognition of the plasma and urinary ionogram (so the outputs) in order to
redress the electrolytes and the parameters of the microAstrup method in order tp correct
acid-base imbalances.
Plasma ionogram
(normal value)
Urinary ionogram Astrup parameters
Na = 140 mEq/L Na = 110-1180 mEq/L pH = 7,35 7,45
206
K = 5 mEq/L K = 35 55 mEq/L pCO
2
= 46 mmHg (in
arterial blood = 40 mmHg)
Ca = 7-10 mEq/L BS = 25-28 mEq/L
Mg = 7-8 mEq/L BE = 2,3
Cl = 110 mEq/L (pO
2
= 40 mmHg; arterial
= 100 mmHg oximetry is
obtained not by Astrup).
PO
4
= 25-30 mEq/L
SO
4
= 20-30 mEq/L
The general formula
mEq administration. = (Cd Ca) x 0,3 (0,6) x G
Cd = the desired figure (n)
Ca = current figure (of the apparatus)
0,3 =the coefficient of the extracellular space
0,6 = distribution factor for Na (differs for K, HCO
3
)
Acid-base disorder diagnosis
The
disorder
pH
(BE)
pCO
2
BS
(RA)
Renal compensation
Pulmonary
compensation
Metabolic
acidosis
+ + + Acidic urine |
NH
4
| HCO
3 reabsorption
rapid, ample v.
| pCO
2
Respiratory
acidosis
+ | |
Idem
Metabolic
alkalosis
| | | alkaline urine +
NH
A
+ HCO
3
reabsorption
superficial, rare v.
+ CO
2
Respiratory
alkalosis
| + +
Idem
Legend:
BE = excesul de baze; RA = alkaline reserve; v = vantilation, * = compensation.
207
RECURRENT ABDOMINAL PAIN (RAP)
Definitions
Apley and Naish in 1958 defined recurrent abdominal pain (RAP) as a syndrome
characterized by intermittent episodes of abdominal pain, with variable duration and
intensity, occurred over a period of at least 3 months, without any identifiable cause or which
interferes with the child's daily activities. Occasional, transient pains, which do not disrupt
the normal activity of a child are excluded from RAP. RAP has a duration of a few minutes
up to 1-3 hours (80%) and over 24 hours (10%). With time the criteria were modified, the
term recurrent was replaced with chronic or functional pain.
Chronic abdominal pain is one of the most common symptoms that occur in childhood and
adolescence, with a prevalence of 1-19% and represents 2-4% of cases of going to the
pediatrician. It is characterized by continuous, chronic abdominal pain, recurrent with quiet
periods which are short and rare, the pain not being well localized and changing the child's
daily activities. Chronic abdominal pain is functional and organic.
Today the terms of recurrent or chronic abdominal pain were abandoned and were replaced
with the term pain-related functional gastrointestinal disorders (FGID
s
).
In 1999 in Rome an expert group of pediatricians gastroenterologists have made an attempt to
establish criteria for the diagnosis of FGID
s
named as Roma II criteria. On this occasion the
classification of RAP in children in 4 groups of FGID
s
did not have support to sustain a
classification. However, there are 4 groups of FGID
s
: functional dyspepsia (FD), irritable
bowel syndrome (IBS), functional abdominal pain (FAP) and abdominal migraine.
Subsequent studies have expanded, so that in 2006 s- diagnostic criteria for FGID
s
were
revised and updated, and they are known as pediatric Rome III criteria. Thus due to the high
variability and phenotypic presentation of children with FGID
s
, the category of functional
abdominal pain from the previous classification was divided into two separate problems,
namely: childhood functional abdominal pain and childhood functional abdominal pain
syndrome (FAPS). In addition the duration of symptoms was changed from 2 to 3 months.
The new classification is shown in the following table.
Classification of functional abdominal pain according to the Rome III criteria
Functional dyspepsia (FD)
- Persistent or recurrent pain or discomfort centered in the upper abdomen (above the
umbilicus)
208
- Not relieved by defecation or associated with the onset of a change in stool frequency
or stool form (i.e., not irritable bowel syndrome)
- No evidence of an inammatory, anatomic, metabolic or neoplastic process
- that explains the subjects symptoms
- Criteria fulfilled at least once per week, at least two months prior to diagnosis
Irritable Bowel Syndrome (IBS)
- Abdominal discomfort (uncomfortable sensation not described as pain) or pain
associated with two or more of the following, at least 25% of the time:
a) Improvement with defecation
b) Onset associated with a change in frequency of stool
c) Onset associated with a change in form (appearance) of stool
- Criteria fulfilled at least once per week, at least two months prior to diagnosis
Symptoms, which through cumulation, support the diagnosis of irritable bowel are: 1.
abnormal stools (four or more times/ day and two or less/ week), 2. abnormal aspect of the
stool (coarse/ consistent or unformed/ watery diarrhea), 3. abnormal discharge (tension,
urgency, feeling of incomplete discharge), 4. mucus and 5. bloating or feeling of abdominal
distension.
Abdominal migraine
- Paroxysmal episodes of intense, acute periumbilical pain that lasts for 1 hour or more
- Intervening periods of usual health lasting weeks to months
- The pain interferes with normal activities
- The pain is associated with 2 of the following:
a) Anorexia
b) Nausea
c) Vomiting
d) Headache
e) Photophobia
f) Pallor
- All the above criteria must be included and performed more than twice in the last 12
months
Functional Abdominal Pain
- Episodic or continuous abdominal pain
- Insucient criteria for other FGIDs
209
- Must satisfy criteria for functional abdominal pain and have at least 25% of the time
one or more of the following:
1. some loss of daily functioning
2. additional somatic symptoms such as headache, limb pain, or diculty sleeping
Criteria fullled at least once per week for at least 2 months prior to diagnosis
* No evidence of an inammatory, anatomic, metabolic, or neoplastic process
that explains the subjects symptoms
Epidemiology
The incidence of recurrent abdominal pain (RAP) ranged from 0.3 to 19%, with an average of
8.4%. The disease is very rare, under the age of 3. It is more common in schoolchildren and
adolescents. There are two peaks of age that develop recurrent abdominal pain, that is: first
peak around the age of 5 and the second one at 8 10 years. In the prepubertal period there is
gender equality and in adolescence the ratio F/ M = 2/1.
Pathophysiological mechanisms
The exact etiology and pathogenesis of the pain is known.
Since 1987 it is known that pain is perceived and stored since the fetal period. CNS
immaturity at birth and incomplete myelination do not let pain to be perceived less because
the algo conductive paths are not affected. Children perceive pain as adults, but perception
increases depending on the stage of cognitive development.
Visceral pain perception performs a complex relationship between the peripheral and the
central nervous system. The enteric nervous system (ENS) is organized into two major
plexuses which provide the intrinsic innervation of the bowel: Auerbachs myenteric plexus,
located between the outer longitudinal layer and the inner circular muscle layer and
Meissner's submucosal plexus; there is a functional fusion between them forming a mini-
brain, intestinal brain ". ENS can work individually; he receives impulses from the CNS of
which is bound by related and efferent fibers. SNC continuously integrates information from
the gastrointestinal tract with information from other organs or from the environment; CNS
initiates appropriate responses, which explains the gastrointestinal response to stress or
emerging clinical manifestations (cyclical vomiting, diarrhea, etc.). ENS and brain use
multiple excitatory type neurotransmitters: acetylcholine, P substance, nitric oxide, ATP,
vasoactive intestinal peptide - VIP, cholecystokinin, etc. So at this age "the gastrointestinal
tract is the resonance box of the whole body."
210
There are some "ailments", negative emotions (psycho-emotional factors) that the child
perceives as RAP. The pathogenesis of functional painful disorders involves the relationship
between altered gastrointestinal motility and changes in visceral sensations visceral
hyperalgesia.
The symptoms for altered motility are: diarrhea, constipation, abdominal distension, and
those for hypersensitivity to pain and discomfort..
Factors that are incriminated in the pathogenesis of abdominal pain syndrome include:
- visceral hypersensitivity,
- altered central modulation of pain sensations
- genetic factors - children with irritable bowel syndrome (IBS) have parents with
functional gastrointestinal disorders
- Serotonin - the key mediator in modulating visceral sensitivity and motility.
- inflammation - role in the pathogenesis of IBS
- stress and psychological factors (depression, hypochondriasis, hysteria), or behavioral
disorders (school phobia, pain by imitation).
- Dysmotility
- aerophagia
Clinical symptoms: about 50% occur daily, 30% have a painful episode/ week, 20% have
one episode/ month.
Characteristics of pain:
Organic pain is precisely localized, constant and radiates; if the baby wakes up from sleep it
means the pain is organic; when the pains are generalized, the child especially perceives them
in flanks. It occurs in 8-27% of the cases. The presence of fever, accelerated ESR, weight loss
lead toward organic pain.
Functional pain (inorganic) is usually diffuse and localized around the navel (60%) and then
epigastric (26%) or in other places; it can associate headache, nausea, vomiting, and
constipation. Sometimes painful crisis can be connected with psycho-emotional events (tests,
theses, festivals, school fights, Monday morning colic); even sexual feelings in puberty can
be translated into RAP. The pain may have the form of a colic (50%), dull (30%) or cramps
(20%).
The diagnosis of functional abdominal pain
Because the exact etiology and pathogenesis of the abdominal pain is unknown, there are no
specific markers for the diagnosis of functional abdominal pain.
211
Because most of the time abdominal pain does not have an organic cause, it is important to
make a minimum investigation at the beginning that will be extended depending on the
serevrity of the case.
The diagnostic algorithm of functional abdominal pain is presented in the chart below:
Algorithm for evaluation of children with recurrent abdominal pain
Chronic abdominal pain
History and physical examination
The presence of some alarm signals
1. Involuntary weight loss
2. Growth retardation
3. Delayed puberty
4. Significant vomiting
5. Diarrhea
6. Gastrointestinal bleeding
7. Extraintestinal symptoms
8. Unexplained fever
9. Family history of IBD
10. Right iliac fossa pain
11. Abnormalities on physical
examination
Yes
Additional examinations
No
Criteria for constipation
Yes
Treatment of
constipation
No
Diagnosis related to pain of functional
gastrointestinal disorders
Diagnostic tests
1. Complete CBC
2. ESR
3. Metabolism examination
4. Investigations for celiac
5. Urinalysis
6. Parasitological examination
7. Tests for H. Pylori (atg.
from stool, respiratory and
urea test,)
8. Lactose test
Modified
tests
Yes
Additional investigations
No
Initiation of appropriate treatment
Subtype diagnostic - Rome III criteria
Isolated pain: Functional abdominal pain
With associated spt: Functional abdominal pain
syndrome
With alteration of the peristaltic: Irritable Bowel
Syndrome
Paroxysms.: abdominal migraine
In the diagnosis of FGID
s
the following are important:
History and physical examination of the patient: In most cases, the abdominal pain is
functional, being organic only 8-27% of the cases. History will be done thoroughly, focusing
on the characteristics of pain, detection of psychological and emotional factors; in children
with an "irritable bowel atopic, colopatic or neurotic family history is always detected. The
Irritable Bowel Syndrome has symptoms according to age: colic in infants, nonspecific
diarrhea in children between 1-5 years old, RAP Between the ages 5-13, diarrhea-
212
constipation alternating in adolescents and abdominal pain with diarrhea and/ or constipation
in adults.
Laboratory tests include:
- CBC
- Hepatic analyses: transaminases, bilirubin, GGT, LDH
- Renal analyses: creatinine, urea, uric acid
- Amylase
- ESR
- Urinalysis and urine culture
- Stool analyses, including the detection of occult blood in the stool and fecal exam
- Total protein, protein electrophoresis
- atc IgE and IgG for diagnosing food allergies
- atc. Anti endomisium, anti-reticulin (celiakie)
- Serological tests for the detection of Helicobacter pylori
- Abdominal ultrasound
- Digestive and inferior endoscopy
- Esophageal pH meter
- Barium transit
The differential diagnosis of chronic recurrent abdominal pain is made between the
following conditions, which represent the most common causes of recurrent abdominal pain:
- Functional abnormalities
- Functional abdominal pain
- Functional abdominal pain syndrome
- Irritable bowel syndrome
- Functional dyspepsia
- Abdominal migraine
- Aerophagia
- Gastrointestinal tract
- Gastro-oesophageal reflux disease
- Helicobacter pylori gastritis
- Peptic ulcer
- Esophagitis
- Lactose intolerance
213
- Celiac disease
- Parasitic infestation (Gyardia, Blastocystis hominis)
- inflammatory bowel disease
- Meckel diverticulum
- Intestinal malrotation with intermittent volvulus
- Chronic appendicitis
- Gall bladder, liver and pancreas
- Cholelithiasis
- Choledochal cyst
- Hepatitis
- Liver abscess
- Recurrent pancreatitis
- Genitourinary Tract
- Urinary tract infection
- Hydronephrosis
- Urolithiasis
- Dysmenorrhea
- Pelvic inflammatory disease
- Various Causes
- Gilberts syndrome
- Family Mediterranean Fever
- Malignancies
- Sickle cell
- Lead poisoning
- Vasculitis (especially Sconlein-Henoch)
- Angioedema
- Acute intermittent porphyria
Treatment
The treatment includes education, identification and modification of psychological factors
and stress, dietary therapy, drug therapy
1. Education is very important in the treatment of children with chronic functional abdominal
pain.The patient will be given the necessary empathy and will be explained to him and to his
family that the so-called functional abdominal pain is the most common cause of RAP. It
214
requires a normal lifestyle, with a regular school activity, the child's involvement in
extracurricular activities, normal sleep schedule.
Identification of stress factors and provision of appropriate psychological support
Cognitive behavioral therapy and hypnotherapy (especially in IBS) is very important.
2. Dietary treatment:
- fibers (cereals) especially in constipation decreasing the intestinal transit time
- avoiding lactose (lactose intolerance)
- elimination diet on the basis of the suspected food allergy. In food allergy Sodium
cromoglycate 60 mg/ kg/ day plays an essential role
- Probiotics have a role in preventing the growth of pathological bacterial flora and
maintaining the integrity of the mucosal barrier. Biotics, Enterol 2 x 1 caps/ day
Ecoflorina 2 x 1 vial/ day
3. Medication useful for modulating gastrointestinal motor function, neurohormonal response
to stress, cytokines involved in the inflammatory process.These include:
- H
2
blockage Famotidine in patients with functional affections
- Serotonergic agents: Pizotifen, Citalopram, alosetron, Tegaserod.
Only the first two have been used in limited batches in children and decreased the
frequency of painful episodes/ day. Controlled studies are still needed in order to
include them into treatment.
- Tricyclic antidepressants used in the past, today only in adults (Amitriptyline,
Nortriptyline, Clomipramine, Imipramine)
- Tranquilizers and antispasmodic: Oxifenonium (parasympatholytics synthesis) 3 x
-1 tablet./ day for school children, combats smooth muscle spasm of the
gastrointestinal tract, urogenital and biliary tract; Propantheline (anticholinergic,
antispasmodic, antisecretory); benzodiazepines (minor tranquillizers such as
diazepam, oxazepam, alprazepam the last one is a disinhibitor, administered in case of
anxiety
- Antihistamines: Hydroxyzine for 1 week - good results in the regulation of sleep;
- Neuroleptics: Thioridazine and Levomepromazine - weak action (sedatives),
Chlorpromazine (Largactil) average action and Haloperidol with strong action
(antipsychotic).
- Complementary therapy: peppermint oil (relaxes smooth muscles of the
gastrointestinal tract), ginger useful for patients with nausea, dyspepsia, diarrhea.
215
- For organic cases - specific treatment of the underlying disease: giardiasis, ITU, renal
calculus, gastritis, peptic ulcer, colitis, Meckels diverticulum, hernias of the
abdominal wall, perforation of the hymen.
- In the irritable bowel syndrome fats are reduced in the diet, cold liquids are
prohibited, the is enriched with dietary fibers, in association with medication:
Loperamide: 4 x 1 mg ( tb/ day) between 4-9 years, 3 days; 4 x 2 mg (1 tb/day) over
9 years, for 5 days, in "spastic colon" in order to stimulate motility - Cisapride
(Prepulsid), dopamine antagonists in children over 12 years of 3 x 10 mg (3 x 1 tb/
day) 6 weeks (4 weeks in non-ulcer dyspepsia).
PARASITES
Parasitic infections of the gastrointestinal tract occur in all geographic regions of the world
and cause substantial morbidity in children.
Below only the most important and most common parasites in children are presented.
PROTOZOA
Giardiasis (Giardiasis, Lambliasis)
Giardiasis is an infection caused by the parasite Giardia lamblia which is found in the normal
duodenum and jejunum.
Fecal-oral transmission makes this parasite to be frequent in units where there are children;
but it is also common among healthcare workers (25% of the cases)
Symptoms are extremely varied, and can also be manifested by diarrhea with an insidious
onset, steatorrhea, irritability with weight loss, recurrent abdominal pain. In 25-30% of cases
it is asymptomatic.
Positive diagnosis is made by:
- Highlighting cysts in stool. In one infected case the cystic form is found in the stool in
a percentage of 30%, so the examination of the stool will be repeated at least 3 times,
which increases the chance of detection to 50%. In heavy infections mobile
trophozoites can be observed in the freshly emitted stool. Poor highlighting of the
cysts is due to their irregular excretion.
- Highlighting the vegetative form from the duodenal juice. Highlighting of
trophozoites helps to put the accurate diagnosis, however, infants and young children
hardly bear the duodenal survey. The entero-test is more acceptable.
216
- Serological tests are sometimes used as well: indirect immunofluorescence and
immunoassay analysis - IgM.
The differential diagnosis is done with other causes of chronic abdominal pain and
celiachiform syndrome.
Treatment
1. Atebrina (Mepacrin) 1 tablet. = 0.100 g;. 6 mg/kg/day (max. = 0,3 g), divided into 2
to 3 daily doses for 6 days (cause yellow coloration of the whites).
2. Metronidazole 1 tablet = 0.250 g, 20 mg/ kg/ day (max = 1 g), divided in 2-3 daily
doses for 7-8 days.
3. Tinidazol (Tinidazole, Tinigyn) 1 tablet = 0,500 g, 50 mg/kg/day (max. = 2 g) in a
single dose, 80% of cases resolved. Some people prefer it as a consolidation
treatment after using Atebrina or Metronidazole over a period of 2-3 days and
divided into 2-3 doses.
4. In infants and young children a combination of erythromycin + furazolidone is used.
- Erythromycin 20 mg/ kg/ day administered 30 minutes before meals,
- Furazolidon 5 mg/ kg/ day after meals. This combination is given for 5 days (10
days).
This treatment is well tolerated but it is only effective in a percentage of 40% therefore,
usually, the treatment needs to be repeated after 6 weeks.
Another scheme uses only Furazolidone 8 mg/kg/day in 3 divided doses for 10 days. (The
results are good provided that food is properly chewed).
5. Ornidazol (Tiber). Dose: children under 1 year 2 x tablet./ day, 1 - 6 years 2 x
tablet./ day, 7-12 years 2 x tablet./ day, in the morning and in the evening after
meals, for 5-10 days.
6. Albendazole 400 mg/ day in a single dose from 5 to 7 days.
Because giardiasis is associated with oidium albicans, Stamicina or yogurt will be associated
to the basic treatment.
Infection control will be done after 6 weeks, period considered necessary to eliminate drugs
and remultiplication of the parasite, not a mandatory control.
A single treatment is recommended to be done.
217
NEMATODES
Strongiloidosis
Strongiloidosis is caused by the parasite Strongiloides which has two forms: a parasitic one
and one with a free life.
The route of entry is dermal, from here through the blood vessels reaches the pulmonary
capillaries where produces alveolar hemorrhage and bronchopneumonia and affects the
gastrointestinal system as well causing villous atrophy. From here through the lymphatic
system may disseminate anywhere in the body.
Clinical symptoms
Many patients may be asymptomatic.
Patients become rapidly symptomatic after penetration of the skin presenting: local skin
reaction, respiratory symptoms: cough, wheezing, pulmonary infiltrates, watery diarrhea,
abdominal cramps, urticarial rash, occasional bowel obstruction, sepsis, meningitis, etc.
Diagnosis
- Hypereosinophilia > 500 cells/l
- Detection of larva migrans in the stool, sputum, jejunal biopsy
- Positive serology (> 80% of cases)
Treatment
- Ivermectin 150-200 mg/ kg single dose, repeated after 1 week. Or
- Ivermectin 200 g/kg/day for 3 days.
TRICHINELLA SPIRALIS
Trichinella spiralis occurs in communities where infected pork is consumed.
After ingestion of infected meat, the cysts release their larvae in the stomach which reach
maturity in 5 10 days in the small intestine. Mature females create new larvae which
penetrate through the intestinal wall and migrate at the level of the striated muscles and rarely
at the level of the brain and heart.
Clinical symptoms
They appear only in heavily infested people and consist of: abdominal colic, watery and
bloody diarrhea, vomiting, dehydration. In the stage of larval invasion facial or periorbital
edema, myalgia, lymphadenopathy satellite, swelling of the salivary glands, fever can occur.
Heart rhythm disorders, neurological symptoms meningoencephalitis can occur as well.
The diagnosis is based on the symptoms, elevated LDH and CPK, muscle biopsy (at 3-4
weeks after infection), serological reactions
218
Treatment
Mebendazole 200 mg x 2/ day or Thiabendazole 2 x/ day for 10 days.
ASCARIASIS
Ascaris lumbricoides infestation occurs through ingestion transmitted by dirty fingers, dirty
eggs, water or food contaminated. After ingestion the eggs reach the duodenum where they
transform into rhabdoid larva, then they get into the port system and liver, then the lungs (by
venous or lymphatic way).
The clinical picture
Most patients are asymptomatic. The disease becomes manifest in massive infestation.
Children may present somatic and neuropsychiatric retard, pulmonary symptoms -
pneumonia (by the migrating parasite), digestive symptoms: abdominal pain, nausea,
vomiting, flatulence, diarrhea, intestinal obstruction, hepatobiliary and pancreatic symptoms.
Diagnosis
- Elimination of the parasite
- Ultrasound or endoscopy with retrograde cholangiopancreatography.
Treatment
- Albendazole in a single dose of 200 mg/day in children of 2 to 5 years old and
400 mg/day in children> 5 years old or
- Decaris (Levamizol) 5 mg/ kg in a single dose.
ENTEROBIASIS (OXYURIS)
Enterobius vermicularis infests the human being by ingestion of the embryonated eggs. Eggs
are disintegrated in the stomach and migrate to the cecum. They have sizes less than 1 cm and
they are white. During the night the females migrate to the perianal region where they lay
their eggs.
The clinical picture
The disease may develop asymptomatically, but children may present nocturnal anal pruritus,
agitation, insomnia, weight loss, scratches.
Diagnosis:
- Highlighting the adult worms in the stool or detecting their eggs
Treatment
- Albendazole 200 mg/ day in children under 5 years old and 400 mg/ day for children
over 5 years old as a single dose
219
- Mebendazole 2 x 100 mg/ day for 3 days
- Pyrantel pamoate or piperazine
VISCERAL LARVA MIGRANS (TOXOCARIASIS)
Toxocara infestation occurs in young children, 1-4 years old, if living in close contact with
dogs and cats. Soil contamination with feces of dogs and cats contributes to the spread of the
infestation. Infection in humans occurs by ingestion of parasite eggs. After ingestion the eggs
give rise to larvae which penetrate the wall of the digestive tract and migrate to the liver,
lung, brain, kidneys, heart, eyes.
Clinical symptoms: fever, cough, wheezing, severe respiratory failure, seizures, abdominal
pain, hepatomegaly, skin rash, lymphadenopathy. The ocular form may occur as well
characterized by decreased visual acuity, strabismus, etc.
Diagnosis: Increased eosinophilia confirmed by serological reactions ELISA tests, specific
atc.
Treatment
- Thiabendazole 25 - 50 mg/ kg/ day for 5-days or
- Albendazole 2 x 400 mg/ day for 5-days
- In the location of the eye: Prednisone 2 mg/ kg/ day until symptoms improve.
CESTODES
ECHINOCOCCOSIS (HYDATID DISEASE)
The disease caused by Echinococcus granulosus is endemic in regions characterized by
intensive rearing of sheep, goats and cattle.
The adult worm is localized in the small intestine of some organisms which are the definitive
hosts of the parasite (dog, cat, wolf), and in the larva state (hydatid cyst) is found in the
viscera of some ruminants (sheep, cattle, goats) or of mammals (pig) that are intermediate
hosts. By ingesting parasite viscera by the definitive hostsof the parasite in their small
intestine scolexs are released which are anchored to the intestinal or duodenal mucosa and
adult worms are developed, which after maturing produce eggs that are eliminated through
faeces.
The clinical picture: the disease may develop long asymptomatically for a long time due to
the slow growth of the cyst (for years). It is manifested clinically by large hydatid or broken
cysts when the patient may present irregular hepatomegaly, portal hypertension (rarely),
220
allergic manifestations, chest pain, dyspnoea, cough or signs of intracranial haemorrhage and
focal neurological signs in cerebral localization
Diagnosis
Eo , TST Cassoni positive, monoclonal atc
Treatment
- Surgical removal of the cyst
- Postoperative treatment with albendazole aimed to destroy possible small hydatid
cysts, undetectable clinically or through laboratory investigations
- If the cyst cannot be treated surgically 10-15 mg/ kg/ day of Albendazole is
administered divided in three doses during 3 months
- In disseminated forms and in peritoneal echinococcosis, Albendazole is recommended
in 4-6 cures each one for 4 weeks with intervals of 2 weeks between them.
221
CHAPTER VI - NUTRITION AND DEFICIENCY DISEASES
Conf. Univ. Dr. Mrginean Oana, Asist. Univ. Dr. Pitea Ana Maria, Asist.
Univ. Dr. Chincean Mihaela, Asist. Univ. Dr. Grama Alina
MALNUTRITION DISTROPHY PROTEIN-ENERGETIC MALNUTRITION MPE
Definition: Chronic nutritional disorder
The body incapacity to cover quantitative and/or qualitative the needs (caloric, nitrous) by
lack of intake or the impossibility of the digestive tube to accept, process or absorb the food
properly.
Etiopathogeny
I Determinant causes
a) ex alimentatione
dietary mistakes - hypocaloric diets desequilibrum
b) ex infectione- all infections digestive tolerance
more dangerous
o infections of the digestive tube
o repeated infections different causes
c) e morbo- chronic diseases
malformations
enzymopathies
malabsorption
parasitosis
II. Favoring causes
a) ex constitutione:
constitutional diathesis
hydrolability
b) ex curatione - care conditions
Etiology - multifactorial (a single cause can be rarely incriminated)
Etiological factors determines process of (starvation). The center of pathogeny is caloric and
proteic insufficiency.
Insufficient caloric intake: org. cons. glucides (reserve ~1% from weight), then lipids (in
absence of glucides they burn with formation of cetonik corps, so uneconomical)
222
Prolongued fast determines protein burn (autophagy).
Insufficient protein intake
The absence unique source of nitrogen results in burntof proteins themselves.
The aim is energetic, in the plastic detrimental, with negative nitrogen balance.
To burn 1 g lipids , 2 g glucides are needed.
Caloric and proteic insufficiencies once with the gluconeogenesis initiation
Many synthesis are stopped:
decrease of digestive enzymes determines decrease digestive tolerance
antibodies synthesis leads to low antimicrobian defense, so without any
defense, the body is exposed to many affections which, in these conditions,
evolve more prolonged and more severe
Positive diagnosis
Positive diagnosis is based on clinical symptoms and support of anthropometric
measurements.
I. Anthropometric measurements
Anthropometric indicators based on body (physical) measurements are height or size
(nutritional index), weight, thorax perimeter, cranial perimeter (useful in the first 2 years of
life), abdominal circumference, buttock circumference, mean arm circumference, skin fold,
abdominal fold, tricipital fold and others (related to age and sex of the individual), with the
advantage of being inexpensive and non-invasive.
Three of the most commonly used indicators for infants and children are weight for
height (WFH weight for height), height for age (height for age HFA) and weight for age
(weight for age WFA) which can be obtained by comparing the indicators core, weight,
height and age, separately by gender, with reference data for children "healthy". The
following can be used:
Weighted index (WI) (= actual weight / ideal weight), normally between 0.9-1.2. If at
WI over 1.2 we have obesity, below 0.9 we have dystrophy (first degree dystrophy:
0.90 to 0.75 in II degree dystrophy: 0.75 to 0.60, and III degree: below 0.60).
Weight deficit (IP)
(DP) =
Ideal W Real W x 100
Ideal W
I degree = < 25%
II degree = 25 40%
III degree = > 40%
223
Body Mass Index (IMC, sau BMI - Body Mass Index) W/H
2
(normal 18,00 - 25,00
kg/m
2
).
By comparing the results of measurements of similar individuals (in terms of age and
sex), anthropometric indices are converted to reference data. There are three ways to express
these comparisons:
a. z-score (standard deviation score): the difference between the value for an individual
and the mean of the reference population of the same age or height, divided by the
standard deviation of the reference population.
b. The percentage of median: ratio of the measured or observed value in an individual
and the mean reference data for the population of the same sex, and age or height.
c. percentile: an individual's position on a given reference distribution, determined by
what percentage of the reference group, the person overlaps with or exceedes.
Other indicators: waist (nutritional index) head circumference (in the first 2 years)
abdominal fold, tricipital fold, etc.
There are several ways to define malnutrition in children. In the past Gomez
classification wa used, which employed only weight for height, a classification used today
only for didactic reasons and which classified malnutritition into: Ist degree - mild
malnutrition (WFA 70-90%), medium II degree (WFA 60-74%), severe -. III degree (WFA
<60%)
II. Clinical symptoms
Clinical - infant, small child - 3 degrees (didactic)
Malnutrition, I degree
normal aspect
decreased adipose tissue on the belly and thorax
the weight curve increases slower
digestive tolerance relatively good
good resistence to infections
Malnutrition II degree
the child is pale, anemic
cellular tissue is dissapeared on the belly and thorax and diminished on the face and
limbs
stationary weight curve decrease slow or gradually
low digestive tolerance (often diarrhea)
224
decreased rezistence to infections (pyoderma, otitis)
symptoms specific to the metabolism of starvation: hyipotermia and bradycardia
Malnutrition III
rd
degree
grey color (dirty)
cellular tissue is dissapeared (Bichat bubble too)
face has aged aspect (simian, volterian)
the skin seems too large - tobacco sack (buttocks)
persistent turgor, weight curve - collapsed
digestive tolerance very decreased, the child does not tolerate the ration of
maintenance
hypoglicemia, hyperinsulinism (starvation)
very low rezistence to infections: frequent infections (pneumonia, septicemy, TBC),
biological reactions which are not interpretable, impossible vaccinations
neuromental retard
Malnutrition III
rd
degree particular clinical forms:
kwashiorkor
marasm
marasmic kwashiorkor
a). Kwashiorkor (red child)
protein nutrition
can get the normal ration of calories
proteins absent, often replaced by flour
the edematous form appears in big child, extremely rare in us
associates anemia, distended abdomen, undigested food/feces
areas of skin depigmentated and hyperpigmentated
thin, frail hair
apathy, irritability frequent emotional disorders
b). Marasm
insufficient nutritional intake (not only proteic)
proteic-energetical malnutrition (proteic-caloric)
can appear in infant too
clinical severe cachexia with emaciere
melting muscle and subcutaneous tissue
hypotonia
225
crying/characteristic groaning
frequent form in our patients
high share in the infantsmortality
c). Kwashiorkor marasmic
characteristic to marasm
plus edemas
Antropometric measurements - MPE 3 degrees
Weight index (I.P.) = G. real /G ideal
Ist degree.: 0,89 0,76 W = weight in kg
II degree: 0,75 0,61
III degree: under 0,60
Weight deficiency
(DP) = ( ideal W real W x 100)/ ideal W
MPE degrees after anthropometry:
I = < 25%
II = 25 40%
III = > 40%
Other index :
waist (nutritional index)
cranial perimeter (in the first 2 years)
abdominal crease, tricipital, and so on
Degree of weakness and height retard is made after Waterloo classification:
Waterloo classification
evaluates the state of nutrition
distinguish weakness as acute sign of MPE compared to stop of the growth as sign of
chronic malnutrition and reflected through a Height for age decrease
W for waist > 80% W for waist < 80%
Waist for age > 90% Normal wasting
Waist for age < 90% Height retard wasting with height retard
WHO classification uses:
226
- z score for WFH (Wasting), defining acute malnutrition which can be moderate (z score -3
z <-2) or severe (z score <-3) or
- z-score for HFA - defining chronic malnutrition - can be moderate (z score -3 z <-2) or
severe (z score <-3)
To assess nutritional status MUAC, TSF can be used with high accuracy, which, associated
with proteinemia (albumin) well define the nutritional profile of the child.
