Professional Documents
Culture Documents
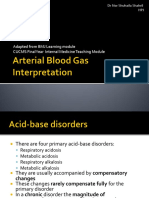
Interpretation of Arterial Blood Gases
Uploaded by
Elisha RosalynCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Interpretation of Arterial Blood Gases
Uploaded by
Elisha RosalynCopyright:
Available Formats
Interpretation of Arterial Blood Gases (ABGs) David A.
Kaufman, MD Chief, Section of Pulmonary, Critical Care & Sleep Medicine Bridgeport Hospital-Yale New Haven Health Assistant Clinical Professor, Yale University School of Medicine (Section of Pulmonary & Critical Care Medicine) Introduction:
Interpreting an arterial blood gas (ABG) is a crucial skill for physicians, nurses, respiratory therapists, and other health care personnel. ABG interpretation is especially important in critically ill patients. The following six-step process helps ensure a complete interpretation of every ABG. In addition, you will find tables that list commonly encountered acidbase disorders. Many methods exist to guide the interpretation of the ABG. This discussion does not include some methods, such as analysis of base excess or Stewarts strong ion difference. A summary of these techniques can be found in some of the suggested articles. It is unclear whether these alternate methods offer clinically important advantages over the presented approach, which is based on the anion gap. Readers are welcome to discuss their observations and share their comments on the ATS Critical Care Forums.
6-step approach: Step 1: Assess the internal consistency of the values using the Henderseon-Hasselbach equation: [H+] = 24(PaCO2) [HCO3-] If the pH and the [H+] are inconsistent, the ABG is probably not valid.
pH
Approximate [H+] (mmol/L) 100 89 79 71 63 56 50 45
7.00 7.05 7.10 7.15 7.20 7.25 7.30 7.35
7.40 7.45 7.50 7.55 7.60 7.65
Step 2: Is there alkalemia or acidemia present?
40 35 32 28 25 22
pH < 7.35 acidemia pH > 7.45 alkalemia
You will need to check the PaCO2, HCO3- and anion gap Step 3: Is the disturbance respiratory or metabolic? What is the relationship between the direction of change in the pH and the direction of change in the PaCO2? In primary respiratory disorders, the pH and PaCO2 change inopposite directions; in metabolic disorders the pH and PaCO2 change in the same direction.
This is usually the primary disorder Remember: an acidosis or alkalosis may be present even if the pH is in the normal range (7.35 7.45)
Acidosis Acidosis Alkalosis Alkalosis
Respiratory Metabolic& Respiratory Metabolic
pH pH pH pH
PaCO2 PaCO2 PaCO2 PaCO2
Step 4: Is there appropriate compensation for the primary disturbance? Usually, compensation does not return the pH to normal (7.35 7.45).
Disorder
Expected compensation
Correction factor
Metabolic acidosis
PaCO2 = (1.5 x [HCO3-]) +8
Acute respiratory acidosis
Increase in [HCO3-]= PaCO2/10
Chronic respiratory acidosis (3-5 days)
Increase in [HCO3-]= 3.5( PaCO2/10)
Metabolic alkalosis
Increase in PaCO2 = 40 + 0.6(HCO3-)
Acute respiratory alkalosis
Decrease in [HCO3-]= 2( PaCO2/10)
Chronic respiratory alkalosis
Decrease in [HCO3-] = 5( PaCO2/10) to 7( PaCO2/10)
If the observed compensation is not the expected compensation, it is likely that more than one acid-base disorder is present. Step 5: Calculate the anion gap (if a metabolic acidosis exists): AG= [Na+]-( [Cl-] + [HCO3-] )-12 2
A normal anion gap is approximately 12 meq/L. In patients with hypoalbuminemia, the normal anion gap is lower than 12 meq/L; the normal anion gap in patie nts with hypoalbuminemia is about 2.5 meq/L lower for each 1 gm/dL decrease in the plasma albumin concentration (for example, a patient with a plasma albumin of 2.0 gm/dL would be approximately 7 meq/L.) If the anion gap is elevated, consider calculating the osmolal gap in compatible clinical situations.
Elevation in AG is not explained by an obvious case (DKA, lactic acidosis, renal failure Toxic ingestion is suspected
OSM gap = measured OSM (2[Na+] - glucose/18 BUN/2.8
The OSM gap should be < 10 Step 6: If an increased anion gap is present, assess the relationship between the increase in the anion gap and the decrease in [HCO 3-].