Evolution of weight curve (the degrees of MPE which are known are valid)
stage I: passes unnoticed, the child has normal aspect
stage II: diminished turgor, signs of starvation appear (hypotermia, bradycardia)
stage III: subnutrition involves the immune system, so MPE is accompanied by
infection (diarrhea, pneumonia, TBC...)
Laboratory biological balance
Hgb, Htc, erithrocytes number, constant E
dehydrations degree
anemia (Fe/folic acid, B12, hemolysis)
Glucose - hypoglycemia
Electrolytes (Na, K, Mg, pH, Cl, CO3HNa)
hyponatremia and dehydrations type
hypokalemia, alkalosis, acidosis
T protein, transferrin grade of proteic deficiency
Creatinine renal function
Number of. L, PCR, serology - bacterial/ viral infections
Coprologic examination- presence of parasites
Hypoalbuminemia
present in all 3 forms of MPE
not only in edematous forms
Socio-economic conditions common in all forms
poverty
ignorance
taboo foods
Malnourished mothers who do not have breast milk
Unsanitary housing
227
Prophilactic treatment
Avoid the factors which lead to malnutrition
Encourage breastfeeding
Avoid dietary imbalances
evicia infeciilor (clire, including vaccinations)
Measurements to improve the social conditions, environment
The treatment objectives are:
Improve energy, protein and micronutrient intake
Promote weight gain for catch-up growth
Correct any nutritional deficiencies
Encourage adequate oral intake to meet nutritional requirements
Support parents through dietary changes
Commence enteral support if oral intake is insufficient
Monitor, monitor.
Curative treatment
team (doctor, dietetician, social nurse)
aim: avoid rehospitalism
rule: correct rehydration, progressive feeding restart
nutritional rehabilitee ~ a month
mpe production needs months
complete recovery the same
undernourishment acts at least 4 months before to influence length growth
Rehydration
i.v. good experience with the Starter solution
i.v./oral max. 60 ml/kg the first 2-3 days (the volume of myocard is )
: 80 - 100 ml zilele 5-7
progresively to cover the total hydric necessitiesle (120 - 150 ml/kg/day)
Caloric intake
ensure 60 80 kcal/kg/day the first 3 days
then 100 kcal/kg/day in the next 4 days
In the first week do not administrate solid foods
The 2
nd
week progresively at 150 200 kcal/day
228
Breast milk- important for the intake of IgA
After the first week, the protein intake of 9% is ensured
then 12% (from the whole energetical intake) as long as it exists in the formulas for
infants
Proteins
will gradually in nutrition
4 g/kg/day daily supervising of the renal function
(35 40 kcal for each gram of protein)
Carbohydrates
glucose (10 15 g/kg/zi)
fructose (7-8 g/kg/zi)
Polimers of glucose (dextrin - maltose)
total/partial formulas without lactose (monosaccharides and polimers of glucose)
Tolerance to lactose improves slowly (weekly), restored - after 3-4 months
Lipids
administrate 0,5 g/kg/day
Up to 4-5 g/kg/day
exploratory with vegetal oil, dietetic pp. degresate, parial degresate
carnitina from preparations favors the transfer TG with long chain through
mitochondrial membrane
Minerals, oligoelements (zinc, iron, iodine) - additional 6 weeks. Are essential in restoring
the growth rate
Vitamins-administered at least 3 months. Vitamin A and Vitamin D are important in the
recovery phase.
Syndrom of renutrition
Severe hypophosphatemia - the first week of realimentare
Body reserve of P, Mg, K are decreased (intracel.)
With food intake, glucides determines insulinic response which forces the
intracellular absorbtion of P, Mg, K resulting in decrese of plasmatic (daily
measurement in the first week)
low P plasmatic s 0,5 mmlo/L may determine:
shivering - rhabdomyolysis
cardio-vascular insufficiency - arrhythmia
229
convulsions - consiences alteration
death
Criteria of care and treatment efficiency
normal intestinal transit
reluarea weight gain after 2-3 weeks
Nutritional rehabilitee after a month
Immune recovery at 25 30 days
clinical recovery at 6 8 weeks
Evolution is favorable, with exception : rare cases of enzymopathy or malformations
Prognosis
Reserved in MPE III
rd
degree
in the period of infant and if prolonged
they are 2-3 cm smaller in waist than their others at the same age
do not have psycho-intelectual performances
less resistant to diseases
IRON DEFICIENCY ANEMIA
Etiology: iron deficiency develops especially in childhood periods of rapid growth, such as
infancy and puberty.
Obstetrical and neonatal causes:
- maternal iron deficiency
- gemelarity, prematurity
- intrauterine hypotrophy
- fetal-maternal transfusion
- neonatal bleeding
Dietary causes:
- extended exclusively lactate feeding
- insufficient intake of dietary iron
Disorders of intestinal iron absorption:
- chronic enteropathy: celiac disease, cow's milk protein intolerance
Gastrointestinal blood loss:
- intestinal parasites
- chronic occult bleeding secondary to aspirin treatment
- peptic esophagitis
230
- gastritis, gastric ulcer
- meckel diverticulum
- intestinal polyposis
Extra-digestive blood loss:
- menometrorrhagia
- pulmonary hemosiderosis
- recurrent bleeding in children with hemostasis disorders
- repeated blood harvesting in small infants
Effects of iron deficiency manifest throughout the body:
On tissues:
- anorexia
- atrophic glossitis
- gastric hypoacidity
- exudative enteropathy
- malabsorption syndrome
- decreased activity of intestinal enzymes
On CNS:
- irritability, abnormal behavior
- fatigue
- delayed psychomotor development
- decreased attention, reduced cognitive performance
- poor school performance
- headache
On the cardiovascular system:
- tachicardia
- cardiomegaly
On the musculoskeletal system
- decreased muscle activity
- decreased exercise performance
Clinical manifestations: occurs most often in the age of 6-24 months; usually the child is fed
exclusively on milk.
Symptoms: moderate anemia is frequently asymptomatic; irritability, anorexia, fatigue appear
as iron deficiency increases.
231
Signs: on clinical examination, the child with iron deficiency anemia is fat and pale, often
presents tachycardia and systolic murmur. In severe forms (Hg <3 g / dl) or complications
requiring intensive cardiovascular activity, congestive heart failure occurs.
Diagnosis
Laboratory tests:
- CBC
- morphological examination of erythrocytes (May-Grunwald-Giemsa smear)
- erythrocyte indices: MCV, MCH, MCHC
- iron levels (serum iron) low
- ferritin
- total iron binding capacity (TIBC) increased
- coefficient of saturation of transferrin - low
Other tests (rarely necessary):
- protein diagram
- highlighting stool blood (Gregersen reaction)
- myelogram
Differential diagnosis: with other microcytic, hypochromic, anemias.
Hemoglobinopathies: beta-thalassemia minor: hypochromic microcytic anemia with
reticulocytosis hypersideremia, erythrocytes with basophilic stippling, shaped
erythrocytes; diagnosis is indicated by hemoglobin electrophoresis.
Lead poisoning: erythrocytes with basophilic stippling
Infectious and chronic inflammation anemia: red cells are normochromic and normo-
or microcytic; serum iron is low, TIBC is low; normal or high ferritin being an acute
phase protein.
Sideroblastic anemia (sideroacrestic) idiopathic or secondary: presence of iron excess
in macrophages and increased sideroblasts.
Congenital atransferrinemia: severe microcytic hypochromic anemia, with neonatal
onset and almost complete absence of plasma iron
Treatment
Prophylactic treatment
Prophylactic treatment begins with proper nutrition during the mother's pregnancy (elemental
Fe content of 10-15 mg/ day) and supplementary iron therapy in the last 3 months of
pregnancy.
232
The premature child is considered to have iron deficiency since it is born with low iron
stores. Prophylactic treatment of iron deficiency anemia in premature children starts at the
age of 4 weeks with 1-2 mg elemental Fe / kg / day 2-3 months.
Food diversification is important in preventing iron deficiency anemia. Iron-fortified cereals
and milk prevent iron deficiency anemia in high-risk infants and young children.
Curative treatment
1. Oral administration of iron: dose of 6 mg / kg / day elemental iron (up to 10 mg), divided
into 2-3 doses, 30 minutes before meals or between meals, with citrus juice, or vitamin C,
which promotes the absorption. We prefer simple iron soluble salts (sulphate, ferrous
fumarate). Iron is administered to normalize blood count, then the same dose is continued
for a further 2 -3 months to replenish iron reserves.
It is important to consume iron-rich foods (meat, liver, eggs, fruits, vegetables) and
reduce the amount of milk to 500 ml / day.
2. Parenteral administration of iron is rarely indicated and is reserved for special situations.
Indications:
a. Low digestive tolerance (diarrhea, vomiting)
b. Low iron absorption
c. Chronic losses
The formula for total administered iron mg:
mg parenteral iron = (ideal Hb - actual Hb) x 80 x 3.4 x 1.5 / 100
- 80 = blood volume in ml / kg
- 3.4 = mg iron necessary to increase Hb by 1 g
- 1.5 = correction factor to ensure completion of iron deposits
There are dextran iron or polymaltose iron ampoules (ampoules of 100 mg elemental iron).
Parenteral iron (i.v. / i.m.) is administered every 2-3 days, in 2-4 doses. In infants not more
than 50 mg / dose and in young children not more than 100 mg / dose should be used.
3. Red cell transfusion: is indicated only in severe iron deficiency anemia (Hb <4-5 g / dl)
with cardiovascular decompensation and / or severe infections. Izogroup izoRh red blood
cells mass is used, at a dose of 3-5 ml / kg / day.
Evolution and prognosis: are favorable, provided generating causes are removed. Mild
forms have a tendency of self-correction on proper diet. Lack of response to iron therapy
raises questions about the accuracy of diagnosis, compliance with therapeutic indications or
the existence of associated diseases (malabsorption, intestinal parasites).
233
DEFFICIENT RACHITISM RICKETS
(common, vitamin-D sensitive)
Definition
Osteodistrophy deficiency
Lack of bone mineralization => Lack of vitamin D
Affects growing bones => bones deformation
osteomalacia affects the bones which do not grow
Etiopatogeny
Lack of vit. D
dietary
lack of exposure to UV rays- sun
Plasmatic stockage of vit. D
reflects the reserves
decreases in deficiency
Calcitriol - main role in intestinal absorption of Ca
Vit. D: >40 metabolits - actions incompletely known
Receptors for calcitriol
lung
endocrine organs
hematoformatoare organs
other tissues
Daily need
Infant:
400 800 u.i./day.
infants nutrition is poor in vit. D
exposure to sun is not enough
Lack of vitamin D
abs. Ca => hipocalcemia
h-Ca stimulates secretion of PTH => Hyperreactional paratiroidism
consequences:
renal reabsorption of phosphorus => hyperphosphaturia and hypophosphatemia
intestinal abs. of Ca and renal elimination
fixes calcium in bones
234
Through these pathogenic links
hypocalcemia can be corrected
tribut is paid by the bone through reabsorption or bone modifications
Decisive factors
The deficiency of vit. D from food
normal nutrition ensures 15%
Insufficient exposure to sun
ensures 85% of the necessity of vit. D
Vit. D main role in homeostasis Ca and P
| intestinal absorption of Ca and P
| renal absorption of P
the increase of Ca, P deposits at the level of the bones ( hydroxiapatity formation)
Vit. D interferes in other processes:
Participate to synthesis ATP muscular, basic element of contr. musculare (rachitic
= hipoton)
favors the absence of Iron and Co at the level of intestines (anemia of rachit)
When vitamin D is lacking=> slow metabolic process, favoring the metabolites
accumulation acidosis pres. osmotic intracel. attract the water (pasty
aspect of rachitic children)
Favoring factors
Small age (3 months - 2 years)
Fast growth (premature,twins, vigorous children)
Nutritional Factors - inadequate diets
Artificial nutrition (cow milk is poor in vit. D)
Consume dairy products which are not enriched with vit. D
Vegetarian diet
Food rich in flour (fitai), oxalate, P
Total parenteral nutrition
Life conditions
temperate climate - october-april, r.U.V.
poluted environment - towns the powders filtrate r.U.V.
exposure to sun
Skin Pigmentation
235
limits the skin syntheses
Affections which prevent hydroxilation
hepatic
renal
Affections which prevent intestinal absorption
cystic fibrosis
celiachia
biliary atrezy
Medicines
cortisone
anticonvulsivants
iron pp
heparin
chelatoare
Maternal factor
Many pregnant women (season, life style) weak exposure to sun lack of
vitamin D
Their new born small reserve of vitamin D (or )
A lot of new born have decreased conc of vit. D (Calcidiol) in winter or at the
beginning of spring
N.B.! Associate the favoring factors!!
Diagnosis
clinical signs
biological aspects
radiological elements
Clinical description
Onset
Not characteristic
It can pass unnoticed
irascibility
anxiety
capricious apetite
agitation
sweat (nape)
236
reduced sleep
Period of state
bone modifications
term. II - head
term. III - thorax
term. IV limbs
cranian
Craniotabes (precoceous 3-6 months)
parietal softening
occipital softening
clogging
sensation ping-pong ball
Teeth
tardive eruption
enamel hypoplazia
carii dentare
in tardive forms affect definitive teeth
Forehead and head
high forehead (olimpian)
cap natiform
brahicefalie (occipit turtit)
plagicephaly (turtit postero-lateral)
suturile do not close on time
fontanel remains open for a long time
Thorax
deformations
torace in funnel
in careen
"chondrocostal rosary (osteoid) - at the level of the axial ant.lines
Harisson ditches
submammary ditches
at diaphragm insertion
thorax base splay
the spine
237
Different degrees of scoliozis
lordoze
cifosis (reductible)
Basin
tight future distocice births (in )
Limbs
hands
rachitic bracelets
epiphysis tumefied
visible thickening
or palpable thickening of distal extremities of radiusului
development of demineralized bone tissue
Lower limbs
Changes which appear after the child walks
o coxa vara
o coxa valga
o genu varum (O - paranthesis)
o genu valgum (X - mai rarely)
Other modifications in rachitism
rachitic Nanism today it is very rare
laxe ligaments large movements
hypotone Muscles motor retard
big abdomen - batracian
hepato-splenomegaly
anemia - paleness
Other extra bone modifications
infant- as manifestations of tetanie
convulsions
laringospasm
Sweats a lot
hipotony
la respiratory muscles ventilation disorders and bronchopulmonary infections
(rachitic pulmonul )
proeminent abdomen
238
late motor development
big child and adolescent
Similar to adults osteomalacia
artralgia
astenia
Tiredness at walking
Hypocrom anemia (rachitic anemia )
90% of rachitic children are anemic too
Clinical forms
Rickets of premature
precoceous
severe
favors the severe pulmonary complications
Common rickets
- florid severe form
- medium common form
- frust
Tardive rickets - 6-7 years, puberty
Common florid rickets
severe form
tetanic convulsions
craniotabes present
or crisis of tetany
Common medium rickets - common form
Common rough rickets- minor symptoms
late walking
open fontanels
late teeth appearance
soft and sweats a lot (neck)
rtg.of the hand - salutar
Tardive rickets
Favored by skin pigmentation
Insufficient sun exposure
Foods deficient in Calcium (milk, yoghurt,cow cheese) for a long time.
239
practically extremely rare, a calcium deficiency
In adolescents who say that they have bone pains, especially the lower limbs (and do
not suffer of renal or intestinal affections) lets think about R.C.!
Laboratory
Hipocalcemia - 50% of the cases
Without correlation with the intensity of bone manifestations
< 6 months show infraclinic rachitism (with discrete radiological manifestations)
intercurences (gastroenteritis) aggravates the Ca deficiency
calcemia can be normal (Ca = 2,42-2,60 mmol/L)
calciuria practically nule
Hypophosphatemia
P normal = 1,56-2,10 mmol/L
Maybe the most important analyze
Precocious sign (before clinical signs)
phosphaturia a little bit increased
Serical alc phosphatases
Always increased > 40-100 U.I
Osteoblastic activity in the context of calcium deficiency
normal > 10-20 UB or 50-350 UI/l
Period of recovery: normal phosphatemia, Ca appears in urine
PTH
normal 4-8 mg/ml
secondary
o hyperparatiroidia
o hyperphosphaturia
o hyperaminoaciduria
lack of calcium in urine (r. Sulcowitch negative)
Plasmatic:
H-Mg.ziemia
citremia
25-HO-vit. D: 10-30 ng/ml
= stocks or metabolism anomalies
1,25-(HO)2-vit. D: 40 pg/ml
Urinary
240
hyperaminoaciduria (H-paratiroidism reactional prevents the renal reabsorbtion of aa)
Sulkovich reaction
evidence the urinary calcium
after high doses of vitamin D, calciuria
reaction +
interrupt the vitamin treatment
Biochemical - 3 evolutive stages
Stage I
hypocalcemia
normophosphatemia
fosf. alcaline slightly increased
Stage II
normocalcemia
hypofosfatemia
increased fosf. alcaline
Stage III
hypocalcemia
hypophosphatemia
ALP a lot increased
Radiology useful Rtg. knee, hand
Modifications at 2-3 weeks since the onset
Hand rtg.:
Enlarge of the diaphyzo-epiphyseal space
Enlarge of metaphysis with metaphyso-epiphyseal line deleted, laced
cortical extended to epiphysis through 2 rachitic spur
diaphysis extremity with cup aspect
Delayed ossification of nuclei - size than their age, demineralized, with
imprecise outline
More demineralized structure of diafizei
periosteum "duplicated" through calcification
Rtg. pursuit is indispensable to confirm recovery
after 2-3 weeks of treatment appears a new line of metaphysar calcification
Positive diagnosis
Anamnesis: food, sun exposure, prophilaxy with vitamin D
241
Clinical signs
Laboratory: phosphats decreased, ALP increased
Confirmation
bone Rtg (characteristic lesions)
Differential diagnosis
R. vitamin D resistent pseudocarential
autosomal-recesive
appears after 1 year
clinical signs like R.C.
treatment with vitamin D is inefficient, neces. D vit.D
forms through deficiency of 1-alfa-hidroxilasis, and others
cellular resistance to calcitriol
hypoglicemie (renal incapacity of hidroxilation)
R. hypophosphatemic
transmitere X-linkate transmission
very decreased phosphatemia
normal calcemia
treatment with vitamin D is not enough
R. from malabsorption, tubulopathies, hepatic/ renal insufficiency
All have a clinical and biological evocative context
rarely needs a differential diagnosis of:
craniotabes TO bone softening in premature
rachitic nanism other nanisme
Hypomagneziemic rachitism
defined as R.C. in which it is
hypomagneziemia (n = 1,5-2 mg%)
moderate hypocalcemia
decreased alkaline phosphatases
o in RC are increased
adm. of Mg - 8 mg/kg/day for 1-2 months in this form of rachitism, has good results
Prophilaxy
Romania - compulsory 6 years
Pregnant woman in III
rd
term - 1000 u/day oral- 2 drops Vit.D
2
ol.
New born
242
Will get from the 7
th
day- 1 drop/day , it does not matter how it will be fed
In the first 7 days vit.D can not metabolyze
The infant and child under 2 years
Needs 2 drops/day (1000 u.i.)
Except the warm months (may-september) if the child is correctly exposed to sun
and the weather is sunny - gets 1 drop/day
Premature,twins,underweight, malnutrited, those from areas intensively
polluted, with poor environmental conditions or with anticonvulsivant
treatment
Need 2 drops/day
In cold season 3 drops/day
in special medical or family situations
vit. D
2
/ D
3
- injections I.M. - 200.000 u.i. at 6-8 weeks, totally 1.200.000 UI in
the first year of life efficient for most children
Children over 2 years
It is good to get 1-2 drops of Vit.D in cold season, until school period
Add calcium
Only in premature and children who get less than 400 ml milk/day
Recommended dose - 50 mg/kg/day Ca elemental (500 mg gluconate of calcium
1 f gluconate Ca 10%)
Profilaxy RC
It does not mean only administration of vit.D
equally important, or maybe the measures of body hardening are more important
o Sun exposure
o Correct nutrition rich in meat, eggs
Treatment
Hygieno-dietetic treatment
Correct nutrition
Breastfeeding at least 3 months
Correct diversification (aport de vit. D, Ca)
Adequate life style - aired
Heliomarine cure > 1 year
Sunny , aired room
Body heardening - bathing, frections, shower, massage, gymnastics
243
Shoes with flexible sole
Curative treatment
Recommended in infants with
clinical signs
radiological
and biological signs of florid rachitism
3 therapeutically schemes are recommended and accepted in our country
Scheme I
the most used
oral adm.of vit. D: 2.000-5.000 u.i.
means 4-10 drops./day
for 1-2 months
then it will be introduced in a scheme of prophilaxy
Scheme II
- 3 doses i.m. de 100.000 UI D
2
/ D
3
- adm. at 3 days
- a total of 300.000 UI, in a week
- after 30 days a new adm. - 200.000 UI i.m.
- then vit. D in prophylaxis doses
Scheme III
adm. Of a single dose of 600.000 UI D
3
,
after 30 days continue with a prophylactic dose
if it is possible, it is recommended a daily dose of 0,5-2 mg 1,25
hidroxicolecalcipherol - 4 weeks
Calcitherapy
2-3 days before administration of vit. D
D.: 40-50 mg/kg/day as Ca gluconic, lactic, effervescent, and so on
sol. Ca gluconic 10% - in tea, soup, juice
adm. I.V. of Ca necessary only in crisis of tetany
if the nutrition is deficient in calcium, it can be prescribed for 1-4 weeks
Supplementary administration of vitamin A and C
renal eliminations of Ca
Pharmaceutic preparations
fish oil
244
fish liver oil
different combinations vit. A + D
2
/D
3
+ fluor
Vigantol, Vigantoletten, Vigorsan, Sterogyl, AT 10, Rocaltrol, Halycitrol, Calcipat
D
3
, Zymaflour
Heliomarine cure
Rules of the treatment with vit. D
splited treatment po the most efficient
pp vit. D
3
- hidrosoluble - abs.good
adm. During meals
stop 2 weeks before a helio-marine diet (recommended after 1 year)
some forms need administration of Mg
vaccination antipolio - only po; diarrhea not CI adm. vit. D
prolonged anticonvulsivant and corticotherapy - vit. D during treatment
doses when pp enriched with vit. D is administred
Evolution and prognosis
After vitaminotherapy, the biological parameters are normalized thus:
3-4 days calcemia
2-3 weeks fosfatemia and plasmatic PTH
6-8 weeks alkaline phosphatases (their normalization confirm the biological
recovery of RC)
Radiological recovery
starts after 2-4 weeks of treatment
normalization of metaphyze and epifizelor is made after 3 months
appears the line of doliu
the deformations of the long bones are corrected very slowly, under the effect of bone
remodelation (4-5 years)
some sechele will be corrected with gymnastics,
others - exceptional orthopedic correction
Recovery
"spontaneous" or through treatment with vitamins
Mild forms recovery in a few weeks, sechele
Complete recovery when the bone structure is restaurated
recovery with defect" deformations which disappear in months/ years since
treatment is started.
245
Evolution
under treatment - favorable
without treatment threatened by infections
good prognosis
some bone deformations - definitive
others need ortopedic treatment > v. 3-5 years (exceptional)
dispensarization 3 years from healing
Hypervitaminosis D - Intoxication with vit. D
Manifestations:
- rebel anorexia - vomiting
- dehydration - constipation
- azotate retention - hypercalcemia
- hypercalciuria > 5 mg/kg/24h -
is rare - should stop the administration
no exposure to UV rays - no foods rich in Ca
hospitalization in severe cases - corticotherapy
TETANY
Definition: Hyperexcitability state, neuromuscular produced by the modification of the main
ions concentration, clinically manifested through muscular spasms and seizure.
Etiology
formula of excitability Na
+
K
+
OH
-
/ Ca
++
Mg
++
H
+
hyperexcitability is produced through denominator reduction (more frequent - Ca
++
)
can be precipitated by the coexistence of a hyper-K-thousands or alkalosis
Clinical forms
tetany from rachitism
tetany-other origins
new borns tetany
Tetany from rachitism
85% of the children with tetany are rachitic
Appears mostly in cases fruste
In sunny months or after administration of vitamin D
246
in the period of R.C recovery .
When there is certain hypocalcaemia
deposit of Ca in the bones
Tetany-other origins
new born , from difficult births (diencephalic dysfunctions, mezencephalic)
intestinal affections: CF, EGS
severe nephropathies
respiratory alkalosis (after vomiting, exaggerated intake of bicarbonate, citrate,
phosphates)
hyperproteinemia
hyperpotasemia
hypomagnezemia
Clinical manifestations of tetany
spasmophilia (latent form)
- hiperexcitabilitatea neuromuscular hyper excitability manifests only when it is
caused
Tetany itself (the form manifests)
Spasmofilia (latent form)
Tests of mechanical provocation:
The Trousseau sign
applied on the cuff of the measuring device TA on the arm
it is pumped at a pressure a little over TA max.
let it 3 minutes
positive test when appearsmamos hand
The Chvostek sign
with a finger we percuss at the half distance between the tragus and oral comisura
the test is positive when it produces the contraction of orbicular m. of the lips, of
noses wing or the whole hemifee
he most faithful sign
appears the earliest
it is the last which gives up
Weiss sign
we percuss with a finger the exterior angle of the eyes
the test is positive at contraction of orbicular m. of the eyelashes
247
Lust sign
we percuss fibulas head
the test is positive when abduction and dorsal flexion of the leg is produced
EKG
elongation of the QT interval, T ample, sharp
EMG
On the normal line appear accidents which are repeated at short intervals
(doublets)
Laboratory
Ca seric (< 7 mg% or 2,25 mmol/L)
indirect, shows Ca
++
ionic, the fraction which caused the symptoms (n = 3-3,5
mg%)
Tetany itself
Intercurrent infections, mainly acute, Ca plasmatic => spasmophilia changes in tetany
Clinical signs
Tonico-clonic sizures
more often generalized
duration 15 sec. 15 min
recurrent
symetric, unpainful
days - weeks
Carpo-pedal spasm
the hand gets the aspect of mamos hand
the leg gets the aspect of equin leg
Muscle contractions
at the limbs radix
does not produce spasms
lips contraction - the mouth in fish mouth
Muscle hypertonicity
surprinde in a hypotonic rachitic patient!
the muscular contractions and hypertonicity are symmetric
sometimes painful
can associate paresthesia
Laryngospasmul
248
spasm of the glottis (of adductorilor laringelui)
wheezzing inspiration, prolonged, uncomfortable, followed by short breathing
modifications, jerky, then apnea
children are agitated, with the neck in hyperextension, cyanotic face, dilated nostrils
apnea is defeated and then a whizzing breathing appears again
the accesses last for a few minutes and repeat many times a day
Visceral spasms
makes gastric T.
cardiac T.
bronchotetany
pharynx spasms
diaphragm spasms
New borns s tetany
In the first 2 months of life, due to a transitory hypoparatiroidism => neonatal
hypocalcemia
2 forms:
early hypocalcemia
late hypocalcemia
Early Hypocalcemia
in the first 36-48 h of life
often crisis of apnea or letargy
rare convulsions, hypertonicity, laringospasm
Favoring factors:
prematurity
asphyxia, acidosis
difficult, prolonged birth
the child of a diabetic mother
Late Hypocalcemia
after feeding
iatrogenic
more often between the 5-10
th
day of life up to 6 weeks
in new born at term, artificially fed (LV, LP =rich in P, while LM is poor in P)
immature glomerular filtration P seric fa de Ca => raport Ca/P (n = 2/1)
249
insufficient paratiroidele can not compensate the situation => T
Clinical symptoms in new born
atypical, cheating
nutritional difficulties
vomiting
crisis of apnea
even lethargy instead of convulsions
Positve diagnosis
in both forms - value of calcemia
Diferential diagnosis
epilepsy
tetanus
laryngitis striduloas (pseudocroup)
tetany-other origins: hipoMg, hiperK, hypoproteinemia, alcalosis
Tetanies treatment
General measuress
ensure a quiet atmosphere
not many manipulations
airways permeability, O
2
Emergency treatment
In all clinical forms adm. of
Ca gluconic 10%2ml/kg I.V. slow
Ca gluconic repeated after 15 min.
Fast adm. => a too large quantity of Ca
++
in the atriul dr. would inhibit the
sinusal nodule => bradicardie, bloc sau stop cardiac
Paravenous adm. or I.M. leads to necrosis and calcifications
The dose can be adm. ulterior every 6 hours up to cuparea of all symptoms
in practice in a child with convulsions or laringospasm, adm.:
Diazepam 0,3 mg/kg I.V., repeated after 20-30 min.
If the convulsions do not - Ca gluconic IV
If convulsions last hypertonic Glucose 20% 2 ml/kg I.V. (logical treatment
based on the more frequent etiology of convulsions, but inefficient in case of
hypocalcemia)
In late hypocalcemia
250
interest is to keep P in the intestine through administration of Ca salts in excess
(gluconate, carbonate, lactate) => fosfat de Ca neabsorbabil
adm. 2-3 g/day disolved in milk, 7-10 days
In tetany from rachitism
after emergency treatment, therapeutically doses of Ca and vit. D are
administrated
Evolution
Characteristic tends to relapse
The disease can remain latent for a long time
Manifests only in case of precipitant factors
Mainly injections
Prognosis is good.
DIABETES MELLITUS (DM)
Definition: Diabetes mellitus is a chronic metabolic disease caused by a relative or absolute
deficiency of insulin which causes the body's inability to use glucose as an energy source.
Absence, destruction or loss of Langerhans islet beta cells cause an absolute deficiency of
insulin, which triggers type 1 diabetes (insulin-dependent diabetes - IDD).
Epidemiology: The geographical distribution of the disease varies, the world's highest rates
of incidence being found in Northern Europe (Finland, Sweden, Norway).
Low incidence of IDD are found in Asian and African populations, in Australia, New
Zealand, Central Europe.
In Romania: The risk of IDD in children in Romania is low and it remains relatively
constant during adolescence. IDD incidence in children of 0-14 years is 5.5 cases/100000
inhabitants / year. In our country, the prevalence of known cases of the disease is considered
of 3.2%. In recent years, the incidence of type 1 diabetes nearly doubled in all countries,
which advocates for significant intervention of environmental factors.
- Gender: similar trend for both sexes
- Age: The incidence rate increases with age until mid-puberty, followed by a decline
after puberty. Onset in the first year of life, although uncommon, can occur and should
be investigated in any infant or young child with unexplained or evocative symptoms.
Etiopathogeny:
251
Currently there are multiple arguments to support the theory that diabetes is the result of the
combined action of main factors:
- Genetic factors - HLA antigens common in patients with diabetes: HLA B8, B15, B18
and HLA DR3, HLA-DR4
- Immunological factors -selfdestructive factors of beta islet cells
- Islet cell antibody (ICA), which can be noticed in the patients blood several years
before clinical manifestations of the disease and are present in 60-80% of newly
diagnosed patients.
- Anti-insulin antibodies (AIA), which are present before the onset of insulin
treatment and can be evidenced in almost 100% of patients in whom the disease is
manifest before the age of 5 years.
- Antibodies to glutamic acid decarboxylase (GADA) - their appearance precedes
the clinical manifestations of the disease by a few years.
- Environment factors triggers
- Viral factors: the urlian, mumps, rubella, Coxsackie viruses, varicella-zoster,
cytomegalovirus
- Dietary factors: consumption of cow's milk introduced early in the diet, intake of
foods containing nitrosamines, chemicals found in smoked foods and some water
supply networks
- Chemical and toxic agents: aloxan, streptozotocin
Pathophysiology:
The main pathophysiologic link is the inadequate insulin activity or inability to use normal
peripheral glucose. Defining clinical manifestations are: hyperglycemia, glycosuria, ketosis,
ketonemia, ketonuria, metabolic acidosis, dehydration. Insulin deficiency causes a decrease in
the uptake of glucose in tissues, resulting in the occurrence of hyperglycemia (glucose> 200
mg / dL or 11 mmol / l).
Glycosuria occurs when the renal glucose threshold is exceeded (blood glucose> 180 mg /
dl). The kidneys can not reabsorb the excess of glucose load, causing glycosuria, osmotic
diuresis, thirst and dehydration (hyponatremia, hypokalemia). A particular type of
dehydration is installed - hypertonic with hyponatremia, hyperglycemia-induced
hyperosmolarity.
Ketonemia resulting from increased degradation of fats and fatty acids with increased
elimination of urine - ketonuria.
252
Metabolic acidosis occurs through keto-acid excess and decreased bicarbonate buffer,
innitially being compensated by decreased PaCO2 - acidotic polypneea, and when the
possibilities for compensation are exceeded, decompensated metabolic acidosis installs.
Other metabolic changes:
- increased degradation of fats and proteins leads to the production of ketones and weight
loss
- decreased triglycerides formation occurs and increased mobilization of free fatty acids
from peripheral adipose tissue
- protein production is reduced, amino acids use for gluconeogenesis in the liver increases.
Disruption of protein metabolism explains somatic growth disorder and cachexia found in
decompensated juvenile diabetes.
Classification of Diabetes mellitus (Clinical Practice Consensus Guidelines - ISPAD):
1. DM type 1 or insulin-dependent diabetes usually sets in under the age of 25 years and
can be frequently complicated by diabetic ketoacidosis.
2. Type 2 diabetes or non-insulin dependent - usually starts after the age of 30 years, and is
characterized by hyperglycemia and insulin resistance; ketoacidosis is rare.
3. Adult type diabetes of the young (MODY - maturity-onset diabetes of the young) is an
inherited form of diabetes caused by autosomal dominant transmission of defective
pancreatic cell function. Depending on the location of the genetic mutation, several
types have been described. Disease severity can vary considerably from one type to
another, but most often MODY acts like a mild form of type 1 diabetes.
4. Secondary forms of diabetes - in which the trigger is known
- diseases of the exocrine pancreas: pancreatitis, trauma, cystic fibrosis, cancer
- endocrinopathies: acromegaly, Cushing syndrome, pheochromocytoma,
hyperthyroidism
- genetic syndromes: Down, Klinefelter, Turner, Prader Willi syndrome, porphyria
- drugs, toxic substances: glucocorticoids, thyroid hormones, thiazide
- infections: congenital rubella, cytomegalovirus, others.
5. Gestational diabetes with onset or diagnosed during pregnancy
Clinical presentation
Onset:
253
1. Acute or rapid onset - occurs in small children in 4% of cases. Symptoms of a rapid onset
within 2-3 days: coma / pre-coma, thirst, abdominal pain (50% of cases), quickly installed
exicosis without vomiting and diarrhea;
2. Intermediary onset - is the most common (80-90% of cases), within 2-4 up to 6-8 weeks,
with the following suggestive signs: polyuria, polydipsia, polyphagia, weight loss,
fatigue, loss of concentration, vomiting abdominal pain;
3. Slow (extended) onset - rarely found (6% of cases), in older children and adolescents.
Sign evolution develops in months or even a year or two. Characteristic signs: thirst,
progressive polyuria, progressive weight loss (5-10 kg), decreased exercise capacity,
hunger or appetite, itching, secondary dermatitis or pyoderma.
Physical examination may reveal issues associated with other autoimmune
endocrinopathies, with a higher incidence in children with DID (thyroid disease with
symptoms of hypo-or hyperactivity and possibly palpable goiter). Cataracts may occur
commonly in girls, with a long prodrome of mild hyperglycemia. Necrobiosis lipoidica often
appears on the front of the leg as well delineated red atrophic areas.
Laboratory diagnosis:
Table X Investigations for DM
Mandatory investigations
Supplementary
investigations
Investigations for diagnosis
of complications and
treatment monitoring
fasting glucose > 126 mg% (7
mmol / l)
glycemic profile
glycosuria
cetonuria
DM suspicion?
Oral glucose tolerance test (OGTT)
HbA1c (n = 4.5 to 5.4%)
Insulinemia
C peptide
pancreatic beta cell
antibodies
Anti-islet antibodies
HLA
Leukocytosis: infection,
metabolic stress
Lipids: triglycerides, free
fatty acids, cholesterol
Ionogram, pH
T3, T4, TSH, antithyroid Atb
Microalbuminuria annually
(indicator for risk of diabetic
nephropathy)
Diagnosis criteria (According to ISPAD 2011)
- specific symptoms (polyuria, polydipsia, polyphagia, blurred vision, weight loss) +
glucose> 200 mg / dl
254
- fasting plasma glucose > 126 mg / dl
- 2-hour OGTT-glucose > 200 mg / dL (1.75 g / kg max 75 g)
- HbA1c 6.5
In the presence of obvious, intense, clinical symptoms, random screening of blood sugar,
anytime during the day, with a value > 200 mg / dl (11 mmol / l), and a fasting blood
glucose > 126 mg / dl (7 mmol / l) certifies diagnosis; transient hyperglycemias are
excluded during acute and stress diseases.
In the absence of symptoms, the physician must confirm these results on different days.
Glycemia can be determined by the capillary method, the strip or the blood glucose
meters; these are conventional techniques for daily monitoring of diabetes control.
Glycosuria - a positive test for glycosuria is suggestive, but not certain for the diagnosis
of DID. The diagnosis should be confirmed by a combination of high glycemia and
possibly ketonuria.
Ketonuria - confirms lipolysis and gluconeogenesis, which is normal during periods of
fasting.
Hyperglycemia with marked glycosuria and ketonuria = marker of insulin deficiency and
possibly diabetic acidocetosis.
Oral glucose tolerance test is performed if blood glycemia levels are not indicative. A value
of fasting blood glycemia is obtained, and then glucose is administered orally in 250 ml of
water: children under 3 years - 2g/kg, 3-10 years - 1.75 g / kg (maximum 50 g) over 10 years
- maximum 75 g; blood glycemia is again determined at 2 hours (table. ..)
Table.. Diagnosis criteria for glucose intolerance and DM
Interpretation
Diagnosis criteria
Glucose
Fasting at 2 hours
Normal values < 110 mg% < 140 mg%
Decrease of glucose tolerance 110-126 mg% 140-200 mg%
DM 126 mg% 200 mg%
255
Stages of type 1 diabetes
I. Pre-diabetes - no clinical manifestations, antibodies may be revealed (ICA, IAA, GADA)
II. Low tolerance to glucides
III. Remission "honeymoon" phase - occurs at a variable interval after the start of insulin
treatment and is due to remaining pancreatic cell hyperfunction in their attempt to produce
enough insulin to compensate the hyperglycemia.
IV. Manifest tipe 1 DM - during the remission phase, continues destruction of pancreatic
cells and eventually leads to the total lack of endogenous insulin, total diabetes being
installed.
Differential diagnosis
Table... Differential diagnosis
Mainly with Initial coma Clinical signs
With other
glycosuria
diabetes insipidus
pancreatitis
hyperthyroidism
pheochromocytoma
Cushing sdr
Genetic sdr: Down,
Turner, etc.
transient blood
sugar
stress: burns,
trauma, infections
medications:
corticosteroids,
thiazide
poisoning with
salicylates
meningoencephaliti
s - neurological
brain: edema/
infectious vascular
rupture
hyperosmolar coma
hypoglycemic coma
hyperglycaemic
coma
acute abdomen
encephalitis
other ketosis
severe dehydration
in infants
(toxicosis)
metabolic acidosis
in hereditary
metabolism
diseases
renal diabetes
chronic
tubulopathy
poisoning with
Pb, Hg
haemoglobinuria
myoglobinuria
pyelonephritis
galactozuria,
fructozuria,
pentozuria,
zaharozuria
Treatment:
Objectives:
- immediate: so that the child could have a normal life and avoid hypo- and hyper-
glycaemia,
256
- long-term: ensuring normal growth and development, psychosocial and vocational
integration, prevention of chronic complications.
Means :
1. insulin therapy
2. nutrition (diet)
3. exercise
4. medical education
5. self blood glucose control
1. Insulin therapy is always necessary in the treatment of insulin-dependent DM, its
absence being fatal (table X)
Insulin analogues (other than the chemical structure of human insulin by 1-2 amino acids) can
be short and long-term acting.
They could provide a predictable pattern of action and may eventually replace traditional
forms.
Combinations of intermediate and fast-acting insulin are available in a variety of
concentrations varying around the world from the mixture 10/90 (10% IR and 90% isophane)
to the 50/50 mixture. Premixed insulins are Humulin M and Mixtard (table X)
Table X Pre-mixed insulins
Insulin type
Ratio
Rapid insulin Semi-slow insulin
Pre-mixed Insulins
(fast + semi-slow
acting)
Mixtard 10 Actrapid 10% Insulatard 90%
Mixtard 20 Actrapid 20% Insulatard 80%
Mixtard 30 Actrapid 30% Insulatard 70%
Mixtard 50 Actrapid 50% Insulatard 50%
Humulin M2 Humulin R 20% Humulin R 80%
Humulin M3 Humulin R 30% Humulin R 70%
257
Table X Insulin preparations from Romania (according to V. erban 2007)
Product Composition Onset
(min)
Maximum
result (h)
Duration
(h)
Presentation
I. Insulin analogues with rapid action
Clear solution
1. Humalog
(Eli Lily)
Lispro insulin 5-15 1-2 3,5-4 Cartridges
(3 ml)
2. Novo Rapid
(Novo
Nordisk)
Aspart insulin 10-20 1-3 3-5 Cartridges
(3 ml)
FlexPen- pen
3. Apidra
(Sanofi-
Aventis)
Insulin glulisin 5-15 1-2 3-4 Cartridges
(3 ml)
Product Composition Onset
(min)
Maximum
result (h)
Duration
(h)
Presentation
II.Insulin with short or regular action or human soluble
Clear solution
1. Actrapid HM
(Novo Nordisk)
Human insulin
Recombined
DNA
30 2-4 Maximum
8
Vials (10 ml)
Cartridges
(3 ml)
Novolet-pen
2. Humulin R
(Eli Lily)
Human insulin
Recombined
DNA
30-60 2-4 6-8 Vials 10 ml
Cartridges
(3 ml)
3. Insuman Rapid
(Sanofi-
Aventis)
Human insulin
Recombined
DNA
15-20 1-4 7-9 Vials (10 ml)
Cartridges
(3 ml)
OpiSet-pen
Product Composition Onset
(min)
Maximum
result (h)
Duration
(h)
Presentation
258
III.Insulins with intermediary action
Turbid solution
1. Insulatard HM
(Novo Nordisk)
NPH
(Izofan)
90 4-12 16-20 Vials (10 ml)
Cartridges
(3 ml)
Novolet-pen
2. Humulin N
(Eli Lily)
NPH
(Izofan)
60-120 4-10 16-20 Vials 10 ml
Cartridges
(3 ml)
3. Insuman bazal
(Sanofi-Aventis)
NPH
(Izofan)
45-60 4-10 16-20 Vials (10 ml)
Cartridges
(3 ml)
OpiSet-pen
Product Composition Onset
(min)
Maximum
result (h)
Duration
(h)
Presentation
IV.Insulin analogues with long-lasting action
Clear solution
1 Lantus
(sanofi-Aventis)
Diarginine
glycine
(glargine)
120 - 24 Vials (10 ml)
Cartridges
(3 ml)
OpiSet-pen
2. Levemir
(Novo-Nordisk)
60-
120
- Maximum
4
Cartridge (3 ml)
FlexPen-pen
Insulin is administered in the subcutaneous tissue as 2-4 injections daily or, intravenously in
crisis. Rapid insulin therapy regime before meals and intermediate-acting insulin at bedtime
has become a widely used scheme. Insulin doses will be adjusted according to the child's
individual needs and varies according to the stage of diabetes development:
259
Table X Insulin Doses
Insulin needs 1 UI/kg/zi
- Onset period 0,5-1,5 UI/ kg/day
- Remission period (honeymoom) 0,5 UI/kg/day
- perioada de stare state period
- small children, school children (pre-puberty)
- puberty
- post puberty
1 UI/kg/day
1 UI/kg/day, to 1,5-2 UI/kg/dayi
0,8-1 UI/kg/day
- acute diseases, accidents, operations Higher doses of rapid insulin
Complications of insulin therapy:
Somogyi phenomenon as a result of hypoglycaemia during the night, due to release of
hormone antagonists, hyperglycemia occurs in the morning
Dawn phenomenon: in the morning between 5-8:00 because of low tissue sensitivity to
insulin, hyperglycemia occurs (without prior nocturnal hypoglycaemia)
allergic manifestations - local reactions may occur (redness, rash, burning, itching) at the
injection site; they are spontaneously remitted in a few days
emergence of anti-insulin antibodies
lipodystrophy - due to inadequate technique or lack of rotation of the injection site
hypoglycemia - suddenly installs in minutes; is manifested by pallor, sweating, trembling,
intense hunger, tachycardia, drowsiness.
Causes of hypoglycemia: too large dose of insulin, exercising too intensely, skipping a meal.
The treatment consists in administration of fast-absorbing glucydes orally if the patient is
conscious or intramuscular glucagon, glucose solution I.V., respectively, if the patient has
lost consciousness.
2. Diet
Daily caloric intake should be ensured according to universal recommendations, as follows:
50-55% carbohydrates
30-35% lipids (the ratio mono, polyunsaturated vegetal fats / animal saturated fat = 1)
10-15% proteins
Caloric needs (cal/day) = 1000 + 100 x age (years)
Number of recommended meals : 3 main meals + 3 snacksOverall percentage distribution of
caloric intake and carbohydrates in meals:
260
- Breakfast 20%
- Lunch 30%
- Dinner 20%
- Snacks of 10 % each (at 10, 16, 22 oclock).
The meal plan must be tailored to family habits, the school program, and insulin therapy
should be adjusted; the diet aims to balance food intake with insulin intake as well as physical
activity and get a blood sugar as much as possible within the reference range, eliminating
extremes such as hypoglycemia and hyperglycemia. Adequate intake of complex
carbohydrates (cereals) is important in the evening before bedtime in order to eliminate
nocturnal hypoglycemia.
3. Physical activity
Physical activity is a major indication for glycemic control improvement in diabetic patients,
with certain precautions. Children with diabetes should not be exempt from physical
education classes at school minimum 30-60 minutes of daily moderate exercise are
necessary. If it is unbalanced, the child will be exempt from sports until the glycemic balance
is restored.
Recommendations
glycemic selfcontrol before, during and after exercise;
sugar should always be carried along;
progressive increase in intensity and duration of physical exercise;
in the first three hours preceding effort, slow absorption carbohydrates should be eaten to
saturate muscle and liver glycogen reserves;
in case of prolonged effort children should drink sweet drinks (water with 6-8% glucose)
before exercise, during exercise and after exercise, a general recommendation is to
consume 15 g of glucydes every 40 minutes of sport;
glycemic control before bedtime following an exercise is important in order to prevent
nocturnal hypoglycemia;
dose reduction of insulin acting during or immediately after exercise;
avoid injecting insulin in an area subject to physical effort.
Complications
261
Table X DM complications
Acute complications Chronic complications
Associated autoimmune
diseases
- Hypoglycaemia
- Hyperglycemia
- Diabetic ketoacidosis
- Nutritional (Nobcourt sdr.,
Mauriac sdr.)
- Metabolic dyslipidemias
- Degenerative:
1. vascular:
- Diabetic retinopathy
- Diabetic nephropathy and
hypertension
- Diabetic neuropathy
- Atherosclerosis,
cardiomyopathy
2. Lipodystrophy and
hypertrophy at injection site
3.limitation or joint mobility.
Hypothyroidism
Hyperthyroidism
Addison's disease
Celiac disease
Necrobiosis lipoidica
Diabetic ketoacidosis - can be a life-threatening emergency - the cause is the imbalance
between insulin requirements and intake, and may be encountered at the:
- onset (inaugural ketoacidosis)
- increased insulin requirements - intercurrent infections, surgery, trauma with
progressive onset
- omission of insulin therapy or low dose administration.
Clinical presentation:
The onset is gradual: thirst, polyuria, loss of appetite, abdominal pain, polypnea, lack of
dynamism;
The state period:
Digestive symptoms (ketosis): loss of appetite, vomiting, abdominal pain
Respiratory symptoms (acidosis) polypnea, hyperpnea - Kussmaul breathing
Neurological symptoms: lack of dynamism, drowsiness, sensory obnubilation, psycho-motor
agitation, coma
Acute dehydration syndrome with diuresis (glycosuria causes osmotic diuresis), collapse
262
Particular clinical signs: acetone odor of breath (rotten apples) - halitosis acetonaemia
Diagnostic explorations :
- hyperglycemia> 200 mg / dl
- glycosuria, ketonuria
- Astrup parameters (metabolic acidosis pH <7.3, HCO3 <15 mmol / L)
- ionogram, urea, creatinine
- CBC (haemoconcentration by dehydration)
- bacteriological tests (blood cultures, urine culture, throat and ear secretion)
- EKG, SaO2
Complications:
cerebral edema, hemorrhage, thrombosis
metabolic disorders: hypokalemia, hyperkalemia, hypoglycemia
infections: septicemia
aspiration pneumonia, pulmonary edema, adult type respiratory distress syndrome
heart failure, cardiac arrhythmias, thrombosis in large vessels
pneumomediastinum, subcutaneous emphysema
Pancreatitis, intestinal necrosis
Renal failure.
Treatment : figure....
Childhood and adolescence are a time of intensive education and treatment can prevent or
delay the onset and progression of complications. Retinopathy causes vision loss and
blindness. Diabetic nephropathy causes hypertension and renal failure. Neuropathy causes
pain, numbness, muscle weakness and autonomic dysfunction. Macrovascular disease causes
heart disease, stroke and peripheral vascular disease with limb loss.
1. Good glycemic control reduces the risk of installation and progression of vascular
complications
2. Blood pressure measured annually (< 95th percentile for age)
3. Patients with diabetes should not smoke
4. Eye fundus examination should be performed immediately after the diagnosis of diabetes
- for early detection of cataract and refractive errors requiring treatment. Eye fundus
examination should be performed by a physician experienced in diabetic eye examination.
Subsequently eye fundus examination is performed once / year.
5. Screening for retinopathy and nephropathy (microalbuminuria) should be performed from
the age of 11 years and for 2 years after diagnosis.
263
6. Lipid profile - performed at diagnosis of diabetes in patients aged> 12 years. If the values
are within normal limits, then it should be repeated every 5 years.
7. Neurological examination - for the diagnosis of peripheral and autonomous neuropathy -
after the age of 11 years and for 2 years after diagnosis.
Forensic dangers, traps :
- diabetes is easy to miss in infants or pre-school children. In case of doubt, urine
glucose and glycemia are checked.
- ketoacidosis may manifest as respiratory distress (dyspnea).
- inappropriate or excessive treatment of hypoglycaemia can lead to serious
consequences.
- omission of systematic analysis of complications, particularly in the kidney and eye.
264
Chronic complications
Positive Diagnosis
KETOACIDOSIS
DIABETIC
History
Polyuria
Polydipsia
Weight loss
Abdominal pains
Vomiting
Weakness
Paraclinical
Hyperglicemia
Ketonuria
Metabolic acidosis
Clinical signs
Dehidration
Kussmaul breath
Halitosis acetonaemmia
Obnubilation
Resuscitation
Respiratory tract nazogastric
probe
Oxigenotherapy
NaCl 0,9% : 10-20 ml/kg
in 1-2 h, repeated if
necessary, without exceeding
iv Treatment
Liquid need is adjusted in 48 h
Na Cl 0,9%
EKG (T wave modifications) : add
KCl
NaHCO
3
at pH < 6,9
Shock (weak peripheric puls)
Obnubilation/Coma
Deshidration > 5%
Hyperventilation
Vomiting
No shock
Minim deshidration
Digestive tolerance
Treatment
Insulin sc
Oral hidration
Insulin 0,1 U/kg/h
at 1-2 h after initiation of hidration
Monitoring
Glucose
Ingesta-excreta
Neurologic
status
Ionogram
Acidosis persists
Glucose > 250 mg %
Glucose < 250 mg %
Neurological deterioration
Headache
Irritability
Omnubilation
Reevaluation
Calculation of iv
liquids
Insulin
Sepsis ?
iv Treatment
NaCl 0,9% (glucose > 250 mg %)
Glucose 5 % (glucose < 250 mg
%)
Exclusion
Hypoglycemia
Cerebral edema
Improvement
Good general condition
Oral hydratation
Treatment
Manitol 0,5-1g/kg
Liquid restriction
Intensive therapy
Insulina sc
Unsuccessful
treatment
Fig.... Management of
Diabetic ketoacidosis
Acc. to ISPAD 2011
265
Prognosis :
DM generally has a low immediate morbidity, except for severe ketoacidosis or
hypoglycemia.
Mortality is low, but can occur in ketoacidotic coma.
The risk of complications is related to diabetes control.
With good care, patients have the prospect of living a normal, healthy life.
insulin pumps and pancreas transplantation may improve prognosis.
Bibliography
1. American Diabetes association Standards of Medical Care in Diabetes 2013. Diabetes Care, vol 36,
Supp 1, jan 2013, p. S11-S66, care.diabetes.journals.org
2. Ghidul ISPAD 2011 pentru managementul Diabetului zaharat de tip 1 la copil i adolescent -
International Diabetes Federation, global IDF/ISPAD guideline for diabetes in childhood and
adolescence, ISBN 2-930229-72-1, 2011
3. Man Sorin C., Nanulescu Mircea V. Pediatrie practic, Ed. Risoprint, Cluj-Napoca, 2006, ISBN
973-751-131, p. 448-472
4. Micle Ioana Diabetul zaharat al copilului i adolescentului n Georgescu A. Ciofu E - Ghiduri i
protocoale n Pediatrie, Ed. Medical Amaltea, Bucureti, 2008, p. 77-109
5. Mihai Cristina Maria, Catrinoiu Doina. Ghidul de tratament al copilului i adolescentului cu diabet
zaharat, Ed. Universitar Carol Davila, Bucureti, 2008, ISBN : 978-973-708-328-9
6. Moraru Dan, Evelina Moraru, Carmen Oltean, Laura Bozomitu, Bogdan A. Stana. Recent Data on
Type 1 Diabetes Mellitus in Children. Revista Romn de Pediatrie Vol. LVII, Nr. 3, 2008, p. 214-
227
7. Popa I, Velea I. - Cap. Diabetul zaharat n Ciofu E., Ciofu Carmen Pediatria Tratat, Ed. Medical,
Bucureti, 2001, p. 1304-1320
8. Ramin Alemzadeh, David T. Wyatt - Diabetes Mellitus in Children n Kliegman R.M., Behrman R.E.,
Jenson H.B. et al (eds) - Nelson Textbook of Pediatrics, 18
th
edition, Saunders Elsevier, Philadelphia,
2007, p. 2404-2433
9. erban V Diabetul zaharat de tip 1 al copilului i tnrului Ghid practic, Ed. Marineasa,
Timioara, 2007
10. Velea I., Corina Paul. Diabetul zaharat n Nanulescu M. - Protocoale de diagnostic i tratament n
pediatrie, Ed. Medical Amaltea, Bucureti, 2013, p. 212-224
266
CHAPTER VII - RENOURINARY SYSTEM DISORDERS
ef lucr. Dr. Duicu Carmen
URINARY TRACT INFECTIONS (UTI)
Definition
UTI are defined as an inflammatory bacterial processes of the urinary tract and/or renal gap,
characterized by localizing symptoms or systemic features and significant bacteriuria.( the
American Academy of Pediatrics (AAP) criteria for the diagnosis of UTI in children 2-24
months are the presence of pyuria and/or bacteriuria on urinalysis and of at least 50,000
colony-forming units (CFU) per mL of a uropathogen from the quantitative culture of a
properly collected urine specimen)
Termincludes localizations such as cystitis, pyelitis, pyelonephritis, with hard delimitation in
children.
Precise estimates of rates of UTI are difficult to ascertain, because of asymptomatic forms
that may lead a minus in diagnosis, while the improper method of collection of a urine
sample may cause excess in UTI diagnosis.
Frequency increases with age. It is generally more common in females. During the first year
of life, the male: female ratio is 2.8-5.4: 1, appearing even forms of urosepsis. There are
differences in frequency related to age and sex, so in newborns and in infants symptomatic
UTI is 3 times more common in males than females. After this age it is more common in
females (2.8%). The risk of relapse is proportional to the previous ITU. After the first UTI,
60-80% of girls will develop a second UTI within 10 months.
After 1 year of age there is a striking female preponderence, with a male: female ratio of
1:10; while at school age it is 30 times higher in girls than in boys.
Ethiology
UTIs are caused mainly by colonic bacteria, with a predominence of Gram-negative
organisms: Eserichia coli ( more than 80% of childhood UTIs), Enterobacter (5-10%),
Proteus, Klebsiella and Pseudomonas; the gram-positive organisms: Staphylococcus (is
usually considered a contaminant, but it can cause illness), Enteroccocus fecalis, Group B
Streptocuccus; other bacteria: Chlamydia trachomatis. Viral infections, particularly
adenovirus, also may occur, especially as a cause of cystitis.
267
More recently Mycoplasma homminis and Ureaplasma urealyticum are involved in the
etiology of UTIs; the bacteria being responsible for urogenital tract infection, sexual
transmited disease.
Risk factors for UTIs:
Female gender- shorter urethra < 2 cm, opened in the anatomic contaminated area
Obstructive uropathy- congenital/aquired anomalies,vesicoureteral reflux,
ureteropelvic junction(UPJ) obstruction, kidney stones, kidney dysplasia,
hydronephrosis, polycystic kidney disease, etc
stasis constipation, pregnancy, neuropathic bladder
vesicoureteral reflux (in 20-70% of the children with UTIs) stasis; infection can
cause retrograde flow
race Caucasian children incidence vs. afro-americans
other causes: Wiping from back to front in females, toilet training, urethral
instrumentation, genital infections , Sexual activity, Pinworm infestation, high blood
pressure, diabetes mellitus, cirrhosis, hypogammaglobulinemia, failure to thrive, etc
Voiding dysfunction
Uncircumcised male
Anatomic abnormality (labial adhesion)
Tight clothing (underwear)
Factors related to the causative organisms:
- nefritigene strains of E. coli with capsular polysaccharide surface antigens (K1,
K2, K3, K12, K13) resistance to opsonization, phagocytosis and bactericidal
activity of serum
- virulence strains of E. coli fimbriae, P fimbriae (are more likely to cause
pyelonephritis)
- Epithelial receptors influence the adherence
- Endotoxins of the germs
Pathogenesis
Virtually all UTIs are ascending infections. The bacteria arise from fecal flora, colonize the
perineum, and enter the bladder via the urethra. In uncircumcised boys, the bacterial
pathogens arise from the flora beneath the prepuce. Rarely, renal infection may occur by
hematogenous spread, as in endocarditis or in some neonates. If bacteria ascend from the
bladder to the kidney, acute pyelonephritis may occur.
268
Classification
Depending on symptoms and location:
- Symptomatic: upper UTI (pyelonephritis - DMSA scan) or lower UTI (cystitis)
- Asymptomatic: asymptomatic bacteriuria (most common in girls)
Depending on the presence of complications:
-uncomplicated
-complicated (hypertension, sepsis)
Depending on evolution: acute UTI; recurrent UTIs (unresolved or reinfection), persitent UTI
(chronic).
Functional: with or without renal failure
Clinical manifestation
The history and clinical course of a UTI vary with the patient's age and the specific diagnosis.
No one specific sign or symptom can be used to identify UTI in infants and children.
Neonates and infants up to age 2 months who have pyelonephritis usually do not have
symptoms localized to the urinary tract. UTI is discovered as part of an evaluation for
neonatal sepsis. Neonates with UTI may display the following symptoms: fever, jaundice,
failure to thrive, poor feeding, vomiting, irritability, etc
Infants and children aged 2 months to 2 years: symptoms are nonspecific, usually they
present with systemic features such as: poor feeding, high fever, vomiting, strong-smelling
urine, abdominal pain or tenderness, irritability, malaise, etc
Children aged 2-6 years:Preschoolers with UTI can display the following symptoms:
gastrointestinal signs, such as vomiting and diarrhoea, abdominal pain, fever, strong-smelling
urine, cloudy urine, enuresis, urinary symptoms (dysuria, urgency, frequency)
Children older than 6 years and adolescents.School-aged children with UTI can display the
following symptoms: fever, vomiting, abdominal pain, flank/back pain, strong-smelling
urine, urinary symptoms (dysuria, urgency, frequent voiding), enuresis, incontinence;
suprapubic, abdominal or lumbar pain may appear with or without fever.
Physical examination. It is mandatory to look for phimosis, labial adhesion, signs of
pyelonephritis, epididymo-orchitis, and stigmata of spina bifida, e.g. hairy patch on the sacral
skin. The absence of fever does not exclude the presence of an infective process.
Physical examination findings in pediatric patients with UTI can be summarized as follows:
- Costovertebral angle tenderness
- Abdominal tenderness to palpation
- Suprapubic tenderness to palpation
269
- Palpable bladder
- Dribbling, poor stream, or straining to void
Clinical evaluation includes: physical exam, blood pressure measurement, genitalia exam,
lumbar sacral region exam.
Laboratory tests
The definitive diagnosis of infection in children requires a positive urine culture. Urine must
be obtained under bacteriologically reliable conditions when undertaking a urine specimen
culture. A positive urine culture is defined as the presence of more than 100,000 cfu/mL of
one pathogen. The urine specimen may be difficult to obtain in a child less than 4 years old
and different methods are advised since there is a high risk of contamination.
If the culture shows >100,000 colonies of a single pathogen, or if there are 10,000
colonies and the child is symptomatic, the child is considered to have UTI.
The American Academy of Pediatrics (AAP) criteria for the diagnosis of urinary tract
infection (UTI) in children 2-24 months are the presence of pyuria and/or bacteriuria on
urinalysis and the presence of at least 50,000 colony-forming units (CFU) per mL of a
uropathogen from the quantitative culture of a properly collected urine specimen. In neonates
younger than 2 months of age, criteria include the presence of lower amounts of a single
pathogen (10,000-50,000 CFU/mL).
Collection of the urine:
Midstream urine collection is possible and reliable in older children with sphincteric control.
Suprapubic bladder aspiration is the most sensitive method, even though urine may be
obtained in 23-99% of cases.
Bladder catheterization is also a most sensitive method, even though there is the risk of
introduction of nosocomial pathogens.
Plastic bag attached to the genitalia Prospective studies showed a high incidence of false-
positive results, ranging from 85-99%.
Quantification of bacteriuria
The final concentration of bacteria in urine is directly related to the method of collection,
diuresis, method of storage and transport of the specimen. Promp plating of the urine sample
is important, because if the urine sits at room temperaturefor more than 60 min, overgroth of
a minor contaminant may suggest a UTI when the urine may not, in fact, be infected.
Refrigeration (4
0
C), for maximum 24 hours, is a reliable method of storing the urine until it
can be cultured.
270
A urinalysis shoul be performed from the same specimen that was cultured.
The presence of pyuria (more than 5 leucocytes per field) and bacteriuria in a fresh urine
sample will reinforce the clinical diagnosis of UTI.
Pyuria (leucocytes in the urine, > 5 leucocytes/ power field) suggest infection, but infection
can occur in the absence of pyuria, consequently this finding is more confirmatory than
diagnostic. Conversely, pyuria can be present without UTI.
Nitrites and leucocyte esterase ussually are positive in infected urine.
Whide blood cell casts in urinary sediment suggest renal involvment.
If the child is asymptomatic and the urinalysis result is normal, it is unlikly that there is a
UTI. However, if the child is symptomatic, a UTI is possible, even if the urinalysis result is
negative !!!
Gram staining:
Other analyses: Urinary sediment , complet blood count, reactants of acute phase (ESR,
CRP); renal function: urea, creatinine; electrolytes, immunogram, proteinogram, glycemia,
blood culture pyelonephritis, sepsis in new born with UTI
Table x. Criteria of UTI in children (according to European Association of Urology
Guideline):
Urine specimen from
suprapubic
bladder puncture
Urine specimen from
bladder
catheterization
Urine specimen from
midstream
void
Any number of cfu/mL (at
least 10
identical colonies)
> 1,000-50,000 cfu/mL > 104 cfu/mL with symptoms
> 105 cfu/mL without
symptoms
Bacteriuria without pyuria may be found:
in bacterial contamination
in colonization (asymptomatic bacteriuria)
when collecting a specimen before the onset of an inflammatory reaction.
In such cases, it is advisable to repeat the urinalysis after 24 hours to clarify the
situation
Pyuria without bacteriuria may be due to:
incomplete antimicrobial treatment of UTI
271
urolithiasis and foreign bodies
infections caused by Mycobacterium tuberculosis and other fastidious bacteria, e.g.
Chlamydia trachomatis.