Assess the ratio of the change in the anion gap (AG ) to the change in [HCO3-] ([HCO3-]): AG/[HCO3-] This ratio should be between 1.0 and 2.0 if an uncomplicated anion gap metabolic acidosis is present. If this ratio falls outside of this range, then another metabolic disorder is present:
If AG/[HCO3-] > 2.0, then a concurrent metabolic alkalosis is likely to be present. It is important to remember what the expected normal anion gap for your patient should be, by adjusting for hypoalbuminemia (see Step 5, above.) Table 1: Characteristics of acid-base disturbances
If AG/[HCO3-] < 1.0, then a concurrent non-anion gap metabolic acidosis is likely to be present.
Disorder
pH
Primary problem
Compensation
Metabolic acidosis
in HCO3-
in PaCO2
Metabolic alkalosis
in HCO3-
in PaCO2
Respiratory acidosis
in PaCO2
in [HCO3-]
Respiratory alkalosis
in PaCO2
in [HCO3-]
Table 2: Selected etiologies of respiratory acidosis
Airway obstruction - Upper - Lower
COPD asthma other obstructive lung disease
CNS depression Sleep disordered breathing (OSA or OHS) Neuromuscular impairment Ventilatory restriction Increased CO2 production: shivering, rigors, seizures, malignant hyperthermia, hypermetabolism, increased intake of carbohydrates
Incorrect mechanical ventilation settings Table 3: Selected etiologies of respiratory alkalosis
CNS stimulation: fever, pain, fear, anxiety, CVA, cerebral edema, brain trauma, brain tumor, CNS infection Hypoxemia or hypoxia: lung disease, profound anemia, low FiO2 Stimulation of chest receptors: pulmonary edema, pleural effusion, pneumonia, pneumothorax, pulmonary embolus Drugs, hormones: salicylates, catecholamines, medroxyprogesterone, progestins Pregnancy, liver disease, sepsis, hyperthyroidism
Incorrect mechanical ventilation settings Table 4: Selected causes of metabolic alkalosis
Hypovolemia with Cl- depletion
GI loss of H+
Vomiting, gastric suction, villous adenoma, diarrhea with chloride-rich fluid
Renal loss H+ Loop and thiazide diuretics, post-hypercapnia (especially after institution of mechanical ventilation)
Hypervolemia, Cl- expansion
Renal loss of H+: edematous states (heart failure, cirrhosis, nephrotic syndrome), hyperaldosteronism, hypercortisolism, excess ACTH, exogenous steroids, hyperreninemia, severe hypokalemia, renal artery stenosis, bicarbonate administration Table 5: Selected etiologies of metabolic acidosis
Elevated anion gap:
Methanol intoxication Uremia Diabetic ketoacidosisa, alcoholic ketoacidosis, starvation ketoacidosis Paraldehyde toxicity Isoniazid Lactic acidosisa
Type A: tissue ischemia Type B: Altered cellular metabolism
Ethanolb or ethylene glycolb intoxication
a b
Salicylate intoxication Most common causes of metabolic acidosis with an elevated anion gap Frequently associated with an osmolal gap
Normal anion gap: will have increase in [Cl-]
GI loss of HCO3-
Diarrhea, ileostomy, proximal colostomy, ureteral diversion
Renal loss of HCO3proximal RTA carbonic anhydrase inhibitor (acetazolamide)
Renal tubular disease ATN Chronic renal disease Distal RTA Aldosterone inhibitors or absence
NaCl infusion, TPN, NH4+ administration Table 6: Selected mixed and complex acid-base disturbances
Disorder
Characteristics
Selected situations
Respiratory acidosis with metabolic acidosis
in pH in HCO3 in PaCO2
Cardiac arrest Intoxications Multi-organ failure
Respiratory alkalosis with metabolic alkalosis
in pH in HCO3 in PaCO2
Cirrhosis with diuretics Pregnancy with vomiting Over ventilation of COPD
Respiratory acidosis with metabolic alkalosis
pH in normal range in PaCO2, in HCO3-
COPD with diuretics, vomiting, NG suction Severe hypokalemia
Respiratory alkalosis with metabolic acidosis
pH in normal range in PaCO2 in HCO3
Sepsis Salicylate toxicity Renal failure with CHF or pneumonia Advanced liver disease
Metabolic acidosis with metabolic alkalosis
pH in normal range HCO3- normal
Uremia or ketoacidosis with vomiting, NG suction, diuretics, etc.