Imaging studies
- the goal of imaging studies in children with a UTI is to identify anatomic
abnormalities that predispose to infection
- are mandatory from the first episode(ultrasonography for all children with UTI !)
- the gender does not matter
Indications:
- All newborns
- Recurrent UTI
- pyelonephritis
1. renal ultrasound: reveals malformations, hydronephrosis, renal duplicity,
ureterocele, UPJ obstructions, kidney stones, obstructive uropathy, etc. In acute
pyelonephritis: enlarged kidney, loss of corticomedullary differentiation, increased
renal echogenicity
2. Voiding cystourethrogram (VCUG) is performed to detect vesicoureteral reflux. Is
recommended after upper UTI, recurrent UTI or when renal sonogram shows a
significant abnormality: hydronephrosis, disparity of renal length, bladder wall
thickening, bladder obstruction: posterior urethral avlve.
3. Renal scanning with DMSA (dimercaptosuccinic acid)- static and dynamic (with
DTPA + furosemid). DMSA scan demonstrate renal focal abnormalities, renal scars,
determine differential renal function
4. Nativ Renal X-ray : for radio-opacue calculi /stones
5. Intravenous pyelography: has been replaced by renal ultrasound and DMSA scan;
give informations about: size, shape of the kidney, pyelocaliceal system,
ureters,urinary bladder
6. urodinamic investigations (uroflowmetry)
- Assessment of lower urinary tract
- Bladder function - storage, transport, emptiness
7. Pelvic exam
Diagnosis has the next steps:
Establish the diagnosis of ITU
Etiologic diagnosis
272
localization (upper/ lower UTI)
presence of risk factors
UTI rebound upon the renal function
Clinical forms:
1. Acute pyelonephritis (upper UTI) Clinic: abdominal or flank pain, malaise, nausea,
vomiting, sometimes diarrhea. In newborn, nonspecific symptoms: decreased appetite,
irritability, weight loss, prolonged jaundice, etc. Involvment of the renal parenchima =
acute pyelonephritis, whereas if there is no parenchymal involvment= pyelitis.
2. Pyonephrosis: accumulation of purulent material in the renal pelvis and renal
collecting system with obstructive hydronephrosis. Symptomatologia-result similar to
that of acute pyelonephritis.
3. Renal abscess is established by the hematogenous spread of the infection pathway in
other dynamic sites without genitourinary tract or by extension a high ITU. Clinic:
signs of severe pyelonephritis, fever, pain in the flanks, leukocytosis and occasionally
sepsis. The diagnosis is ultrasound.
4. Cystitis (lower UTI) - bladder involvement - and those can be viral (adenovirus).
Symptoms: dysuria, urgency micturition, pollakiuria, suprapubic pain, urinary
incontinence, smelly urine, hyperchrome.
5. Asymptomatic bacteriuria - is defined by positive urine culture in the absence of
any symptoms of urinary infection. Occurs more frequently in women at preschool
and school age groups. Incidence is declines with increasing age. It does not cause
kidney damage.
Positive diagnosis
Significant bacteriuria
piuria
Evidence the germs
Other analyzes
Diferential diagnosis
I. Between upper and lower UTI
II. urethrites (irritative- soap), vaginitis,vulvovaginites, traumas, sphincter- detrusor
dissinergy (which produces incontinence)
III. other causes of enuresis/ voiding disfunction
IV. pneumonia, gastroenteritis, apendicitis, pelvic inflammations- with symptoms similar
to acute pyelophritis with general manifestations
273
Complications
septicemia (new born, urinary malformations)
Renal scars ( HBP, risk of CRF)
calculogenezis
chronic pyelonephritis
Hospital Admission Criteria:
Hospitalization is necessary for the following patients with UTI:
- Patients who are toxemic or septic
- Patients with signs of urinary obstruction or significant underlying disease
- Patients unable to tolerate adequate oral fluids or medications
- Infants younger than 2 months with febrile UTI (presumed pyelonephritis)
- All infants younger than 1 month with suspected UTI, even if not febrile
Treatment
General treatment
1. Hygiene
Wipe in the correct direction, from front to back, after using the bathroom
Clean the bladder area first when washing to prevent contamination with bacteria from other
parts of the body.
Take showers and avoid prolonged baths.
Use tampons for periods. Tampons are advised during the menstrual period rather than
sanitary napkins or pads because they keep the bladder opening area drier than a sanitary pad,
thereby limiting bacterial overgrowth.
Extremely effective is avoiding long intervals between urinating. Try to empty the bladder at
least every 4 hours during the day while awake, even if the need or urge to void is absent.
When feeling the need to empty the bladder, do not try to hold it until a more convenient
time or place.
2.Clothing: Cotton underwear for general use is suggested.
3. Diet: Empty the bladder at least every 4 hours. Drink more water and consider drinking
cranberry juice (or taking cranberry pills). It cannot harm. Start with 1 extra glass with each
meal. If the urine appears any darker than a very pale yellow, this means not enough liquid is
being ingested; increase the fluid intake.
4. Activities:
make sure to empty the bladder frequently and drink plenty of water and other fluids.
274
Take special precautions after sexual activity; such activity may also increase risk because it
can introduce bacteria into the bladder area. The bladder should be emptied after intercourse;
drink 2 extra glasses of water.
- Combat/treat constipation
- Urine acidification (1-2 tb. Vit. C 200) germs proliferation
(Not if it gets aminoglicozids, which has a better action in the alkaline environment)
II. Medicines
parenteral treatment (I.V.) with antibiotics
Indications
Febrile cases
complications (urinary malformations, renal abces)
New born, infants and children under 2 years old
Reduced compliance
Gastric intolerance: nausea, vomiting, diarrhea
It can be used:
Aminoglycoside antibiotic- parenteral route
Amikacin (Pierami, Amikin): 15 mg/kgc/day, 2 (3) doses I.V./I.M.
Netilmicin (Netromycin): 6-7,5 mg/kgc/day, in 2 (3) doses I.V./I.M.
Tobramycin (Nebcin, Brulamycin): 5 mg/kgc/day, in 3 doses I.V./I.M.
Gentamicin: 7,5 mg/kg/day, in 3 doses, I.V./I.M., it will be given only if
there is no other treatment option (because of nephrotoxicity and ototoxicity)
Cephalosporins - i.v.
Ceftriaxon (Cefort, Rocephin): 75 -100 mg/kgc/day, 1 dose.
Cefuroxim (Axetine): (50)-100 mg/kgc/day, in 2-3 doses
Cefotaxim (Cefotax): 150 mg/kgc/day, in 3-4 doses
Ceftazidim (Ceftami): 100150 mg/kg/day, in 3 doses
In acute febrile infection sugestive of pyelonephritis, a 10 to 14- day cours of antibiotics
capable of reaching significant tissue level is preferable. Children who are dehydrated, are
vomiting, or unable to drink fluids, newborns and infants or in whom urosespis is a
possibility shoult be attmited to the hospital for intravenous antibiotiv therapy and
rehidrattion. Parenteral antibiotics may be used with daily follow-up until the patient is
afebrile for 24 hours.
275
Complete 10-14 days of therapy with an oral antibiotic that is active against the infecting
bacteria. For a safety period of 24-36 hours, parenteral therapy should be administered. When
the child becomes afebrile and is able to take fluids, he/she may be given an oral agent to
complete the 10-14 days of treatment, which may be continued on an outpatient basis.
b. Oral treatment is recommanded in the other cases.
Aminopenicillins:
- amoxicillin/clavulanate (Augmentin Bis, Amoxiklav susp 457mg/5ml: 40-50 mg/kgc/day
in 2 doses
Sulphonamides:
- sulfamethoxazole-trimethoprim (SMZ-TMP). ( Sumetrolim, Epitrim, Biseptol, Bactrim):
6-12 mg/kgc/day TMP and 30-60 mg/kg/day SMZ in 2 doses
- Sulfisoxazole 120150 mg/kg/day in 4 doses
Cephalosporins:
Third generation
Cefixime ( Eficef, Suprax,etc ) 8 mg/kg/day in 1-2 dose PO
Cefpodoxime 10 mg/kg/day in 2 doses PO
Ceftibuten (Cedax): 9 mg/kgc/day in 1 dose P.O.
Second generation:
Cefuroxim axetil (Zinnat, Axycef susp 125mg/5ml sau cp a 250mg, 500mg) 20-
30mg/kgc/day in 2 doses
Cefprozil (Cefzil,Procef, Cronocef) 30 mg/kg/day in 2 doses
Cefaclor (Ceclor, Cefaclor, Ceclodyne): 20 mg/kgc/day in 3 doses P.O.
First Generation:
Cefalexin (Keflex, Ospexin): 25-50 mg/kgc/day in 2-4 doses P.O.
Cefadroxil (Cexyl susp 250mg/5ml) 25mg/kg/day in 2 doses P.O.
A simple UTI is considered to be a low-risk infection in children. The duration of treatment
in uncomplicated UTIs treated orally should be 5-7 days.
Nitrofurantoin 5-7 mg/kg/24 hr in 3 to 4 divided doses, reomended just in lower UTIs (! It
does not achive significant renal tissue levels).
in forms with resistant germs (ex Pseudomonas) treatment is based on the culture sensibility
Meronem (Meropenem) 10-20 mg/kg/dose every la 8 hous, I.V.
Imipenem (Tienam) 15 mg/kg/dose, every 6 hours, I.V.
Ciprofloxacin,Norfloxacin, Levofloxacin 15 mg/kgc/day in 2 doses P.O./IV
276
Ceftazidim (Ceftamil) 100150 mg/kg/day, in 3 doses
Ticarcilina (Timentin) 300mgmg/kg/day in 3 doses I.V
Prevention of reccurent UTI- is recomanded in case of:
- Reccurent UTIs
- Abnormal renal ultrasound in neonates
- Bladder catheterization
- After an episod of acute pyelonephritis (upper UTI): for 4 to 6 weeks until the
imagistic studies are completed or if there are risk factors
In case of renal anomalies (obstructive uropathy, vesicuretheral reflux, etc ) prophylaxis is
recomended until the abnormality is solved by medical or surgical treatment. Sometimes it is
necessary life long. If there is an increased risk of pyelonephritis, e.g. VUR, and recurrent
UTI, low-dose antibiotic prophylaxis is recommended. It may also be used after an acute
episode of UTI until the diagnostic work-up is completed.
For prophilaxis it may be used:
sulfamethoxazole-trimethoprim (SMZ-TMP).: 2 mg/kgc/day (TMP), single dose-
evening
Nitrofurantoin: 1-2 mg/kgc/day, 1 dose- evening
Nalidixic Acid (Negram, Nalixid, etc): 20 mg/kgc/day in 1-2 doses
Cephalexin, Cefaclor: 10 mg/kgc/day, 1 doses- evening
Augmentin Bis: 10 mg/kgc/day, 1 dose evening (amoxicilina)
In simple UTIs we may reccomand:
- Urinary antiseptics (Uricol, Urisan, Urinal, Cystenal, etc)
- Cranberry products
- Immunotherapy with Uro-Vaxom 1 cps/day P.O. , a 3 months cours.
III. Surgical treatment is recommended in case of congenital kidney anomalies, kidney
stones, etc.
Evolution: with adequate treatment is favorable. We can not predict the recurrency, but we
may prevent them.
Without treatment, acute pyelonephritis may lead to renal scars and kidney damage
Prognosis: is good, depends on diagnosis precocity and treatment.
Chronic pyelonephritis is an important ethiologic factor in chronic kidney disease (CKD).
277
VESICOURETERAL REFLUX (VUR)
Retrograde flow of urine from bladder to the ureter and renal pe4lvis is referred as
vesicoureteral reflux.
It can be unilateral or bilateral.
VUR represents the main cause of UTI in children (it is found in 15-70% of patients with
UTIs, depending on age).
Classification:
1. Based on grading of the reflux
Voiding cystourethrography (VCUG) is the criterion standard in diagnosis of VUR, providing
precise anatomic detail and allows grading of the reflux. The International Classification
System for VUR is as follows:
- Grade I - Reflux into nondilated ureter
- Grade II - Reflux into renal pelvis and calyces without dilation
- Grade III - Reflux with mild to moderate dilation and minimal blunting of fornices
- Grade IV - Reflux with moderate ureteral tortuosity and dilation of pelvis and calyces
- Grade V - Reflux with gross dilation of ureter, pelvis, and calyces, loss of papillary
impressions, and ureteral tortuosity
Fig ccc. International grading system for vesicoureteral reflux (From International reflux
Study Comittee, Pediatrics 1981;67:392-400)
2. Based on ethiology:
- Primary: congenital incompetence of the valvular mechanism of the vesicoureteral
junction or associated with other malformations of the ureterovesical junction
(ureteral duplication, ureterocele with duplication, ureteral ectopia, etc)
278
- Secondary to: increased intravesical pressure(neuropathic bladder, posterior
urthral valve, etc); inflammatory processes (foreign bodies, vesical calculi, etc);
surgical procedures involving the ureterovesical junction
Types of refluxes:
- Reflux occuring during bladder filling= low pressure or passive reflux: a
permanent retrograde flow of urine statis chronic pyelonephritis reflux
nephropathy CKD
- Reflux during voiding is tremed as high-pressure or active reflux
Clinical manifestation:
- clinical UTI
- hydronephrosis, often prenatally identified using ultrasonography.: VCUG: VUR
in 40%
- voiding disfunction/ enuresis
- renal insufficiency:
- hypertension
Diagnosis: based on VCUG
Signs of poor outcome: UTI reccurency despite prophylaxis, hypertension, proteinuria and
CKD
Treatment: the goals are to prevent pyelonephrities, renal injury and other complications of
reflux
- medical treatment: antimicrobial prophylaxis
- surgical therapy:endoscopic antireflux techniques (Deflux), open surgical
techniques for children who fail medical therapy (development of new renal
scars, failure of reflux to resolve, a low chance to resolve: grade V VUR,
reccurent UTI despite appropiate antibiotic prophylaxis, etc)
Follow-up:
- periodic urinalysis: initially monthly, then at 3 or 6 month; immediately in case of
febrile illness)
- Assessment of renal function once a year: urea, creatinine, proteinuria
- annual BP measurement
- imaging studies- reassessment (ultrasound, VCUG, DMSA scan)
279
ACUTE GLOMERULONEPHRITIES (AGN)
Acute glomerulonephrities (GN) comprises a specific set of renal diseases in which an
immunologic mechanism triggers inflammation and proliferation of glomerular tissue that
can result in damage to the basement membrane, mesangium, or capillary endothelium.
Acute GN involves both structural changes and functional changes.
Hyalinization or sclerosis indicates irreversible injury.
These structural changes can be focal, diffuse or segmental, or global.
Functional changes include proteinuria, hematuria, reduction in GFR (ie, oligoanuria), and
active urine sediment with red bloob cells (RBCs) and RBC casts. The decreased glomerular
filtration rate (GFR) and avid distal nephron salt and water retention result in expansion of
intravascular volume, edema, and, frequently, systemic hypertension.
Etiology:
-most frequent postinfections:
- bacterial infections: frequent Streptococcus group A; pneumococcus,
Staphylococcus, etc
- viral infections: Epstein-Barr virus, parvovirus B19, CMV, coxsackie, rubella,
mumps, Hepatitis B, etc
- parasites: Plasmodium malariae, Plasmodium falciparum, Schistosoma mansoni,
Toxoplasma gondii, Filaria
- secondary GN: Henoch-Schonlein purpura, systemic lupus erythematosus (SLE),
bacterial endocarditis, Goodpasture syndrome
- toxic or allergic factors: drugs, vaccine, etc
Evaluation
1. Anamnesis:
- Case history: acute streptococcal tonsillitis (1-2 weeks previously), pyodermitis/
impetigo (3 weeks previously), vetriculoperitoneal shunt
- Family history: hematuria/ renal failure deathness = Alport syndrome
Autoimmune diseases: SLE, etc
280
2. History (table 2)
Macroscopic hematuria:
- Painless, Dark brown-colored urine; with the same
aspect during micturition
- GN
Post upper respiratory tract infection, macroscopic
hematuria during acute episode, otherwise microscopic
hematuria
1-3 days: IgA nephropathy(Berger
disease)
Post acute tonsillitis/ pyodermitis; edema, HBP,
hematuria, oliguria
7-10 days: postinfectious GN
(recurency- less reliably)
Concomitent with an upper resiratory tract infection, a
positive case history of glomerular disease; anemia+
hyperazotemia from begining, high blood pressure
(HBP)
Acute phase of chronic GN
Edema, weight gain | Nephrotic
syndrome/glomerulonephrities;
Chronic renal failure
Edema, hematuria, Diminished urine output (300-150
ml/m
2
/day), HBP
AGN (acute glomerulonephrities)
Rash (95-100%), Palpable purpura, particularly on the
buttocks and legs , Gastrointestinal symptoms, arthritis
(big joints)
Henoch Schonlein Purpura (HSP)
Glomerulonephities, hemolitic anaemia,
trombocytopenia, purpura
Hemolitic uremic syndrome
+ case history , hematuria, proteinuria, HBP, fever,
hepatosplenomegaly, arthritis, purpura; + blood culture
Shunt nephritis
HBP, nepfromegalia, renal insufficiency, familal history
of hematuria
ADPKD(Autosomal Dominant
Polycystic Kidney Disease)
Fever, arthritis (small joints), rash, females SLE
Hematuria, proteinuria, dry cough +/-hemoptysis, HBP,
chronic renal failure
Goodpasture sdr
Clinical manifestations of endocarditis+
micro/macroscopic hematuria, proteinuria, + blood
culture
Acute/subacute bacterial
endocarditis
281
3. Clinical characteristics:
Skin :
- pallor: haemolytic uraemic syndrome (HUS), systemic lupus erythematosus ,
glomerulonephritis
- Rash : Henoch- Schonlein purpura , SLE, HUS , other vasculitis ,
fat
- Swelling : nephrotic syndrome , glomerulonephritis, acute/chronic renal failure
Osteoarticular system
- Arthritis: Henoch- Schonlein purpura , SLE
Cardiovascular System
- HBP,
- Tachycardia, gallop rhythm
- Turgid jugular vein, venous pulsation at this level
- Murmurs : bacterial endocarditis
Respiratory System : tachypnea ( secondary to fluid overload )
- acute pulmonary edema signs ( polipnea , orthopnea , cough with frothy sputum ,
rodents, anxiety, sweating, cyanosis, stetacustic: pulmonary crackles )
Digestive System:
Oral and nasal bleeding at this level: ANCA + vasculitis ( Wegner granulomatosis )
abdomen :
- Nephromegalia : parenchymal nephropathy
- Hepato + / - splenomegaly : systemic disease , shunt nephritis
- marked abdominal pain: HSP
Nervous system and sense organs :
- Ocular abnormalities and / or hearing : Allport syndrome
- Signs of acute cerebral edema (Amaurosis fugax = transient monocular or binocular
visual loss), headache, vomiting, seizures, coma ) :AGN
4. Labs tests
The first line/intention:
Urinalysis with sediment:! RBCs- dysmorphic, erythrocyte casts, hyaline and granular
casts
Proteinuria/24 hours: moderate / significant (gold standard), or report protein / creatinine
and urinary albumin / creatinine urine from urinary spot
at family members (Alport sdr.)
282
- ! nonselective protinuria
2. Blood: Complete CBC, urea, creatinine, ionogram, protein,! Serum complement
levels: CH50,C3, C4; antistreptolysin O (ASO), anti-DNAse B, antistreptokinase, anti-
NADase, antihyaluronidase antibody
Later stage: acute phase reactions, immunogram, CIC, antinuclear antibody, anti-DNA
antibody, ANCA, anti-GBM antibody, serology for EBV and hepatitis B and C; renal
ultrasound, renal biopsy (light microscopy and immunofluorescence)
Other investigations: ASTRUP, EKG, fundus examination
Acute nephritic syndrome is the most serious and potentially devastating form of the various
renal syndromes.
GLOMERULONEPHRITIS ASSOCIATED WITH INFECTIONS
Most often, at least in children, acute nephritic syndrome is secondary to acute postinfectious
glomerulonephritis.
Definition: = immune inflammatory processes involving the renal glomeruli with exudative
and proliferative lesions of the glomerular capillary. When damage of glomeruli is uniform,
we speak about diffuse acute glomerulonephritis.
Glomerular lesions in acute GN are the result of glomerular deposition or in situ formation of
immune complexes. On gross appearance, the kidneys may be enlarged up to 50%.
Histopathologic changes include swelling of the glomerular tufts and infiltration with
polymorphonucleocytes. Immunofluorescence reveals deposition of immunoglobulins and
complement.
Ethiology:- see above
Postinfectious GN can occur at any age but usually develops in children. Most cases occur in
patients aged 5-15 years; only 10% occur in patients older than 40 years. Outbreaks of PSGN
are common in children aged 6-10 years. Acute nephritis may occur at any age, including
infancy.
Acute GN predominantly affects males (2:1 male-to-female ratio). Postinfectious GN has no
predilection for any racial or ethnic group. A higher incidence (related to poor hygiene) may
be observed in some socioeconomic groups.
Nephritic syndrome is defined by the presence of characteristic clinical manifestations and
laboratory findings.
1. Oliguria/oligoanuria. Diminished urine output: 300-150 ml/m
2
/day, (urine
output <1ml/kg/day in infants; <0.5ml/kg/day in children) .
283
2. Edema (peripheral or periorbital) are soft, white. It is reported in approximately 85% of
pediatric patients; edema may be mild (involving only the face) to severe, bordering on a
nephrotic appearance.
3. Hypertension and cardiovascular overload. HBP is due to increased peripheral resistance
(due to arterial vasoconstriction produced as a result of increased secretion of renin) and
vascular overload.
Overloading the circulation may be evidenced by hepatomegaly, jugular vein turgit, gallop
rhythm, to pulmonary edema .
4. Hematuria . It can be macro- or microscopic. It appear as a dark coloured urine, reddish
brown like beer; like meat or tea-colored washings concentrated .
Urinary sediment contain RBCs, RBC casts, hyaline and granular casts.
5. Proteinuria. As the volume and concentration of urine depends on liquids ingestion and
renal function is more accurate to determin proteinuria in urine collected within 24 hours.
Normal is less than 100 mg/24 h .
In AGN proteinuria varies between 300 mg 1-2g / 24h .
100-500 mg/24 - mild proteinuria
500-2000 mg/24 h - moderate proteinuria
> 2000 mg/24 - massive proteinuria
6. Azotemia is the result of reduced glomerular filtration rate leading to increased blood urea
nitrogen, creatinine, uric acid , phosphates , etc.
7. Anemia is mild, normochromic with Hgb 9-11 g/dl .
8. Electrolyte and acid-base disorders :
-hyperkalemia resulting from a reduction in urinary excretion of K + concomitent with the
ingestion and contribution of cellular catabolism .
-metabolic acidosis - installed with reduced urine output and becomes obvious when severe
oliguria is present.
Pathology
There are some common signs in most forms of AGN. Glomeruli are enlarged, some
capillaries are blocked, capillary edema and polymorphonuclear infiltration, mesangial
edema, cellular proliferation of one or more types of glomerular cells (endothelial, mesangial
and epithelial).
Sometimes can be found the gap infiltrated with mononuclear or polymorphonuclear.
284
ACUTE POSTSTREPTOCOCCAL GLOMERULONEPHRITIS (APSGN)
Definition: It is a self-limiting complication of poststreptococcal infections, an upper
respiratory tract or a skin infection with a nephritogenic strain group A |-hemolytic
streptococci. It is a proliferative glomerulonephritis that occurs with increased frequency in
boys between 5-15 years.
- Is the main cause of acute nephritic syndrome (80% of cases).
APSGN is characterized by:
Clinical: an acute nephritic syndrome
Etiology: group A | hemolytic Streptococcus
pathogenesis: mediated by circulating immune complexes
pathological: diffuse endocapillary proliferative glomerulonephritis with numerous
polynuclear cells and the presence of humps on the external side of GBM
evolution is usually favorable, with complete resolution and healing, with restitutio ad
integrum for 95% of children with APSGN
The most common (60-95% of the child AGN) and typical form of AGN
Etiology:
a). nephritogenic strains of group A beta-hemolytic streptococci: serotype 12 ( throat
infection (pharyngitis)) and serotype 49 (skin infection (impetigo) ).
Between streptococcal infection and apparent disease onset there is an asymptomatic latency
period (5-14 days), or more rarely with uncharacteristic symptoms (fatigue, low grade fever,
anorexia).
b). rarely- Group C streptococci, have been responsible for recent epidemics of APSGN (eg,
Streptococcus zooepidemicus).
Favoring factors:
a) age: childhood and adolescence, most common 5-15 years
b) sex: male predominance (male-to-female ratio 2:1)
c) cold and wet climate (autumn and winter)
d) in communities with densely populated dwellings that have poor hygienic conditions with
a high incidence of malnutrition, anemia, and intestinal parasites.
e) immunological status of the patient
Pathogenesis
Most forms of acute poststreptococcal glomerulonephritis (APSGN) are mediated by an
285
immunologic process. Cellular and humoral immunity is important in the pathogenesis of this
disease, and humoral immunity particularly in APSGN.
An immune complexmediated mechanism is the most widely proposed mechanism leading
to the development of APSGN. In most circumstances, glomerular inflammation begins with
an antigen-antibody reaction, either direct antibody binding to an antigen expressed or
trapped in the glomerulus, or the localization of a circulating complex in the kidney.
This incites injury by activating one or more systems of inflammatory mediators: the
complement cascade, coagulation factors, cytokines, growth factors, and others. The
inflammation is marked by proliferation of resident glomerular cells and infiltration by
lymphocytes or neutrophils.
Complement activation from both serum profiles and immunofluorescence patterns for
glomerular deposits indicates that C3 activation in APSGN is predominantly via the
alternative pathway. The immune deposits consist of immunoglobulin G (IgG), C3,
properdin, and C5.
Physiopathogeny
The glomerular inflammation and expansion impairs the microcirculation, reducing the
glomerular filtration rate (GFR) and usually resulting in an increase in BUN and creatinine.
This reduction in GFR, in turn, leads to the retention of salt and water, causing fluid overload.
The degree of fluid overload in AGN can vary considerably. In severe situations, it can be
manifest by life-threatening hypertension and pulmonary edema. Indeed, hypertensive
encephalopathy may be the presenting complaint in some children with AGN.
Streptococcal infection
+
Immune complex formation+ deposide in GBM
+
Complement system acivated low serum complement
+
Immune injuries
Cellular proliferation GBM fracture
+ +
Capillary lumen narrowed hematuria
286
+ proteinuria
Glomerular blood flow decreased
+
Oliguria : GFR+ distal Na reasorption
+
Retention of water and Na
+
Blood volume|
+
Edema
hypertension
Fig 2. Physipathology of APSGN
Clinical manifestation
The typical patient develops an acute nephritic syndrome 1-2 week after an antecedet
streptococcal pharyngitis or 3-6 week after a streptococcal pyoderma. Sometimes within the
physiacl exam we may detect angina or other streptococcal infections.
a. The onset may be:
- Acute onset after infection, with acute oliguria, edema, macroscopic hemtauria, HBP
- an insidious or slow (common) with: anorexia, asthenia, pallor, low back discomfort, eyelid
edema, tonsillitis, fever, headache, vomiting, abdominal pain, urine: proteinuria and
hematuria ( dysuria, pollakiuria)
- a dramatic (more rarely) by one of the acute complications: acute cerebral edema
(amaurosis, headache, vomiting, seizures, coma) or pulmonary edema.
- frequent atypical onset (diagnosis errors!)
Period of state: in typical forms is dominated by the 4 cardinal syndromes of the disease:
1. Syndrome of hydro-saline retention (edematous, hidropigen)
discrete/moderate edema soft, white, on the eyelids and face
More pronounced in the morning
Lead to weight gain
Sometimes noticed only in diuresis resumption weight
2. Urinary syndrome
287
oliguria < 300 ml/m
2
/24h
Macroscopic hematuria (meat wash)
laboratory
a. specific gravity normal or mild decreased (>1020)
b. Moderate nonselective proteinuria (0,5-1g/24h), later selective
c. glomerular hematuria (dysmorphic hematuria)
d. Erytrocite casts but also hialin or granulous casts
3. Hypertensive syndrome and cardiovascular overloading
The acute phase of the disease is characterized by frequent and sudden
changes in BP that requires frequent monitoring (every 4-6 hours). It is a sistolo-diastolic
HBP.
Signs of cardio-vascular overloading:
a.tachicardy, gallop rithm, cardiomegaly
b. Venous stasis (jugular turgescence, jugular pulsations, CVP )
c. hepatomegaly, hepatojugular reflux
d. Severe forms - mimic APE
4. Syndrome of nitrogen retention characterized by: urea > 40 mg%, uric acid
>4 mg%, creatinine > 1,2 mg%
Specific symptoms as malaise, lethargy, abdominal or flank pain, fever are common.
The acute phase generally resolves within 6-8 weeks.
Although urinary protein excretion and hypertension usually normalize by 4-6 weeks after the
onset, persistent microscopic hematurea may persist for 1-2 years after the initial
presentation.
Diagnosis:
1. urinalysis RBC , RBC casts, proteinuria, polymorphnuclear leukocytes.
2. There may be mild normochromic anemia due to hemodilution and low-grade
hemolysis.
3. C3 is usually in acute phase and return to normal level after 6-8 weeks.
4. The diagnosis is confirmed by the clear evidence of invasive streptococcal infections
:
a. positive throat culture may support diagnosis or represent carrier state.
b. A rising antibody titer to streptococcal antigens confirms a recent streptococcal
infection. These include :
288
ASO titer is commonly after pharyngeal infection but rarely after
streptococcal skin infection.
The best single antibody titer to document cutaneous infection is the
deoxyribo- nuclease (DNAase) B antigen.
The streptozyme test is alternative study which detects antibodies to
streptolysin O, DNAase B, hyaluronidase, & streptokinase using a slide
agglutination test.
5. increased ESR,
2
and globuline
6. urinary protein electrophoresis initially nonselective, in convalescence selective
proteinuria
7. The electrolyte profile is usually normal; hyperkalemia and metabolic acidosis are only
present in patients with significant renal functional impairment. The same applies to
hyperphosphatemia.
8. EKG: signs of overloading left ventricle
9. FO papillar edema, retinal vessels stasis
10. Circulating immune complexes (CIC)
11. ANCA, antinuclear antibodies, anti-DNA antibodies, anti-GBM antibodies, serology
for EBV and hepatitis B and C differential diagnosis
12. Renal biopsy should be considered :
a) In the early stages:
- Short latency period
- Severe anuria
- Rapid unfavorable outcome/ acute renal failure
- HBP > 2 weeks
- Low GFR > 2 weeks
- normal level of C3
- Absence of evidence of streptococcal infections, ASO- insignificant titre
- Non-renal manifestations
b) convalescence period:
- Low GFR > 4 weeks
- Hypocomplementemia > 12 weeks
- Persistent proteinuria > 6 months
- Persistent microscopic hematuria > 18 months
289
Positive diagnosis is sustained by clinical description and laboratory data .
1. There is no signs of systemic disease associated with typical cluster.
2. Evidence of streptococcal disease (positive throat culture or skin infection, evaluation of
antibody titers in both acute and convalescent).
3. Serum complement levels: C3 decreased in the acute phase, normal C4; C3 values return to
normal in 6-8 weeks.
4. Improvement of symptoms in the first week of illness: resumtion of diuresis, normalization
of BP, decreased nitrogen retention.
5. Normalization of urinary sediment: the disappearance of macroscopic hematuria in 2-3
weeks, 3-6 months disappearance of proteinuria, microscopic hematuria disappearance during
the first year.
Differential diagnosis:
-other causes of hematuria
1. GN during infection - intrainfectious onset, Alb-uria, Complementemia-N., no
edema, without HTA, renal function-N., self-limited disease
2. hemolitic-uremic syndrome hemorrhagic nephritis Renal failure
3. UTI bacteriuria and leucocyturia
4. Secondary GN -systemic diseases (SLE, PN)
5. Acute exarcebation of chronic glomerulonephritis- previous nephropathy, viral uppert
respiratory tract infection, anemia, azotemia from the onset, C level N/, renal biopsy
6. other hematuria (trauma, lithiasis, anticoagulant)
7. pielonephritis/viral hemorrhagic cystitis
8. nephritis from purpura Schonlein Henoch
9. nephrotic syndrome massive P-uria, monstrous edema , H-lipemia, hAlb.
10. AGN with CIC - non-streptococcal
11. Acute glomerulonephritis following other infections like staphylococci, streptococcus
pneumonia, Gram negative bacteria, bacterial endocarditis
Clinical course
Spontaneous improvement typically begins within 1 week with resolution of edema in 5-10
days and hypertension in 2-3 week, but urinalysis may be abnormal (persistent microscopic
hematuria) for 1-2 year after the initial presentation. Creatinine improves in 1 week and
become normal in 3-4 weeks, albuminuria may last a few months. C3 levels normalized in 6-
8 weeks.
290
Figure 2. Natural history of acute post-streptococcal glomerulonephritis
Complications:
Hypertension : seen in 60% of cases and may lead to hypertensive encephalopathy in
10%.
Acute renal dysfunction : hyperkalemia, hyperphosphatemia, hypocalcemia, acidosis,
seizure, uremia.
Heart failure.
Prevention
Early systemic antibiotic treatment for streptococcal throat and skin infection does not
eliminate the risk of glomerulonephritis.
Family members of the patient should be cultured for group A -hemolytic streptococci
and treated if culture is positive.
Treatment:
Treatment of APSGN is largely that of supportive care. Usually, patients undergo a
spontaneous diuresis within 7 to 10 days after the onset of their illness - strict monitoring
nephrotic chart + fluid restriction until dieresis is restored
Management is directed at treating the acute effects of renal insufficiency and hypertension.
General measures (Hygieno-dietetic treatment):
Bed rest: only indicated during the oliguric phase (1st week). Relative rest 2-4 weeks,
without violent physical activity for 1 year; then normal activity
Diet :
3-6 wks / 2wks
291
high carbohydrates diet to provide adequate calories, min. caloric 300-400kcal/m
2
/day
through oral or i.v. glucose solution
and low protein and salts during oliguric phase and with complications as severe
hypertension and marked vascular congestion
without NaCl, restriction of K
initially-proteins restriction; they will be introduced >7-10 days- vegetals
Fluid balance : During the oliguric phase, measurement of the daily urinary output is
important. The total daily fluid intake should be equal to the urinary output + insensible
water loss; liquid restrictions - 500ml/m
2
/day + diuresis of the previous day,
Specific measures :
a)etiologic: although a 10-day course of systemic antibiotic therapy with penicillin is
recomended to limit the spread of the nephrogenic organisms, antibiotic therapy does not
affect the natural history of glomerulonephritis.
Penicillin 50.000-100.000UI/Kgcorp/day, im, 4 doses, 10 days
Eryttromycin 30-50mg/kgbody/day po
Moldamin for prophilaxy 600 000 < 12 years, 1 200 000 > 12 years weekly p.la ext.
b). Control of hypertension : decrease Na+ intake, diuretics, Ca+2 channel antagonists,
vasodilators, & angiotensin converting enzyme inhibitors. [ captopril 0.5-1 mg/kg/day,
hydralazine 1-2 mg/kg/day, propronalol 1-2 mg/kg/day, the dose of each drug is divided 3-4
times ].
c). Control of edema: In most cases, edema subsides spontaneously at the end of 1st week and
with the onset of diuresis. Reduced fluid and salt intake during the 1st week is usually
important. In more severe cases, negativeve fluid balance is required. Diuretics as furocemide
may be used.
d). Treatment of complications :
1. Severe hypertension (hypertensive crisis) : Na+ nitroprusside infusion (0.5-10
microgram/kg/minute), Labetalol infusion (0.25-3 mg/kg/hour), Esmolol infusion
(150-300 microgram/kg/minute).
2. Heart failure.
3. Renal failure.
Antihypertensives are usually not necessary after the child leaves the hospital, although mild
hypertension may persist for as many as 6 weeks. The medications that can be used span the
entire range of antihypertensives, such as vasodilators (eg, hydralazine), calcium channel-
292
blocking agents (eg, long-acting nifedipine, amlodipine), or angiotensin-converting enzyme
(ACE) inhibitors (eg, enalapril).
Carefully monitor blood pressure (BP) for at least 1 week after the drug is discontinued to
ensure that rebound hypertension does not occur.
Long-term follow-up for a patient following acute poststreptococcal glomerulonephritis
(APSGN) primarily consists of blood pressure measurements and urine examinations for
protein and blood.
In general, examinations are performed at 4- to 6-week intervals for the first 6 months and at
3- to 6-month intervals thereafter, until both hematuria and proteinuria have been absent and
the blood pressure has been normal for 1 year. Documenting that the low C3 has returned to
normal after 8-10 weeks may be useful.
Prognosis
Fortunately, most cases of AGN in children are either self-limited or amenable to therapy
although there may be devastating complications of the illness during the acute phase. Less
commonly, what begins as an apparent AGN may presage the development of a chronic
process, which ultimately may progress into irreversible end-stage renal disease (ESRD).
APSGN excellent prognosis
Complete recovery occurs in > 95% of patients
Decission upon recovery assert after 1-2 years from the onset
5-10% - progressive evolution, persistent
Mortality rate in the acute phase can be avoided by appropriate treatment of acute
renal failure, heart failure, & hypertension.
Infrequently, the acute phase may be severe & may chronic renal insufficiency.
Recurrences are extremely rare.
NEPHROTIC SYNDROME (NS)
Nephrotic syndrome is primarily a pediatric disorder and is 15 times more common in
children than adults.
Definitions:
Nephrotic syndrome, or nephrosis, is defined by the presence of nephrotic-range proteinuria,
edema, hyperlipidemia, and hypoalbuminemia.
293
Nephrotic-range proteinuria in children is defined as protein excretion of more than 40
mg/m
2
/h or a first-morning urine protein/creatinine of 2-3 mg/mg creatinine or greater and
correlates with results from 24-hour urine collection.
Remission: marked reduction in proteinuria; urinary protein excretion < 4 mg/m
2
/hour or
urine dipstix nil/trace for 3 consecutive days.
Relapse: recurrence of massive proteinuria; urinary protein excretion > 40 mg/m
2
/hour or
urine dipstix ++ or more for 3 consecutive days.
Frequent relapses: Two or more relapses within 6 months of initial response or four or more
relapses within any 12 month period.
Steroid dependent NS: Two consecutive relapses occurring during the period of steroid
taper or within 14 days of its cessation.
Steroid sensitive NS: Normalization of proteinuria within 4 weeks after start of standard
initial therapy with daily oral predinisolone (patients who enter remission in response to
corticosteroid treatment alone)
Steroid resistance NS: Failure to achieve remission in spite of 6-8 weeks of standard
corticosteroid treatment.
The annual incidence of NS in most countries is estimated to range from 2-7 new cases per
100.000 children. There is a male preponderance among young children, at a ratio of 2:1 to
females.
Etiology:
Most children (90%) with NS have a form of idiopathic NS. Causes of idiopathic NS include
minimal change disease (85%), mesangial proliferation (5%), and focal segmental
glomerulosclerosis (FSGS) (10%). The remaining 10% of children with NS have secondary
NS related to systemic or glomerular disease such as membranous nephrotahy or
membranoproliferative glomerulonephrities.
Table 3. Causes of nephritic syndrome
Genetic Primary or Idiopathic - no
known aetiology
Secondary
Congenital NS
Infantile NS
Genetic
Minimal change disease
(MCD)
Focal Segmental
Systemic disease
- Systemic lupus erythematosus
(SLE)
294
syndromes
etc
Glomerulosclerosis (FSGS)
Membranous nephropathy
- Henoch-Scholein Purpura (HSP)
- Diabetes mellitus (DM)
Infections
- Post-infectious GN
- Hepatitis B, C; HIV
- Syphilis, Malaria, Toxoplasmosis
Drugs: D-penicilamin, gold,
mercury, heroin, nonsteroidal anti-
inflammatory, interferon, ACEIs, etc
Toxins and allergen food
allergens, bee sting
Associated with malignant
disease
- lymphoma, leukemia
Minimal Change Nephrotic Syndrome (MCNS)
- also known as: pure NS, lipoid nephrosis
In MCNS (85% of cases of NS in children), the glomeruli appear normal or show a minimal
increase in mesangial cells and matrix. Findings on immunofluorescence microscopy are
typically negative, and electron microscopy simply reveals effacement of the epithelial foot
processes. More than 95% of children with minimal change disease respond to corticosteroid
therapy.
It is called pure because are present elements that define the syndrome: proteinuria,
hypoalbuminemia, hyperlipemia, while hematuria, hyperazotemia and hypertension (the 3 H)
are absent (the 3 H are present in impure NS form).
Pathophysiology
The hallmark of INS is massive proteinuria, leading to decreased circulating albumin levels.
The initiating event that produces proteinuria remains unknown. However, strong evidence
suggests that INS, at least in part, has an immune pathogenesis.
The glomerular filtration barrier consists of the fenestrated capillary endothelium, the
extracellular basement membrane, and the intercalated podocyte foot processes, connected by
295
35-45 nm slit diaphragms. Nephrotic syndrome is associated with the biopsy finding of fusion
(effacement) of podocyte foot processes.
Figure 3. Epithelial cell injury and destruction of the basement membrane as a result of
immune complex in the glomerulus. (Kumar et al. Kidney and Its Collecting System in
Robbins Basic Pathology. 9th edition, Elsevier, 2012)
Normally, the basement cell membrane does not filter large molecules such as albumin
(70,000 kD), which is present in urine if the membrane is damaged.The underlying
abnormality in nephrotic syndrome is an increase in permeability of the glomerular capillary
wall, wich leads to massive proteinuria and hypoalbuminemia.
In MCNS it is possible that T-cell dysfunction leads to alteration of cytokines, which causes a
loss of negatively charged glycoproteins within the glomerular capillary wall.
In its normal state, the glomerular basement membrane is negatively charged because of the
presence of various polyanions along this surface, such as heparan sulfate, chondroitin
sulfate, and sialic acid. This negative charge acts as a deterrent to filtration of negatively
charged proteins, such as albumin. Children with MCNS have been reported to have
decreased anionic charges in the glomerular basement membrane.
In addition to the traditional immunological theories of INS pathogenesis, it has become clear
in recent years that INS is a podocytopathy. Podocytes also possess glucocorticoid receptors,
which can lead to stabilization of the podocyte cytoskeleton and inhibit apoptosis.
Cyclosporine, another important treatment for INS, can act directly on the podocyte by
inhibiting phosphorylation of the podocyte protein synaptopodin, which plays an important
role in the maintenance of the glomerular basement membrane.
296
In most instances, massive urinary protein loss leads to hypoalbuminemia, which cause a
decrease in the plasma oncotic pressure and transudation of fluid from the intravascular
compartment to the interstitial space, followed by intravascular volume depletion. The
reduction in intravascular volume decreases renal perfusion pressure, activating the RAAS,
which stimulates tubular reasorbtion of sodium and also stimulates the release of antidiuretic
hormone, which enhance the reasorbtion of watter in collectin duct.
INS is accompanied by disordered lipid metabolism. The traditional explanation for
hyperlipidemia in INS was the increased synthesis of lipoproteins that accompany increased
hepatic albumin synthesis due to hypoalbuminemia. Elevations in triglyceride levels occur
with severe hypoalbuminemia. Low and very low-density lipoproteins are responsible for the
transport of cholesterol and triglycerides. There is also an increase in the hepatic synthesis of
cholesterol.
Clinical manifestation
INS is more common in males than in females (2:1), and most commonly appears between
the ages of 2 and 6 years.
Puffiness around the eyes, characteristically in the morning.
Pitting edema over the legs.
Pitting edema is the presenting symptom in about 95% of children with nephrotic syndrome.
It is typically found in the lower extremities, face and periorbital regions, scrotum or labia,
and abdomen (ascites). Generalized edema throughout the body is known as anasarca.
The onset may be: sudden (more often) or insidious
Other signs and symptoms of nephrotic syndrome may include the following:
Respiratory tract infection - a history of a respiratory tract infection immediately
preceding the onset of nephrotic syndrome is frequent
Anorexia, irritability, abdominal pain, diarrhea- are common
Microscopic hematuria- in 23% of cases
Symptoms of infection - such as fever, lethargy, irritability, or abdominal pain due to
sepsis or peritonitis
Hypotension and signs of shock - can be present in children presenting with sepsis
Hypertension (rare)
Respiratory distress /Dyspnea- due to either massive ascites and thoracic compression or
frank pulmonary edema, effusions, or due to diaphragmatic compression with ascites.
Tachypnea - to compensate for mechanical restriction to breathing
Seizure - due to cerebral thrombosis
297
Hepatomegalia, umbilical herina, rectal prolaps
In time the signs of malnutrition will appear
When the following signs appear : hematuria, hypertension, hyperazotemia, we discuss about
nephritis-nephrosis and a kidney biopsy is recommended.
Differential diagnosis:
allergic edema
protein-losing enteropathy (urine and cholesterol - normal)
hepatic failure: chirrosis, hepatitis, etc; jaundice, dilated veins over umbilicus (caput
medusae), encephalopathy, etc, anomalies in the liver function tests
congestiv heart failure: cardiomegalia, murmurs, location and colour of edema
acute or chronic glomerulonephritis (APSGN, Membrano-prolipherative GN)
protein malnutrition
Pure NS/Impure NS
Secondary NS
Laboratory evaluation
The diagnosis of NS is confirmed by the triad of generalized edema, proteinuria, albuminuria
and hypoalbuminemia (serum albumin <2,5g/dl), although hypercholesterolemia is also
commonly present.
In order to establish the presence of nephrotic syndrome, laboratory tests should confirm the
existence of (1) nephrotic-range proteinuria, (2) hypoalbuminemia, and (3) hyperlipidemia.
- hypoproteinemia: < 6g% - Alb < 2,4g% (n:4g% ); seric protein electrophoresis:
disproteinemia, Alb and globulines; and glob.( lipoproteic fractions); a
decreased A/G ratio (a decreased A/G ratio, consider the following: Neoplasm,
infectious disease including AIDS, Intestinal disease, Liver disease, Renal disease,
The cachexic patient, CHF)
- erythrocyte sedimentation rate (ESR) is increased due to increased fibrinogen & other
plasma contents and because of disproteinemia, increased fibrinogen (n: 0,200 -
0,400g%) and no of platelets
- lipid profile: hyperlipemia > 1g and hypercholeterolemia > 250mg; specifically elevated
LDL, usually with concomitantly elevated VLDL
- ureea and creatinin may be increased in 1/3 of the cases (transient)
- immunogram: decreased plasmaIgG levels (secondary to urinary loss)
- plasma Ionogram: hypokalemia, Na ~ normal values
298
- URINE: froty, sometime opalescent aspect
- Nephrotic range proteinuria; proteinuria is "selective" for albumin (ie, > 85%
albumin)( tested by urine protein electrophoresis)
- Urine sediment examination: granular casts ; Viewed by polarizer, the oval fat bodies
and fatty casts cause a "Maltese cross" appearance
-Other tests: Complete blood count (CBC), Metabolic panel - levels of serum electrolytes,
calcium, phosphorus, and ionized calcium, as well as of blood urea nitrogen (BUN) and
creatinine ; Testing for HIV, hepatitis B and C; Complement studies (C3, C4), Antinuclear
antibody (ANA), antidouble-stranded DNA antibody (in selected patients), genetic tests.
Renal Biopsy
For childhood nephrotic syndrome, a renal biopsy is indicated for the following:
Congenital nephrotic syndrome
Children older than 8 years at onset
Steroid resistance
Frequent relapses or steroid dependency
Significant nephritic manifestations
Positive diagnosis: clinical manifestation and lab test
Complications of INS include:
Edema
Hyperlipidemia-atherosclerosis
Thrombosis- hypercoagulable state due to urinary losses of antithrombin,
thrombocytosis fibrinogen and number of platelets (renal vein thrombosis, deep
vein thrombosis, and pulmonary embolism are the most frequently encountered TEC
in children)
Infection (spontaneous bacterial peritonitis- the most coomon; sepsis, cellulitis)
Acute kidney failure (rare) due to hypovolemia
anemia and rickets are associated - transferin and ferritin; and the proteins which
binds Ca (calcium levels should be adjusted based on the albumin level and ionized
calcium levels should be checked)
Hypothyroidism: deficiency of the thyroglobulin transport protein thyroxin due to
decreased thyroid binding globulin.
Proetin malnutrition: this occurs when the amount of protein that is lost in the urine is
greater than that ingested, this leads to a negative nitrogen balance
299
Growth retardation: can occur in cases of relapse or resistance to therapy. Causes of
growth retardation are protein deficiency from the loss of protein in urine, anorexia
(reduced protein intake), and steroid therapy (catabolism).
Vitamin D deficiency can occur. Vitamin D binding protein is lost.
Cushing's Syndrome
Medication adverse effects (steroids, diuretics, albumin, steroid-sparing agents).
Treatment
1. Diet and activity
The diet in patients with nephrotic syndrome should provide adequate energy (caloric) intake
and adequate protein (1-2 g/kg/d). A diet with no added salt will help to limit fluid overload.
Fluid restriction per se is not required.
There are no activity restrictions for patients with nephrotic syndrome. Ongoing activity,
rather than bedrest, will reduce the risk of blood clots.
School attendance as soon as possible, also under corticotherapy or immunosupressors
2. Pathogenic treatment
The management of steroid-sensitive nephrotic syndrome in children aged 118 years
according to KDIGO:
- Initial treatment: Oral prednisone, starting as a daily dose of 60 mg/m
2
/day or 2
mg/kg/day (maximum, 60 mg/day) for 46 weeks. After 46 weeks, switch to 40
mg/m
2
or 1.5 mg/kg (maximum, 40 mg) on alternate days for 25 months with
tapering, with a minimum total duration of treatment of 12 weeks.
- Treatment of infrequent relapse (1 relapse in 6 months or 13 relapses in 12 months):
Administer initial treatment dose (60 mg/m
2
/day or 2 mg/kg/day) until urinary protein
is negative for 3 days. After urine is negative for protein for 3 days, change
prednisone to 40 mg/m
2
or 1.5 mg/kg (maximum, 40 mg) on alternate days for 4
weeks, then stop or taper dose.
- Treatment of frequent relapse (2 relapses in 6 months or 4 relapses in 12 months):
Continue infrequent relapse treatment for 3 months at lowest dose to maintain
remission or use corticosteroid-sparing agents, including alkylating agents,
levamisole, calcineurin inhibitors, mycophenolate mofetil.
- immunosuppressive medication, other than steroid and immunomodulators are
indicated in:
o corticoresistant NS
o Side effects to corticosteroid treatment
300
o Frequent relapses
3. Simptomatic treatment
- For edema: diuretics are needed. Furosemide (1 mg/kg/d) and spironolactone (2
mg/kg/d) will help when fluid retention is severe, provided no signs of renal failure or
volume contraction are evident.
- achieving a satisfactory diuresis is difficult when the patient's serum albumin level is
less than 1.5 g/dL. Albumin in a dose of 1 g/kg may be given, followed by
intravenous furosemide.
- Hyperlipidemia- lipid-lowering agents: It is administrated for the consequences upon
the cord and vessels(hyperlipemia accelerates the glomerulosclerosis)
- In case of infection: antibiotherapy, and not for rutine
- in preventing thromboembolic complications: An antiplatelet drug (antiaggregant)
- angiotensin-converting enzyme (ACE) inhibitors and/or angiotensin II receptor
blockers. These may reduce proteinuria by reducing the systemic blood pressure, by
reducing intraglomerular pressure, and also by direct action on podocytes.
- Supplemental calcium and vitamin D may attenuate bone loss.
- Painful abdominal crisis:
- Corect the hidroelectrolyte imbalances
- Maybe paracentesis
- Severe renal insufficiency - unusual needs peritoneal dialysis, hemodialysis
Long-term follow-up
Follow-up care in patients with nephrotic syndrome includes immunization, treatment of
relapses of steroid-responsive nephrotic syndromes, monitoring for steroid toxicity, and
monitoring of diuretic and angiotensin antagonist regimens.
Routine immunizations should be delayed until the patient is free of relapses and has been off
immunosuppression for 3-6 months.
Transmissible diseases and vaccins - special problems: *measles or chickenpox specific
immunoglobulines
*vaccination antipolio and BCG only after remission, imediately after corticotherapy, at 6
months after imunosupressors
Monitoring for steroid toxicity every 3 months in the outpatient clinic is necessary to help
detect adverse effects and to record growth in children.
A yearly checkup is necessary to help detect cataracts.
Prognosis
301
Pediatric nephrotic syndrome is a chronic illness characterized by relapses and remissions,
which can extend throughout childhood.
Evolution is good in those who had a good response to initial corticotherapy (> 90% of the
cases)
The prognosis for patients with minimal-change nephropathy is good.
Most children respond to steroid therapy; still, about 50% of children have 1 or 2 relapses
within 5 years and approximately 20% of them continue to relapse 10 years after diagnosis.
Only 25-30% of children never have a relapse after the initial episode. Approximately 5% of
patients who initially respond to steroids become steroid-resistant.
Recurrences can not be prevented.
In some cases- relapses at > 5 -10 years from the apparent recovery
Fig 4. NS prognosis
302
Fig5. Proposed algorithm for SRNS treatment (expert meeting, Londra 2005)
ACUTE KIDNEY INJURY (AKI)
Acute kidney injury (AKI) (previously called acute renal failure), is defined as an abrupt or
rapid decline in renal filtration function. This condition is usually marked by a rise in serum
creatinine concentration or by azotemia (a rise in blood urea nitrogen [BUN] concentration).
AKI is a clinical and biological syndrome that result to the sudden decrease in renal function,
impaired renal function, ruling out normal clearout substances such as blood urea, creatinine,
potassium, and on the other hand uremia and electrolyte disorders causing numerous
symptoms such as pulmonary edema, hypervolemia, hypertension, heart failure, cardiac
arrhythmias, pericarditis, lethargy, vomiting, seizures, coma, etc..
AKI may be classified into 3 general categories, as follows:
Prerenal - As an adaptive response to severe volume depletion and hypotension, with
structurally intact nephrons
SRNS - FSGS
Gene testing Rule out other undelying diseses
leading to FSGS
Positive for mutation in
podocin, WT
1
, CD
2
AP,
TRPC
6
,etc
Not done/ not available
nedisponibil /Negative
Careful watching,
antiproteinuric treatment
with ACE-inhibitors,
angiotensin receptor
blocker
kidney transplantation
Trial with Cyclosporin +
concomitant Prednison
for at least 6 months
No respons
Respons
Continue cyclosporine as
lang-term treatment
(years)
303
Intrinsic - In response to cytotoxic, ischemic, or inflammatory insults to the kidney,
with structural and functional damage (acute tubular necrosis, glomerulonephritis, APSGN,
HUS, renal artery/vein trombosis, drugs, etc)
Postrenal - From obstruction to the passage of urine (ureteric obstruction, urethral
obstruction, etc)
Clinic:
- decrease circulating volume (pallor, pulse, BP, neurological, etc.)
- state of hydration (dehydration, hyperhydration)
- assessment of vital signs (tachypnea, hypo / hypertension, tachycardia)
- neurological assessment mandatory
- Fever, rash, petechiae, purpura, ecchymosis, abdominal collections, pleural effusion,
pericardial
- lower/upper gastrointestinal bleading
Lab tests
Complete blood count (CBC), peripheral smear,
Serum biochemistries: urea, creatinine, uric acid, ASTRUP, electolytes, blood
glucose, cystatin C, amylase, lipase, creatinine clearance
Urine output, specific gravity, Urine analysis with microscopy, urine sediment, Urine
electrolytes
Immunology: Complement levels, Antinuclear antibody (ANA), Antineutrophil
cytoplasmic antibody (ANCA), Anti-glomerular basement membrane (anti-GBM) antibody,
Hepatitis B and C virus studies, Antistreptolysin (ASO)
Imaging studies: chest x-ray, abdominal ultrasound, nuclear scanning:
99m
Tc-
diethylenetriamine penta-acetic acid (
99m
Tc-DTPA), angiography, NO i.v urography
Diagnosis:
- oliguria (<0.5 ml / kg / hr or 500 ml / 1.73m2/day)
- increased serum creatinine
- decreased creatinine clearance
Complications:
- Common (acute pulmonary edema, congestive heart failure, uremic pericarditis,
hypertension + acute cerebral edema, coma, convulsions, lower/upper gastrointestinal
bleading, polyuria, hyperkalemia, Hypo/ hyper phosphatemia, hypoCalcemia, decompensated
metabolic acidosis, infection, death)
304
- MSOF (respiratory failure, heart failure, liver failure, pancreatitis,uremic pericarditis,
uremic coma)
Treatment:
- the current treatment for AKI is mainly supportive
- Maintenance of volume homeostasis and correction of biochemical abnormalities remain
the primary goals of treatment
-Dietary changes are an important facet of AKI treatment. Restriction of salt and fluid
becomes crucial in the management of oliguric renal failure. K and Ph: restriction or dietary
supplementation and IV replacement
- sometime - renal replacement therapy, dialysis-required in approx 20% of cases of AKI
Prognosis
The prognosis of AKI is highly dependent on the underlying etiology of the AKI.
CHRONIC KIDNEY DISEASE (CKD)
Chronic kidney disease is characterized by an irreversible deterioration of renal function that
gradually progresses to end-stage renal disease (ESRD).
CKD is a clinical syndrome with multiple etiology, with a slow onset; pathophysiology
characterized by the inability of the kidneys to ensure normal function due to organ damage,
bilateral or located at a single kidney in conditions of unique congenital or surgical kidney,
with irreversible changes by death in years.
It is characterized by a decreased glomerular filtration rate (GFR), as defined by a GFR of
less than 75 mL/min per 1.73 m
2
Etiology
Obstructive uropathy, Hypoplastic or dysplastic kidneys, Reflux nephropathy
Focal segmental glomerulosclerosis as a variant of childhood nephritic syndrome
Polycystic kidney disease,
Secondary GN,
Vascular nephropaties (HUS, HBP, DM, renal vein trombosis, etc)
The frequency of chronic kidney disease increases with age and is much more common in
adults than children. Among children, chronic kidney disease is more common in children
older than 6 years than in those younger than 6 years.
Once chronic kidney disease (CKD) occurs, progression to end-stage renal disease (ESRD)
appears certain.
305
Children with chronic kidney disease and their families should receive education about the
importance of compliance with secondary preventative measures, natural disease progression,
prescribed medications (highlighting their potential benefits and adverse effects), diet, and
types of long-term renal replacement modalities.
Clinical manifestation
Unexplained anemia or short stature is sometimes the only presentation in a child with
chronic kidney disease (CKD). A high index of suspicion is required for early diagnosis.
Chronic kidney disease (CKD) is asymptomatic in its earliest stages (stage I and stage II),
although urinalysis findings or blood pressure may be abnormal. As chronic kidney disease
progresses to more advanced stages, signs and symptoms greatly increase. Signs of acute
disease may appear in the context of intercurrent infections or acute dehydration syndrome .
1. Growth failure: occurs in 50 % of cases of CKD and is particularly serious if renal failure
is installed before the age of 2 years.
2 . Chronic anemia. Anemia that not respond to treatment with preparations containing iron
may indicate a chronic anemia
- .Urinary : polyuria / polydipsia , oliguria / anuria , enuresis, UTI, stones
- Gastroenterology- nausea, vomiting , stomatitis , gingivitis , gastritis,
colitis, anorexia: uremia , pancreatic insufficiency, pain , hepatitis B , C
- Respiratory system : uremic lung, acute lung disease, pleural efusions
- Cardio-vascular: hypertension, infectious and / or uremic pericarditis, uremic /
metabolic cardiomyopathy, cardiac arrhythmias, heart failure,LVH, APE,
atherosclerosis
- Neurological: poor school performance, unexplained headache, uremic
encephalopathy , somnolence, dizziness, seizure, uremic coma, ACE, ICH, stroke,
hypertensive encephalopathy
- Hematologic: normochromic - normocytic anemia , thrombocytopenia /
thrombasthenia ,
moderate leukocytosis, etc
- Neuropathy : asterixis, paresthesia, restless legs, muscle syndrome, carpal Tunnel
- Metabolic: fluid overload / dehydration, malnutrition, hyperlipoproteinemia ,
carbohydrates intolerance, hypothermia
- Other events: endocrine, dermatological, ocular, musclular.
306
Clinical and biological assessment:
BP measurement- use an appropriate cuff for (age, arm size)
Biochemical: complete blood cell (CBC) , urea, serum creatinine, serum sodium,
potassium, calcium, phosphorus, bicarbonate, alkaline phosphatase, parathyroid hormone
(PTH), and cholesterol and fractionated lipid levels, renal osteodystrophia -
hyperparathyroidism (Ca, P, Ca x P, hypocalcemia, PTH , APh), endocrine
dysfunction,etc
Urine: specific gravity (urine-concentrating capacity). Urine microscopy (red blood
cells (RBCs), white blood cells (WBCs), and casts), proteinuria and albuminuria analysis,
cystatin C- the plasma cystatin C concentration may correlate more closely with the GFR
than with the PCr, urinary electolytes
Imaging studies such as ultrasonography and radionuclide studie, x-ray (bone,
heart,lung), i.v.Urography /VCUG, renal tomography
kidney biopsy
Diagnosis based on plasma creatinine concentration (PCr), proteinuria, blood pressure, GFR,
urinary sediment, renal ultrasound
Differential Diagnoses
Acute Renal Failure
Chronic Glomerulonephritis
Diabetic Nephropathy
Nephrosclerosis
Rapidly Progressive Glomerulonephritis
Treatment of chronic kidney disease should include the following:
Specific therapy based on diagnosis
Evaluation and management of reversible causes of renal dysfunction
Prevention and treatment of complications of decreased kidney function (eg, anemia,
bone disease, cardiovascular manifestations, hypertension, growth failure)
Evaluation and management of comorbid conditions
Slowing the loss of kidney function
Preparation for kidney failure therapy
Replacement of kidney function with dialysis and transplantation if signs and
symptoms of uremia are present
Management of complications
307
Prognosis
About 70% of children with chronic kidney disease develop ESRD by age 20 years.
Children with ESRD have a 10-year survival rate of about 80% and an age-specific mortality
rate of about 30 times that seen in children without ESRD.
The most common cause of death in these children is cardiovascular disease, followed by
infection.
References:
2. Blgrdean Mihaela. Rinichiul n patologia copilului. Vol 1. Ed Universitar Carol davila, Bucureti 2011
3. Coman I., Stanca DV., Miu N., Bizo A. Infeciile de tract urinar la copil. Abordare nefro-urologic. Ed
Medical Universitar Iuliu Haieganu Cluj-Napoca 2003
4. Elie V, Fakhoury M, Deschnes G, Jacqz-Aigrain E. Physiopathology of idiopathic nephrotic syndrome:
lessons from glucocorticoids and epigenetic perspectives. Pediatr Nephrol. Aug 2012; 27(8):1249-56.
5. Gbadegesin R, Smoyer W.E. Nephrotic syndrome in Comprehensive Pediatric Nephrology, Ed Mosby
Elsevier 2008, 205-218
6. KDIGO CLINICAL PRACTICE GUIDELINE FOR GLOMERULONEPHRITIS 2011
7. Lombel RM, Gipson DS, Hodson EM. Treatment of steroid-sensitive nephrotic syndrome: new guidelines
from KDIGO. Pediatr Nephrol. Mar 2013; 28(3):415-26
8. Man Sorin C, Nanulescu Mircea V. Pediatrie Practic, Risoprint Cluj-Napoca, 2006, 311-316
9. Nanulescu Mircea. Aparatul reno-urinar n Protocoale de diagnostic i tratament n pediatrie. Ed medical
Amaltea 2012, 108-119
10. Davis ID, Avner ED. Nephrology In Nelson. Textbook of pediatrics. Ed Saunders Elsevier, 18th edition
2007, 2163-2219
11. Niuadet Patrick. Nephritic syndrome in Comprehensive Pediatric Nephrology, Ed Mosby Elsevier 2008,
195-204
12. Schrier RW, Wang W, Poole B, Mitra A. Acute renal failure: definitions, diagnosis, pathogenesis, and
therapy. J Clin Invest. Jul 2004; 114(1):5-14.
13. Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and
Management.Urinary Tract Infection: Clinical Practice Guideline for the Diagnosis and Management of the
Initial UTI in Febrile Infants and Children 2 to 24 Months. Pediatrics Vol. 128 No. 3 September 1, 2011 pp.
595 -610 (doi: 10.1542/peds.2011-1330)
14. Tryggvason K, Patrakka J, Wartiovaara J. Hereditary proteinuria syndromes and mechanisms of proteinuria.
N Engl J Med. Mar 30 2006; 354(13):1387-401.