Suggested additional reading:
Rose, B.D. and T.W. Post. Clinical physiology of acid-base and electrolyte disorders, 5th ed. New York: McGraw Hill Medical Publishing Division, c2001. Fidkowski, C And J. Helstrom. Diagnosing metabolic acidosis in the critically ill: bridging the anion gap, Stewart and base excess methods. Can J Anesth 2009;56:247-256. Adrogu, H.J. and N.E. Madias. Management of life-threatening acid-base disordersfirst of two parts. N Engl J Med 1998;338:26-34. Adrogu, H.J. and N.E. Madias. Management of life-threatening acid-base disorderssecond of two parts. N Engl J Med 1998;338:107-111.
You might also like
- Bahan Telaah Ilmiah MataDocument2 pagesBahan Telaah Ilmiah MataElisha RosalynNo ratings yet
- Dapus Lapsus Dr. RIDocument1 pageDapus Lapsus Dr. RIElisha RosalynNo ratings yet
- Irregular Verb .... BDocument1 pageIrregular Verb .... BElisha RosalynNo ratings yet
- Cover PhantomDocument1 pageCover PhantomElisha RosalynNo ratings yet
- Effects of Serving High Sugar Cereals On Children's Breakfast-Eating BehaviourDocument1 pageEffects of Serving High Sugar Cereals On Children's Breakfast-Eating BehaviourElisha RosalynNo ratings yet
- Daftar Pustaka MataDocument1 pageDaftar Pustaka MataElisha RosalynNo ratings yet
- Tugas Air Pollution IndexDocument7 pagesTugas Air Pollution IndexElisha RosalynNo ratings yet
- Effects of Serving High Sugar Cereals On Children's Breakfast-Eating BehaviourDocument1 pageEffects of Serving High Sugar Cereals On Children's Breakfast-Eating BehaviourElisha RosalynNo ratings yet
- Translate TugasDocument2 pagesTranslate TugasElisha RosalynNo ratings yet
- AQHI System Explained in DetailDocument10 pagesAQHI System Explained in DetailElisha RosalynNo ratings yet
- Cover PhantomDocument1 pageCover PhantomElisha RosalynNo ratings yet
- Irregular VerbDocument3 pagesIrregular VerbElisha RosalynNo ratings yet
- Bahan HepatitisDocument11 pagesBahan HepatitisElisha RosalynNo ratings yet
- Epidemiologi OnikomikosisDocument2 pagesEpidemiologi OnikomikosisElisha RosalynNo ratings yet
- Case FixDocument31 pagesCase FixElisha RosalynNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaElisha RosalynNo ratings yet
- Cover GuidelineDocument1 pageCover GuidelineElisha RosalynNo ratings yet
- Bahan Partus KasepDocument1 pageBahan Partus KasepElisha RosalynNo ratings yet
- How To Insert A Central Line'Document6 pagesHow To Insert A Central Line'Elisha RosalynNo ratings yet
- Cover GuidelineDocument1 pageCover GuidelineElisha RosalynNo ratings yet
- Congenital Talipes Equinovarus 222Document9 pagesCongenital Talipes Equinovarus 222Elisha RosalynNo ratings yet
- Daftar Pustaka Kak BojesDocument2 pagesDaftar Pustaka Kak BojesElisha RosalynNo ratings yet
- Child Pugh ScoreDocument1 pageChild Pugh ScoreElisha RosalynNo ratings yet
- Child Pugh ScoreDocument1 pageChild Pugh ScoreElisha RosalynNo ratings yet
- AutopsyDocument8 pagesAutopsyElisha RosalynNo ratings yet
- Immunodeficiency References ListDocument1 pageImmunodeficiency References ListElisha RosalynNo ratings yet
- Disorders of the immune system explainedDocument2 pagesDisorders of the immune system explainedElisha RosalynNo ratings yet
- Peripheral Block For Hand SurgeryDocument1 pagePeripheral Block For Hand SurgeryElisha RosalynNo ratings yet