15. Welch Thomas R. An Approach to the Child with Acute Glomerulonephritis. International Journal of
Pediatrics Volume 2012, Article ID 426192, 3 pages, doi:10.1155/2012/426192
16. White Brett. Diagnosis and Treatment of Urinary Tract Infections in Children.Am Fam Physician. 2011
Feb;83(4):409-415.
308
CHAPTER VIII CENTRAL NERVOUS SYSTEM DISEASES
Conf. Univ. Dr. Mrginean Oana, Asist. Univ. Dr. Grama Alina
MENINGITIS
Definition: Meningitis is an inflammatory disease of the protective membrane that covers the
brain and spinal cord, known collectively as the meninges. The inflammation can be caused
by infection with viruses, bacteria or other microorganisms, and less commonly by non-
infectious agents. Meningitis can be life-threatening because of the proximity of the
inflammation to the brain and spinal cord; therefore, the condition is classified as a medical
emergency.
Meningean syndrome = all clinical manifestations due to meninges damage.
The etiology varies according to age:
Age Etiology of bacterial meningitis
0-1 month Streptococcus agalactiae (streptococul betahemolitic group B)
Escherichia coli
Other Enterobacteriaceae
Listeria monocytogenes
1-3 months Streptococcus agalactiae
Streptococcus pneumoniae
Haemophilus influenzae
Listeria monocytogenes
3months-5 years Haemophilus influenzae
Neisseria meningitidis
Streptococcus pneumoniae
> 5years Streptococcus pneumoniae
Neisseria meningitidis
Staphylococus aureus
Streptococi
Haemophilus influenzae (rarely)
309
Other causative pathogenic agents (chlamydia, mycoplasmas, protozoa, fungi) occur
especially in patients with a history of compromised biological background, with poor
immunological mechanisms.
Contributing factors :
- anatomical abnormalities and surgical procedures (post-neurosurgery)
- inflammatory diseases of the cephalic extremity (mastoiditis, pansinusitis)
- endocranial lesions with CSF circulation disorders (brain abscess, subdural empyema,
hydrocephalus)
- neurological trauma and skull base fracture
- various immunodeficiency syndromes (asplenia, hypogammaglobulinemia,
myeloproliferative diseases, immunosuppressive, rheumatic diseases)
Physiopathology :
Microorganisms can reach the central nervous system in three ways:
- through the bloodstream - from a primary infection outbreak
- contiguous from a parameningian infectious outbreak (sinus, otic, dental)
- direct sowing of CSF by cranio-cerebral injury and rarely iatrogenic.
In newborns, the infection occurs due to "harvesting" the germ from the mother during birth.
In infants, who are susceptible to infection with Gram-negative enteric bacteria, the large
intestine is the pathogen source. Colonization of the nasopharynx is the starting point for
meningitis in older children. In meningitis pathogeny, increased intracranial pressure,
cerebral edema, and increased volume of CSF occur:
Diagnosis algorithm:
A. History :
Prodromal signs, changing the general condition, headache, nausea, vomiting, agitation,
seizures, and fever are crucial signs. In newborns, attention may be drawn by an abnormal
sleepiness or irritability, shrill screams, toxic state.
B. Clinical evaluation :
The clinical features of bacterial meningitis vary with age, etiology, predisposing factors,
disease duration prior to making clinical examinations and individual response to infection.
(table XX)
Table XX Clinical features of bacterial meningitis
Age Symptoms and signs Bear in mind
310
newborn Malaise
Apnea, respiratory distress
Hypotonia, short scream
Vomiting, diarrhea, jaundice, flatulence
Hypothermia / hyperthermia
Shock
Petechiae, purpura, pustules
Anterior fontanelle sometimes bulges -
usually late sign
Rarely present, even if the
infection is severe:
Neck stiffness
Kernig sign
Brudzinski sign
infant, child Symptoms of meningeal irritation :
- Neck stiffness
- Kernig sign (when bending the trunk,
bends the knees)
- Brudzinski sign (when bending the
head bends the knees)
Fever
Seizures (more common in infants,
usually generalized)
Cutaneous hyperesthesia, reducing
ROT, paresis / paralysis
Increased intracranial pressure :
bulging fontanelle, bradycardia,
headache, vomiting, photophobia
Encephalitic symptoms: drowsiness,
agitation, coma (meningoencephalitis)
Manifestations from other organs :
diarrhea, purpura, etc.
Signs and symptoms of
meningitis under 18 months
are not specific despite the
disease severity!!!
In older children, the
symptoms are clearer from
the onset: symptoms of
meningean irritation,
headache, photophobia,
vomiting, "gun cock"
position
C. Paraclinical examinations
1. Confirmation of the diagnosis of meningitis is based on CSF examination (table...), for
which lumbar puncture should be performed in all patients who are suspected of meningitis;
it is contraindicated in certain situations (table. Xx)
311
a. Gram staining is a simple and rapid diagnosis method of bacterial meningitis. Although it
has an 80% sensitivity, its advantage is the rapid performance.
b. Other tests of CSF that can make the difference between a viral and a bacterial
meningitis, include determination of endotoxin, C-reactive protein, fibronectin, and
lactate concentration. Tests for the determination of antigens are expensive and are not
routinely used.
312
Table...Interpretation of CSF results in meningitis (infants and children)
Normal Bacterial Viral Tuberculosis
Bacterial partially
treated
Macroscopic Clear Turbid Opalescent/clear Clear Variable
Cytorahia
(cells/mm
3
)
5
100-60000
(usually >1000)
10-1000
(usually < 300)
< 1000
(usually 50-100)
1-10000
(usually 200-5000)
Predominant
Cells
Mononuclear
(1PMN/mm
3
)
PMN >50%
Initially PMN, then
mononuclear
Initially PMN, then lymphocytes
PMN or
mononuclear
Proteinorahia
(mg/dl)
< 40
(usually 100-500)
N/
(usually 40-200)
(usually 100-500)
(usually >100)
Glycorahia
(% of Glycemia)
> 60 N /N /N
Gram Smear Negative Usually positive Negative
Negative (Ziehl-Nielsen smear can
be positive)
Can be negative
Bacterial
cultures
Sterile Usually positive Sterile
Sterile (M.tuberculosis cultures
can be positive)
Can be sterile
* in newborns normal values are: cytorahia 30; predominant cells 40% PMN; proteinorahia < 170; glycorahia > 50
313
314
Table XX Indications and contraindications of lumbar puncture
Indications :
Bacteremia in newborns
Septicemia (especially in infants)
Seizures associated with fever and age <18 months
Complex febrile seizures
Children with fever associated with lethargy, hypotonia, irritability, decreased
appetite, vomiting, shock, dehydration, without satisfactory explanation
Classic manifestations of meningitis: fever, headache, stiff neck
Coma or neurological changes without explanation
Skin lesions of meningococcemia
Facial cellulitis in small children or cellulitis regardless of location in infants
Absolute contraindications
Poor cardiorespiratory status
Significant intracranial hypertension
Brain abscess, subdural empyema
Relative contraindications
Severe coagulopathy
Thrombocytopenia (<50.000/mm3)
Malformation of the lumbar spine or spinal cord
Skin infection at the puncture site
2. Other examinations :
- Blood count, differential leucocyte count, platelet
- ESR, PCR
- Ionogram (Na, K, Ca, Ph)
- Urea, creatinine
- Transaminases
- Exploration of hemostasis: APTT, Quick time, degradation of fibrinogen / fibrin
- Determination of blood gases (acid-base balance)
- Fasting plasma glucose (FPG) important compared to glicorahia
- Serum protein electrophoresis, immunogram
- Urine examination
315
- Cultures of blood, urine, stool, purpuric lesions, abscesses, secretory otitis, pharynx
- Eye fundus, sinus Rx, mastoids, lung Rx
- transfontanellar ultrasound in infants
- EEG shows diffuse involvement of the brain, but it does not help in locating the cause of
injury
- CT or MRI are indicated to diagnose the cause of outbreak signs
- interdisciplinary consultation - neurology, infectious diseases
Differential diagnosis:
1. Meningism there are signs of meningeal irritation (neck stiffness frequently) and
increased CSF pressure, but no other changes in CSF appear; in infections located outside the
CNS infections (flu, pneumonia, scarlet fever, dysentery) and subarachnoid hemorrhage
2. Meningeal reaction - where there is a meningeal clinical syndrome and mild changes
in CSF: increased cytology (40-50 elem/mm3), slight increase in the CSF albumins, the
presence of red blood cells; no germs of the disease in the CSF, element of differential
diagnosis with a real meningitis.
3. Other causes of neck stiffness:
- Cervical lymphadenitis
- Retrofaringean abscess
- Intracranial hemorrhage or tumor
- Cervical Trauma
- Juvenile Idiopathic Arthritis
- Spinal Abnormalities
- Torticolis
- Tetanus
4. Other causes of headache and vomiting: sunstroke
5. Medulloblastoma and leukemic infiltration, where glycorahia is low
Treatment :
I. Hygienic-dietary and electrolytic treatment :
- Food po if the sensors are clear; absolute digestive rest if the patient vomits, has seizures
or altered sensors (risk of aspiration);
- In case of dehydration, deficit recovery will be made with isotonic fluids; for maintenance
needs, hypotonic fluids are administered evenly over 24 hours (1500ml/m2/day);
316
- in case of sepsis, Waterhouse-Friederichson syndrome - dehydration and shock treatment
is installed, with volume-expanders (crystalloid / colloid), if necessary with hemodynamic
monitoring.
II. Antibiotic treatment: empirical treatment of meningitis must take into account the most
common etiology for age and possible resistance to the incriminated microorganism
Table XX Types of recommended antibiotic therapy for bacterial meningitis
Type of bacteria Antibiotic to be chosen
Duration of
treatment
Gram colouring
Coci
Gram positive
Gram negative
Vancomicin + CFS large spectrum
(cefotaxime/ceftriaxone)
Penicilin G
Bacili
Gram positive
Gram negative
Ampicilin + AMG (Gentamicin)
CFS large spectrum
On cultures
S. pneumoniae
Penicilin G or Vancomicina, Meropenem
+ CFS large spectrum (ceftriaxone)
10-14 days
Streptococ agalactiae
Penicilin G + Gentamicin
or Ampicilina + Gentamicin
14-21 days (in
newborns)
H. influenzae Ceftriaxone/ Cefotaxime 10-14 days
N. meningitidis Penicilin G 7-10 days
L. monocytogenes Ampicilin + Gentamicin 14-21 days
Enterobacteriaceae
CFS large spectrum (cefotaxime/
ceftriaxone) + Gentamicin
21 days
Pseudomonas aeruginosa,
Acinetobacter
Ceftazidime + AMG (Gentamicin) 21 days
!!! Treatment duration should be individualized according to the clinical and microbiological
response
317
Table ... Antibiotic posology in bacterial meningitis
*
Antibiotic Newborn Infants and children
0-7 days 8-28 days
Ampicilin 100-150 (3) 150-200 (4) 200-300 (4)
Cefotaxim 100-150 (2) 150-200 (3-4) 200 (4)
Ceftriaxon Is avoided Is avoided 80-100 (2)
Ceftazidim 60 (2) 90 (3) 125-150 (3)
Gentamicin 5 (2) 7,5 (3) 7,5 (3)
Amikacin 15-20 (2) 20-30 (3) 20-30 (3)
Penicilin G 150 000 UI (3) 200 000 UI (4) 300 000 UI (4-6)
Vancomicin
**
20-30 (2-3) 30-40 (3) 40 (4)
Meropenem 60-120 (3)
*
the dose is expressed in mg/kb/day, and for Penicilin G in UI/kg/day (the no of doses/day in
brackets)
**
administered in 1 hour EVP
III. Treatment of complications and neurologic manifestations :
Medical treatment of intracranial hypertension :
- hyperventilation - effects of cerebral vasoconstriction cuased by hypocapnia lead to
decreased cerebral blood flow and intracranial hypertension decrease
- hypertonic solution (Mannitol) is usually effective in reducing intracranial
hypertension
- Treatment of seizures :
- Diazepam 0.2 to 05 mg / kg / dose intravenously which can be repeated every 15
minutes
- Phenobarbital 15-20 mg / kg / dose endotracheal intubation
- metabolic imbalances should be found and treated!
IV. Dexametazone
absolute indication in H. influenzae meningitis, is adminstered in a dose of 0.15 mg /
kg body / dose iv every 6 hours for 4 days
relative indication in children over 6 weeks with meningococcal or pneumococcal
bacterial meningitis
V. Imunotherapy : in some forms of meningitis (Streptococcus agalactiae in neonates) iv
immunoglobulin can be administered
VI. Monitorization :
318
A. Acute phase:
1. Vital Signs: heart rate, respiratory frequency, blood pressure, hydration status, weight
2. Neurological signs: pupillary reflexes, sensors, muscle strength, cranial nerves, cranial
perimeter measurement (infants 1x/day) every 4 h during the first 72 hours, afterwards
1x/day
3. Laboratory: Hb, leukocytes, platelets, serum ionogram, fibrinogen, APTT, Quick T,
creatinine, urine summary
4. lumbar puncture
- Indications of repetition: in newborns with no response or poor response after 48-72
hours of treatment
- CSF signs of improvement: emergence of mononuclei, glycorahia growth, Gram
smear shows no germs, sterile culture
B. Afterwards :
1. audiological evaluation 1 month after discharge
2. psychological assessment
3. neurologic rating
VII. Prophylaxy :
Chemical prophylaxy
of contacts
Inclusion criteria Regimen
Hemofilus influenzae
- Family members (if there is
at least one child < 4 years
in the family)
- groups (nursery,
kindergarten)
- supervising personnel (if in
the community 2 cases
occurred within 2 months)
Rifampicina po : 20
mg/kg/day (max 600
mg/day), in single dose
4 days
Neiseria meningitidis
- Family members
- Contacts in groups
- Persons who come into
contact with oral secretions
of the case
Rifampicina po : 20
mg/kg/day (max 600
mg/day), in 2 doses, 2 days
or
Ceftriaxon im :
125 mg in children < 12
319
years
250 mg in children > 12
years, adults, single dose
Complications :
A. Acute
1. Neurologic
- Convulsions - Paralysis of cranial nerves
- Cerebral hernia - Loculation of the meningeal suppurative process
- Subdural empyema - Subdural effusion (up to 50%)
- Cerebral abscess - Cortical vein or cortical venous sinuses thrombosis
- SIADH (syndrom of inappropriate antidiuretic hormone secretion)
2. Systemic
- Apnea Disseminated Intravascular Coagulation
- Toxi-infectious shock Hypoglycemia
- Pneumonia, endocarditis, pericarditis, septic arthritis
B. Chronic (seqelae)
1. Mental retardation
2. Convulsion
3. Delayed speech
4. Hearing loss
5. Visual disturbances
6. Behavioral disorders
7. Motor deficits
8. Hydrocephalus
9. Central diabetes insipidus
Prognosis The reserved prognosis factors:
- age < 6 months - poor nutritional status
- late sterilization of CSF - over 10
6
bacterial colonies / ml CSF
- glycorahia < 20 mg/dl - coma
- SIADH - signs of outbreak on hospital admission
- delayed / inadequate antibiotic therapy - cerebral infarction
- toxic and septic shock - disseminated intravascular coagulation
- E. coli or Pseudomonas aeruginosa meningitis
320
- recurrent seizures lasting > 4 days after therapy initiation
ACUTE ENCEPHALITIS
Definition: Encephalitis is an acute inflammation of the CNS caused by multiple etiological
agents, (particularly viruses) and different pathogenic mechanisms, characterized clinically
by an infectious syndrome associated with neuropsychic pain, sometimes with self-limited
evolution, but generally unpredictable.
Etiology:
1. Viral encephalitis - are the most common and important encephalitises:
a) Primary: with identified virus (arboviruses, rubella virus, influenza and parainfluenza,
mumps v., rabies v.) or unidentified virus;
b) Secondary:
- to general viral diseases (measles, influenza, chickenpox, infectious mononucleosis,
adenoviruses)
- post-vaccination (BCG vaccination, measles, polio, smallpox)
2. Non-viral encephalitis caused by rickettsiae, Mycoplasma pneumoniae, bacteria: TB,
spirochete: syphilis, listeriasis, protosoa: Toxoplasma gondii, fungi, echinococcosis,
cysticercosis
Positive diagnosis :
1. History - plays an important role in specifying encephalitis diagnosis and frequently it
can orient towards its etiology.
a. Presence of acute viral infections like: measles, rubella, varicella or anti-rabies, anti-
measles vaccination in the recent history can guide to the diagnosis of postinfection
encephalitis;
b. The presence of other cases of encephalitis with epidemic aspect in the patients region
has special value for primitive viral encephalitis.
2. Clinical features :
The incubation period ranges 7 days up to 2-3 weeks
usually sudden onset with high fever, impaired general condition, headache, chills,
nausea; in infants: unexplained crying, colicky abdominal pain, vomiting
There are signs of general infection
Further disease progresses with intense headache, irritability, anorexia, vomiting,
indicating cerebral edema
321
Signs of encephalus impairment: mental disorders - obnubilation, disorientation,
slurred speech, hallucinations, encephalitic cry, psychomotor agitation or drowsiness,
coma of varying degrees
Signs cerebral trunk impairment: cranial nerve palsies, hemiplegia, bulbar paralytic
syndromes with swallowing and respiratory disorders
Meningeal signs: positive Babinski sign, neck stiffness, changes in tendon reflexes
Characteristic: Very short intervals variability of symptoms and progressive
enlargement of cerebral edema with impaired brain functions in different areas
3. Paraclinical examinations
- Haematological exploration does not bring useful information, blood count is usually
normal, and acute phase reactants are missing
- Eye fundus examination to exclude intracranial hypertension syndrome
- Lumbar puncture with CSF examination
- clear CSF, hypertensive
- slightly elevated albuminorahia and glycorahia
- tens-hundreds of elements/mm3 pleocytosis (with predominance of lymphocytes)
- bacteriological examination for possible bacterial etiology
- tissue culture seeding for a possible viral etiology (expensive)
- serological determinations for early identification of viral and bacterial antigens
(by immunofluorescence), as well as dosage of specific Atb.
- viral cultures of CSF, throat swab, stool, and research specific Atb. such as IgMin
the blood and CSF
- EEG, transfontanelar Eco, cranial CT
Differential diagnosis :
- metabolic encephalopathies: hypoglycemic, uremic, hepatic; those of inborn
errors of carbohydrates or proteins metabolism
- toxic encephalopathies: from drug intoxication, ethanol, insecticides, Reye sdr
- subarahnoidine hemorrhages caused by arteriovenous malformation of the brain
or brain aneurysms
- intracranial expansive processes: tumors, abscesses
- status epilepticus, heatstroke
- neuro-psychiatric diseases: hysteria, schizophrenia
- general infectious diseases of various etiologies
322
- bacterial cerebral embolism, secondary to subacute endocarditis
Treatment : intensive, precocious
A. General measures :
bed rest, hospitalization
hygiene of the skin and mucous membranes, latch position, suctioning of
tracheobronchial secretions, ensurance of bowel and urine output, permanent
surveillance
ensurance of sufficient intake of calories and protein, hydration and feeding (by
parenteral or nasogastric tube)
B. Etyologic treatment :
Acyclovir - herpetic virus, gancyclovir cytomegalovirus, interferon and
izoprinozina
specific human IgG (anti-measles, antiherpetic, antiurlian, anti varicella- Zoster)
gamma globulin intravenously
Encephalitis of non-viral etiology benefit from chemotherapy and antibiotics
according to the sensitivity of the causative germ
C. Pathogenic treatment : is crucial due to the lack of etiologic treatment
corticotherapy is applied early: hydrocortisone hemisuccinate 10-20 mg / kb / day iv
2-3 days, continued with Prednisone 1-2 mg / kg / day po for 1-2 months, depending
on the clinical evolution
to reduce cerebral edema, hypertonic solutions: Mannitol 20% 1,5-2 g / kg / day in
endovenous perfusion repeated every 4-6 hours, 33% hypertonic glucose, furosemide
1-3 mg / kg / day iv or i.m.
patient sedation with Phenobarbital 5-8 mg / kg / day po or i.m. in 3-4 doses, with or
without Diazepam 0.3 mg / kg / dose for convulsion cropping
hydro-electrolitic and acid-base balancing
decompressive lumbar puncture in cases of convulsions or marked agitation
vitamin therapy and neurotrophic medication: Vitamin C, B1, B2, B6, B12, Piracetam
antibiotics (Meropenem, Imipenem, CFS Generation III) are indicated if bacterial
superinfection occurred or there is a high risk of superinfection (profound/prolongued
coma, assisted ventilation).
Complications :
323
- neuro-psychological and varied motor sequelae (motor incoordination, convulsion
syndrome, sensory deficits, behavioral disorders, spastic paralysis, hydrocephalus,
mental retardation, loss of motor acquisition, deterioration of school performance)
- cardiovascular, lung, liver, eyes, etc.
Prophylaxy :
- Combating arthropods-bearing and other main vectors (mosquitoes, ticks)
- Vaccination of high risk population
- Early diagnosis and appropriate and rapid treatment of such infection.
Bibliography :
1. Baghiu Maria Despina Caiete de Semiologie Pediatric, Ed. University Press, Trgu-Mure, 2012, p. 53-
56
2. Iagru Rozina, Ceauu E. Boli infecioase bacteriene i virale la copil n Ciofu E., Ciofu Carmen
Pediatria Tratat, Ed. Medical, Bucureti, 2001, p. 1492-1502, 1542-1547
3. Lazr C. Sindromul de hipertensiune intracranian n Nanulescu M. - Protocoale de diagnostic i
tratament n pediatrie, Ed. Medical Amaltea, Bucureti, 2013, p. 271-276
4. Man Sorin C., Nanulescu Mircea V. Pediatrie practic, Ed. Risoprint, Cluj-Napoca, 2006, p. 577-589
5. Muntean I. Vademecum de Pediatrie, Ed. Medical, Bucureti, 2007, p. 442-447
6. Popescu V. Algoritm diagnostic i terapeutic n pediatrie, vol I, Ed. Medical Amaltea, Bucureti, 1999,
p. 485
7. Popescu V. Algoritm diagnostic i terapeutic n pediatrie, vol II, Ed. Medical Amaltea, Bucureti,
1999, p. 372-378
8. Prober G. Charles - Central Nervous System Infections n Kliegman R.M., Behrman R.E., Jenson H.B. et
al (eds) - Nelson Textbook of Pediatrics, 18
th
edition, Saunders Elsevier, Philadelphia, 2007, p. 2513-2523
SEIZURES
SEIZURES (PAROXISTIC DISORDERS)
Definition: seizures are a series of involuntary, tonic, clonic, tonico-clonic muscle
contractions, partial or generalized, with or without loss of consciousness, representing a
symptom and NOT a disease.
Classification
- non epileptic = the normal brain reaction to noxes; they disappear when the cause is
removed
- epileptic = pathologic cerebral reactivity through neural epileptogenic lesions, having
a recurrent character
324
Etiological classification
1. Acute seizures (non recurrent, non epileptic, occasional)
a) febrile
b) metabolic - hCa, hNa, hMg, HNa, hG, hCu
c) neuroinfections - meningitis, encephalitis, abscess, malaria, typhoid fever, cavernous
sinus, thrombophlebitis
d) cerebral hemorrhage - obstetrical trauma, hemorrhagic disease of newborns,
aneurysms, subdural hematoma
e) toxic - drugs, tetanus, Shigella, Salmonella
f) brain tumors
g) anoxia
h) acute cerebral edema
i) Various - porphyria, SLE
2.Chronic seizures (recurrent, epileptic)
a) Idiopathic epilepsy (primary, cryptogenic, genuine)
- Hereditary
- Acquired
b) organic epilepsy (secondary, symptomatic)
- Posttraumatic (brain tissue rupture)
- Posthaemorrhagic (intra-postnatal, haemorrhagic disease)
- Postanoxic (severe neonatal asphyxia)
- Postinfectious (meningitis, encephalitis, abscess, thrombophlebitis)
- Postintoxication (nuclear jaundice, Pb, As)
- Degenerative (idiopathic atrophy, encephalitis)
- Congenital (cerebral aplasia, porencephaly, holoprosencephaly)
- Parasitosis (cysticercosis, toxoplasmosis)
- Post-hypoglycemia sequelae
c) Sensory epilepsy
- reading, light, music, sound
- touching
- sensorially self-induced
Positive diagnosis
History
325
- infection, trauma, poisoning, anticonvulsive medication (inadequate dosage, lack of
treatment)
- History, pregnancy, birth, perinatal period
Physical examination
- fever
- dysmorphia, microcephaly/ macrocrania, hypo-/hypertelorism
- fontanelle, noise at cranial percussion, hemangiomas
- depigmented areas, stains, hematoma
- nervous - meningeal irritation, motor disorders
Paraclinical
a. blood pressure
b. Lumbar puncture and CSF examination mandatory under the age of 2 years
c. Eye fundus examination- hemorrhage, chorioretinitis, choroidal tubercles, retinitis
pigmentosa, macular cherry spot, angioma, papilloedema
d. cranial radiography - fractures, ICH signs
e. EEG (electroencephalogram) - 8-10 days postcritic
f. Biological - Ca, Ph, alkaline phosphatase, Mg, Glucose, ionogram, Astrup, urea,
enzymes, hemoculture, karyotype
g. Computer tomography - brain tumors, structural abnormalities, cerebral edema,
hemorrhage
Differential diagnosis
1. Syncope - at pain, the sight of blood
2. Sobbing spasm - 6-18 months, neurotic constitution - excessive anxiety of the mother
or of the family environment
3. Narcolepsy - sudden episodic fall in sleep
4. Bouts of vertigo - 1 - 2 years sudden stop from work
5. Spasm mutans - 4-12 months - head shaking in neglected infants
6. Sleep disorders
7. Paroxistic visceral manifestations
8. Nocturnal ambulatory automatism Sleepwalking
9. night pavor - crying / screaming in deep sleep with vegetative reactions: tachycardia,
tachypnea, mydriasis, cold sweat; reactive perturbations within the instinctual
reactive and vegetative sphere
10. Nocturnal verbal automatism somnilocvia
326
11. Masticatory automatisms bruxism
12. Paroxistic visceral manifestations
13. Abdominal epileptic seizures: hyperreactivity + neurovegetative dystonia
14. recurrent idiopathic ketosis
15. Bouts of headache
FEVERISH SEIZURES (FS)
Convulsive syndrome: characterized by paroxysmal seizures of central origin, translated
by seizures triggered by disordered sudden and violent activity of brain neurons.
Febrile seizures (hyperpiretic) convulsive episodes during a febrile extracerebral
illness in a child <5 years, previously normal neurologically and who had not had
convulsions, and if he had, these have always occurred because of high temperature.
Etiology
Without an identifiable cause - occurs in 4% of children
Heredity - "threshold", a predisposition to febrile seizures, however ,> 30% of children with
FS have at least one relative with seizures
Fever - > 38 C is considered to act as a natural contaminant on the CNS
Age (3 months / 6 years) - mostly under 3 years
Infections - FS are more freq. in ear, urinary and respiratory infections,
Pathogenesis
by anoxia and
decreased intake of glucose in the CNS
=> convulsive seizure = response of a normal brain to cerebral aggression
Clinical description - overlaid the epileptic description
Typical forms (simple feverish seizures)
- A feverish child loses consciousness
- a generalized tonic contracture occurs
- overlapping clones
- gradually decrease in number
- crisis ends with a new contracture
- a position of muscle resolution (relaxation) follows, then sleep
- duration less than 20 minutes, usually shorter
327
- changes occur in crisis: pulse, BP, mydriasis, glandular hypersecretion (sweating,
salivation), skin redness, cyanosis (hypoxia and venous return)
- in some cases - the emission of urine and faeces
- post-crisis - more sleepy, lower motility and tone
Atypical forms (complex seizures):
- various aspects: tonic seizures
- unilateral hypotonic crises
- crisis longer than 20 minutes
- partial
- always with worse prognosis than typical forms
Laboratory
- Lumbar puncture (LP)- normal CSF
- LP is mandatory for depletoric effect, diagnosis and it is not dangerous
EEG post - critical (after 10 - 14 days)
- no paroxysmal abnormalities
- similar aspect in crisis to the epilepsy
- the peak wave abnormalities places convulsions in the category of complex seizures
Main diagnosis criteria for feverish seizures:
- occur in connection with temperature> 38
C
- fever is not related to an acute disease of the CNS (meningitis, encephalitis)
- the child does not have a history of neurological disorders (pre-, peri-, postnatal)
Secondary criteria for feverish seizures:
- crisis lasts < 20 minutes
- does not realize the state of convulsive malaise
- clinically: widespread crisis
- age of onset of the first FS - under 3 years
- EEG reveals no pathological abnormalities at 10-14 days after the crisis
Dfferential diagnosis :
- epileptic seizures, other convulsions
- meningitis, encephalitis
- hypocalcemic seizures, hypoglycemia, dehydration (hypo-Na), intoxications
(organophosphorus)
Treatment
328
I. Crisis treatment: - common to all seizures
General measures: silence, head on one side, airways permebealization, O2 administration,
spontaneous recovery may occur.
Medicines: Diazepam iv if the crisis> 3 min - 0.3 mg / kg, repeated 2-3 times, t ~ 15 min.
If the vein cannot be approached quickly- 0.5 mg / kg ir without prior enema (max. 20 mg)
reaches anticonvulsant dose in 4 min. (vs. 20-30 min. at i.m. administration)
Desitin - Diazepam rectal - tube - 5 mg <15 kg and 10 mg> 15 kg, repeated every 2-4 h (in
status epilepticus after 10-15 min. + Glucose + thiamine, vitamin B6); in the absence of
Diazepam, Phenobarbital 10 mg / kg im this will be mentioned on the referral since in the
case of Diazepam administration there is a risk of respiratory arrest or hypo BP.
Diazepam is not associated with any other drug due to frequent incompatibility.
Fighting fever physically
- Tylenol 50 mg / kg / day in 3-4 divided doses p.o. or rectally
- Ibuprofen 20-30 mg / kg / day in 3-4 divided doses p.o. or rectally, over the age of 2
months
II. Post-crisis treatment
Indicated only in recurrent febrile seizures (3-5 FS / year).
Phenobarbital administration of 3-5 mg / kg / day po, - 2 times daily (last 1h before bedtime)
Prophylactic treatment is administered to prevent relapses and is recommended only in case
of frequent relapses in patients with altered EEG. EEG is performed at 7-10 days post-crisis
(immediate EEG is unjustified).
Alternative:
t> 38
C administration of Diazepam i.r. and anti-pyretic (5 years)
Na valproate 20-40 mg / kg / day continuously for children under 3 years
Evolution and prognosis
Immediate evolution - good
- Treated correctly no sign of complications
- 40% relapses
Late prognosis - reserved
- Approximately 5% ( 2% at 5 years, 7% at 25 years) will develop a secondary epilepsy
(residual)
- Follow-p for 6 months from the FS.
- Prognosis depends on many factors
329
Table xxx Risk factors for recurrence of febrile seizures
Major risk factors
Duration of fever < 24 hr
Fever 38-39
0
C
Minor risk factors
Family history of febrile seizures
Family history of epilepsy
Complex febrile seizure
Day care
Male gender
Lower serum sodium
Table xx - Risk factors for occurrence of subsequent epilepsy
Risk factor Risk for subsequent epilepsy
Simple febrile seizure 1%
Neurodevelopmental abnormalities 33%
Focal complex febrile seizure 29%
Family history of epilepsy 18%
Fever < 1 hr before febrile seizure 11%
Complex febrile seizure, any type 6%
Recurrent febrile seizure 4%
330
History
Exam
Manage acute febrile seizure and acute illness (first aid,
midazolam, diazepam, diagnostic tests) as needed.
Determine risk factors for recurrence and estimate risk of
recurrence of the febrile seizures
Counsel parents about risk of
recurrence and how to provide
first aid and manage fever
Determine risk factors for later
epilepsy
Low risk
No therapy or
investigations are
necessary
Intermediate or high risk
1. Consider EEG and imaging
2. Consider intermitent oral diazepam or,
in exceptional cases that recur,
continuous therapy
Figure xxx Management of febrile seizures
Criteria of unfavorable prognosis are:
Small age (under 1 year)
Severity of crisis
Frequency of recurrencesof recurrences
CHRONIC RECURRENT SEIZURES (EPILEPSY)
Epilepsy
Recurrent paroxysms which manifest suddenly with modifications of motor, sensorial,
psychic function and characteristic EEG modifications;
convulsive attack (ictus) can be clinically presented
- as a convulsion
- minor motor movements
- a certain sensation
- momentary stop of activity
- impaired consciousness (not always)
Etiology
80% of the cases - unknown (primary, idiopathic, crypto genetic, essential epilepsy)
331
20% - secondary epilepsy, symptomatic, organic
Secondary epilepsy:
congenital metabolic disease and degenerative (fenilcetonuria)
Cerebral diseases (vascular, tumors, congenital anomalies)
traumatisms (at birth, anorexia) or anoxia?
infections (encephalitis, meningitis)
intoxications (lead) (plumb)
Classification:
Chronic seizures depending on EEG signs
- partial
- generalized
Simple partial seizures:
focal (localized epileptogenic focus) usually motor without loss/alteration of
consciousness
adverse eyes and head turn in opposite position of the focal lesion
Partially complex seizures:
Psychomotor or of temporal lobe
- start as focal, accompanied by sensorial, behavioral, psychomotor, vegetative or
psychic manifestations and generalize secondarily associated with alteration/ loss
of consciousness they manifest as a grand-mal crisis with aura (in idiopathic
epilepsy there is no aura and loss of consciousness is primary)
- the behavioral or affectivity changes can be subtle and difficult to attribute to
epilepsy.
- focus in the frontal lobe
These are adverse or jacksonian seizures, with local motor symptoms (face, hand, leg) which
spread to other muscles. They start suddenly, but do not affect the consciousness, determining
only obnubilation. If they generalize => loss of consciousness
Focal parietal - rare
- they manifest as sensitive jacksonian seizures (paresthesic, painful), with short
duration and no alteration of consciousness
Occipital focal epilepsy
332
They present visual hallucinations (colored points); macro-, microsomia, cecity; their EEG
diagnosis is difficult since it is only suggestively in crisis, 20% from epileptic children have
normal intercritical EEG
GENERALIZED SEIZURES
Tonic-clonic convulsions (grand-mal - GM)
Classical epileptic seizures (described at FS)
There is a prodromal phase, of discomfort which can precede the seizure with ~ hours
(it should be distinguished from aura)
If they start with sensorial or motor aura indicate the cortical focus and will be
classified as complex partial seizures with secondary generalization
focal EEG modifications
no aura in grand-mal.
Petit-mal epilepsy primary generalized forms - 5-15 years
PM absence
- Short crises, below 10-20'', with no sudden loss of consciousness
- The attack can be repeated more times a day precipitated by H-ventilation and
strong light
- without aura or remission, localized automatisms
- EEG complex discharges of peak-wave of 3 cycles/sec.: bilateral, symmetrical,
synchronical
- Myoclonic PM
Short-term loss of consciousness
Myoclonic diskinesia of the face or axorizomelic muscles
symmetrical/ asymetrical myoclonus
recede with the crisis
EEG discharging of peak wave: bilateral, symmetrical, synchronous, with different
rhythm in different patients
f ppoli-wave bilateral, , syncr
- Amiotonic-akinetic PM
Sudden loss of consciousness
Cancelling of the muscle tone
collapse, no other motor manifestations
below 1 minute
333
EEG - discharging of slow sinusoidal, ample waves, on all the derivations: bilateral,
synchronic, symmetrical verysyncron
- Enuretic or encompretic PM
They can transform into GM crisis or temporal epilepsy
Infantile myoclonic encephalopathy with hypsarrhythmia - infantile spasml the West
disease
- Severe affection, appears at 5-6 months
- 3 major manifestations
- Muscle spasms arms and head flexion
Mental degradation
characteristic EEG - hypsarrhythmia total degradation of the route -
hypervolted beta, delta waves
Epileptic encephalopathy with variant PM - B. Lennox Gastaut
- Severe affection but with low incidence
- Varied epileptic manifestations
- muscular atony with body or head falling on the chest no consciousness
modification most frequently (necessaryforo diagnosis)
- Can be atypical tonic, psychomotor, myoclonic PM, GMcrisis,
- specific EEG (petit-mal variant) - complex peak-wave of 1,5-2,5 cycles/sec.
EPILEPTIC STATUS
Succession of convulsive crises which last more than 20 min., repeated without
consciousness recovery
GM, PM or focal type
Can reappear spontaneously, often favored by infections, traumatisms, metabolic
disorders, intoxications, usually appear at lack of anticonvulsive treatment
Life-threatening through hypoglycemia, hypoxia, acidosis, high BP and ICH,
hyperpyrexia
EEG shows activity of neuronal disorder
It is the main element in the classification of convulsions
334
correct classification is crucial in finding the right treatment
In partial convulsions (simple or complex), the electrical line indicates the epileptogen
focus
grand-mal crisis- highly volted peaks
Crisis of absence peak or slow wave at 3 cycle/s on a normal basic rhythm
myoclons- multifocal peaks at 2-4 cycle/s.
infantile spasm (West Dis.) hypsarrhythmia with irregular peaks or waves
General treatment
Keep the vital functions (dezobstruation, O
2
, intubation, cardiac massage)
DZ - 0,2-0,3 mg/kg i.v. slowly, repeatable 2-3x or i.r. 0,5 mg/kg, max. 20 mg
(plasmatic anticonvulsivant conc. in 4 minutes)
Fight the main causes (metabolic)
succession (after blood collection for laboratory tests):
- sol. G 20% 2 ml/kgc i.v
- sol. gluconic Ca 10% 1-2 ml/kgc i.v. slowly
- sol. SO
4
Mg 25% 0,2 ml/kgc i.m (!)
- Piridoxin 50-100 mg/ dose i.v.
Treatment of bad convulsive state
a) Maintain the vital functions
- monitoring, control hypoxia - bladder catheterization
- venous way - combat hyperpyrexia and acidosis
- treat ICH - corect the metabolic disorders
- emergency anticonvulsive treatment
b) Stop the seizures
Diazepam 0,3 mg/kg/D i.v. slow or PEV in SF solution
Fenitoin - 10-12 mg/kg, i.v ( conv. in 5-10 min.)
Phenobarbital 5-7 mg/kg i.v./i.m. ( conv. n 20 min.; !associated with DZ depresses
respiration)
Paraldehid 4%, 2-4 ml/kg i.r.
Xilin 5-10 mg/kg/h i.v. EKG monitoring
Na Valproate 30-50 mg/kg i.r.
Total anesthesia and curing
335
Antitermics in febrile convulsions
in CF
Post-crisis Treatment
- Phenobarbital 3-5 (6) mg / day, po, 2 doses, the last before bedtime in recurrent
prolonged, focal seizures,
- Na valproate or 0.3 mg / kg / day - 2 doses po
- Prophylactic treatment 3-4 years follow-up
- Gradually decrease the dose for 2 months, then stopping treatment
Follow-up of epileptic patients
Periodic clinical control+ EEG every 6 months or when needed
If the patient does not have crisis for 3-5 years, medication is stopped
Compulsory follow-up
Orientation towards jobs without danger of traumatisms, accidents
In adolescent s epilepsy has good prognosis, but the treatment will last (more than 2-
3 years)
336
CHAPTER IX HEMATOLOGY
Asist. Univ. Dr. Chincean Mihaela
ANEMIA IN CHILDREN PRINCIPLES OF DIAGNOSIS
Definition: Anemia is defined by decrease in the number of circulating red blood cells
associated with parallel decreases in hematocrit and hemoglobin concentration. It is not an
independent disease, rather a symptom of a particular disease.
Criteria of hospital admission:
- Any severe anemia with Hb <6 g / dl, regardless of age
- Newborns with Hb <13 g / dl, infants under 6 months with Hb <8 g / dl and clinical signs
Positive diagnosis of the type of anemia is made through: history, physical examination and
laboratory data.
A. History
- detection of possible sources of bleeding, occult blood loss
- duration of symptoms
- existence of recent or repeated infections
- amendment of the type of infant feeding, consumption of meat, milk, iron
deficiency anemia under treatment (curative / preventive), consumption of beans
(G6PD deficiency anemia)
- drugs intake: Chloramphenicol
- neonatal pathology: prolonged jaundice, hemolytic disease, prematurity, twins
- ethnic group
- family history of anemia
B. Physical examination: complete; BP is measured and heart rate is monitored
Symptoms: lethargy, fatigue, dyspnea
Signs:
- Pallor (elective areas of evaluation: pinna, lips, sclera, oral mucosa, palms, plants, nail
bed)
- Jaundice (hemolysis)
- Active bleeding, petechiae
- Adenomegalia
- Hepato-splenomegaly
337
- Bone abnormalities; dysmorphia
- Stool with altered appearance
C. Laboratory
- complete blood count with peripheral smear
- reticulocyte count (> 2% if bone marrow functions normally)
- MCV (mean corpuscular volume)
- total bilirubin and direct and indirect fractions
- urea, creatinine, ionogram, sideremia
- blood group
- urine test
- stool test for occult bleeding
Hypochromic microcytic anemia: MCV <70 fl under 5 years <75 fl 5 years
Additional tests: ferritin, hemoglobin electrophoresis to rule out a hemoglobinopathy.
Iron deficiency anemia is investigated according to the protocol for iron deficiency anemia.
Normocytic normochromic anemia: MCV between 70-90 fl
If serum bilirubin is increased and is associated with reticulocytosis these suggest a
haemolytic anemia.
Macrocytic anemia: MCV> 90 fl
Is rare in child pathology and suggests vitamin B 12 and / or folic acid deficiency secondary
to malabsorption.
Normal valuesof red blood cells in the period 0-18 years of age are shown in Table I.
Table I - Erythrocyte values according to age (average, lower limit of normal
lower limit is given by two standard deviations below the mean)
Age
Hemoglobin (%) Hematocrit (%) MCV (fl)
Average
Inferior
limit
Average
Inferior
limit
Average
Inferior
limit
1-3 days 18.5 14.5 56 45 108 95
1 month 14.0 10.0 43 31 104 85
2 months 11.5 9.0 35 28 96 77
3-6 months 11.5 9.5 35 29 91 74
6 months-2 12.0 11.0 36 33 78 70
338
years
2-6 years 12.5 11.5 37 34 81 75
6-12 years 13.5 11.5 40 35 86 77
12-18 years
females
14.0 12.0 41 36 90 78
12-18 years
males
14.5 13.0 43 37 88 78
IMMUNE THROMBOCYTOPENIC PURPURA (ITP; IDIOPATHIC PT;
WERLHOFF DISEASE)
Definition: purpuric syndrome caused by low platelet count (below 100.000/mm3) due to
peripheral damage by immunological mechanisms, which exceeds the capacity of normal
compensatory thrombocytopoiesis, hematologically translated by thrombocytopenia with
megakaryocytosis.
Etiologic classification
Idiopathic (primary): 5 -10 %
Secondary
- postinfectious (EBV, CMV infection, varicella, rubella, measles, tuberculosis, HIV)
- after vaccination
- collagen diseases
- lymphoproliferative syndromes
- solid tumors
- medicines:
antibiotics: ampicillin, gentamicin, penicillin, rifampicin, trimethoprim,
vancomycin, sulfamethoxazole
NSAIDs: acetaminophen, aspirin, gold salts, phenylbutazone
other: digoxin, allopurinol, carbamazepine, cimetidine, diazepam
heparin, spironolactone, morphine
- pregnancy
- other (hemophilia A, Hashimoto thyroiditis, sarcoidosis)
339
Epidemiology: in up to 90% of the cases, the immunological nature of the disease can be
proven. It mostly occurs in children aged 2-8 years and adolescents, often 2-3 weeks after an
intercurrent infection and has an increased seasonal incidence (March to October).
Pathogeny: The disease is caused by immunological mechanisms (antiplatelet and
antimegakarocytic antibodies) where the spleen plays a role in removing the sensitized
platelets and acts as a source of antiplatelet antibodies. In 30% of cases other organs,
particularly the liver, may be involved as well.
Clinical manifestations: The onset may be gradual or insidious (more frequently chronic
ITP). During the state period, mucocutaneous purpura and visceral bleeding appear. Bleeding
is spontaneous and prolonged; there is no serious bleeding and the overall condition is good.
- skin purpura: the skin petechiae and bruising appear in minimal traumas or
spontaneously, especially in exposed areas (legs), giving the appearance of
"bludgeoned child " or leopard skin
- mucosal bleeding: epistaxis, gingival bleeding, haemorrhagic bullae, endo oral
purpura = wet purpura
- visceral bleeding: meningo-cerebral hemorrhage is the most feared
- puberty menorrhagia: may be the only manifestation
- splenomegaly; adenomegaly - rarely
Clinical elements of severity:
- association in the onset or during the evolution of a diffuse purpura on the
abdomen
- oral bleeding bubbles
- hematuria
- retinal hemorrhage - may herald impending meningocerebral hemorrhage.
Laboratory
- complete blood count: Thrombocytopenia <100.000/mm
3
- prolonged bleeding time, normal clotting time
- PTT and PT
- Coombs test
antiplatelet antibodies
immune complexes fixed on platelets
marrow examination: pronounced megakaryopoiesis, with deviation to
the left of the megakaryogram.
Typical aspect for ITP:
340
Tr <50.000/mm Hb > 10 to 11 g%
WBC: 4000-5000/mm Granulocytes: 1500-2000 / mm
Peripheral smear of normal appearance
Positive diagnosis is based on the following criteria:
- clinical criteria: cutaneous and mucosal petechiae purpura, no adeno-
hepatosplenomegaly
- peripheral haematological and bone marrow criterion: isolated thrombocytopenia;
normal or increased number of megakaryocytes in the bone marrow, with deviation to
the left of the megakaryogram
- exclusion of other causes of excessive platelet destruction
- immunological criterion (optional): antiplatelet antibodies or immune complexes
fixed on platelets
Differential diagnosis:
1. Schonlein-Henoch Purpura the number of platelets is normal
2. Other thrombocytopenias:
- congenital bone marrow production deficiency : Fanconi anemia, TAR syndrome,
osteopetrosis, thrombocytopenia of metabolic diseases
- acquired bone marrow production deficiency: aplastic anemia, leukemia,
lymphoma, infections, medications, toxic substances.
- excessive destruction: immunological; trombocytoliytic (post-vaccination, viral
infection, drug); splenic sequestration (congestive splenomegaly); excessive
consumption (DIC, hemolytic syndrome) mechanical destruction (prosthetic heart
valves).
Treatment
General measures: Being a self-limited disease, most patients with ITP are doing well
without medication. Bed rest, avoidance of trauma, injections and vaccinations at least 18-24
months as well as drugs that interfere with platelet function (NSAIDs, Aspirin) are important.
1. Initial treatment
Corticotherapy: various schemes; inhibits platelet phagocytosis by splenic macrophages;
enhances capillary resistance and inhibits antibody synthesis.
- Prednisone 1-2 mg / kg / day po in three divided doses for 14-21 days, with gradual
reduction and discontinuation in 4-6 weeks
- Prednisone 4 mg / kg / day po divided into three doses for 7 days, with progressive
reduction and remission in 3 weeks
341
- Methylprednisolone 30 mg / kg / day iv for 3-4 days.
Depending on the response to corticosteroids, there are ITP corticosensibile forms,
corticosteroid dependent or corticoresistant forms.
Immunoglobulin intravenously:
- 400 mg / kg / day 4 consecutive days or 1-2 g / kg / day for 2 consecutive days
Red cell mass: only in severe forms, with life-threatening bleeding.
Emergency plasmapheresis or splenectomy may be necessary in patients refractory to
first-line treatments mentioned above.
2. Treatment of refractory forms
Immunosuppressive therapy:
Azathioprine (Imuran) 1-2 mg / kg / day
6-Mercaptopurine 1.5-2.5 mg / kg / day
Cyclophosphamide 1-2 mg / kg / day
Vincristine 1.5 mg / m / week
Interferon
Cyclosporine
Monoclonal macrophage antibodies (Rituximab)
Splenectomy is indicated only after the age of 4 years, in chronic forms, after at least 12
months of evolution and appropriate preparation (pneumococcal polysaccharide,
meningococcal and antihemophylus vaccines). Splenectomy is effective in 70-80% of cases;
in 20-30% may not be effective if the platelets are sequestered and destroyed in the liver and /
or bone marrow.
Complications
- cerebral hemorrhage in 1% of cases
- fatal hemorrhages
- infectious complications after splenectomy
- viral infection after therapy with blood products or immunoglobulins
Evolution and prognosis
The prognosis is generally favorable. ITP is an evolving self-limited benign disease in 80-
90% of cases. In 10-20% of cases chronicity risk exists, especially in over 10 year-old girls,
with lack of response in the first 3 weeks of disease development.
342
HEMOPHILIA
Definition: Haemophilia is a hereditary coagulopathy characterized by low levels of blood
coagulation factor VIII (haemophilia A), IX (Hemophilia B) and XI (Hemophilia C).
Haemophilia A is four times more common than haemophilia B.
Pathophysiology: Coagulation factors VIII and IX are important in the formation of
thrombin. When an injury occurs, a primary thrombus is produced that will then be woven by
fibrin filaments. Haemophilia is characterized by delayed abnormal thrombus formation.
Deep hemorrhage (intra-articular, intramuscular) is characteristic in hemophilia. The
thrombus is brittle and recurrent bleeding is frequent.
Figure I. Coagulation cascade
Etiopathogeny: The defective gene is located on chromosome X, and X-linked transmission
is recessive, so women carriers transmit the disease and it manifests in boys.
Figure II. X-linked transmission
Female carrier Affected male
-50% risk of daughter carriers -All daughters are carriers
-50% risk of boys with hemophilia - No boy will be affected
343
Epidemiology: Haemophilia A is the most common hereditary coagulopathy, its prevalence
being 10-20/100.000 newborn males. Hemophilia A occurs in 85% of haemophilia patients
and haemophilia B just in 15%.
Severity: Is assessed by the level of the factor affecting the patient's blood:
- severe form: factor VIII less than 1%
severe bleeding either spontaneously or with minimal traum
- average form: factor VIII between 1-5%
bleeding from minor or moderate trauma
- mild form: factor VIII > 5%
late diagnosis, bleeding from surgery or major trauma.
344
Clinical manifestations:
Haemophilia A is rarely revealed in the neonatal period; 2% of neonates with hemophilia
have cerebral hemorrhage and 30% bleed profusely during circumcision. Most commonly,
the diagnosis is made only at the age of 1-5 years, first signs of the disease often occurring
during tooth eruption or walking, when small accidents involve bleeding.
Bleeding characteristics:
Caused hemorrhage (minor trauma, injection, puncture)
Appearance of "spontaneous" bleeding in very low concentrations of factor VIII
Prolonged duration of outward bleeding without tendency of spontaneous stopping
Profound hemorrhage localization : intracavitary, intratissular, intravisceral
No petechial lesions
The most common bleeding manifestations are:
Hemarthrosis: large joints - knees, elbows, ankles, hips, shoulders
Bruising and superficial subcutaneous or intramuscular hematoma (buttocks
muscles, deltoids, pectorals) and profound (ilio-psoas muscle, retroperitoneal)
Epistaxis, "open" buccal and lingual bleeding wounds, bruise / cut skin wounds
Hematuria
Meningocerebral hemorrhage - life-threatening
Gastrointestinal bleeding
Laboratory
normal bleeding time (BT)
extended clotting time (CT)
normal platelets, leukocytes and erythrocytes
normal Quick Time (PT)
prolonged activated partial thromboplastin time (APTT)
low factor VIII level
Hemophilia cannot be diagnosed without the coagulogram !!
Positive diagnosis: In a male patient is based on personal history, present or absent family
history of bleeding in conjunction with clinical and laboratory manifestations (deep or
externalized bleeding) are suggestive.
Differential diagnosis
- Haemophilia through factor IX deficiency (Hemophilia B) or XI (Hemophilia C): the
thromboplastin generation test
- ITP: petechiae and bruises that occur spontaneously; decreased platelets
345
- Acute leukemia: characteristic clinical and hematologic features
Treatment
Prophilactic treatment
- genetic counseling
- counterindication of im injections and Aspirin
- lifestyle that avoids trauma and aggressive sports; choosing a profession that will not
expose to accidents and injuries
- prophylactic treatment with factor VIII three times a week at a dose of 20-40 U / kg
iv.
Curative treatment: consists in substitution of the deficient factor. The treatment begins
when bleeding occurs, within the first hour of bleeding. The hemorrhage is difficult to control
when the replacement therapy is delayed.
Factor VIII dose = % x G (kg) / 2
% = the value at which we want to increase the factor VIII level in the patients blood and it
depends on the location and severity of bleeding (bleeding from the mouth 30-40%; joint or
muscle bleeding 40-60%; hematuria 40-50%; cerebral hemorrhage 100%). The half-life of factor
VIII is 12 hours, therefore, the calculated dose is administered twice a day i.v. (every 12 hours).
Factor VIII products:
Factor VIII recombinant
Factor VIII concentrate extracted from human plasma
Cryoprecipitate (a bag of cryoprecipitate contains about 100 U of factor VIII)
Fresh frozen plasma 10 to 15 ml / kg / dose
Adjuvant therapy: In mild bleeding or lesions, application of ice, local pressure are useful;
local agents (Gelaspon, thrombin sponges); in mucosal bleeding antifibrinolytic therapy is
used (epsilon-aminocaproic acid, tranexamic acid).
Complications
- disease-linked: joint ankylosis, nerve compression, muscle contractions and
retractions
- the advent of anti factor VIII inhibitors
- viral infections by administration of inappropriate products (HIV, Hepatitis A, B, C,
CMV, EBV, parvovirus, etc.)
Prognosis: is favorable in a correctly followed up patient. Childhood trauma are more
frequent; after the age of 15 bleeding tendency decreases. With chronic replacement therapy
at a young age, the quality of life increases.
346
References:
1. Arceci Robert J, Hann Ian M, Smith Owen P. Pediatric hematology, 3th edition. Blackwell Publishing,
2006
2. Baghiu Maria Despina, Horvath Adriennne. Hematologie, oncologie i endocrinologie pediatric. Note de
curs pentru medici rezideni. Litografia UMF Trgu Mure, 2007
3. Lanzkowsky P. Manual of Pediatric Hematology and Oncology, 4th edition. Elsevier, 2005
4. Man Sorin C, Nanulescu Mircea V. Pediatrie practic. Ed.Risoprint Cluj-Napoca, 2006
5. Muntean I i colab. Vademecum de pediatrie. Ed.Medical Bucureti, 2007
6. Schwartz M.William, Bell Louis M, Bingham Peter M. et al. 5-Minute Pediatric Consult, 5
th
edition.
Lippincott Williams & Wilkins, 2008
7. erban Margit, Ioni Hortensia, Poenaru D, Ritli L.O via cu hemofilie. Ed. Brumar Timioara, 2009
8. erban Margit, Schramm W. Hemostazeologie clinic. Ed.Brumar Timioara, 2001
347
CHAPTER X ONCOLOGY
Asist. Univ. Dr. Chincean Mihaela
LEUKEMIAS
Although rare in childhood, malignancies are the 2nd leading cause of death, following
accidents. Leukemia is the most common malignancy in children, followed by brain tumors
and lymphomas. The incidence is 3.5 cases / year / 100,000 children under 15 years.
Classification
1. Acute leukemias:
- Acute lymphoblastic leukemia (80%)
- Acute myeloblastic leukemia (20%)
2 . Chronic leukemias:
- Chronic granulocytic leukemia (1%).
ACUTE LYMPHOBLASTIC LEUKEMIA (ALL)
Epidemiology: Acute lymphoblastic leukemia occurs more frequently in boys at the age of
2-5 years.
Etiology:
Environment Factors:
- ionizing radiation - after the atomic bomb (Japan) - increased incidence of ALL
- toxic chemicals: benzene, pesticides, herbicides
- alcohol
- medicines: alkylating substances, Leukeran, Cyclophosphamide
- diagnostic irradiation in pregnant women increases by 5 times the risk of leukemia in
the fetus during the first term
Viral infections:
- Epstein-Barr virus can produce mature B-cell ALL (FAB L3)
- T lymphotropic human virus may cause T-cell ALL
- HIV (or secondary immunodeficiency) predisposes to malignancy
Immunodeficiencies:
348
- Primary: Bruton agammaglobulinemia, Wiskott-Aldrich sdr., ataxia telangiectasia,
congenital neutropenia, etc.
- Secondary: HIV infection, chemotherapy treatments, cortisone treatments
Chromosomal abnormalities and other genetic diseases:
- Down Sdr.(trisomy 21) - leukemias are 10-18 times more common
- Neurofibromatosis
- Fanconi Anemia (pronounced chromosomal fragility)
- in families with ALL children - 2-3 times higher risk to other children than in the
general population
- monozygotic twins - 25% risk of the twin to develop leukemia
Pathogeny
Through malignant transformation of a lymphoid precursor, a malignant clone forms that will
be able of infinite self-replication. At least two sequential mutations in genes that check cell
proliferation are necessary in order to produce leukemia. Malignant transformation and clonal
proliferation may occur at different stages of lymphoid differentiation (maturation).
Clinical manifestations
Signs and symptoms may rarely occur suddenly, within a few days, but most commonly the
onset is insidious, taking a few weeks or months. The clinical picture is given by the fact that
the bone marrow is infiltrated with lymphoblasts and production of normal cellular elements
disappears, blastic extramedullary infiltrations appearing as well.
Marrow infiltration with lymphoblasts determine:
Anemia: pallor, fatigue, dizziness
Neutropenia: fever, infections
Thrombocytopenia: bleeding skin and mucosa
Extramedullary leukemic infiltrations:
- Adenomegaly - Hepato-splenomegaly
- Bone pain - Renal infiltrations
- Pericarditis - Infiltration of the myocardium
(cardiomyopathy)
- Pleurisy - Mediastinal tumor (in ALL with T cells)
- Testicular impairment - CNS symptoms: headache, vomiting, seizures
- Skin signs - Eye infiltration
Laboratory
Blood count highlights three major events:
349
- aregenerative normochromic, normocytic anemia
- thrombocytopenia (<100.000/mm )
- leukocyte abnormalities: leukemia-form (Leukocytes > 10.000/mm )
subleukemic form (Leukocytes 5-10.000/mm )
aleukemic-form (Lekocytes <5.000/mm )
Peripheral smear: monomorphic lymphoblasts give a monomorphic character to the
peripheral smear
Bone marrow: marrow examination shows decreasing numbers of normal hematopoietic
series and their replacement with pathological lymphoblasts morphologically similar to those
in the periphery. The presence of lymphoblasts, higher or equal to 25% in the bone marrow
establishes the ALL diagnosis.
- Morphological examination of the bone marrow: lymphoblasts are classified based on
morphological aspect into 3 types (FAB classification): L1, L2, L3. In terms of prognosis,
L1 has the best prognosis, L2 poorer and L3 corresponds to mature B cell with the
poorest prognosis.
- Cytochemical examination: the lymphoblast is PAS (periodic acid Schiff) positive and
peroxidase negative
- Immunologic examination of the blasts is performed with monoclonal antibodies.
Lymphoblasts may be B and T cell line at various stages of differentiation. Markers for
cell line B: CD 19, CD20, CD21, CD24 and T cell lines are: CD1, CD2, CD3, CD4, CD5,
CD7, CD8.
- Cytogenetic examination: Changes in the number or structure of chromosomes are
observed in the malignant transformed cells. Of the changes in number (ploidy),
hiperployd forms have better prognosis and of the structural changes, deletions,
translocations, duplications. Some translocations have favorable prognosis, t (12, 21),
other unfavorable t (8, 14), t (9, 22), t (4, 11).
- Changes in molecular genetics: gene rearrangements can be observed.
CSF examination: in case of meningeal damage, there are changes in the cerebrospinal fluid:
increased cellularity, increased proteinorahia, low glicorahia; CSF smear shows
lymphoblasts.
Laboratory in tumor lysis syndrome: increased LDH, uric acid, phosphorus and calcium.
Imagistic explorations
- Chest Rx: widening of mediastinum or tumor mass and / or adenomegaly.
- Long bones X-ray: osteoporosis and vertebral body deformity.
350
- Abdominal ultrasound: nephromegaly, abdominal lymphadenopathy, hepato-
splenomegaly.
Eye fundus examination: papilledema, retinal hemorrhages, tortuous vessels (CNS disease)
Brain MRI / CT: brain infiltration (CNS disease)
Differential diagnosis
Histologically benign diseases
- Rheumatoid Arthritis - Infectious mononucleosis
- Pertussis - ITP
- Aplastic Anemia - Acute infectious lymphocytosis
Malignancies
- Neuroblastoma
- Retinoblastoma
- Rhabdomyosarcoma
Other: hypereosinophilic syndrome
Prognostic factors
Favorable prognosis
- age 1-6 years
- females
- initial number of leukocytes <20.000/mm3
- rapid response to corticosteroids (Day 8- absolute number of lymphoblasts in
peripheral blood <1.000/mm3)
- complete remission on day 33
- L1 morphology according to FAB classification
- pre-B immunology
- absence of Philadelphia chromosome and other adverse translocations
Unfavourable prognosis
- age <1 year or> 6 years
- males (testicular relapse, at ALL more frequently with Tcells)
- poor response to corticosteroid therapy (day 8 number of blasts> 1.000/mm3 in
peripheral blood)
- lack of remission on day 33
- immunology: ALL with B mature cells, ALL with T cells, presence of Philadelphia
chromosome t (9, 22)
- cytogenetics: hypoploidy, euploidy
351
- CNS symptoms in the onset
- poor nutrition
Treatment: is done in specialized centers according to treatment protocols and proper
stratification of patients into risk groups. Intensity of treatment depends on leukemia
malignancy; chemotherapy and supportive treatment is applied in parallel.
The goal of the treatment: treating the patient with minimal risk of drug specific acute
toxicity and late complications and achieving long term total remission (disappearance of
signs and symptoms, normal blood count and peripheral smear, <5% lymphoblasts in the
bone marrow).
Treatment principles:
- Induction: induction treatment lasts two months, the aim being to achieve total
remission. It includes the following medication: high-dose prednisone and cytostatics:
asparaginase, citozinarabinozide, cyclophosphamide, daunorubicin, purinethol,
vincristine, intrathecal methotrexate.
- Consolidation/ intensification treatment: lasts two months, aiming to further
decrease the number of lymphoblasts in the body. It includes chemotherapy that is
different than in the induction: high-dose methotrexate IV, intrathecal methotrexate,
purinethol p.o.
- Re-induction treatment: lasts 6 weeks and is similar to induction with some
modifications in order to eradicate minimal residual disease.
- Maintenance treatment: lasts 2-2.5 years, so that all the treatment takes just three
years, calculated from the first day of treatment. It includes purinethol po once daily
and methotrexate po once/ week, with re-induction twice a month with a dose of
vincristine po, and prednisone 5 days po; at 3-4 months intrathecal methotrexate is
administered for CNS prophylaxis.
- Cranial irradiation: is indicated in all cases of high and medium risk of CNS
symptoms in the onset or T-cell leukemia and is applied at the beginning of the
maintenance treatment.
- Allogeneic bone marrow transplantation: is indicated in high-risk forms and
relapses, if remission can be achieved again.
- Support treatment:
Isolation of the patient to protect him from infection: compliance with the rules of
hygiene
352
Appropriate diet: hypo-sodic diet during corticosteroid therapy, avoiding salads, raw
food, salami, etc., during severe marrow aplasia; otherwise, varied, balanced diet.
Prophylaxis of infections that are frequent and severe in immunocompromised
patients:
- carinii pneumonia prophylaxis with Biseptol 6-8 mg / kg / day, 3 days / week
throughout cancer therapy.
- chickenpox can be fatal, so avoid contact with chickenpox patients; in case of
contact: high-dose acyclovir, 14 to 28 days po. In case of chickenpox, specific
anti-chickenpox Ig and acyclovir are administered i.v. Vaccination (live
attenuated varicella vaccine) is absolutely counter-indicated in immune-
compromised patients (may cause chickenpox).
- any acute bacterial infection is treated vigorously with broad-spectrum antibiotics
in high dose intravenously.
Management of transfusion:
- anemia is adjusted to Hgb <8 g%, except in septicemia, where red blood cell
mass is administered in Hgb values <10 g%.
- thrombocytopenia is adjusted to Tr <10.000/mm3 or at any value if the patient
bleeds - standard platelet mass is administered/ obtained through cytapheresis.
- Fresh frozen plasma may be administered for hemostasis disorders or CID.
- Administration of granulocyte-monocyte colony stimulating factors:
in the case of severe neutropenia (<500/mm
3
) associated with infection, the aim
being to shorten the neutropenic period.
Prognosis: total remission can be achieved in 75% of the patients; 25% die from
complications or cytostatic drug resistance. 30% of patients may present BM or extra-
medullar relapse (testicle, CNS). The occurrence of relapses implies a poor prognosis,
especially if they appear under chemotherapy or within the first 6 months after treatment
(early relapses); late relapse prognosis is more favorable.