- Peripheral Block For Hand SurgeryDocument1 pagePeripheral Block For Hand SurgeryElisha RosalynNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Acute. KetoacidosisdocxDocument12 pagesAcute. KetoacidosisdocxShara SampangNo ratings yet
- ABG Cases Rev 2.0Document10 pagesABG Cases Rev 2.0Maram AbdullahNo ratings yet
- Metabolic AcidosisDocument6 pagesMetabolic AcidosisMustafa Cuneyt GezenNo ratings yet
- RTA Types NidisaaDocument16 pagesRTA Types NidisaaNidisaaNo ratings yet
- Acid Base BalanceDocument104 pagesAcid Base BalanceKevin VillaranteNo ratings yet
- American Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)Document7 pagesAmerican Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)humberto_2No ratings yet
- 01 Lactic AcidosisDocument23 pages01 Lactic Acidosishanady alsnedNo ratings yet
- Guideline ADA 2010 in Hyperglicemia CrisisDocument9 pagesGuideline ADA 2010 in Hyperglicemia CrisisAissyiyah Nur An NisaNo ratings yet
- Inborn Errors of Metabolism in Infancy: A Guide To DiagnosisDocument11 pagesInborn Errors of Metabolism in Infancy: A Guide To DiagnosisEdu Diaperlover São PauloNo ratings yet
- Clinical Chemistry Tests and ConceptsDocument23 pagesClinical Chemistry Tests and ConceptsMISS RMTNo ratings yet
- Acid-Base TutorialDocument20 pagesAcid-Base Tutorialomar ahmedNo ratings yet
- Acid-Base Metabolism Disorders and PhysiologyDocument88 pagesAcid-Base Metabolism Disorders and PhysiologydrToikNo ratings yet
- Acid-Base Balance and DisodersDocument86 pagesAcid-Base Balance and DisodersPrincewill SeiyefaNo ratings yet
- 02 26 CCDocument5 pages02 26 CCJeanel SamonteNo ratings yet
- Abg by DR Manna, Department of Emergency Medicine, Amrita Institute of Medical Sceinces, Kochi, KeralaDocument50 pagesAbg by DR Manna, Department of Emergency Medicine, Amrita Institute of Medical Sceinces, Kochi, KeralaAETCM Emergency medicine100% (1)
- Clinical Chemistry I: Tests, Disorders & Lab TechniquesDocument34 pagesClinical Chemistry I: Tests, Disorders & Lab TechniquesCoțovanu IulianNo ratings yet
- Jurnal Kad Dan HonkDocument9 pagesJurnal Kad Dan Honksimpati91No ratings yet
- BPTP - Lesson5 SiboDocument22 pagesBPTP - Lesson5 SiboLukasNo ratings yet
- Acid-Base Disturbance in a Man with Alcoholic Liver Disease and HypotensionDocument92 pagesAcid-Base Disturbance in a Man with Alcoholic Liver Disease and HypotensionManmeet SNo ratings yet
- Acid/Base and ABG Interpretation Made SimpleDocument45 pagesAcid/Base and ABG Interpretation Made SimpleekadtorNo ratings yet
- (OPTIMA) Pembahasan CBT To 2 Agustus 2020Document1,906 pages(OPTIMA) Pembahasan CBT To 2 Agustus 2020Rachel MadaiNo ratings yet
- Fish HandbookDocument61 pagesFish HandbookHooman AhmadianNo ratings yet
- DAHİLİYE'DETUS SORULARI Eng PDFDocument83 pagesDAHİLİYE'DETUS SORULARI Eng PDFKhalid ShafiqNo ratings yet
- Blood Gas Book Workbook 2008Document41 pagesBlood Gas Book Workbook 2008May Boonpeng100% (1)
- RTA Type 1 TreatmentDocument4 pagesRTA Type 1 TreatmentJane RamosNo ratings yet
- Hydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionDocument15 pagesHydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionElisha WorworNo ratings yet
- DocxDocument99 pagesDocxVanessa AbboudNo ratings yet
- Blood Gases, PH, & Buffer SystemsDocument51 pagesBlood Gases, PH, & Buffer SystemsDiether LanderoNo ratings yet
- Arterial Blood Gas InterpretationDocument65 pagesArterial Blood Gas InterpretationDaniel AryanNo ratings yet
- IONIX ModelDocument6 pagesIONIX ModelTrường Bửu TrầnNo ratings yet