Complications
Complications caused by the underlying disease:
- DIC with cerebral hemorrhage
- acute renal tumor through the lysis syndrome
- leukemic infiltration of the brain that can cause seizures, intracranial hypertension
- mediastinal compression
Treatment-induced complications:
353
- Corticotherapy: osteoporosis, hypokalemia, psychosis, ulcers, cataracts, iatrogenic
diabetes, cardiomyopathy, Cushingoid appearance, muscle weakness, high blood
pressure.
- Early chemotherapy-induced complications: infections of any type, anemia, anorexia,
nausea, vomiting, mucositis, alopecia, peripheral neuropathy, myopathies, hemostasis
disorders.
- Late cytostatic- induced complications: mental disorders,learning difficulties,
infertility, endocrine disorders (most commonly hypothyroidism), the appearance of
the second tumor (even after 10 to 15 years), cardiomyopathy, liver fibrosis,
psychosocial disorders (isolation).
Patient follow-up
- during treatment every week, or every 4 weeks depending on treatment
- follow up care continue even after the end of chemotherapy, for at
- least 5 years, preferably throughtout lifetime.
MALIGNANT LYMPHOMA
HODGKIN LYMPHOMA
Epidemiology:
The disease occurs more frequently in two age groups: at the age of 20 and 50 years; in
childhood it is more common over the age of 5 years. Boys are more prone to the disease than
girls. A relationship between infection with Epstein-Barr virus (EBV) and Hodgkin's disease
occurrence was established, the presence of EBV genome embedded in the DNA of Reed-
Sternberg cells and positive serology for anti EBV Ab.
Biology:
Reed-Sternberg cells are formed from malignant transformation of activated B-cells.
Malignant transformation is triggered by a genetic abnormality or external environmental
factors. Malignant giant Reed-Sternberg cell produces cytokines that act like growth factors
on Reed-Sternberg cells and other cells (lymphocytes B, T, eosinophils, granulocytes).
Histology:
Malignant cells form <1% of the tumor cell population, the rest being represented by
inflammatory infiltrate with histiocytes, plasma cells, lymphocytes, eosinophils, neutrophils
354
and fibrosis, caused by the action of cytokines secreted by tumor cells. In diagnosis
development, Reed-Sternberg cell, inflammatory infiltration and fibrosis must be present.
Reed-Sternberg cells may be present in other malignancies (sarcoma, non-Hodgkin
lymphoma, carcinoma) and in non-malignant diseases (infectious mononucleosis).
Histological types of lymphoma
- Lymphocytic predominance: occurs in 10-15% of patients and has the best prognosis. It
is characterized by a benign inflammatory infiltrate, and if the few Reed-Sternberg cells
are not found, it may be mistaken for reactive lymphocytic hyperplasia.
- Mixed cellularity: occurs in 25-30% of patients, especially under the age of 10 years;
usually patients present to the doctor in advanced stages.
- Lymphocytic depletion: rare in childhood, is the form with the most severe prognosis;
Develops bone and bone marrow metastases. It is characterized histologically by the
paucity of lymphocytic infiltrate and presence of more Reed-Sternberg cells.
- Nodular sclerosis: occurs in 40% of younger children and 70% of adolescents. Reed-
Sternberg cells are difficult to highlight.
Clinical features
- Volume increase of lymph nodes: latero-cervical or supra-clavicular nodes are
frequent, of firm consistency; sometimes node conglomerates; mediastinal lymph
nodes causing compression signs: rare irritative cough, dyspnoea, face edema, face
cyanosis. Rarely, the disease begins with the swelling of axillary or inguinal lymph
nodes.
- Splenomegaly, frequently
General signs - may be present: fatigue, weight loss, anorexia.
Subjective signs - "B symptoms" - have worse prognosis and are used in staging: fever, night
sweats, loss of > 10% of body weight in the last 6 months
- itching, sometimes just excoriations from scratching
- extranodal implications: bone marrow, liver, CNS (10-15%)
- bone and lung implications: rarely
Laboratory
Blood count: leukocytosis, neutrophilia, lymphopenia (in advanced cases), eosinophilia,
monocytosis, moderate microcytic anemia with hypersideremia
ESR may be increased and may be an element of evolution and prognosis
Liver function tests modified in cases of hepatic involvement
355
LDH (lactic dehydrogenase), cupremia and ferritin are increased and are markers for
evolution and prognosis
Node biopsy: essential in the diagnosis
Chest Rx: hilar lymphadenopathy or mediastinal masses
Thoracic and abdominal CT: show node, pulmonary, hepatic and splenic involvement.
Bone marrow examination: shows marrow involvement in advanced cases
Bone scan: shows bone involvement in advanced cases
PET / CT exam (positron emission tomography combined with CT) allows accurate staging
of the disease and response assessment to treatment
Ann Arbor Staging
- Stage I: damage to a single lymph node region or a single extra-lymphatic organ
Stage II: 2 or more lymph node regions on the same side of the diaphragm, or
extra-lymphatic organ + ganglion on the same side of the diaphragm
- Stage III: impaired lymph node region on both sides of the diaphragm spleen
(IIIS) extralymphatic organ (IIIES)
- Stage IV: disseminated disease (liver, skin, bone, bone marrow).
Differential diagnosis
Lymphadenopathy should be distinguished from
- inflammatory origin: tuberculosis, toxoplasmosis, infectious mononucleosis
- Non-Hodgkin Lymphoma
- Metastases: nasopharingeal carcinoma, sarcoma of soft parts
Mediastinal tumor: differs from normal thymus
Treatment
Chemotheropy
ABVD (adriamycin, bleomycin, vinblastine, dacarbazine)
COPP (cyclophosphamide, oncovin, prednisone, procarbazine)
- Radiotherapy: Hodgkin lymphoma is sensitive to radiotherapy
- Autologous stem cell transplantation, bone marrow transplantation: indicated in relapses
after further chemotherapy
Prognosis: survival over five years is possible in 90% of cases; in stage IV - 65%.
356
NON-HODGKIN LYMPHOMA
Epidemiology:
5-7% of child malignancies; is rarer in children than in adults; the incidence increases with
age. Burkitt lymphoma from Africa is known as endemic whereas forms from other
geographic regions are known as sporadic. Epstein-Barr virus infection is attributed a role in
the etiology of endemic Burkitt lymphoma (BL).
Classification
B-cell Lymphomas
T-cell Lymphomas
In precursor tumors, thymus is affected especially in the T-cell lymphoblastic lymphoma.
Burkitt lymphoma (BL), Burkitt-like, and large B-cell (LBCL) are mature B-cell lymphoma;
lymphoblastic lymphoma (LL) is in particular a pre-T cell lymphoma and anaplastic
lymphoma with large cells (ALCL) derive from T cells or natural killer (NK).
Clinical features: varies depending on the histological type. Usually it has extra-nodal
location. B-cell lymphomas are in the abdominal cavity and T-cell lymphomas in the thorax.
General signs (fever, weight loss) are rarely encountered.
Sporadic Burkitt Lymphoma:
- abdominal location: abdominal pain, vomiting, diarrhea, abdominal distention,
palpable abdominal mass, ascites, hepatosplenomegaly
- frequently invades the retroperitoneal structures (pancreas, kidney)
- frequent ovary infiltration
- nasopharingeal location - rarely (unilateral tonsillar hypertrophy) or paranasal sinuses
- skin and mediastinal location - extremely rare
- lymphomatous infiltration of the breast - in pre-pubertal girls and breast-feeding
mothers
Endemic Burkitt lymphoma: common in Africa, affecting mostly the jawbone
Lymphoblastic lymphoma:
- pre-T LL: mediastinal mass
- pleurisy, pericarditis
- superior vena cava syndrome (pain, dysphagia, dyspnea, orthopnea, swelling of
the neck, face and upper limbs)
- CNS damage -10% of cases
Laboratory
357
- node biopsy: essential for diagnosis - complete blood count
- assessment of liver and kidney function; LDH - ionogram
- infectious profile: anti HIV Atb, hepatitis A and B, C, CMV, varicella
- CSF examination: CNS involvement - BM test
- chest Rx and CT - abdominal ultrasound
- bone scan - PET / CT
Diagnosis: based on histopathological examination with CD45 positivity (LCA = leucocyte
common antigen) the haematological origin of the tumor may be proved
Staging
Stage I
A single extranodal tumor or single node region, except for the abdomen and
mediastinum
Stage II
Single extranodal tumor with regional lymph node involvement;
On the same side of the diaphragm: 2 or more lymph node regions, 2 extranodal tumors
with nodal involvement
Completely resectable primary gastrointestinal tumor, nodal involvement
Stage III
On both sides of the diaphragm: 2 extranodal tumors, two or more lymph node
regions
All primary chest tumors (mediastinal, pleura, thymus)
All abdominal tumors are extended, inoperable
All of primary tumors are para-spinal or epidural
Stage IV
CNS or BM symptoms (> 25%)
Differential diagnosis
- localized infectious adenopathies
- mediastinal and abdominal masses: neuroblastoma, Wilms tumor
- bone tumors in case of primary bone location
- brain tumors if HIC phenomena or paralysis of cranial nerves appear.
Treatment
Emergency treatment: is often necessary since the tumors grow rapidly; the symptoms are
caused by compression of organs or metabolic disturbances. Mediastinal tumors cause
tracheal compression, pericarditis, pericardial tamponade, superior vena cava compression.
358
Abdominal tumors cause intestinal obstruction, ureteral compression, bleeding and severe
metabolic disorders: tumor lysis syndrome and acute renal failure. CNS location can produce
convulsions, paraplegia, paralysis of cranial nerves, meningeal irritation.
Chemotherapy: because of many complications that can occur at the beginning of treatment,
it begins in an intensive care unit, even if the patient's condition is satisfactory.
- Lymphoblastic lymphoma: chemotherapy according to protocols for lymphoblastic
ALL
- Burkitt lymphoma (BL): treatment is shorter and more intensive - cytotoxic blocks
administered every two weeks
- Large B-cell lymphoma (ALCL) identical with LB treatment
Supportive hematologic treatment: identical to ALL support therapy
Prognosis: depends on the stage of disease, histological and genetic appearance; 3 years
survival in stage I and II - 90-95% in stage III - 86% in stage IV - 75%.
SOLID TUMORS
NEUROBLASTOMA
Epidemiology:
8% of child malignancies; 28-39% of newborn malignancies; average age of neuroblastoma
diagnosis - 2 years, 90% of cases are diagnosed under 5 years; higher frequency in males and
in white patients. Evolution is unique and can present spontaneous regression, especially in
infants in stages 1 and 4S of the disease.
Etiology: unknown.
- risk factors: intrauterine exposure to alcohol, drugs, hormones, hair dyes
- association with other neural crest cell disorders: neurofibromatosis, B.Hirschprung
Syndrome, DiGeorge Syndrome, Beckwith-Wiedemann Syndrome.
- Neuroblastoma cells: chromosomal changes (deletion of the short arm of chromosome
1), in advanced forms and unfavorable prognosis
- amplification of n-myc proto-oncogenes (oncogene located on the short arm of
chromosome 2) indicates poor prognosis.
Clinical features: appears to be a tumor on the sympathetic chain; the symptoms are
polymorphic, according to symptom location and neuroendocrine symptomatology of the
tumor.
359
1. Simptoms given by the tumor mass
- abdominal location: localized abdominal pain, abdominal distension, constipation,
palpable abdominal tumor exceeding midline
- chest location: dyspnoea, cough, or discovered by chance
- cervical location: severe dyspnea, difficult swallowing, Horner syndrome (miosis,
enophthalmos, palpebral ptosis, iris heterochromia of the affected side)
- pelvic location: difficulty in defecation and urination
- paramedular and intramedular locations: pain in the spine, sphincter dysfunction, gait
disturbances, paresis (due to compression)
2. Paraneoplastic syndrome
- symptoms due to hypersecretion of catecholamines: hypertension, tachycardia, fever,
sweating, paleness, headache, increased urinary excretion of degradation products:
Vanilmandelic acid, homovanillic acid
- symptoms due to hypersecretion of intestinal vasoactive peptide: diarrhea
unresponsive to treatment, abdominal distention, hypokalemia
- acute myoclonic encephalopathy (rare): myoclonus, opsoclonus (sudden movements
of the eyes), trunk ataxia, head restlessness
- manifestations due to metastatic locations: adenopathy, hepatomegaly, brain
metastases, bone marrow, skin (bluish skin nodules only in babies)
- nonspecific signs: lethargy, anorexia, pallor, weight loss, abdominal pain, irritability
Laboratory
- CBC: anemia and thrombocytosis; cytopenia in case of medullar metastasis
- serum ferritin, LDH, ESR, neuron specific enolase - usually high
- Vanil-mandelic acid (VMA) of 24-hour urine high
- aspirate / bone marrow biopsy metastasis bilaterally: tumor cells similar to
lymphoblasts in nest locations
- chest radiography: mass in the posterior mediastinum: calcifications in the tumor
(pathognomonic for neuroblastoma)
- abdominal ultrasound
- thorax, abdomen, pelvis CT: extension of the tumor, metastases, calcifications
MRI: para-vertebral tumor; bone metastases
bone scintigraphy (MIBG, Tc-99): bone metastases
PET / CT
Positive diagnosis
360
Obligatory elements for positive diagnosis (INSS recommendation)
- presence of neuroblasts in primary tumor with characteristic histologic picture
- in the bone marrow: neuroblast nests and / or high level of blood catecholamine or urine
metabolites
Staging
Stage I: localized tumor, completely resectable.
Stage IIA: localized tumor with incomplete resection, ipsia and controlateral lymph nodes are
microscopically negative.
Stage IIB: localized tumor with complete or partial resection, positive ipsilateral node and
negative controlateral node.
Stage III: inoperable tumor beyond the midline with or without lymph node involvement.
Stage IV: distant metastases: in the removed lymphnodes, liver, bone, bone marrow, skin and
other organs.
Stage IVS: localized primary tumor (Ist or IInd degree) with metastases in the skin, liver,
bone marrow in children under 1 year of age.
Differential diagnosis
- other abdominal masses: Wilms tumors, ovarian germ tumors, rabdomiosarcoamas,
lymphomas
- fecaloma from constipation
- intestinal duplication
Treatment
Surgical excision: the localized disease: curative excision; in metastatic disease: "second
look" surgery
Chemotherapy: preoperative and postoperative
Autologous bone marrow transplantation: stage IV and age over 1 year; n-myc gene
amplification irrespective of the stage
Radiotherapy
Pprognosis: according to stage, genetic and age modifications; survival in patients under one
year of age: 75% and only 25% in patients over one year.
NEPHROBLASTOMA (WILMS TUMOR)
Epidemiology:
361
The most common malignant renal tumor that occurs only in childhood, most commonly in
the age group of 1-5 years; 5-6% of child malignancies, with an incidence of 1: 10,000 in
newborns and equal frequency in both sexes. In 10% of cases it is bilateral. It is commonly
associated with aniridia and genitourinary malformations.
Etiology: unknown; cases occur mostly in young children with genetic anomalies or
familial predisposition, but there are sporadic forms as well. It is a mixt embryonic kidney
neoplasm formed of 3 components: blastemal, stromal and epithelial. The gene responsible
for Wilms tumor is located on chromosome 11.
Clinical features
- abdominal tumor located on a flank; it does not exceed the midline, and is not
breathing-mobile
- abdominal pain, vomiting
- fever, weight loss
- micro / macroscopic hematuria, rarely dysuria, polyuria
- moderate hypertension in 75% of cases (through increased release of renin by the
kidney tumor or compressed kidney tissue)
- metastases are produced by local extension or by hematogenous way: tumor invasion
of the renal vein and inferior vena cava; heart, lung; liver.
Laboratory
- Blood count: anemia - Urine test: haematuria, urinary tract infection
- LDH, elevated ESR - Urea, creatinine - usually normal
- Cytogenetic exam
- Histopathology: favorable histology (90%), unfavorable histology (anaplastic and
sarcoma with clear cells) (10%).
- Abdominal ultrasound: highlights renal tumor; possibly liver metastases, in the
inferior vena cava or lymph nodes
- AP and LL chest Rx: presence of metastases
- Abdominal CT: evidence of Wilms tumor as heterogeneous mass, with intratumoral
necrosis contrast
- Bone scan, MRI and / or head CT: for head or bone metastases in forms with
unfavorable histology
Differential diagnosis
- Non-neoplastic renal masses: hidronefrotic kidney, polycystic kidney, renal
hematoma
362
- Neuroblastoma: tumor mass that displaces the kidney, exceeds the median line;
increased AVM
- Hepatoblastoma, lymphomas
- Splenomegaly
- intestinal tumor
Staging of Wilms tumor
Stage I: completely resectable intrarenal tumor
Stage II: The tumor destroys the renal capsule; peri-renal extension but completely
resectable. Regional lymph nodes are negative
Stage III: macroscopic or microscopic residue after tumor removal,
tumor-infiltrated regional lymph nodes
Stage IV: presence of distant metastases (hematogenous) in the lungs, brain, bone, liver.
Stage V: bilateral tumor.
Treatment
Surgical treatment: formation resection in an oncologic surgical department; if the inferior
vena cava is invaded, chemotherapy and then resection are performed
Chemotherapy: preoperative and postoperative
Radiotherapy: for stages III and IV and forms with unfavorable histology
Prognosis: depends on the initial tumor staging, histological type and treatment; the chance
of survival in 90% of cases.
References:
1. Baghiu Maria Despina, Horvath Adriennne. Hematologie, oncologie i endocrinologie pediatric. Note de
curs pentru medici rezideni. Litografia UMF Trgu Mure, 2007
2. Lanzkowsky P. Manual of Pediatric Hematology and Oncology, 4th edition. Elsevier, 2005
3. Muntean I i colab. Vademecum de pediatrie. Ed.Medical Bucureti, 2007
4. Pinkerton Ross, Shankar A.G, Matthay Katherine. Evidence-based pediatric oncology. 2th edition;
Blackwell Publishing, 2007
You might also like
- Nursing School Necessities Cheat SheetDocument3 pagesNursing School Necessities Cheat SheetRevNo ratings yet
- Pediatrics 5 Minute ReviewDocument206 pagesPediatrics 5 Minute ReviewMarius CreangaNo ratings yet
- Start and Run Sandwich and Coffee Shops PDFDocument193 pagesStart and Run Sandwich and Coffee Shops PDFsap7e88% (8)
- MediterraneanDocument39 pagesMediterraneanJeff Lester PiodosNo ratings yet
- Paediatric Emergency PortocolDocument106 pagesPaediatric Emergency Portocolمحمد عبد القاهر السروريNo ratings yet
- General PediatricsDocument21 pagesGeneral PediatricsShanmugam Balasubramaniam100% (2)
- Radiation Protection 2018Document213 pagesRadiation Protection 2018Ricardo EdanoNo ratings yet
- Pocketbook WHO PediatricsDocument398 pagesPocketbook WHO PediatricsNashria RusdhyNo ratings yet
- Pediatric Antibiotic Dosing Card 2012Document2 pagesPediatric Antibiotic Dosing Card 2012yoshilimsiacoshigyoNo ratings yet
- Pediatrics - Michael GrantDocument78 pagesPediatrics - Michael GrantPappitha RajaNo ratings yet
- Neonatal Cholestasis: Priyanka VishwakarmaDocument38 pagesNeonatal Cholestasis: Priyanka VishwakarmaAlex100% (1)
- Hot Topics of Pediatrics (Muhadharaty) PDFDocument577 pagesHot Topics of Pediatrics (Muhadharaty) PDFdr.sasikumarNo ratings yet
- Endocrine Surgery: Butterworths International Medical Reviews: SurgeryFrom EverandEndocrine Surgery: Butterworths International Medical Reviews: SurgeryI. D. A. JohnstonNo ratings yet
- PEDIATRIC GROWTH CHART AND DRUG DOSING REFERENCEDocument9 pagesPEDIATRIC GROWTH CHART AND DRUG DOSING REFERENCEjandale100% (1)
- Pediatric Emergencies 2015Document90 pagesPediatric Emergencies 2015tatiana feliciaNo ratings yet
- Drug Master FileDocument62 pagesDrug Master FileAjay GuptaNo ratings yet
- Neonatology Cambridge Pocket ClinicianDocument601 pagesNeonatology Cambridge Pocket Clinicianjuanse1994No ratings yet
- RopDocument172 pagesRopMurali Krishna DNo ratings yet
- Surgical Instruments and Drains PDFDocument117 pagesSurgical Instruments and Drains PDFNariska CooperNo ratings yet
- Paediatric and Neonatal Critical Care Transport: Edited by Peter Barry and Andrew LeslieDocument161 pagesPaediatric and Neonatal Critical Care Transport: Edited by Peter Barry and Andrew Lesliewifi idyuNo ratings yet
- Neonatal Diseases PDFDocument41 pagesNeonatal Diseases PDFmomobelle100% (1)
- Clinical Approach To Syncope in ChildrenDocument6 pagesClinical Approach To Syncope in ChildrenJahzeel Gacitúa Becerra100% (1)
- Pediatric Diagnosis PedDocument153 pagesPediatric Diagnosis PedIceNo ratings yet
- Ricoh Ap610 Service ManualDocument298 pagesRicoh Ap610 Service Manualuzed4serviceNo ratings yet
- Paediatric AsthmaDocument246 pagesPaediatric AsthmaOxana TurcuNo ratings yet
- An III - Pediatrie - C2Document9 pagesAn III - Pediatrie - C2Cristiana Ionescu RoteaNo ratings yet
- BCSC Reading Schedule 2019-2020Document11 pagesBCSC Reading Schedule 2019-2020Mari Martinez100% (1)
- Pediatrics (Toronto Notes For PDA 2004)Document70 pagesPediatrics (Toronto Notes For PDA 2004)Worawut PhromwangNo ratings yet
- Pediatric Nutrition Handbook: An Algorithmic ApproachFrom EverandPediatric Nutrition Handbook: An Algorithmic ApproachDavid SuskindNo ratings yet
- Kuwait Pediatric GuideLinesDocument124 pagesKuwait Pediatric GuideLinesemicurudimov100% (1)
- Rwanda Paediatric Emergencies GuidelinesDocument244 pagesRwanda Paediatric Emergencies GuidelinesAmber MonroeNo ratings yet
- The Children's Hospital of Philadelphia Guide to Asthma: How to Help Your Child Live a Healthier LifeFrom EverandThe Children's Hospital of Philadelphia Guide to Asthma: How to Help Your Child Live a Healthier LifeJulian Lewis Allen, M.D.No ratings yet
- Division of Perinatology Department of Child Health Medical School University of Sumatera UtaraDocument37 pagesDivision of Perinatology Department of Child Health Medical School University of Sumatera UtaraJosephine IrenaNo ratings yet
- Recommendation WHODocument176 pagesRecommendation WHODananjaya JuniorNo ratings yet
- Interpretare ASTRUPDocument2 pagesInterpretare ASTRUPMaximillian Bogdan100% (1)
- Guidelines for Competency Based Training in Pediatric GastroenterologyDocument26 pagesGuidelines for Competency Based Training in Pediatric GastroenterologysenthiljayanthiNo ratings yet
- Boli Eruptive ViraleDocument83 pagesBoli Eruptive ViraleNagy Eva100% (3)
- Pediatrie FinalDocument79 pagesPediatrie Finallordrip100% (5)
- PQCNC 2023 Standardizing The Care of Late-Preterm InfantsDocument17 pagesPQCNC 2023 Standardizing The Care of Late-Preterm InfantskcochranNo ratings yet
- Prem Puri: EditorDocument1,276 pagesPrem Puri: EditorGuillermos Rivera100% (1)
- Cognidox - A Complete Guide To Medical Device DevelopmentDocument38 pagesCognidox - A Complete Guide To Medical Device DevelopmentcivicbladeNo ratings yet
- Global Guidelines For The Prevention of Surgical Site InfectionDocument186 pagesGlobal Guidelines For The Prevention of Surgical Site InfectionLe Ngoc Quynh GiaoNo ratings yet
- Prezentare de CazDocument9 pagesPrezentare de CazDan Cristian100% (1)
- PM.M., 8 ani, cu otita medie acuta si adenopatie laterocervicalaDocument6 pagesPM.M., 8 ani, cu otita medie acuta si adenopatie laterocervicalaRolandNo ratings yet
- Tratat Elementat de Pediatrie PDFDocument43 pagesTratat Elementat de Pediatrie PDFRusu Bianca ElenaNo ratings yet
- Ingrijirea Si Alimentatia Prematurului Si Nou-Nascutului Cu Greutate MicaDocument13 pagesIngrijirea Si Alimentatia Prematurului Si Nou-Nascutului Cu Greutate MicaRoxana Gabor100% (1)
- Anatomie PatologicaDocument107 pagesAnatomie PatologicaGabriela PicioreaNo ratings yet
- CamScanner Document ScansDocument80 pagesCamScanner Document ScansAvarvarei Moisa RalucaNo ratings yet
- Diabesity: A New Paradigm of Metabolic ConnexionDocument37 pagesDiabesity: A New Paradigm of Metabolic ConnexionatezorNo ratings yet
- Memomed 2023Document17 pagesMemomed 2023Anamaria Rizac60% (5)
- Varicela, herpes zoster - infectii virale cu exantem cutanatDocument63 pagesVaricela, herpes zoster - infectii virale cu exantem cutanatRegele BrânzăNo ratings yet
- Sindroamele HemoragiceDocument5 pagesSindroamele HemoragiceIoana GalNo ratings yet
- Reflux Gastro Esofagian in PediatrieDocument6 pagesReflux Gastro Esofagian in PediatrieAnca HudisteanuNo ratings yet
- Curs An Iii Puericultura, Pediatrie Si Nursing Specific-10Document11 pagesCurs An Iii Puericultura, Pediatrie Si Nursing Specific-10Cristian NastaseNo ratings yet
- Valori Normale in PediatrieDocument8 pagesValori Normale in PediatrieAlexandra VastagNo ratings yet
- Travel Guide Provides Essential Medical Contact InformationDocument211 pagesTravel Guide Provides Essential Medical Contact InformationRegarde Le Ciel Ici0% (1)
- Caz ClinicDocument4 pagesCaz ClinicAna-MariaCioti100% (1)
- Icter - Definitii Si EtiologieDocument60 pagesIcter - Definitii Si EtiologieAlexandraNo ratings yet
- Pediatrics National Clinical Treatment Guideline Ok Version After CorrectionsDocument176 pagesPediatrics National Clinical Treatment Guideline Ok Version After CorrectionsmomocamuiNo ratings yet
- 530 PediatrieDocument128 pages530 PediatrieAnaCereteu100% (1)
- Cow's Milk Protein AllergyDocument46 pagesCow's Milk Protein AllergyChyntia PutriNo ratings yet
- 7 Sindromul Klippel TrenaunayDocument5 pages7 Sindromul Klippel TrenaunayCosmin NicolescuNo ratings yet
- Diarrhea (Ped) DDX - Gastroenteritis - Food Poisoning - Uti - Uri - Cow Milk Protein Allergy Dopcsfaaa AbcoDocument34 pagesDiarrhea (Ped) DDX - Gastroenteritis - Food Poisoning - Uti - Uri - Cow Milk Protein Allergy Dopcsfaaa AbcofeawefNo ratings yet
- Recommended BooksDocument2 pagesRecommended BooksVijayakanth VijayakumarNo ratings yet
- PAEDIATRICS Notes 3 Update PDFDocument69 pagesPAEDIATRICS Notes 3 Update PDFMateen ShukriNo ratings yet
- Chapter4 Infant Formula FeedingDocument20 pagesChapter4 Infant Formula FeedingMuhammad AbdulazizNo ratings yet
- Short StatureDocument36 pagesShort StatureAldho BramantyoNo ratings yet
- Handbook of Paediatrics - StudentDocument21 pagesHandbook of Paediatrics - StudentayunisallehNo ratings yet
- Anemia AplastikDocument33 pagesAnemia AplastikEvelin SimarmataNo ratings yet
- Ricoh Aficio MP 3500-4500 Network GuideDocument134 pagesRicoh Aficio MP 3500-4500 Network GuideRobinNo ratings yet
- Reversing Heart DiseaseDocument673 pagesReversing Heart DiseasecubixmuresNo ratings yet
- Ricoh 3035 3045 - Complete ManualDocument922 pagesRicoh 3035 3045 - Complete ManualSMART REFILL71% (7)
- Service Manual MP 9000Document1,254 pagesService Manual MP 9000cubixmures75% (4)
- Parts Guide Manual: Bizhub 420/bizhub 500Document152 pagesParts Guide Manual: Bizhub 420/bizhub 500George ConstantinoiuNo ratings yet
- Skill 10 (1) ..Throat CultureDocument1 pageSkill 10 (1) ..Throat Culturenetsquad100% (1)
- Girlshare - Ro - Minolta CF2002, CF3102 Service ManualDocument298 pagesGirlshare - Ro - Minolta CF2002, CF3102 Service ManualwilbingNo ratings yet
- Does It Worth? Does It Worth? Does It Worth? Does It Worth?: Gergely Éva ArankaDocument72 pagesDoes It Worth? Does It Worth? Does It Worth? Does It Worth?: Gergely Éva ArankacubixmuresNo ratings yet
- Ulrich Merzenich2007Document13 pagesUlrich Merzenich2007oka samiranaNo ratings yet
- CementumDocument26 pagesCementumPrathik RaiNo ratings yet
- Declaration of Erin EllisDocument4 pagesDeclaration of Erin EllisElizabeth Nolan BrownNo ratings yet
- Hand Injuries & Their ManagementsDocument78 pagesHand Injuries & Their ManagementsKuruNo ratings yet
- 116 Draft OilsDocument233 pages116 Draft OilsMarcela Paz Gutierrez UrbinaNo ratings yet
- New TNMDocument157 pagesNew TNMShouvik ChowdhuryNo ratings yet
- Multicontrol Level 2: Cat. No. Pack Name Packaging (Content)Document2 pagesMulticontrol Level 2: Cat. No. Pack Name Packaging (Content)NonameNo ratings yet
- Study Data Reviewer's Guide: LDCP, Inc. Study LDCP-0242-005Document16 pagesStudy Data Reviewer's Guide: LDCP, Inc. Study LDCP-0242-005anon_181306460No ratings yet
- Work Authorization Permit.Document1 pageWork Authorization Permit.Gabriel TanNo ratings yet
- Certification of Psychology Specialists Application Form: Cover PageDocument3 pagesCertification of Psychology Specialists Application Form: Cover PageJona Mae MetroNo ratings yet
- Civil Tender Volume-1Document85 pagesCivil Tender Volume-1Aditya RaghavNo ratings yet
- From Solidarity To Subsidiarity: The Nonprofit Sector in PolandDocument43 pagesFrom Solidarity To Subsidiarity: The Nonprofit Sector in PolandKarimMonoNo ratings yet
- Pulse Oximetry: Review Open AccessDocument7 pagesPulse Oximetry: Review Open AccessAlain SoucotNo ratings yet
- C & W Meat Packers Carly Courtney Cynthiana KY Notice of Suspension Humane Treatment LivestockDocument4 pagesC & W Meat Packers Carly Courtney Cynthiana KY Notice of Suspension Humane Treatment LivestockghostgripNo ratings yet
- Marriage and Later PartDocument25 pagesMarriage and Later PartDeepak PoudelNo ratings yet
- Herbal Toothpaste FactsDocument26 pagesHerbal Toothpaste Factsmahek_dhootNo ratings yet
- 2017EffectofConsumptionKemuningsLeafMurrayaPaniculataL JackInfusetoReduceBodyMassIndexWaistCircumferenceandPelvisCircumferenceonObesePatientsDocument5 pages2017EffectofConsumptionKemuningsLeafMurrayaPaniculataL JackInfusetoReduceBodyMassIndexWaistCircumferenceandPelvisCircumferenceonObesePatientsvidianka rembulanNo ratings yet
- Improving Healthcare Quality in IndonesiaDocument34 pagesImproving Healthcare Quality in IndonesiaJuanaNo ratings yet
- Chronic Cough in Dogs: Published With The Permission of LAVC Close Window To Return To IVISDocument4 pagesChronic Cough in Dogs: Published With The Permission of LAVC Close Window To Return To IVISJuanEstebanOspinaNo ratings yet
- Women in Leadership - South West Conference 2019Document24 pagesWomen in Leadership - South West Conference 2019Gareth NoyesNo ratings yet
- List of 220KV Grid Stations-NTDCDocument7 pagesList of 220KV Grid Stations-NTDCImad Ullah0% (1)